Summary
Despite developments in coronary interventional cardiology, plaque calcification is a critical issue of stent expansion. AngioSculpt Scoring Balloon Catheter® (AngioSculpt; AngioScore Inc., Fremont, CA, USA) can produce more ‘scoring’ marks, which leads to prevention of ‘plaque shift’ and ‘balloon slippage’; moreover, the ‘scoring’ produces some cutting effect, leading to successful stent implantation even on severe calcified lesions. We have applied AngioSculpt on severe calcified lesions to achieve its adequate expansion, and report the mechanism of the ‘scoring’ and its efficacy evaluated by three-dimensional stereoscopic reconstruction (3-D) of optical coherence tomography (OCT; LightLab Imaging, Inc., Westford, MA, USA). The patient is a 64-year-old male, who had diffuse stenosis in the left circumflex coronary artery (LCX) with severe calcifications, and was treated using AngioSculpt. AngioSculpt predilatation with a high pressure led to successful stent implantation. The radial scores were clearly imaged by 3-D OCT, demonstrating that radial nitinol wires made spiral indents from the relative weak points at the surface adjacent to calcification, which resulted in a less traumatic and safe dilatation although the scoring mark was not recognized clearly in intravascular ultrasound.
This report suggests AngioSculpt might become one of the options for a severe calcified lesion.
Keywords: AngioSculpt, Calcified lesion, Optical coherence tomography (OCT), Scoring, 3-D OCT
Introduction
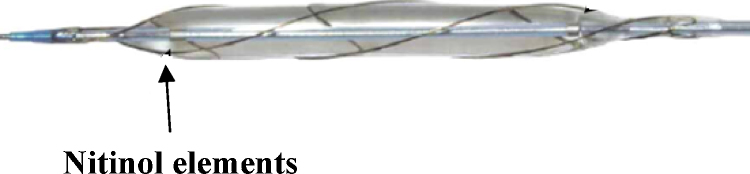
Despite recent remarkable advances in techniques and devices in coronary interventional cardiology, plaque calcification is still a critical hazard of stent expansion, causing infrequent restenosis and thrombosis. Histological and intravascular ultrasound (IVUS) observations have suggested that complex lesions especially with severe calcification frequently interfere with stent expansion. It has been recommended that an adequate prior preparation improves the clinical outcomes of stent implantation 1, 2. The AngioSculpt (AngioScore Inc., Fremont, CA, USA) was developed as a coronary interventional device, which consists of a semi-compliant balloon surrounded by spiral nitinol element that works in tandem with the balloon in order to ‘score’ the target lesion upon balloon inflation 1, 2 (Fig. 1). This device is designed to make a ‘scoring’ effect to complex lesions. As the balloon inflates, the spiral wires slide and rotate over the balloon, and the radial forces are concentrated along the surfaces of the nitinol element to achieve its fully open configuration, which is expected to lead to a reduction in critical coronary dissection and balloon slippage, and then allow higher inflation pressures when dealing with severely calcified lesions.
Figure 1.
The structure of AngioSculpt. The AngioSculpt consists of a semicompliant balloon surrounded by spiral nitinol element, the purposes of which are to dilate and make a ‘scoring’ effect to complex lesions.
The three-dimensional reconstruction of optical coherence tomography (3D-OCT) imaging was performed by a commercially available 3D-stereoscopic representation system (AVIZO 6.2 Visualization Sciences Group, Burlington, MA, USA). This user-friendly system could demonstrate a three-dimensional stereoscopic structure and mechanism of coronary expansion from various angles of view-point.
Therefore, we applied an AngioSculpt on a severely calcified lesion to achieve its adequate expansion and then 3D-OCT was performed to elucidate the mechanism of ‘score’ and its efficacy.
Case report
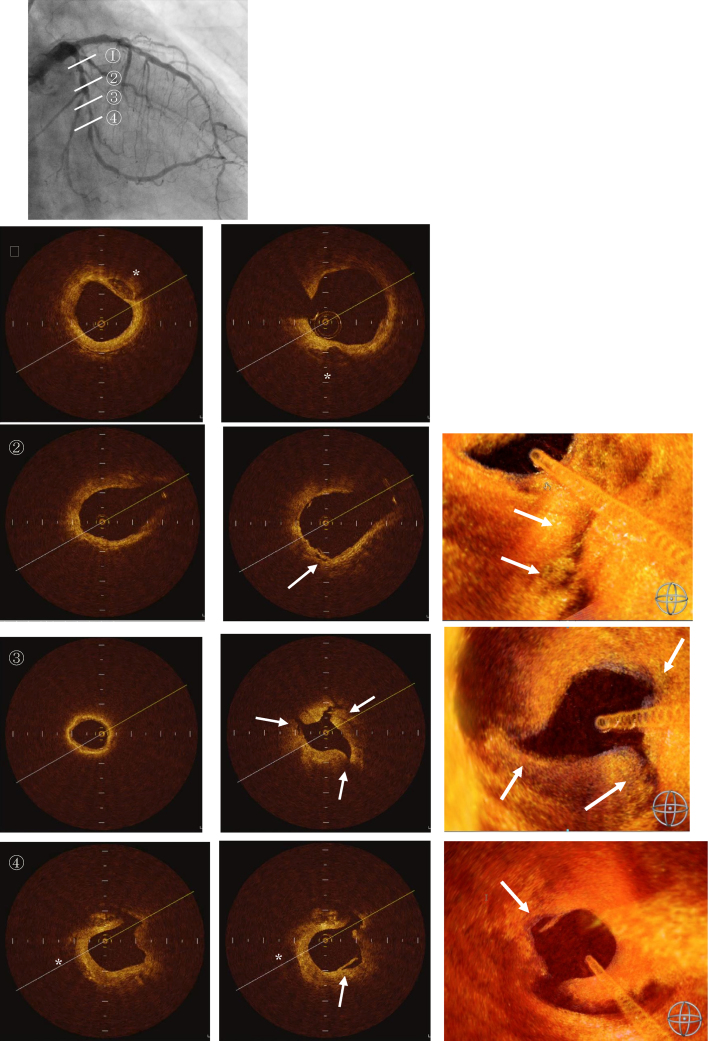
A 64-year-old male with a history of hypertension, diabetes mellitus, who had a plain ordinary balloon angioplasty in the left anterior descending artery (LAD) due to acute myocardial infarction in 1997, was admitted for his chest oppression on effort in April 2009. Coronary angiography (CAG) was performed, and revealed no re-stenosis in LAD but diffuse stenosis in the left circumflex artery (LCX) with localized severe calcification (Fig. 2). An elective percutaneous coronary intervention was planned and performed for the severely calcified lesion. IVUS observation was tried but could not be passed through the lesions; however, the OCT wire could be passed through the lesions in the LCX (Fig. 3). In the first balloon angioplasty, predilatation of the lesion with a Marverick balloon catheter® (2.5 mm/12 mm) (Boston Scientific Corporation, Minneapolis, MN, USA) was tried but it was not possible to achieve sufficient dilatation due to the severe calcification. Therefore, we applied AngioSculpt on the severely calcified lesion to achieve adequate expansion of the lumen for stent implantation. AngioSculpt (2.5 mm/10 mm) could be inserted through the target lesion. Then, predilatation with a high pressure was performed by this device, and sufficient coronary dilatation was achieved to result in successful stent implantation. In addition, the radial scoring marks by AngioSculpt could be detected by 3D-OCT (Fig. 3). The radial scores were clearly visualized by OCT/3D-OCT demonstrating that radial nitinol wires made spiral indents from the relatively weak points at the surface adjacent to calcification, which resulted in a less traumatic dilatation. As luminal diameter becomes smaller relative to the balloon size, the scoring marks seem to become bigger and deeper. The proximal portion of LCX thus had only a small exfoliation, whereas three distinct radial ‘scoring’ marks from the luminal surface into the vessel wall were observed having no unfavorable dissection at non-calcified segment. Finally, an efficient dilatation of the calcified plaque in the smaller calcified vessel at the distal potion of LCX lesion could be achieved (Fig. 3).
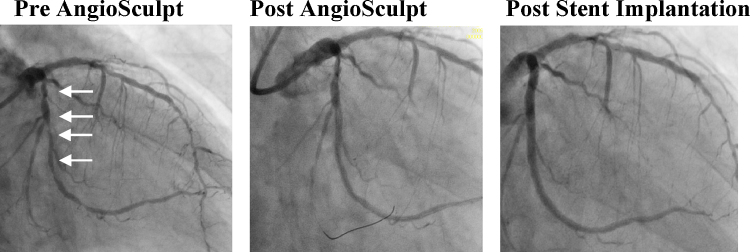
Figure 2.
Coronary angiograms are shown before and after the procedure of the AngioSculpt 2.5/10 mm for predilatation of left circumflex artery lesions (arrows), and after the stent implantation (TAXUS-Liberte® 3.0/28 mm, TAXUS-Liberte® 3.5/28 mm; Boston Scientific Corporation, Minneapolis, MN, USA).
Figure 3.
Two- and three-dimensional optical coherence tomography (OCT) images before and after AngioSculpt scoring. The OCT images before and after the procedure with AngioSculpt are presented, which correspond to the numbered section of angiogram of left circumflex artery. The panels of the same level of two-dimensional OCT images are in the same position (left: before scoring; right: after scoring). Three-dimensional representations of the OCT images around the lesions scored by this device are shown in the right panels. Severe calcifications are shown (*). Apparent ‘scoring’ marks can be observed (arrow ↑) having a safe dissection at non-calcified segment and an efficient dilatation of the calcified plaque.
After the dilatation by AngioSculpt, stents were successfully deployed with an adequate expansion but without an abrupt vessel closure, distal embolization, coronary dissection, nor coronary perforation.
Discussion
Encountering unexpected severely calcified lesions, some options are available as a prior preparation before stent implantation: (1) predilatation by a short high pressure balloon; (2) Cutting balloon; (3) Rotablator® (Boston Scientific Corporation); and (4) AngioSculpt. The short high pressure balloon might be ineffective not only for a long lesion but also for a spotty lesion because of the frequent likelihood of balloon slippage, although it is easier to use. The cutting balloon could prevent the balloon slippage and may be effective even for a calcified lesion, but it would burden a high risk for coronary perforation when predilatation is performed in high pressure. Currently, Rotablator® might be the most effective modification device; however, its procedure needs a complicated and specialized skill with expensive peripheral equipment. And the Rotablator® still has a relatively high prevalence of coronary perforation and no-reflow phenomenon. Compared to these options, the AngioSculpt seems to allow us to achieve safer- and higher-pressure expansion with some unique ‘cutting effect’ for a severely calcified lesion.
The mechanisms of conventional coronary balloon angioplasty are mainly divided into four areas, which are: (1) compression and disruption of plaque; (2) dissection of coronary plaque; (3) extension of coronary artery; and (4) axial extension of coronary plaque. In the case of severely calcified lesions, a major mechanism of coronary dilatation would be a dissection of coronary plaque due to restriction for the extension of coronary artery itself. Plain old balloon angioplasty sometimes causes a major dissection of vessel wall especially in severely calcified areas due to eccentric dilatation of the vessel wall. According to material physics, the tensile stress is preferably concentrated just at the edge of calcified mass, which is a frequent entry point of coronary wall dissection [3].
Takano et al. previously demonstrated the effect of the AngioSculpt on coronary plaque observed by OCT [4]; however, this is the first report showing its dilatation mechanism by the 3D-OCT especially for severely calcified wall. This analysis also proved a safe scoring and dilating mechanism of calcified lesion by the AngioSculpt.
AngioSculpt scoring balloon makes some scores intentionally, which prevents balloon slippage, plaque shift by balloon dilatation, and focal overstress at the balloon angioplasty. This device might also prevent the perforation and no-reflow phenomenon, since it would not crush or destruct calcified plaque. Therefore, lesions especially with large and longitudinal calcification, with a sharp edge prone to have excess stress concentration, and with adjacent mixed or complex lipid-rich components prone to have perforation or no-reflow phenomenon, might be suitable for this device. This would result in a successful dilatation of severely calcified coronary artery without critical dissection. OCT has an advantage over other imaging modalities for calcium assessment due to its ability for three-dimensional volumetric characterization. This would help in deciding appropriate lesions for using this device in the future.
In conclusion, the AngioSculpt might be one of the beneficial devices for lesion modification before stenting in severely calcified lesions to achieve sufficient lumen size. Further prospective study would be necessary to clarify suitable lesion morphology for this device and its clinical feasibility.
References
- 1.Moses J.W., Carlier S., Moussa I. Lesion preparation prior to stenting. Rev Cardiovasc Med. 2004;5(Suppl. 2):S16–S21. [PubMed] [Google Scholar]
- 2.Finet G., Weissman N.J., Mintz G.S., Satler L.F., Kent K.M., Laird J.R., Adelmann G.A., Ajani A.E., Castagna M.T., Rioufol G., Pichard A.D. Mechanism of lumen enlargement with direct stenting versus predilatation stenting: influence of remodelling and plaque characteristics assessed by volumetric intracoronary ultrasound. Heart. 2003;89:84–90. doi: 10.1136/heart.89.1.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fitzgerald P.J., Ports T.A., Yock P.G. Contribution of localized calcium deposits to dissection after angioplasty. An observational study using intravascular ultrasound. Circulation. 1992;86:64–70. doi: 10.1161/01.cir.86.1.64. [DOI] [PubMed] [Google Scholar]
- 4.Takano M., Yamamoto M., Murakami D., Takano H., Asai K., Yasutake M., Seino Y., Mizuno K. Optical coherence tomography after new scoring balloon angioplasty for in-stent restenosis and de novo coronary lesions. Int J Cardiol. 2010;141:e51–e53. doi: 10.1016/j.ijcard.2008.11.154. [DOI] [PubMed] [Google Scholar]