Abstract
Breast cancer (BC) is one of the most prominent diseases in the world, and the treatments for BC have many limitations, such as resistance and a lack of reliable biomarkers. Currently the Hippo pathway is emerging as a tumor suppressor pathway with its four core components that regulate downstream transcriptional targets. In this review, we introduce the present targeted therapies of BC, and then discuss the roles of the Hippo pathway in BC. Finally, we summarize the evidence of the small molecule inhibitors that target the Hippo pathway, and then discuss the possibilities and future direction of the Hippo-targeted drugs for BC therapy.
Keywords: hippo pathway, breast cancer, targeted therapy, YAP, TAZ, LATS, MST
1. Introduction
1.1. Targeted Treatment of Breast Cancer
BC is the most frequently diagnosed cancer among females, accounting for 25% of all cancer cases worldwide [1]. Over the past decades, despite substantial efforts made to improve the survival and quality of life, BC remains a deadly threat for patients. For most types of BC, treatment involves surgery, radiation therapy, hormone therapy, chemotherapy, and the latest targeted therapy [2]. Up to the present day, multiple targeted drugs have been approved in the treatment of BC by FDA as illustrated in Table 1, including inhibitors of estrogen receptor (ER), aromatase, cyclin-dependent kinase (CDK) 4/6, mTOR (rapamycin), and poly(ADP-ribose) polymerase (PARP), and epithelial growth factor receptor (EGFR) and human epithelial growth factor receptor 2 (HER2)-targeted agents [3]. Additionally, studies about the antitumor effects of many other inhibitors such as inhibitors of vascular endothelial growth factor (VEGF), farnesyl transferase, and fibroblast growth factor receptor (EGFR) also show a promising future and have caught attentions as well [4].
Table 1.
Approved targeted drugs for breast cancer.
| Target | Drugs | Mechanism | References |
|---|---|---|---|
| ER | Tamoxifen | Competitively inhibits the binding of estradiol to ER, resulting in a reduction in DNA synthesis and cellular response to estrogen | [10] |
| Fulvestrant | Binds competitively to ER, resulting in ER deformation and decreased estrogen binding | [11] | |
| Toremifene | Chemically related to tamoxifen, binds competitively to ER | [12] | |
| Aromatase | Anastrozole | Selectively binds to and reversibly inhibits the enzyme aromatase, which catalyzes the final step in estrogen biosynthesis and may result in growth inhibition of estrogen-dependent breast cancer cells | [13] |
| Exemestane | Binds irreversibly to and inhibits aromatase | [14] | |
| Letrozole | Selectively and reversibly inhibits aromatase | [15] | |
| HER2 | Trastuzumab | Binds to HER2 on the tumor cell surface, induces an antibody-dependent cell-mediated cytotoxicity against tumor cells that overexpress HER2 | [16] |
| Pertuzumab | Binds to the dimerization domain of the HER2, therefore prevents the activation of HER signaling pathways, resulting in tumor cell apoptosis | [9] | |
| Ado-trastuzu-mab emtansine | The maytansinoid DM conjugated to the HER2-targeting transtuzumab is released and binds to tubulin, thereby inhibiting cell division and the proliferation of cancer cells that overexpress HER2 | [17] | |
| EGFR, HER2 | Lapatinib | Selectively inhibits both EGFR and HER2 tyrosine kinases | [18] |
| Neratinib maleate | Binds to and inhibits both HER2 and EGFR | [19] | |
| mTOR | Everolimus | Binds to the immunophilin FKBP-12 to generate an immunosuppressive complex that binds to and inhibits the activation of the mammalian Target of Rapamycin (mTOR) | [20] |
| CDK4/6 | Palbociclib | Selectively inhibits CDK4 and CDK6, thereby inhibiting Rb protein phosphorylation, which suppresses DNA replication and decreases tumor cell proliferation | [21] |
| Ribociclib | Specifically inhibits CDK4/6 | [22] | |
| Abemaciclib | Specifically inhibits CDK4/6 | [23] | |
| PARP | Olaparib | Selectively binds to and inhibits PARP and PARP-mediated repair of single strand DNA breaks | [24] |
ER, Estrogen receptor; HER2, Human epidermal growth factor receptor 2; EGFR, epithelial growth factor receptor; FKBP-12, FK Binding Protein-12; CDK4/6, Cyclin-dependent kinase 4 and 6; Rb, retinoblastoma.
However, current treatment has its own limitations. First of all, BC subtypes show different responses to systemic therapy, suggesting the treatment should be more specific for each patient [5,6]. By detecting the expression levels of ER and progesterone receptor (PgR), as well as the HER2 and Ki-67, BC were identified into categories with similar clinical implications, including Luminal A, Luminal B, HER2-positive, and triple-negative breast cancer (TNBC) subtypes [7]. Among them, TNBC shows a relatively poor prognosis, while the Luminal and HER2-positive subtypes respond sensitively to endocrine therapy and targeted therapy [8]. Secondly, drug resistance, especially to monotherapy, has limited the curative efficacy, resulting in a low response rate. Thirdly, the lack of reliable indicators for most of the targeted agents makes it a challenge to select doses and predict the prognosis of patients [9]. Therefore, identifying novel breast cancer therapeutic targets, revealing the mechanisms underlying drug resistances, discovering new biomarkers and developing rational combinations of targeted therapy remain urgent and important.
1.2. The Hippo Pathway
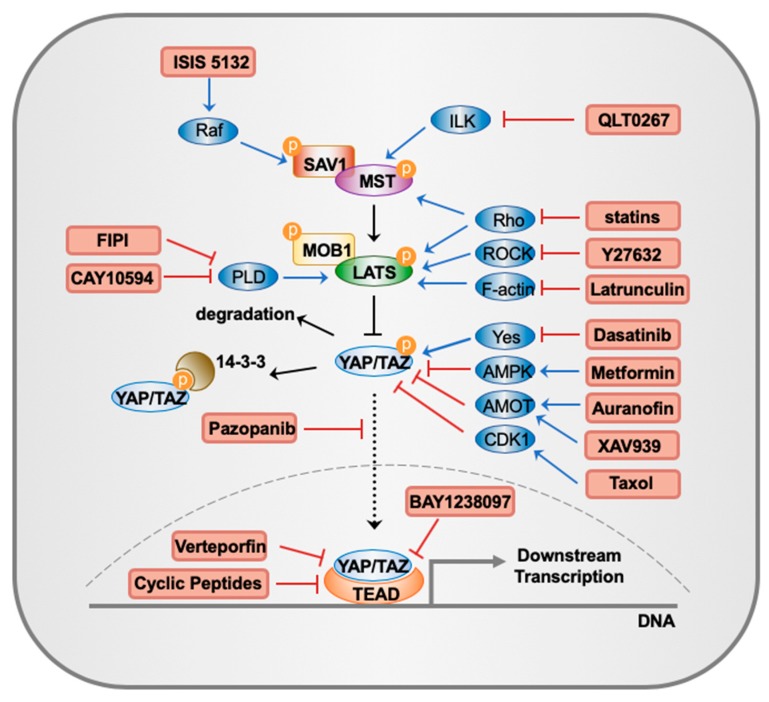
The Hippo pathway, named after the Drosophila Hpo kinase, is a highly conserved signal transduction pathway that plays important roles in organ size control, tissue regeneration, immune response, stem cell function and tumor suppression [25,26,27]. In mammals, the canonical Hippo pathway consists of four core components that function through phosphorylation: mammalian sterile 20-like kinase (MST; homolog of Drosophila Hpo), large tumor suppressor (LATS) kinases, scaffold proteins Salvador homolog 1 (SAV1) and Mps One Binder kinase activator protein 1 (MOB1) (Figure 1). In certain conditions such as high cell density, extracellular matrix stiffness and lack of nutrients, the Hippo pathway is activated, with MST and LATS successively phosphorylated with the support of SAV1 and MOB1 [26]. Then, the activated LATS phosphorylates transcriptional co-activator Yes-associated protein (YAP) and its paralog transcriptional coactivator with PDZ-binding motif (TAZ), which prevent TAZ/YAP from entering the nucleus by anchoring them to 14-3-3 protein and/or promoting their degradation in the cytoplasm (Figure 1) [28,29]. This interrupts their interactions with the transcription factor TEA domain (TEAD) family proteins, which subsequently inhibits cell proliferation and oncogenic transformation and induces apoptosis. Conversely, the dysregulation of the Hippo pathway increases the nuclear functions of TAZ/YAP, leading to active gene expression [30,31], such as several growth-promoting factors, including secretory proteins connective tissue growth factor (CTGF) and CYR61 [32,33], AXL receptor tyrosine kinase [34], c-myc and survivin [35].
Figure 1.
Main components of the Hippo pathway and the current Hippo-targeted inhibitors discussed in this review. In mammals, the canonical Hippo pathway consists of four core components that function through phosphorylation: MST, SAV1, LATS, MOB1. Activated LATS phosphorylates YAP/TAZ, preventing them from entering the nucleus by anchoring them to 14-3-3 protein and/or promoting their degradation in the cytoplasm. This interrupts their interactions with the transcription factor TEAD family proteins, which subsequently inhibits cell proliferation and oncogenic transformation and induces apoptosis. Besides, current Hippo-targeted inhibitors discussed in this review, as well as their targets and major mechanisms, are shown in the figure.
Aside from TAZ/YAP-TEAD interaction, TAZ/YAP can also regulate transcription mediated by RUNX, SMADs, TP73, NKX2.1, OCT4 and PPARγ. When the Hippo pathway engages in crosstalk such as with Wnt, TGFβ, Notch and PI3K, the functions of TAZ/YAP are further stimulated [30,32]. With increasing studies, many regulators of TAZ/YAP have been identified in addition to the core Hippo pathway components. For example, TAZ/YAP activity can be regulated in a LATS-independent way, by binding to Angiomotin (AMOT) family proteins, ZO-1/2, α-catenin, β-catenin, PTPN14 and Scribble [36]; the receptor tyrosine kinase EphA2 could activate TAZ/YAP through Rho-ROCK signaling [37]. In this era of targeted therapy, the Hippo pathway appears to be a promising target for the treatment of breast cancer. Here, we summarize the current evidence to demonstrate the mechanisms beneath and provide an overview of the current development of Hippo-targeted therapy for breast cancer.
2. The Roles of the Hippo Pathway in Breast Cancer
In 1999, St John et al. discovered that mice lacking Lats1, a mouse homology of Drosophila lats, display pituitary hyperplasia and develop tumors [38]. Later our studies provided evidence that LATS is a tumor suppressor in human cancer cells [39]. Since then many studies support the role of the Hippo pathway as a tumor suppressor pathway in diverse human cancers, including breast cancer [40,41]. In the following text, we will discuss how each component of the core Hippo pathway is involved in the tumorigenesis and metastasis of breast cancer.
2.1. YAP and TAZ
High YAP are more common in BC lacking functional adherens junctions [40]. The expression status of YAP is also associated with the molecular subtypes, tumoral and cellular components of BC, and could be a prognostic marker for patents, pointing to an oncogenic role [42]. YAP overexpression enhances multiple processes for tumorigenesis and metastasis in BC cells, including cellular proliferation, transformation, migration, and invasion [43]. Previous studies reported that overexpression of YAP in human non-transformed mammary epithelial cells induces epithelial-to-mesenchymal transition (EMT), suppression of apoptosis, growth factor-independent proliferation, and anchorage-independent growth on soft agar [44].
Besides, the divergent tumor-suppressive roles of YAP have also been recognized [41,45,46,47,48,49,50,51], which could be explained by many reasons. YAP exists in two major isoforms (YAP1 and YAP2) that may have their own transcriptional targets. Therefore, the relative levels of those two isoforms might decide whether YAP is acting as a tumor suppressor or otherwise in BC cells [52,53]. In addition, YAP1 can translocate to the nucleus and associate with tumor suppressor p73, resulting in apoptosis through transcriptional activation of the proapoptotic gene puma [46]. Another explanation for the tumor-suppressive role of YAP is that deregulated TAZ/YAP activity in BC cells induces an anti-tumorigenic immune surveillance response, ultimately leading to the eradication of tumor cells so BC cells have to restrain YAP activity consequently [54,55]. Moreover, studies reported that YAP can bind and signal through anti-apoptotic protein (delta)ΔNp63 isoform to protect cancer cells from DNA damage. Therefore, it is possible that only in certain conditions like DNA damage, YAP can selectively induce p73-mediated apoptosis [56,57]. Additionally, more investigations considering different intrinsic subtypes of BC and stem cells should be done to explain the dramatic effects of YAP [41].
TAZ has also been identified as an oncogene that plays a critical role in the migration, invasion, and tumorigenesis of BC cells [58,59]. It is conspicuously overexpressed in human breast cancer tissues from patients in which its expression levels generally correlate with the TNBC diagnosis [60] and patient prognosis [41]. Overexpression of TAZ in low-expressing MCF10A non-tumorigenic mammary cells leads to the acquisition of a spindle-shaped morphology and increases migratory and invasiveness [58], while the depletion of TAZ inhibits cell growth in 184A1 and HCC1937 breast cancer cells [61] and retards the anchorage-independent growth on soft agar and tumorigenesis in nude mice in MCF7 cells [58]. Additionally, TAZ has been implicated in BC-associated metastatic bone disease, partly through its interaction with hypoxia inducible factor-1α [62]. Recent studies show that TAZ is required for sustaining self-renewal, tumor-initiation capacities [63], and metastatic activity [59] in BC stem cells (BCSCs). The connection between TAZ and BCSCs has been correlated with its interaction with established inducers of the cancer stem cell phenotype such as hypoxia-inducible factor 1 (HIF1) and extracellular cues [64,65,66].
YAP/TAZ act as central players of multiple cancer-associated features such as proliferation and cell survival, migration and metastasis [41], and the tumor-initiating functions. All of these functions rely on their interaction with TEAD transcriptional factors. TAZ/YAP-TEAD complexes directly promote the expression of many oncogenic factors that contribute to BC progression [43], such as cysteine-rich angiogenic inducer 61 (CYR61) and connective tissue growth factor (CTGF) (also known as CCN1 and CCN2, respectively) [32,67,68]. TAZ-TEAD can activate BMP4, which will enhance signaling downstream of TAZ, and then promote Smad1/5 intracellular signaling and cell migration [69]. YAP-TEAD also could control receptor for hyaluronan-mediated motility (RHAMM) transcription leading to ERK activation and cancer metastasis by binding to RHAMM promoter at specific sites [70]. Glutamine metabolism is critical to many tumor cells including BC cells, and it could be regulated by TAZ/YAP. Through the increased expression of downstream genes SLC1A5 and GLS, TAZ/YAP could promote glutamine uptake and therefore upregulate the amount of intracellular glutamine [37]. Besides TEADs, TAZ/YAP can bind to other transcriptional factors, such as the krueppel-like factor 5 (KLF5) and transforming growth factor β (TGFβ)-activated SMAD2/3. The overexpression of YAP could upregulate KLF5 protein levels and mRNA expression levels of its downstream target genes including FGFBP1 and ITGB2 that promote BC cell proliferation and survival [71]; the interaction between TAZ/YAP and SMAD2/3 regulates novel targets such as NEGR1 and UCA1 that are necessary for tumorigenic activity in metastatic BC cells [68]. YAP function is also required for cancer-associated fibroblasts (CAFs) to promote matrix stiffening, cancer cell invasion and angiogenesis [72].
2.2. Other Components
The upstream components of the Hippo pathway (Figure 1) were found to be tumor suppressors in human breast cancer, and their functions are not limited through the inactivation of TAZ/YAP. In human BC, the downregulation of MST has been identified to be a predictable biomarker for prognosis [73]. MST regulates a diverse array of substrates in addition to the core Hippo pathway components such as LATS, SAV1 and MOB1. Studies have shown that MST also target histone H2B, FOXO, GA-binding protein (GABP) and LATS-related kinases Ndr1/Ndr2 [74,75,76,77], pointing to a tumor-suppressive role.
Clinical evidence has shown reduced expression of LATS in human BC, and functional studies show that overexpression of LATS1 can modulate CDC2 kinase activity and induce pro-apoptotic Bax expression, which causes G2/M cell cycle arrest and induction of apoptosis [78]. Additionally, LATS1 can interact with actin, and Zyxin and LIMK1 [79,80], two regulators of actin filament assembly, regulating actin polymerization [81]. Besides, LATS could phosphorylate angiomotin (AMOT) and thus inhibit cell migration in vitro and angiogenesis [82]. More recently, a direct interaction between LATS and ERα signaling was identified, suggesting that in the presence of LATS, ERα was targeted for ubiquitination and Ddb1–cullin4-associated-factor 1 (DCAF1)-dependent proteasomal degradation, which is a novel non-canonical effect of LATS in the regulation of human breast cell fate [83].
Together, these studies showed that the Hippo pathway is involved in the development of human BC through diverse mechanisms, thus could be a therapeutic target of BC. The therapeutic strategy could be divided into two directions: to inhibit the TAZ/YAP-TEAD interaction, or to up-regulate the upstream components and regulators (Figure 1), since TAZ/YAP activity is mainly governed by LATS kinases [84].
3. The Roles of the Hippo Pathway in Therapeutic Drug Resistance of Breast Cancer
3.1. Resistance to Chemotherapy
Our laboratory for the first time identified TAZ as a novel gene target responsible for drug resistance in BC. Enhanced levels of TAZ render resistance of mammary epithelial cells to chemotherapeutic drug Taxol (paclitaxel) through the downstream activation of CYR61/CTGF promoters, while TAZ knockdown in TAZ-high/drug-resistant MDA-MB231 BC cells turned them sensitive to Taxol [33]. Later we found that TAZ phosphorylation by CDK1 sensitizes BC cells to antitubulin drugs, suggesting a possible novel target for the treatment of antitubulin-resistant cancers [85]. Moreover, TAZ-expressing BC cells and stem cells were reported to be more resistant than control groups to two widely used chemotherapeutic drugs: doxorubicin and paclitaxel [63,86].
Previous study revealed that the expression of YAP could protect BC cells from chemotherapeutic agents Taxol and cisplatin [44]. Recent evidence suggested that YAP resistance to antitubulin drugs is modulated by a Hippo-independent pathway, since antitubulin drugs activate CDK1 and then YAP is phosphorylated on five sites independent of the Hippo pathway [87]. This result suggests YAP and its phosphorylation status to be novel prognostic predictor for antitubulin treatment for BC patients. Besides, low levels of LATS2 mRNA could be a predictor for favorable response to epirubicin plus cyclophosphamide in breast cancers [88]. This role of LATS2 may be explained by the disruption of the checkpoint function at the G1/S phase induced by down-regulation of LATS2.
3.2. Resistance to Targeted Therapy
Several targeted drugs have been approved for the treatment of BC, but the effectiveness varies greatly because of innate and acquired resistance. Current study revealed that the expression levels of TAZ could predict the response to trastuzumab and chemotherapy in Luminal B and HER2-positive BC patients [89]. Besides, in HER2-positive BC cells, TAZ/YAP have been discovered to play a role in the resistance to EGFR/HER2 inhibitor lapatinib by improving the matrix rigidity via the mechanotransduction arm of the Hippo pathway. In HER2-positive BC tumor xenograft mouse model, YAP inhibition increases the sensitivity to lapatinib, suggesting targeting matrix stiffness could be an adjuvant strategy for treating drug-resistant patients [90,91].
3.3. Resistance to Endocrine Therapy
Over two-thirds of breast cancer patients express ERα and respond to ERα antagonists (e.g., tamoxifen and fulvestrant), or drugs that reduce ER ligand estrogen (e.g., letrozole). However, resistance to endocrine therapy occurs frequently and the prognosis of patients does not meet the expectations [92]. Phosphorylation of ERα is one of the mechanisms associated with resistance to endocrine therapy, and LATS2 has been demonstrated to activate ERα transcription. LATS2 co-localizes with ERα in the nucleus, and thus contributes to the resistance to tamoxifen and other ER antagonists in ER+ breast cancer [93].
4. Current Drugs Targeting the Hippo Pathway for Breast Cancer Treatment
4.1. MST and LATS Activation
As mentioned before, MST and LATS are crucial kinases in the Hippo pathway, and they are frequently found to be hypermethylated in BC. Although up till the present moment no direct agents to activate MST and LATS has been discovered, but those indirect activators of MST and LATS still have the potentialities to be targeted drugs for breast cancer cells.
ISIS 5132 is an antisense oligonucleotide designed to hybridize to c-Raf mRNA (Table 2) [94], and Raf-1 was recently found to be an upstream regulator of MST2 [95] (Figure 1). By sequestering MST2 into an inactive complex, Raf-1 could inhibit the apoptosis of BC cells. Preclinical data for ISIS 5132 showed anti-tumor effects in breast cancer and other solid xenograft mouse models, but the agent was withdrawn because of the failure in Phase II clinical trials in patients with colorectal, ovarian or prostate cancer [96]. However, the possibility of ISIS 5132 for the treatment of BC shall need further investigation.
Table 2.
Agents targeting the Hippo pathway in breast cancer.
| Target | Drugs | Major Mechanisms | References |
|---|---|---|---|
| Raf | ISIS 5132 | Hybridizes to c-Raf mRNA, stopping the inactivation of MST | [94,95,96] |
| F-actin | Latrunculin | Activates LATS through regulating F-actin polymerization | [98,99,100] |
| ROCK | Y27632 | Activates LATS through inhibition of ROCK | [101,102] |
| HMG-CoA | Statins | Activates MST/LATS activity through Rho GTPases | [103,104] |
| PLD | CAY10594, FIPI | Reduces the production of PA, which could directly bind to and disrupt LATS and NF2 | [105] |
| ILK | QLT0267 | Activates MST by inhibiting ILK | [106,107] |
| Yes | Dasatinib | Activates kinase activity of Yes to activate YAP | [108,109] |
| PKC | Auranofin | Inhibits YAP through AMOT by inhibiting PKC | [110,111,112] |
| CDK1 | Taxol | Inhibits TAZ/YAP activity by activating CDK1 | [87,113] |
| BRD4 | BAY1238097 | Interacts with TAZ/YAP and downregulates their transcriptional activities by inhibiting BRD4 | [114] |
| AMPK | Metformin | Inhibits YAP activity by activating AMPK | [115,116,117] |
| YAP | Verteporfin | Disrupts YAP-TEAD interaction | [57,118,119,120] |
| AMOT | XAV939 | Suppresses YAP-TEAD transcriptional activities by maintaining the stabilization of AMOT | [124,125] |
| VEGFR & PDGFR | Pazopanib | Inhibits TAZ/YAP nuclear localization by inhibiting VEGFR and PDGFR | [127] |
| YAP | Cyclic Peptides | Peptides disrupting YAP-TEAD interaction | [128] |
Likewise, since F-actin is the inhibitor of MST/LATS, then the negative regulators of F-actin can indirectly activate MST/LATS activity [97]. The marine-derived macrolides latrunculin are known to reversibly bind actin monomers, disrupting their polymerization. Studies have demonstrated the anti-proliferative and anti-invasive effects of latrunculin in BC cell lines (Table 2) [98,99,100]. Besides, Y27632 could indirectly activate MST/LATS through the inhibition of Rho-associated, coiled-coil containing protein kinase (ROCK) (Figure 1) [101], making itself another targeted agent for BC. Furthermore, anti-Rho siRNAs also could inhibit the proliferation and invasiveness of BC cells in vitro and in vivo [102].
Additionally, statins can also activate LATS through Rho inhibition by suppressing HMG-CoA reductase activity (Figure 1; Table 2) [103]. A case control study suggests that the use of statins is associated with a 51% risk reduction of BC after controlling for age, smoking, alcohol use and diabetes [104]. In a new research, phosphatidic acid (PA) was identified to be a key player in the Hippo pathway, mainly by binding to LATS and NF2 (Figure 1). Therefore, inhibitors of PA and its regulator phospholipase D (PLD) could suppress the oncogenic function of YAP. In MDA-MB-231 cells, PLD inhibitor CAY10594 (Table 2) could suppress cell viability and cell migration in vitro, while another PLD inhibitor FIPI could suppress BC xenograft tumor growth [105]. QLT0267, an integrin-linked kinase (ILK) inhibitor, reduces BC cell growth by activating MST [106]. Moreover, QLT0267 can combine with docetaxel to enhance cytotoxicity, reduce phosphorylated AKT (pAKT) levels, alter F-actin architecture and improve treatment outcomes in an orthotopic BC tumor xenograft mouse model [107].
4.2. Targeting TAZ/YAP Regulators
The SRC kinase inhibitor dasatinib is able to inhibits YAP1 nuclear localization and stabilization by reducing Yes-mediated YAP1 phosphorylation or by increasing YAP1 phosphorylation mediated by SRC-PI3K-LATS [108]. Since it suggests promising sensitivity in TNBC cell lines, a Phase II trial examined the efficacy and safety of single-agent dasatinib in unselected patients with advanced TNBC [109]. However, the result showed the effect of single-agent dasatinib is quite limited, so future studies shall investigate other therapeutic settings, such as chemotherapy combinations.
Auranofin was originally used to cure rheumatoid arthritis but recent studies have revealed its antitumor effects [110]. In lung and ovarian cancer, a PKC-AMOT-YAP axis was revealed and auranofin thus could inhibit YAP through AMOT by inhibiting PKC (Figure 1; Table 2) [111]. In breast cancer cells, auranofin induces apoptosis. However, the effect of auranofin could also be explained by prolonged elevation of calcium so further experiments are needed [112].
Additionally, studies showed that taxol also can inactivate TAZ/YAP by activating CDK1 [85,87]. In addition, Bromodomain-containing protein 4 (BRD4), a chromatin-binding protein [113], has been reported to be able to regulate YAP/TAZ transcriptional activity. A potent BRD4 inhibitor named BAY1238097 was tested in human TNBC cell lines and showed satisfying antitumor effect, which might offer new perspectives on the treatment of TNBC patients through modulation of YAP/TAZ (Figure 1; Table 2) [114]. Moreover, energy stress induced by metformin can activate AMP kinase, which directly phosphorylates AMOTL1 and consequently promotes YAP activity in a LATS-independent way (Figure 1; Table 2) [115,116]. A short-term clinical trial in patients with breast cancer showed that, the tumor associated antigen CA15-3 significantly decreased after metformin treatment. However, since metformin may affect breast cancer in other ways as systemic changes in insulin metabolism, more trials should be performed in the future [117].
4.3. Inhibition of YAP/TAZ-TEAD Interaction
Through a screen using a luciferase reporter for TEAD response element, verteporfin (VP) was identified to be able to disrupt the interaction between YAP and TEADs (Figure 1; Table 2) in vitro and in vivo [57]. Later, similar study confirmed that VP acts as a potential inhibitor of TAZ/YAP-driven signaling and tumorigenicity in BC [118]. A recent research explored the possibility to combine VP and paclitaxel treatment for patients with TNBC, and the result suggested that both agents are capable of eliminating BC cells and do not interfere with each other [119]. There is an ongoing Phase II clinical trial of continuous low-irradiance photodynamic therapy (CLIPT) using VP for cutaneous BC patients and so far, the null hypothesis of RR ≤ 5% has been rejected [120]. However, VP itself may not be a very promising Hippo-targeted drug for BC treatment due to difficulty for large-scale synthesis, low solubility and stability, and Hippo-independent effects [121,122].
Besides VP, the other members of the porphyrin family, such as hematoporphyrin and protoporphyrin IX are both currently identified as disruptors of YAP-TEAD interaction in xenograft mouse models [123], which could be the next candidates for BC treatment. In addition, current in vitro studies found that tankyrase inhibitor XAV939 could suppress YAP-TEAD transcriptional activities by maintaining the stabilization of AMOT (Figure 1; Table 2) [124,125], while another study revealed XAV939 could reduce tumorsphere formation in TNBC model by suppressing Wnt pathway [126]. Thus, the mechanism of how XAV939 affects BC cells still need more investigations.
Previous studies also show that in BC cells thiazovivin, dasatinib, lovastatin, cucurbitacin I, and pazopanib inhibited YAP-TEAD interaction by changing the nuclear localization of YAP (Figure 1). Among these drugs, dasatinib, statins, and pazopanib are approved as clinically used drugs (Table 2). Therefore, more researches shall be done focusing on those agents. It is notable that pazopanib can also induce proteasomal degradation of TAZ/YAP by the ubiquitin-proteasome system [127]. Additionally, cyclic YAP-like peptides have been designed to occupy the interface 3 on TEAD, which disrupts YAP-TEAD interaction and proves its therapeutic potency [128]. These and the previously mentioned ones are listed in Table 2.
5. Ongoing Challenges
There is no doubt that the Hippo pathway plays a critical role in cancer development and therefore presents a promising target for the treatment of BC. However, some ongoing challenges remain urgent and unresolved. First, the exact effects of pathway crosstalk and signaling circuitry on therapeutic outcomes are unknown. For example, a relationship between the Hippo pathway and the Wnt pathway has been discussed for a long time, as the Hippo pathway can restrict or activate the Wnt pathway under certain conditions, while CD44, a target of the Wnt pathway, could interact with the Hippo upstream regulator NF2 and therefore activate the Hippo pathway [129,130]. The Hippo pathway is known to engage other pathways such as TGF-β [131], Ras [132], Hedgehog [133], Notch [134] signaling, so the underlying mechanisms require more investigations. Second, it is clear that the Hippo pathway can serve as a therapeutic target for BC patients, but more experiments and clinical trials shall be conducted to get the data about the sensitivity and the response rate of the Hippo-targeted agents, and to identify reliable biomarkers to predict drug responses. Our lab established the first LATS biosensor that could monitor LATS activity in real-time with high sensitivity non-invasively [135]. Since the system could work in vitro and in vivo, it could be used to examine the effects of the potential targeted agents for BC in mice. Third, we shall discover more novel targets and corresponding inhibitors. For example, PP1A phosphatase was identified to be cable to antagonize the function of LATS, and thus regulate the reversible activation of TAZ, suggesting that PP1A phosphatase inhibitor may acts as an antitumor agent [136]. Additionally, no Hippo-targeted agent has been approved to clinical use for breast cancer yet, so to find out their doses and combination strategies, we still have a long way to go.
6. Conclusions and Future Directions
The past decade has witnessed the raising time of the Hippo pathway and the era of targeted therapy. From all the studies mentioned, the Hippo pathway represents both opportunities and challenges for the treatment of breast cancer. In the future, it might be urgent and meaningful to develop drugs that directly target Hippo components (e.g., LATS and YAP/TAZ) or dissociate the TAZ/YAP-TEAD interaction. These drugs can be used alone or combined with other therapeutic drugs (e.g., chemotherapy, target therapy, and immunotherapy) for more effective treatment of drug-resistant or/and metastatic BC in the future.
Acknowledgments
We would like to thank Leda Raptis for revising the manuscript.
Author Contributions
L.W. and X.Y. wrote and revised the review.
Funding
This work was supported by grants from Canadian Institute of Health Research (CIHR#119325, 148629), Canadian Cancer Society (CRS)/Canadian Breast Cancer Foundation (CBCF) to XY. We have received funds for covering the costs to publish in open access.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Torre L.A., Bray F., Siegel R.L., Ferlay J., Lortet-tieulent J., Jemal A. Global Cancer Statistics, 2012. CA Cancer J. Clin. 2015;65:87–108. doi: 10.3322/caac.21262. [DOI] [PubMed] [Google Scholar]
- 2.Aebi S., Davidson T., Gruber G., Cardoso F. Primary breast cancer: Esmo clinical practice guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2011;22:12–24. doi: 10.1093/annonc/mdr371. [DOI] [PubMed] [Google Scholar]
- 3.Álvarez R.H. Present and future evolution of advanced breast cancer therapy. Breast Cancer Res. 2010;12:S1. doi: 10.1186/bcr2572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Coates A.S., Winer E.P., Goldhirsch A., Gelber R.D., Gnant M., Piccart-Gebhart M., Thürlimann B., Senn H.-J. Tailoring therapies—Improving the management of early breast cancer: St Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2015. Ann. Oncol. 2015;26:1533–1546. doi: 10.1093/annonc/mdv221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Goldhirsch A., Wood W.C., Coates A.S., Gelber R.D., Thürlimann B., Senn H.-J. Strategies for subtypes—Dealing with the diversity of breast cancer: Highlights of the St Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2011. Ann. Oncol. 2011;22:1736–1747. doi: 10.1093/annonc/mdr304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rouzier R. Breast Cancer Molecular Subtypes Respond Differently to Preoperative Chemotherapy. Clin. Cancer Res. 2005;11:5678–5685. doi: 10.1158/1078-0432.CCR-04-2421. [DOI] [PubMed] [Google Scholar]
- 7.Parker J.S., Mullins M., Cheang M.C.U., Leung S., Voduc D., Vickery T., Davies S., Fauron C., He X., Hu Z., et al. Supervised Risk Predictor of Breast Cancer Based on Intrinsic Subtypes. J. Clin. Oncol. 2009;27:1160–1167. doi: 10.1200/JCO.2008.18.1370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brenton J.D., Carey L.A., Ahmed A.A., Caldas C. Molecular Classification and Molecular Forecasting of Breast Cancer: Ready for Clinical Application? J. Clin. Oncol. 2005;23:7350–7360. doi: 10.1200/JCO.2005.03.3845. [DOI] [PubMed] [Google Scholar]
- 9.Duffy M.J., Harbeck N., Nap M., Molina R., Nicolini A., Senkus E., Cardoso F. Clinical use of biomarkers in breast cancer: Updated guidelines from the European Group on Tumor Markers (EGTM) Eur. J. Cancer. 2017;75:284–298. doi: 10.1016/j.ejca.2017.01.017. [DOI] [PubMed] [Google Scholar]
- 10.Fisher B., Costantino J.P., Wickerham D.L., Cecchini R.S., Cronin W.M., Robidoux A., Bevers T.B., Kavanah M.T., Atkins J.N., Margolese R.G., et al. Tamoxifen for the prevention of breast cancer: Current status of the National Surgical Adjuvant Breast and Bowel Project P-1 study. J. Natl. Cancer Inst. 2005;97:1652–1662. doi: 10.1093/jnci/dji372. [DOI] [PubMed] [Google Scholar]
- 11.Howell A., Robertson J.F.R., Albano J.Q., Aschermannova A., Mauriac L., Kleeberg U.R., Vergote I., Erikstein B., Webster A., Morris C. Fulvestrant, formerly ICI 182,780, is as effective as anastrozole in postmenopausal women with advanced breast cancer progressing after prior endocrine treatment. J. Clin. Oncol. 2002;20:3396–3403. doi: 10.1200/JCO.2002.10.057. [DOI] [PubMed] [Google Scholar]
- 12.Lewis J.D., Chagpar A.B., Shaughnessy E.A., Nurko J., McMasters K., Edwards M.J. Excellent outcomes with adjuvant toremifene or tamoxifen in early stage breast cancer. Cancer. 2010;116:2307–2315. doi: 10.1002/cncr.24940. [DOI] [PubMed] [Google Scholar]
- 13.Dukes M., Edwards P.N., Large M., Smith I.K., Boyle T. The preclinical pharmacology of “Arimidex” (Anastrozole; ZD1033)—A potent, selective aromatase inhibitor. J. Steroid Biochem. Mol. Biol. 1996;58:439–445. doi: 10.1016/0960-0760(96)00064-7. [DOI] [PubMed] [Google Scholar]
- 14.Goss P.E., Ingle J.N., Alés-Martínez J.E., Cheung A.M., Chlebowski R.T., Wactawski-Wende J., McTiernan A., Robbins J., Johnson K.C., Martin L.W., et al. Exemestane for Breast-Cancer Prevention in Postmenopausal Women. N. Engl. J. Med. 2011;364:2381–2391. doi: 10.1056/NEJMoa1103507. [DOI] [PubMed] [Google Scholar]
- 15.The Breast International Group (BIG) 1-98 Collaborative Group A Comparison of Letrozole and Tamoxifen in Postmenopausal Women with Early Breast Cancer. N. Engl. J. Med. 2005;353:2747–2757. doi: 10.1056/NEJMoa052258. [DOI] [PubMed] [Google Scholar]
- 16.Vogel C.L., Cobleigh M.A., Tripathy D., Gutheil J.C., Harris L.N., Fehrenbacher L., Slamon D.J., Murphy M., Novotny W.F., Burchmore M., et al. Efficacy and Safety of Trastuzumab as a Single Agent in First-Line Treatment of HER2 -Overexpressing Metastatic Breast Cancer. J. Clin. Oncol. 2002;20:719–726. doi: 10.1200/JCO.2002.20.3.719. [DOI] [PubMed] [Google Scholar]
- 17.Baron J.M., Boster B.L., Barnett C.M. Ado-trastuzumab emtansine (T-DM1): A novel antibody-drug conjugate for the treatment of HER2-positive metastatic breast cancer. J. Oncol. Pharm. Pract. 2014;21:132–142. doi: 10.1177/1078155214527144. [DOI] [PubMed] [Google Scholar]
- 18.Konecny G.E., Pegram M.D., Venkatesan N., Finn R., Yang G., Rahmeh M., Untch M., Rusnak D.W., Spehar G., Mullin R.J., et al. Activity of the dual kinase inhibitor lapatinib (GW572016) against HER-2-overexpressing and trastuzumab-treated breast cancer cells. Cancer Res. 2006;66:1630–1639. doi: 10.1158/0008-5472.CAN-05-1182. [DOI] [PubMed] [Google Scholar]
- 19.Burstein H.J., Sun Y., Dirix L.Y., Jiang Z., Paridaens R., Tan A.R., Awada A., Ranade A., Jiao S., Schwartz G., et al. Neratinib, an irreversible ErbB receptor tyrosine kinase inhibitor, in patients with advanced ErbB2-positive breast cancer. J. Clin. Oncol. 2010;28:1301–1307. doi: 10.1200/JCO.2009.25.8707. [DOI] [PubMed] [Google Scholar]
- 20.Baselga J., Campone M., Piccart M., Burris H.A., Rugo H.S., Sahmoud T., Noguchi S., Gnant M., Pritchard K.I., Lebrun F., et al. Everolimus in Postmenopausal Hormone-Receptor–Positive Advanced Breast Cancer. N. Engl. J. Med. 2012;366:520–529. doi: 10.1056/NEJMoa1109653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Beaver J.A., Amiri-Kordestani L., Charlab R., Chen W., Palmby T., Tilley A., Zirkelbach J.F., Yu J., Liu Q., Zhao L., et al. FDA Approval: Palbociclib for the Treatment of Postmenopausal Patients with Estrogen Receptor-Positive, HER2-Negative Metastatic Breast Cancer. Clin. Cancer Res. 2015;21:4760–4766. doi: 10.1158/1078-0432.CCR-15-1185. [DOI] [PubMed] [Google Scholar]
- 22.Hortobagyi G.N., Stemmer S.M., Burris H.A., Yap Y.-S., Sonke G.S., Paluch-Shimon S., Campone M., Blackwell K.L., André F., Winer E.P., et al. Ribociclib as First-Line Therapy for HR-Positive, Advanced Breast Cancer. N. Engl. J. Med. 2016;375:1738–1748. doi: 10.1056/NEJMoa1609709. [DOI] [PubMed] [Google Scholar]
- 23.Patnaik A., Rosen L.S., Tolaney S.M., Tolcher A.W., Goldman J.W., Gandhi L., Papadopoulos K.P., Beeram M., Rasco D.W., Hilton J.F., et al. Efficacy and safety of Abemaciclib, an inhibitor of CDK4 and CDK6, for patients with breast cancer, non–small cell lung cancer, and other solid tumors. Cancer Discov. 2016;6:740–753. doi: 10.1158/2159-8290.CD-16-0095. [DOI] [PubMed] [Google Scholar]
- 24.Tutt A., Robson M., Garber J.E., Domchek S.M., Audeh M.W., Weitzel J.N., Friedlander M., Arun B., Loman N., Schmutzler R.K., et al. Oral poly(ADP-ribose) polymerase inhibitor olaparib in patients with BRCA1 or BRCA2 mutations and advanced breast cancer: A proof-of-concept trial. Lancet. 2010;376:235–244. doi: 10.1016/S0140-6736(10)60892-6. [DOI] [PubMed] [Google Scholar]
- 25.Taha Z., J. Janse van Rensburg H., Yang X. The Hippo Pathway: Immunity and Cancer. Cancers. 2018;10:94. doi: 10.3390/cancers10040094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Halder G., Johnson R.L. Hippo signaling: Growth control and beyond. Development. 2011;138:9–22. doi: 10.1242/dev.045500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ramos A., Camargo F.D. The Hippo signaling pathway and stem cell biology. Trends Cell Biol. 2012;22:339–346. doi: 10.1016/j.tcb.2012.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Liu C.-Y., Zha Z.-Y., Zhou X., Zhang H., Huang W., Zhao D., Li T., Chan S.W., Lim C.J., Hong W., et al. The Hippo Tumor Pathway Promotes TAZ Degradation by Phosphorylating a Phosphodegron and Recruiting the SCFβ-TrCP E3 Ligase. J. Biol. Chem. 2010;285:37159–37169. doi: 10.1074/jbc.M110.152942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhao B., Li L., Tumaneng K., Wang C.-Y., Guan K.-L. A coordinated phosphorylation by Lats and CK1 regulates YAP stability through SCF(β-TRCP) Genes Dev. 2010;24:72–85. doi: 10.1101/gad.1843810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yu F.X., Guan K.L. The Hippo pathway: Regulators and regulations. Genes Dev. 2013;27:355–371. doi: 10.1101/gad.210773.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Holden J.K., Cunningham C.N. Targeting the Hippo Pathway and Cancer through the TEAD Family of Transcription Factors. Cancers. 2018;10:81. doi: 10.3390/cancers10030081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhao B., Ye X., Yu J., Li L., Li W., Li S., Yu J., Lin J.D., Wang C.-Y., Chinnaiyan A.M., et al. TEAD mediates YAP-dependent gene induction and growth control. Genes Dev. 2008;22:1962–1971. doi: 10.1101/gad.1664408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lai D., Ho K.C., Hao Y., Yang X. Taxol resistance in breast cancer cells is mediated by the hippo pathway component TAZ and its downstream transcriptional targets Cyr61 and CTGF. Cancer Res. 2011;71:2728–2738. doi: 10.1158/0008-5472.CAN-10-2711. [DOI] [PubMed] [Google Scholar]
- 34.Xu M.Z., Chan S.W., Liu A.M., Wong K.F., Fan S.T., Chen J., Poon R.T., Zender L., Lowe S.W., Hong W., et al. AXL receptor kinase is a mediator of YAP-dependent oncogenic functions in hepatocellular carcinoma. Oncogene. 2011;30:1229–1240. doi: 10.1038/onc.2010.504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zeng Q., Hong W. The Emerging Role of the Hippo Pathway in Cell Contact Inhibition, Organ Size Control, and Cancer Development in Mammals. Cancer Cell. 2008;13:188–192. doi: 10.1016/j.ccr.2008.02.011. [DOI] [PubMed] [Google Scholar]
- 36.Piccolo S., Dupont S., Cordenonsi M. The Biology of YAP/TAZ: Hippo Signaling and Beyond. Physiol. Rev. 2014;94:1287–1312. doi: 10.1152/physrev.00005.2014. [DOI] [PubMed] [Google Scholar]
- 37.Edwards D.N., Ngwa V.M., Wang S., Shiuan E., Brantley-Sieders D.M., Kim L.C., Reynolds A.B., Chen J. The receptor tyrosine kinase EphA2 promotes glutamine metabolism in tumors by activating the transcriptional coactivators YAP and TAZ. Sci. Signal. 2017;10:eaan4667. doi: 10.1126/scisignal.aan4667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.St John M.A.R., Tao W., Fei X., Fukumoto R., Carcangiu M.L., Brownstein D.G., Parlow A.F., McGrath J., Xu T. Mice deficient of Lats1 develop soft-tissue sarcomas, ovarian tumours and pituitary dysfunction. Nat. Genet. 1999;21:182–186. doi: 10.1038/5965. [DOI] [PubMed] [Google Scholar]
- 39.Yang X., Li D.M., Chen W., Xu T. Human homologue of Drosophila lats, LATS1, negatively regulate growth by inducing G2/M arrest or apoptosis. Oncogene. 2001;20:6516–6523. doi: 10.1038/sj.onc.1204817. [DOI] [PubMed] [Google Scholar]
- 40.Vlug E.J., van de Ven R.A.H., Vermeulen J.F., Bult P., van Diest P.J., Derksen P.W.B. Nuclear localization of the transcriptional coactivator YAP is associated with invasive lobular breast cancer. Cell. Oncol. 2013;36:375–384. doi: 10.1007/s13402-013-0143-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Maugeri-Saccà M., Barba M., Pizzuti L., Vici P., Di Lauro L., Dattilo R., Vitale I., Bartucci M., Mottolese M., De Maria R. The Hippo transducers TAZ and YAP in breast cancer: Oncogenic activities and clinical implications. Expert Rev. Mol. Med. 2015;17:e14. doi: 10.1017/erm.2015.12. [DOI] [PubMed] [Google Scholar]
- 42.Kim S.K., Jung W.H., Koo J.S. Yes-associated protein (YAP) is differentially expressed in tumor and stroma according to the molecular subtype of breast cancer. Int. J. Clin. Exp. Pathol. 2014;7:3224–3234. [PMC free article] [PubMed] [Google Scholar]
- 43.Lamar J.M., Stern P., Liu H., Schindler J.W., Jiang Z.-G., Hynes R.O. The Hippo pathway target, YAP, promotes metastasis through its TEAD-interaction domain. Proc. Natl. Acad. Sci. USA. 2012;109:E2441–E2450. doi: 10.1073/pnas.1212021109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Overholtzer M., Zhang J., Smolen G.A., Muir B., Li W., Sgroi D.C., Deng C.-X., Brugge J.S., Haber D.A. Transforming properties of YAP, a candidate oncogene on the chromosome 11q22 amplicon. Proc. Natl. Acad. Sci. USA. 2006;103:12405–12410. doi: 10.1073/pnas.0605579103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Basu S., Totty N.F., Irwin M.S., Sudol M., Downward J. Akt Phosphorylates the Yes-Associated Protein, YAP, to Induce Interaction with 14-3-3 and Attenuation of p73-Mediated Apoptosis. Mol. Cell. 2003;11:11–23. doi: 10.1016/S1097-2765(02)00776-1. [DOI] [PubMed] [Google Scholar]
- 46.Matallanas D., Romano D., Yee K., Meissl K., Kucerova L., Piazzolla D., Baccarini M., Vass J.K., Kolch W., O’Neill E. RASSF1A Elicits Apoptosis through an MST2 Pathway Directing Proapoptotic Transcription by the p73 Tumor Suppressor Protein. Mol. Cell. 2007;27:962–975. doi: 10.1016/j.molcel.2007.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Strano S., Monti O., Pediconi N., Baccarini A., Fontemaggi G., Lapi E., Mantovani F., Damalas A., Citro G., Sacchi A., et al. The Transcriptional Coactivator Yes-Associated Protein Drives p73 Gene-Target Specificity in Response to DNA Damage. Mol. Cell. 2005;18:447–459. doi: 10.1016/j.molcel.2005.04.008. [DOI] [PubMed] [Google Scholar]
- 48.Yuan M., Tomlinson V., Lara R., Holliday D., Chelala C., Harada T., Gangeswaran R., Manson-Bishop C., Smith P., Danovi S.A., et al. Yes-associated protein (YAP) functions as a tumor suppressor in breast. Cell Death Differ. 2008;15:1752–1759. doi: 10.1038/cdd.2008.108. [DOI] [PubMed] [Google Scholar]
- 49.Danovi S.A., Rossi M., Gudmundsdottir K., Yuan M., Melino G., Basu S. Yes-Associated Protein (YAP) is a critical mediator of c-Jun-dependent apoptosis. Cell Death Differ. 2008;15:217–219. doi: 10.1038/sj.cdd.4402226. [DOI] [PubMed] [Google Scholar]
- 50.Levy D., Adamovich Y., Reuven N., Shaul Y. The Yes-associated protein 1 stabilizes p73 by preventing Itch-mediated ubiquitination of p73. Cell Death Differ. 2007;14:743–751. doi: 10.1038/sj.cdd.4402063. [DOI] [PubMed] [Google Scholar]
- 51.Strano S., Munarriz E., Rossi M., Castagnoli L., Shaul Y., Sacchi A., Oren M., Sudol M., Cesareni G., Blandino G. Physical Interaction with Yes-associated Protein Enhances p73 Transcriptional Activity. J. Biol. Chem. 2001;276:15164–15173. doi: 10.1074/jbc.M010484200. [DOI] [PubMed] [Google Scholar]
- 52.Camargo F.D., Gokhale S., Johnnidis J.B., Fu D., Bell G.W., Jaenisch R., Brummelkamp T.R. YAP1 Increases Organ Size and Expands Undifferentiated Progenitor Cells. Curr. Biol. 2007;17:2054–2060. doi: 10.1016/j.cub.2007.10.039. [DOI] [PubMed] [Google Scholar]
- 53.Komuro A., Nagai M., Navin N.E., Sudol M. WW domain-containing protein YAP associates with ErbB-4 and acts as a co-transcriptional activator for the carboxyl-terminal fragment of ErbB-4 that translocates to the nucleus. J. Biol. Chem. 2003;278:33334–33341. doi: 10.1074/jbc.M305597200. [DOI] [PubMed] [Google Scholar]
- 54.Moroishi T., Hayashi T., Pan W.-W., Fujita Y., Holt M.V., Qin J., Carson D.A., Guan K.-L. The Hippo Pathway Kinases LATS1/2 Suppress Cancer Immunity. Cell. 2016;167:1525–1539.e17. doi: 10.1016/j.cell.2016.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Elster D., Tollot M., Schlegelmilch K., Ori A., Rosenwald A., Sahai E., von Eyss B. TRPS1 shapes YAP/TEAD-dependent transcription in breast cancer cells. Nat. Commun. 2018;9:3115. doi: 10.1038/s41467-018-05370-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Tomlinson V., Gudmundsdottir K., Luong P., Leung K.-Y., Knebel A., Basu S. JNK phosphorylates Yes-associated protein (YAP) to regulate apoptosis. Cell Death Dis. 2010;1:e29. doi: 10.1038/cddis.2010.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Yuan M., Luong P., Hudson C., Gudmundsdottir K., Basu S. c-Abl phosphorylation of ΔNp63α is critical for cell viability. Cell Death Dis. 2010;1:e16. doi: 10.1038/cddis.2009.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Siew W.C., Chun J.L., Guo K., Chee P.N., Lee I., Hunziker W., Zeng Q., Hong W. A role for TAZ in migration, invasion, and tumorigenesis of breast cancer cells. Cancer Res. 2008;68:2592–2598. doi: 10.1158/0008-5472.CAN-07-2696. [DOI] [PubMed] [Google Scholar]
- 59.Bartucci M., Dattilo R., Moriconi C., Pagliuca A., Mottolese M., Federici G., Di Benedetto A., Todaro M., Stassi G., Sperati F., et al. TAZ is required for metastatic activity and chemoresistance of breast cancer stem cells. Oncogene. 2015;34:681–690. doi: 10.1038/onc.2014.5. [DOI] [PubMed] [Google Scholar]
- 60.Díaz-Martín J., López-García M.Á., Romero-Pérez L., Atienza-Amores M.R., Pecero M.L., Castilla M.Á., Biscuola M., Santón A., Palacios J. Nuclear TAZ expression associates with the triple-negative phenotype in breast cancer. Endocr. Relat. Cancer. 2015;22:443–454. doi: 10.1530/ERC-14-0456. [DOI] [PubMed] [Google Scholar]
- 61.Zhao D., Zhi X., Zhou Z., Chen C. TAZ antagonizes the WWP1-mediated KLF5 degradation and promotes breast cell proliferation and tumorigenesis. Carcinogenesis. 2012;33:59–67. doi: 10.1093/carcin/bgr242. [DOI] [PubMed] [Google Scholar]
- 62.Bendinelli P., Maroni P., Matteucci E., Luzzati A., Perrucchini G., Desiderio M.A. Hypoxia inducible factor-1 is activated by transcriptional co-activator with PDZ-binding motif (TAZ) versus WWdomain-containing oxidoreductase (WWOX) in hypoxic microenvironment of bone metastasis from breast cancer. Eur. J. Cancer. 2013;49:2608–2618. doi: 10.1016/j.ejca.2013.03.002. [DOI] [PubMed] [Google Scholar]
- 63.Cordenonsi M., Zanconato F., Azzolin L., Forcato M., Rosato A., Frasson C., Inui M., Montagner M., Parenti A.R., Poletti A., et al. The hippo transducer TAZ confers cancer stem cell-related traits on breast cancer cells. Cell. 2011;147:759–772. doi: 10.1016/j.cell.2011.09.048. [DOI] [PubMed] [Google Scholar]
- 64.Xiang L., Gilkes D.M., Hu H., Takano N., Luo W., Lu H., Bullen J.W., Samanta D., Liang H., Semenza G.L. Hypoxia-inducible factor 1 mediates TAZ expression and nuclear localization to induce the breast cancer stem cell phenotype. Oncotarget. 2014;5:12509–12527. doi: 10.18632/oncotarget.2997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Frangou C., Li Y.-W., Shen H., Yang N., Wilson K.E., Blijlevens M., Guo J., Nowak N.J., Zhang J. Molecular profiling and computational network analysis of TAZ-mediated mammary tumorigenesis identifies actionable therapeutic targets. Oncotarget. 2014;5:1–11. doi: 10.18632/oncotarget.2570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Chang C., Goel H.L., Gao H., Pursell B., Shultz L.D., Greiner D.L., Ingerpuu S., Patarroyo M., Cao S., Lim E., et al. A laminin 511 matrix is regulated by Taz and functions as the ligand for the α6Bβ1 integrin to sustain breast cancer stem cells. Genes Dev. 2015;29:1–6. doi: 10.1101/gad.253682.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Zhang H., Liu C.-Y., Zha Z.-Y., Zhao B., Yao J., Zhao S., Xiong Y., Lei Q.-Y., Guan K.-L. TEAD Transcription Factors Mediate the Function of TAZ in Cell Growth and Epithelial-Mesenchymal Transition. J. Biol. Chem. 2009;284:13355–13362. doi: 10.1074/jbc.M900843200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Hiemer S.E., Szymaniak A.D., Varelas X. The Transcriptional Regulators TAZ and YAP Direct Transforming Growth Factor β-induced Tumorigenic Phenotypes in Breast Cancer Cells. J. Biol. Chem. 2014;289:13461–13474. doi: 10.1074/jbc.M113.529115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Lai D., Yang X. BMP4 is a novel transcriptional target and mediator of mammary cell migration downstream of the Hippo pathway component TAZ. Cell. Signal. 2013;25:1720–1728. doi: 10.1016/j.cellsig.2013.05.002. [DOI] [PubMed] [Google Scholar]
- 70.Wang Z., Wu Y., Wang H., Zhang Y., Mei L., Fang X., Zhang X., Zhang F., Chen H., Liu Y., et al. Interplay of mevalonate and Hippo pathways regulates RHAMM transcription via YAP to modulate breast cancer cell motility. Proc. Natl. Acad. Sci. USA. 2014;111:E89–E98. doi: 10.1073/pnas.1319190110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Zhi X., Zhao D., Zhou Z., Liu R., Chen C. YAP promotes breast cell proliferation and survival partially through stabilizing the KLF5 transcription factor. Am. J. Pathol. 2012;180:2452–2461. doi: 10.1016/j.ajpath.2012.02.025. [DOI] [PubMed] [Google Scholar]
- 72.Calvo F., Ege N., Grande-Garcia A., Hooper S., Jenkins R.P., Chaudhry S.I., Harrington K., Williamson P., Moeendarbary E., Charras G., et al. Mechanotransduction and YAP-dependent matrix remodelling is required for the generation and maintenance of cancer-associated fibroblasts. Nat. Cell Biol. 2013;15:637–646. doi: 10.1038/ncb2756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Lin X., Cai F., Li X., Kong X. Prognostic significance of mammalian sterile 20-like kinase 1 in breast cancer. Tumor Biol. 2013;34:3239–3243. doi: 10.1007/s13277-013-0895-8. [DOI] [PubMed] [Google Scholar]
- 74.Cheung W.L., Ajiro K., Samejima K., Kloc M., Cheung P., Mizzen C.A., Beeser A., Etkin L.D., Chernoff J., Earnshaw W.C., et al. Apoptotic phosphorylation of histone H2B is mediated by mammalian sterile twenty kinase. Cell. 2003;113:507–517. doi: 10.1016/S0092-8674(03)00355-6. [DOI] [PubMed] [Google Scholar]
- 75.Vichalkovski A., Gresko E., Cornils H., Hergovich A., Schmitz D., Hemmings B.A. NDR Kinase Is Activated by RASSF1A/MST1 in Response to Fas Receptor Stimulation and Promotes Apoptosis. Curr. Biol. 2008;18:1889–1895. doi: 10.1016/j.cub.2008.10.060. [DOI] [PubMed] [Google Scholar]
- 76.Wu H., Xiao Y., Zhang S., Ji S., Wei L., Fan F., Geng J., Tian J., Sun X., Qin F., et al. The Ets transcription factor GABP is a component of the hippo pathway essential for growth and antioxidant defense. Cell Rep. 2013;3:1663–1677. doi: 10.1016/j.celrep.2013.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Lehtinen M.K., Yuan Z., Boag P.R., Yang Y., Villén J., Becker E.B.E., DiBacco S., de la Iglesia N., Gygi S., Blackwell T.K., Bonni A. A Conserved MST-FOXO Signaling Pathway Mediates Oxidative-Stress Responses and Extends Life Span. Cell. 2006;125:987–1001. doi: 10.1016/j.cell.2006.03.046. [DOI] [PubMed] [Google Scholar]
- 78.Visser S., Yang X. LATS tumor suppressor: A new governor of cellular homeostasis. Cell Cycle. 2010;9:3892–3903. doi: 10.4161/cc.9.19.13386. [DOI] [PubMed] [Google Scholar]
- 79.Hirota T., Morisaki T., Nishiyama Y., Marumoto T., Tada K., Hara T., Masuko N., Inagaki M., Hatakeyama K., Saya H. Zyxin, a regulator of actin filament assembly, targets the mitotic apparatus by interacting with h-warts/LATS1 tumor suppressor. J. Cell Biol. 2000;149:1073–1086. doi: 10.1083/jcb.149.5.1073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Yang X., Yu K., Hao Y., Li D.M., Stewart R., Insogna K.L., Xu T. LATS1 tumour suppressor affects cytokinesis by inhibiting LIMK1. Nat. Cell Biol. 2004;6:609–617. doi: 10.1038/ncb1140. [DOI] [PubMed] [Google Scholar]
- 81.Visser-Grieve S., Zhou Z., She Y.M., Huang H., Cyr T.D., Xu T., Yang X. LATS1 tumor suppressor is a novel actin-binding protein and negative regulator of actin polymerization. Cell Res. 2011;21:1513–1516. doi: 10.1038/cr.2011.122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Chan S.W., Lim C.J., Guo F., Tan I., Leung T., Hong W. Actin-binding and Cell Proliferation Activities of Angiomotin Family Members Are Regulated by Hippo Pathway-mediated Phosphorylation. J. Biol. Chem. 2013;288:37296–37307. doi: 10.1074/jbc.M113.527598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Britschgi A., Duss S., Kim S., Couto J.P., Brinkhaus H., Koren S., De Silva D., Mertz K.D., Kaup D., Varga Z., et al. The Hippo kinases LATS1 and 2 control human breast cell fate via crosstalk with ERα. Nature. 2017;541:541–545. doi: 10.1038/nature20829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Shi P., Feng J., Chen C. Hippo pathway in mammary gland development and breast cancer. Acta Biochim. Biophys. Sin. (Shanghai) 2014;47:53–59. doi: 10.1093/abbs/gmu114. [DOI] [PubMed] [Google Scholar]
- 85.Zhao Y., Yang X. Regulation of sensitivity of tumor cells to antitubulin drugs by Cdk1-TAZ signalling. Oncotarget. 2015;6:21906–21917. doi: 10.18632/oncotarget.4259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Zhao Y., Yang X. Targeting the Hippo Pathway to Improve Response to Chemotherapy. In: Johnson D.E., editor. Targeting Cell Survival Pathways to Enhance Response to Chemotherapy. Volume 3. Elsevier; London, UK: 2019. pp. 169–185. [Google Scholar]
- 87.Zhao Y., Khanal P., Savage P., She Y.M., Cyr T.D., Yang X. YAP-induced resistance of cancer cells to antitubulin drugs is modulated by a hippo-independent pathway. Cancer Res. 2014;74:4493–4503. doi: 10.1158/0008-5472.CAN-13-2712. [DOI] [PubMed] [Google Scholar]
- 88.Takahashi Y., Miyoshi Y., Morimoto K., Taguchi T., Tamaki Y., Noguchi S. Low LATS2 mRNA level can predict favorable response to epirubicin plus cyclophosphamide, but not to docetaxel, in breast cancers. J. Cancer Res. Clin. Oncol. 2007;133:501–509. doi: 10.1007/s00432-007-0194-0. [DOI] [PubMed] [Google Scholar]
- 89.Vici P., Mottolese M., Pizzuti L., Barba M., Sperati F., Terrenato I., Di Benedetto A., Natoli C., Gamucci T., Angelucci D., et al. The Hippo transducer TAZ as a biomarker of pathological complete response in HER2-positive breast cancer patients treated with trastuzumab-based neoadjuvant therapy. Oncotarget. 2014;5:9619–9625. doi: 10.18632/oncotarget.2449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Lin C.-H., Pelissier F.A., Zhang H., Lakins J., Weaver V.M., Park C., LaBarge M.A. Microenvironment rigidity modulates responses to the HER2 receptor tyrosine kinase inhibitor lapatinib via YAP and TAZ transcription factors. Mol. Biol. Cell. 2015;26:3946–3953. doi: 10.1091/mbc.e15-07-0456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Kim M.H., Kim J. Role of YAP/TAZ transcriptional regulators in resistance to anti-cancer therapies. Cell. Mol. Life Sci. 2017;74:1457–1474. doi: 10.1007/s00018-016-2412-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Shou J., Massarweh S., Osborne C.K., Wakeling A.E., Ali S., Weiss H., Schiff R. Mechanisms of Tamoxifen Resistance: Increased Estrogen Receptor—HER2 / neu Cross—Talk in ER/HER2—Positive Breast Cancer. JNCI J. Natl. Cancer Inst. 2004;96:926–935. doi: 10.1093/jnci/djh166. [DOI] [PubMed] [Google Scholar]
- 93.Lit L.C., Scott S., Zhang H., Stebbing J., Photiou A., Giamas G. LATS2 is a modulator of estrogen receptor alpha. Anticancer Res. 2013;33:53–63. [PubMed] [Google Scholar]
- 94.Monia B.P., Johnston J.F., Geiger T., Muller M., Fabbro D. Antitumor activity of a phosphorothioate antisense oligodeoxynucleotide targeted against C-raf kinase. Nat. Med. 1996;2:668–675. doi: 10.1038/nm0696-668. [DOI] [PubMed] [Google Scholar]
- 95.O’Neill E. Role of the Kinase MST2 in Suppression of Apoptosis by the Proto-Oncogene Product Raf-1. Science. 2004;306:2267–2270. doi: 10.1126/science.1103233. [DOI] [PubMed] [Google Scholar]
- 96.Khazak V., Astsaturov I., Serebriiskii I.G., Golemis E.A. Selective Raf inhibition in cancer therapy. Expert Opin. Ther. Targets. 2007;11:1587–1609. doi: 10.1517/14728222.11.12.1587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Sun S., Irvine K.D. Cellular Organization and Cytoskeletal Regulation of the Hippo Signaling Network. Trends Cell Biol. 2016;26:694–704. doi: 10.1016/j.tcb.2016.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.El Sayed K.A., Khanfar M.A., Shallal H.M., Muralidharan A., Awate B., Youssef D.T.A., Liu Y., Zhou Y.D., Nagle D.G., Shah G. Latrunculin A and its C-17-O-carbamates inhibit prostate tumor cell invasion and HIF-1 activation in breast tumor cells. J. Nat. Prod. 2008;71:396–402. doi: 10.1021/np070587w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Khanfar M.A., Youssef D.T.A., El Sayed K.A. Semisynthetic latrunculin derivatives as inhibitors of metastatic breast cancer: Biological evaluations, preliminary structure-activity relationship and molecular modeling studies. ChemMedChem. 2010;5:274–285. doi: 10.1002/cmdc.200900430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Bruna A., Greenwood W., Le Quesne J., Teschendorff A., Miranda-Saavedra D., Rueda O.M., Sandoval J.L., Vidakovic A.T., Saadi A., Pharoah P., et al. TGFβ induces the formation of tumour-initiating cells in claudinlow breast cancer. Nat. Commun. 2012;3:1055. doi: 10.1038/ncomms2039. [DOI] [PubMed] [Google Scholar]
- 101.Leonel C., Ferreira L.C., Borin T.F., Moschetta M.G., Freitas G.S., Haddad M.R., de Camargos Pinto Robles J.A., Aparecida Pires de Campos Zuccari D. Inhibition of Epithelial-mesenchymal Transition in Response to Treatment with Metformin and Y27632 in Breast Cancer Cell Lines. Anticancer Agents Med. Chem. 2017;17 doi: 10.2174/1871520617666170102153954. [DOI] [PubMed] [Google Scholar]
- 102.Pille J.Y., Denoyelle C., Varet J., Bertrand J.R., Soria J., Opolon P., Lu H., Pritchard L.L., Vannier J.P., Malvy C., et al. Anti-RhoA and anti-RhoC siRNAs inhibit the proliferation and invasiveness of MDA-MB-231 breast cancer cells in vitro and in vivo. Mol. Ther. 2005;11:267–274. doi: 10.1016/j.ymthe.2004.08.029. [DOI] [PubMed] [Google Scholar]
- 103.Borgquist S., Bjarnadottir O., Kimbung S., Ahern T.P. Statins: A role in breast cancer therapy? J. Intern. Med. 2018;284:346–357. doi: 10.1111/joim.12806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Kochhar R., Khurana V., Bejjanki H., Caldito G., Fort C. Statins to reduce breast cancer risk: A case control study in U.S. female veterans. J. Clin. Oncol. 2005;23:514. doi: 10.1200/jco.2005.23.16_suppl.514. [DOI] [Google Scholar]
- 105.Han H., Qi R., Zhou J.J., Ta A.P., Yang B., Nakaoka H.J., Seo G., Guan K.-L., Luo R., Wang W. Regulation of the Hippo Pathway by Phosphatidic Acid-Mediated Lipid-Protein Interaction. Mol. Cell. 2018;72:328–340.e8. doi: 10.1016/j.molcel.2018.08.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Serrano I., McDonald P.C., Lock F., Muller W.J., Dedhar S. Inactivation of the Hippo tumour suppressor pathway by integrin-linked kinase. Nat. Commun. 2013;4:2976. doi: 10.1038/ncomms3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Kalra J., Warburton C., Fang K., Edwards L., Daynard T., Waterhouse D., Dragowska W., Sutherland B.W., Dedhar S., Gelmon K., et al. QLT0267, a small molecule inhibitor targeting integrin-linked kinase (ILK), and docetaxel can combine to produce synergistic interactions linked to enhanced cytotoxicity, reductions in P-AKT levels, altered F-actin architecture and improved treatment outc. Breast Cancer Res. 2009;11:R25. doi: 10.1186/bcr2252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Johnson R., Halder G. The two faces of Hippo: Targeting the Hippo pathway for regenerative medicine and cancer treatment. Nat. Rev. Drug Discov. 2014;13:63–79. doi: 10.1038/nrd4161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Finn R.S., Bengala C., Ibrahim N., Roché H., Sparano J., Strauss L.C., Fairchild J., Sy O., Goldstein L.J. Dasatinib as a single agent in triple-negative breast cancer: Results of an open-label phase 2 study. Clin. Cancer Res. 2011;17:6905–6913. doi: 10.1158/1078-0432.CCR-11-0288. [DOI] [PubMed] [Google Scholar]
- 110.Marzano C., Gandin V., Folda A., Scutari G., Bindoli A., Rigobello M.P. Inhibition of thioredoxin reductase by auranofin induces apoptosis in cisplatin-resistant human ovarian cancer cells. Free Radic. Biol. Med. 2007;42:872–881. doi: 10.1016/j.freeradbiomed.2006.12.021. [DOI] [PubMed] [Google Scholar]
- 111.Wang Y., Justilien V., Brennan K.I., Jamieson L., Murray N.R., Fields A.P. PKCι regulates nuclear YAP1 localization and ovarian cancer tumorigenesis. Oncogene. 2017;36:534–545. doi: 10.1038/onc.2016.224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Varghese E., Büsselberg D. Auranofin, an anti-rheumatic gold compound, modulates apoptosis by elevating the intracellular calcium concentration ([Ca2+]i) in MCF-7 breast cancer cells. Cancers. 2014;6:2243–2258. doi: 10.3390/cancers6042243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Devaiah B.N., Case-Borden C., Gegonne A., Hsu C.H., Chen Q., Meerzaman D., Dey A., Ozato K., Singer D.S. BRD4 is a histone acetyltransferase that evicts nucleosomes from chromatin. Nat. Struct. Mol. Biol. 2016;23:540–548. doi: 10.1038/nsmb.3228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Zanconato F., Battilana G., Forcato M., Filippi L., Azzolin L., Manfrin A., Quaranta E., Di Biagio D., Sigismondo G., Guzzardo V., et al. Transcriptional addiction in cancer cells is mediated by YAP/TAZ through BRD4. Nat. Med. 2018;24:1599–1610. doi: 10.1038/s41591-018-0158-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Zakikhani M., Dowling R., Fantus I.G., Sonenberg N., Pollak M. Metformin is an AMP kinase-dependent growth inhibitor for breast cancer cells. Cancer Res. 2006;66:10269–10273. doi: 10.1158/0008-5472.CAN-06-1500. [DOI] [PubMed] [Google Scholar]
- 116.deRan M., Yang J., Shen C.H., Peters E.C., Fitamant J., Chan P., Hsieh M., Zhu S., Asara J.M., Zheng B., et al. Energy stress regulates Hippo-YAP signaling involving AMPK-mediated regulation of angiomotin-like 1 protein. Cell Rep. 2014;9:495–503. doi: 10.1016/j.celrep.2014.09.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Yee D., Paoloni M., van’t Veer L., Sanil A., Yau C., Forero A., Chien A., Wallace A., Moulder S., Albain K., et al. Abstract P6-11-04: The evaluation of ganitumab/metformin plus standard neoadjuvant therapy in high-risk breast cancer: Results from the I-SPY 2 trial. Cancer Res. 2017;77:P6-11-04. doi: 10.1158/1538-7445.SABCS16-P6-11-04. [DOI] [Google Scholar]
- 118.Sun H., Ying M. Abstract 4444: Small molecule drug Verteporfin inhibits TAZ/YAP-driven signaling and tumorigenicity of breast cancer cells. Cancer Res. 2015;75:4444. doi: 10.1158/1538-7445.AM2015-4444. [DOI] [Google Scholar]
- 119.Sulaiman A., Yao Z.-M., Wang L.-S. Re-evaluating the role of epithelial-mesenchymal-transition in cancer progression. J. Biomed. Res. 2018;32:81–90. doi: 10.7555/JBR.31.20160124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Isakoff S.J., Rogers G.S., Hill S., McMullan P., Habin K.R., Park H., Bartenstein D.W., Chen S.T., Barry W.T., Overmoyer B. An open label, phase II trial of continuous low-irradiance photodynamic therapy (CLIPT) using verteporfin for the treatment of cutaneous breast cancer metastases. J. Clin. Oncol. 2017;35:TPS1121. doi: 10.1200/JCO.2017.35.15_suppl.TPS1121. [DOI] [Google Scholar]
- 121.Gong R., Hong A.W., Plouffe S.W., Zhao B., Liu G., Yu F.X., Xu Y., Guan K.L. Opposing roles of conventional and novel PKC isoforms in Hippo-YAP pathway regulation. Cell Res. 2015;25:985–988. doi: 10.1038/cr.2015.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Zhang H., Ramakrishnan S.K., Triner D., Centofanti B., Maitra D., Győrffy B., Sebolt-Leopold J.S., Dame M.K., Varani J., Brenner D.E., et al. Tumor-selective proteotoxicity of verteporfin inhibits colon cancer progression independently of YAP1. Sci. Signal. 2015;8:ra98. doi: 10.1126/scisignal.aac5418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Liu-Chittenden Y., Huang B., Shim J.S., Chen Q., Lee S.-J., Anders R.A., Liu J.O., Pan D. Genetic and pharmacological disruption of the TEAD–YAP complex suppresses the oncogenic activity of YAP. Genes Dev. 2012;26:1300–1305. doi: 10.1101/gad.192856.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Wang W., Li N., Li X., Tran M.K., Han X., Chen J. Tankyrase Inhibitors Target YAP by Stabilizing Angiomotin Family Proteins. Cell Rep. 2015;13:524–532. doi: 10.1016/j.celrep.2015.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Troilo A., Benson E.K., Esposito D., Garibsingh R.A., Reddy E.P., Mungamuri S.K., Aaronson S.A. Angiomotin stabilization by tankyrase inhibitors antagonizes constitutive TEAD-dependent transcription and proliferation of human tumor cells with Hippo pathway core component mutations. Oncotarget. 2016;7:28765–28782. doi: 10.18632/oncotarget.9117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Johnson J.P.S., Kumar P., Koulnis M., Patel M., Simin K. Crucial and novel cancer drivers in a mouse model of triple-negative breast cancer. Cancer Genomics Proteomics. 2014;11:115–126. doi: 10.1038/sj.cdd.4401094. [DOI] [PubMed] [Google Scholar]
- 127.Oku Y., Nishiya N., Shito T., Yamamoto R., Yamamoto Y., Oyama C., Uehara Y. Small molecules inhibiting the nuclear localization of YAP/TAZ for chemotherapeutics and chemosensitizers against breast cancers. FEBS Open Bio. 2015;5:542–549. doi: 10.1016/j.fob.2015.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Zhou Z., Hu T., Xu Z., Lin Z., Zhang Z., Feng T., Zhu L., Rong Y., Shen H., Luk J.M., et al. Targeting Hippo pathway by specific interruption of YAP-TEAD interaction using cyclic YAP-like peptides. FASEB J. 2015;29:724–732. doi: 10.1096/fj.14-262980. [DOI] [PubMed] [Google Scholar]
- 129.Morrison H., Sherman L.S., Legg J., Banine F., Isacke C., Haipek C.A., Gutmann D.H., Ponta H., Herrlich P. The NF2 tumor suppressor gene product, merlin, mediates contact inhibition of growth through interactions\rwith CD44. Genes Dev. 2001;15:968–980. doi: 10.1101/gad.189601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Varelas X., Miller B.W., Sopko R., Song S., Gregorieff A., Fellouse F.A., Sakuma R., Pawson T., Hunziker W., McNeill H., et al. The Hippo Pathway Regulates Wnt/β-Catenin Signaling. Dev. Cell. 2010;18:579–591. doi: 10.1016/j.devcel.2010.03.007. [DOI] [PubMed] [Google Scholar]
- 131.Ye S., Eisinger-Mathason T.S.K. Targeting the Hippo pathway: Clinical implications and therapeutics. Pharmacol. Res. 2016;103:270–278. doi: 10.1016/j.phrs.2015.11.025. [DOI] [PubMed] [Google Scholar]
- 132.Hong X., Nguyen H.T., Chen Q., Zhang R., Hagman Z., Voorhoeve P.M., Cohen S.M. Opposing activities of the Ras and Hippo pathways converge on regulation of YAP protein turnover. EMBO J. 2014;33:2447–2457. doi: 10.15252/embj.201489385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Huang J., Kalderon D. Coupling of Hedgehog and Hippo pathways promotes stem cell maintenance by stimulating proliferation. J. Cell Biol. 2014;205:325–338. doi: 10.1083/jcb.201309141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Yu J., Poulton J., Huang Y.-C., Deng W.-M. The hippo pathway promotes Notch signaling in regulation of cell differentiation, proliferation, and oocyte polarity. PLoS ONE. 2008;3:e1761. doi: 10.1371/journal.pone.0001761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Azad T., Janse van Rensburg H.J., Lightbody E.D., Neveu B., Champagne A., Ghaffari A., Kay V.R., Hao Y., Shen H., Yeung B., et al. A LATS biosensor screen identifies VEGFR as a regulator of the Hippo pathway in angiogenesis. Nat. Commun. 2018;9:1061. doi: 10.1038/s41467-018-03278-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Liu C.Y., Lv X., Li T., Xu Y., Zhou X., Zhao S., Xiong Y., Lei Q.Y., Guan K.L. PP1 cooperates with ASPP2 to dephosphorylate and activate TAZ. J. Biol. Chem. 2011;286:5558–5566. doi: 10.1074/jbc.M110.194019. [DOI] [PMC free article] [PubMed] [Google Scholar]