Summary
A 50-year-old man in chemotherapy for an advanced lung adenocarcinoma presented with chest pain and cutaneous rash during carboplatin infusion with electrocardiographic (ECG) evidence of an inferior lesion wave. The administration of steroids and nitrates promptly resulted in clinical and ECG normalization, without enzymatic dismission. This reaction was considered compatible with allergic coronary vasospasm (also known as Kounis syndrome), a rare but possible complication of chemotherapy. In these cases prompt diagnosis and a correct approach can avoid useless invasive interventions.
Keywords: Carboplatin, Kounis, Vasospasm
Introduction
Cardiac damage cause caused by chemotherapy is a complex topic and its pathogenesis is still unclear. Here we report a case of coronary vasospasm caused by carboplatin hypersensitivity, a phenomenon never reported before in the literature.
Case report
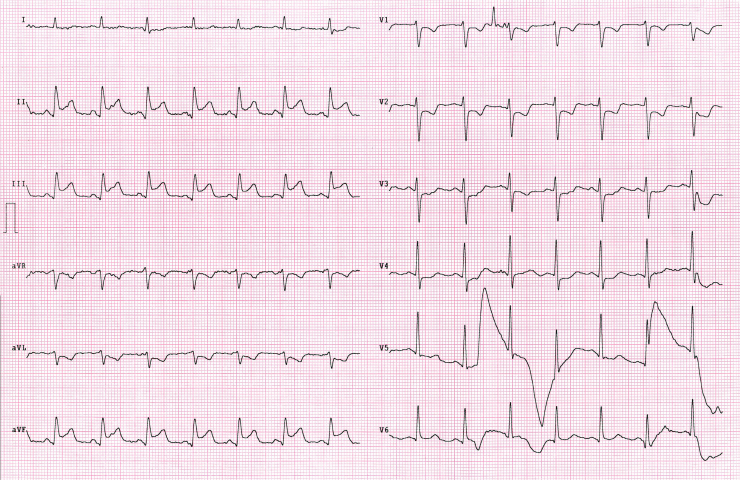
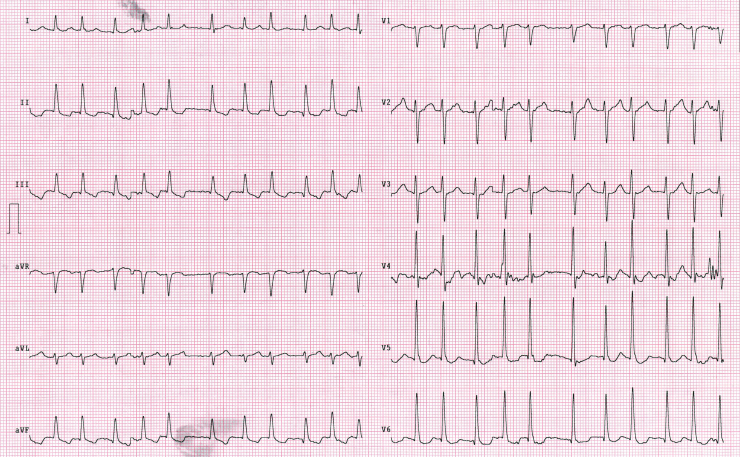
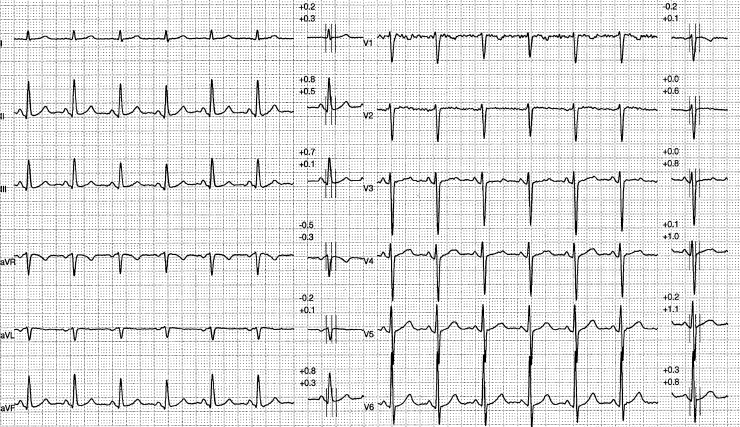
A 50-year-old man was admitted to the oncology department for the 6th cycle of chemotherapy for an inferior left lung adenocarcinoma, diagnosed four years previously. A few weeks after diagnosis he was subjected to pulmonary lobectomy, without evidence of lymphonodal involvement. In the third year of follow-up a technetium positron emission tomography examination showed hypercaptation in left hylar and subclavear lymph nodes with an increase in plasmatic carcinoembryonic antigen (CEA), and chemotherapy with carboplatin plus paclitaxel was initiated. The patient's family and clinical history were negative for cardiovascular disease, but he had smoked about 10 cigarettes per day for 30 years. His pharmacological history included a proton pump inhibitor (omeprazole). He stayed in hospital for two days on each of the first five cycles with a free interval of two weeks between doses. The basal electrocardiogram (ECG) at every admission was normal. During the 6th infusion of 450 mg of carboplatin in dextrose 5% he suffered intense chest pain and a diffuse cutaneous rash. An ECG performed during the pain (Fig. 1) showed a 2.5-mm ST segment elevation in inferior leads (II, III, aVF) with reciprocal ST depression in V1–V3. Before the arrival of the cardiologist a sublingual nitroglycerin tablet and 40 mg of metylprednisolone IV were administered, with prompt relief of symptoms and fast regression of the cuteneous rash. A second ECG (Fig. 2) performed 30 min later showed inversion of T waves in inferior leads with the onset of fast atrial fibrillation (140 bpm). Plasmatic values of troponin T, creatine kinase-MB, and myoglobin were not significant at 0, 6, and 12 h after the event. Arterial blood pressure maintained values above 100/60 mmHg. The patient refused further invasive procedures (e.g. coronary angiography) and requested hospital discharge the day after the event. Complete blood count showed only mild eosinophilia (5%) and neutrophilia (75%) with no abnormalities of other blood cells. Hepatic, electrolyte, creatine kinase, blood urea nitrogen, and creatine findings were normal. Total serum IgE was elevated (306 kU/L), but serum histamine and tryptase levels were not performed. Skin tests were not performed, due to the patient's refusal. An ECG before discharge (Fig. 3) showed normalization of T waves and spontaneous restoration of sinus rhythm. The patient was dismissed with aspirin therapy and did not refer to chest pain during a 6-month follow-up period. An ambulatory ECG stress test 2 months after the event was negative for ischemic ST-T alterations and an echocardiogram showed no alterations in systolic and diastolic function compared to a pre-event control. On that occasion, the repeated serum IgE level had returned to normal (80 kU/L) with no alterations in the blood count.
Figure 1.
Electrocardiogram during pain.
Figure 2.
Electrocardiogram after pain cessation.
Figure 3.
Electrocardiogram at discharge.
Discussion
Cardiac damage caused by antineoplastic agents has been frequently reported in the literature. Most chemotherapeutic drugs seem to be directly cardiotoxic and their harmful effects can cause several heart problems such as arrhythmias, left ventricular dysfunction, and ischemia. However, not all chemotherapeutics are directly correlated with cardiotoxicity and only a few of them have been associated with cardiac ischemia. There is strong clinical evidence [1] that some antimetabolic agents (capecitabine, 5-FU), antimicrotubular agents (paclitaxel, docetaxel), and tyrosine kinase inhibitors (sorafenib, bevaciuzmab) can cause cardiac ischemia, but their pathogenic mechanism is unknown. On the other hand, platinum compounds seem to be less cardiotoxic, but they are more frequently involved in hypersensitivity reactions [2].
Kounis syndrome, or allergic angina, was first described in 1991 as the coincidental occurrence of chest pain and allergic reaction accompanied by clinical and instrumental findings of classic angina pectoris [3]. At a later date, Kounis et al. [4] proposed a differentiation between two variants of the syndrome: the “Type I” in which coronary spasm occurs in normal vessels and may represent a manifestation of microvascular angina (such as X syndrome), and the “Type II” in which the allergic reaction seems to damage a previously quiescent atherosclerotic plaque, resulting in its rupture with the consequent “classic” acute coronary syndrome.
The pathogenesis of this phenomenon may be explained by an abnormal reaction of coronary smooth muscle to many inflammatory mediators. In particular, rapid mast cells’ degranulation (mainly IgE-mediated) that occurs during an anaphylactic reaction can cause the release of many inflammatory mediators such as histamine, neutral proteases, platelet activating factor, and arachidonic acid derivatives. All these compounds can induce coronary spasm, even in the absence of atherosclerotic plaques. Moreover, histamine can activate platelets and stimulate tissue factor expression causing a prothrombotic state [5].
In recent years, several cases of Kounis syndrome have been documented in the literature with a various range of allergic triggers, such as drugs, foods, and even insect bites. This phenomenon is probably underdiagnosed because often chest pain is not the main symptom referred to by the patient and consequently an ECG is not performed.
At present, only two cases of acute coronary syndrome with ST elevation induced by carboplatin have been reported, one with chest pain as the only clinical presentation [6] and the other with acute shock [7]. Both resolved in a short period and both cases with normal coronaries at angiography were presentations compatible with coronary vasospasm.
Neither of these cases presented with signs of an allergic reaction, as found in this patient (who had a massive cutaneous rash and ST elevation). Even if the patient declined angiographic examination, negative cycloergometric ECG stress test and echocardiogram were considered sufficient for the exclusion of major coronary artery stenosis. Considering all these elements, this case can be interpreted as the first one described in the literature of a complete manifestation of Kounis syndrome type I.
This report also suggests that a rapid search for hypersensitivity signs or symptoms (such as cutaneous rash, urticaria, asthma, etc.) should be done in patients with a new onset of angina and ST-elevation during chemotherapy and, most of all, an ECG should always be performed in patients with an important allergic reaction.
References
- 1.Yeh E.T., Tong A.T., Lenihan D.J., Yusuf S.W., Swafford J., Champion C., Durand J.B., Gibbs H., Zafarmand A.A., Ewer M.S. Cardiovascular complications of cancer therapy: diagnosis, pathogenesis, and management. Circulation. 2004;109:3122–3131. doi: 10.1161/01.CIR.0000133187.74800.B9. [DOI] [PubMed] [Google Scholar]
- 2.Pagani M. The complex clinical picture of presumably allergic side effects to cytostatic drugs. Med Clin North Am. 2010;94:835–852. doi: 10.1016/j.mcna.2010.03.002. [DOI] [PubMed] [Google Scholar]
- 3.Kounis N.G., Zavras G.M. Histamine-induced coronary artery spasm: the concept of allergic angina. Br J Clin Pract. 1991;45:121–128. [PubMed] [Google Scholar]
- 4.Nikolaidis L.A., Kounis N.G., Gradman A.H. Allergic angina and allergic myocardial infarction: a new twist on an old syndrome. Can J Cardiol. 2002;18:508–511. [PubMed] [Google Scholar]
- 5.Kounis N.G. Kounis syndrome (allergic angina and allergic myocardial infarction): a natural paradigm? Int J Cardiol. 2006;110:7–14. doi: 10.1016/j.ijcard.2005.08.007. [DOI] [PubMed] [Google Scholar]
- 6.Yano S., Shimada K. Vasospastic angina after chemotherapy by with carboplatin and etoposide in a patient with lung cancer. Jpn Circ J. 1996;60:185–188. doi: 10.1253/jcj.60.185. [DOI] [PubMed] [Google Scholar]
- 7.Chasen M.R., Ebrahim I.O. Carboplatin hypersensitivity presenting as coronary vasospasm—a case report. Cancer Chemother Pharmacol. 2002;50:429–431. doi: 10.1007/s00280-002-0518-3. [DOI] [PubMed] [Google Scholar]