Summary
Mitral annular calcification (MAC) is a common finding especially among the elderly. Caseous calcification of the mitral annulus (CCMA) is a rare variant of MAC, which may be mistaken for an intracardiac tumor or abscess. The clinical significance of CCMA and its potential as a source for cerebral embolism is not known.
A 76-year-old woman with an acute ischemic stroke was found to have CCMA on echocardiography apparent as a round mass with a central echolucent area and an echo-dense smooth border, in the periannular position of the mitral valve. She subsequently suffered a second embolic stroke. The central cavity of the CCMA seemed to communicate with the left atrium on echocardiography, suggesting the causal relationship between the second brain attack and the CCMA. She was anticoagulated and has not suffered any further strokes.
Previous case reports have suggested that CCMA is a benign condition. This detailed report suggests that CCMA may be a potential source of embolic stroke.
Keywords: Mitral annular calcification, Transthoracic echocardiography, Embolic stroke
Case report
A 76-year-old woman was admitted to National Cerebral and Cardiovascular Center after having the sudden onset of altered consciousness and quadriplegia. She had a history of controlled hypertension. On admission, her height, weight, and body temperature were 160 cm, 55 kg, and 36.1 °C, respectively. Her blood pressure was 192/96 mm Hg and heart rate 78 beats/min with regular rhythm. The electrocardiogram showed sinus rhythm, without any ST–T wave changes. Magnetic resonance imaging (MRI) of the brain showed new infarct lesions in the left thalamus and the cerebellum. Prompt treatment with intravenous recombinant tissue plasminogen activator (t-PA) and edaravone, a free radical scavenger, was associated with dramatic improvement in her neurological condition. The cerebral angiography on the next day showed severe atherosclerotic changes in the basilar artery. She was treated with clopidogrel, but no anticoagulant agent.
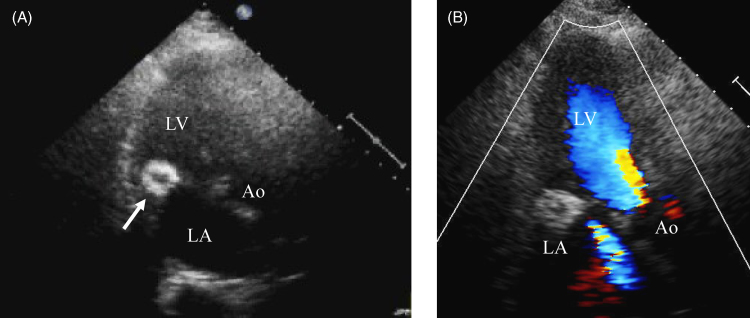
Transthoracic echocardiography showed a round mass with a central echolucent area and an echo-dense smooth border in the periannular position of the mitral valve (Fig. 1A). It appeared globular rather than cylindrical by scanning, without acoustic shadow. Mild mitral regurgitation was detected in color Doppler echocardiography, and no color Doppler flow was detected in the mass (Fig. 1B). We recognized the mass as caseous calcification of the mitral annulus (CCMA) and because of previous reports of its benign nature [1], [2], we did not believe it was the source of a cerebral embolus and did not administer anticoagulation therapy to the patient. No other potential sources of embolism were identified. The carotid artery Doppler echocardiography showed no stenosis or complex plaques.
Figure 1.
(A) Apical three-chamber view on initial transthoracic echocardiography. A round echo-dense mass with smooth borders (arrow) is seen in the posterior mitral annular region. (B) Doppler color-flow mapping of the initial echocardiography. Mild mitral regurgitation was detected. Ao, aorta; LA, left atrium; LV, left ventricle.
Her neurological condition steadily improved with rehabilitation. However, on the eighth day after admission, she suddenly developed worsening of dysarthria and right hemiparesis. Urgent MRI revealed new discrete frontal ischemic lesions in the left anterior cerebral artery area, not in the basilar area. It was most likely to be of cardiogenic embolic origin.
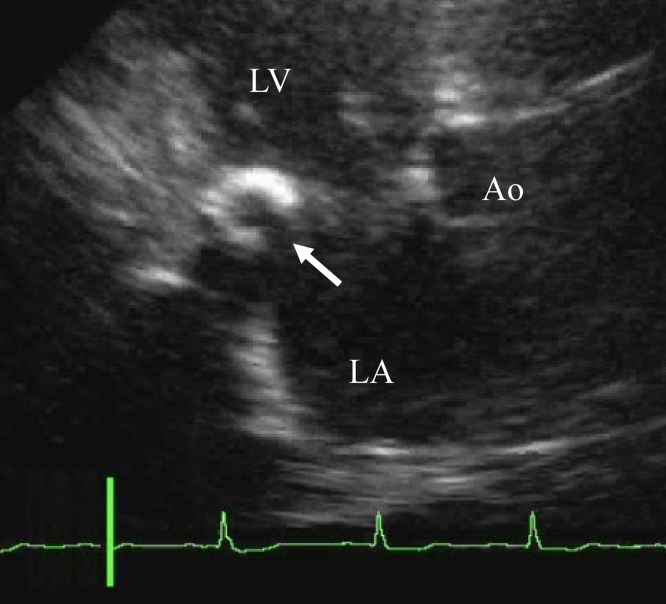
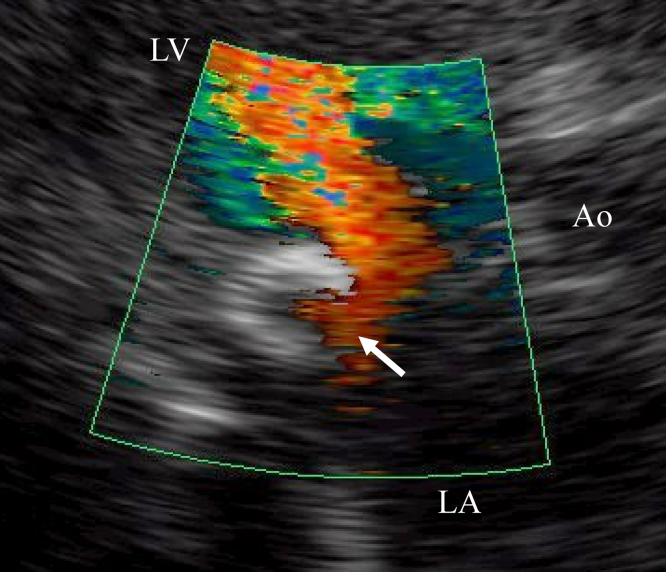
We were suspicious that the CCMA lesion might be the possible source of the embolism. The cavity of the CCMA communicated with the left atrium (Fig. 2). The echolucent area of the CCMA looked enlarged and the inward flow into the CCMA lesion in systole was apparent on the color Doppler flow (Fig. 3). The CCMA diminished in size in diastole, and enlarged in systole. This cyclic variation in the size of the mass was not prominent on the first echocardiogram. We administrated aspirin and low-molecular-weight dextran in addition to previous medication and started anticoagulant therapy with warfarin for stroke prevention. The patient improved gradually and was discharged. The follow-up echocardiography after 10 months showed no morphological change of CCMA. She has suffered no further strokes.
Figure 2.
Apical three-chamber view on transthoracic echocardiography after second attack. There is a partial deficit (arrow) on the rim of the caseous calcification of the mitral annulus. Ao, aorta; LA, left atrium; LV, left ventricle.
Figure 3.
Doppler color-flow mapping on transthoracic echocardiography after second attack. Inward flow into the caseous calcification of the mitral annulus (arrow) in systole was observed. Ao, aorta; LA, left atrium; LV, left ventricle.
Discussion
Although previous reports suggested that CCMA as a benign condition [1], [2], our patient indicates that CCMA may be the source of cerebral emboli.
Mitral annular calcification (MAC) is a common finding on transthoracic echocardiography reported to have some relation with stroke [3]. CCMA is a very rare variant observed in 0.06–0.07% of all echocardiographic examinations and 0.6–0.7% of all MACs [1], [2]. It is sometimes misdiagnosed as tumors, thrombi, or abscesses [4], [5], [6]. Several papers about the relationship between MAC and stroke have already been reported. However, those cases had an obviously morbid appearance; massively calcified [7], ulcerated [8], or accompanying mobile calcification with MAC [9]. On the other hand, although few reports mention the possibility that the CCMA could be a cause of stroke [10], caseous MAC has been considered as a benign lesion per se, despite its distinguished appearance [1], [2]. This is the first detailed report of a stroke apparently resulting from embolization from CCMA.
For several reasons, we believe that there was a causal relationship between the CCMA lesion and the brain infarction in our case. First, our patient's two strokes occurred in separate arterial distributions and there was no evidence of significant atherosclerosis in the anterior circulation. In addition the lesions were discrete and multiple. These findings suggested that the strokes were due to embolization. Second, the central cavity within the CCMA lesion communicates with the systemic circulation. A partial deficit of the echo-dense border of CCMA opened into the left atrium (Fig. 2). Color Doppler demonstrated that there was flow into the CCMA lesion in systole (Fig. 3). The CCMA changed in size with the cardiac cycle, enlarging in systole, shrinking in diastole. Considering that there was no other demonstrable embolic source, we believe that the CCMA lesion had a causal relationship with the brain infarction in our case.
Yasaka et al. reported a second cardioembolic stroke soon after t-PA administration for the first attack in a patient with intracardiac thrombi [11]. They proposed that t-PA accelerated breakup or detachment of the thrombi caused subsequent embolization. In analogy, in our case the t-PA might have degraded a clot associated with the CCMA.
The therapy for CCMA has not been established [1], [2]. We suggest that anticoagulant therapy for the brain attack with CCMA if there is no other cause of stroke. Even if there is another cause of infarction, careful examination about CCMA is warranted. If there was a communication between CCMA and systemic circulation, anticoagulant therapy should be prescribed even in the presence of other causes of stroke.
Acknowledgments
We wish to thank Dr. William C. Little for assistance in preparing the manuscript. This work was supported by grants from the Japan Cardiovascular Research Foundation.
References
- 1.Deluca G., Correale M., Ieva R., Del Salvatore B., Gramenzi S., Di Biase M. The incidence and clinical course of caseous calcification of the mitral annulus: a prospective echocardiographic study. J Am Soc Echocardiogr. 2008;21:828–833. doi: 10.1016/j.echo.2007.12.004. [DOI] [PubMed] [Google Scholar]
- 2.Harpaz D., Auerbach I., Vered Z., Motro M., Tobar A., Rosenblatt S. Caseous calcification of the mitral annulus: a neglected, unrecognized diagnosis. J Am Soc Echocardiogr. 2001;14:825–831. doi: 10.1067/mje.2001.111877. [DOI] [PubMed] [Google Scholar]
- 3.Benjamin E.J., Plehn J.F., D’Agostino R.B., Belanger A.J., Comai K., Fuller D.L. Mitral annular calcification and the risk of stroke in an elderly cohort. N Engl J Med. 1992;327:374–379. doi: 10.1056/NEJM199208063270602. [DOI] [PubMed] [Google Scholar]
- 4.Kato M., Nakatani S., Okazaki H., Tagusari O., Kitakaze M. Unusual appearance of mitral annular calcification mimicking intracardiac tumor prompting early surgery. Cardiology. 2006;106:164–166. doi: 10.1159/000092827. [DOI] [PubMed] [Google Scholar]
- 5.Kronzon I., Winer H.E., Cohen M.L. Sterile, caseous mitral annular abscess. J Am Coll Cardiol. 1983;2:186–190. doi: 10.1016/s0735-1097(83)80391-x. [DOI] [PubMed] [Google Scholar]
- 6.Stone E., Cohn D., Deal C., Pollock C. Calcific atrial mass in end-stage renal failure. Nephrol Dial Transplant. 1997;12:807–810. doi: 10.1093/ndt/12.4.807. [DOI] [PubMed] [Google Scholar]
- 7.Ridolfi R.L., Hutchins G.M. Spontaneous calcific emboli from calcific mitral annulus fibrosus. Arch Pathol Lab Med. 1976;100:117–120. [PubMed] [Google Scholar]
- 8.Lin C.S., Schwartz I.S., Chapman I. Calcification of the mitral annulus fibrosus with systemic embolization. A clinicopathologic study of 16 cases. Arch Pathol Lab Med. 1987;111:411–414. [PubMed] [Google Scholar]
- 9.Shohat-Zabarski R., Paz R., Adler Y., Vaturi M., Jortner R., Sagie A. Mitral annulus calcification with a mobile component as a possible source of embolism. Am J Geriatr Cardiol. 2001;10:196–198. doi: 10.1111/j.1076-7460.2001.00018.x. [DOI] [PubMed] [Google Scholar]
- 10.Davidson M.J., Cohn L.H. Surgical treatment of caseous mitral valve annulus calcification. J Thorac Cardiovasc Surg. 2006;131:738–739. doi: 10.1016/j.jtcvs.2005.11.025. [DOI] [PubMed] [Google Scholar]
- 11.Yasaka M., Yamaguchi T., Yonehara T., Moriyasu H. Recurrent embolization during intravenous administration of tissue plasminogen activator in acute cardioembolic stroke. A case report. Angiology. 1994;45:481–484. doi: 10.1177/000331979404500611. [DOI] [PubMed] [Google Scholar]