Abstract
Objective:
To examine how cognitive and motor limitations in children with heart disease are associated with education and participation in extracurricular activities.
Design:
Using 2009–2010 parent-reported data from the National Survey of Children with Special Health Care Needs (NS-CSHCN), we examined prevalence of five functional limitations (learning/ concentration, communication, self-care, gross motor skills, and fine motor skills) by diagnosed heart disease status using chi-square tests and multivariable logistic regression. Among CSHCN with heart disease, we examined the associations between severity of each functional limitation and missing ≥11 days of school in the past year, receiving special education services, and interference with extracurricular activities.
Results:
CSHCN with heart disease (n = 1,416), compared to CSHCN without (n = 28,385), more commonly had “a lot” of difficulty in the five functional areas (P < .01; adjusted odds ratios: 1.8–3.3). Among CSHCN with heart disease, “a lot” of difficulty with learning/concentration was most common (35%), followed by communication (21%), self-care (14%), gross motor skills (12%), and fine motor skills (10%). Among CSHCN with heart disease, compared to those without, respectively, 27% and 15% missed ≥11 days of school, 45% and 29% received special education services, and 49% and 29% experienced interference with extracurricular activities (P < .01 for all). Level of difficulty with the five functional areas was associated with receipt of special education services and participation in extracurricular activities (P < .001).
Conclusion:
These results support the American Heart Association recommendations to screen children with congenital heart disease for age-appropriate development and provide services when needed.
Keywords: congenital heart defect, congenital heart disease, intellectual disability, motor skills, school absenteeism, special education
1 |. INTRODUCTION
Recent studies have documented that children with congenital heart disease (CHD) have a higher prevalence of cognitive and motor limitations compared to their peers.1–5 Additionally, children with CHD are more likely to receive special education services3,6,7 and are at higher risk for grade retention.8 The etiology of these limitations is most likely multifactorial and may be due to genetic or chromosomal abnormalities, abnormalities in fetal brain development secondary to altered cerebral circulation in utero,9 as well as perioperative factors including single ventricle physiology, hospital length of stay, and duration of cardiopulmonary bypass.4,7,10
Less is known about how functional limitations experienced by school-aged children and adolescents with CHD may affect their education and participation in extracurricular activities.11 There are few population-based estimates of the percentage of children and adolescents with CHD who experience functional limitations or need special education services.2,3,6,7 Therefore, using the National Survey of Children with Special Health Care Needs (NS-CSHCN) we examined the prevalence of functional limitations among children with special healthcare needs (CSHCN) with diagnosed heart problems, including CHD. While this sample of children may include those with congenital and acquired heart disease, in the general population, the prevalence of congenital heart disease (1 in 110 at birth, with an estimated 85%–90% surviving into adulthood),12,13 far exceeds that of acquired heart disease (3 in 10,000 for rheumatic heart disease14 to <1 in 100,000 for infective endocarditis15) In particular, we focused on whether children with heart disease have more functional limitations in regard to learning/concentration, communication, self-care, gross motor skills, and fine motor skills compared to CSHCN without heart problems. Additionally, we sought to evaluate whether these functional limitations were associated with school attendance, receipt of special education services, and participation in extracurricular activities.
2 |. METHODS
The 2009–2010 NS-CSHCN is a population-based survey of U.S. children ages 0–17 years with special healthcare needs conducted by the National Center for Health Statistics (https://www.cdc.gov/nchs/slaits/cshcn.htm). The NS-CSHCN used a complex sampling strategy with random-digit dialing of both landline and cell phones to contact households in the 50 states and the District of Columbia. The survey is cross-sectional and children are not followed over time. Parents or guardians (hereafter referred to as parents) were asked a series of five questions about whether a child in the household used prescription medicine, had more healthcare encounters than other children their age, had limitations compared to other children their age, needed physical, occupational, or speech therapy, and/or had an emotional, developmental or behavioral problem in need of counseling or treatment. If the parent answered “yes” to any one of the five questions above, the parent was asked two additional questions on whether the specific healthcare need arose from a medical, behavioral, or other health condition and whether that condition had lasted or is expected to last 12 months or longer. If the parent answered “yes” to both of the two additional questions, then the child was considered to have a special healthcare need and was eligible for inclusion in NS-CSHCN. If more than one CSHCN resided in the household, the interviewer would randomly select one child as the focus of the interview.
A parent of a CSHCN was asked whether his/her child has ever been diagnosed with “a heart problem, including congenital heart disease,” excluding “harmless or innocuous heart murmurs” (yes/no). A “heart problem” may include both congenital and acquired heart diseases, as well as syndromes affecting the heart. CHD has a birth prevalence of about 1 per 110 children,12 while acquired heart diseases, such as rheumatic heart disease,14 Kawasaki disease,16 cardiomyopathy,17 and infective endocarditis,15 all have prevalence estimates between 3 per 10,000 to <1 per 100,000, and 22q11.2 deletion syndrome, 1 in 4,000 (https://ghr.nlm.nih.gov/). We hereafter refer to these children as having “heart disease.”
Parents were also asked whether their child’s condition(s) “affects his/her ability to do things other children do,” and about whether the child “experiences a lot, a little, or no difficulty” with “learning, understanding, or paying attention” (learning/concentration), “speaking, communicating, or being understood” (communication), “taking care of him/ herself” (self-care), “coordination” (gross motor skills), and “using his/ her hands” (fine motor skills). In addition, parents with children aged 5 years and older were asked the number of school days the child missed in the past year (dichotomized as <11 and ≥11 days as a marker of absenteeism affecting school performance),18 whether the child needed special education services, and whether the child’s condition interfered with his/her ability to participate in sports, clubs, or other organized activities. Demographic characteristics included the child’s sex, age, race/ethnicity, and type of health insurance, whether the child has a medical home, parental marital status, the highest educational level of any household member, and family income as a percent of the federal poverty level. A CSHCN was considered to have a medical home if he/she met all five of the following medical home criteria as defined by the American Academy of Pediatrics: 1) having a personal doctor or nurse, 2) having a usual source for sick and well care, 3) receipt of family-centered care, 4) no problems getting needed referrals, and 5) receipt of effective care coordination when needed.19
We limited this analysis to children aged 6–17 years because some 5-year-olds have not reached school age. Among children 6–17 years, we examined differences in demographic characteristics by heart disease status. Among the same groups, we examined differences in the ability to do things other children do and the five functional limitations listed above using chi-square tests and multinomial logistic regression. Among CSHCN with heart disease, we examined differences in days of school missed in the past year, receipt of special education services, and interference with extracurricular activities, by level of difficulty with functional area. In sensitivity analyses, we excluded individuals with Down syndrome and, separately, we stratified analyses by age group (6–9, 10–13, 14–17 years) because type of heart disease and functional limitations may differ by age. All analyses were conducted in SUDAAN to account for complex sampling design and weighted to provide population-based estimates.
3 |. RESULTS
In the 2009–2010 NS-CSHCN, there were 32,948 CSHCN aged 6–17 years; extrapolating to the general population this would represent 8.8 million CSHCN. Of those sampled, 32,916 (99.9%) had information on heart disease and 29,801 (90.5%) had information on functional limitations, educational outcomes, and demographic characteristics of interest. CSHCN excluded from the analysis due to missing data, compared to those included, were more likely to be Hispanic, lower income, from less well-educated households, insured publicly or uninsured, have unmarried parents, and have difficulty with learning/concentration and communication (P < .05 for all). The analytic sample comprised 1,416 CSHCN with heart disease (5.0%; representing 400,000 U.S. CSHCN) and 28,385 CSHCN without heart disease (95.0%; representing 7.5 million U.S. CSHCN). Down syndrome was reported by 130 CSHCN with heart disease (7.3%) and 149 CSHCN without heart disease (0.5%).
The majority of CSHCN with heart disease were non-Hispanic white (62%), had private insurance (60%), had a family member with more than a high school education (67%), had married parents (61%), and did not have a medical home (64%). CSHCN with heart disease, compared to those without, respectively, were more commonly female (48.6% and 39.9%) and less likely to have a medical home (35.9% and 43.2%) than CSHCN without heart disease (chi-square P-value <.05 for both). Age, race/ethnicity, household income as a percent of the federal poverty level, child’s insurance coverage, highest educational level in household, and parental marital status did not differ between CSHCN with heart disease and those without (chi-square P-value .05 for all).
A larger percentage of CSHCN with heart disease, compared to those without, respectively, had parents who said their child’s condition(s) always (27% and 14%) or usually (14% and 10%) affected his/ her ability to do things other children their age do (P < .001; Figure 1). CSHCN with heart disease, compared to those without, had parents who said their child more commonly had “a lot” of difficulty in the five functional areas (P < .01; Figure 2). Among CSHCN with heart disease, “a lot” of difficulty with learning/concentration was most common (35%), followed by communication (21%), self-care (14%), gross motor skills (12%), and fine motor skills (10%).
FIGURE 1.
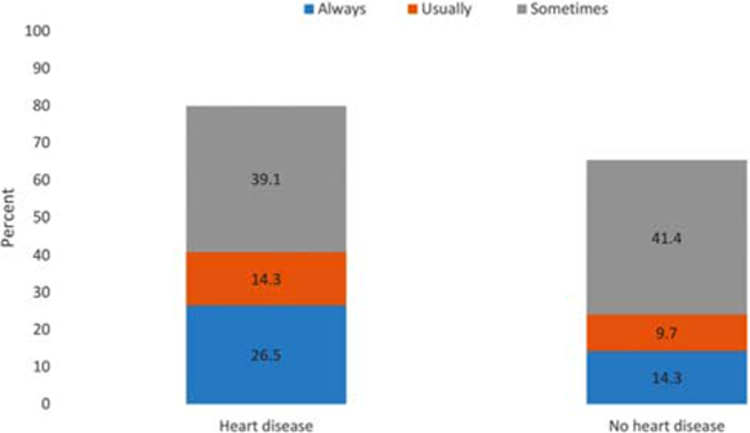
Frequency of the ability to do things other children do, by heart disease status, among children with special healthcare needs aged 6–17 years, National Survey of Children with Special Health Care Needs, 2009–2010
FIGURE 2.
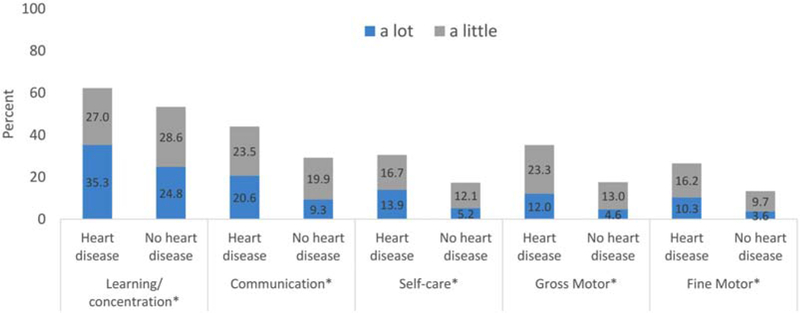
Difficulty in functional area, by heart disease status, among children with special healthcare needs aged 6–17 years, National Survey of Children with Special Health Care Needs, 2009–2010
In all age groups, having heart disease was associated with not being able to do things other children do, although this association was strongest among those aged 14–17 years. Among CSHCN aged 6–9 years and 10–13 years, respectively, those with heart disease, compared to those without, had 3.0 (95% CI: 1.8, 4.9) and 2.0 (95% CI: 1.2, 3.4) times the odds of their condition always affecting their ability to do things other children do (Table 1). In CSHCN aged 14–17 years, those with heart disease, compared to those without, had 5.1 times the odds (95% CI: 3.2, 8.0) of their condition always affecting their ability to do things other children do. Age group did not modify the associations with the five functional areas. Among all age groups combined, CSHCN with heart disease, compared to those without, had 1.8 to 3.3 times the odds of having “a lot” of difficulty with all five functional areas, and 1.5 to 2.2 times the odds of having “a little” difficulty for four of the five functional areas (communication, self-care, fine motor skills, and gross motor skills). Excluding individuals with Down syndrome from the models lowered the magnitude of point estimates slightly but did not affect the direction or statistical significance of the associations (data not shown).
TABLE 1.
Functional limitations by heart disease among children with special healthcare needs aged 6–17 years, National Survey of Children with Special Health Care Needs, 2009–2010
| Adjusted odds ratioa | 95% Confidence interval | |
|---|---|---|
| Condition(s) affect ability to do things other children do | ||
| 6–9 year-olds | ||
| Always | 3.0 | 1.8, 4.9 |
| Usually | 2.3 | 1.2, 4.2 |
| Sometimes | 1.3 | 0.9, 2.0 |
| Never | 1.0 | |
| 10–13 year-olds | ||
| Always | 2.0 | 1.2, 3.4 |
| Usually | 2.2 | 1.2, 4.2 |
| Sometimes | 1.3 | 0.9, 2.1 |
| Never | 1.0 | |
| 14–17 year-olds | ||
| Always | 5.1 | 3.2, 8.0 |
| Usually | 3.2 | 1.8, 5.8 |
| Sometimes | 2.4 | 1.6, 3.6 |
| Never | 1.0 | |
| 6–17 year-olds | ||
| Difficulty with learning/concentration | ||
| A lot | 1.8 | 1.4, 2.3 |
| A little | 1.2 | 0.9, 1.5 |
| None | 1.0 | |
| Difficulty with communication | ||
| A lot | 2.8 | 2.1, 3.7 |
| A little | 1.5 | 1.2, 2.0 |
| None | 1.0 | |
| Difficulty with self-care | ||
| A lot | 3.1 | 2.2, 4.3 |
| A little | 1.7 | 1.3, 2.1 |
| None | 1.0 | |
| Difficulty with gross motor | ||
| A lot | 3.2 | 2.3, 4.5 |
| A little | 2.2 | 1.8, 2.8 |
| None | 1.0 | |
| Difficulty with fine motor | ||
| A lot | 3.3 | 2.3, 4.7 |
| A little | 2.1 | 1.6, 2.7 |
| None | 1.0 |
Adjusted for sex, age, race/ethnicity, % federal poverty level, health insurance, highest level education of any household member, marital status, having a medical home.
Among CSHCN with heart disease, 27% missed ≥11 days of school in the past 12 months, 45% received special education services, and 49% experienced interference with participation in extracurricular activities (Table 2); these percentages were significantly higher than those among CSHCN without heart disease (15%, 29%, and 29%, respectively, P < .01 for all). Level of difficulty with learning/concentration, self-care, gross motor skills, and fine motor skills was associated with missing ≥11 days of school (P < .05 for all); among CSHCN with heart disease who had “a lot” of difficulty in these four functional areas, 36% to 46% reported missing ≥11 days of school, compared to 20% to 24% of CSHCN with heart disease who had no difficulty. Level of difficulty with communication was not statistically associated with missing ≥11 days of school. Level of difficulty in the five functional areas was associated with receipt of special education services (P <.0001 for all). Among CSHCN with heart disease who had “a lot” of difficulty with the five functional areas, 70% to 83% received special education services, compared to 15% to 34% of CSHCN with heart disease who had no difficulty. Level of difficulty in the five functional areas was associated with interference with extracurricular activities (P <.01 for all). Among CSHCN with heart disease who had “a lot” of difficulty with the five functional areas, 62% to 80% experienced interference with participation in extracurricular activities, compared to 38% to 44% of CSHCN with heart disease who had no difficulty (P <.001 for all). Neither excluding the 279 CSHCN with Down syndrome from the analysis nor stratifying by age group affected prevalence estimates for missed school days, receipt of special education services, or participation in extracurricular activities.
TABLE 2.
School attendance, special education needs, and interference with extracurricular activities overall and by functional limitations among children with special healthcare needs with heart disease, aged 6–17 years, National Survey of Children with Special Health Care Needs, 2009–2010
| Days of school missed in past 12 months N = 1,394a |
Received special education services N = 1,407b |
Condition interferes with extracurricular activities N = 1,407 |
||||
|---|---|---|---|---|---|---|
| ≥11 Weighted % (95% CI) |
<11 Weighted % (95% CI) |
Yes Weighted % (95% CI) |
No Weighted % (95% CI) |
Yes Weighted % (95% CI) |
No Weighted % (95% CI) |
|
| Total | 27.0 (23.1, 31.2) | 73.0 (68.8, 76.9) | 44.7 (40.1, 49.5) | 55.3 (50.5, 60.0) | 49.2 (44.5, 53.9) | 50.8 (46.1, 55.5) |
| Difficulty with | ||||||
| self-carec,d,e | ||||||
| A lot | 37.2 (26.0, 50.0) | 62.8 (50.0, 74.0) | 77.2 (64.1, 86.5) | 22.9 (13.5, 35.9) | 72.1 (56.0, 83.9) | 28.0 (16.1, 44.0) |
| A little | 34.1(24.5, 45.3) | 65.9 (54.7, 75.5) | 68.1 (57.3, 77.3) | 31.9 (22.8, 42.7) | 59.4 (49.3, 68.9) | 40.6 (31.1, 50.7) |
| None | 23.2 (18.8, 28.2) | 76.8 (71.8, 81.2) | 32.5 (27.3, 38.3) | 67.5 (61.7, 72.7) | 42.1 (36.6, 47.8) | 57.9 (52.2, 63.4) |
| Gross motorc,d,e | ||||||
| A lot | 46.2 (32.2, 60.9) | 53.8 (39.2, 67.8) | 83.4 (74.1, 89.8) | 16.6 (10.2, 25.9) | 77.5 (60.6, 88.5) | 22.5 (11.5, 39.4) |
| A little | 33.8 (25.3, 43.4) | 66.2 (56.6, 74.7) | 57.0 (47.6, 65.9) | 43.0 (34.1, 52.4) | 66.6 (57.2, 74.8) | 33.5 (25.2, 42.8) |
| None | 21.0 (16.7, 26.1) | 79.0 (74.0, 83.4) | 33.0 (27.6, 39.0) | 67.0 (61.0, 72.4) | 37.6 (32.0, 43.6) | 62.4 (56.4, 68.0) |
| Fine motorc,d,e | ||||||
| A lot | 42.5 (28.8, 57.4) | 57.5 (42.6, 71.2) | 82.9 (71.9, 90.2) | 17.1 (9.8, 28.1) | 80.4 (67.4, 89.1) | 19.6 (10.9, 32.6) |
| A little | 28.9 (20.2, 39.5) | 71.1 (60.6, 79.8) | 68.6 (57.4, 78.0) | 31.4 (22.0, 42.6) | 61.6 (50.7, 71.4) | 38.4 (28.6, 49.3) |
| None | 24.4 (19.9, 29.4) | 75.7 (70.6, 80.1) | 34.0 (28.8, 39.7) | 66.0 (60.3, 71.2) | 42.0 (36.6, 47.6) | 58.0 (52.4, 63.4) |
| Learning or concentrationc,d,e | ||||||
| A lot | 36.3 (28.9, 44.4) | 63.7 (55.6, 71.1) | 70.1 (61.7, 77.3) | 29.9 (22.7, 38.3) | 62.4 (53.8, 70.2) | 37.6 (29.8, 46.2) |
| A little | 24.7 (17.7, 33.3) | 75.3 (66.7, 82.3) | 52.6 (44.1, 60.9) | 47.4 (39.1, 56.0) | 42.0 (33.9, 50.5) | 58.1 (49.5, 66.1) |
| None | 19.8 (14.8, 25.9) | 80.2 (74.1, 85.2) | 15.2 (10.2, 21.9) | 84.9 (78.1, 89.8) | 41.9 (34.8, 49.5) | 58.1 (50.5, 65.2) |
| Communicationd,e | ||||||
| A lot | 35.0 (25.4, 45.9) | 65.1 (54.1, 74.6) | 79.3 (68.2, 87.2) | 20.8 (12.8, 31.8) | 67.8 (56.8, 77.1) | 32.2 (22.9, 43.2) |
| A little | 26.2 (18.9, 35.2) | 73.8 (64.8, 81.1) | 63.6 (53.4, 72.7) | 36.4 (27.4, 46.6) | 45.5 (35.8, 55.6) | 54.5 (44.5, 64.2) |
| None | 24.3 (19.5, 29.8) | 75.7 (70.2, 80.5) | 23.8 (19.0, 29.4) | 23.8 (19.0, 29.4) | 43.8 (38.0, 49.8) | 56.2 (50.2, 62.0) |
Abbreviation: CI, Confidence interval.
Limited to children who attend school outside of the home.
Limited to children who attend school or are home-schooled.
P < .05 for chi-square association with ≥11 days of school missed in past 12 months.
P < .0001 for chi-square association with received special education services.
P < .001 for chi-square association with interference with extracurricular activities.
4 |. DISCUSSION
This is the first population-based study to our knowledge on functional limitations, educational needs and participation in extracurricular activities among school-aged CSHCN with diagnosed heart disease. We found that for 40% of CSHCN with heart disease, their condition always or usually prevented them from doing things other children do, and CSHCN with heart disease experienced a greater level of difficulty with learning/concentration, communication, self-care, gross and fine motor skills than CSHCN without heart disease. CSHCN with heart disease also missed more days of school, more commonly received special education services, and participated less in extracurricular activities than CSHCN without heart disease. Among CSHCN with heart disease, these outcomes were more common among those with functional limitations. While a large percentage of CSHCN with heart disease and functional limitations received special education services, up to 30% with “a lot” of difficulty in one or more functional areas reported not receiving special education services. It is unknown what percentage of children in this sample have CHD, acquired heart disease, or syndromes affecting the heart, but based on published population estimates, the large majority likely have CHD.
These parent-reported results on functional limitations are consistent with previous literature, based on results of assessment tools and validated questionnaires, which report a higher level of cognitive and motor limitations among children with CHD.5,8,11,20,21 While some studies,8,22 but not all,11,20 have found intelligence is generally within the normal range for individuals with CHD, studies show that executive functioning, problem solving, memory, and attention are impaired more often in children and adolescents with CHD as compared to healthy population controls5,8,21–25 and siblings.20 Researchers have found delayed language development in toddlers with CHD,10 compared to population means, which might be due to decreased brain white matter volume.26 Delays in gross and fine motor development have also been reported more commonly in toddlers23,27,28 and young children29 with CHD compared to healthy controls, siblings/twins, and population norms. Delays in motor skills have been associated with longer cumulative hospital stays,29 younger gestational age at birth,8 univentricular CHD anatomy,28 and genetic or extracardiac anomalies.23 Additionally, functional limitations among individuals with CHD seem to persist into adulthood, with reported increased prevalence of cognitive difficulties as well as deficits in visuospatial skills and working memory.30,31 Adults with more severe CHD are also more likely to be unemployed and receive disability benefits.30 Of the limited published studies on associations between acquired heart diseases, specifically Kawasaki disease, and cognition and attention disorders, none found statistically significant associations.32,33 Heart-related syndromes, such as 22q11.2 deletion syndrome, are associated with a higher risk of developmental delays, learning disabilities, attention deficit hyperactivity disorder, and autism spectrum disorder (https://ghr.nlm.nih.gov).
Children with CHD, compared to those without, are also more likely to receive special education services,3,6–8 have lower academic achievement scores,7,34 and report more school absenteeism.2 However, less is known about how functional limitations are associated with educational outcomes.35,36 In a study of 148 children and adolescents with d-transposition of the great arteries, tetralogy of Fallot, or single-ventricle CHD requiring a Fontan surgical procedure, patients reported decreased metacognition (working memory and organization of tasks) and more behavioral problems than the general population, with decreased metacognition predicting poor school performance; an association that was strongest for older adolescents.11 Similarly, our results also showed that disparities in being able to do things other children do may increase with age. As children with CHD age, cognitive deficits and functional limitations may become more apparent37 and lead to lower physical and psychosocial quality of life.38,39 However, interventions shown effective among other CSHCN, such as structured computerized training programs, mindfulness training, occupational therapy, aerobic exercise,35 and special education services may prevent or mitigate functional limitations in children with heart disease and improve educational and social outcomes.
There are several limitations in the current analysis. All information is based on parent report; however, parent report of children’s medical conditions has been shown to correlate well with medical record data in one study.40 As stated earlier, “diagnosed heart problem” is a heterogeneous group, comprised of children with congenital and acquired heart problems and syndromes, the percentages of which in our parent-reported data are unknown. However, the prevalence of congenital heart disease (1 in 110 at birth, with an estimated 85%–90% surviving into adulthood),12,13 far exceeds that of acquired heart diseases (prevalence of 3 in 10,000 for rheumatic heart disease,14 incidence of 21/100 000 for Kawasaki disease, and incidence of <1 in 100 000 for infective endocarditis15) Therefore, the sample is likely largely children with CHD. These results are generalizable to CSHCN only, and not to all children with heart disease. Additionally, we excluded 10% of the eligible individuals due to missing data, and heart disease status did not differ among individuals included and excluded from the analysis. Additionally, the results did not change substantially when excluded individuals were included in unadjusted models. Finally, CSHCN with heart disease, compared to those without, were more commonly female and less likely to have a medical home. We adjusted for these differences in multivariable models. Even with the limitations above, this analysis is one of the first to examine the U.S. prevalence of functional limitations among school-aged CSHCN with diagnosed heart disease and their associations with school absenteeism, receipt of special education services, and participation in extracurricular activities.
5 |. CONCLUSION
Our results show that CSHCN with diagnosed heart disease experience more functional limitations and educational challenges than CSHCN without heart disease. These results support the American Heart Association recommendation to screen children with CHD for age-appropriate development, starting early in life and continuing through-out school age and adolescence, and provide preventive and/or therapeutic services for those in need.4
ACKNOWLEDGMENTS
The authors thank Dr. Nancy McClung for replicating the analysis and Ms. Aspen Riser for reviewing final results.
Funding Information
N/A; All work was done as part of employment with the U.S. federal government
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Footnotes
CONFLICTS OF INTEREST
The authors have no conflicts of interest or financial relationships relevant to this article to disclose.
REFERENCES
- [1].Snookes SH, Gunn JK, Eldridge BJ, et al. A systematic review of motor and cognitive outcomes after early surgery for congenital heart disease. Pediatrics 2010;125(4):e818–e827. [DOI] [PubMed] [Google Scholar]
- [2].Razzaghi H, Oster M, Reefhuis J. Long-term outcomes in children with congenital heart disease: National Health Interview Survey. J Pediatr 2015;166(1):119–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Oster ME, Watkins S, Hill KD, Knight JH, Meyer RE. Academic outcomes in children with congenital heart defects: a population-based cohort study. Circ Cardiovasc Qual Outcomes 2017;10(2):e003074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Marino BS, Lipkin PH, Newburger JW, et al. Neurodevelopmental outcomes in children with congenital heart disease: evaluation and management: a scientific statement from the American Heart Association. Circulation 2012;126(9):1143–1172. [DOI] [PubMed] [Google Scholar]
- [5].Cassidy AR, White MT, DeMaso DR, Newburger JW, Bellinger DC. Executive function in children and adolescents with critical cyanotic congenital heart disease. J Int Neuropsychol Soc 2015;21(01):34–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Riehle-Colarusso T, Autry A, Razzaghi H, et al. Congenital heart defects and receipt of special education services. Pediatrics 2015; 136(3):496–504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Mulkey SB, Bai S, Luo C, et al. School-age test proficiency and special education after congenital heart disease surgery in infancy. J Pediatr 2016;178:47–54.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Sarrechia I, Miatton M, De Wolf D, et al. Neurocognitive development and behaviour in school-aged children after surgery for univentricular or biventricular congenital heart disease. Eur J Cardiothorac Surg 2016;49(1):167–174. [DOI] [PubMed] [Google Scholar]
- [9].Khalil A, Suff N, Thilaganathan B, Hurrell A, Cooper D, Carvalho JS. Brain abnormalities and neurodevelopmental delay in congenital heart disease: systematic review and meta-analysis. Ultrasound Obstet Gynecol 2014;43(1):14–24. [DOI] [PubMed] [Google Scholar]
- [10].Mussatto KA, Hoffmann R, Hoffman G, et al. Risk factors for abnormal developmental trajectories in young children with congenital heart disease. Circulation 2015;132(8):755–761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Gerstle M, Beebe DW, Drotar D, Cassedy A, Marino BS. Executive functioning and school performance among pediatric survivors of complex congenital heart disease. J Pediatr 2016;173:154–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Hoffman JI, Kaplan S. The incidence of congenital heart disease. J Am Coll Cardiol 2002;39(12):1890–1900. [DOI] [PubMed] [Google Scholar]
- [13].Moons P, Bovijn L, Budts W, Belmans A, Gewillig M. Temporal trends in survival to adulthood among patients born with congenital heart disease from 1970 to 1992 in Belgium. Circulation 2010;122 (22):264–2272. [DOI] [PubMed] [Google Scholar]
- [14].Carapetis JR, Steer AC, Mulholland EK, Weber M. The global burden of group A streptococcal diseases. Lancet Infect Dis 2005;5(11):685–694. [DOI] [PubMed] [Google Scholar]
- [15].Hoen B, Duval X. Infective endocarditis. N Engl J Med 2013;369(8): 785. [DOI] [PubMed] [Google Scholar]
- [16].Burns JC, Kushner HI, Bastian JF, et al. Kawasaki disease: A brief history. Pediatrics 2000;106(2):E27. [DOI] [PubMed] [Google Scholar]
- [17].Lee TM, Hsu DT, Kantor P, et al. Pediatric Cardiomyopathies. Circ Res 2017;121(7):855–873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].National Quality Measures Clearinghouse (NQMC). Measure summary: Missed school days: number of school days that children missed in the past 12 months due to illness or injury. In: National Quality Measures Clearinghouse (NQMC) [Web site]. Rockville (MD: ): Agency for Healthcare Research and Quality (AHRQ); 2013. April 01 [cited 2017 Jun 23]. Available: https://qualitymeasures.ahrq.gov. [Google Scholar]
- [19].Medical Home Initiatives for Children With Special Needs Project Advisory Committee. American Academy of Pediatrics. The medical home. Pediatrics 2002;110(1):184–186. [PubMed] [Google Scholar]
- [20].Murphy LK, Compas BE, Reeslund KL, et al. Cognitive and attentional functioning in adolescents and young adults with tetralogy of Fallot and d-transposition of the great arteries. Child Neuropsychol 2017;23(1):99–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Sanz JH, Berl MM, Armour AC, Wang J, Cheng YI, Donofrio MT. Prevalence and pattern of executive dysfunction in school age children with congenital heart disease. Congenit Heart Dis 2017;12(2): 202–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Bergemann A, Hansen JH, Rotermann I, et al. Neuropsychological performance of school-aged children after staged surgical palliation of hypoplastic left heart syndrome. Eur J Cardiothorac Surg 2015;47 (5):803–811. [DOI] [PubMed] [Google Scholar]
- [23].Gaynor JW, Stopp C, Wypij D, et al. Neurodevelopmental outcomes after cardiac surgery in infancy. Pediatrics 2015;135(5): 816–825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Bellinger DC, Wypij D, Rivkin MJ, et al. Adolescents with d-transposition of the great arteries corrected with the arterial switch procedure: neuropsychological assessment and structural brain imaging. Circulation 2011;124(12):1361–1369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Bellinger DC, Rivkin MJ, DeMaso D, et al. Adolescents with tetralogy of Fallot: neuropsychological assessment and structural brain imaging. Cardiol Young 2015;25(02):338–347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Rollins CK, Asaro LA, Akhondi-Asl A, et al. White Matter Volume Predicts Language Development in Congenital Heart Disease. J Pediatr 2017;181:42–48 e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Long SH, Galea MP, Eldridge BJ, Harris SR. Performance of 2-year-old children after early surgery for congenital heart disease on the Bayley Scales of Infant and Toddler Development, Third Edition. Early Hum Dev 2012;88(8):603–607. [DOI] [PubMed] [Google Scholar]
- [28].Sananes R, Manlhiot C, Kelly E, et al. Neurodevelopmental outcomes after open heart operations before 3 months of age. Ann Thorac Surg 2012;93(5):1577–1583. [DOI] [PubMed] [Google Scholar]
- [29].Brosig CL, Bear L, Allen S, et al. Preschool neurodevelopmental outcomes in children with congenital heart disease. J Pediatr 2017; 183:80–86.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Ilardi D, Ono KE, McCartney R, Book W, Stringer AY. Neurocognitive functioning in adults with congenital heart disease. Congenit Heart Dis 2017;12(2):166–173. [DOI] [PubMed] [Google Scholar]
- [31].Tyagi M, Austin K, Stygall J, Deanfield J, Cullen S, Newman SP. What do we know about cognitive functioning in adult congenital heart disease? Cardiol Young 2014;24(01):13–19. [DOI] [PubMed] [Google Scholar]
- [32].Kuo HC, Chang WC, Wang LJ, Li SC, Chang WP. Association of attention deficit hyperactivity disorder and Kawasaki disease: a nationwide population-based cohort study. Epidemiol Psychiatr Sci 2016;25(06):573–580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Wang LJ, Kuo HC. Cognitive development after Kawasaki disease-clinical study and validation using a nationwide population-based cohort. Circ J 2018;82(2):517–523. [DOI] [PubMed] [Google Scholar]
- [34].Mulkey SB, Swearingen CJ, Melguizo MS, et al. Academic proficiency in children after early congenital heart disease surgery. Pediatr Cardiol 2014;35(2):344–352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Calderon J, Bellinger DC. Executive function deficits in congenital heart disease: why is intervention important? Cardiol Young 2015; 25(07):1238–1246. [DOI] [PubMed] [Google Scholar]
- [36].Calderon J, Bonnet D, Pinabiaux C, Jambaque I, Angeard N. Use of early remedial services in children with transposition of the great arteries. J Pediatr 2013;163(4):1105–1110.e1. [DOI] [PubMed] [Google Scholar]
- [37].Calderon J Executive function in patients with congenital heart disease: only the tip of the iceberg? J Pediatr 2016;173:7–9. [DOI] [PubMed] [Google Scholar]
- [38].Bertoletti J, Marx GC, Hattge SP, Pellanda LC. Health-related quality of life in adolescents with congenital heart disease. Cardiol Young 2015;25(03):526–532. [DOI] [PubMed] [Google Scholar]
- [39].Uzark K, Zak V, Shrader P, et al. Assessment of quality of life in young patients with single ventricle after the Fontan operation. J Pediatr 2016;170:166–172 e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Porter SC, Forbes P, Manzi S, Kalish LA. Patients providing the answers: narrowing the gap in data quality for emergency care. Qual Saf Health Care 2010;19(5):e34. [DOI] [PubMed] [Google Scholar]


