Summary
An isolated persistent left superior vena cava (PLSVC) with absent right superior vena cava is a rare and generally asymptomatic congenital malformation. It is usually discovered incidentally during a pacemaker implantation or electrophysiological procedures. We report an adult male who underwent successful dual chamber permanent pacemaker implantation through left subclavian approach with a 7-year follow-up showing a still appropriate function of the device. We discuss the technical issues and solutions to overcome such technical difficulties.
Keywords: Persistent left superior vena cava, Absent right superior vena cava, Permanent pacemaker implantation
Introduction
Persistent left superior vena cava (PLSVC) is the most common variation in the anomalous venous return to the heart and accounts for 0.2–4.3% of all congenital cardiac anomalies [1]. Associated absent right superior vena cava (RSVC) in an otherwise normal heart is an exceedingly rare anomaly [2]. These venous anomalies are usually asymptomatic and discovered incidentally during imaging and the aberrant position of a pacemaker lead, central venous catheters, or retrograde cardioplegia for cardiac surgery [3], [4].
Case report
In April 2004, a 54-year-old diabetic, hypertensive male was admitted to our institute with a history of recurrent pre-syncope, and one episode of syncope. He denied any history of shortness of breath or chest pain. He was using angiotensin-converting enzyme inhibitors for hypertension. Baseline electrocardiography showed left bundle branch block, without any evidence of coronary artery disease. The Holter monitoring revealed intermittent high-grade atrioventricular block (Mobitz type 2 block). Transthoracic echocardiography showed mildly dilated coronary sinus with no other structural heart disease.
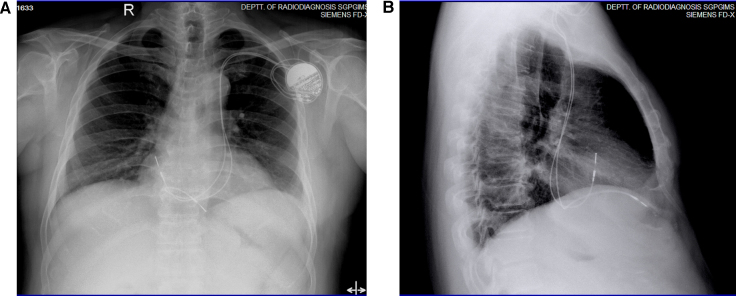
As he was left handed, we planned dual chamber permanent pacemaker implantation via right subclavian approach. To our surprise the wire instead of going on the right side of the spine went to the left side of the spine, indicating persistent left superior vena cava. A venography performed though bilateral antecubital vein revealed absent right superior vena cava and persistent left superior vena cava draining through the coronary sinus (CS) (Fig. 1).
Figure 1.
Simultaneous bilateral subclavian venogram showing absent right superior vena cava (SVC) with persistent left SVC draining into dilated coronary sinus (CS).
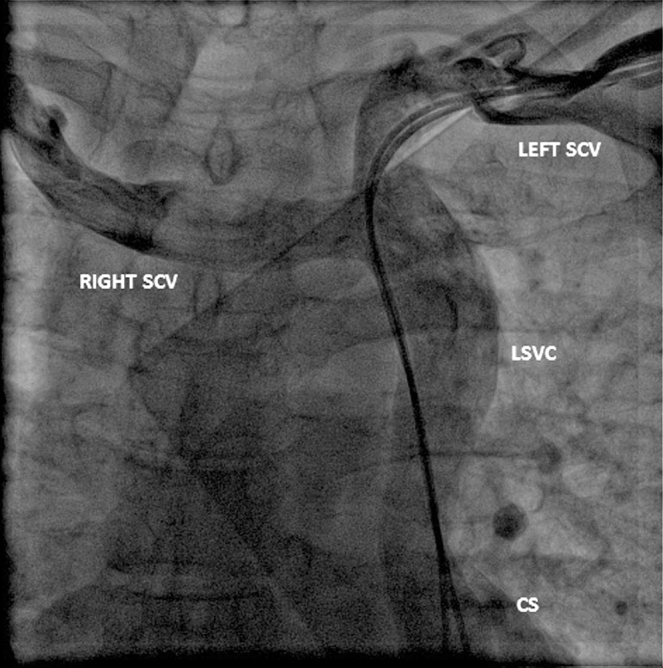
Considering the anticipated technical difficulties, we decided to switch access site to the left subclavian vein approach. A 58 cm tined ventricular (Vitatron-ICM09B, Maastricht, The Netherlands) lead was introduced into the right atrium (RA) via a dilated CS. From there the lead was not crossing the tricuspid valve, so it was pushed into the right ventricle (RV) by making a loop against the lateral wall of the RA. The stylet was shaped into a semicircle which facilitated entry into the RV. The lead was positioned near the RV apex and the position was confirmed in lateral projection of fluoroscopy. Care was taken to form an adequate loop in the RA to prevent dislodgement. A similar lead (58 cm tined ventricular lead, Vitatron-ICM09B) was taken for atrial pacing. This lead was positioned into the RA appendage with little manipulation after entering via the CS (Fig. 2A and B). Both leads showed excellent parameters (threshold of 0.5 mV each and resistance less than 650 Ω). A dual chamber pacemaker (Vitatron VITA2DDD730) was connected to the leads and placed in a deep pocket and the wound was closed in layers.
Figure 2.
Chest radiograph in AP (Panel A) and lateral (Panel B) projections showing both atrial and ventricular pacing leads in respective chambers attaining odd positions.
After 6 weeks of implantation, the patient was asymptomatic and pacemaker interrogation showed no major changes in parameters. For the past 7 years he is under regular follow-up and recent examination in August 2011 showed excellent sustained parameters. Follow-up fluoroscopy showed stable position of pacing leads and venogram done through simultaneous contrast injection into bilateral antecubital veins showed patent bilateral subclavian veins draining to persistent LSVC joining dilated CS.
Discussion
Persistent LSVC demonstrates several congenital variations including variable communication with right-sided superior vena cava (SVC), absence of right-sided SVC, drainage into the left atrium creating a right to left shunt, and association with other congenital heart defects. Persistent LSVC, especially in the absence of right-sided SVC, may be associated with a variety of other congenital malformations of the heart and great vessels, therefore appropriate investigations should be undertaken. Its association with atrial septal defect, bicuspid aortic valves, or coarctation of the aorta in Turner syndrome, left isomerism of the heart, CS ostial atresia, cor triatrium, and several other malformations are well recognized [5]. However, our patient had isolated venous anomaly and detailed clinical examination and echocardiographic study did not reveal any extracardiac or intracardiac defects.
Isolated persistent LSVC is usually not recognized until left cephalic or subclavian approach is used for diagnostic and therapeutic transcatheter procedures. Transvenous procedures, via left subclavian approach, such as right heart catheterization, pacemaker, or implantable cardiovertor-defibrillator (ICD) implantation, biventricular pacing, and electrophysiological assessment may be complicated by technical difficulties in accessing the right ventricle in the presence of a persistent LSVC. Transvenous introduction of a lead from the right atrium to the right ventricle, through the CS, may become a technically demanding procedure in subjects with persistent LSVC, especially when the bridging innominate vein or right SVC is absent as seen in our patient [5].
The technical difficulties associated with persistent LSVC may lead to misplacement of catheter and injury to the vessel wall. Despite their associated complications, the presence of a persistent LSVC does not necessarily prevent successful placement of a pacemaker or ICD lead [4].
PLSVC with absent RSVC is a special problem of transvenous pacing causing great difficulty in manipulation and stability of pacing leads. Placement of ventricular leads may be difficult as it takes acute angle after coming out of CS to cross the tricuspid valve, and to reach the RV apex. Various approaches have been advocated by some authors including epicardial pacing [6]. There are reports of successful implantation of ICDs as well as biventricular pacing [7], [8]. Permanent pacemaker implantation is found to be feasible even in small children with good results [9].
We preferred tined ventricular lead for RV lead and felt that the tined lead could be held in position by coarse trabeculation and safe long-term pacing has been demonstrated in this situation [10]. The difficulty in entering the RV was overcome with careful shaping of the stylet. It seems to be very difficult to place a regular atrial lead because of its shape. Several authors have reported use of active fixation lead in this situation [11], [12]. But the use of an active fixation lead is not always without danger [13]. So we preferred to choose a regular 58 cm tined ventricular lead as an atrial electrode and fixed it in an atrial appendage ensuring an adequate sustained push against the RA wall. In view of the abnormal anatomy, initially this patient was followed up at regular intervals and at 7 years follow-up the pacemaker parameters were found to be normal with phlebography revealing patent bilateral subclavian veins and LSVC.
Conclusion
A PLSVC associated with an absent RSVC is a very rare congenital malformation most commonly discovered incidentally. With an increase in the number of pacemakers and ICDs being implanted worldwide, this challenging situation is expected to be encountered more frequently. Pre-procedural phlebography is extremely useful to identify these silent venous anomalies and to determine precisely the pathway to the right atrium. Even though permanent pacemaker implantation through CS via PLSVC is technically demanding it gives good long-term results as observed in our case. However, these patients need frequent follow-up during the initial period.
References
- 1.Campbell M., Deuchar D.C. The left-sided superior vena cava. Br Heart J. 1954;16:423–439. doi: 10.1136/hrt.16.4.423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mooney D.P., Snyder C.L., Holder T.M. An absent right and persistent left superior vena cava in an infant requiring extracorporeal membrane oxygenation therapy. J Pediatric Surg. 1993;28:1633–1634. doi: 10.1016/0022-3468(93)90125-5. [DOI] [PubMed] [Google Scholar]
- 3.Chan K.L., Abdulla A. Images in cardiology. Giant coronary sinus and absent right superior vena cava. Heart. 2000;83:704. doi: 10.1136/heart.83.6.704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Biffi M., Boriani G., Frabetti L., Bronzetti G., Branzi A. Left superior vena cava persistence in patients undergoing pacemaker or cardioverter-defibrillator implantation: a 10-year experience. Chest. 2001;120:139–144. doi: 10.1378/chest.120.1.139. [DOI] [PubMed] [Google Scholar]
- 5.Ratliff L.H., Yousufuddin M., Lieving R.W., Watson E.B., Malas A., Rosencrance G., McCowan J.R. Persistent left superior vena cava: case reports and clinical implications. Int J Cardiol. 2006;113:242–246. doi: 10.1016/j.ijcard.2005.08.067. [DOI] [PubMed] [Google Scholar]
- 6.Lenox C.C., Zuberbuhler J.R., Park S.C., Neches W.H., Mathews R.A., Fricker F.J., Bahnson H.T., Siewers R.D. Absent right superior vena cava with persistent left superior vena cava: implication and management. Am J Cardiol. 1980;45:117–122. doi: 10.1016/0002-9149(80)90228-3. [DOI] [PubMed] [Google Scholar]
- 7.Beukema R.J., Elvan A., Beukema W.P., Misier A.R.R., Delnoy P.P.H.M., Luttikhuis H.A., Hoorntje J.C. Cardioverter defibrillator implantation in a patient with absent right superior vena cava. Neth Heart J. 2006;14:255–257. [PMC free article] [PubMed] [Google Scholar]
- 8.Gasparini M., Mantica M., Galimberti P., Coltorti F., Simonini S., Ceriotti C., Gronda E. Biventricular pacing via a persistent left superior vena cava: report of four cases. PACE. 2003;26:192–196. doi: 10.1046/j.1460-9592.2003.00015.x. [DOI] [PubMed] [Google Scholar]
- 9.Dalili M., Alizadeh A., Haghjoo M. Successful implantation of transvenous pacing system via persistent left superior vena cava and coronary sinus in small children. Ind Pacing Electrophysiol J. 2010;10:552–555. [PMC free article] [PubMed] [Google Scholar]
- 10.Zerbe P., Bornakowowaski J., Sarnowaski W. Pacemaker electrode implantation in patient with persistent left superior vena cava. Br Heart J. 1992;67:65–66. doi: 10.1136/hrt.67.1.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Roberts D.H., Belllamy C.M., Ramsdale D.R. Implantation of a dual chamber pacemaker in a patient with persistent left superior vena cava. Int J Cardiol. 1992;36:242–243. doi: 10.1016/0167-5273(92)90017-w. [DOI] [PubMed] [Google Scholar]
- 12.Zardo F., Nicolosi G.L., Burelli C., Zanuttini D. Dual chamber transvenous pacemaker implantation via anomalous left superior vena cava. Am Heart J. 1986;112:621–622. doi: 10.1016/0002-8703(86)90534-x. [DOI] [PubMed] [Google Scholar]
- 13.Van Nooten G., Verbeet T., Deuvaert F.E. Atrial perforation by a screw-in electrode via a left superior vena cava. Am Heart J. 1990;119:1439–1440. doi: 10.1016/s0002-8703(05)80206-6. [DOI] [PubMed] [Google Scholar]