Abstract
Sinonasal inverted papilloma (IP) is a benign tumour with an extremely low incidence in children. We report the case of an 11-year-old Caucasian male presenting with recurrent right-sided epistaxis, nasal obstruction and a mass in the right nasal cavity. An initial diagnosis of a nasopharyngeal angiofibroma was considered; however, on detailed histological examination, the mass was found to be an inverted papilloma. This report aims to increase awareness of IP in the paediatric age group, as well as reinforcing the role of endoscopic surgery in the management of this condition.
INTRODUCTION
Inverted papilloma (IP) is the most common benign sinonasal tumour, accounting for between 0.5% and 4% of primary nasal tumours [1–3]. First described by Ward et al. in 1854, IP was originally known as ‘Schneiderian Papilloma’ (SP) of the nose [1]. In 1935, Kramer and Som identified specific histological features of IP, thus distinguishing them from inflammatory nasal polyps [2]. Although generally indolent, IP has a high rate of recurrence (14–78%) [4] particularly if not removed completely including the site of origin which tends to be the lateral wall of the nose. It also has the potential for malignant transformation [3].
The annual incidence of IP is approximately 0.75–1.5 per 100 000 in Europe, with a male:female ratio of 3:1 [5]. Patients with IP typically present in their fifth to –seventh decade with symptoms of unilateral nasal obstruction [5]. Other symptoms may include epistaxis, bloody nasal discharge, headache, facial pain, anosmia, dysosmia and epiphora [5]. IP is exceptionally rare in the paediatric population, and only a handful of cases have been reported.
CASE REPORT
An 11-year-old Caucasian male presented with a 3-month history of right-sided epistaxis and nasal obstruction. He had no other ENT symptoms and was otherwise fit and well. Initial ENT assessment including fibreoptic nasendoscopy revealed a large polypoid mass filling the right nasal cavity and extending into the nasopharynx.
Computerized tomography (CT) and magnetic resonance imaging (MRI) confirmed the presence of a large right-sided sinonasal mass extending posteriorly to the nasopharynx. Irregularity was noted along the posterolateral wall of the maxillary sinus (Figs 1 and 2). In view of the age, sex and clinical presentation, a provisional diagnosis of juvenile nasopharyngeal angiofibroma (JNA) was made.
Figure 1:
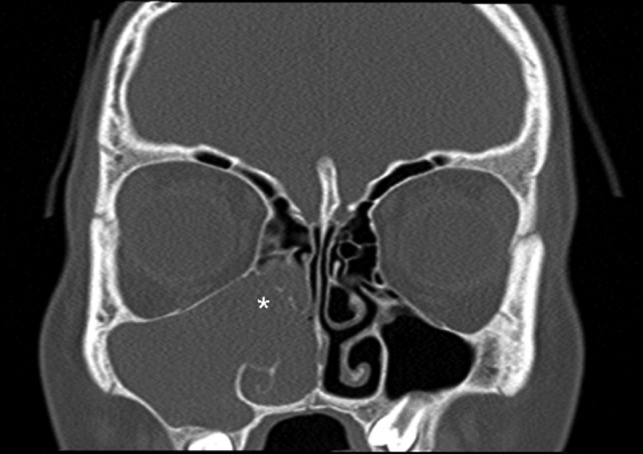
Coronal computed tomography (bone window) image showing a right-sided antrochoanal mass (white asterisk) extending in to the maxillary and ethmoidal sinuses.
Figure 2:
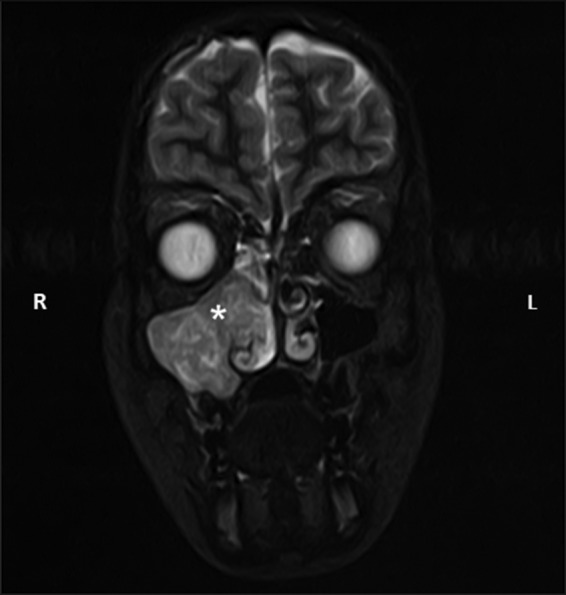
Coronal STIR sequence magnetic resonance image taken as part of the diagnostic investigations, showing the same antrochoanal mass (white asterisk) showing extension into the nasal cavity. L, left; R, right.
Following multidisciplinary discussion, a plan was made for pre-operative embolization prior to definitive surgical excision. However, angiography revealed the lesion to be relatively avascular, and embolization was therefore not performed.
A transnasal endoscopic resection of the right sinonasal tumour was planned. Intraoperative frozen sections showed papillomatous and squamous features consistent with inverted papilloma. The operative findings showed the tumour to be originating from a bony prominence over the postero-lateral wall of the maxillary antrum which was drilled down at the end of the procedure to reduce risk of recurrence. Full macroscopic clearance of the tumour was achieved. The diagnosis of IP was subsequently confirmed on paraffin embedded histological assessment (Fig. 3). No adjuvant therapy was given, and the patient is currently 12 months post-surgery with no endoscopic signs of disease recurrence. Expression of p16 protein which is associated with human papillomavirus status, was negative in this patient.
Figure 3:
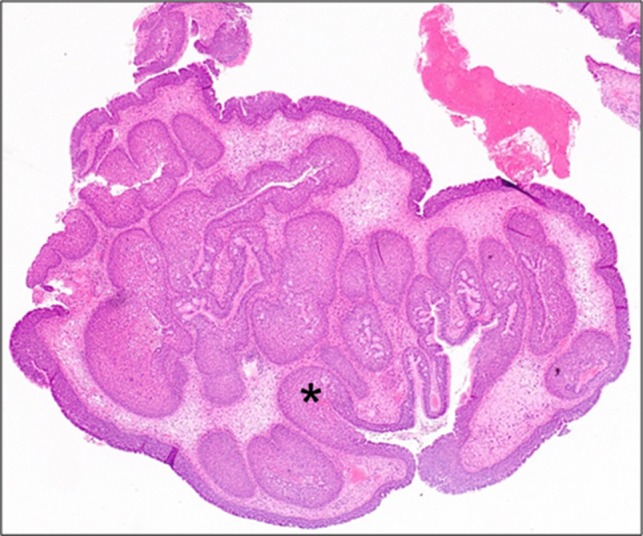
Medium power photomicrograph showing benign proliferative papillomatous type lesion with oedematous stroma and inflammation. There is invagination of the epithelium into the stroma (black asterisk) (H&E; ×20).
The patient was followed up for 5 years and no disease recurrence noted during this time and, therefore, discharged from care at this point.
DISCUSSION
Among sinonasal papillomata, IPs are recognized as benign tumours, albeit with the potential for malignant transformation, as well as the tendency to recur at the primary tumour site even after radical treatment, a feature thought to be related to stromal invasion by the tumour [5]. Whilst IPs are relatively uncommon, their occurrence in the paediatric setting is rare. Previously reported cases of IP in children occurred predominantly in males, at ages ranging from 5 to 15 years old, and arose most commonly from the maxillary sinus, nasal septum and the middle turbinate [6]. Some authors have suggested a possible infective aetiology of IP. It is well established that human papillomavirus can induce transformation in epithelial cells, and a number of studies have aimed to determine whether a viral aetiology may also be responsible for IP [7]. Some studies have suggested that chronic inflammation may induce dysplastic change in allergic nasal polyps, resulting in the development of IP; however, no significant evidence for this theory exists [7].
Investigation of sinonasal masses necessitates imaging in the form of CT and often MRI [7]. Although not pathognomonic, typical radiological features of IP found on CT scanning include intra-mass calcification and bowing, thinning and erosion of the antral wall [7]. A nasal/paranasal mass with a convoluted cribriform pattern on MRI imaging has been shown to be highly suggestive of IP [8].
The high recurrence rate in paediatric patients, and the likely malignant potential of the tumour over time has led most authors to recommend radical surgery and lifelong follow up [6]. Due to the extremely low incidence of paediatric IP, no trials exist that define optimal management. Historically, open surgical approaches have been used to allow en-bloc tumour resection. These include lateral rhinotomy and mid-facial degloving [9]. These techniques are disfiguring and can lead to long-term complications including nasal collapse, formation of synechia and epiphora [9]. In more recent years, surgical techniques have evolved to become less invasive, and the majority of cases can now be managed endoscopically [9]. In addition to the lack of need for an external incision, an endoscopic procedure also has the advantage of reducing surgical morbidity and hospital stay. Although radiotherapy [10] has been utilized, the standard management for IP is complete surgical excision [9]. Disease recurrence has been described as early as 6 months post-surgery and as late as 20 years and therefore long-term monitoring should be undertaken for at least 5 years [9].
Paediatric sinonasal inverted papilloma cases are rare and can pose significant diagnostic and management challenges as illustrated in this case. This report aims to increases awareness of this entity in the paediatric age group as well as reinforce the evolving role of the endoscopic transnasal approach in managing benign and malignant disease involving the sinonasal cavity and anterior skull base.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None
REFERENCES
- 1. Wakley T. A mirror of the practice of medicine and surgery in the hospitals of London. Lancet 1850;55:390–1. [Google Scholar]
- 2. Kramer R, Som ML. True papilloma of the nasal cavity. Arch Otolaryngol 1935;22:22–43. [Google Scholar]
- 3. Vrabec DP. The inverted Schneiderian papilloma: a 25‐year study. Laryngoscope 1994;104:582–605. [DOI] [PubMed] [Google Scholar]
- 4. Phillips PP, Gustafson RO, Facer GW. The clinical behavior of inverting papilloma of the nose and paranasal sinuses: report of 112 cases and review of the literature. Laryngoscope 1990;100:463–9. [DOI] [PubMed] [Google Scholar]
- 5. Syrjänen K, Syrjänen S. Detection of human papillomavirus in sinonasal papillomas: systematic review and meta‐analysis. Laryngoscope 2013;123:181–92. [DOI] [PubMed] [Google Scholar]
- 6. D’Angelo JA, Marlowe A, Marlowe FI, McFarland M. Inverted papilloma of the nose and paranasal sinuses in children. Ear Nose Throat J 1992;71:264–6. [PubMed] [Google Scholar]
- 7. Thapa N. Diagnosis and treatment of sinonasal inverted papilloma. Nepal J ENT Head Neck Surg 2010;1:30–3. [Google Scholar]
- 8. Kim KR. Inverted papilloma. J Rhinol 2001;8:5–10. [Google Scholar]
- 9. Lund V. Optimum management of inverted papilloma. J Laryngol Otol 2000;114:194–7. [DOI] [PubMed] [Google Scholar]
- 10. Gomez JA, Mendenhall WM, Tannehill SP, Stringer SP, Cassisi NJ. Radiation therapy in inverted papillomas of the nasal cavity and paranasal sinuses. Am J Otolaryngol 2000;21:174–8. [DOI] [PubMed] [Google Scholar]


