Abstract
Background.
A large and extensive body of research has examined comorbid anxiety and depression in adults. Children and adolescents also frequently present with comorbid anxiety and depression; however, research and treatment require unique environmental and neurodevelopmental considerations in children. As a result, our understanding of comorbid anxiety and depression in children and adolescents is limited.
Objective.
The goal of this systematic review was to examine current literature focused on comorbid anxiety and depression in children and adolescents. The review included theoretical conceptualizations as well as diagnostic, neurobiologic, prevention, and treatment considerations. In addition, a proposed algorithm for the treatment of comorbid anxiety and depression in children/adolescents is provided.
Methods.
This systematic literature review included three discrete searches in Ovid SP Medline, PsychInfo, and Pubmed.
Results.
The review included and synthesized 115 articles published between 1987 and 2015. The available evidence suggests that anxiety and depression are common in clinical populations of children and adolescents, and that comorbidity is likely underestimated in children and adolescents. Children and adolescents with comorbid anxiety and depression have unique presentations, greater symptom severity, and treatment resistance compared with those who have either disease in isolation. A dimensional approach may be necessary for the future development of diagnostic strategies and treatments for this population. Nascent neuroimaging work suggests that anxiety and depression each represents a distinct neurobiological phenotype.
Conclusion.
The literature that is currently available suggests that comorbid anxiety and depression is a common presentation in children and adolescents. This diagnostic picture underscores the importance of comprehensive dimensional assessments and multimodal evidence-based approaches given high disease severity. Future research on the neurobiology and treatment of these common clinical conditions is warranted.
Keywords: anxiety, depression, child, adolescent, comorbidity
Depressive and anxiety symptoms frequently overlap in adults,1,2 and an accumulating body of literature has substantiated their comorbidity across the adult lifespan. However, there is a dearth of evidence regarding the comorbidity and phenomenologic overlap of anxiety and depression in pediatric populations. Children and adolescents often present with distinct neuropsychiatric symptomatology that is compounded by unique environmental stressors and influenced by ongoing neurodevelopmental processes. These complex and dynamic factors warrant specific assessment and treatment considerations,1 particularly since comorbidity of anxiety and depression in pediatric patients has received little attention.1–6
In this article, we systematically review and examine accumulating evidence related to comorbid anxiety and depressive symptoms in child and adolescent populations in order to 1) enhance theoretical conceptualizations of these disorders; 2) improve assessment and diagnosis, 3) enhance prevention and treatment strategies, and 4) guide future research. Moreover, with the recent release of the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5),7 there are new changes to the psychiatric diagnostic conceptualization of the comorbidity of anxiety and depressive symptoms, especially with regard to subsyndromal symptomatology, which will be addressed here.
This systematic literature review was based on three independent searches using Ovid SP Medline (1948 to the present), PsychInfo (1806 to the present), and PubMed (1948 to the present), using the following terms: anxious depression, child (including psychiatry and psychology), adolescent (including psychiatry and psychology), depressive disorder, anxiety disorder, depression comorbid anxiety, and mixed anxiety depression. The search was limited to articles that were written in English and contained the following terms: mixed anxiety depression, anxious depression, anxious mood, major depressive disorder (MDD) comorbid anxiety, child, and adolescent. These searches resulted in a total of 115 articles included in this systematic review. These articles were published between 1987 and 2015 in the United States and the United Kingdom.
PREVALENCE OF COMORBIDITY
Anxiety and depression represent distinct disorders with specific clinical features, disease course, pathophysiology, and unique treatment strategies.8 Anxiety and depression independently contribute to a significant proportion of the prevalence of mental health disorders. The World Health Organization (WHO) has identified depression as the leading cause of disability (as measured by years lived with a disability) and the second largest contributor to the global burden of disease (as measured by disability adjusted life years).9 Despite advances in mental health care, the WHO has noted that depression is currently the second largest contributor to global burden of disease among those 15–44 years of age for both sexes combined, and by 2020 will be the first contributor to global burden for all persons.9 Anxiety disorders are presently the most common form of psychiatric illness in children and adolescents,10–13 with annual prevalence rates that range from 5.7 to 17.7%.14 Further, a significant proportion of anxious children will experience chronic courses of anxiety lasting through adulthood14 and these individuals are at heightened risk for developing depressive disorders15,16 (for review see Wehry et al 201517). Consequently, the long-term effects of chronic anxiety symptoms include increased risk for additional anxiety disorders, MDD, illicit drug use, and poor academic performance.18 In parallel, co-occurring depression and anxiety are commonly observed in epidemiologic samples, including in the National Comorbidity Survey (NCS).19 In the NCS, 58% of patients (15 to 54 years of age) with MDD had a comorbid anxiety disorder.19 The most frequent combinations involved MDD with comorbid generalized anxiety disorder (GAD) at 17.2% and with comorbid panic disorder at 9.9%.19,20 Conversely, nearly a quarter of patients with an anxiety disorder may meet diagnostic criteria for comorbid depression.19,20
Comorbidity rates between depression and anxiety may be even higher in the child and adolescent populations. However, the diagnostic process in these populations is complicated by increased symptom severity and heterogeneous symptom presentations.8 Biederman and colleagues observed that more than 95% of children with MDD had a comorbid diagnosis, with the highest rates for anxiety disorders.4 Data suggest that single diagnoses in children and adolescents are rare, and that more individuals than not will have at minimum 2 psychiatric illnesses.2,4–9,11–14,18–24 Comorbidity may increase symptom severity, predict worsening of global functional status (eg, poorer academic performance, increased familial conflict), increase substance abuse risk, and increase risk for suicide attempts.21 Closer examination of the clinical presentation of comorbid anxiety and depression is necessary as comorbidity appears to be the rule rather than the exception in child and adolescent populations.
A DIMENSIONAL CONCEPTUALIZATION
As anxiety disorders co-occur with MDD at rates beyond what is explainable by chance alone, research suggests this may reflect a causal relationship.1 Depression may precede anxiety, anxiety may precipitate depression, or both disorders may be the manifestation of a common etiopathology. In a study published in 1992 involving a population of adults (17 years of age and older), Coryell et al1 observed that anxiety symptoms confined to an episode of primary depression were symptoms of that depressive disorder rather than being part of a separate disease. Furthermore, patients with primary depression who reported obsessions or compulsions, panic attacks, or phobias that were restricted to their current depressive episode were unlikely to develop these anxiety syndromes as autonomous disorders by the 5-year follow-up. Rather, they had an increased tendency to develop recurrent depressive episodes.1 In addition, in that study, depressed patients with anxiety symptoms had poorer outcomes compared with those without anxiety symptoms. This would be expected if the symptoms were related to a comorbid anxiety disorder1 as opposed to anxiety symptoms that reflect phenemologic overlap between depression and anxiety. However, follow-up of these patients showed that they had no primary anxiety disorder,1 which suggested that these comorbid anxiety syndromes were epiphenomenal features that predicted a more severe and persistent form of depression.1
Additional research has suggested that anxiety and depressive disorders should be grouped together as “distress” and measured along a continuum.25,26 This dimensional conceptualization of anxiety and depression appears to more accurately depict the presentation of these disorders in child and adolescent populations. Using the Child Behavior Checklist (CBCL)27 in pediatric patients, 4 to 18 years of age, Wadsworth et al21 observed features consistent with the mixed anxiety/depressive syndrome and failed to find evidence for a distinct anxiety or depressive disorder. The results from Wadsworth et al reveal the presence of a continuum containing both affective and anxiety problems in children and adolescents.21 These researchers argued that a dimensional conceptualization complements a categorical approach, as some children may fall at one end of the continuum displaying only symptoms of depression, while other children may fall at the opposite end of the continuum exhibiting only symptoms of anxiety.21 The Wadsworth et al. study demonstrated that most children, however, appear to fall in the middle of the continuum, with problems of both anxiety and depression.21 Their findings were consistent with earlier findings from Eaton et al,22 who were unable to identify pure cases of depression devoid of anxiety symptoms. Therefore, whereas some children may exhibit symptoms that meet diagnostic threshold criteria for either a depressive or anxiety disorder, the symptoms in these areas that most children and adolescents exhibit are better explained as being on an affective/anxiety continuum.17,18
ANXIOUS-DEPRESSIVE SYMPTOMATOLOGY
Comorbid psychiatric diseases in general are associated with greater distress, increased disability, poorer response to treatment, and poorer prognosis.26 Specific to comorbid anxiety and depression, complications include additional symptoms of negative self-evaluation, discouragement, and more severe depressed mood.28 The anxious depressive symptomatology is comprised of additional psychiatric symptoms that include diurnal variation (with mood worse in the morning), somatic concerns (gastrointestinal symptoms, hypochondriasis), increased anergia, insomnia, agitation, poor concentration, depersonalization, subjective anger, obsessive thoughts and compulsive behaviors, distrustfulness, hypophagia, and lack of mood reactivity to changes in circumstances.20,28
Children and adolescent populations have similarly demonstrated greater disease severity when they present with coexisting anxiety and depressive symptoms.18 Youth may also be more likely to present with increased somatic complaints compared with adult samples.29–32 For example, Woodward and Ferguson33 examined adolescent outpatients and determined that both anxiety and depression accentuated the reporting of somatic complaints. These somatic complaints often led to increased school avoidance and poorer academic performance.33 Moreover, Woodward and Ferguson found that the presence of autonomic symptoms (eg, shakiness/trembling, flushes/chills, sweating, headaches) was most significantly associated with greater absence from school.33 Somatic complaints and school refusal in this population are important to acknowledge, because poor school attendance (especially when the result of anxiety and depressive symptoms) may lead to longitudinal academic difficulties and loss of peer relationships.30 Findings from a study by Henker et al13 that used electronic diaries in adolescents suggested that teenagers in the high anxiety group not only reported higher levels of anxiety and stress than those in the low anxiety group, but also experienced more depressive symptoms than those in the low anxiety group. Furthermore, anxious teenagers have been reported to disengage from socially constructive behaviors (eg, they have fewer conversations with friends, less participation in recreational activities) and to be more likely to engage in socially destructive behaviors (eg, increased smoking, increased isolation).13
The influence of the family milieu on child and adolescent symptomatology is also an important factor with regard to anxiety and depressive symptoms. Adolescents with high levels of anxiety symptoms report more family “chaos,” less autonomy and openness, less intimacy/warmth in their families, and they are more likely to have controlling and overprotective parents.32,34 In children and adolescents with MDD, depressive symptoms were linked with family disengagement.32,34 One heritability study suggested that, through a reactive correlation between genotype and environment, anxious and depressed children may actually elicit a certain type of parenting style that is often more punitive and overbearing in nature, which in turn produces an environment that maintains or exacerbates anxious and depressive symptoms.35 Targeting these family characteristics should be part of therapeutic treatment, which may improve family functioning and thereby decrease the severity and course of comorbid anxiety and depressive disorders.
NEUROBIOLOGICAL CORRELATES
To date, neuroimaging research has primarily focused on studies of pediatric depression or anxiety as opposed to comorbid conditions. However, common brain structures or neurocircuitry are often implicated in both disorders. In some but not all studies, adolescents with depression have demonstrated increased amygdala activity in the context of fearful stimuli when compared with healthy comparison groups.36,37 Adolescents with MDD have also demonstrated hypoperfusion in the dorsolateral prefrontal cortex (DLPFC), anterior cingulate cortex (ACC), and amygdala when compared with healthy participants.38 Other research has demonstrated increased striatal-dorsomedial prefrontal and striatal-ACC functional connectivity in adolescent subjects with MDD.39 It should be noted that symptom severity was correlated with striatal and dorsomedial prefrontal functional connectivity in that study.39 Neuroanatomical studies have demonstrated that depressed adolescents have decreased gray matter volumes in the caudate, DLPFC, ACC, and temporal lobe when compared with healthy subjects40,41
Parallel work in youth with anxiety implicates the prefrontal-amygdala network. This includes work demonstrating increased functional activity in the anterior cingulate cortex,42,43 amygdala,37,44 and ventrolateral prefrontal cortex.37,45–47 Although results are not consistent, studies have also have observed neuroanatomical abnormalities in prefrontal-amygdala networks.48–52 One group found increased right and overall amygdala volumes in pediatric patients with GAD.48 Other studies have observed decreased left50 and right51 amygdala gray matter volumes in pediatric patients with a mixture of anxiety disorders. Other groups have reported decreased anterior hippocampal gray matter volumes in anxious youth.51 De Bellis and colleagues demonstrated that youth with GAD had increased gray and white matter volumes in the superior temporal gyrus.49 A voxel-based morphometry study found increased gray matter volumes in the right precentral and right precuneus of adolescents with GAD compared with healthy controls. The patients with GAD also had lower gray matter volumes in the left orbitofrontal cortex and posterior cingulated.52
To date, little neuroimaging work has examined pediatric patients with anxiety and comorbid depression.53 Studies in adults included a 2014 functional magnetic resonance imaging (fMRI) comparison of adults with MDD without anxiety, adults with MDD and panic disorder, and healthy subjects.54 Adults with MDD displayed increased dorsal anterior cingulate cortex activation with reward anticipation, whereas the other groups did not.54 A neurostructural study examined adults who had MDD with comorbid anxiety, adults with MDD only, and adults with anxiety only.55 All 3 groups had decreased gray matter in the rostral anterior cingulate when compared with healthy controls but no differences were found among the patient groups.55 Another neurostructural study of adults compared patients with MDD with anxiety symptoms, patients with MDD only, and healthy subjects.56 Both patient groups had decreased gray matter in the superior parietal lobe. The patients with anxiety and comorbid depression had increased gray matter in the right temporal cortex.56 Recently, Wehry and colleagues completed a voxel-based morphometry study comparing gray matter volumes among depressed adolescents without anxiety, depressed adolescents with comorbid anxiety, and healthy controls.57 Adolescents with anxious depression had decreased gray matter in the right dorsolateral prefrontal cortex compared with depressed adolescents. However, compared with healthy adolescents, participants with anxiety and comorbid depression had increased gray matter in the pre- and post-central gyri.57 Although evidence is nascent, youth with anxiety and comorbid depression may have distinct patterns of structural and functional abnormalities compared with youth with anxiety or depression alone. Further work could delineate more biologically oriented classification systems for clinical practice to assist with treatment selection.57
EFFECTS OF ANXIOUS DEPRESSIVE COMORBIDITY ON THE COURSE OF ILLNESS
While anecdotally some clinicians believe that depressed patients who experience comorbid anxiety and depressive symptoms present with a less severe course of depressive illness,28 the preponderance of research suggests otherwise—that is, that patients with comorbid anxiety and depressive symptoms have more severe depression, a more chronic course of illness, and decreased response to treatment.28,58,59 Furthermore, comorbid anxiety and depression is associated with increased rates of physical morbidity, cardiovascular disease, mortality, and likelihood of suicide relative to the rates of these conditions in isolation.60 Anxiety symptoms also significantly predict family illness and course, as seen in Clayton et al.’s sample28 of adults with primary depressive disorders who had high anxiety. The familial prevalence of primary depressive disorder was increased, and, when followed longitudinally over the course of 5 years, these individuals experienced poorer outcomes.
The increased risk for suicidal behaviors in this adult population is of critical concern. Cumulative lifetime prevalence estimates for suicide attempts in studies that assessed youth between the ages of 9 to 19 ranged from 3% to 7%, with the largest risk factors being mood, anxiety, disruptive, and substance use disorders.61–69 Indeed comorbidity with an anxiety disorder is more common in suicidal youth, suggesting that comorbidity results in greater severity of the psychiatric illness and more functional burden.61,62 The Great Smoky Mountains Study, published in 2006, prospectively evaluated 1420 youth (9–16 years of age) with anxiety disorders (specifically GAD) comorbid with depression and demonstrated an increased suicidal risk.61 This raised the possibility that depression plus GAD represents a highly discriminating pattern of symptoms or other risk factors, as this was the only profile that independently predicted suicidality regardless of the severity of symptoms or impairment.61 Similarly, in adults surveyed in the Netherlands Mental Health Survey and Incidences Study (NEMESIS),62 the presence of an anxiety disorder was unequivocally associated with increased suicidal ideation and the co-occurrence of an anxiety disorder with MDD increased the likelihood of a suicide attempt. Psychological autopsy studies have reported that most completed suicides occur on the first suicide attempt, thus children and adolescents who present with both anxiety and depressive symptoms may require immediate suicidal assessment and therapeutic intervention.
ANXIETY AND DEPRESSIVE DISORDERS IN DSM-5
Of growing concern is the prevalence of subthreshold depressive and anxiety symptoms in the child and adolescent population. Those who do not meet full diagnostic criteria for either disorder may be overlooked and consequently not receive adequate treatment, more than quadrupling the risk for the development of an anxious or depressive psychiatric disorder.70,71 The 12-month prevalence rates for subthreshold depressive disorders in children and adolescents range between 3% and 7%, and the lifetime prevalence rate through late adolescence has been reported to be as high as 26%.70–72 A study conducted by Klein et al. reported that almost half of all adolescents with subthreshold depressive disorder in a community sample developed full syndromal depressive disorder by the time they were 30 years of age.70 The study suggested that 7 unique variables, including anxiety syndrome, female sex, greater depression severity, increased medical conditions, history of suicidal ideation, psychomotor disturbance, and family history of depressive disorders significantly predicted the escalation from subsyndromal to full-syndrome depressive disorder in adolescents.70 This finding substantiates the importance of documenting and treating subthreshold anxiety and depressive symptoms.
Earlier editions of the DSM have relied on categorical approaches to diagnosis (either patients meet criteria for a disorder or they do not). This diagnostic approach has limitations in the child and adolescent population, particularly because of the subsyndromal comorbid symptomatology described above. The DSM-5, however, has incorporated dimensional approaches to assessment and diagnosis. This dimensional assessment of psychopathology provides for a more accurate assessment of subclinical presentations of disorders, disorder severity, and how symptoms change dynamically over time (with repeated assessment).73,74 Dimensional ratings can also be made to capture symptoms that cut across multiple diagnoses, better representing the full presentation of symptoms within an individual and capturing diagnostic comorbidity.73,74
In addition to adopting a more dimensional approach, the DSM-5 Task Force carefully considered the order of diagnostic categories in the manual. Anxiety disorders follow depressive disorders, obsessive-compulsive and related disorders follow anxiety disorders, which are followed by trauma- and stressor-related disorders and then dissociative disorders.75 This sequence is intended to emphasize the close relationships among some of the conditions in these adjacent sections.75 Furthermore, the order of anxiety diagnoses in the anxiety section is intended to reflect the developmental progression of certain anxiety disorders. The typical age of onset is used to sequence the disorders, with separation anxiety disorder first in the chapter, followed by selective mutism, specific phobia, social anxiety disorder, panic disorder, agoraphobia, and ending with generalized anxiety disorder.
Recognizing the prevalence and clinical implications of comorbid presentations (specifically subsyndromal anxiety symptoms in depression), the DSM-5 has included criteria for a specifier “with anxious distress” for major depressive disorder and bipolar disorder.76,77 The anxious distress specifier is defined as the presence of at least 2 of the following anxiety symptoms during the majority of days of a depressive episode in major depressive disorder, or during an episode of mania, hypomania, or depression in bipolar disorder: feeling keyed up or tense, feeling unusually restless, difficulty concentrating because of worry, fear that something awful may happen, or feeling that one might lose control of oneself. In addition, a severity rating is to be applied to this specifier. Clinicians can rate the anxious distress as mild (2 of the above symptoms present), moderate (3 symptoms), moderate-severe (4 or 5 symptoms), or severe (4 or 5 symptoms with motor agitation). Adding a dimensional scale to these categorical diagnoses reflects the increasing awareness that the presence of anxiety symptoms can have a significant impact on the treatment course and outcomes of existing diagnoses.77
MOOD AND ANXIETY SYMPTOMS IN DIAGNOSTIC ASSESSMENTS BY CHILD AND ADOLESCENT SELF-REPORT
A concern in children and adolescents, particularly with younger children, is that their ability to express and verbally describe psychiatric symptoms—including anxiety and depressive symptoms—may be limited by language development and cognitive factors. Thus, psychiatric assessments commonly rely upon parents/caregivers, and other reliable informants such as teachers to provide information, as children are thought be unreliable reporters of their own mental state.78 However, adult reporters may fail to accurately recognize mood symptoms in younger children; therefore, corroborating evidence concerning symptoms from the child’s own perspective would be of value in a clinical diagnostic assessment.78 Some studies have suggested that even young children may be able to report symptoms. Jensen and colleagues observed a correlation between child and parental reports of various psychiatric diagnoses in children and adolescents aged 9 to 17 years,79 and they specifically noted that reports about internalizing symptoms (eg, depression, anxiety) are highly correlated between child and parent informants.79 This finding suggests that children may be reliable reporters of their symptoms, particularly internalizing symptoms, and that they can add valuable information to the psychiatric diagnostic process.78,79. In addition, Luby et al. evaluated the validity of symptom reporting by preschool age children (4 to 5.6 years of age)78 and found a strong relationship between younger children’s self-reports of basic depressive and anxious symptoms and their parents’ reports of these symptoms,78 although some difficulty was observed with regard to the reporting of abstract psychiatric symptoms (eg, loneliness, self-esteem). Taken together, these findings suggest that parents are able to accurately assess and report their child’s symptoms and, conversely, that children, even at young ages, are able to provide accurate information to help inform the diagnostic assessment.78,79
PSYCHOPHARMACOLOGIC TREATMENT OF ANXIOUS-DEPRESSION IN YOUTH
In contrast to the many psychopharmacologic treatment studies that have evaluated adult patients with “anxious depression,”80–83 pediatric studies have largely focused on patients with depression or anxiety (eg, social phobia, separation anxiety disorder, GAD, or the combination) and have generally excluded anxious patients with comorbid MDD.84–88 Abundant evidence suggests that selective serotonin reuptake inhibitors (SSRIs) are effective in treating both pediatric MDD and anxiety disorders,89–91 and, on the basis of randomized controlled trials of SSRIs and selective serotonin norepinephrine reuptake inhibitors (SNRIs) (Table 1), recommendations can be extrapolated regarding the treatment of anxious depression in pediatric patients.
Table 1:
Randomized Controlled Trials of Selective Serotonin Reuptake Inhibitors (SRIs) and Selective Serotonin Norepinephrine Reuptake Inhibitors (SNRIs) in Pediatric Anxiety Disorders
| PEDIATRIC ANXIETY DISORDERS | PEDIATRIC MAJOR DEPRESSIVE DISORDER | |||||||
|---|---|---|---|---|---|---|---|---|
| Medication | Anxiety Reference |
Anxiety Disorder |
Anxiety Dose Range (mg/day) |
Anxiety Effect Size |
MDD Reference |
MDD Dose Range (mg/day) |
MDD Effect Size |
|
|
SSRIs |
Sertraline |
Walkup et al 200888 | GAD SoP SAD |
25–200 | 0.4 | Wagner et al 200396 | 50–200 | 0.28 |
| Rynn et al 200185 | GAD |
25 (week 1) 50 (week 2–9) |
0.7 |
|||||
| Fluoxetine | Beidel et al 200792 | SoP | 10–40 | Simeon et al 199097 | 20 | 0.21 | ||
| Birmaher et al 200393 | GAD SoP SAD |
10 (week 1) 20 (week 2–12) |
0.2 | Emslie et al 199798 | 20 | 0.60 | ||
| Emslie et al 200299 | 20 | 0.50 | ||||||
| March et al 2004100 | 10–40 | 0.40 | ||||||
| Paroxetine | Wagner et al 200494 | SoP | 10–50 | Keller et al 2001101 | 20–40 | 0.22 | ||
| Berard et al 2006102 | 20–40 | 0.07 | ||||||
| Emslie et al 2006103 | 10–50 | −0.06 | ||||||
| Fluvoxamine | RUPP 200195 | GAD SoP SAD |
300 (maximum) | 0.5 | N/A not studied | |||
| Citalopram | Wagner et al 2004104 | 20–40 | 0.32 | |||||
| von Knorring et al 2006105 | 10–40 | −0.01 | ||||||
| Escitalopram | Ongoing trials | Wagner et al 2006106 | 10–20 | 0.13 | ||||
| Emslie et al 2009107 | 10–20 | 0.27 | ||||||
|
SSNRIs |
Venlafaxine ER | March et al 200784
Rynn et al 200786 |
SoP GAD |
37.5–225 37.5–225 |
0.9 0.4/0.5 |
Emslie et al 2007108 | 37.5–200 | 0.14 |
| Duloxetine | Strawn et al 201587 | GAD | 30–120 | 0.48 | Emslie et al 2014109 |
30–120 | N/A, neg. | |
| Atkinson et al 2014110 |
30–120 | N/A, neg. | ||||||
Like psychopharmacologic treatment studies in pediatric patients with MDD, most clinical trials in pediatric patients with anxiety disorders have focused on SSRIs and SNRIs. In general, studies of pediatric anxiety disorders have focused on anxiety as a homogeneous entity (eg, “childhood anxiety” or the combination of separation anxiety disorder, GAD, and social phobia/social anxiety disorder).88,91 More recently, however, several studies have focused on specific anxiety disorders (eg, GAD, separation anxiety disorder) in these populations.86,87,92 In randomized, controlled trials of patients with multiple anxiety disorders, fluvoxamine has been associated with significant clinical improvement and is generally well-tolerated; however, these trials excluded patients with MDD.95 Two open-label trials of fluoxetine in pediatric patients with mixed anxiety disorders have also suggested benefit in alleviating anxiety symptoms.92 In addition, in a randomized placebo-controlled trial of pediatric patients with GAD, separation anxiety disorder, and social anxiety disorder, improvement was observed on all efficacy measures in patients treated with fluoxetine.93
Fixed-dose treatment studies of sertraline in children aged 7–17 years of age found improvement as demonstrated by decreased severity of anxiety symptoms.85 In addition, the Child/Adolescent Anxiety Multimodal Study (CAMS) that involved 488 patients found that the effect of sertraline monotherapy was superior to that of placebo and similar to that of cognitive behavioral therapy (CBT), while combination treatment was superior to both monotherapy conditions.88 In both of these pediatric trials, sertraline was well-tolerated. Fluoxetine and venlafaxine have also been evaluated in pediatric patients with GAD and both were found to be superior to placebo.86,93 However, some issues related to the tolerability of venlafaxine in the pediatric population were noted, as venlafaxine was associated with increased blood pressure, asthenia, pain, anorexia, somnolence, and weight loss and it may also have been associated with treatment-emergent suicidal ideation.86 Finally, one randomized, placebo-controlled trial that examined the efficacy and tolerability of flexibly-dosed buspirone (15–60 mg daily) in children and adolescents with GAD (ages 6 to 17 years) found no difference between buspirone and placebo.111
Paroxetine, citalopram, fluoxetine, and venlafaxine have been evaluated in pediatric patients with social phobia. In a randomized trial, patients treated with paroxetine had response rates of 78% versus 38% for placebo over the course of 16 weeks.94 However, adverse events, including withdrawal symptoms, were twice as likely with paroxetine treatment. Venlafaxine extended release (ER) was associated with improvement in pediatric social anxiety disorder.84 One placebo-controlled trial of pediatric patients with social phobia (7–17 years of age) compared Social Effectiveness Therapy for Children (SET-C) and fluoxetine.92 SET-C included psychoeducational modules, social skills practice in group sessions, social exposures, and individual psychotherapy. Both fluoxetine and SET-C were superior to placebo. Fluoxetine appeared have maximum effect at 8 weeks. Fluoxetine was well tolerated with no reported severe adverse events.92 Finally, open-label studies of citalopram (10–40 mg/d)112 and escitalopram (10–20 mg/d)113 in pediatric patients with social anxiety disorder demonstrated benefit and tolerability.
To date, we are aware of no treatment studies or recommendations that address the management of coexisting anxiety and depression (whether comorbid or subsyndromal) in the pediatric population. However, extrapolation from the available evidence for the psychotherapeutic and psychopharmacologic treatment of both MDD and anxiety disorders in youth suggests that multimodal approaches are superior to monotherapy88,92,96,114 Thus, both the Treatment of Adolescent Depression Study (TADS)115 and the Treatment of SSRI-Resistant Depression in Adolescents (TORDIA)114 study suggest that the combination of an SSRI (or SNRI in the case of TORDIA) plus CBT is superior to monotherapy. Similarly, in children and adolescents with anxiety disorders, treatment with the combination of CBT and sertraline was found to be superior to monotherapy.88 Thus, a first-line approach to the pediatric patient with coexisting anxiety and depression should include evidenced-based psychotherapy in conjunction with an SSRI (Figure 1), given that several SSRIs (eg, sertraline, fluoxetine) have strong evidence of efficacy in both disorders. Alternatively, monotherapy remains an available option for a first-line intervention in pediatric patients with anxiety and depression as SSRIs and several evidence-based psychotherapies are also supported by available evidence as monotherapy for these conditions. With regard to the specific modality of psychotherapy, there is strong evidence for several types of psychotherapy in the available literature on pediatric anxiety and depression, including CBT,100,114 interpersonal psychotherapy for adolescents (IPT-A),116 and psychodynamic psychotherapy117,118
Figure 1: Proposed algorithm for the treatment of comorbid anxiety and depression in children and adolescents.
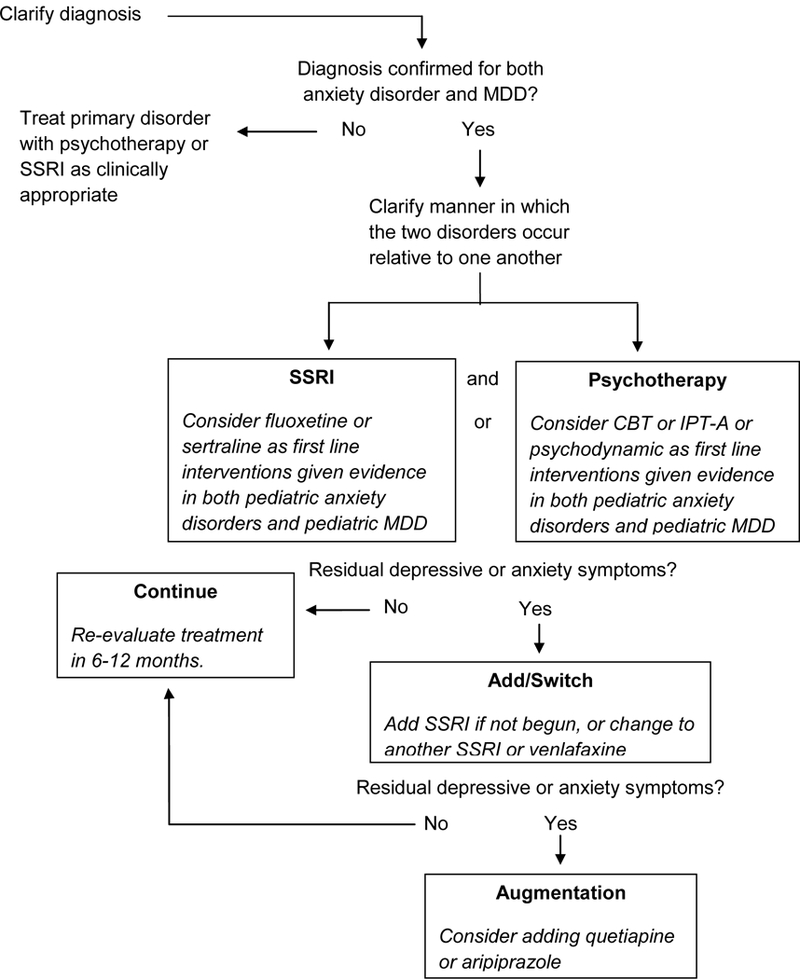
Note: MDD, major depressive disorder; SSRI, selective serotonin reuptake inhibitor; SNRI, serotonin norepinephrine reuptake inhibitor; CBT, cognitive-behavioral therapy; IPT-A, interpersonal psychotherapy for adolescents
Despite the potential efficacy of these “first-line” interventions in youth, many young patients with depressive or anxiety disorders continue to experience residual symptoms.119 It has also been suggested that pediatric patients with comorbid anxiety and depression may have a lower likelihood of achieving remission.119 Currently available data suggest that patients with depressive symptoms (in major depressive disorder) and residual anxiety symptoms (in generalized, social, or separation anxiety disorders) may show benefits after switching from their initial SSRI regimen to an alternate SSRI regimen.114,120 However, beyond switching from one SSRI to another SSRI, data regarding “next step” interventions are limited. Thus, at this level of the treatment algorithm for comorbid anxiety and depression in pediatric patients (Figure 1) our recommendations represent the “expert opinion” level of evidence and are primarily based on data extrapolated from adult studies. Thus, on the basis of double-blind, placebo-controlled trials evaluating the use of quetiapine as an adjunct to ongoing treatment with an antidepressant medication in SSRI-resistant MDD,121,122 and an open-label trial of quetiapine as an adjunct to antidepressant medication in the treatment of SSRI-resistant depression in children and adolescents123 as well as positive double-blind, randomized controlled trials of quetiapine monotherapy in adults with GAD,124,125, it is reasonable to consider quetiapine as an adjunctive agent in the treatment of SSRI-resistant and psychotherapy-resistant depressive or anxiety symptoms in children and adolescents. However, the risks and benefits of second-generation antipsychotic medications should be carefully considered, in accordance with guidelines from the American Academy of Child and Adolescent Psychiatry.126 In addition, based on positive double-blind, placebo-controlled studies evaluating the use of aripiprazole as an adjunct to ongoing treatment with an antidepressant medication in adults with treatment-resistant MDD127,128 and a positive, open-label trial of aripiprazole as an adjunct to SSRI treatment for SSRI-resistant generalized anxiety disorder in adults,129 as well as a retrospective evaluation of aripiprazole as an adjunct to SSRI treatment in depressed and anxious adults,130 it is possible that adjunctive aripiprazole may have a role in the management of functionally impairing depressive or anxiety symptoms that persist in youth with anxious depression, following initial trials of SSRIs and psychotherapy. It is interesting that post-hoc analyses of trials with both aripiprazole and quetiapine have suggested that these agents may have efficacy for anxious depression.83,131 However, use of second-generation antipsychotic medications has been associated with significant adverse effects, including weight gain, diabetes or insulin insensitivity, dyslipidemia, and potential tardive dyskinesia. Thus, the risk and benefits of any medication changes should be weighed to ensure optimal therapeutic outcomes.
CONCLUSION AND IMPLICATIONS FOR FUTURE RESEARCH
Child and adolescent populations most often present with anxiety and mood symptoms that co-occur, which leads to a more difficult diagnostic assessment, increased symptom severity, and complicated treatment methods.1–6,21 In addition, a number of specific considerations arise in treating child and adolescent populations that are not always primary factors in adults, including unique presentations of symptoms (eg, increased somatization, irritability, and agitation), functional impairment in school and social activities during developmentally important years, significantly increased risk for suicidality, and influences from the family system. Although research concerning overlapping anxiety and depressive symptoms in this population is available, more work is warranted to gain a better understanding of the unique factors involved in child and adolescent presentations.
Our review of the available literature suggests that education regarding the anxiety/mood symptoms that present in youth be disseminated to parents, teachers, counselors, school administrators, coaches, physicians, and other caretakers and providers. Furthermore, school refusal and somatic complaints should be considered important indicators that a child/adolescent may be experiencing significant distress due to anxiety and/or depression.31 The implementation of school-based screening and counseling programs geared to the needs of anxious/depressed children and adolescents may enhance early detection, prevention, and appropriate referrals for those with more severe/chronic illness.33 The lack of available data concerning the validity/reliability of assessments of comorbid anxiety and depression in youth is of concern, especially considering that earlier research suggests that youth are prone to significant impairment from co-occurring subsyndromal anxiety/depressive symptoms. Future research should also further explore the utility of available pharmacological and psychosocial treatments in the treatment of comorbid anxiety and depressive disorders in this population.
Acknowledgements:
This work was supported in part by the National Institute of Mental Health [K23 MH087739 (Shawn M. McClintock), K23 MH106037 (Jeffrey R. Strawn) and K23 MH100266 (Paul E. Croarkin).
Contributor Information
Tabatha H. Melton, Therapy Dallas, Clinical Practice, Dallas, TX.
Paul E. Croarkin, Department of Psychiatry and Psychology, Mayo Clinic, Rochester, MN.
Jeffrey R. Strawn, Department of Psychiatry and Behavioral Neuroscience, University of Cincinnati, Cincinnati, OH.
Shawn M. McClintock, Department of Psychiatry and Behavioral Sciences, Duke University School of Medicine, Durham, NC, and Department of Psychiatry, University of Texas Southwestern Medical Center, Dallas, TX..
REFERENCES
- 1.Coryell W, Endicott J, Winokur G. Anxiety syndromes as epiphenomena of primary major depression: outcome and familial psychopathology. Am J Psychiatry. 1992;149:100–107. [DOI] [PubMed] [Google Scholar]
- 2.Rhode P, Lewinsohn PM, Seeley JR. Comorbidity of unipolar depression: II. J Abnorm Psychol. 1991;100:214–222. [PubMed] [Google Scholar]
- 3.Angold A, Costello EJ. Depressive comorbidity in children and adolescents: empirical, theoretical, and methodological issues. Am J Psychiatry. 1993;150:1779–1791. [DOI] [PubMed] [Google Scholar]
- 4.Biederman J, Faraone S, Mick E. Psychiatric comorbidity among referred juveniles with major depression: fact or artifact? Am J Psychiatry. 1995;34:579–590. [DOI] [PubMed] [Google Scholar]
- 5.Keller MB, Lavori PW, Wunder J. Chronic course of anxiety disorders in chilsdren and adolescents. J Am Acad Child Adolesc Pyschiatry. 1992;31:595–599. [DOI] [PubMed] [Google Scholar]
- 6.Lewinsohn PM, Klein DN, Seeley JR. Bipolar disorder in a community sample of older adolescents; prevalence, phenomenology, comorbidity, and course. J Am Acad Child Adolesc Psychiatry. 1995;34:454–463. [PubMed] [Google Scholar]
- 7.American Psychiatric Association (APA). Diagnostic and Statistical Manual of Mental Disorders. Fifth Edition Arlington, VA: APA; 2013. [Google Scholar]
- 8.Balestrieri M, Isola M, Quartaroli M. Assessing mixed anxiety-depressive disorder: a national primary care survey. Psychiatry Res. 2010;176:197–201. [DOI] [PubMed] [Google Scholar]
- 9.World Health Organization (WHO). Depression Fact Sheet No 369. Geneva, Switzerland: WHO; 2015. Available at http://www.who.int/mediacentre/factsheets/fs369/en, accessed January 5, 2016. [Google Scholar]
- 10.Bernstein GA, Shaw K. Psychiatry AAoCaA. Practice Parameters for the Assessment and Treatment of Children and Adolescents with Anxiety Disorders. American Academy of Child and Adolescent Psychiatry. J Am Acad Child Adolesc Psychiatry. 1997;36:69S–84S. [DOI] [PubMed] [Google Scholar]
- 11.Bernstein GA, Borchardt CM, Perwien AR. Anxiety disorders in children and adolescents: a review of the past 10 years. J Am Acad Child Adolesc Psychiatry. 1996;35:1110–1119. [DOI] [PubMed] [Google Scholar]
- 12.Cohen P, Cohen J, Kasen S. An epidemiological study of disorders in late childhood and adolescence. J Child Psychol Psychiatry. 1993;34:851–867. [DOI] [PubMed] [Google Scholar]
- 13.Henker B, Whalen C, Jamner L. Anxiety, affect, and activity in teenagers: monitoring daily life with electronic diaries. J Am Acad Child Adolesc Psychiatry. 2002;41:660–670. [DOI] [PubMed] [Google Scholar]
- 14.World Health Organization (WHO). Prevention of Mental Disorders: Effective Interventions and Policy Options. Geneva: WHO, 2004. Available at http://www.who.int/mental_health/evidence/en/prevention_of_mental_disorders_sr.pdf, accessed December 26, 2015. [Google Scholar]
- 15.Beesdo-Baum K, Knappe S. Developmental epidemiology of anxiety disorders. Child Adolesc Psychiatr Clin N Am. 2012;21:457–478. [DOI] [PubMed] [Google Scholar]
- 16.Pine DS, Cohen P, Gurley D, et al. The risk for early-adulthood anxiety and depressive disorders in adolescents with anxiety and depressive disorders. Arch Gen Psychiatry. 1998;55:56–64. [DOI] [PubMed] [Google Scholar]
- 17.Wehry A, Beesdo-Baum K, Hennely M, et al. Assessment and treatment of anxiety disorders in children and adolescents. Curr Psychiatry Rep. 2015;17:52.[Note to copyeditor: Citation correct as shown] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Layne A, Bernstein G, Egan E. Predictors of treatment response in anxious-depressed adolescents with school refusal. J Am Acad Child Adolesc Psychiatry. 2003;42:319–326. [DOI] [PubMed] [Google Scholar]
- 19.Kessler R, Nelson C, McGonagle K. Comorbidity of DSM-III-R major depressive disorder in the general population: results from the US National Comorbidity Survey. Br J Psychiatry. 2006;168:17–30. [PubMed] [Google Scholar]
- 20.Unic G, Snowden L, Hastings J. Heterogeneity in comorbidity between major depressive disorder and generalized anxiety disorder and its clinical consequences. J Nerv Ment Dis. 2009;197:215–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wadsworth M, Hudziak J, Heath A. Latent class analysis of Child Behavior Checklist Anxiety/Depression in children and adolescents. J Am Acad Child Adolesc Psychiatry. 2001;40:106–114. [DOI] [PubMed] [Google Scholar]
- 22.Eaton W, Dryman A, Sorenson A. DSM-III major depressive disorder in the community: a latent class analysis of data from the NIMH Epidemiologic Catchment Area Programme. Br J Psychiatry. 1989;155:48–54. [DOI] [PubMed] [Google Scholar]
- 23.Ryan N, Puig-Antich J, Ambrosini P. The clinical picture of major depression in children and adolescents. Arch Gen Psychiatry. 1987;44:854–861. [DOI] [PubMed] [Google Scholar]
- 24.Sullivan P, Kessler R, Kendler K. Latent class analysis of lifetime symptoms in the National Comorbidity Survey. Am J Psychiatry. 1998;155:1398–1406. [DOI] [PubMed] [Google Scholar]
- 25.Vink D, Aartsen M, Comijs H. Onset of anxiety and depression in the aging population: comparison of risk factors in a 9-year prospective study. Am J Geriatr Psychiatry. 2009;17:642–652. [DOI] [PubMed] [Google Scholar]
- 26.King-Kallimanis B, Gum A, Kohn R. Comorbidity of depressive and anxiety disorders for older Americans in the National Comorbidity Survey-Replication. Am J Geriatr Psychiatry. 2009;17:789–792. [DOI] [PubMed] [Google Scholar]
- 27.Achenbach T Manual for the Child Behavior Checklist/4–18 and 1991 Profile. Burlington: University of Vermont Department of Psychiatry; 1991. [Google Scholar]
- 28.Clayton P, Grove W, Coryell W, et al. Follow-up and family study of anxious depression. Am J Psychiatry. 1991;148:1512–1517. [DOI] [PubMed] [Google Scholar]
- 29.Livingston R, Taylor J, Crawford S. A study of somatic complaints and psychiatric diagnosis in children. J Am Acad Child Adolesc Psychiatry. 1988;27:185–187. [DOI] [PubMed] [Google Scholar]
- 30.Bernstein G, Massie E, Thuras P. Somatic symptoms in anxious-depressed school refusers. J Am Acad Child and Adolesc Psychiatry. 1997;36:661–668. [DOI] [PubMed] [Google Scholar]
- 31.Bernstein G Comorbidity and severity of anxiety and depressive disorder in a clinic sample. J Am Acad Child Adolesc Psychiatry. 1991;30:43–50. [DOI] [PubMed] [Google Scholar]
- 32.Bernstein G, Warren S, Massie E. Family dimensions in anxious-depressed school refusers. J Anx Dis. 1993;13:513–528. [DOI] [PubMed] [Google Scholar]
- 33.Woodward L, Fergusson D. Life course outcomes of young people with anxiety disorders in adolescence. J Am Acad of Child and Adolesc Psychiatry. 2001;40:1086–1093. [DOI] [PubMed] [Google Scholar]
- 34.Prange M, Greenbaum P, Silver S. Family functioning and psychopathology among adolescents with severe emotional disturbances. J Abnom Child Psychol. 1992;20:83–102. [DOI] [PubMed] [Google Scholar]
- 35.Fanic S, Middeldorp C, Dolan C. Child and adolescent anxiety and depression: beyond heritability. J Am Acad Child Adolesc Psychiatry. 2010;49:820–829. [DOI] [PubMed] [Google Scholar]
- 36.Thomas KM, Drevets WC, Dahl RE, et al. Amygdala response to fearful faces in anxious and depressed children. Arch Gen Psychiatry. 2001;58:1057–1063. [DOI] [PubMed] [Google Scholar]
- 37.Beesdo K, Lau JY, Guyer AE, et al. Common and distinct amygdala-function perturbations in depressed vs anxious adolescents. Arch Gen Psychiatry. 2009;66:275–285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ho TC, Wu J, Shin DD, et al. Altered cerebral perfusion in executive, affective, and motor networks during adolescent depression. J Am Acad Child Adolesc Psychiatry. 2013;52:1076–1091 e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gabbay V, Ely BA, Li Q, et al. Striatum-based circuitry of adolescent depression and anhedonia. J Am Acad Child Adolesc Psychiatry. 2013;52:628–641 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Shad MU, Muddasani S, Rao U. Gray matter differences between healthy and depressed adolescents: a voxel-based morphometry study. J Child Adolesc Psychopharmacol. 2012;22:190–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pannekoek JN, van der Werff SJ, van den Bulk BG, et al. Reduced anterior cingulate gray matter volume in treatment-naive clinically depressed adolescents. Neuroimage Clin. 2014;4:336–342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.McClure EB, Monk CS, Nelson EE, et al. Abnormal attention modulation of fear circuit function in pediatric generalized anxiety disorder. Arch Gen Psychiatry. 2007;64:97–106. [DOI] [PubMed] [Google Scholar]
- 43.Strawn JR, Dominick KC, Patino LR, et al. Neurobiology of pediatric anxiety disorders. Curr Behav Neurosci Rep. 2014;1:154–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Killgore WD, Yurgelun-Todd DA. Social anxiety predicts amygdala activation in adolescents viewing fearful faces. Neuroreport. 2005;16:1671–1675. [DOI] [PubMed] [Google Scholar]
- 45.Monk CS, Nelson EE, McClure EB, et al. Ventrolateral prefrontal cortex activation and attentional bias in response to angry faces in adolescents with generalized anxiety disorder. Am J Psychiatry. 2006;163:1091–1097. [DOI] [PubMed] [Google Scholar]
- 46.Guyer AE, Lau JY, McClure-Tone EB, et al. Amygdala and ventrolateral prefrontal cortex function during anticipated peer evaluation in pediatric social anxiety. Arch Gen Psychiatry. 2008;65:1303–1312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Strawn JR, Bitter SM, Weber WA, et al. Neurocircuitry of generalized anxiety disorder in adolescents: a pilot functional neuroimaging and functional connectivity study. Depress Anxiety. 2012;29:939–947. [DOI] [PubMed] [Google Scholar]
- 48.De Bellis MD, Casey BJ, Dahl RE, et al. A pilot study of amygdala volumes in pediatric generalized anxiety disorder. Biol Psychiatry. 2000;48:51–57. [DOI] [PubMed] [Google Scholar]
- 49.De Bellis MD, Keshavan MS, Shifflett H, et al. Superior temporal gyrus volumes in pediatric generalized anxiety disorder. Biol Psychiatry. 2002;51:553–562. [DOI] [PubMed] [Google Scholar]
- 50.Milham MP, Nugent AC, Drevets WC, et al. Selective reduction in amygdala volume in pediatric anxiety disorders: a voxel-based morphometry investigation. Biol Psychiatry. 2005;57:961–966. [DOI] [PubMed] [Google Scholar]
- 51.Mueller SC, Aouidad A, Gorodetsky E, et al. Gray matter volume in adolescent anxiety: an impact of the brain-derived neurotrophic factor Val(66)Met polymorphism? J Am Acad Child Adolesc Psychiatry. 2013;52:184–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Strawn JR, Wehry AM, Chu WJ, et al. Neuroanatomic abnormalities in adolescents with generalized anxiety disorder: a voxel-based morphometry study. Depress Anxiety. 2013;30:842–848. [DOI] [PubMed] [Google Scholar]
- 53.Ionescu DF, Niciu MJ, Mathews DC, et al. Neurobiology of anxious depression: a review. Depress Anxiety. 2013;30:374–385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Gorka SM, Huggins AA, Fitzgerald DA, et al. Neural response to reward anticipation in those with depression with and without panic disorder. J Affect Disord. 2014;164:50–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.van Tol MJ, van der Wee NJ, van den Heuvel OA, et al. Regional brain volume in depression and anxiety disorders. Arch Gen Psychiatry. 2010;67:1002–1011. [DOI] [PubMed] [Google Scholar]
- 56.Inkster B, Rao AW, Ridler K, et al. Structural brain changes in patients with recurrent major depressive disorder presenting with anxiety symptoms. J Neuroimaging. 2011;21:375–382. [DOI] [PubMed] [Google Scholar]
- 57.Wehry AM, McNamara RK, Adler CM, et al. Neurostructural impact of co-occurring anxiety in pediatric patients with major depressive disorder: a voxel-based morphometry study. J Affect Disord. 2015;171:54–59. [DOI] [PubMed] [Google Scholar]
- 58.Garvey M, Tollefson G, Tuason V. Comparison of major depressions with and without panic attacks. Compr Psychiatry. 1987;28:65–67. [DOI] [PubMed] [Google Scholar]
- 59.Coryell W, Endicott J, Andreasen N. Depression and panic attacks: the significance of overlap as reflected in follow-up and family study data. Am J Psychiatry. 1988;145:293–300. [DOI] [PubMed] [Google Scholar]
- 60.Mykletun A, Bjerkeset O, Dewey M. Anxiety, depression, and cause-specific mortality: the HUNT study. Psychosom Med. 2007;69:323–331. [DOI] [PubMed] [Google Scholar]
- 61.Foley D, Goldston D. Proximal psychiatric risk factors for suicidality in youth. Arch Gen Psychiatry. 2006;63:1017–1024. [DOI] [PubMed] [Google Scholar]
- 62.Saren J, Cox B, Afifi T. Anxiety disorder and risk for suicidal ideation and suicide attempts. Arch Gen Psychiatry. 2005;62:1249–1257. [DOI] [PubMed] [Google Scholar]
- 63.Gould M, King R, Greenwald S. Psychopathology associated with suicidal ideation and attempts among children and adolescents. J Am Acad Child Adolesc Psychiatry. 1998;37:915–923. [DOI] [PubMed] [Google Scholar]
- 64.Pilowsky D, Wu L, Anthony J. Panic attacks and suicide attempts in mid-adolescence. Am J Psychiatry. 1999;156:1545–1549. [DOI] [PubMed] [Google Scholar]
- 65.Lewinsohn P, Rohde P, Seeley J. Adolescent psychopathology, III: the clinical consequences of comorbidity. J Am Acad Child Adolesc Psychiatry. 1995;34:510–519. [DOI] [PubMed] [Google Scholar]
- 66.Lewinsohn P, Rohde P, Seeley J. Psychosocial risk factors for future adolescent suicide attempts. J Consult Clin Psychol. 1994;62:297–305. [DOI] [PubMed] [Google Scholar]
- 67.Velez C, Cohen P. Suicidal behavior and ideation in a community sample of children. J Am Acad Child Adolesc Psychiatry. 1988;27:349–356. [DOI] [PubMed] [Google Scholar]
- 68.Kashani J, Goddard P, Reid J. Correlates of suicidal ideation in a community sample of children and adolescents. J Am Acad Child Adolesc Psychiatry. 1989;28:912–917. [DOI] [PubMed] [Google Scholar]
- 69.Reinherz H, Giaconia R, Silverman A. Early psychosocial risk for adolescent suicidal ideation and attempts. J Am Acad Child Adolesc Psychiatry. 1995;34:599–611. [DOI] [PubMed] [Google Scholar]
- 70.Klein D, Shankman S, Lewinsohn P. Subthreshold depressive disorder in adolescents: predictors of escalation to full-syndrome depressive disorders. J Am Acad Child and Adolesc Psychiatry. 2009;48:703–710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Oldenhinkel A, Wittchen H, Schuster P. Prevalence, 20-month incidence and outcome of unipolar depressive disorder in a community sample of adolescents. Psychol Med. 1999;29:655–668. [DOI] [PubMed] [Google Scholar]
- 72.Lewinsohn P, Shankman S, Gau J. The prevalence and comorbidity of subthreshold psychiatric conditions. Psychol Med. 2004;34:613–622. [DOI] [PubMed] [Google Scholar]
- 73.Lebeau RT, Glenn DE, Hanover LN, et al. A dimensional approach to measuring anxiety for DSM-5. Int J Methods Psychiatr Res. 2012;21:258–272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Moller EL, Majdandzic M, Craske MG, et al. Dimensional assessment of anxiety disorders in parents and children for DSM-5. Int J Methods Psychiatr Res. 2014;23:331–344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Stein D, Craske M, Friedman M, et al. Anxiety disorders, obsessive-compulsive and related disorders, trauma- and stressor-related disorders, and dissociative disorders in DSM-5. Am J Psychiatry. 2014;171:611–613. [DOI] [PubMed] [Google Scholar]
- 76.Zimmerman M, Chelminski I, Young D, et al. A clinically useful self-report measure of the DSM-5 anxious distress specifier for major depressive disorder. J Clin Psychiatry. 2014;75:601–607. [DOI] [PubMed] [Google Scholar]
- 77.Fawcett J Suicide and anxiety in DSM-5. Depress Anxiety. 2013;30:898–901. [DOI] [PubMed] [Google Scholar]
- 78.Luby J, Belden A, Sullivan J. Preschoolers’ contribution to their diagnosis of depression and anxiety: uses and limitations of young child self-report of symptoms. Child Psychiatry Hum Dev. 2007;38:321–338. [DOI] [PubMed] [Google Scholar]
- 79.Jensen P, Rubio-Stipec M, Canino G. Parent and child contributions to diagnosis of mental disorders: are both informants always necessary? J Am Acad Child Adolesc Psychiatry. 1999;38:1569–1579. [DOI] [PubMed] [Google Scholar]
- 80.Domschke K, Deckert J, Arolt V, et al. Anxious versus non-anxious depression: difference in treatment outcome. J Psychopharmacol (Oxford). 2010;24:621–622. [DOI] [PubMed] [Google Scholar]
- 81.Fava M, Rush AJ, Alpert JE, et al. Difference in treatment outcome in outpatients with anxious versus nonanxious depression: a STAR*D report. Am J Psychiatry. 2008;165:342–351. [DOI] [PubMed] [Google Scholar]
- 82.Papakostas GI, Stahl SM, Krishen A, et al. Efficacy of bupropion and the selective serotonin reuptake inhibitors in the treatment of major depressive disorder with high levels of anxiety (anxious depression): a pooled analysis of 10 studies. J Clin Psychiatry. 2008;69:1287–1292. [DOI] [PubMed] [Google Scholar]
- 83.Thase ME, Demyttenaere K, Earley WR, et al. Extended release quetiapine fumarate in major depressive disorder: analysis in patients with anxious depression. Depress Anxiety. 2012;29:574–586. [DOI] [PubMed] [Google Scholar]
- 84.March JS, Entusah AR, Rynn M, et al. A randomized controlled trial of venlafaxine ER versus placebo in pediatric social anxiety disorder. Biol Psychiatry. 2007;62:1149–1154. [DOI] [PubMed] [Google Scholar]
- 85.Rynn MA, Siqueland L, Rickels K. Placebo-controlled trial of sertraline in the treatment of children with generalized anxiety disorder. Am J Psychiatry. 2001;158:2008–2014. [DOI] [PubMed] [Google Scholar]
- 86.Rynn MA, Riddle MA, Yeung PP, et al. Efficacy and safety of extended-release venlafaxine in the treatment of generalized anxiety disorder in children and adolescents: two placebo-controlled trials. Am J Psychiatry. 2007;164:290–300. [DOI] [PubMed] [Google Scholar]
- 87.Strawn JR, Prakash A, Zhang Q, et al. A randomized , placebo-controlled study of duloxetine for the treatment of children and adolescents with generalized anxiety disorder. J Am Acad Child Adolesc Psychiatry. 2015;54:283–293. [DOI] [PubMed] [Google Scholar]
- 88.Walkup JT, Albano AM, Piacentini J, et al. Cognitive behavioral therapy, sertraline, or a combination in childhood anxiety. N Engl J Med. 2008;359:2753–2766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Connolly SD, Bernstein GA. Practice parameter for the assessment and treatment of children and adolescents with anxiety disorders. J Am Acad Child Adolesc Psychiatry. 2007;56:267–283. [DOI] [PubMed] [Google Scholar]
- 90.Strawn JR, Sakolsky DJ, Rynn M. Psychopharmacologic treatment of children and adolescents with anxiety disorders. Child Adolesc Psychiatr Clin N Am. 2012;21:527–539. [DOI] [PubMed] [Google Scholar]
- 91.Strawn JR, Welge JA, Wehry AM, et al. Efficacy and tolerability of antidepressants in pediatric anxiety disorders: a systematic review and meta-analysis. Depress Anxiety. 2015;32:149–157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Beidel DC, Turner SM, Sallee FR, et al. SET-C versus fluoxetine in the treatment of childhood social phobia. J Am Acad Child Adolesc Psychiatry. 2007;46:1622–1632. [DOI] [PubMed] [Google Scholar]
- 93.Birmaher B, Axelson DA, Monk K, et al. Fluoxetine for the treatment of childhood anxiety disorders. J Am Acad Child Adolesc Psychiatry. 2003;42:415–423. [DOI] [PubMed] [Google Scholar]
- 94.Wagner KD, Berard R, Stein MB, et al. A multicenter, randomized, double-blind, placebo-controlled trial of paroxetine in children and adolescents with social anxiety disorder. Arch Gen Psychiatry. 2004;61:1153–1162. [DOI] [PubMed] [Google Scholar]
- 95.The Research Unit on Pediatric Psychopharmacology (RUPP) Anxiety Study Group. Fluvoxamine for the treatment of anxiety disorders in children and adolescents. N Engl J Med. 2001;344:1279–1285. [DOI] [PubMed] [Google Scholar]
- 96.Wagner KD, Ambrosini P, Rynn M, et al. Efficacy of sertraline in the treatment of children and adolescents with major depressive disorder: two randomized controlled trials. JAMA. 2003;290:1033–1041. [DOI] [PubMed] [Google Scholar]
- 97.Simeon JG, Dinicola VF, Ferguson HB, et al. Adolescent depression: a placebo-controlled fluoxetine treatment study and follow-up. Prog Neuropsychopharmacol Biol Psychiatry. 1990;14:791–795. [DOI] [PubMed] [Google Scholar]
- 98.Emslie GJ, Rush AJ, Weinberg WA, et al. A double-blind, randomized, placebo-controlled trial of fluoxetine in children and adolescents with depression. Arch Gen Psychiatry. 1997;54:1031–1037. [DOI] [PubMed] [Google Scholar]
- 99.Emslie GJ, Heiligenstein JH, Wagner KD, et al. Fluoxetine for acute treatment of depression in children and adolescents: a placebo-controlled, randomized clinical trial. J Am Acad Child Adolesc Psychiatry. 2002;41:1205–1215. [DOI] [PubMed] [Google Scholar]
- 100.March J, Silva S, Petrycki S, et al. Fluoxetine, cognitive-behavioral therapy, and their combination for adolescents with depression: Treatment for Adolescents With Depression Study (TADS) randomized controlled trial. JAMA. 2004;292:807–820. [DOI] [PubMed] [Google Scholar]
- 101.Keller MB, Ryan ND, Strober M, et al. Efficacy of paroxetine in the treatment of adolescent major depression: a randomized, controlled trial. J Am Acad Child Adolesc Psychiatry. 2001;40:762–772. [DOI] [PubMed] [Google Scholar]
- 102.Berard R, Fong R, Carpenter DJ, et al. An international, multicenter, placebo-controlled trial of paroxetine in adolescents with major depressive disorder. J Child Adolesc Psychopharmacol. 2006;16:59–75. [DOI] [PubMed] [Google Scholar]
- 103.Emslie GJ, Wagner KD, Kutcher S, et al. Paroxetine treatment in children and adolescents with major depressive disorder: a randomized, multicenter, double-blind, placebo-controlled trial. J Am Acad Child Adolesc Psychiatry. 2006;45:709–719. [DOI] [PubMed] [Google Scholar]
- 104.Wagner KD, Robb AS, Findling RL, et al. A randomized, placebo-controlled trial of citalopram for the treatment of major depression in children and adolescents. Am J Psychiatry. 2004;161:1079–1083. [DOI] [PubMed] [Google Scholar]
- 105.von Knorring AL, Olsson GI, Thomsen PH, et al. A randomized, double-blind, placebo-controlled study of citalopram in adolescents with major depressive disorder. J Clin Psychopharmacol. 2006;26:311–315. [DOI] [PubMed] [Google Scholar]
- 106.Wagner KD, Jonas J, Findling RL, et al. A double-blind, randomized, placebo-controlled trial of escitalopram in the treatment of pediatric depression. J Am Acad Child Adolesc Psychiatry. 2006;45:280–288. [DOI] [PubMed] [Google Scholar]
- 107.Emslie GJ, Ventura D, Korotzer A, et al. Escitalopram in the treatment of adolescent depression: a randomized placebo-controlled multisite trial. J Am Acad Child Adolesc Psychiatry. 2009;48:721–729. [DOI] [PubMed] [Google Scholar]
- 108.Emslie GJ, Findling RL, Yeung PP, et al. Venlafaxine ER for the treatment of pediatric subjects with depression: results of two placebo-controlled trials. J Am Acad Child Adolesc Psychiatry. 2007;46:479–488. [DOI] [PubMed] [Google Scholar]
- 109.Emslie GJ, Prakash A, Zhang Q, et al. A double-blind efficacy and safety study of duloxetine fixed doses in children and adolescents with major depressive disorder. J Child Adolesc Psychopharmacol. 2014;24:170–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Atkinson SD, Prakash A, Zhang Q, et al. A double-blind efficacy and safety study of duloxetine flexible dosing in children and adolescents with major depressive disorder. J Child Adolesc Psychopharmacol. 2014;24:180–189. [DOI] [PubMed] [Google Scholar]
- 111.BuSpar [package insert] Princeton NJ: Bristol-Myers Squibb; 2010. [Google Scholar]
- 112.Chavira DA, Stein MB. Combined psychoeducation and treatment with selective serotonin reuptake inhibitors for youth with generalized social anxiety disorder. J Child Adolesc Psychopharmacol. 2002;12:47–54. [DOI] [PubMed] [Google Scholar]
- 113.Isolan L, Pheula G, Salum GA Jr,et al. An open-label trial of escitalopram in children and adolescents with social anxiety disorder. J Child Adolesc Psychopharmacol. 2007;17:751–760. [DOI] [PubMed] [Google Scholar]
- 114.Brent D, Emslie G, Clarke G, et al. Switching to another SSRI or to venlafaxine with or without cognitive behavioral therapy for adolescents with SSRI-resistant depression: the TORDIA randomized controlled trial. JAMA. 2008;299:901–912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.March J, Silva S, Curry J, et al. The Treatment for Adolescents With Depression Study (TADS): outcomes over 1 year of naturalistic follow-up. Am J Psychiatry. 2009;166:1141–1149. [DOI] [PubMed] [Google Scholar]
- 116.Mufson LH, Dorta KP, Olfson M, et al. Effectiveness research: transporting interpersonal psychotherapy for depressed adolescents (IPT-A) from the lab to school-based health clinics. Clin Child Fam Psychol Rev. 2004;7:251–261. [DOI] [PubMed] [Google Scholar]
- 117.Fonagy P, Target M. Playing with reality: I. Theory of mind and the normal development of psychic reality. Int J Psychoanal. 1996;77(Pt 2): 217–233. [PubMed] [Google Scholar]
- 118.Kernberg PF, Ritvo R, Keable H. Practice parameter for psychodynamic psychotherapy with children. J Am Acad Child Adolesc Psychiatry. 2012;51:541–557. [DOI] [PubMed] [Google Scholar]
- 119.Emslie GJ, Mayes T, Porta G, et al. Treatment of resistant depression in adolescents (TORDIA): week 24 outcomes. Am J Psychiatry. 2010;167:782–791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Walkup J, Labellarte M, Riddle MA, et al. Treatment of pediatric anxiety disorders: an open-label extension of the Research Units on Pediatric Psychopharmacology Anxiety Study. J Child Adolesc Psychopharmacol. 2002;12:175–188. [DOI] [PubMed] [Google Scholar]
- 121.El-Khalili N, Joyce M, Atkinson S, et al. Extended-release quetiapine fumarate (quetiapine XR) as adjunctive therapy in major depressive disorder (MDD) in patients with an inadequate response to ongoing antidepressant treatment: a multicentre, randomized, double-blind, placebo-controlled study. Int J Neuropsychopharmacol. 2010;13:917–932. [DOI] [PubMed] [Google Scholar]
- 122.Bauer M, Pretorius HW, Constant EL, et al. Extended-release quetiapine as adjunct to an antidepressant in patients with major depressive disorder: results of a randomized, placebo-controlled, double-blind study. J Clin Psychiatry. 2009;70:540–549. [DOI] [PubMed] [Google Scholar]
- 123.Pathak S, Johns ES, Kowatch RA. Adjunctive quetiapine for treatment-resistant adolescent major depressive disorder: a case series. J Child Adolesc Psychopharmacol. 2005;15:696–702. [DOI] [PubMed] [Google Scholar]
- 124.Khan A, Joyce M, Atkinson S, et al. A randomized, double-blind study of once-daily extended release quetiapine fumarate (quetiapine XR) monotherapy in patients with generalized anxiety disorder. J Clin Psychopharmacol. 2011;31:418–428. [DOI] [PubMed] [Google Scholar]
- 125.Merideth C, Cutler AJ, She F, et al. Efficacy and tolerability of extended release quetiapine fumarate monotherapy in the acute treatment of generalized anxiety disorder: a randomized, placebo controlled and active-controlled study. Int Clin Psychopharmacol. 2012;27:40–54. [DOI] [PubMed] [Google Scholar]
- 126.McClellan J, Kowatch R, Findling RL. Practice parameter for the assessment and treatment of children and adolescents with bipolar disorder. J Am Acad Child Adolesc Psychiatry. 2007;46:107–125. [DOI] [PubMed] [Google Scholar]
- 127.Fava M, Mischoulon D, Iosifescu D, et al. A double-blind, placebo-controlled study of aripiprazole adjunctive to antidepressant therapy among depressed outpatients with inadequate response to prior antidepressant therapy (ADAPT-A Study). Psychother Psychosom. 2012;81:87–97. [DOI] [PubMed] [Google Scholar]
- 128.Berman RM, Fava M, Thase ME, et al. Aripiprazole augmentation in major depressive disorder: a double-blind, placebo-controlled study in patients with inadequate response to antidepressants. CNS Spectr. 2009;14:197–206. [DOI] [PubMed] [Google Scholar]
- 129.Menza MA, Dobkin RD, Marin H. An open-label trial of aripiprazole augmentation for treatment-resistant generalized anxiety disorder. J Clin Psychopharmacol. 2007;27:207–210. [DOI] [PubMed] [Google Scholar]
- 130.Worthington JJ 3rd, Kinrys G, Wygant LE, et al. Aripiprazole as an augmentor of selective serotonin reuptake inhibitors in depression and anxiety disorder patients. Int Clin Psychopharmacol. 2005;20:9–11. [DOI] [PubMed] [Google Scholar]
- 131.Trivedi MH, Thase ME, Fava M, et al. Adjunctive aripiprazole in major depressive disorder: analysis of efficacy and safety in patients with anxious and atypical features. J Clin Psychiatry. 2008;69:1928–1936. [PubMed] [Google Scholar]


