Abstract
Background:
An incidence of perinatally acquired HIV infection less than 1:100,000 live births is one of the Centers for Disease Control and Prevention (CDC) goals of the United States. Such an estimate has only been possible in recent years because regular nationwide data were lacking.
Method:
Using previously published CDC estimates of the number of infants born with HIV infection in the United States (interpolating for years for which there was no published estimate), and census data on the annual number of live-born infants, estimated incidence was calculated for 1978–2013. Exact 95% confidence intervals (CIs) were calculated using the Poisson distribution.
Results:
Estimated incidence of perinatally acquired HIV infection peaked at 43.1 (95% CI: 41.1 to 45.1) in 1992 and declined rapidly after the use of zidovudine prophylaxis was recommended in 1994. In 2013, estimated incidence of perinatally acquired HIV infection in the United States was 1.8 (95% CI: 1.4 to 2.2), a 96% decline since the peak.
Conclusion:
Estimated incidence of perinatally acquired HIV infection in the United States in 2013 was 1.8/100,000 live births.
Keywords: HIV, incidence, infants, United States
From the beginning of the HIV epidemic, for many years, data were insufficient to answer the question: how many infants with HIV infection are born annually in the United States? Until recently, therefore, it has been necessary to estimate that number by modeling or other means.
Since the mid-1980s, AIDS reporting was mandatory in nearly all jurisdictions, whereas name-based reporting of cases of HIV infection was conducted in a subset of states. Not until 2008 had all states implemented name-based reporting, and only when the systems in all jurisdictions had “matured” sufficiently, in 2012, were the data made available for all the United States. Specifically, since 2008, it has been possible to determine the number of infants born with HIV infection in the United States. With these numbers, it has become possible to calculate the incidence of perinatally acquired HIV, thus addressing one of the goals of the Centers for Disease Control and Prevention for the elimination of perinatally acquired HIV,1 namely, an incidence less than 1 per 100,000 live births.
Before 2008, there were several estimates of the number of infants born with HIV infection in all 50 states.2–5 For the earliest years of the epidemic (1978–1993), the number was “back calculated,”2 beginning with the number of infants and children with diagnoses of AIDS. In more recent years, the number of infants born with HIV infection in the United States was determined by Taylor et al6 for the years 2006–2009, accounting for 2 types of delay—birth to diagnosis and diagnosis to report—but had to extrapolate from the states with name-based reporting to the rest of the states; this number is considered “estimated” because it incorporates those 2 weights. These estimated numbers2–6 were used to construct a curve representing the estimated annual number of infants with HIV infection born during 1978–20107; in that report, for years in which no estimate had been made, the numbers of infants with HIV infection were interpolated. A subsequent report8 estimated the numbers of infants with HIV infection for 2002–2013; this report accounted for delays from birth to diagnosis and from diagnosis to report as had been done earlier6 but did not require extrapolation from states which did not have name-based reporting—an improvement over the former method.
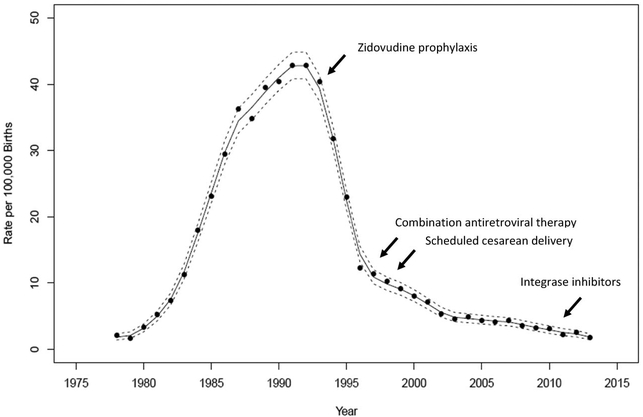
To calculate estimated incidence rates of perinatally acquired HIV infection for 1978–2013 (ie, the number of infants per 100,000 live births), the numbers of infants with perinatal HIV infection estimated for 1978–1993,2 1995–1996,3 2000,4 and 2002–20138 and the interpolated numbers between those years were divided by the respective annual number of live-born infants in the United States.9 Table 1 shows the annual numbers of live-born infants in the United States, the estimated annual number of infants with perinatal HIV born in the United States, and the incidence of perinatal HIV per 100,000 live births with exact 95% confidence intervals (CIs) calculated using the Poisson distribution. The incidence per 100,000 live births is depicted graphically in Figure 1 and fit with a cubic smoothing spline.
TABLE 1.
Annual Number of Live-Born Infants and Estimated Number and Incidence of Perinatal HIV Infection, United States, 1978–2013
| No. of HIV-Infected Infants | Incidence per 100,000 Live Births | ||||
|---|---|---|---|---|---|
| Year | No. of Live-Born Infants | n | 95% CI | n | 95% CI |
| 1978 | 3,333,279 | 70 | 54.6 to 88.4 | 2.1 | 1.6 to 2.7 |
| 1979 | 3,494,398 | 60 | 45.8 to 77.2 | 1.7 | 1.3 to 2.2 |
| 1980 | 3,612,258 | 120 | 99.5 to 143.5 | 3.3 | 2.8 to 4.0 |
| 1981 | 3,629,238 | 190 | 163.9 to 219.0 | 5.2 | 4.5 to 6.0 |
| 1982 | 3,680,537 | 270 | 238.8 to 304.2 | 7.3 | 6.5 to 8.3 |
| 1983 | 3,638,933 | 410 | 371.3 to 451.7 | 11.3 | 10.2 to 12.4 |
| 1984 | 3,669,141 | 660 | 610.6 to 712.3 | 18.0 | 16.6 to 19.4 |
| 1985 | 3,760,561 | 870 | 813.1 to 929.8 | 23.1 | 21.6 to 24.7 |
| 1986 | 3,756,547 | 1100 | 1035.9 to 1167.0 | 29.3 | 27.6 to 31.1 |
| 1987 | 3,809,394 | 1390 | 1317.9 to 1465.0 | 36.5 | 34.6 to 38.5 |
| 1988 | 3,909,510 | 1360 | 1288.7 to 1434.2 | 34.8 | 33.0 to 36.7 |
| 1989 | 4,040,958 | 1590 | 1512.8 to 1670.1 | 39.3 | 37.4 to 41.3 |
| 1990 | 4,158,212 | 1690 | 1610.4 to 1772.5 | 40.6 | 38.7 to 42.6 |
| 1991 | 4,110,907 | 1760 | 1678.7 to 1844.2 | 42.8 | 40.8 to 44.9 |
| 1992 | 4,065,014 | 1750 | 1669.0 to 1834.0 | 43.1 | 41.1 to 45.1 |
| 1993 | 4,000,240 | 1630 | 1551.8 to 1711.1 | 40.7 | 38.8 to 42.8 |
| 1994 | 3,952,767 | 1263 | 1194.3 to 1334.6 | 32.0 | 30.2 to 33.8 |
| 1995 | 3,899,589 | 895 | 837.3 to 955.6 | 23.0 | 21.5 to 24.5 |
| 1996 | 3,891,494 | 480 | 438.0 to 524.9 | 12.3 | 11.3 to 13.5 |
| 1997 | 3,880,894 | 441 | 400.8 to 484.1 | 11.4 | 10.3 to 12.5 |
| 1998 | 3,941,553 | 403 | 364.6 to 444.3 | 10.2 | 9.3 to 11.3 |
| 1999 | 3,959,417 | 364 | 327.6 to 403.4 | 9.2 | 8.3 to 10.2 |
| 2000 | 4,058,814 | 325 | 290.6 to 362.3 | 8.0 | 7.2 to 8.9 |
| 2001 | 4,025,933 | 286 | 253.8 to 321.1 | 7.1 | 6.3 to 8.0 |
| 2002 | 4,021,726 | 216 | 188.2 to 246.8 | 5.4 | 4.7 to 6.1 |
| 2003 | 4,089,950 | 189 | 163.0 to 218.0 | 4.6 | 4.0 to 5.3 |
| 2004 | 4,112,052 | 203 | 176.0 to 232.9 | 4.9 | 4.3 to 5.7 |
| 2005 | 4,138,349 | 182 | 156.5 to 210.4 | 4.4 | 3.8 to 5.1 |
| 2006 | 4,265,555 | 175 | 150.0 to 202.9 | 4.1 | 3.5 to 4.8 |
| 2007 | 4,316,233 | 190 | 163.9 to 219.0 | 4.4 | 3.8 to 5.1 |
| 2008 | 4,247,694 | 153 | 129.7 to 179.3 | 3.6 | 3.1 to 4.2 |
| 2009 | 4,130,665 | 135 | 113.2 to 159.8 | 3.3 | 2.7 to 3.9 |
| 2010 | 3,399,386 | 105 | 85.9 to 127.1 | 3.1 | 2.5 to 3.7 |
| 2011 | 3,953,590 | 90 | 72.4 to 110.6 | 2.3 | 1.8 to 2.8 |
| 2012 | 3,952,841 | 103 | 84.1 to 124.9 | 2.6 | 2.1 to 3.2 |
FIGURE 1.
Estimated incidence of perinatal HIV infection per 100,000 live births, United States 1978–2013. The estimated incidence of perinatal HIV infections per 100,000 live births (points) with a smoothed curve (solid line) and 95% confidence bands (dashed lines). The timing of important advances in recommendations for prevention of maternal-to-child transmission of HIV is noted on the figure. The arrows indicate the year in which the interventions (eg, “Zidovudine prophylaxis”) occurred.
From Figure 1, several observations are possible. Peak estimated incidence occurred in 1992, with 43.1 per 100,000 live births (95% CI: 41.1 to 45.1). Overall, since the implementation of antiretroviral prophylaxis to prevent mother-to-child HIV transmission,10 that is, during 1994–2013, the incidence of perinatally acquired HIV in the United States has decreased approximately 94%. There is an approximately 96% decrease from the peak, which was reached in 1992 several years before the 1994 recommendation to use zidovudine prophylaxis for pregnant women with HIV infection and their newborn infants.10 The incidence of HIV infection in infants declined rapidly in a brief period once zidovudine prophylaxis became standard, a 71% decrease by 1996. That is, a large proportion of the overall decrease occurred in the period when most, if not all, perinatal prophylaxis regimens used a single drug, zidovudine.
In the years immediately after the initial large decrease, 2 major interventions were introduced. The first was the use of 3-drug antiretroviral regimens (known then as “highly active antiretroviral therapy,” or HAART, known for a while as “combination antiretroviral therapy” or cART; now simply known as antiretroviral therapy, ART).11 Although the recommendations did not specify whether such therapy should continue after pregnancy, by 1998, nearly half of women who began ART during pregnancy continued post-partum,12,13 with higher percentages in the years immediately after.14,15 The second major intervention was the introduction of scheduled cesarean delivery for pregnant women with HIV infection whose plasma levels of HIV (“viral load”) were not well controlled.16–18
During 2002–2007, although there was still no specific recommendation to continue ART postpartum, it seems that the practice was becoming more common.15 In the subsequent period, new antiretroviral drugs were introduced and became components of preferred or alternative regimens for HIV-infected pregnant women. Tenofovir and darunavir were recommended for alternative regimens in 2012,19 which also included raltegravir for special circumstances. “Preferred” regimens recommended in 201420 and 2016,21 respectively, included tenofovir and raltegravir, reflecting increased use of such regimens in the years immediately preceding. In addition, in 2012 (March 27), treatment guidelines for adults recommended unequivocally that ART should be started for all HIV-infected persons and should not be discontinued.22 Concurrent with this change in practice, between 2007 and 2013, there was a 64% decline in the incidence of perinatally acquired HIV infections in the United States. During this period, the proportion of pregnant women with HIV infection receiving an integrase strand inhibitor as part of their regimen appears to have increased dramatically; in 2015, 43% of pregnant women enrolled in the Perinatal HIV/AIDS Cohort Study were receiving an integrase strand inhibitor as a component of their ART (20% dolutegravir, 20% elvitegravir, and 3% raltegravir).23 The lowest estimated incidence of perina-tally acquired HIV was in 2013, with 1.8 per 100,000 live births (95% CI: 53.7 to 87.3), still lower than CDC’s incidence goal.
Perinatal HIV transmission continues to occur in the United States, for well-recognized reasons: late maternal diagnosis and incomplete uptake of ART.8 Despite these factors, we describe here a continued—albeit protracted—decline in the incidence curve of perinatally acquired HIV infection. The degree that this curve is affected by the numbers of women of childbearing age is undetermined, but it is interesting that the number of women of childbearing age (13–44 years) living with HIV declined approximately 10% during 2008–2014,24 and the number of new diagnoses of women in this age range declined approximately 30%.25 There is reason to believe that the number of births to women living with HIV has declined significantly in recent years.26 The relative impact of these declines, the apparently increasing birth rate among women living with HIV,27 and the dramatic increase in the use of more potent antiretroviral therapy with integrase inhibitors—with their improved tolerability and ability to rapidly reduce HIV viral load—have yet to be determined.
Acknowledgments
Written work prepared by employees of the Federal Government as part of their official duties is, under the U.S. Copyright Act, a “work of the United States Government” for which copyright protection under Title 17 of the United States Code is not available. As such, copyright does not extend to the contributions of employees of the Federal Government.
Footnotes
All the authors are employees or contractors of the US government. The authors have no funding or conflicts of interest to disclose.
REFERENCES
- 1.Nesheim S, Taylor A, Lampe MA, et al. A framework for elimination of perinatal transmission of HIV in the United States. Pediatrics. 2012;130: 738–744. [DOI] [PubMed] [Google Scholar]
- 2.Davis SF, Byers RH, Lindegren ML, et al. Prevalence and incidence of vertically acquired HIV infection in the United States. JAMA. 1995;274: 952–955. [PubMed] [Google Scholar]
- 3.Lindegren ML, Byers RH Jr, Thomas P, et al. Trends in perinatal transmission of HIV/AIDS in the United States. JAMA. 1999;282: 531–538. [DOI] [PubMed] [Google Scholar]
- 4.Fleming P, Lindegren M, Byers R, et al. Estimated Number of Perinatal HIV Infections, U.S., 2000. Barcelona, Spain; 2002. p. Abstract No. TuPeC4773. Available at: http://www.iasociety.org/Default.aspx?pageId=11&abstractId=7403. Accessed April 1, 2017.
- 5.McKenna MT, Hu X. Recent trends in the incidence and morbidity that are associated with perinatal human immunodeficiency virus infection in the United States. Am J Obstet Gynecol 2007;197(suppl 3):S10–S16. [DOI] [PubMed] [Google Scholar]
- 6.Taylor AW, Little KM, Zhang X, et al. Estimated perinatal antiretroviral exposures, cases prevented and infected infants in the era of antiretroviral prophylaxis in the United States Conference on Retroviruses and Opportunistic Infections. Seattle, WA: 2011. Accessed March 5–8, 2012 Abstract T 103. [Google Scholar]
- 7.Little KM, Taylor AW, Borkowf CB, et al. Perinatal antiretroviral exposure and prevented mother-to-child HIV infections in the era of antiretroviral prophylaxis in the United States, 1994–2010. Pediatr Infect Dis J 2017;36:66–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Taylor AW, Nesheim SR, Zhang X, et al. Estimated perinatal HIV infection among infants born in the United States, 2017 Estimated perinatal HIV infection among infants born in the United States, 2002–2013. JAMA Pediatr 2017;171:435–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.CDC. National Center for Health Statistics: National Vital Statistics Reports Vol. 64 Available at: https://www.cdc.gov/nchs/data/nvsr/nvsr64/nvsr64_12.pdf Accessed May 4, 2017. [Google Scholar]
- 10.Centers for Disease Control and Prevention. Recommendations of the U.S. Public Health Service Task Force on the use of zidovudine to reduce perinatal transmission of human immunodeficiency virus. MMWR Recomm Rep 1994;43:1–20. [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention. Public Health Service Task Force recommendations for the use of antiretroviral drugs in pregnant women infected with HIV-1 for maternal health and for reducing perinatal HIV-1 transmission in the United States. Centers for Disease Control and Prevention. MMWR Recomm Rep 1998;47:1–30. [PubMed] [Google Scholar]
- 12.Tedaldi E, Willard S, Gilmore J, et al. Continuation of postpartum antiretroviral therapy in a cohort of women infected with human immunodeficiency virus. J Assoc Nurses AIDS Care. 2002;13:60–65. [DOI] [PubMed] [Google Scholar]
- 13.Turner BJ, Newschaffer CJ, Zhang D, et al. Antiretroviral use and pharmacy-based measurement of adherence in postpartum HIV-infected women. Med Care. 2000;38:911–925. [DOI] [PubMed] [Google Scholar]
- 14.Ejedepang-Koge I, Theall K, Clark R. Pre- and post-partum antiretroviral choices among HIV-infected pregnant women. J Acquir Immune Defic Syndr 2004;35:428–429. [DOI] [PubMed] [Google Scholar]
- 15.Watts DH, Lu M, Thompson B, et al. Treatment interruption after pregnancy: effects on disease progression and laboratory findings. Infect Dis Obstet Gynecol 2009;2009:456717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.International Perinatal HIV Group. The mode of delivery and the risk of vertical transmission of human immunodeficiency virus type 1–a meta-analysis of 15 prospective cohort studies. The International Perinatal HIV Group. N Engl J Med 1999;340:977–987. [DOI] [PubMed] [Google Scholar]
- 17.European Mode of Delivery Collaboration. Elective caesarean section versus vaginal delivery in prevention of vertical HIV-1 transmission: a randomised clinical trial. Lancet. 1999;353:1035–1039. [DOI] [PubMed] [Google Scholar]
- 18.Committee on Obstetric Practice. ACOG committee opinion scheduled cesarean delivery and the prevention of vertical transmission of HIV infection. Number 234, May 2000 (replaces number 219, August 1999). Int J Gynaecol Obstet 2001;73:279–281. [DOI] [PubMed] [Google Scholar]
- 19.Panel on Treatment of HIV-Infected Pregnant Women and Prevention of Perinatal Transmission. Recommendations for Use of Antiretroviral Drugs in Pregnant HIV-1-Infected Women for Maternal Health and Interventions to Reduce Perinatal HIV Transmission in the United States. Available at: http://aidsinfo.nih.gov/contentfiles/lvguidelines/PerinatalGL.pdf. Version July 31, 2012. Accessed December 9, 2016.
- 20.Panel on Treatment of HIV-Infected Pregnant Women and Prevention of Perinatal Transmission. Recommendations for Use of Antiretroviral Drugs in Pregnant HIV-1-Infected Women for Maternal Health and Interventions to Reduce Perinatal HIV Transmission in the United States. Available at: http://aidsinfo.nih.gov/contentfiles/lvguidelines/PerinatalGL.pdf. Version March 28, 2014. Accessed December 9, 2016.
- 21.Panel on Treatment of HIV-Infected Pregnant Women and Prevention of Perinatal Transmission. Recommendations for Use of Antiretroviral Drugs in Pregnant HIV-1-Infected Women for Maternal Health and Interventions to Reduce Perinatal HIV Transmission in the United States. Available at: https://aidsinfo.nih.gov/contentfiles/PerinatalGL003435.pdf. Version October 26, 2016. Accessed April 13, 2017.
- 22.Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the Use of Antiretroviral Agents in HIV-1-Infected Adults and Adolescents: Department of Health and Human Services. Available at: http://aidsinfo.nih.gov/ContentFiles/AdultandAdolescentGL.pdf. Version March 27, 2012. Accessed May 1, 2017.
- 23.Pediatric HIV/AIDS Cohort Study (PHACS) Surveillance Monitoring of ART Toxicities (SMARTT) Study. Annual Administrative Report. 2016. Cited with permission of George Seagem December 2016. [Google Scholar]
- 24.NCHHSTP Atlas. HIV Prevalence | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | All Races/Ethnicities | Female | 13–24 | 25–34 | 35–44 | All Transmission Categories | United States. Available at: https://www.cdc.gov/nchhstp/atlas/is. Accessed March 22, 2017.
- 25.NCHHSTP Atlas. HIV Diagnoses | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | All Races/Ethnicities | Female | 13–24 | 25–34 | 35–44 | All Transmission Categories | United States. Available at: https://www.cdc.gov/nchhstp/atlas/is. Accessed March 22, 2017.
- 26.Nesheim SR, FitzHarris LF, Lampe MA, et al. How many women with HIV infection give birth annually in the United States? Manuscript in preparation. [DOI] [PMC free article] [PubMed]
- 27.Haddad LB, Wall KM, Mehta CC, et al. Trends of and factors associated with live-birth and abortion rates among HIV-positive and HIV-negative women. Am J Obstet Gynecol 2017;216:71.e1–71.e16. [DOI] [PMC free article] [PubMed] [Google Scholar]