Summary
Although calcium channel blockers have been reported to aggravate Brugada-type electrocardiogram (ECG) abnormalities, there have been few reports in clinical settings. We present a case of Brugada syndrome coexisting with vasospastic angina, in whom Brugada-type ST-segment elevation was aggravated and ventricular fibrillation attacks occurred by calcium channel blocker treatment. When prescribing calcium channel blockers to patients with Brugada syndrome, it is important to pay careful attention to changes in their ECG pattern.
Keywords: Vasospastic angina, Brugada syndrome, Calcium channel blockers, Diltiazem, Ventricular fibrillation
Introduction
Brugada syndrome is one of the causes of sudden cardiac death, which is characterized by a peculiar electrocardiogram (ECG) pattern consisting of a pseudo-right bundle branch block and ST-segment elevation in leads V1 to V3. Vasospastic angina (VSA) can also cause sudden cardiac death [1], and the coexistence of Brugada syndrome and VSA has been reported previously [2], [3]. Calcium channel blockers (Ca blockers) are the first-choice drugs for treating VSA. Ca blockers have been reported to suppress lethal arrhythmia in patients with VSA [1]. On the other hand, Ca blockers, especially verapamil, have been reported to aggravate Brugada-type ECG abnormalities [4], [5], [6], [7], [8], [9], but there have been few reports [8], [9] in clinical settings. We report a patient in whom Brugada syndrome and VSA were found to coexist and in whom Brugada-type ST-segment elevation was aggravated and ventricular fibrillation (VF) attacks occurred by Ca blocker treatment.
Case report
A 39-year-old man was admitted to our hospital for further examination after successful resuscitation from cardiac arrest.
He had suffered convulsions and collapsed while sleeping early in the morning after drinking alcohol. After the arrival of the ambulance, an ECG monitor detected VF. The VF was successfully terminated via the application of a direct current shock with an automated external defibrillator. Soon after the patient's heartbeat had returned to sinus rhythm, an ECG monitor showed elevation of the ST-segment (Fig. 1A). He recovered without any neurological deficits and was referred to our department for further examinations of the cause of his cardiac arrest.
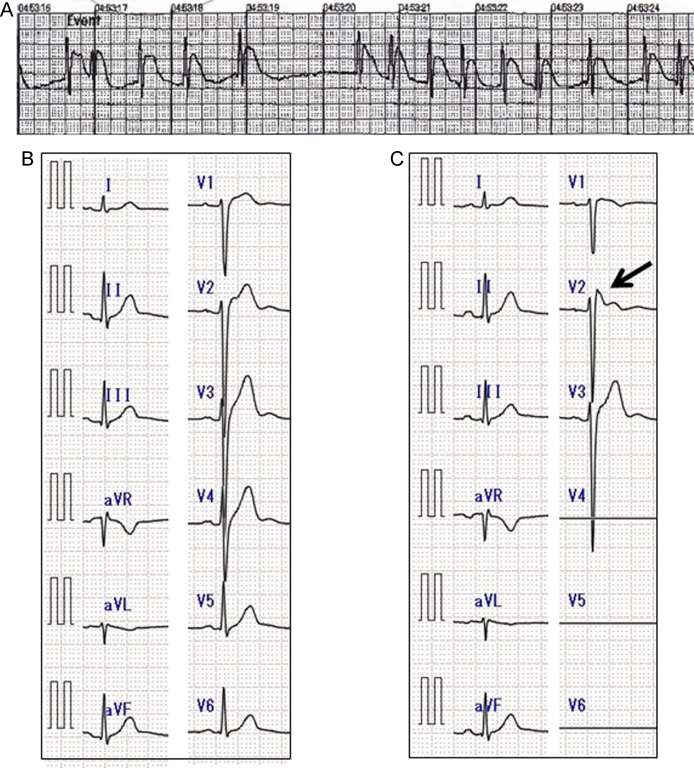
Figure 1.
An electrocardiogram (ECG) monitor after the termination of ventricular fibrillation (A) and 12-lead ECGs on admission (B, C). An ECG monitor (A) soon after recovery from cardiac arrest showed elevation of the ST-segment. A 12-lead ECG (B) showed no Brugada-type ST-segment elevation, but an ECG in high chest leads (C) revealed type 2 saddle back-type ST segment elevation in lead V2 (arrow).
He had no history of syncope or chest pain and no family history of sudden death. He had not been taking any drugs until the above event occurred.
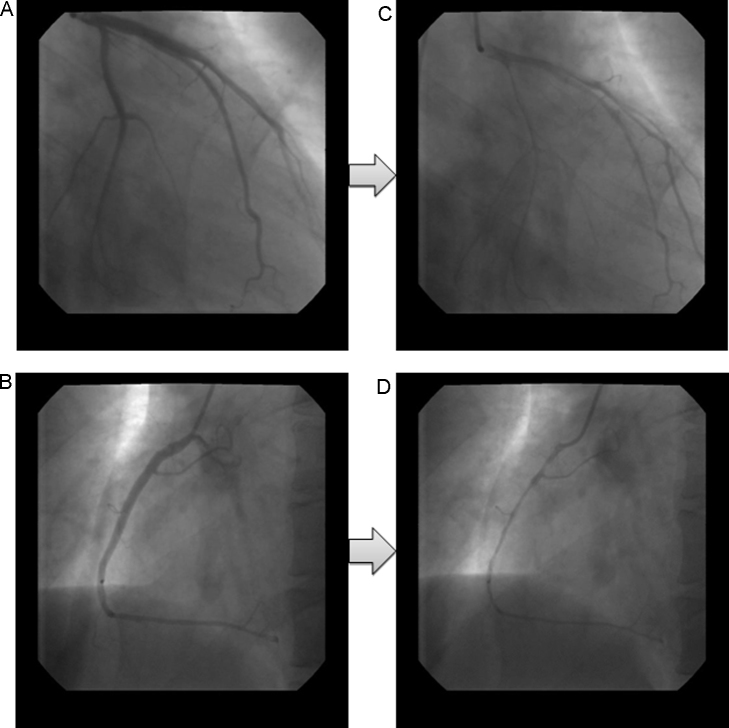
He was admitted to our hospital 11 days after being resuscitated. On admission, neither physical nor neurological abnormalities were observed. Laboratory analysis and chest X-rays were normal. Transthoracic echocardiograms showed a normal cardiac structure. A 12-lead ECG showed no Brugada-type ST-segment elevation, but an ECG in high chest leads revealed type 2 saddle back-type ST segment elevation in lead V2 (Fig. 1B, C). A Holter ECG showed no abnormalities, and treadmill exercise stress testing showed negative results for myocardial ischemia and the induction of arrhythmia. Late potential was negative in signal averaged ECG. We considered VSA as a differential diagnosis because the pattern of the 12-lead ECG did not match the typical Brugada ECG pattern and because cardiac arrest occurred early in the morning after drinking alcohol. Thus, cardiac catheterization was performed. A coronary angiogram showed no significant stenosis. Diffuse coronary spasms were induced in both the right and left coronary arteries by ergonovine maleate injection (Fig. 2), although they were not accompanied by significant ST-T changes. An electrophysiological study was performed. VF was not induced by the single, double, or triple extra-stimuli to the right ventricular apex and outflow tract. The intravenous injection of pilsicainide (50 mg) caused type 1 coved-type ST-segment elevation in the precordial leads.
Figure 2.
Coronary angiograms. A coronary angiogram showed no significant stenosis (A, B). Diffuse coronary spasms were induced in both the left (C) and right (D) coronary arteries by ergonovine maleate injection.
The patient met the diagnostic criteria for Brugada syndrome, and the coexistence of VSA was highly suspected. VSA has been reported to be accompanied by Brugada syndrome, both of which can cause VF. Therefore, an implantable cardioverter-defibrillator (ICD) was implanted as a treatment for his Brugada syndrome, and diltiazem (100 mg/day) was prescribed to treat his VSA.
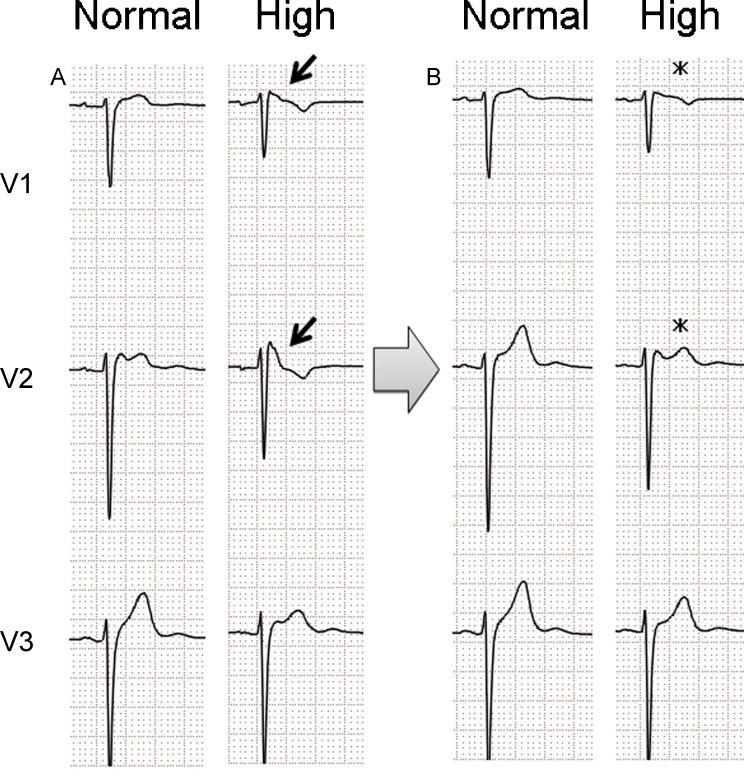
Two weeks after he had been discharged, the patient experienced seven ICD shocks while sleeping early in the morning. All episodes involved VF, and the ICD worked appropriately. An ECG monitor in the ICD showed no ST-segment changes before or after the VF attack. Follow-up ECG using the high chest leads showed type 1 coved-type ST-segment elevation (Fig. 3). According to experimental studies [4], [5], [6], Ca blockers have been reported to aggravate Brugada-type ST-segment elevation by decreasing the inward currents in the epicardium in a similar manner to sodium channel blockers. As there was a possibility that diltiazem had induced VF attacks in this case, its administration was discontinued and nitrate treatment was started. After the diltiazem had been discontinued, no further VF attacks occurred, and the type 1 coved-type ST-segment elevation disappeared (Fig. 3).
Figure 3.
Follow-up electrocardiograms (ECGs). After the diltiazem treatment was started (A), follow-up ECG in high chest leads showed type 1 coved-type ST-segment elevation in leads V1 and V2 (arrow). After the diltiazem treatment had been discontinued (B), the type 1 coved-type ST-segment elevation in leads V1 and V2 disappeared (asterisk). Normal, normal 12-lead ECG; High, ECG in high chest leads.
Discussion
This case was diagnosed as symptomatic Brugada syndrome from the patient's history of sudden cardiac arrest and type 1 coved-type ST-segment elevation in pilsicainide-induced ECG. On the other hand, the coexistence of VSA was suspected from the induction of diffuse coronary spasms in both the right and left coronary arteries by ergonovine maleate injection. Chinushi et al. [2] reported that the coexistence of VSA was recognized in 13.1% of patients with Brugada syndrome. Both Brugada syndrome and VSA can cause sudden cardiac death [1]. In addition, they also show other similarities; i.e. the incidences of the two diseases are high in relatively young men, and they are associated with an imbalance between sympathetic and parasympathetic tone, resulting in high incidence early in the morning. Therefore, in cases involving the coexistence of Brugada syndrome and VSA, it may be difficult to decide which of the two conditions is the direct cause of sudden cardiac arrest, resulting in treatments being administered for both as we did in this case.
The first-choice medication for VSA is Ca blockers, and we prescribed diltiazem (100 mg/day) in this case. Several experimental studies [4], [5], [6] have reported that Ca blockers, as well as other drugs such as sodium channel blockers, can aggravate Brugada-type ECG abnormalities and induce VF attacks. However, there are few reports [8], [9] about patients who showed aggravation of Brugada-type ECG and VF attacks with Ca blocker in clinical settings. According to a previous report [2], a low dose of Ca blockers neither worsens Brugada-type ECG abnormalities nor increases the frequency of VF attacks. However, the susceptibility to Ca blockers may differ among individuals [7], [10]. In our case, the dose of diltiazem (100 mg/day) used was the same as is applied in general clinical practice, but it aggravated the Brugada-type ECG abnormalities. Ca blockers work on both myocardium and smooth muscles of vessels. Verapamil works on the myocardium predominantly. According to a previous reports [2], [8], [9], we can recognize that verapamil can aggravate Brugada-type ECG abnormalities. Diltiazem is one of the antiarrhythmic drugs like verapamil and also has a strong effect on myocardium, therefore there was a possibility that the continuation of diltiazem treatment would have increased the risk of lethal arrhythmia. Diltiazem was discontinued, and treatment with a nitrate was started. It is well known that Brugada-type ECG abnormalities spontaneously fluctuate on a day-to-day basis and depend on the patient's condition. Therefore, it cannot be stated that diltiazem was directly related to the aggravation of ECG abnormalities or VF facilitation in this case. However, the patient's Brugada-type ST-segment elevation was alleviated and no VF attacks occurred after the diltiazem treatment was discontinued.
The present case suggests that when prescribing Ca blockers for patients with Brugada syndrome, we should recognize that lethal arrhythmia can be induced even with a dose of general clinical use and should perform careful follow-up to detect changes in the ECG pattern. When Brugada-type ECG abnormalities are aggravated after the start of treatment with Ca blockers, we have to consider changing the patient's medication.
References
- 1.Sovari A.A., Cesario D., Kocheril A.G., Brugada R. Multiple episodes of ventricular tachycardia induced by silent coronary spasm. J Interv Card Electrophysiol. 2008;21:223–226. doi: 10.1007/s10840-008-9207-4. [DOI] [PubMed] [Google Scholar]
- 2.Chinushi M., Furushima H., Tanabe Y. Similarities between Brugada syndrome and ischemia-induced ST segment elevation. Clinical correlation and synergy. J Electrocardiol. 2005;8:18–21. doi: 10.1016/j.jelectrocard.2005.06.004. [DOI] [PubMed] [Google Scholar]
- 3.Noda T., Shimizu W., Taguchi A., Satomi K., Suyama K., Kurita T., Aihara N., Kamakura S. ST-segment elevation and ventricular fibrillation without coronary spasm by intracoronary injection of acetylcholine and/or ergonovine maleate in patients with Brugada syndrome. J Am Coll Cardiol. 2001;40:1841–1847. doi: 10.1016/s0735-1097(02)02494-4. [DOI] [PubMed] [Google Scholar]
- 4.Morita H., Zipes D.P., Morita S.T., Wu J. Genotype–phenotype correlation in tissue models of Brugada syndrome simulating patients with sodium and calcium channelopathies. Heart Rhythm. 2010;7:820–827. doi: 10.1016/j.hrthm.2010.01.039. [DOI] [PubMed] [Google Scholar]
- 5.Fish J.M., Antzelevitch C. Role of sodium and calcium channel block in unmasking the Brugada syndrome. Heart Rhythm. 2004;1:210–217. doi: 10.1016/j.hrthm.2004.03.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yan G.X., Antzelevitch C. Cellular basis for the Brugada syndrome and other mechanisms of arrhythmogenesis associated with ST-segment elevation. Circulation. 1999;100:1660–1666. doi: 10.1161/01.cir.100.15.1660. [DOI] [PubMed] [Google Scholar]
- 7.Miyazaki T., Mitamura H., Miyoshi S., Soejima K., Aizawa Y., Ogawa S. Autonomic and antiarrhythmic modulation of ST segment elevation in patients with Brugada syndrome. J Am Coll Cardiol. 1996;27:1061–1070. doi: 10.1016/0735-1097(95)00613-3. [DOI] [PubMed] [Google Scholar]
- 8.Chinushi M., Iijima K., Tagawa M., Komura S., Furushima H., Aizawa Y. Effects of verapamil on anterior ST segments and ventricular fibrillation cycle length in patients with Brugada syndrome. J Electrocardiol. 2009;42:367–373. doi: 10.1016/j.jelectrocard.2009.03.009. [DOI] [PubMed] [Google Scholar]
- 9.Chinushi M., Tagawa M., Nakamura Y., Aizawa Y. Shortening of the ventricular fibrillatory intervals after administration of verapamil in a patient with Brugada syndrome and vasospastic angina. J Electrocardiol. 2006;39:331–335. doi: 10.1016/j.jelectrocard.2005.10.002. [DOI] [PubMed] [Google Scholar]
- 10.Vernooy K., Sicouri S., Dumaine R., Hong K., Oliva A., Burashnikov E., Timmermans C., Delhaas T., Crijns H.J.G.M., Antzelevitch C., Rodriguez L.M. Genetic and biophysical basis for bupivacaine-induced ST segment elevation and VT/VF. Anesthesia unmasked Brugada syndrome. Heart Rhythm. 2006;3:1074–1078. doi: 10.1016/j.hrthm.2006.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]