Abstract
Communities across the U.S. are implementing programs and policies designed to address the epidemic of childhood obesity. These programs vary widely in their approaches, including the intensity level, duration, funding, target population, and implementation techniques. However, no previous studies have examined these variations and determined how such aspects of community programs and policies are related to childhood obesity outcomes. The Healthy Communities Study is an observational study that is assessing the associations between characteristics of community programs and policies and BMI, nutrition, and physical activity in children. The Healthy Communities Study was funded in 2010, field data collection and medical record abstraction will be completed in 2015, and data cleaning and analyses will be completed by mid-year 2016. One-hundred and thirty communities (defined as a high school catchment area) and up to 81 children in kindergarten through eighth grade and their parents have been recruited from public elementary and middle schools across the country. The study is examining quantitative and qualitative information obtained from community-based initiatives; measures of community characteristics (e.g., school environment); and child and parent measures, including children's physical activity levels and dietary practices and children's and parent's BMI. The Healthy Communities Study employs a complex study design that includes a diverse sample of communities across the country and combines current/cross-sectional and retrospective data (abstracted from children's medical records). This paper describes the rationale for the Healthy Communities Study, the study aims and logic model, and a brief overview of the study design.
Introduction
Childhood obesity has increased dramatically over the past 30 years, although obesity rates have begun to stabilize in recent years.1 Little information is known about the factors responsible for the stabilization of rates during the last decade. Communities across the U.S. have implemented programs and policies designed to reduce childhood obesity, but the characteristics of these programs and policies that may have played a role in the stabilization of rates is unknown. Understanding the role of community programs and policies in reducing childhood obesity is an important public health issue that warrants further study.2
Although national data suggest that the prevalence of obesity may have stabilized among most children, and even decreased for those aged !5 years, overall prevalence remains high, with 17% of children aged 2–19 years considered obese (“95th percentile of the BMI for age growth charts).1 Moreover, disparities in obesity exist between population subgroups1-3; obesity prevalence is higher among Hispanic (22%) and black (20%) children, compared with non-Hispanic white (14%) children.1, 4 By region, prevalence of obesity for adults is higher in the Midwest (30%) and South (30%) than in the Northeast (25%) and West (25%).5 The prevalence may also vary by urban/rural setting; according to national data from 2003–2006, more rural children (22%) than urban children (17%) were obese.6
In addition, obesity leads to inequities in disease burden and resultant medical costs. Childhood obesity has been linked to cardiovascular risk factors, including high levels of blood pressure, triglycerides, and low-density lipoprotein cholesterol, and reduced insulin sensitivity.7, 8 For obese children, the lifetime direct medical cost of obesity is $19,000, relative to normal weight children who maintain a normal weight through adulthood.9
Programs and Policies Targeting Childhood Obesity
Numerous federal programs have targeted childhood obesity. CDC launched two large initiatives: Communities Putting Prevention to Work (CPPW) and the Community Transformation Grants (CTGs). In 2010, CDC funded the CPPW program for 2 years in 50 communities to address obesity and tobacco use.10 In 2011, CDC awarded $103 million in CTGs to 61 state and local government agencies, tribes and territories, and non-profit organizations in 36 states to implement community-level programs that prevent chronic diseases and focus on active living and healthy living strategies.11 Another well-publicized federal initiative, Let's Move, aims to promote healthy eating and physical activity among children.12 Similarly, NIH implemented the Ways to Enhance Children's Activity & Nutrition (We Can!)® program in 2005, a science-based childhood obesity program, for communities and parents/families.13
Several private foundations also have developed initiatives to address childhood obesity. In 2007, the Robert Wood Johnson Foundation (RWJF) pledged $500 million to fund efforts to help reverse the childhood obesity epidemic.14 One of RWJF's childhood obesity efforts is Healthy Kids, Healthy Communities, a national program to implement healthy eating and active living initiatives focusing on children who are most at risk for obesity.15 Similarly, in 2010, the California Endowment pledged $1 billion to build healthy communities to improve the health and well-being of its residents.16 The Alliance for a Healthier Generation, founded by the American Heart Association and the Clinton Foundation, also supports efforts to address childhood obesity by focusing on building healthier school environments, promoting healthy eating and physical activity, improving access to healthier foods and beverages and physical activity, and working on an approach to obtain reimbursement for obesity prevention services.17
In addition to these federal and non-federal programs, many obesity-related policies have been enacted at the federal, state, and local levels. An example at the federal level is the Menu Labeling Law, enacted in 2010, that requires restaurant chains with 20 or more establishments to display calorie information on menus and menu boards.18 Several states also have implemented obesity-related policies. For instance, the Arkansas Child and Adolescent Obesity Initiative included legislation to establish annual BMI checks for all children.19 Similar legislation has been enacted in other states. California, for example, passed legislation regulating the sale of competitive foods in public schools, with the goal of limiting children's intake of the high-sugar, high-fat foods that contribute to weight gain. Positive changes in BMI trends were observed after implementation.20, 21 Other state-level obesity-related policies have had mixed results. For example, in states with weak competitive food laws for middle schools, children were 20% more likely to be overweight or obese than children in states with either no or strong competitive food laws.22 On a district-wide or single-school scale, school policies are related to an improved food environment and dietary intake among school children, but a clear link with BMI has not been established.23-25
Some cities, towns, or regions in the U.S. have sought to address the multilevel determinants of obesity by implementing population-based “whole of community interventions” that target the obesity status of entire populations.26 For example, Shape Up Somerville (SUS) was a comprehensive, 2-year, non-randomized controlled trial in three communities: one intervention community and two sociodemographically matched control communities.27 SUS was a partnership that included a variety of intervention components: school breakfast program, walk to school campaign, school staff professional development, classroom curriculum, enhanced recess, school food service, school wellness policy development, after-school nutrition and physical activity curriculum, outreach to parents, community advisory council, and various community events. SUS demonstrated a decrease in mean BMI z-scores in children.27 Other population-based or whole of community intervention approaches, in the U.S. and other countries, also have been effective in reducing weight among children.26 Although community interventions have achieved some success in reducing BMI, it is unclear which strategies are optimal and which components or combinations of strategies are key to success.28
With the increase in community programs and policies targeting childhood obesity, studies are needed that systematically examine such natural experiments.29-32 A natural experiment refers to “naturally occurring circumstances in which different populations may or may not be exposed to a potentially causal factor or intervention such that the circumstances resemble a true experiment in which participants may be assigned to exposed or unexposed groups.33” Implementation of various programs and policies targeting childhood obesity in communities can be seen as potential natural experiments, because community programs and policies are implemented across time, geography, and content such that some populations are exposed to the intervention components while others are not.34 Natural experiments hold advantages for external validity because they reflect the real-world challenges of implementing programs and policies that cannot be assured in the unusual circumstances of community trials or effectiveness studies.33
The NIH initiated the Healthy Communities Study (HCS) in 2010 to address the growing research gap related to understanding the relationship between natural experiments in communities across the U.S. and how they are associated with childhood obesity. The HCS is an observational study to assess the relationships between characteristics of community programs and policies and BMI, diet, and physical activity in children. The National Heart, Lung, and Blood Institute (NHLBI) leads the HCS in collaboration with the Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institute of Diabetes and Digestive and Kidney Diseases, National Cancer Institute, and NIH Office of Behavioral and Social Sciences Research. The purpose of this paper is to describe the HCS's rationale, aims, and logic model, and to provide a brief overview of the study design. The other papers in this supplement will present more detailed information on the statistical design (Strauss et al.),35 operational elements (John and colleagues),36 weight status measures (Sroka et al.),37 dietary measures (Ritchie and colleagues),38 physical activity measures (Pate et al.),39 and measures of community programs and policies (Fawcett and colleagues).40
Description of the Healthy Communities Study
Study Rationale
Community programs and policies targeting childhood obesity are being implemented across the U.S., and wide variations exist in the approaches, intensity levels, duration, funding, target population, and implementation techniques of these programs. However, no previous studies have systematically examined these community programs and policies to identify how differing aspects and approaches are related to childhood obesity outcomes. The HCS is not designed to evaluate any one specific program, policy, or community effort; instead, it is systematically assessing whether characteristics of programs and policies in diverse communities across the country are associated with BMI, nutrition, and physical activity in children. The study design allows for the simultaneous examination of BMI, nutrition behaviors, physical activity, and community-level characteristics. Some examples of community-level characteristics include community and school programs and policies targeting childhood obesity as well as the school's physical environment (e.g., lunchroom setting, school outdoor physical activity resources) and the physical characteristics of the immediate area surrounding the participant's home.
Study Aims
The HCS is grounded in a socioecologic model and systems approach. The socioecologic framework emphasizes the multiple spheres of influence on health. Thus, childhood obesity is a function of individual, interpersonal (e.g., family), institutional and organizational (e.g., schools), community (e.g., parks), and broader policies and systems (e.g., state BMI screening policies). A systems approach addresses the dynamic interplay between the different levels of influence.41
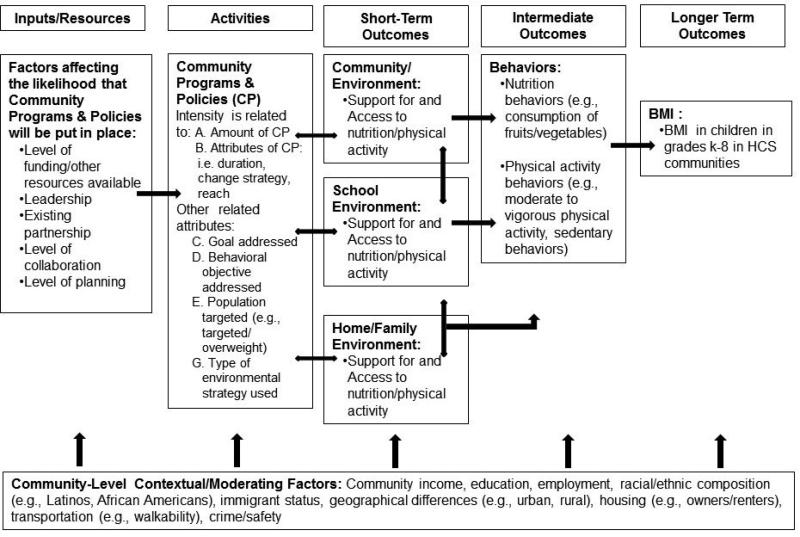
The HCS logic model (Figure 1) depicts the hypothesized pathways of influence of community programs and policies targeting childhood obesity on a continuum of obesity-related outcomes. The HCS logic model illustrates how inputs/resources, such as level of funding, may be related to characteristics of community programs and policies, which may then be related to the short-term outcomes, including community, school, and home/family environments. The short-term outcomes may be related to the intermediate outcomes of nutrition and physical activity behaviors and ultimately BMI. Underlying all of these variables are community-level contextual/moderating factors such as mean community income and geographic differences. The arrows in the logic model illustrate that there is interplay among the various variables.
Figure 1.
Healthy Communities Study logic model.
The main objectives and study aims of the HCS are concerned with examining associations with BMI, not the prevalence of obesity. The HCS was not designed to measure the prevalence of obesity for the entire U.S. or within each community. In addition, the intent in developing the logic model was to not specify the direction of the association between community programs and policies and any of the outcomes in order to allow for the possibility of negative associations.
The HCS has three main aims:
to determine the associations between characteristics of community programs and policies and BMI, diet, and physical activity in children;
to identify community, family, and child factors that modify or mediate the associations between characteristics of community programs and policies and BMI, diet, and physical activity in children; and
to examine the associations between characteristics of programs and policies and BMI, diet, and physical activity in children in communities that have a high proportion of groups experiencing health disparities (e.g., African American, Latino, or low-income residents).
One-hundred and thirty diverse communities, and up to 81 children and their parents/caregivers per community, participated in the HCS. For the purposes of the study, a community is defined as a high school catchment area, and child participants are students at public elementary and middle schools (kindergarten through eighth grade) within the catchment areas. The study is examining quantitative and qualitative information obtained from community-based initiatives; community characteristics (e.g., school environment); measurements of children's physical activity, dietary practices, height, and weight; and parent/caregiver's height and weight.
Overview of Study Design
A unique aspect of the HCS is that it includes both retrospective and cross-sectional components. The retrospective data include children's height and weight abstracted from medical charts and details of community programs and policies dating back 10 years. The cross-sectional data include in-home assessment of children's height, weight, diet, and physical activity, and current information on community programs and policies. The retrospective data will allow for an assessment of how community programs and policies have unfolded over the previous 10 years in each community. Those data will be compared with BMI trajectories over the same time period, which will be calculated by combining BMI measured at baseline with BMI calculated from height and weight data abstracted from participant medical records.
A hybrid sampling approach was used to select communities eligible to participate. Some communities were selected from a stratified national probability-based sample, whereas others were chosen because these communities (referred to as “certainty” communities) had implemented promising programs and policies targeting childhood obesity. The communities from the probability-based sample (i.e., those that were not “certainty communities”) were sampled using a stratified probability-based sampling approach, using weights proportional to the number of children aged 4–15 years in each Census Tract. Thus, they were randomly selected with weights proportional to size. A more detailed description of the sampling approach for communities, schools, and households can be found in Strauss et al.35 in this issue. One benefit of the hybrid approach is that it ensured the inclusion of communities that had implemented promising programs and policies targeting childhood obesity, rather than leaving inclusion of those types of communities to chance. The hybrid sampling approach will maximize the opportunity to identify approaches and strategies that are associated with a reduction in childhood obesity and related measures in communities with different characteristics, and yield results that are applicable to communities across the U.S., with a particular focus on Hispanic/Latino, African American, and low-income children.
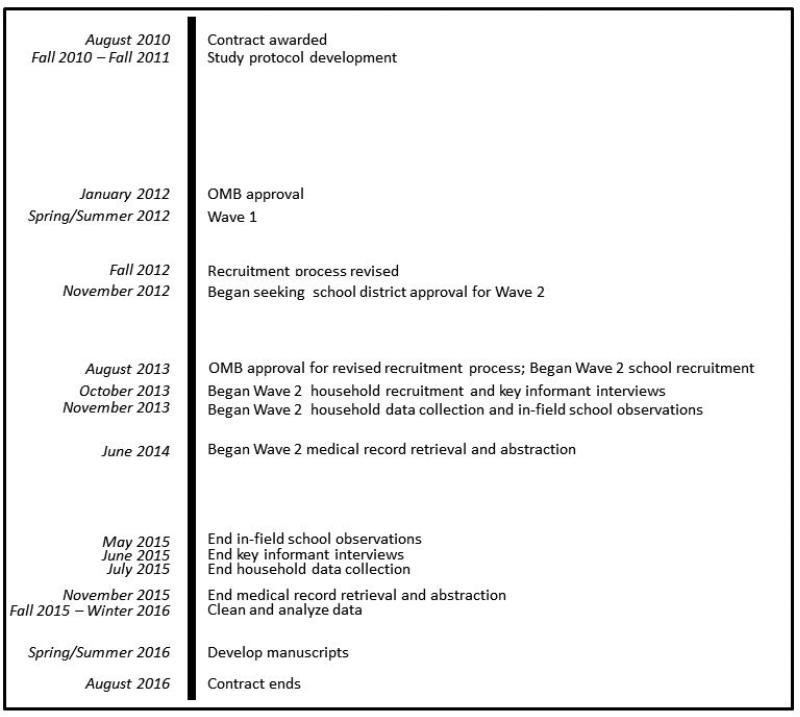
The HCS was funded in 2010, field data collection and medical record abstraction will be completed in 2015, and data cleaning and analyses will be completed by mid-year 2016. Figure 2 shows the HCS timeline. During the study period, HCS implemented two different waves of data collection. Wave 1 consisted of four communities, and Wave 2 consisted of 130 communities. Wave 1 was intended as an opportunity to refine the recruitment and data collection processes. During Wave 1, HCS recruited participants through InfoUSA for a random sample of households with landlines that were within the public high school catchment area. Wave 1 results indicated that this strategy yielded a sample that was not always reflective of the selected community with respect to race/ethnicity; furthermore, more than 30% of the telephone numbers were disconnected, while an additional 20% refused to participate, often before recruiters could provide any information about the study. In recent years, there has been a significant decrease in the use of landlines, especially by low-income and ethnic minority households (key targets for the HCS).42 Thus, it was determined that the Wave 1 recruitment strategy of using landlines was not a viable approach, and that households would be recruited through schools for Wave 2. The rationale for modifying the recruitment approach was that participants recruited from schools would likely better represent students in the community and would allow the HCS to more directly associate planned observations of schools’ physical activity and nutrition environments with the study population results, because the sampled children attended the recruited schools.
Figure 2.
Healthy Communities Study timeline.
The original approach of using landlines would have allowed for inclusion of children from public, private, and home schools, but the disadvantages of this methodology, as mentioned above, were considerable. The HCS decided to recruit children only from public schools because it was possible to ascertain elementary and middle public schools for a given public high school catchment area. The disadvantage of not recruiting from private and home schools is that the sample may not be representative of the community. The findings of the HCS will be limited to children who attended public schools. More information on the HCS recruitment process is provided in John and colleagues36 in this issue.
The revised recruitment approach for Wave 2 was complex and required several layers of approval. First, the school district had to approve the study. Then, individual principals of selected schools in the high school catchment area had to agree to their school's participation in the study. After the schools were recruited, households were recruited through these schools. Wave 2 was originally designed to recruit a larger number of communities, but the recruitment goal was reduced to 130 communities owing to several factors (i.e., the considerable time required to receive U.S. Office of Management and Budget approval for the revised recruitment strategy and time needed to recruit school districts, schools, and households). Wave 2 data collection lasted about 1.5 years. Despite the reduction in the number of communities, there is still sufficient statistical power in the sample to be able to detect meaningful differences. More information on the HCS power estimates can be found in Strauss et al.35 in this issue.
The HCS collected data at the community, school, and individual levels. Although field data collection is complete, data editing and analysis are ongoing. Thus, the sections below describe the data collection approaches at the various levels, but findings will be published in subsequent manuscripts. At the community level, data were collected to assess the number and types of programs and policies that were implemented and to examine how they evolved over the past 10 years. These retrospective and current data were collected through standardized interviews with community key informants and document review (Fawcett et al.40 in this issue provides a detailed description of the community measurement approach). In each community, ten to 14 key informants with knowledge of community programs and policies addressing childhood obesity were interviewed. The key informants were recruited from various sectors, including schools, health organizations/coalitions, government, and non-profit organizations. Data also were collected through document review, with reports and other documents either supplied by the key informant or located through online searches by the study staff.
At the school level, children were recruited from two public elementary and two public middle schools in each community (John et al.36 in this supplement describes the recruitment, training, and quality control/quality assurance procedures). School staff distributed informational materials and interest forms to children at school, and families who completed the forms were contacted by the study. Within the participating schools, trained study personnel observed the lunchroom environment and outside physical activity resources and conducted interviews with key school staff (e.g., school principal, physical education teacher) to assess programs and policies being implemented within the school. The district food service administrator/manager in each community was asked to complete a web-based survey on the food environment for each of the recruited schools within their school district. A school staff member was asked to complete a web-based survey on school policies and practices related to nutrition and physical activity for each school.
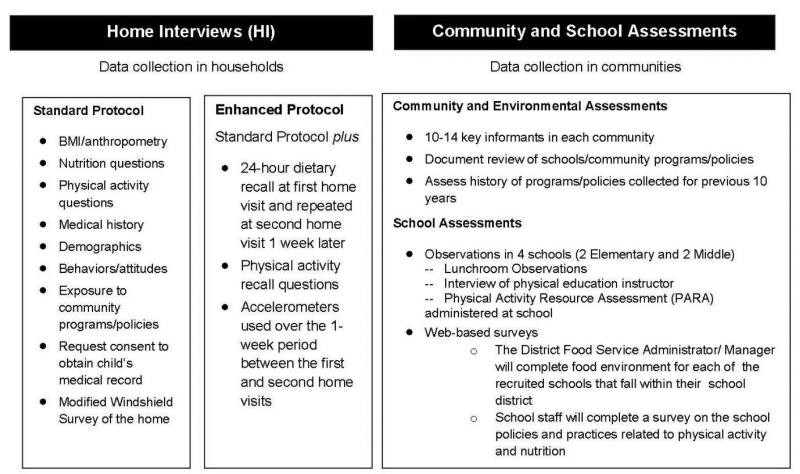
At the household level, trained field data collectors conducted interviews and collected data in the home. Data collection at the household level included a less intensive standard protocol of measures, which was administered to all participants, and a more detailed enhanced protocol, administered to approximately 10% of participants (Figure 3). The standard protocol consisted of height, weight, and waist circumference measurements of the child; height and weight measurements or reported measurements of the parents/caregivers; general demographic and background questions; and brief nutrition and physical activity behavior questionnaires. The enhanced protocol included all of the standard protocol measures plus more-detailed measures of nutrition (i.e., two 24-hour dietary recalls) and physical activity (i.e., accelerometry data captured during waking hours for 1 week and completion of the Physical Activity Behavior Recall instrument). Medical records were abstracted on approximately 70% of the children after obtaining parental consent, in order to develop longitudinal BMI trajectories. A detailed description of the HCS weight status measures can be found in Sroka and colleagues37 in this issue.
Figure 3.
Healthy Communities Study primary data collection activities.
Study Governance and Oversight
Investigators at Battelle Memorial Institute and its academic partners (University of California at Berkeley, University of South Carolina, and University of Kansas), the NIH staff, and partners at CDC and RWJF formed the Steering Committee that designed the study and developed the measures and protocol. An Executive Committee composed of representatives from Battelle, the academic partners, and the NIH worked to implement the study and monitor progress. Detailed planning and monitoring were conducted by eight study committees—Design and Analysis, Physical Activity, Nutrition, Community Measurement, BMI and Medical Records, Recruitment and Retention, Presentations and Publications, and Public Relations—which reported to the Executive Committee.
The Battelle Memorial Institute's IRB provides oversight for the study. IRB approval was received in 2011 with annual review. HCS also has an NHLBI-appointed Observational Study Monitoring Board, which serves as an advisory board to the NHLBI and provides oversight on participant burden, safety, and overall study progress. All data collection forms received approval from the U.S. Office of Management and Budget (OMB #0925-0649).
Discussion
The HCS is one of the largest studies ever conducted in the U.S. to assess the associations between characteristics of community programs and policies and BMI, diet, and physical activity in children. The study was designed to include a diverse sample of U.S. communities that will facilitate drawing conclusions about multilevel approaches and strategies that are associated with childhood obesity. The results should be applicable to diverse communities across the U.S., including communities with a higher proportion of Latino, African American, and low-income children.
The HCS has several limitations. The study's findings will not be representative of students across the country; thus, findings will not be generalizable to all U.S. public elementary and middle school children. Additionally, the HCS was not designed to evaluate the effectiveness of any one particular program or policy in a given community. Another limitation is that programs and policy variations are constantly developing and evolving; the HCS may not capture all programs and policies occurring within each of the sampled communities. Finally, the HCS is an observational study. Therefore, the analyses will not be able to determine if a causal relationship exists between the programs and policies and any changes observed in children's BMI or dietary and physical activity behaviors. Trials that randomize communities to implement a specific set of programs and policies can test the effects of particular combinations of programs and policies. However, such trials are costly and challenging to design and conduct and have limited external validity; that is, they use implementation supports typically not available in most communities. The findings from HCS regarding associations between the intensity of existing community programs and policies and childhood obesity outcomes can be used to generate hypotheses to be tested in future studies.
The HCS addresses a major gap identified by the IOM's Committee on Evaluating Progress on Obesity Prevention Efforts33: a lack of understanding about which community programs and policies are being implemented to address obesity, and how those programs and policies are associated with obesity-related outcomes. The HCS will identify which community approaches are most closely associated with reductions in childhood obesity. Results from the HCS will enable federal, state, and local governments, as well as organizations charged with improving children's health, to better understand the types of programs and policies that influence obesity in children and youth. Specifically, the findings will improve the understanding of which combinations and characteristics of community programs and policies may be more strongly related to childhood obesity across diverse communities.
Acknowledgments
The Healthy Communities Study is funded with federal funds from the National Heart, Lung, and Blood Institute, in collaboration with the Eunice Kennedy Shriver National Institute of Child Health and Development, National Institute of Diabetes and Digestive and Kidney Disorders, National Cancer Institute, and NIH Office of Behavioral and Social Sciences Research; DHHS, under Contract No. HHSN268201000041C.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
No financial disclosures were reported by the authors of this paper.
References
- 1.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA. 2014;311(8):806–814. doi: 10.1001/jama.2014.732. http://dx.doi.org/10.1001/jama.2014.732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Farley TA, Dowell D. Preventing childhood obesity: What are we doing right? Am J Public Health. 2014;104(9):1579–1583. doi: 10.2105/AJPH.2014.302015. http://dx.doi.org/10.2105/AJPH.2014.302015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.CDC Vital Signs: Obesity among low-income, preschool-aged children- United States, 2008-2011. MMWR Morb Mortal Wkly Rep. 2013;(62):1–6. [PMC free article] [PubMed] [Google Scholar]
- 4.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999-2010. JAMA. 2010;307(5):483–490. doi: 10.1001/jama.2012.40. http://dx.doi.org/10.1001/jama.2012.40 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.CDC. [August 11, 2014];CDC Overweight and Obesity. 2014 www.cdc.gov/obesity/data/adult.html.
- 6.Davis AM, Bennett KJ, Befort C, Nollen N. Obesity and related health behaviors among urban and rural children in the United States: Data from the National Health and Nutrition Examination Survey 2003-2004 and 2005-2006. J Pediatr Psychol. 2010;36(6):669–676. doi: 10.1093/jpepsy/jsq117. http://dx.doi.org/10.1093/jpepsy/jsq117 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Freedman DS, Mei Z, Srinivasan S, Berenson GS, Dietz W. Cardiovascular risk factors and excess adiposity among overweight children and adolescents: The Bogalusa Heart Study. J Pediatr. 2007;150:12–17. doi: 10.1016/j.jpeds.2006.08.042. http://dx.doi.org/10.1016/j.jpeds.2006.08.042 . [DOI] [PubMed] [Google Scholar]
- 8.Shashaj B, Bedogni G, Graziani MP, et al. Origin of cardiovascular risk in overweight preschool children: A cohort study of cardiometabolic factors at the onset of obesity. Pediatrics. 2014:E1–E7. doi: 10.1001/jamapediatrics.2014.900. http://dx.doi.org/10.1001/jamapediatrics .2014.900. [DOI] [PubMed] [Google Scholar]
- 9.Finkelstein EA, Graham WCK, Malhorta R. Lifetime direct medical costs of childhood obesity. Pediatrics. 2014;133:854–862. doi: 10.1542/peds.2014-0063. http://dx.doi.org/10.1542/peds.2014-0063 . [DOI] [PubMed] [Google Scholar]
- 10.CDC. [August 18, 2014];Communities Putting Prevention to Work. 2013 www.cdc.gov/nccdphp/dch/programs/CommunitiesPuttingPreventiontoWork/index.htm.
- 11.CDC. [August 18, 2014];Investments in Community Health, Community Transformation Grants Program. www.cdc.gov/NCCDPHP/dch/programs/communitytransformation/pdf/ctg-factsheet-update.pdf.
- 12.Let's Move [August 11, 2014];Let's Move: America's Move to Raise a Healthier Generation of Kids. 2014 www.letsmove.gov/about.
- 13.National Heart Lung and Blood Institute [September 17, 2014];We Can! Ways to Enhance Children's Activity and Nutrition, Background. 2013 www.nhlbi.nih.gov/health/educational/wecan/about-wecan/background.htm.
- 14.Robert Wood Johnson Foundation [August 18, 2014];About RWJF Our Work. www.rwjf.org/en/our-work.html.
- 15.Robert Wood Johnson Foundation [August 18, 2014];About Healthy Kids, Healthy Communities. 2014 www.healthykidshealthycommunities.org/about.
- 16.The California Endowment [August 28, 2014];The California Endowment: Building Healthy Communities. http://www.calendow.org/building-healthy-communities/.
- 17.Alliance for a Healthier Generation [August 18, 2014];Alliance for a Healthier Generation, Schools. 2014 www.healthiergeneration.org/take_action/schools/.
- 18.FDA. [August 23, 2014];Menu and Vending Machine Labeling Requirements. 2014 www.fda.gov/food/ingredientspackaginglabeling/labelingnutrition/ucm217762.htm.
- 19.Ryan KW, Card-Higginson P, McCarthy SG, Justus MB, Thompson J. Arkansas fights fat: Translating research into policy to combat childhood and adolescent obesity. Health Aff. 2006;25(4):992–1004. doi: 10.1377/hlthaff.25.4.992. http://dx.doi.org/10.1377/hlthaff.25.4.992 . [DOI] [PubMed] [Google Scholar]
- 20.Sanchez-Vaznaugh EV, Sanchez BN, Baek J, Crawford PB. ‘Competitive’ food and beverage policies: Are they influencing childhood overweight trends? Health Aff. 2010;29(3):436–446. doi: 10.1377/hlthaff.2009.0745. http://dx.doi.org/10.1377/hlthaff.2009.0745 . [DOI] [PubMed] [Google Scholar]
- 21.Madsem KA, Weedn A, Crawford PB. Disparities in peaks, plateaus, and declines in prevalence of high BMI among adolescents. Pediatrics. 2010;126(3):434–443. doi: 10.1542/peds.2009-3411. http://dx.doi.org/10.1542/peds.2009-3411 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hennessy E, Oh A, Agurs-Collins T, et al. State-level school competitive food and beverage laws are associated with children's weight status. J Sch Health. 2014;84(9):609–616. doi: 10.1111/josh.12181. http://dx.doi.org/10.1111/josh.12181 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nanney MS, Nelson T, Wall M, et al. State school nutrition and physical activity policy environments and youth obesity. Am J Prev Med. 2010;38(1):9–16. doi: 10.1016/j.amepre.2009.08.031. http://dx.doi.org/10.1016/j.amepre.2009.08.031 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nanney MS, Maclehose R, Kubik MY, Davey CS, Coombes B, Nelson TF. Recommended school policies are assicated with student sugary drink and fruit vegetable intake. Pre Med. 2014;62:179–181. doi: 10.1016/j.ypmed.2014.01.026. http://dx.doi.org/10.1016/j.ypmed.2014.01.026 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Constante Jaime P, Lock K. Do school-based food and nutrition policies improve diet and reduce obesity? Pre Med. 2009;48:45–53. doi: 10.1016/j.ypmed.2008.10.018. http://dx.doi.org/10.1016/j.ypmed.2008.10.018 . [DOI] [PubMed] [Google Scholar]
- 26.Wolfenden L, Wyse R, Nichols M, Allender S, Millar L, McElduff P. A systematic review and meta-analysis of community interventions to prevent excessive population weight gain. Prev Med. 2014;62:193–200. doi: 10.1016/j.ypmed.2014.01.031. http://dx.doi.org/10.1016/j.ypmed.2014.01.031 . [DOI] [PubMed] [Google Scholar]
- 27.Economos CD, Folta SC, Goldberg J, et al. A community intervention reduces BMI z-score in children: Shape Up Sommerville first year results. Obesity. 2007;15:1325–1336. doi: 10.1038/oby.2007.155. http://dx.doi.org/10.1038/oby.2007.155 . [DOI] [PubMed] [Google Scholar]
- 28.Swinburn B. Obesity prevention in children and adolescents. Child Adolesc Psychiatr Clin N Am. 2009;18(1):209–223. doi: 10.1016/j.chc.2008.07.015. http://dx.doi.org/10.1016/j.chc.2008.07.015 . [DOI] [PubMed] [Google Scholar]
- 29.McKinnon RA, Orleans TC, Kumanyika SK, et al. Considerations for an obesity policy agenda. Am J Prev Med. 2009;36(4):351–357. doi: 10.1016/j.amepre.2008.11.017. http://dx.doi.org/10.1016/j.amepre.2008.11.017 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.IOM. Bridging the Evidence Gap in Obesity Prevention: A Framework to Inform Decision Making. National Academies Press; Washington DC: 2010. [PubMed] [Google Scholar]
- 31.NIH. NIH Obesity Research [August 24, 2014];Strategic Plan for NIH Obesity Research. 2011 www.obesityresearch.nih.gov/about/strategic-plan.aspx.
- 32.Sallis J, Story M, Lou D. Study design and analytic strategies for environmental and policy research on obesity, physical activity, and diet. Am J Prev Med. 2008;36(2 Suppl):S72–S77. doi: 10.1016/j.amepre.2008.10.006. http://dx.doi.org/10.1016/j.amepre.2008.10.006 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.IOM. Evaluating Obesity Prevention Efforts: A Plan for Measuring Progress. Washington DC: The National Academies Press. 2013 [Google Scholar]
- 34.Hunter CM, McKinnon RA, Esposito L. News from the NIH: research to evaluate “natural” experiments related to obesity and diabetes. Transl Behav Med. 2014;4:127–129. doi: 10.1007/s13142-013-0250-z. http://dx.doi.org/10.1007/s13142-013-0250-z . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Strauss WJ, Sroka CJ, Frongillo EA, et al. Statistical design features of the Healthy Communities Study. Am J Prev Med. 2015 doi: 10.1016/j.amepre.2015.06.021. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.John LV, Gregoriou M, Pate RR, et al. Operational implementation of the Healthy Communities Study: How communities shape children's health. Am J Prev Med. 2015 doi: 10.1016/j.amepre.2015.06.019. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sroka CJ, McIver KL, Sagatov RDF, Arteaga SS, Frongillo EA. Weight status measures collected in the Healthy Communities Study: Protocol and analyses. Am J Prev Med. 2015 doi: 10.1016/j.amepre.2015.07.001. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ritchie LD, Wakimoto P, Woodward-Lopez G, et al. The Healthy Communities Study nutrition assessments: Child diet and the school nutrition environment. Am J Prev Med. 2015 doi: 10.1016/j.amepre.2015.06.016. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pate RR, McIver KL, Colabianchi N, et al. Physical activity measures in the Healthy Communities Study. Am J Prev Med. 2015 doi: 10.1016/j.amepre.2015.06.020. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fawcett SB, Collie-Akers VL, Shultz JA, Kelley M. Measuring community programs and policies and their intensity in the Healthy Communities Study. Am J Prev Med. 2015 doi: 10.1016/j.amepre.2015.06.027. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Huang TG, Drewnowski A, Kumanyika S, Glass TA. A systems-oriented multi-level framework for addressing obesity in the 21st century. Prev Chronic Dis. 2009;6(3):1–10. [PMC free article] [PubMed] [Google Scholar]
- 42.CDC. [April 21, 2015];Wireless Substitution: Early Release of Estimates from the National Health Interview Survey. 2013 Jul-Dec; 2014 www.cdc.gov/nchs/data/nhis/earlyrelease/wireless201407.pdf.