Abstract
The year 2013 marks the 25th anniversary of the Automated Method for islet isolation. The dissociation chamber at the core of the Automated Method was developed by Dr. Camillo Ricordi in 1988 to enhance the disassembling of the pancreatic tissue via a combined enzymatic and mechanical digestion while preserving endocrine cell cluster integrity. This method has ever since become the gold standard for human and large animal pancreas processing, contributing to the success and increasing number of clinical trials of islet transplantation worldwide. Herein we offer an attempt to a comprehensive, yet unavoidably incomplete, historical review of the progress in the field of islet cell transplantation to restore beta-cell function in patients with diabetes.
Keywords: Pancreatic islets, Diabetes, Islet transplantation, Automated method, History
“…This cell has a small and polygonal structure. Its cytoplasm is perfectly brilliant and free from granules, with a distinct nucleus that is round and of discrete dimension. This type of cell clusters, generally in large number, is diffusely scattered in the glandular parenchyma. These clusters have generally a diameter of 0.1-0.24 mm and may be easily distinguished in fragmented pancreatic preparations…”1. With these words, the German anatomist and anthropologist Paul Langerhans described for the first time the pancreatic islets in his dissertation published in 1869 summarizing the results of his research as medical student in Berlin in the laboratory of Rudolf von Virchow’s1. In 1893, the French pathologist and histologist Gustave-Édouard Laguesse associated the Langerhans’ name to that of islets (“îlots de Langerhans”) having observed similar structures in the human pancreas2. In those years, insulin had not yet been discovered (until 1922, by Fredrik Bating and Charles Best from London, Ontario) and part of the scientific discussion was polarized on whether the pancreas produced or not “a substance able to destroy glucose”. Thus, the research was primarily focused on attempts to demonstrate that pancreatic fragments transplanted into diabetic animals could cure the disease. The first success was reported in the medical literature in 1882 by doctors Oscar Minkowski and Joseph von Mering at the University of Strasburg demonstrating transient improvement of glycosuria following subcutaneous transplantation of autologous pancreatic fragments in a pancreatectomy-induced diabetic dog3. The following year (1883), doctor P. Watson Williams and surgeon William H. Harsant at Bristol Royal Infirmary in the UK attempted the first transplant of three fresh sheep pancreatic fragments in the subcutaneous space of a 15-year old boy with ketoacidosis, who eventually died and histopathological assessment demonstrated “fibrous stroma” in the grafts4.
In the subsequent years, most of the research aimed at demonstrating the hypothesis of the presence in the pancreas of beneficial secretion through transplantation of fragments in sited alternative to the subcutaneous space. In 1896, Italian surgeon Roberto Alessandri at the Royal University in Rome reported for the first time the transplant of autologous pancreatic fragments in the dog spleen after pancreatectomy, though without achieving measurable graft function5; similar results were reported by others6–8. Alessandri also tried for the first time the intrahepatic site with poor success5, 8. Despite these failures, the attempts increased and it is noteworthy the series of small pancreatic fragment allografts performed into liver, spleen, peritoneal cavity and subcutaneous space of experimental animals by doctor Donato Ottolenghi in 1901 in Turin, Italy7; despite the extremely small size of the fragments utilized, all grafts underwent necrosis and resorption within a couple of days, even if in a few cases preserved insular tissue was observed at histopathological evaluation. In 1903, doctor James Allan at Glasgow Royal Infirmary attempted another xenotransplant using feline pancreatic fragments in a patient with diabetes who died two weeks later with ketoacidosis9. The British surgeon Frederick Charles Pybus, in light of initial success obtained with adrenal grafts in the treatment of Addison disease, attempted in 1916 the transplant of allogeneic pancreatic tissue into patients with diabetes10; considering that previous attempts with xenogeneic tissue had failed, he recovered a human pancreas immediately after the death of a trauma victim and transplanted slices into the abdominal subcutaneous space of two males with diabetes (32 and 37 years old, respectively). Despite transient reduction of glycosuria in one patient, none of the grafts yielded reversal of diabetes10. The disappointing outcome and the subsequent discovery and implementation of insulin therapy for diabetes tempered the interest and limited the development of further research on the transplantation of pancreatic tissue in the following years.
An important intuition that impacted significantly the progress of experimental research was the hypothesis that function and viability of the endocrine pancreatic graft was impaired by the presence of exocrine acinar tissue. In order to overcome the potential detrimental effect of acinar tissue in pancreatic grafts, two hypothetical solutions were developed. One of the approaches considered transplanting a tissue “enriched” of islets such as fetal or neonatal pancreas, since the development of the exocrine and endocrine pancreas is not synchronous with endocrine cells appearing early during organo-genesis11 and being able to synthesize and secrete insulin and glucagon in the period preceding exocrine differentiation. Studies in experimental animals demonstrated that the survival of the graft was influenced by donor age11–13 and that survival over 56 days could be achieved with fetal and neonatal pancreatic grafts implanted in the cheek of hamsters13. The other methodological approach pursued was to separate the endocrine tissue from the exocrine component before the transplant.
The idea to physically separate the endocrine component from the exocrine pancreas was originally proposed by Russian doctor Leonid W. Ssobolew from Saint Petersburg in 190214, but was not pursued at least for almost 60 years before the isolation of the islets of Langerhans was reported in the medical literature15. In fact, the development of pancreatic islet isolation techniques was characterized by a first era relying on microdissection under the microscope as described in 1964 by doctor Claes Hellerstöm at Uppsala University in Sweden15, though with poor results both in terms of yields and quality (namely, substantial functional impairment). Considering the paucity of endocrine pancreatic tissue, the research focused on transplantation in experimental animal models did not progress much in this period. A renewed impulse to the field followed the discovery of the action of collagenases on pancreatic fragments and the introduction of the enzymatic processing. Polish doctor Stanisław Moskalewski described in 1965 a novel method isolate the islets from the minced Guinea pig pancreas using collagenase action that resulted in loss of acinar tissue and freeing of pancreatic islet clusters16. His method was further improved by U.S. doctors Paul E. Lacy and Mery Kastianovsky at Washington University in Saint Louis, MO, with the introduction of intra-ductal injection of cold saline buffer to obtain the distension of the pancreas prior to mincing and enzymatic digestion followed by had-picking under the dissecting microscope17. Clearly, this approach did not allow obtaining adequate islet yields for transplant experiments into animals, with the purification step being the limiting factor of the process. A step forward toward overcoming this hurdle was the introduction of density gradient purification that was initially based on sugar or albumin. Subsequently, the use of discontinuous gradient purification with Ficoll by Arnold Lindall and Coll. at University of Minnesota contributed to achieving higher yields after islet isolation even though initially the cell product obtained with this technique was not functional18. Only when Ficoll was dialyzed and lyophilized in doctor Lacy’s laboratory vital islets could be obtained for experimental transplant studies. Indeed, Lacy established the two phases of islet cell processing: (i) islet cluster dissociation and dispersion followed by (ii) islet purification from the pancreas. The technique became the standard for rodent islet isolation for the following decade that led to remarkable volume of studies addressing pancreatic islet metabolism, physiology and immunobiology. In 1972, U.S. doctors Walter F. Ballinger II and Lacy reported the first successful reversal of experimental diabetes in rats following intraperitoneal implantation of 400-600 islets and also that retrieval of transplanted tissue resulted in the reoccurrence of diabetes, as well as the presence of both alpha and beta-cells in explanted tissue at histopathological analysis19. A further step forward in experimental islet transplant was the 1973 study by doctor Charles B. Kemp and Coll. at Washington University describing that the technique of islet embolization into the liver of recipient rats through the portal vein improved the efficiency of transplanted islets compared to the intraperitoneal site with recovery of glucose homeostasis within 2-3 days from implant20. This study set the basis for the choice of the intraportal islet infusion technique in the clinical setting that still today remains the transplant site of choice.
The islet isolation technique developed in the rat by doctor Lacy resulted in a significant increase of experimental studies in rodents. However, for several years the attempts to extend the Lacy isolation protocol to large animal pancreas (i.e., dog, nonhuman primate and human) yielded poor results with no reports of purified islet cell preparations until 197721. In the mid 1970’s the approach of avoiding the purification process for large animal pancreas because of the big islet loss gained favor. Several reports in the literature describe attempts to use pancreatic fragments containing unpurified islets to cure experimental diabetes in large animals22,23.
An important innovative approach to enhance the isolation protocol for large animal pancreas was described by doctors Atsushi Horaguchi and Ronald C. Merrell at Stanford University using a dog model24. Their protocol consisted of three phases: (i) the cannulation of pancreatic duct with intra-ductal injection of collagenase solution to better digest the fibrotic stmctures; (ii) mechanical dissociation with digestion at 37 °C; and (iii) filtration of the pancreatic digest through a 400 μm filter mesh24. With this approach, islet recovery was estimated of 57 % with a purification of approximately 10%: thus, it became possible obtaining adequate islets for transplantation from a single donor. In the same period, doctors Garth L. Warnock, Ray V. Rajotte and A.W. Procyshyn at the University of Alberta demonstrated that improvements in the technique of pancreatic micro-fragment transplantation into the splenic sinusoids could result to the achievement of sustained normoglycemia in diabetic dogs25,26. This allowed for the development in experimental models of immunosuppression as well as of cryopreservation protocols by doctor Rajotte and Coll. for the storage pancreatic fragments at −196°C27.
At the end of 1970’s, the technique by Horaguchi and Merrell applied to the human pancreas led to initial attempts of unpurified pancreatic micro-fragment transplantation in the clinical arena by doctors John S. Najarian, David E.R. Sutherland, Arthur J. Matas, Fred C. Goetz and Coll. at the University of Minnesota28,29, though resulting in poor metabolic control30 and did not solve the numerous clinical issues associated with inadequate immunosuppression, suboptimal endocrine mass transplanted vis-à-vis the complications associated with the lack of purification of the grafted tissue (namely, portal hypertension and disseminated intravascular coagulation).
The first report of successful transplantation of allogeneic pancreatic fragments into patients with Type 1 diabetes was reported in 1979 by doctors Felix Largiadèr, E. Kolb and Ulrich Binswanger at Zurich University30,31; one of the patients, a 22 years old with T1D and severe retinopathy and nephropathy underwent simultaneous allogeneic kidney along intrasplenic pancreatic micro-fragments (obtained from two donors) transplantation under anti-lymphocyte serum, azathioprine, cyclophosphamide and prednisone treatment and showed sustained normoglycemia 1 year post-transplant. Over the months post-transplant, besides improvement of renal graft function, a progressive reduction of exogenous insulin requirements was observed, with achievement of insulin independence by 8 months that lasted for ten months, when rejection of the kidney was associated with hyperglycemia recurrence. The patients died a month later and intrasplenic pancreatic islets could be detected in the necroptic specimens30,31. More substantial, both in terms of numbers and measurable success, was the clinical experience with autologous intrahepatic islet transplantation as a palliative treatment of pain in patients with chronic pancreatitis undergoing total pancreatectomy performed by doctors Najarian, Sutherland, Matas and Goetz at the University of Minnesota28,29,32,33.
In the 1980’s, new progress were reported with the islet isolation techniques from dog and human pancreata by doctor Daniel H. Mintz’s group at the University of Miami and doctor Derek W. Gray and Coll. at Oxford University34–37. Briefly, the protocol consisted of intraductal injection collagenase injection, dispersion of the pancreatic tissue by mechanical agitation and passing through a series of graded needles followed by purification using filtration and centrifugation on density gradient solution – a method that would allow yields of approximately purity of 20-40% from human glands35,36. The technique showed some promise in canine islet transplantation models, particularly for the autografts while it required more than one donor in the allografts37–39. Using modifications of this method, doctors Rodolfo Alejandro, Daniel H. Mintz and Coll. at the University of Miami initiated in 1985 a pilot clinical trial of 5 allogeneic islet transplantation in four C-peptide negative patients with Type 1 diabetes with evidence of retinopathy, nephropathy and neuropathy as islet after kidney (IAK) and simultaneous islet-kidney (SIK) transplantation (negative serum crossmatch and ABO compatible donor:recipient combination)36,40. Novelty introduced in the field through this clinical trial include: preservation of the pancreas by hypothermic pulsatile perfusion with cryoprecipitated silica-treated human plasma, the use of transhepatic portal vein cannulation for three procedures with monitoring of portal vein pressure before and after islet infusion, as well as modulation of islet immunogenicity by treatment with anti-Ia monoclonal antibody in vitro. The longest islet graft function was measured for 26 and 18 weeks in two transplants, and graft failure invariable occurred in all cases possibly consequent to inadequate levels of immunosuppression36.
During the same years modifications in the canine islet isolation procedures allowed to obtain adequate numbers in volumes of pancreatic tissue to be safely infused in the portal system without inducing portal hypertension while treating diabetes were introduced by doctors Mark S. Cattral, Warnock, Norman M. Kneteman, and Rajotte at the University of Alberta by combining intraductal perfusion with collagenase of the pancreas, gentle dissociation and purification of density gradients41,42.
A turning point for clinical islet transplantation was the introduction of the “Automated Method” of pancreas dissociation by doctor Camillo Ricordi, who, after obtaining his medical degree from the University of Milan, received an NIH Research Trainee Award in 1986 to join doctor Lacy’s team at Washington University. The method consisted of a mechanically enhanced enzymatic digestion based on a dissociation/filtration chamber allowing pancreatic fragments and islets freed from gland to be removed promptly from the system to avoid overdigestion while preserving cluster integrity (Figures 1 and 2). The method was first published in 198843 and has represented ever since the gold standard for virtually all research centers working on human44 and large animal islets45, besides its application also for the isolation of other tissues46. Shortly after the introduction of the automated method, the initial success with islet transplantation in humans were reported by doctors David W. Scharp, Lacy, Ricordi and Coll. at Washington University with a first series of patients with T1D and established or incipient nephropathy to ascertain if insulin independence could be attained and if immunosuppression could be discontinued one year after transplantation without rejection. Three subjects received approximately 6,000 islet equivalents per kg of body weight but all lost graft function despite ongoing immunosuppressive regimen (azathioprine, prednisone and cyclosporine)47; additional islet transplants were performed with some degree of success thereafter47–49. Using a more elaborated islet isolation technique50, doctors Warnock, Rajotte and Coll. at the University of Alberta reported a good production of C-peptide in two recipients with T1D following SIK (from the same donor). They received conventional triple immunosuppression that had to be reduced in both cases due to CMV infection 6 week post-transplant with subsequent loss of islet graft function.
Figure 1.
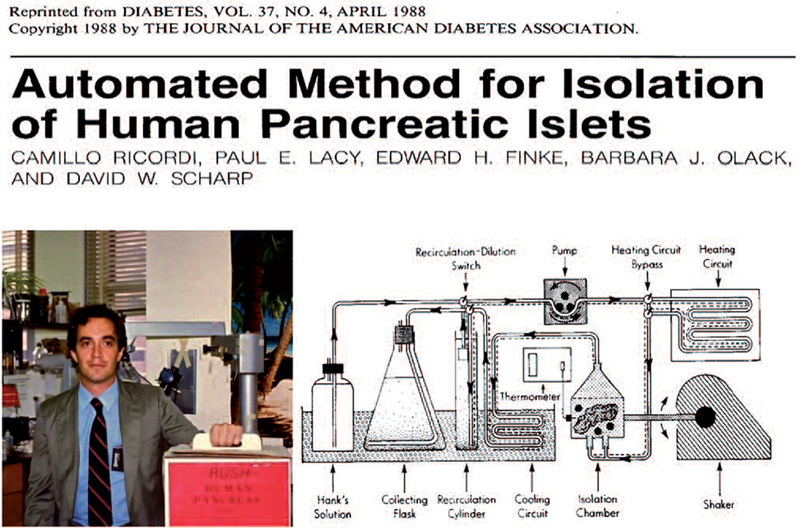
The headings of the manuscript describing the Automated Method and a picture of Dr. Ricordi with one of the first human pancreas shipments from NDRI that was processed in Saint Luis.
Figure 2.
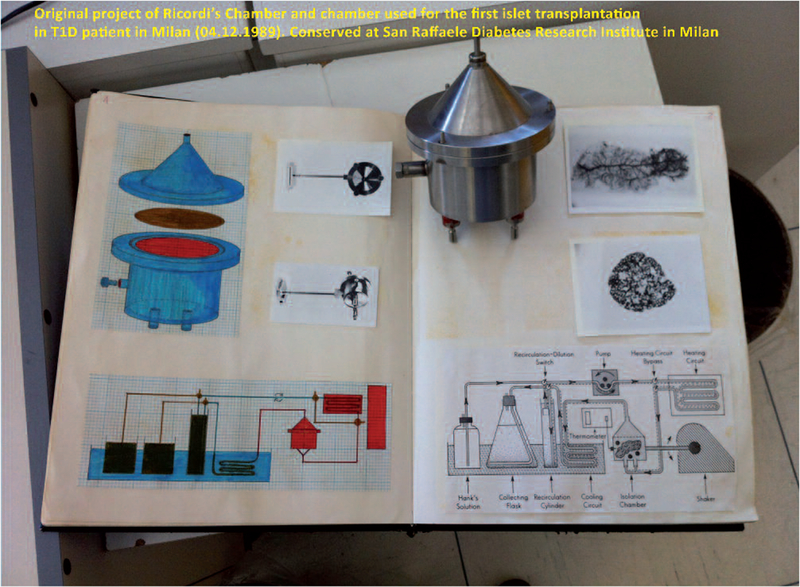
One of the initial prototypes of the stainless steel Dissociation Chamber and Dr. Ricordi’s Laboratory Notebook describing the concept and drafts of the Automated Method for islet isolation. Photo by L. Piemonti (Milan, 3rd March 2013).
Further improvements were introduced in the late 1980’s. Amongst these were techniques aimed at optimizing the efficiency of the purification of large animal and human islets using a semiautomated method of density gradient separation using computerized cell separator by doctors Stephen P. Lake and Coll. from the Leicester Royal Infirmary in UK51 and doctors Alejandro and Mintz from the University of Miami52; improved gradients that incorporated cold preservation solutions by student Barbara J. Olack and Coll. at Washington University53; techniques to stain islet cell clusters with zinc dye by doctor R. Alejandro and Coll.54 and by doctor W. A. Hansen and Coll. from Hagedorn Research Laboratory in Gentofte, Denmark; as well as the publication of consensus papers aimed at standardizing human islet assessment55 contributed to progress in the field.
In the 1990, the introduction of novel techniques to improve the efficiency of isolation techniques resulting in high yields of pancreatic islets contributed to the development of numerous clinical protocols around the World. In the early 1990’s, doctor Ricordi moved to the University of Pittsburgh to direct the Cellular Transplantation Division of the Transplantation Institute headed by doctor Thomas Starzl. Also doctors Alejandro and Mintz from the University of Miami joined forces with doctors Ricordi and Starzl’s Team to help optimizing protocols and accelerate the progress in the field of islet transplantation. The first series of sustained insulin independence was obtained in nine patients undergoing excision of liver and pancreas (that would result in surgery-induced diabetes) and receiving allogeneic liver and islet transplantation from the same cadaveric donor; the first clinical case of sustained insulin independence following allogeneic islet transplantation was a 15 years old girl whose visceral organs were excided for cancer who received multi-visceral organ (liver, small bowel and islet) transplantation56,57. These trials allowed improving the transplant technique with the introduction of the use of slow infusion (by gravity) of the islet graft kept in suspension into an infusion bag to reduce the risk of portal hypertension56,58.
In 1990, doctors Scharp, Lacy and Coll. at Washington University reported the first case of transient exogenous insulin independence obtained following transplantation of 800,000 cultured allogeneic islets with 95% purity (pool of two allogeneic islet preparations) isolated using the automated method into a patient with T1D receiving Minnesota anti-lymphocyte serum, azathioprine and cyclosporine48. Ten days after transplantation, the patient achieved normoglycemia (albeit with glucose intolerance) and could discontinue exogenous insulin therapy for 2 weeks48. Insulin independence following islet transplantation from a single donor obtained using the automated method was reported by doctor Carlo Socci and Coll. at the San Raffaele Institute in Milan, Italy in a patient with T1D transplanted on April 25 199059. Subsequently, insulin independence and/or consistent graft function after islet transplantation was reported by Centers across the World using also cryopreserved60 along to fresh allogeneic islets, paving the way for a possible clinical application of cellular therapies to restore beta-cell function in patients with T1D.
In 1994, German doctors Bernard J. Hering, Reinhard G. Bretzel and Coll. at Justus-Liebig University in Giessen reported 30% insulin independence after allogeneic islet transplantation in patients treated with cyclosporine and steroids and receiving an anti-oxidant therapy and intense intravenous insulin management in the peritransplant period61. In 1997, doctors Antonio Secchi, Socci, Guido Pozza and Coll. at the San Raffaele Institute in Milan reported a 45% insulin independence rate by administering elevated islet numbers (~11,000 islet equivalents per kg of body weight) under cyclosporine and steroid immunosuppression62. Also, Alejandro, Ricordi, Joshua Miller, Mintz, and Coll. at the University of Miami reported long-term (6 years) function in patients with T1D recipients of allogeneic islets and kidneys40, two of which maintained detectable C-peptide for 13 years63. The development of better purified and characterized enzyme blends characterized by reduced endotoxin contamination64–67 resulted in higher reproducibility, when compared to other collagenase blends available at the time (i.e., Collagenase P), contributing significantly to achieving improved islet yields from human pancreata68–70. At the same time, initial attempts of fetal porcine islet cell cluster transplantation were performed in uremic patients with diabetes receiving a renal allograft by doctors Carl G. Groth, Olle Korsgren, Anita Tibell and Coll. at the Karolinska Institute in Stockholm, Sweden71. The grafts were implanted intra-hepatically or under the renal capsule under conventional immunosuppression with anti-thymocyte globulin or 15-deoxyspergualin, and showed detectable c-peptide in the urines for up to 200-400 days71 without evidence of porcine endogenous retrovirus infections72. In 1992 doctor Ricordi funded the Cell Transplantation Society (CTS) during the first meeting that was held in Pittsburgh, PA. The CTS that is now a section of The International Transplantation Society (TTS), has steadily grown gaining an important role for advancements of the field of islet transplantation and for cellular transplantation by and large.
The Islet Transplantation Registry (http://www.med.uni-giessen.de/itr/) collected the experience on a total of 267 transplants performed in several Centers voluntarily reporting the outcome of their trials from 1990 until 200173. Collectively, the outcome was overall rather modest with only 12.4% of the 267 transplants achieving insulin independence for periods greater than a week and only 8.2% for over one year73. A new era in the field of islet transplantation begun with the introduction of the ‘Edmonton Protocol’ in 1999 by doctors A.M. James Shapiro, Jonathan R.T. Lakey, Edmond A. Ryan, Gregory S. Korbutt, Ellen Toth, Garth L. Warnock, Norman M. Kneteman, and Ray V. Rajotte at the University of Alberta in Canada74. The trial showed 100% insulin independence at 12 months in 7 consecutive individuals with brittle T1D and was characterized by: (i) implantation of large numbers of freshly isolated (no culture) cadaveric allogeneic islets (mean of 11,574 islet equivalents/kg per recipient obtained from multiple donors), (ii) the use of human albumin instead of fetal bovine serum in the media utilized for cell processing, and (iii) the use of a steroid-free immunosuppressive regimen based on sirolimus, tacrolimus and anti-IL-2 antibody74. This protocol was subsequently reproduced in a multicenter international trial75 that yielded 58% insulin independence at one year and revealed the important impact of the center experience in islet cell processing and patient management on clinical outcomes76.
In the meanwhile, the ‘Edmonton Protocol’ was adopted with or without various modifications at several institutions contributing to increasing the numbers of islet transplants performed worldwide. Overall, the results from these single center trials showed consistent achievement of metabolic improvements with normalization of HbA1c and glycemic excursions using low exogenous insulin doses and complete insulin independence after transplantation of adequate islet numbers, paralleled by a significant reduction/elimination of severe hypoglycemic episodes and improved quality of life in patients with unstable diabetes receiving islet transplant alone (ITA), islet-after kidney (IAK) or simultaneous islet-kidney (SIK) transplantation50,75,77–93.
At the evaluation of the extended follow up of patients receiving the ‘Edmonton Protocol’ it was revealed that progressive loss of insulin independence occurred over time, with need to reintroduce exogenous insulin resulting in excellent metabolic control long term and HbA1c. While approximately 80% of the patients showed sustained graft function (measured as persistence of detectable C-peptide), only 10% of study subjects maintained independence from exogenous insulin five years after transplantation94. The possible causes of the progressive loss of graft function are multifold95. Since 2005 to date, the clinical research has focused on the major objectives of obtaining and maintaining the longest possible time high rates of insulin independence with lowest islet numbers. At the present time, in at least 5 centers (namely, Edmonton, Minneapolis, Geneva, Lille and Milan) have been reported proportions of insulin independence between 40-50% at five years after transplantation96–99, which are not too far from those of pancreas transplant alone. Furthermore, the data available through the CITR confirm an overall trend toward an improvement of insulin independence at 3 years (approximately 44% of patients) following islet transplantation.
The islet transplant community is rapidly growing. The Collaborative Islet Transplant Registry (CITR; www.citregistry.org) has been established in 2001 and has been collecting data from over thirty Centers in North America, Europe and Oceania through self-reporting their activity. In the most recent CITR Report100, a total of 571 recipients received 1,072 islet infusions from 1,187 donor pancreata, the majority of transplant being ITA. The availability of pooled data from different centers is invaluable as it allows analyses of clinical outcomes and provide insights on potential variables associated with higher success rates of islet transplantation93, 101–105. Notably, the community is likely much larger than what currently captured by the CITR, since several Centers in Europe, Asia and South America that have and/or are performing islet transplantation trials in recent years do not necessarily report to the Registry; these include, amongst others: the trial by doctors Frantisek Saudek and Coll. at Prague University in Czech Republic106; by doctor Shinichi Matzumoto and Coll. at Kyoto University107,108; the trial by doctor Pablo F. Argibay and Coll. in Argentina109; the trial by doctor Mari Cleide Sogayar and Coll. in Brazil110; and the trial introducing Campath-1H in SIK transplant recipients by doctor Janming Tan and Coll. at Xiamen University in China111.
Amongst the several progresses of the recent years, it is worth mentioning at least a few that contributed moving the field forward. The introduction of CD25 targeting in islet transplant recipients by doctor Philip Morel and Coll. at the University of Geneva112. The development of islet transplant consortia to maximize efficiency of the transplant programs, such as the Portland/Minneapolis, the Huddinge/Giessen, the Swiss-French GRAGIL89,113–115, the Miami/Huston and Miami/Dallas116–120 the Miami/Washington DC121,122; the Geneva/Athens123 networks. The introduction of iodixanol-University of Wisconsin solution density gradients to enhance large animal124–126 and later human127 islet separation by doctor Michel P.M. van der Burg and Coll. at Leiden University in the Netherland. The utilization of cultured islets by the University of Minnesota and University of Miami groups128–130. The implementation of anti-CD3 antibody at induction by doctor Bernard J. Hering and Coll. at the University of Minnesota128. The attempts at inducing hematopoietic chimerism in islet transplant recipients by combined bone marrow-derived stem cell and islet transplantation at the University of Miami63,131,132. The invaluable report describing the histopathological features of bioptic specimens obtained from a patient who passed away >13 years of insulin independence following islet transplantation by doctor Thierry Berney and Coll. at the University of Geneva in Switzerland133. The understanding of the critical role of stress-activated signal transduction pathways occurring in the pancreas and islets due to ischemia following donor cerebral death, organ preservation and islet isolation resulting in amplification of acute, nonspecific inflammation on islet yields, quality and immunogenicity reported by several research groups, including doctors Stephen Paraskevas, Laurence Rosenberg and Coll. in Montreal, Canada134, Saida Abdelli, Christophe Bonny and Coll. at the University of Lausanne in Switzerland135,136, Rita Bottino, Massimo Trucco and Jon D. Piganelli and Coll. at the University of Pittsburgh137, amongst others138,139. The discovery of islet production of tissue factor, described by doctors Lisa Moberg, Bo Nillson and Coll. at the Karolinska Institute (140), MCP-1/CCL2 described by doctors Lorenzo Piemonti, Federico Bertuzzi and Coll. at the San Raffaele Institute in Milan, Italy141–144, CD40 described by doctor Ricardo L. Pastori and Coll. at the University of Miami145, amongst others. The description that targeting the TNF pathway after transplantation may be beneficial to improve islet engraftment in rodents by doctors Alan C. Farney and Coll. in 1993 at the University of Minnesota146, which was substantiated by the demonstration of the significant release of pro-inflammatory cytokines such as TNF-alpha and the induction of endothelial cell activation upon intrahepatic embolization of allogeneic rat islets or inert beads which could be partially reduced via macrophage depletion as shown by doctors Rita Bottino, Luis Fernandez, Camillo Ricordi, Luca Inverardi and Coll. at the University of Miami in 1998147, thus justifying the subsequent introduction of TNF-alpha signaling blockers in clinical islet transplant recipients by the University of Miami130,131,148 and University of Minnesota97,129, which retrospectively was confirmed as one of the key factors associated with the success of islet transplantation101. The demonstration of synergy when combining blockade of TNF-alpha and IL-1-beta signaling by doctors Morihito Takita, Shinichi Matsumoto, Marlon F. Levy and Coll. at Baylor Research Institute in Dallas, TX149. The description of the triggering of an instant blood mediated inflammatory reaction involving coagulation factors, platelets and leukocytes immediately after intra-portal islet implantation by doctors William Bennet, Carl G. Groth, Olle Korsgren and Coll. at the Karolinska Institute150, which led to implementation of targeted anti-inflammatory strategies to improve islet engraftment and survival including the introduction of novel anti-inflammatory treatment targeting CXCR1/2 by doctor Piemonti and Coll. at the San Raffaele Institute (151). The optimization of pancreas preservation solution containing per-fluorocarbons to improve oxygenation during cold storage (‘Two Layer Method’) by doctors Yoshikazu Kuroda, T Kawamura, Yoichi Saitoh and Coll. at Kobe University in Japan (152–157). The introduction of trypsin and protease inhibitors during pancreas preservation by doctor Kuroda and Coll. in 1988 and other groups158–162. The introducetion of a controlled pancreatic distension to increase the reproducibility of islet isolation techniques by doctors Jonathan R. Lakey, Ray V. Rajotte and Coll. in Edmonton163. The recent evaluation of extra-hepatic transplantation sites for islet cells, including intramuscularly164 and subcutaneous space165 by doctors Keith Reemtsma, Collin J. Wever, Mark A. Hardy and Coll. at Columbia University in the late 1970’s, unfortunately without function, followed more recently by better results reported with the intramuscular site by doctor Ehab Rafael and Coll. at the Karolinska Institute166 and by doctor Sabrina Dardenne and Coll. at the University of North France in Lille167; as well as new pilot experiments with an intra-bone marrow site by doctor Piemonti and Coll. in Milan98, 168, and the use of intra-peritoneal site mainly for initial clinical attempts to transplant encapsulated porcine or human islets to confer immunoprotection by doctors Robert B. Elliot, Christina Buchanan and Coll. at the University of Auckland in New Zealand169, and by doctors Giuseppe Basta, Giovanni Luca, Riccardo Calafiore and Coll. at the University of Perugia in Italy170,171, amongst others. The use of noninvasive imaging techniques to detect islet grafts using paramagnetic beads for magnetic resonance imaging in experimental animals by doctor Frantisek Saudek and Coll. in Prague172,173 and in the clinical settings by doctors Christian Toso, Thierry Berney and Coll. in Geneva174, and the use of positron emission tomography by doctors Olof Eriksson, Torbjorn Lundgren and Coll. in Sweden175. The use of supplemental islet infusion and or the use of exenatide in patients developing graft dysfunction by the Miami group148,176,177. The introduction of novel approaches to seal the tract of trans-hepatic catheterization of the portal vein to reduce the risk of hemorrhage and improve safety of the islet transplant procedure by doctors Tatiana Froud, Ricordi, Alejandro and Coll. at the University of Miami178. The introduction of exenatide treatment for islet transplant recipients to favor engraftment by the University of Illinois at Chicago and the Miami groups179,180. The use of living-related segmental pancreas donor by doctor Shinichi Matsumoto and Coll. at Kyoto University107,108. The introduction of Campath-1H as lympho-depleting agent by doctor Tan and Coll. at Xiamen University111, the University of Miami132 and the University of Alberta99,181.
The field of islet transplantation has significantly evolved since the initial attempts by doctors Minkowski and von Mering in 1882, with remarkable acceleration over the last three decades thanks to the incredible effort of the research community across the Worlds yielding to the achievement of steady improvements in the cell processing and transplantation techniques, patient management and immunotherapy protocols utilized (Figure 3). Preservation of beta-cell function is reproducibly currently attained in recipients of islet autografts, a therapeutic option that should be considered for individuals undergoing total pancreatectomy for non-malignant conditions and as recently reported also for malignant condition182. Restoration of beta-cell function can be obtained by transplantation of allogeneic islets in both nonuremic (ITA) and uremic (SIK and IAK) subjects with diabetes, allowing for long-term sustained function and associating with improved metabolic control even when required exogenous insulin (i.e., suboptimal islet mass transplanted or development of graft dysfunction). The introduction of Ricordi’s Automated Method twenty-five years ago has definitely given a remarkable impulse to the field, contributing to the expansion of the number of transplants performed worldwide since the early 1990’s. Islet transplantation has been approved as a reimbursable procedure in several Countries, including Australia, Canada (selected provinces), France, Italy, Switzerland, the National Institute for Health and Clinical Excellence in the United Kingdom, Sweden and the Nordic Network. In the U.S.A., autologous islet transplantation is currently reimbursed. The completion of registration trials by the Clinical Islet Transplant consortium (CIT-06 and CIT-07) will likely lead to biological licensure by the U.S. Food and Drug Administration shortly. This is an important step, as islet transplant activity in the United States has been severely restricted by limited access to research funds, with the exception of a joint Medicaid/Medicare initiative that is currently supporting the islet-after-kidney trial (CIT-06).
Figure 3.
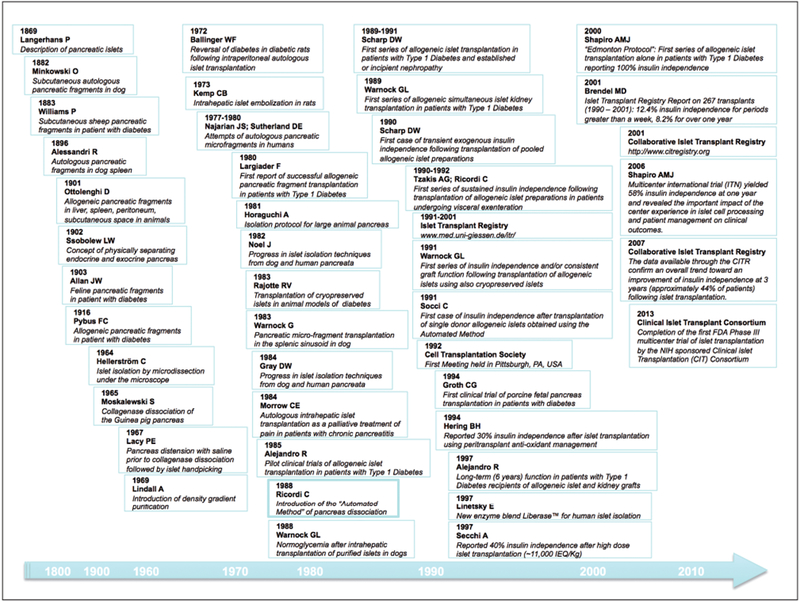
Timeline of pancreatic islet transplantation.
We are currently experiencing an exciting stage of innovation and renewed promise for cellular-based therapies to restore beta-cell function. Novel extra-hepatic transplant sites and tissue engineering approaches are being explored which may allow for improved engraftment and sustained function with cadaveric human, xenogeneic or stem-cell derived islet cells in the near future. It has been and still is an exceptional journey!
Acknowledgements
Dr. Piemonti has been supported by grants from the Italian Minister of Health (Ricerca Finalizzata RF-2009-1469691, Ricerca Finalizzata RF041234), Ministry of Education, University and Research (PRIN 2008, prot. 2008AFA7LC), EU (HEALTHF5-2009-241883-BetaCellTherapy; DIAPREPP Project, HEALTH-F2-2008-202013), Associazione Italiana per la Ricerca sul Cancro (AIRC, bando 5 × 1,000 N_12182 and Progetto IGN_11783), Telethon Italy and the Juvenile Diabetes Research Foundation (JT01Y01 and grant 6-2006-1098), EFSD/JDRF/Novo Nordisk Type 1 Diabetes Research Programme, and CARIPLO Foundation. Dr. Pileggi has been supported by grants from the National Institutes of Health (5U19AI050864-10, U01DK089538, 5U42RR016603-08S1, 1DP2DK083096-01, 1R01EB008009-02, 5R01DK059993-06, 1 R21 DK076098-01, 1 U01 DK70460-02, 5R01DK25802-24, 5R01DK56953-05), the Juvenile Diabetes Research Foundation International (17-2010-5, 4-2008-811, 6-39017G1, 4-2004-361, 4-2000-947), The Leona M. and Harry B. Helmsley Charitable Trust, the University of Miami Interdisciplinary Research Development Initiative, the American Diabetes Association (7-13-IN-32), the Diabetes Research Institute Foundation, and Converge Biotech. The funders had no role in the content, presentation, decision to publish, or preparation of the manuscript. A.P. is a co-founder, member of the scientific advisory board, and stock option holder of Converge Biotech and NEVA Pharmaceuticals. He has no conflict of interests to disclose regarding the content of this manuscript.
References
- 1.Langerhans P Beiträge zur mikroskopischen Anatomie der Bauchspeicheldrüse. Berlin: Gustav Lange; 1869. [Google Scholar]
- 2.Laguesse E Dur la formation dels îlots de Langerhans dans le pancréas. Compt Reud de la Soc Biol. 1893;45(9):819–820. [Google Scholar]
- 3.Minkowski O Weitere mittheilungen über den Diabetes mellitus nach exstirpation des pankreas. Berl Klin Wochenschr. 1892;29:90–94. [Google Scholar]
- 4.Williams P Notes on diabetes treated with extract and by grafts of sheep’s pancreas. Br Med J. 1894;2:1303–1304. [Google Scholar]
- 5.Alessandri R Innesti di tessuti viventi adulti ed embrionali in alcuni organi del corpo. Policlinico. 1896;III-C:253–271. [Google Scholar]
- 6.Kyrle K Über die Degenerationsvorgange im tierischen Pankreas. Arch f mikr Anat u Entwcklugsgesch. 1908;72:141. [Google Scholar]
- 7.Ottolenghi D Sur la transplantation du pancreas. Arch Ital Biol. 1901;36:447. [Google Scholar]
- 8.Pratt J, Murphy FT. Pancreatic transplantation in the spleen. J Exp Med. 1913;17:252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Allan JW. Transplantation of pancreas in diabetes. Br Med J. 1903;1(2204):764. [Google Scholar]
- 10.Pybus FC. Notes on suprarenal and pancreatic grafting. Lancet. 1924;204(5272):550–551. [Google Scholar]
- 11.Browing H, Resnik P. Homologus and heterologus transplantation of pancreatic tissue in normal and diabetic mice. Yale J Biol Med. 1951;24:141. [PMC free article] [PubMed] [Google Scholar]
- 12.Coupland RE. The survival and growth of pancreatic tissue in the anterior chamber of the eye of the albino rat. J Endocrinol. 1960;20:69–77. [DOI] [PubMed] [Google Scholar]
- 13.House EL, Burton C, Cooper H, Anderson E. The implantation of neonatal pancreas into the cheek pouch of the alloxan diabetic hamster. Endocrinology. 1958;63:389–91. [DOI] [PubMed] [Google Scholar]
- 14.Ssobolew LW. Zur normalen und pathologischen morphologie der inneren secretion der bauchspeicheldrüse. Die eseutung der langerhansschen inseln. Virchows Arch. 1902;168:91. [Google Scholar]
- 15.Hellerstroem C A method for the microdissection of intact pancreatic islets of mammals. Acta Endocrinol. 1964;45:122–32. [PubMed] [Google Scholar]
- 16.Isolation Moskalewski S. and culture of the islets of Langerhans of the Guinea pig. Gen Comp Endocrinol. 1965;44:342–53. [DOI] [PubMed] [Google Scholar]
- 17.Lacy PE, Mery Kostianovsky M. Method for the isolation of intact islets of Langerhans from the rat pancreas. Diabetes. 1967;16(1):35–39. [DOI] [PubMed] [Google Scholar]
- 18.Lindall A, Steffes M, Sorenson R. Immunoassayable insulin content of subcellular fractions of rat islets. Endocrinology. 1969;85(2):218–23. [DOI] [PubMed] [Google Scholar]
- 19.Ballinger WF, Lacy PE. Transplantation of intact pancreatic islets in rats. Surgery. 1972;72(2):175–86. [PubMed] [Google Scholar]
- 20.Kemp CB, Knight MJ, Scharp DW, Ballinger WF, Lacy PE. Effect of transplantation site on the results of pancreatic islet isografts in diabetic rats. Diabetologia. 1973;9(6):486–91. [DOI] [PubMed] [Google Scholar]
- 21.Lorenz D, Lippert H, Panzig E, Kohler H, Koch G, Tietz W, et al. Transplantation of isolated islets of Langerhans in diabetic dogs. III. Donor selection by mixed lymphocyte reaction and immunosuppressive treatment. J Surg Res. 1979;27(3):205–13. [DOI] [PubMed] [Google Scholar]
- 22.Kolb E, Ruckert R, Largiader F. Intraportal and intrasplenic autotransplantation of pancreatic islets in the dog. Eur Surg Res. 1977;9(6):419–26. [DOI] [PubMed] [Google Scholar]
- 23.Kretschmer GJ, Sutherland DE, Matas AJ, Steffes MW, Najarian JS. The dispersed pancreas: transplantation without islet purification in totally pancreatectomized dogs. Diabetologia. 1977;13(5):495–502. [DOI] [PubMed] [Google Scholar]
- 24.Horaguchi A, Merrell RC. Preparation of viable islet cells from dogs by a new method. Diabetes. 1981;30(5):455–8. [DOI] [PubMed] [Google Scholar]
- 25.Warnock GL, Rajotte RV, Procyshyn AW. Normoglycemia after reflux of islet-containing pancreatic fragments into the splenic vascular bed in dogs. Diabetes. 1983;32(5):452–9. [DOI] [PubMed] [Google Scholar]
- 26.Warnock GL, Rajotte RV, Kneteman NM, Ellis D, Toth K. Oral glucose tolerance and response to mixed meals in dogs bearing long-term transplanted islets of Langerhans. Transplant Proc. 1987;19(1 Pt 2):969–73. [PubMed] [Google Scholar]
- 27.Rajotte RV, Warnock GL, Bruch LC, Procyshyn AW. Transplantation of cryopreserved and fresh rat islets and canine pancreatic fragments: comparison of cryopreservation protocols. Cryobiology. 1983;20(2):169–84. [DOI] [PubMed] [Google Scholar]
- 28.Najarian JS, Sutherland DE, Matas AJ, Steffes MW, Simmons RL, Goetz FC. Human islet transplantation: a preliminary report. Transplant Proc. 1977;9(1):233–6. [PubMed] [Google Scholar]
- 29.Sutherland DE, Matas AJ, Goetz FC, Najarian JS. Transplantation of dispersed pancreatic islet tissue in humans: autografts and allografts. Diabetes. 1980;29 Suppl 1:31–44. [DOI] [PubMed] [Google Scholar]
- 30.Largiader F, Kolb E, Binswanger U. A long-term functioning human pancreatic islet allotransplant. Transplantation. 1980;29(1):76–7. [DOI] [PubMed] [Google Scholar]
- 31.Largiader F, Kolb E, Binswanger U, Illig R. [Successful allotransplantation of an island of Langerhans]. Schweizerische medizinische Wochenschrift. 1979;109(45):1733–6. [PubMed] [Google Scholar]
- 32.Morrow CE, Cohen JI, Sutherland DE, Najarian JS. Chronic pancreatitis: long-term surgical results of pancreatic duct drainage, pancreatic resection, and near-total pancreatectomy and islet autotransplantation. Surgery. 1984;96(4):608–16. [PubMed] [Google Scholar]
- 33.Bellin MD, Balamurugan AN, Pruett TL, Sutherland DE. No islets left behind: islet autotransplantation for surgery-induced diabetes. Curr Diab Rep. 2012;12(5):580–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Noel J, Rabinovitch A, Olson L, Kyriakides G, Miller J, Mintz DH. A method for large-scale, high-yield isolation of canine pancreatic islets of Langerhans. Metabolism. 1982;31(2):184–7. [DOI] [PubMed] [Google Scholar]
- 35.Gray DW, McShane P, Grant A, Morris PJ. A method for isolation of islets of Langerhans from the human pancreas. Diabetes. 1984;33(11):1055–61. [DOI] [PubMed] [Google Scholar]
- 36.Alejandro R, Mintz DH, Noel J, Latif Z, Koh N, Russell E, et al. Islet cell transplantation in type I diabetes mellitus. Transplant Proc. 1987;19(1 Pt 3):2359–61. [PubMed] [Google Scholar]
- 37.Alejandro R, Cutfield R, Shienvold FL, Latif Z, Mintz DH. Successful long-term survival of pancreatic islet allografts in spontaneous or pancreatectomy-induced diabetes in dogs. Cyclosporine-induced immune unresponsiveness. Diabetes. 1985;34(8):825–8. [DOI] [PubMed] [Google Scholar]
- 38.Alejandro R, Cutfield RG, Shienvold FL, Polonsky KS, Noel J, Olson L, et al. Natural history of intrahepatic canine islet cell autografts. J Clin Investig. 1986;78(5):1339–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Alejandro R, Latif Z, Polonsky KS, Shienvold FL, Civantos F, Mint DH. Natural history of multiple intrahepatic canine islet allografts during and following administration of cyclosporine. Transplantation. 1988;45(6):1036–44. [DOI] [PubMed] [Google Scholar]
- 40.Alejandro R, Lehmann R, Ricordi C, Kenyon NS, Angelico MC, Burke G, et al. Long-term function (6 years) of islet allografts in type 1 diabetes. Diabetes. 1997;46(12):1983–9. [DOI] [PubMed] [Google Scholar]
- 41.Warnock GL, Cattral MS, Rajotte RV. Normoglycemia after implantation of purified islet cells in dogs. Can J Surgery. 1988;31(6):421–6. [PubMed] [Google Scholar]
- 42.Cattral MS, Warnock GL, Kneteman NM, Rajotte RV. Transplantation of purified single-donor canine islet allografts with cyclosporine. Transplantation. 1989;47(4): 583–7. [DOI] [PubMed] [Google Scholar]
- 43.Ricordi C, Lacy PE, Finke EH, Olack BJ, Scharp DW. Automated method for isolation of human pancreatic islets. Diabetes. 1988;37(4):413–20. [DOI] [PubMed] [Google Scholar]
- 44.Ricordi C Islet transplantation: a brave new world. Diabetes. 2003;52(7):1595–603. [DOI] [PubMed] [Google Scholar]
- 45.Ricordi C, Socci C, Davalli AM, Staudacher C, Baro P, Vertova A, et al. Isolation of the elusive pig islet. Surgery. 1990;107(6):688–94. [PubMed] [Google Scholar]
- 46.Vizzardelli C, Potter ED, Berney T, Pileggi A, Inverardi L, Ricordi C, et al. Automated method for isolation of adrenal medullary chromaffin cells from neonatal porcine glands. Cell Transplant. 2001;10(8):689–96. [PubMed] [Google Scholar]
- 47.Scharp D, Lacy P, Ricordi C, Boyle P, Santiago J, Cryer P, et al. Human islet transplantation in patients with type I diabetes. Transplant Proc. 1989;21(1 Pt 3):2744–5. [PubMed] [Google Scholar]
- 48.Scharp DW, Lacy PE, Santiago JV, McCullough CS, Weide LG, Falqui L, et al. Insulin independence after islet transplantation into type I diabetic patient. Diabetes. 1990;39(4):515–8. [DOI] [PubMed] [Google Scholar]
- 49.Scharp DW, Lacy PE, Santiago JV, McCullough CS, Weide LG, Boyle PJ, et al. Results of our first nine intraportal islet allografts in type 1, insulin-dependent diabetic patients. Transplantation. 1991;51(1):76–85. [DOI] [PubMed] [Google Scholar]
- 50.Warnock GL, Kneteman NM, Ryan EA, Evans MG, Seelis RE, Halloran PF, et al. Continued function of pancreatic islets after transplantation in type I diabetes. Lancet. 1989;2(8662):570–2. [DOI] [PubMed] [Google Scholar]
- 51.Lake SP, Bassett PD, Larkins A, Revell J, Walczak K, Chamberlain J, et al. Large-scale purification of human islets utilizing discontinuous albumin gradient on IBM 2991 cell separator. Diabetes. 1989;38 Suppl 1:143–5. [DOI] [PubMed] [Google Scholar]
- 52.Alejandro R, Strasser S, Zucker PF, Mintz DH. Isolation of pancreatic islets from dogs. Semiautomated purification on albumin gradients. Transplantation. 1990;50(2):207–10. [DOI] [PubMed] [Google Scholar]
- 53.Olack B, Swanson C, McLear M, Longwith J, Scharp D, Lacy PE. Islet purification using Euro-Ficoll gradients. Transplant Proc. 1991;23(1 Pt 1):774–6. [PubMed] [Google Scholar]
- 54.Latif ZA, Noel J, Alejandro R. A simple method of staining fresh and cultured islets. Transplantation. 1988;45(4): 827–30. [PubMed] [Google Scholar]
- 55.Ricordi C, Gray DW, Hering BJ, Kaufman DB, Warnock GL, Kneteman NM, et al. Islet isolation assessment in man and large animals. Acta Diabetol Lat. 1990;27(3):185–95. [DOI] [PubMed] [Google Scholar]
- 56.Tzakis AG, Ricordi C, Alejandro R, Zeng Y, Fung JJ, Todo S, et al. Pancreatic islet transplantation after upper abdominal exenteration and liver replacement. Lancet. 1990;336(8712):402–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ricordi C, Tzakis AG, Carroll PB, Zeng YJ, Rilo HL, Alejandro R, et al. Human islet isolation and allotransplantation in 22 consecutive cases. Transplantation. 1992;53(2):407–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Baidal DA, Froud T, Ferreira JV, Khan A, Alejandro R, Ricordi C. The bag method for islet cell infusion. Cell transplant. 2003;12(7):809–13. [DOI] [PubMed] [Google Scholar]
- 59.Socci C, Falqui L, Davalli AM, Ricordi C, Braghi S, Bertuzzi F, et al. Fresh human islet transplantation to replace pancreatic endocrine function in type 1 diabetic patients. Report of six cases. Acta diabetologica. 1991;28(2): 151–7. [DOI] [PubMed] [Google Scholar]
- 60.Warnock GL, Kneteman NM, Ryan E, Seelis RE, Rabinovitch A, Rajotte RV. Normoglycaemia after transplantation of freshly isolated and cryopreserved pancreatic islets in type 1 (insulin-dependent) diabetes mellitus. Diabetologia. 1991;34(1):55–8. [DOI] [PubMed] [Google Scholar]
- 61.Hering BJ, Bretzel RG, Hopt UT, Brandhorst H, Brandhorst D, Bollen CC, et al. New protocol toward prevention of early human islet allograft failure. Transplant Proc. 1994;26(2):570–1. [PubMed] [Google Scholar]
- 62.Secchi A, Socci C, Maffi P, Taglietti MV, Falqui L, Bertuzzi F, et al. Islet transplantation in IDDM patients. Diabetologia. 1997;40(2):225–31. [DOI] [PubMed] [Google Scholar]
- 63.Pileggi A, Ricordi C, Kenyon NS, Froud T, Baidal DA, Kahn A, et al. Twenty years of clinical islet transplantation at the Diabetes Research Institute—University of Miami. Clinical transplants. 2004:177–204. [PubMed] [Google Scholar]
- 64.Fetterhoff TJ, Cavanagh TJ, Wile KJ, Wright MJ, Dwulet FE, Gill J, et al. Human pancreatic dissociation using a purified enzyme blend. Transplant Proc. 1995;27(6):3282–3. [PubMed] [Google Scholar]
- 65.Cavanagh TJ, Lakey JR, Dwulet F, Wright MJ, Wile K, Albertson T, et al. Improved pig islet yield and post-culture recovery using Liberase PI purified enzyme blend. Transplant Proc. 1998;30(2):367. [DOI] [PubMed] [Google Scholar]
- 66.Berney T, Molano RD, Cattan P, Pileggi A, Vizzardelli C, Oliver R, Ricordi C, Inverardi L. Endotoxin-mediated delayed islet graft function is associated with increased intra-islet cytokine production and islet cell apoptosis. Transplantation. 2001;71(1):125–32. [DOI] [PubMed] [Google Scholar]
- 67.Vargas F, Vives-Pi M, Somoza N, Armengol P, Alcalde L, Marti M, et al. Endotoxin contamination may be responsible for the unexplained failure of human pancreatic islet transplantation. Transplantation. 1998;65(5):722–7. [DOI] [PubMed] [Google Scholar]
- 68.Linetsky E, Bottino R, Lehmann R, Alejandro R, Inverardi L, Ricordi C. Improved human islet isolation using a new enzyme blend, liberase. Diabetes. 1997;46(7):1120–3. [DOI] [PubMed] [Google Scholar]
- 69.Lakey JR, Cavanagh TJ, Zieger MA, Wright M. Evaluation of a purified enzyme blend for the recovery and function of canine pancreatic islets. Cell Transplant. 1998;7(4):365–72. [DOI] [PubMed] [Google Scholar]
- 70.Linetsky E, Selvaggi G, Bottino R, Kong SS, Qian T, Alejandro R, et al. Comparison of collagenase type P and Liberase during human islet isolation using the automated method. Transplant Proc. 1995;27(6):3264. [PubMed] [Google Scholar]
- 71.Groth CG, Korsgren O, Tibell A, Tollemar J, Moller E, Bolinder J, et al. Transplantation of porcine fetal pancreas to diabetic patients. Lancet. 1994;344(8934):1402–4. [DOI] [PubMed] [Google Scholar]
- 72.Heneine W, Tibell A, Switzer WM, Sandstrom P, Rosales GV, Mathews A, et al. No evidence of infection with porcine endogenous retrovirus in recipients of porcine islet-cell xenografts. Lancet. 1998;352(9129):695–9. [DOI] [PubMed] [Google Scholar]
- 73.Brendel MD, Hering BJ, Schultz AO, Bretzel RG. International Islet Transplant Registry. Giessen, Germany: 2001. 18 April, 2013. Report No.: Contract No.: 1. [Google Scholar]
- 74.Shapiro AM, Lakey JR, Ryan EA, Korbutt GS, Toth E, Warnock GL, et al. Islet transplantation in seven patients with type 1 diabetes mellitus using a glucocorticoid-free immunosuppressive regimen. New Engl J Med. 2000;343(4):230–8. [DOI] [PubMed] [Google Scholar]
- 75.Shapiro AM, Ricordi C, Hering B. Edmonton’s islet success has indeed been replicated elsewhere. Lancet. 2003;362(9391):1242. [DOI] [PubMed] [Google Scholar]
- 76.Shapiro AM, Ricordi C, Hering BJ, Auchincloss H, Lindblad R, Robertson RP, et al. International trial of the Edmonton protocol for islet transplantation. New Engl J Med. 2006;355(13):1318–30. [DOI] [PubMed] [Google Scholar]
- 77.Ryan EA, Lakey JR, Rajotte RV, Korbutt GS, Kin T, Imes S, et al. Clinical outcomes and insulin secretion after islet transplantation with the Edmonton protocol. Diabetes. 2001;50(4):710–9. [DOI] [PubMed] [Google Scholar]
- 78.Ryan EA, Lakey JR, Paty BW, Imes S, Korbutt GS, Kneteman NM, et al. Successful islet transplantation: continued insulin reserve provides long-term glycemic control. Diabetes. 2002;51(7):2148–57. [DOI] [PubMed] [Google Scholar]
- 79.Markmann JF, Deng S, Huang X, Desai NM, Velidedeoglu EH, Lui C, et al. Insulin independence following isolated islet transplantation and single islet infusions. Ann Surg. 2003;237(6):741–9; discussion 9–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Ryan EA, Shandro T, Green K, Paty BW, Senior PA, Bigam D, et al. Assessment of the severity of hypoglycemia and glycemic lability in type 1 diabetic subjects undergoing islet transplantation. Diabetes. 2004;53(4):955–62. [DOI] [PubMed] [Google Scholar]
- 81.Frank A, Deng S, Huang X, Velidedeoglu E, Bae YS, Liu C, et al. Transplantation for type I diabetes: comparison of vascularized whole-organ pancreas with isolated pancreatic islets. Ann Surg. 2004;240(4):631–40; discussion 40–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Geiger MC, Ferreira JV, Hafiz MM, Froud T, Baidal DA, Meneghini LF, et al. Evaluation of metabolic control using a continuous subcutaneous glucose monitoring system in patients with type 1 diabetes mellitus who achieved insulin independence after islet cell transplantation. Cell Transplant. 2005;14(2–3):77–84. [DOI] [PubMed] [Google Scholar]
- 83.Rickels MR, Schutta MH, Mueller R, Markmann JF, Barker CF, Naji A, et al. Islet cell hormonal responses to hypoglycemia after human islet transplantation for type 1 diabetes. Diabetes. 2005;54(11):3205–11. [DOI] [PubMed] [Google Scholar]
- 84.Poggioli R, Faradji RN, Ponte G, Betancourt A, Messinger S, Baidal DA, et al. Quality of life after islet transplantation. Am J Transplant 2006;6(2):371–8. [DOI] [PubMed] [Google Scholar]
- 85.Paty BW, Senior PA, Lakey JR, Shapiro AM, Ryan EA. Assessment of glycemic control after islet transplantation using the continuous glucose monitor in insulin-independent versus insulin-requiring type 1 diabetes subjects. Diabetes Technol Ther. 2006;8(2):165–73. [DOI] [PubMed] [Google Scholar]
- 86.O’Connell PJ, Hawthorne WJ, Holmes-Walker DJ, Nankivell BJ, Gunton JE, Patel AT, et al. Clinical islet transplantation in type 1 diabetes mellitus: results of Australia’s first trial. Med J Aust. 2006;184(5):221–5. [DOI] [PubMed] [Google Scholar]
- 87.Rickels MR, Schutta MH, Mueller R, Kapoor S, Markmann JF, Naji A, Teff KL. Glycemic thresholds for activation of counterregulatory hormone and symptom responses in islet transplant recipients. J Clin Endocrinol Metab. 2007;92(3):873–9. [DOI] [PubMed] [Google Scholar]
- 88.Cure P, Pileggi A, Froud T, Messinger S, Faradji RN, Baidal DA, et al. Improved metabolic control and quality of life in seven patients with type 1 diabetes following islet after kidney transplantation. Transplantation. 2008;85(6):801–12. [DOI] [PubMed] [Google Scholar]
- 89.Benhamou PY, Milliat-Guittard L, Wojtusciszyn A, Kessler L, Toso C, Baertschiger R, et al. Quality of life after islet transplantation: data from the GRAGIL 1 and 2 trials. Diabet Med. 2009;26(6):617–21. [DOI] [PubMed] [Google Scholar]
- 90.Vantyghem MC, Balavoine AS, Caiazzo R, Kerr-Conte J, Noel C, Pattou F. Diabetes cell therapy: a decade later. Minerva Endocrinol. 2011;36(1):23–39. [PubMed] [Google Scholar]
- 91.Vantyghem MC, Raverdy V, Balavoine AS, Defrance F, Caiazzo R, Arnalsteen L, et al. Continuous glucose monitoring after islet transplantation in type 1 diabetes: an excellent graft function (beta-score greater than 7) Is required to abrogate hyperglycemia, whereas a minimal function is necessary to suppress severe hypoglycemia (beta-score greater than 3). J Clin Endocrinol Metab. 2012;97(11):E2078–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Walsh RM, Saavedra JR, Lentz G, Guerron AD, Scheman J, Stevens T, et al. Improved quality of life following total pancreatectomy and auto-islet transplantation for chronic pancreatitis. J Gastrointest Surg. 2012;16(8):1469–77. [DOI] [PubMed] [Google Scholar]
- 93.Hirsch D, Odorico J, Danobeitia JS, Alejandro R, Rickels MR, Hanson M, et al. Early metabolic markers that anticipate loss of insulin independence in type 1 diabetic islet allograft recipients. Am J Transplant. 2012;12(5):1275–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Ryan EA, Paty BW, Senior PA, Bigam D, Alfadhli E, Kneteman NM, et al. Five-year follow-up after clinical islet transplantation. Diabetes. 2005;54(7):2060–9. [DOI] [PubMed] [Google Scholar]
- 95.Mineo D, Pileggi A, Alejandro R, Ricordi C. Point: steady progress and current challenges in clinical islet transplantation. Diabetes Care. 2009;32(8):1563–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Vantyghem MC, Kerr-Conte J, Arnalsteen L, Sergent G, Defrance F, Gmyr V, et al. Primary graft function, metabolic control, and graft survival after islet transplantation. Diabetes Care. 2009;32(8):1473–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Bellin MD, Kandaswamy R, Parkey J, Zhang HJ, Liu B, Ihm SH, et al. Prolonged insulin independence after islet allotransplants in recipients with type 1 diabetes. Am J Transplant. 2008;8(11):2463–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Maffi P, Scavini M, Socci C, Piemonti L, Caldara R, Gremizzi C, et al. Risks and benefits of transplantation in the cure of type 1 diabetes: whole pancreas versus islet transplantation. A single center study. Rev Diabet Stud. 2011;8(1):44–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Shapiro AMJ, Toso C, Imes S, Koh A, Kin T, O’Gorman D, et al. Five-year results of islet-alone transplantation match pancreas-alone transplantation with alemtuzumab, Tac/MMF, with strong suppression of auto and alloreactivity. Rev Diabet Stud. 2011;8(1):95. [Google Scholar]
- 100.Registry CIT. Seventh Annual Report. Collaborative Islet Transplant Registry, 2011. December 30, 2011. Report No. [Google Scholar]
- 101.Alejandro R, Barton FB, Hering BJ, Wease S. 2008 Update from the Collaborative Islet Transplant Registry. Transplantation. 2008;86(12):1783–8. [DOI] [PubMed] [Google Scholar]
- 102.2007 update on allogeneic islet transplantation from the Collaborative Islet Transplant Registry (CITR). Cell Transplant. 2009;18(7):753–67. [DOI] [PubMed] [Google Scholar]
- 103.Barton FB, Rickels MR, Alejandro R, Hering BJ, Wease S, Naziruddin B, et al. Improvement in outcomes of clinical islet transplantation: 1999–2010. Diabetes care. 2012;35(7):1436–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Bellin MD, Barton FB, Heitman A, Harmon JV, Kandaswamy R, Balamurugan AN, et al. Potent induction immunotherapy promotes long-term insulin independence after islet transplantation in type 1 diabetes. Am J Transplant. 2012;12(6):1576–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Naziruddin B, Wease S, Stablein D, Barton FB, Berney T, Rickels MR, et al. HLA class I sensitization in islet transplant recipients: report from the Collaborative Islet Transplant Registry. Cell Transplant. 2012;21(5):901–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Saudek F, Girman P, Kriz J, Berkova Z, Zacharovova K, Koblas T, et al. [Islet transplantation for treatment of type-1 diabetes mellitus]. Cas Lek Cesk. 2011;150(1):49–55. [PubMed] [Google Scholar]
- 107.Matsumoto S, Okitsu T, Iwanaga Y, Noguchi H, Nagata H, Yonekawa Y, et al. Insulin independence after living-donor distal pancreatectomy and islet allotransplantation. Lancet. 2005;365(9471):1642–4. [DOI] [PubMed] [Google Scholar]
- 108.Matsumoto S, Okitsu T, Iwanaga Y, Noguchi H, Nagata H, Yonekawa Y, et al. Follow-up study of the first successful living donor islet transplantation. Transplantation. 2006;82(12):1629–33. [DOI] [PubMed] [Google Scholar]
- 109.Argibay P, Hyon S, Groppa R, Barbich M, Grossembacher L, Giudice C, et al. Initial experience with clinical islet transplantation in Argentina. Transplant Proc. 1998;30(2):308. [DOI] [PubMed] [Google Scholar]
- 110.Eliaschewitz FG, Aita CA, Genzini T, Noronha IL, Lojudice FH, Labriola L, et al. First Brazilian pancreatic islet transplantation in a patient with type 1 diabetes mellitus. Transplant Proc. 2004;36(4):1117–8. [DOI] [PubMed] [Google Scholar]
- 111.Tan J, Yang S, Cai J, Guo J, Huang L, Wu Z, et al. Simultaneous islet and kidney transplantation in seven patients with type 1 diabetes and end-stage renal disease using a glucocorticoid-free immunosuppressive regimen with alemtuzumab induction. Diabetes. 2008;57(10): 2666–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Oberholzer J, Triponez F, Mage R, Andereggen E, Buhler L, Cretin N, et al. Human islet transplantation: lessons from 13 autologous and 13 allogeneic transplantations. Transplantation. 2000;69(6):1115–23. [DOI] [PubMed] [Google Scholar]
- 113.Kempf MC, Andres A, Morel P, Benhamou PY, Bayle F, Kessler L, et al. Logistics and transplant coordination activity in the GRAGIL Swiss-French multicenter network of islet transplantation. Transplantation. 2005;79(9):1200–5. [DOI] [PubMed] [Google Scholar]
- 114.Badet L, Benhamou PY, Wojtusciszyn A, Baertschiger R, Milliat-Guittard L, Kessler L, et al. Expectations and strategies regarding islet transplantation: metabolic data from the GRAGIL 2 trial. Transplantation. 2007;84(1):89–96. [DOI] [PubMed] [Google Scholar]
- 115.Borot S, Niclauss N, Wojtusciszyn A, Brault C, Demuylder-Mischler S, Muller Y, et al. Impact of the number of infusions on 2-year results of islet-after-kidney transplantation in the GRAGIL network. Transplantation. 2011;92(9):1031–8. [DOI] [PubMed] [Google Scholar]
- 116.Goss JA, Schock AP, Brunicardi FC, Goodpastor SE, Garber AJ, Soltes G, et al. Achievement of insulin independence in three consecutive type-1 diabetic patients via pancreatic islet transplantation using islets isolated at a remote islet isolation center. Transplantation. 2002;74(12):1761–6. [DOI] [PubMed] [Google Scholar]
- 117.Goss JA, Goodpastor SE, Brunicardi FC, Barth MH, Soltes GD, Garber AJ, et al. Development of a human pancreatic islet-transplant program through a collaborative relationship with a remote islet-isolation center. Transplantation. 2004;77(3):462–6. [DOI] [PubMed] [Google Scholar]
- 118.Lee TC, Barshes NR, Brunicardi FC, Alejandro R, Ricordi C, Nguyen L, et al. Procurement of the human pancreas for pancreatic islet transplantation. Transplantation. 2004;78(3):481–3. [DOI] [PubMed] [Google Scholar]
- 119.Ponte GM, Pileggi A, Messinger S, Alejandro A, Ichii H, Baidal DA, et al. Toward maximizing the success rates of human islet isolation: influence of donor and isolation factors. Cell Transplant. 2007;16(6):595–607. [DOI] [PubMed] [Google Scholar]
- 120.Ichii H, Sakuma Y, Pileggi A, Fraker C, Alvarez A, Montelongo J, et al. Shipment of human islets for transplantation. Am J Transplant. 2007;7(4):1010–20. [DOI] [PubMed] [Google Scholar]
- 121.Khan A, Jindal RM, Shriver C, Guy SR, Vertrees AE, Wang X, et al. Remote processing of pancreas can restore normal glucose homeostasis in autologous islet transplantation after traumatic whipple pancreatectomy: technical considerations. Cell Transplant. 2012;21(6):1261–7. [DOI] [PubMed] [Google Scholar]
- 122.Jindal RM, Ricordi C, Shriver CD. Autologous pancreatic islet transplantation for severe trauma. New Engl J Med. 2010;362(16):1550. [DOI] [PubMed] [Google Scholar]
- 123.Papas KK, Karatzas T, Berney T, Minor T, Pappas P, Pattou F, et al. International workshop: islet transplantation without borders enabling islet transplantation in Greece with international collaboration and innovative technology. Clin Transplant. 2013;27(2):E116–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.van der Burg MP, Gooszen HG, Ploeg RJ, Scherft JP, Field MJ, Guicherit OR, et al. Comparison of islet isolation techniques in dogs: over 90% purified islets using UW solution. Transplant Proc. 1990;22(2):795–6. [PubMed] [Google Scholar]
- 125.van der Burg MP, Gooszen HG, Ploeg RJ, Guicherit OR, Scherft JP, Terpstra JL, et al. Pancreatic islet isolation with UW solution: a new concept. Transplant Proc. 1990;22(4):2050–1. [PubMed] [Google Scholar]
- 126.van der Burg MP, Basir I, Bouwman E. No porcine islet loss during density gradient purification in a novel iodixanol in University of Wisconsin solution. Transplant Proc. 1998;30(2):362–3. [DOI] [PubMed] [Google Scholar]
- 127.Van der Burg MPM, Ranuncoli A, Molano R, Kirlew T, Ringers J, Bouwman E, et al. , editors. Efficacy of the novel iodixanol-UWS density gradient for human islet purification. 18th Workshop of the AIDSPIT Study Group; 1999 January 24–26, 1999; Igls, Austria. [Google Scholar]
- 128.Hering BJ, Kandaswamy R, Harmon JV, Ansite JD, Clemmings SM, Sakai T, et al. Transplantation of cultured islets from two-layer preserved pancreases in type 1 diabetes with anti-CD3 antibody. Am J Transplant. 2004;4(3):390–401. [DOI] [PubMed] [Google Scholar]
- 129.Hering BJ, Kandaswamy R, Ansite JD, Eckman PM, Nakano M, Sawada T, et al. Single-donor, marginal-dose islet transplantation in patients with type 1 diabetes. JAMA. 2005;293(7):830–5. [DOI] [PubMed] [Google Scholar]
- 130.Froud T, Ricordi C, Baidal DA, Hafiz MM, Ponte G, Cure P, et al. Islet transplantation in type 1 diabetes mellitus using cultured islets and steroid-free immunosuppression: Miami experience. Am J Transplant. 2005;5(8):2037–46. [DOI] [PubMed] [Google Scholar]
- 131.Mineo D, Ricordi C, Xu X, Pileggi A, Garcia-Morales R, Khan A, et al. Combined islet and hematopoietic stem cell allotransplantation: a clinical pilot trial to induce chimerism and graft tolerance. Am J Transplant. 2008;8(6):1262–74. [DOI] [PubMed] [Google Scholar]
- 132.Froud T, Baidal DA, Faradji R, Cure P, Mineo D, Selvaggi G, et al. Islet transplantation with alemtuzumab induction and calcineurin-free maintenance immunosuppression results in improved short- and long-term outcomes. Transplantation. 2008;86(12):1695–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Muller YD, Gupta S, Morel P, Borot S, Bettens F, Truchetet ME, et al. Transplanted human pancreatic islets after long-term insulin independence. Am J Transplant. 2013;13(4):1093–7. [DOI] [PubMed] [Google Scholar]
- 134.Paraskevas S, Aikin R, Maysinger D, Lakey JR, Cavanagh TJ, Hering B, et al. Activation and expression of ERK, JNK, and p38 MAP-kinases in isolated islets of Langerhans: implications for cultured islet survival. FEBS Lett. 1999;455(3):203–8. [DOI] [PubMed] [Google Scholar]
- 135.Abdelli S, Ansite J, Roduit R, Borsello T, Matsumoto I, Sawada T, et al. Intracellular stress signaling pathways activated during human islet preparation and following acute cytokine exposure. Diabetes. 2004;53(11):2815–23. [DOI] [PubMed] [Google Scholar]
- 136.Abdelli S, Abderrahmani A, Hering BJ, Beckmann JS, Bonny C. The c-Jun N-terminal kinase JNK participates in cytokine- and isolation stress-induced rat pancreatic islet apoptosis. Diabetologia. 2007;50(8):1660–9. [DOI] [PubMed] [Google Scholar]
- 137.Bottino R, Balamurugan AN, Tse H, Thirunavukkarasu C, Ge X, Profozich J, et al. Response of human islets to isolation stress and the effect of antioxidant treatment. Diabetes. 2004;53(10):2559–68. [DOI] [PubMed] [Google Scholar]
- 138.Fornoni A, Pileggi A, Molano RD, Sanabria NY, Tejada T, Gonzalez-Quintana J, et al. Inhibition of c-jun N terminal kinase (JNK) improves functional beta cell mass in human islets and leads to AKT and glycogen synthase kinase-3 (GSK-3) phosphorylation. Diabetologia. 2008;51(2):298–308. [DOI] [PubMed] [Google Scholar]
- 139.Pileggi A, Ribeiro MM, Hogan AR, Molano RD, Cobianchi L, Ichii H, et al. Impact of pancreatic cold preservation on rat islet recovery and function. Transplantation. 2009;87(10):1442–50. [DOI] [PubMed] [Google Scholar]
- 140.Moberg L, Johansson H, Lukinius A, Berne C, Foss A, Kallen R, et al. Production of tissue factor by pancreatic islet cells as a trigger of detrimental thrombotic reactions in clinical islet transplantation. Lancet. 2002;360(9350): 2039–45. [DOI] [PubMed] [Google Scholar]
- 141.Piemonti L, Leone BE, Nano R, Saccani A, Monti P, Maffi P, et al. Human pancreatic islets produce and secrete MCP-1/CCL2: relevance in human islet transplantation. Diabetes. 2002;51(1):55–65. [DOI] [PubMed] [Google Scholar]
- 142.Bertuzzi F, Marzorati S, Maffi P, Piemonti L, Melzi R, de Taddeo F, et al. Tissue factor and CCL2/monocyte chemoattractant protein-1 released by human islets affect islet engraftment in type 1 diabetic recipients. J Clin Endocrinol Metab. 2004;89(11):5724–8. [DOI] [PubMed] [Google Scholar]
- 143.Melzi R, Piemonti L, Nano R, Clissi B, Calori G, Antonioli B, et al. Donor and isolation variables associated with human islet monocyte chemoattractant protein-1 release. Transplantation. 2004;78(10):1564–7. [DOI] [PubMed] [Google Scholar]
- 144.Marzorati S, Antonioli B, Nano R, Maffi P, Piemonti L, Giliola C, et al. Culture medium modulates proinflammatory conditions of human pancreatic islets before transplantation. Am J Transplant. 2006;6(11):2791–5. [DOI] [PubMed] [Google Scholar]
- 145.Barbe-Tuana FM, Klein D, Ichii H, Berman DM, Coffey L, Kenyon NS, et al. CD40-CD40 ligand interaction activates proinflammatory pathways in pancreatic islets. Diabetes. 2006;55(9):2437–45. [DOI] [PubMed] [Google Scholar]
- 146.Farney AC, Xenos E, Sutherland DE, Widmer M, Stephanian E, Field MJ, et al. Inhibition of pancreatic islet beta cell function by tumor necrosis factor is blocked by a soluble tumor necrosis factor receptor. Transplant Proc. 1993;25(1 Pt 2):865–6. [PubMed] [Google Scholar]
- 147.Bottino R, Fernandez LA, Ricordi C, Lehmann R, Tsan MF, Oliver R, et al. Transplantation of allogeneic islets of Langerhans in the rat liver: effects of macrophage depletion on graft survival and microenvironment activation. Diabetes. 1998;47(3):316–23. [DOI] [PubMed] [Google Scholar]
- 148.Faradji RN, Tharavanij T, Messinger S, Froud T, Pileggi A, Monroy K, et al. Long-term insulin independence and improvement in insulin secretion after supplemental islet infusion under exenatide and etanercept. Transplantation. 2008;86(12):1658–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Takita M, Matsumoto S, Shimoda M, Chujo D, Itoh T, Sorelle JA, et al. Safety and tolerability of the T-cell depletion protocol coupled with anakinra and etanercept for clinical islet cell transplantation. Clin Transplant. 2012;26(5):E471–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Bennet W, Sundberg B, Groth CG, Brendel MD, Brandhorst D, Brandhorst H, et al. Incompatibility between human blood and isolated islets of Langerhans: a finding with implications for clinical intraportal islet transplantation? Diabetes. 1999;48(10):1907–14. [DOI] [PubMed] [Google Scholar]
- 151.Citro A, Cantarelli E, Maffi P, Nano R, Melzi R, Mercalli A, et al. CXCR1/2 inhibition enhances pancreatic islet survival after transplantation. J Clin Investig. 2012;122(10):3647–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Tanioka Y, Sutherland DE, Kuroda Y, Gilmore TR, Asaheim TC, Kronson JW, et al. Excellence of the two-layer method (University of Wisconsin solution/perfluorochemical) in pancreas preservation before islet isolation. Surgery. 1997;122(2):435–41; discussion 41–2. [DOI] [PubMed] [Google Scholar]
- 153.Kuroda Y, Kawamura T, Suzuki Y, Fujiwara H, Yamamoto K, Saitoh Y. A new, simple method for cold storage of the pancreas using perfluorochemical. Transplantation. 1988;46(3):457–60. [DOI] [PubMed] [Google Scholar]
- 154.Kawamura T, Kuroda Y, Suzuki Y, Fujiwara H, Fujino Y, Yamamoto K, et al. Seventy-two-hour preservation of the canine pancreas by the two-layer (Euro-Collins’ solution/perfluorochemical) cold storage method. Transplantation. 1989;47(5):776–8. [DOI] [PubMed] [Google Scholar]
- 155.Tsujimura T, Kuroda Y, Kin T, Avila JG, Rajotte RV, Korbutt GS, et al. Human islet transplantation from pancreases with prolonged cold ischemia using additional preservation by the two-layer (UW solution/perfluorochemical) coldstorage method. Transplantation. 2002;74(12):1687–91. [DOI] [PubMed] [Google Scholar]
- 156.Ricordi C, Fraker C, Szust J, Al-Abdullah I, Poggioli R, Kirlew T, et al. Improved human islet isolation outcome from marginal donors following addition of oxygenated perfluorocarbon to the cold-storage solution. Transplantation. 2003;75(9):1524–7. [DOI] [PubMed] [Google Scholar]
- 157.Ichii H, Wang X, Messinger S, Alvarez A, Fraker C, Khan A, et al. Improved human islet isolation using nicotinamide. Am J Transplant. 2006;6(9):2060–8. [DOI] [PubMed] [Google Scholar]
- 158.Kuroda Y, Suzuki Y, Kawamura T, Fujiwara H, Ashida T, Matsuo M, et al. Pancreatic secretory trypsin inhibitor as a marker for early detection of rejection in canine pancreas allotransplantation. Transplantation. 1988;46(4): 493–5. [DOI] [PubMed] [Google Scholar]
- 159.Lakey JR, Helms LM, Kin T, Korbutt GS, Rajotte RV, Shapiro AM, et al. Serine-protease inhibition during islet isolation increases islet yield from human pancreases with prolonged ischemia. Transplantation. 2001;72(4):565–70. [DOI] [PubMed] [Google Scholar]
- 160.Heiser A, Ulrichs K, Muller-Ruchholtz W. Isolation of porcine pancreatic islets: low trypsin activity during the isolation procedure guarantees reproducible high islet yields. J Clin Lab Anal. 1994;8(6):407–11. [DOI] [PubMed] [Google Scholar]
- 161.Noguchi H, Ueda M, Hayashi S, Kobayashi N, Okitsu T, Iwanaga Y, et al. Comparison of trypsin inhibitors in preservation solution for islet isolation. Cell Transplant. 2009;18(5):541–7. [DOI] [PubMed] [Google Scholar]
- 162.Basir I, van der Burg MP, Scheringa M, Tons A, Bouwman E. Improved outcome of pig islet isolation by Pefabloc inhibition of trypsin. Transplant Proc. 1997;29(4): 1939–41. [DOI] [PubMed] [Google Scholar]
- 163.Lakey JR, Warnock GL, Shapiro AM, Korbutt GS, Ao Z, Kneteman NM, et al. Intraductal collagenase delivery into the human pancreas using syringe loading or controlled perfusion. Cell Transplant. 1999;8(3):285–92. [DOI] [PubMed] [Google Scholar]
- 164.Weber CJ, Hardy MA, Pi-Sunyer F, Zimmerman E, Reemtsma K. Tissue culture preservation and intramuscular transplantation of pancreatic islets. Surgery. 1978;84(1):166–74. [PubMed] [Google Scholar]
- 165.Reemtsma K, Weber CJ, Pi-Sunyer FX, Lerner RL, Hardy MA. Alternatives in pancreatic islet transplantation: tissue culture studies. Diabetes. 1980;29 Suppl 1:45–51. [DOI] [PubMed] [Google Scholar]
- 166.Rafael E, Tibell A, Ryden M, Lundgren T, Savendahl L, Borgstrom B, et al. Intramuscular autotransplantation of pancreatic islets in a 7-year-old child: a 2-year follow-up. Am J Transplant. 2008;8(2):458–62. [DOI] [PubMed] [Google Scholar]
- 167.Dardenne S, Sterkers A, Leroy C, Da Mata L, Zerbib P, Pruvot FR, et al. Laparoscopic spleen-preserving distal pancreatectomy followed by intramuscular autologous islet transplantation for traumatic pancreatic transection in a young adult. JOP. 2012;13(3):285–8. [PubMed] [Google Scholar]
- 168.Maffi P, Balzano G, Ponzoni M, Nano R, Sordi V, Melzi R, et al. Autologous Pancreatic Islet Transplantation in Human Bone Marrow. Diabetes. 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Elliott RB, Escobar L, Tan PL, Muzina M, Zwain S, Buchanan C. Live encapsulated porcine islets from a type 1 diabetic patient 9.5 yr after xenotransplantation. Xenotransplantation. 2007;14(2):157–61. [DOI] [PubMed] [Google Scholar]
- 170.Basta G, Montanucci P, Luca G, Boselli C, Noya G, Barbaro B, et al. Long-term metabolic and immunological follow-up of nonimmunosuppressed patients with type 1 diabetes treated with microencapsulated islet allografts: four cases. Diabetes Care. 2011;34(11):2406–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Basta G, Calafiore R. Immunoisolation of pancreatic islet grafts with no recipient’s immunosuppression: actual and future perspectives. Curr Diab Rep. 2011;11(5):384–91. [DOI] [PubMed] [Google Scholar]
- 172.Koblas T, Girman P, Berkova Z, Jirak D, Kriz J, Dovolilova E, et al. Magnetic resonance imaging of intrahepatically transplanted islets using paramagnetic beads. Transplant Proc. 2005;37(8):3493–5. [DOI] [PubMed] [Google Scholar]
- 173.Kriz J, Jirak D, Girman P, Berkova Z, Zacharovova K, Honsova E, et al. Magnetic resonance imaging of pancreatic islets in tolerance and rejection. Transplantation. 2005;80(11):1596–603. [DOI] [PubMed] [Google Scholar]
- 174.Toso C, Vallee JP, Morel P, Ris F, Demuylder-Mischler S, Lepetit-Coiffe M, et al. Clinical magnetic resonance imaging of pancreatic islet grafts after iron nanoparticle labeling. Am J Transplant. 2008;8(3):701–6. [DOI] [PubMed] [Google Scholar]
- 175.Eriksson O, Eich T, Sundin A, Tibell A, Tufveson G, Andersson H, et al. Positron emission tomography in clinical islet transplantation. Am J Transplant. 2009;9(12):2816–24. [DOI] [PubMed] [Google Scholar]
- 176.Faradji RN, Froud T, Messinger S, Monroy K, Pileggi A, Mineo D, et al. Long-term metabolic and hormonal effects of exenatide on islet transplant recipients with allograft dysfunction. Cell Transplant. 2009;18(10):1247–59. [DOI] [PubMed] [Google Scholar]
- 177.Froud T, Faradji RN, Pileggi A, Messinger S, Baidal DA, Ponte GM, et al. The use of exenatide in islet transplant recipients with chronic allograft dysfunction: safety, efficacy, and metabolic effects. Transplantation. 2008;86(1): 36–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Froud T, Yrizarry JM, Alejandro R, Ricordi C. Use of DSTAT to prevent bleeding following percutaneous transhepatic intraportal islet transplantation. Cell Transplant. 2004;13(1):55–9. [DOI] [PubMed] [Google Scholar]
- 179.Cechin SR, Perez-Alvarez I, Fenjves E, Molano RD, Pileggi A, Berggren PO, et al. Anti-inflammatory properties of exenatide in human pancreatic islets. Cell Transplant. 2012;21(4):633–48. [DOI] [PubMed] [Google Scholar]
- 180.Gangemi A, Salehi P, Hatipoglu B, Martellotto J, Barbaro B, Kuechle JB, et al. Islet transplantation for brittle type 1 diabetes: the UIC protocol. Am J Transplant. 2008;8(6):1250–61. [DOI] [PubMed] [Google Scholar]
- 181.Toso C, Edgar R, Pawlick R, Emamaullee J, Merani S, Dinyari P, et al. Effect of different induction strategies on effector, regulatory and memory lymphocyte sub-populations in clinical islet transplantation. Transpl Int. 2009;22(2):182–91. [DOI] [PubMed] [Google Scholar]
- 182.Balzano G, Maffi P, Nano R, Zerbi A, Venturini M, Melzi R, et al. Extending indications for islet autotransplantation in pancreatic surgery. Ann Surg. 2013; in press. [DOI] [PubMed] [Google Scholar]


