Abstract
Objective:
To contribute to decision analysis by estimating utility, defined as an individual’s valuation of specific health states, for different pregnancy contexts.
Study design:
Cross-sectional analysis of data from pregnant women recruited at pregnancy testing clinics during June 2014–June 2015. Utility was measured using the visual analog scale (VAS), PROMIS GSF-derived utility, standard gamble (SG), and time-trade-off (TTO) approaches. Six dimensions of pregnancy context were assessed including: intention, desirability, planning, timing, wantedness, and happiness. Multivariable regression modeling was used to examine the associations between pregnancy context and utility while controlling for women’s sociodemographic and health characteristics.
Results:
Among 123 participants with diverse characteristics, aged 27±6 years, with mean gestation of 7.5±3 weeks, few reported optimal pregnancy contexts. Mean utility of the pregnancy state varied across contexts, whether measured with VAS (0.28–0.91), PROMIS GSF-derived utility (0.66–0.75), SG (0.985–1.00) or TTO (0.9990–0.99999). The VAS-derived mean utility score for unintended pregnancy was 0.68 (95% CI 0.59, 0.77). Multivariable regression analysis demonstrated significant disutility of unintended pregnancy, as well as all other unfavorable pregnancy contexts, when measured by VAS. In contrast, PROMIS GSF-derived utility only detected a significant reduction in utility among ambivalent compared to wanted pregnancy, while SG and TTO did not show meaningful differences in utility across pregnancy contexts.
Conclusions:
Unintended pregnancy is associated with significant patient-reported disutility, as is pregnancy occurring in other unfavorable contexts. VAS-based measurements provide the most nuanced measures of the utility for pregnancy in varying contexts.
Implications:
Decision analyses, including assessments of the cost-effectiveness of pregnancy related interventions, should incorporate measures of the utility of pregnancy in various contexts.
Keywords: London measure of unplanned pregnancy, Unintended pregnancy, Utility, Visual analog scale
1. Introduction
Approximately half (45%) of all U.S. pregnancies are unintended [1], resulting in an estimated $4.5 billion in annual direct medical costs [2] and $21 billion in 2010 Federal and state public expenditures [3]. With increased focus on reducing unintended pregnancy [4], cost-effectiveness analyses are a useful tool to inform decisions regarding efforts to reduce unintended pregnancies and improve reproductive health outcomes by evaluating expected economic and quality of life impact of various interventions [5]. Yet cost effectiveness research related to reproduction, including assessment of utility related to pregnancy, is currently understudied [5,6]. Further, reliable and valid utility measure estimates are necessary for cost-effectiveness analyses regarding unintended pregnancy. To date, the quality of these studies has been limited by lack of objective measures that reflect differences in health utility by pregnancy context.
“Utility” is one way of evaluating health-related quality of life (HRQoL) for specific health states [7]. Existing research on the utility of pregnancy is limited by using utility estimates derived from hypothetical health scenarios among non-pregnant participants [8,9]. As perspectives on hypothetical health states differ from individuals’ actual experiences [10], research is needed to better characterize the utility of pregnancy in unfavorable pregnancy contexts using more relevant study populations. Furthermore, recent literature has called for awareness of the limitations of considering only whether a pregnancy was intended or planned when evaluating the effects of the pregnancy on a woman’s life and health [11,12], Multidimensional pregnancy perspectives may be relevant to women’s perceived utility of pregnancy as well.
To fill this gap, our study aimed to evaluate health utility of pregnancy occurring in a variety of “contexts” measured as intention, wantedness, planning, timing, desirability, and happiness [13] among a cohort of pregnant women. Specifically, we aimed to calculate utility estimates for varied contexts of pregnancy that can be used in future cost-effectiveness analyses. We also compared utilities elicited using the visual analog scale (VAS) approach [9,14], which has demonstrated validity in previous studies examining valuation of pregnancy outcomes [15,16], with those derived from other approaches, including standard gamble [7,17], time-trade-off [18], and the Patient Reported Outcome Measurement Information System (PROMIS) Global Short Form (GSF)-derived utility [19].
2. Methods
2.1. Study setting and design
Data for this analysis came from a sample of women presenting for pregnancy testing services at two clinical sites in New Haven, CT, during the period of June 2014 to June 2015. While the original study included women recruited at various clinical settings (e.g. abortion care sites), the current analysis is restricted to women recruited from pregnancy testing sites only in order to focus on those with a recent pregnancy diagnosis to best assess the relationship between pregnancy context and utility. Women were eligible if they had a positive pregnancy test on the day of recruitment, were English or Spanish speaking, had completed <24 weeks of gestation, were 15–44 years of age, and completed study enrollment within 1 week of their clinical pregnancy test. Participants could complete the study in English or Spanish. Overall, research staff approached 225 women with a positive pregnancy test regarding study participation. Of those, 123 women were eligible and completed the enrollment questionnaire.
The enrollment questionnaire was self-administered and ascertained each participant’s sociodemographic characteristics, medical history, reproductive history, HRQoL and assessments of the utility of their current pregnancy. The study protocol was reviewed and approved by the Yale University Human Research Protection Program. Written consent was obtained from study participants prior to enrollment.
2.2. Measures of pregnancy context
As previously described [13], there are six dimensions of pregnancy context (Appendix A), and assessment of utility scores associated with these pregnancy contexts can enable a more comprehensive understanding of patients’ perceptions about their pregnancy-related health state. These context measures included 3 “pre-pregnancy perspectives,” including intention, wantedness, and planning, and 3 “post-conception perspectives,” including timing, desirability, and happiness. Each of the pregnancy context measures was evaluated as a 3-level categorical variable reflecting a (1) favorable, (2) ambivalent/neutral, or (3) unfavorable pregnancy context. For example, pregnancy intention was categorized as: “intended”, “intentions changing”, or “unintended.” Pregnancy intention, wantedness, and timing were measured using elements from the London Measures of Unplanned Pregnancy (LMUP) construct [20].
2.3. Measures of utility
Utility is a metric quantifying the “relative value placed on a specific health status or an improvement in health status” [21]. Utility values range from 0 to 1, with 0 representing death and 1 representing perfect health state [22], while disutility is defined as the corresponding decrease or measured decrement in overall utility. We measured utility using four different approaches detailed below.
2.3.1. Visual Analog Scale
Visual Analog Scale (VAS) measures utility of health states [9,14] by asking participants to indicate how they felt after learning they were pregnant by placing a mark on a 10-cm line that ranged from 0 (“As if I was dying’) of 10 (“In perfect health”) [9]. Values from the 10-cm scale were then calibrated to a 0–1.0 scale.
2.3.2. PROMIS global short form derived utility
We administered the National Institutes of Health (NIH) Patient Reported Outcome Measurement Information System (PROMIS) Global Short Form (GSF) [23,24] to assess HRQoL [13]. Participants’ responses to the GSF were converted to utility scores based on a previously validated algorithm mapping GSF responses to the EuroQol (EQ-5D) utility score [19].
2.3.3. Standard gamble
The standard gamble [7] elicitation approach used questions previously employed to assess utility of a hypothetical unintended pregnancy [9] (see Appendix B). The accepted risk of death was then converted to a utility score as (1-accepted risk of death). SG is a well-established method grounded in traditional economic theories to elicit individual’s preferences about a given health state under specific conditions of uncertainty [22], In this method, respondents are given choices regarding willingness to accept a risk of death in order to avoid a specified health outcome; specific to this study, participants’ willingness to accept a risk of death to avoid the current pregnancy.
2.3.4. Time trade-off (TTO)
Utility assessed using TTO is based upon willingness to trade time at the end of life to avoid a specific disease or health state [22]. In the TTO approach (see Appendix B), disutility was calculated as the time that a woman reported being willing to give up to avoid being pregnant divided by her life expectancy (life expectancy based on U.S. life tables [25]). Her utility score is then calculated as (1-disutility). For women who selected the upper bound category of time willing to give up (i.e., ≥ 3 months), our primary analysis calculated their utility score assumed 3 months as the maximum time they were willing to give up. We also performed a sensitivity analysis by using 10 years as the maximum time willing to give up for women in this upper bound category [9].
2.4. Patient characteristics
Measures of potential confounding factors in the association between pregnancy context and utility included sociodemographic characteristics (i.e., age, race, ethnicity, level of education, employment, and relationship status), reproductive history (i.e., parity, previous miscarriage, and previous abortion), presence of chronic medical condition (e.g., asthma, diabetes, thyroid problem), depression, anxiety, and substance use during the previous 3 months (smoking and tobacco use, marijuana use and alcohol consumption). Gestational age was measured based on reported last menstrual period at time of enrollment.
2.5. Statistical analysis
Descriptive statistics were estimated to summarize patient characteristics. Bivariate associations between pregnancy contexts and measures of utility were assessed using analysis of variance (ANOVA) or Kruskall-Wallis tests for continuous measures depending on whether the utility score was normally distributed. We also estimated linear regression models for VAS and GSF-derived utility scores with and without adjusting for other covariates to examine the magnitude of difference in utility between different pregnancy contexts. Each pregnancy context was assessed in a separate model, using favorable pregnancy context as the referent group (e.g. intended pregnancy). Pregnancy context was forced into the model and patient characteristics that were significant at p<.20 level in bivariate analysis were included as covariates in the regression model. Such regression analysis was not performed for SG and TTO-derived utility scores because there was very limited variation in the scores.
Twenty-eight women had missing observations for VAS measurement. We assessed their potential impact on interpretation of findings by comparing patient characteristics (sociodemographics, pregnancy context, and utility scores) between women who completed the VAS versus those with incomplete VAS information. Statistical analysis was performed using SAS 9.4 (SAS Institute, Cary, NC, USA).
3. Results
3.1. Patient characteristics and pregnancy context
Among the 123 participants, mean age was 26.7(±6.3) years and average gestational age at enrollment was 7.5(±3.0) weeks (Table 1). Most participants were non-Hispanic Black (36.9%) or Hispanic (45.9%). Few (14.8%) were married or had at least some college education (36.0%). Most women were parous (72.9%), and previous miscarriage was reported by 38.8% and previous abortion by 37.9%.
Table 1.
Participant characteristics and sociodemographics, N= 123.
| Characteristic | n (%) or mean (SD) |
|---|---|
| Total | 123 (100.0) |
| Age | |
| Mean age in yrs. (SD) | 26.7 (±6.3) |
| Gestational age at Enrollment | |
| Mean gestational age in weeks (SD) | 7.5 (±3.0) |
| Language study completed in | |
| English | 85 (69.1) |
| Spanish | 38 (30.9) |
| Race-ethnicity | |
| Black, non-Hispanic | 45 (36.9) |
| White, non-Hispanic | 13 (10.7) |
| Hispanic | 56 (45.9) |
| Multiracial, Other | 8 (6.6) |
| Education | |
| 12 yrs./GED or less | 77 (63.1) |
| Some college, college degree | 45 (36.9) |
| Employment | |
| Unemployed/homemaker | 68 (55.7) |
| Full time/part time | 54 (44.3) |
| Relationship status | |
| Single | 49 (40.1) |
| Married | 18 (14.8) |
| Living with partner, not married | 39 (32.0) |
| Separated, divorced, widowed | 16 (13.1) |
| Chronic medical problem | |
| Yes | 22 (17.9) |
| No | 101 (82.1) |
| Smoking/tobacco products in past 3 months | |
| None | 85 (69.1) |
| Once/twice or monthly | 10 (8.1) |
| Weekly or daily | 28 (22.8) |
| Drinking alcohol past 3 months | |
| None | 56 (45.5) |
| Once/twice or monthly | 52 (42.3) |
| Weekly or daily | 15 (12.2) |
| Marijuana use past 3 months | |
| None | 97 (78.9) |
| Once/twice or monthly | 14 (11.4) |
| Weekly or daily | 12 (9.8) |
| Parity | |
| 0 | 33 (27.1) |
| 1 | 45 (36.9) |
| 2+ | 44 (36.1) |
| Previous miscarriage | |
| Yes | 45 (38.8) |
| No | 71 (61.2) |
| Previous abortion | |
| Yes | 44 (37.9) |
| No | 72 (62.1) |
Totals may not add to N=123 due to missing observations.
Fifty percent of participants reported that they did not intend to become pregnant, 25.2% that they did not want a baby, 17.9% that pregnancy was unplanned, and 19.5% that the pregnancy occurred at the wrong time (Table 2). However, most women reported that they were happy about the pregnancy news (72.4%) and that the pregnancy was desired (60.1%).
Table 2.
Measures of pregnancy context among study sample, N= 123.
| Measures of pregnancy context | n(%) |
|---|---|
| Assessment of pre-pregnancy perspectives | |
| Intention | |
| Intended to get pregnant | 40 (32.5) |
| Intentions changing | 21 (17.1) |
| Did not intend to get pregnant | 62 (50.4) |
| Wanted | |
| Wanted to have a baby | 47 (38.2) |
| Mixed feelings | 45 (36.6) |
| Did not want to have a baby | 31 (25.2) |
| London Measure of Unplanned Pregnancy | |
| Planned | 36 (29.3) |
| Ambivalent | 65 (52.9) |
| Unplanned | 22 (17.9) |
| Assessment of post-conception perspectives | |
| Timing | |
| Right time | 53 (43.1) |
| Ok but not quite right | 46 (37.4) |
| Wrong time | 24 (19.5) |
| Desired | |
| Yes | 74 (60.1) |
| Not sure | 27 (22.0) |
| No | 22 (17.9) |
| Happy | |
| Happy | 89 (72.4) |
| Neither happy/unhappy, not sure | 22 (17.9) |
| Unhappy | 12 (9.8) |
Totals may not add to N =123 due to missing observations.
3.2. Association of pregnancy context with utility
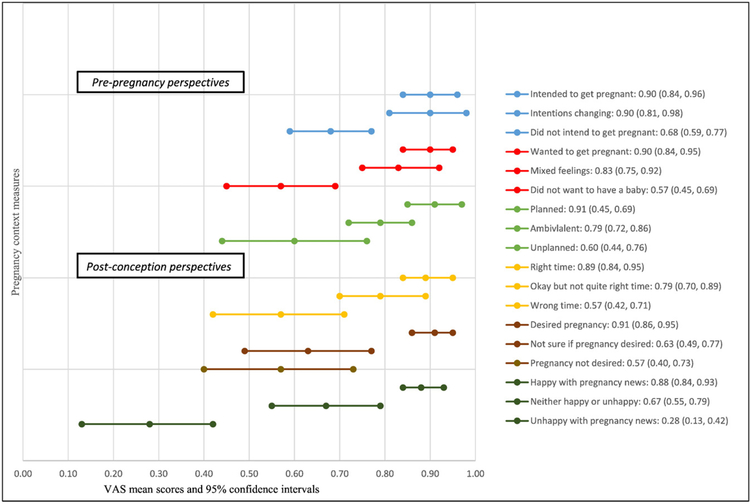
Overall, VAS scores among the sample ranged from 0.04–1.00 with average score of 0.79(±0.27). Mean VAS score varied substantially across different pregnancy context (Fig. 1A, Table 3), with VAS-derived mean utility score for unintended pregnancy of 0.68 (95% CI 0.59, 0.77). Wide variation is observed for context measure of happiness with pregnancy news, ranging from 0.28 among those unhappy, 0.67 for neither happy nor unhappy, and 0.88 among women happy with pregnancy news. Similar patterns are observed for other context measures, with highest VAS scores among those reporting favorable pregnancy contexts, lower for ambivalent categories and the lowest scores among those with unfavorable pregnancy contexts (e.g. unwanted, unintended, unplanned pregnancy). For each of the six measures of pregnancy context, the VAS score differed significantly across the favorable, ambivalent/neutral, and unfavorable perception categories (p<.001 for all).
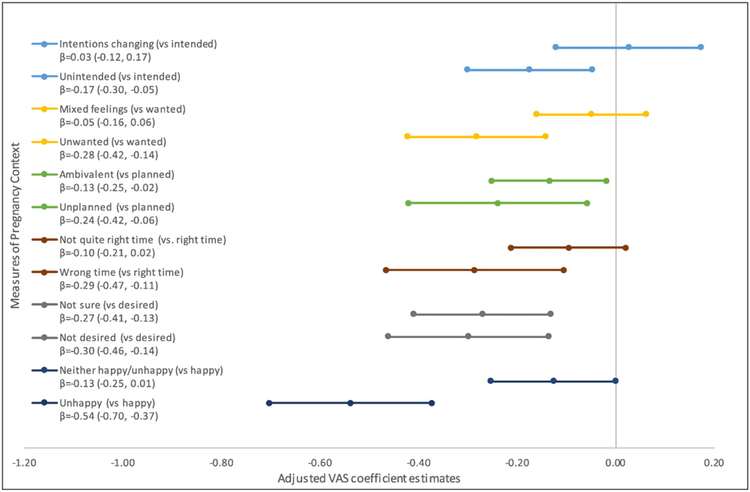
Fig. 1.
(A) Observed mean utility for each measure of pregnancy context Utility defined as an individual’s valuation of specific health states, ranging from 0 (feeling as if dying) to 1 (perfect health). (B) Estimated difference in utility between ambivalent or unfavorable pregnancy context and favorable pregnancy context, based on adjusted regression analysis. Multivariable models adjusted for education, race/ethnicity, smoking, marijuana use, language, recruitment site, history of depression, history of anxiety.
Table 3.
Measures of health utility for different pregnancy contexts.
| Measures of Pregnancy Context | Visual Analog Scale (n=95) | PROMIS GSF-derived utility (n=114) | Standard Gamble (n=121) | Time Trade Off (n=120) | ||||
|---|---|---|---|---|---|---|---|---|
| Mean (SD) | p-Valuea | Mean (SD) | p-Valueb | Mean (SD) | p-Valuea | Mean (SD) | p-Valuea | |
| Overall | 0.79 (0.27) | 0.71 (0.10) | 0.996 (0.017) | 0.9997 (0.001) | ||||
| Assessment of pre-pregnancy perspectives | ||||||||
| Intention | <.001 | .327 | .408 | .046 | ||||
| Intended to get pregnant | 0.90 (0.17) | 0.73 (0.10) | 0.994 (0.023) | 0.99999 (0.0003) | ||||
| Intentions changing | 0.90 (0.17) | 0.71 (0.12) | 1.000 (0.000) | 0.9995 (0.0016) | ||||
| Did not intend to get pregnant | 0.68 (0.30) | 0.70 (0.10) | 0.996 (0.015) | 0.9996 (0.0012) | ||||
| Wanted | <.0001 | .012 | .026 | .004 | ||||
| Wanted to have a baby | 0.90 (0.18) | 0.74 (0.10) | 0.995 (0.022) | 0.9999 (0.0007) | ||||
| Mixed feelings | 0.83 (0.24) | 0.68 (0.10) | 1.000 (0.000) | 0.9997 (0.0013) | ||||
| Did not want to have a baby | 0.57 (0.29) | 0.71 (0.10) | 0.992 (0.020) | 0.9994 (0.0014) | ||||
| London Measures | .001 | .053 | .005 | .005 | ||||
| Planned | 0.91 (0.17) | 0.74 (0.10) | 0.999 (0.008) | 0.9999 (0.0001) | ||||
| Ambivalent | 0.79 (0.25) | 0.71 (0.10) | 0.997 (0.018) | 0.9996 (0.0012) | ||||
| Unplanned | 0.60 (0.33) | 0.67 (0.10) | 0.989 (0.023) | 0.9993 (0.0015) | ||||
| Assessment of post-conception perspectives | ||||||||
| Timing | <.0001 | .001 | 0.100 | .004 | ||||
| Right time | 0.89 (0.17) | 0.75 (0.09) | 0.996 (0.019) | 0.9999 (0.0006) | ||||
| Ok but not quite right | 0.79 (0.26) | 0.68 (0.10) | 0.998 (0.010) | 0.9996 (0.0013) | ||||
| Wrong time | 0.57 (0.31) | 0.68 (0.09) | 0.992 (0.021) | 0.9993 (0.0015) | ||||
| Desired | <.0001 | .017 | .064 | .002 | ||||
| Yes | 0.91 (0.16) | 0.73 (0.09) | 0.997 (0.017) | 0.9998 (0.0008) | ||||
| Not sure | 0.63 (0.30) | 0.69 (0.11) | 0.998 (0.010) | 0.9996 (0.0014) | ||||
| No | 0.57 (0.30) | 0.67 (0.10) | 0.991 (0.022) | 0.9992 (0.0015) | ||||
| Happy | <.0001 | .048 | .019 | .010 | ||||
| Happy | 0.88 (0.19) | 0.72 (0.10) | 0.997 (0.016) | 0.9998 (0.0010) | ||||
| Neither happy/unhappy | 0.67 (0.25) | 0.69 (0.09) | 0.997 (0.011) | 0.9996 (0.0013) | ||||
| Unhappy | 0.28 (0.17) | 0.66 (0.12) | 0.985 (0.028) | 0.9990 (0.0017) | ||||
Missing observations for utility measures: n =28 (VAS); n=9 (GSF-derived utility); n=2 (SG); n=3 (TTO).
Bold text indicates a statistical significance with a p-value of less than 0.05.
Time-trade-off based on 3 months as greatest upper value.
Kruskall-Wallis.
ANOVA.
Range of PROMIS GSF-derived utility scores was 0.46–0.88, averaging 0.71(±0.10) for the sample. PROMIS GSF-derived utility scores demonstrated a similar pattern across pregnancy context, but with somewhat less variation than VAS-derived scores. Mean utility scores demonstrated less variation in range across favorable, ambivalent, and unfavorable contexts, particularly for pregnancy intention, ranging from 0.70–0.73. Additionally, lowest mean utility scores for wantedness were observed among those who reported mixed feelings (0.68), while utility among wanted and unwanted pregnancies was 0.74 and 0.71, respectively. GSF-derived utility scores differed significantly across favorable, ambivalent/neutral, and unfavorable perception categories for four pregnancy contexts (i.e., wantedness, timing, desirability, and happiness).
In contrast, SG and TTO-based utility scores showed very limited variability across the different pregnancy contexts and were clustered around 1.0, with overall scores ranging 0.90–1.0 for SG and 0.994–1.00 for TTO; mean values were 0.996(±0.017) for SG and 0.9997(±0.001) for TTO, respectively. The mean SG-based utility varied slightly from 0.985 in unhappy pregnancy to 1.00 in women who had changing intention or mixed wantedness about pregnancy, while the mean TTO-based utility score varied subtly from 0.9990 in unhappy pregnancy to 0.99999 in intended pregnancy. Although SG and TTO-based utility scores differed statistically across the favorable, ambivalent/neutral, and unfavorable perception categories for three and six of the measures of pregnancy context, respectively, the magnitude of the difference was minimal. Our sensitivity analysis using an upper bound of 10 years for calculation of TTO-based utility score showed no material difference in results.
Unadjusted and adjusted regression analyses for the association of pregnancy context with VAS utility are presented in Fig. 1B and Table 4. After adjusting for patient characteristics, greater disutility was observed among those who did not intend to get pregnant, did not want to have a baby, or were ambivalent or reported unplanned pregnancy (mean adjusted difference ranging from−0.13 to −0.28, p<.03 for these contexts), compared to women reporting their pregnancy was intended, they wanted to have a baby, or pregnancy was planned, respectively. Likewise, women who indicated it was the wrong time to become pregnant, were not sure or not desiring the pregnancy, or were unhappy about the pregnancy news, demonstrated greater disutility measured by VAS compared to those reporting pregnancies that occurred at the right time, were desired, or produced feelings of happiness with the pregnancy news (mean adjusted difference ranging from −0.27 to −0.54, p<.01 for these contexts).
Table 4.
Multivariable assessment of the associations between pregnancy context and health utility.
| Pregnancy context | Visual Analog Scale coefficient estimates | PROMIS GSF−derived utility coefficient estimates | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Unadjusted | Adjusteda | Unadjusted | Adjustedb | |||||||||
| Difference in utility score | 95% Cl | Difference in utility score | 95% Cl | Difference in utility score | 95% Cl | Difference in utility score | 95% Cl | |||||
| Assessment of pre-pregnancy perspectives | ||||||||||||
| Intention | ||||||||||||
| Intended to get pregnant | Ref | Ref | Ref | Ref | ||||||||
| Intentions changing | −0.01 | −0.15, 0.14 | 0.03 | −0.12, 0.17 | −0.02 | −0.08, 0.03 | −0.01 | −0.06, 0.05 | ||||
| Did not intend to get pregnant | −0.22 | −033, −0.11 | −0.17 | −0.30, −0.05 | −0.03 | −0.07, 0.01 | −0.01 | −0.05, 0.03 | ||||
| Wanted | ||||||||||||
| Wanted to have a baby | Ref | Ref | Ref | Ref | ||||||||
| Mixed feelings | −0.06 | −0.17, 0.05 | −0.05 | −0.16, 0.06 | −0.06 | −0.11, −0.02 | −0.05 | −0.09, −0.01 | ||||
| Did not want to have a baby | −0.32 | −0.45, −0.20 | −0.28 | −0.42, −0.14 | −0.03 | −0.08,0.02 | −0.01 | −0.05, 0.04 | ||||
| London Measure of Unplanned | ||||||||||||
| Pregnancy | ||||||||||||
| Planned | Ref | Ref | Ref | Ref | ||||||||
| Ambivalent | −0.12 | −0.23, −0.01 | −0.13 | −0.25, −0.02 | −0.03 | −0.07, 0.01 | −0.01 | −0.05, 0.03 | ||||
| Unplanned | −0.31 | −0.45, −0.16 | −0.24 | −0.42, −0.06 | −0.07 | −0.12, −0.01 | −0.04 | −0.09, 0.02 | ||||
| Assessment of post-conception perspectives | ||||||||||||
| Timing | ||||||||||||
| Right time | Ref | Ref | Ref | Ref | ||||||||
| Ok but not quite right | −0.10 | −0.21, 0.01 | −0.10 | −0.21, 0.02 | −0.07 | −0.11, −0.03 | −0.03 | −0.07, 0.01 | ||||
| Wrong time | −0.33 | −0.46, −0.20 | −0.29 | −0.47, −0.11 | −0.07 | −0.12, −0.02 | −0.04 | −0.09, 0.01 | ||||
| Desired | ||||||||||||
| Yes | Ref | Ref | Ref | Ref | ||||||||
| Not sure | −0.28 | −0.39, −0.16 | −0.27 | −0.41, −0.13 | −0.04 | −0.09, 0.01 | −0.01 | −0.05, 0.04 | ||||
| No | −0.34 | −0.46, −0.21 | −0.30 | −0.46, −0.14 | −0.06 | −0.12, −0.02 | −0.03 | −0.08, 0.02 | ||||
| Happy | ||||||||||||
| Happy | Ref | Ref | Ref | Ref | ||||||||
| Neither happy/unhappy, not sure | −0.21 | −0.31, −0.11 | −0.13 | −0.25, 0.01 | −0.04 | −0.09, 0.01 | 0.01 | −0.05, 0.06 | ||||
| Unhappy | −0.61 | −0.75, −0.46 | −0.54 | −0.70, −0.37 | −0.07 | −0.13, −0.01 | −0.03 | −0.09, 0.03 | ||||
Bold text indicates a statistical significance with a p-value of less than .05.
Adjusted for education, race/ethnicity, smoking, marijuana use, language, recruitment site, history of depression, history of anxiety.
Adjusted for age, chronic medical problems, gestational age at enrollment, alcohol use, smoking, marijuana use, history of depression, history of anxiety.
Table 4 also reported unadjusted and adjusted regression analyses for the association of pregnancy context with PROMIS GSF-derived utility score. After adjusting for patient sociodemographic and health characteristics, PROMIS GSF-derived utility score only differed significantly between women who had ambivalent feelings and those wanting to have a baby (mean adjusted difference=−0.05, p=.01). There was no significant difference in other dimensions of pregnancy context.
Comparison of participants who had complete VAS data versus those with missing data on VAS suggested no statistically significant differences in participant characteristics, pregnancy context, and utility measures (all p values >.05; data not shown in tables).
4. Discussion
Among women with a recent pregnancy diagnosis, pregnancies that were reported to have occurred at the wrong time, were unintended, unwanted, not desired, unplanned or met with unhappiness are associated with disutility as measured by the visual analog scale (VAS). The value and range in variability of utility score for these pregnancy contexts differed by measurement approach, with the VAS-based approach demonstrating more discriminatory ability across pregnancy context than other measurement methods. This analysis provides utility estimates for “unintended pregnancy”, as well as other pregnancy contexts, that can be used in future cost-effectiveness analyses.
A previous study evaluating the utility of unintended pregnancy among 192 non-pregnant women reported a VAS-based score of 0.49 [9]. In contrast, we found a higher VAS-based utility score of 0.68 among women currently experiencing an unintended pregnancy. This is consistent with previous literature suggesting higher utility/lower disutility among individuals experiencing actual health states compared to hypothetical health states [10], highlighting the importance of assessing utility in actual patient populations.
Our study improves upon and extends the literature in several important ways. First, research examining utility regarding pregnancy among currently pregnant women has been sparse [26,27] and previous cost-effectiveness analyses have relied on published utility metrics derived from non-pregnant samples [8,9,28,29]. Earlier studies have often focused on hypothetical scenarios of pregnancy [15,16,30], and therefore may not accurately reflect the experiences of pregnant women, including pregnant women’s experiences of different pregnancy contexts. In contrast, we assessed utility among currently pregnant women close to the time of pregnancy diagnosis, and controlled for potential confounders in multivariable analysis. Further, use of multidimensional context measures beyond traditional measures of planning and intention are integral to improving our understanding of individual pregnancy perspectives and essential for evaluating impact of various strategies for addressing women’s reproductive healthcare needs [11,12]. However, there has been a lack of data on utility with respect to different pregnancy contexts in the literature. In this regard, our study extends analysis of multidimensional pregnancy perspectives, including pregnancy timing, wantedness, desirability, and happiness with pregnancy. Additionally, we evaluated ambivalence as a separate category, which has been largely overlooked in previous research, and demonstrated significant disutility within this context category (e.g. mixed feelings about wanting to be pregnant). This highlights the importance of more attention to this unique group in future research and clinical care.
Based on our findings, VAS captures the variability of utility across various pregnancy contexts and may be the most appropriate metric for use in assessing health utility among pregnant women. Previous research has demonstrated the validity of VAS in evaluating health states related to pregnancy and birth outcomes, reporting high test-retest reliability among a community-based sample [15] and within group reliability among patient, layperson, and professional participant groups [16]. Moreover, VAS measures adequately captured significant differences within specific gynecological conditions including and pelvic inflammatory disease health states [31]. In our analysis, we also found expected differences in VAS-based utility across various pregnancy contexts and significant disutility for ambivalent/unfavorable contexts. On the contrary, GSF-derived utility score only captured variability in selected pregnancy contexts, and SG and TTO-derived utility measures varied minimally across levels of pregnancy context. It is likely that these elicitation methods may not be sensitive enough to detect differences in women’s perceptions about the various pregnancy contexts. In addition, methods based on responses to risk of death (SG) or trading time at the end of life (TTO) were designed to evaluate chronic or terminal disease health states and may not be suitable for assessing utility of pregnancy-related health states which are generally not life-threatening conditions.
An important consideration is that utility measured during pregnancy reflects a short-term, transient health state. While we demonstrate that unfavorable and ambivalent pregnancy contexts are associated with significant disutility, further research is necessary to quantify potential changes in women’s perception about pregnancy over time, i.e. whether their reported utility scores may differ as pregnancy progresses and after pregnancy ends (post-abortal or postpartum). Additionally, we demonstrate those with favorable pregnancy contexts have higher utility (e.g., mean VAS for all favorable contexts between 0.88–0.91). Understanding the duration of disutility associated with unfavorable pregnancy contexts will further inform future cost-effectiveness analyses. With over 6 million women experiencing pregnancy annually in the U.S. [32], these additional data will be particularly important to help enhance overall population health.
There are several limitations to the current study. Our cohort included women recruited from urban clinics and therefore may not be representative of the general population of pregnant women. However, the geographic area of our study recruitment is similar in demographic characteristics to the overall U.S. population [33] and study participants also demonstrated substantial diversity in sociodemographic characteristics, reproductive history, utility scores, and pregnancy context. Additionally, our sample size was relatively small; however, we observed statistically significant differences in utility scores across levels of pregnancy context, suggesting this is not a material concern. Future studies with a larger sample size could permit further informative analyses, such as sub-analyses to identify specific patient characteristics associated with lower or higher utility among women with the same pregnancy context. For SG and TTO, we did not perform multivariable analysis due to the limited variability in overall scores skewed towards 1.0. Additional research with larger sample sizes would be helpful to validate these findings. We also observed missing values for VAS among 28 participants in our analytic sample, which may be due in part to the self-administered format of the questionnaire and the VAS element inadvertently skipped by respondents. However, our assessment of participant characteristics demonstrated no significant differences between those with VAS measures and those without. Further, while VAS may be most appropriate for use among a pregnancy population with varied pregnancy contexts, its strengths and limitations in measuring health utility has been debated. Compared to choice-based elicitation methods such as SG and TTO, the VAS approach has been criticized for being theoretically limited [34] as a single-scale construct that is not choice-based. Yet others have argued it is theoretically grounded and does incorporate an element of choice that is scaled-based using the VAS line, rather than a choice between two options [35]. Further research validating our findings in other samples, including among women seeking abortion, will provide additional insights regarding the most appropriate measurement of utility for different pregnancy contexts.
5. Conclusion
Among a diverse cohort of women with a recent diagnosis of pregnancy, health utility varied by pregnancy context. Unwanted, unintended, unplanned, not desired, poorly timed or unhappy pregnancies were significantly associated with significant disutility. In addition, women with ambivalent pregnancy contexts also reported considerable disutility. These data provided robust utility scores for specific pregnancy contexts to inform future cost-effectiveness evaluations related to pregnancy. Further research examining potential changes in pregnancy-related utility metrics over time is warranted.
Supplementary Material
Acknowledgements
We would like to extend our sincere thanks to the providers and staff at participating clinical sites in New Haven, CT.
Funding: Dr. Lundsberg and Dr. Gariepy were supported by grants received by Dr. Gariepy (NIH CTSA ULITR000142 and the Albert McKern Scholar Awards for Perinatal Research).
Footnotes
Conflicts of Interest: None.
Appendix A. Supplementary data
Supplementary data to this article can be found online at http://dx.doi.org/10.1016/j.contraception.2017.08.003.
References
- [1].Finer LB, Zolna MR. Declines in unintended pregnancy in the United States, 2008–2011. Med 2016;374:843–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Trussell J, Henry N, Hassan F, Prezioso A, Law A, Filonenko A. Burden of unintended pregnancy in the United States: potential savings with increased use of long-acting reversible contraception. Contraception 2013;87:154–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Sonfield A, Kost K. Public costs from unintended pregnancies and the role ofpublic insurance programs in paying for pregnancy-related care: National and state estimates for 2010. New York: Guttmacher Institute; 2015. Available at: https://www.guttmacher.org/report/public-cos1s-iraintendedpregnancies-and-role-public-insurance-programs-paying-pregnancy. [Google Scholar]
- [4].American College of Obstetricians and Gynecologists (ACOG). Reproductive life planning to reduce unintended pregnancy. ACOG Committee opinion no. 654; 2016. Available at: https://www.acog.org/-/media/Committee-Opinions/Committee-on-Health-Care-for-Under-served-Women/co654.pdf?dmc=l&ts=20170720T0115487640.
- [5].Myers ER. How should we estimate the cost-effectiveness of interventions that affect reproduction? Med Decis Making 2015;35: 812–4. [DOI] [PubMed] [Google Scholar]
- [6].Neumann PJ, Farquhar M, Wilkinson CL, Lowry M, Gold M. Lack of cost-effectiveness analyses to address healthy people 2020 priority areas. Public Health 2016;106:2205–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Torrance GW. Measurement of health state utilities for economic appraisal. J Health Econ 1986;5:1–30. [DOI] [PubMed] [Google Scholar]
- [8].Sonnenberg FA, Burkman RT, Hagerty CG, Speroff L, Speroff T. Costs and net health effects of contraceptive methods. Contraception 2004;69:447–59. [DOI] [PubMed] [Google Scholar]
- [9].Schwarz EB, Smith R, Steinauer J, Reeves MF, Caughey AB. Measuring the effects of unintended pregnancy on women’s quality of life. Contraception 2008;78:204–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Ubel PA, Loewenstein G, Jepson C. Whose quality of life? A commentary exploring discrepancies between health state evaluations of patients and the general public. Qual Life Res 2003;12:599–607. [DOI] [PubMed] [Google Scholar]
- [11].Mumford SL, Sapra KJ, King RB, Louis JF, Buck Louis GM. Pregnancy intentions-a complex construct and call for new measures. Fertil Steril 2016;106:1453–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Aiken AR, Borrero S, Callegari LS, Dehlendorf C. Rethinking the pregnancy planning paradigm: unintended conceptions or unrepresentative concepts? Perspect Sex Reprod Health 2016;48:147–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Gariepy A, Lundsberg LS, Vilardo N, Stanwood N, Yonkers K, Schwarz EB. Pregnancy context and women’s health-related quality of life. Contraception 2017;95:491–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Robinson A, Loomes G, Jones-Lee M. Visual analog scales, standard gambles, and relative risk aversion. Med Decis Making 2001;21:17–27. [DOI] [PubMed] [Google Scholar]
- [15].Bijlenga D, Birnie E, Bonsel GJ. Feasibility, reliability, and validity of three health-state valuation methods using multiple-outcome vignettes on m oderate-risk pregnancy at term. Value Health 2009;12:821–7. [DOI] [PubMed] [Google Scholar]
- [16].Bijlenga D, Bimie E, Mol BW, Bonsel GJ. Obstetrical outcome valuations by patients, professionals, and laypersons: differences within and between groups using three valuation methods. BMC Pregnancy Childbirth 2011. ;11:93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Stevens KJ, McCabe CJ, Brazier JE. Mapping between visual analogue scale and standard gamble data; results from the UK health utilities index 2 valuation survey. Health Econ 2006;15:527–33. [DOI] [PubMed] [Google Scholar]
- [18].van der Pol M, Shiell A. Extrinsic goals and time tradeoff. Med Decis Making 2007;27:406–13. [DOI] [PubMed] [Google Scholar]
- [19].Revicki DA, Kawata AK, Harnam N, Chen WH, Hays RD, Celia D. Predicting EuroQol (EQ-5D) scores from the patient-reported outcomes measurement information system (PROMIS) global items and domain item banks in a United States sample. Qual Life Res 2009;18:783–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Barrett G, Smith SC, Wellings K. Conceptualisation, development, and evaluation of a measure of unplanned pregnancy. J Epidemiol Community Health 2004;58:426–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Brown J, Buxton M. The economic perspective. Br Med Bull 1998;54: 993–1009. [DOI] [PubMed] [Google Scholar]
- [22].Tolley K What are health utilities? Newmarket, U.K.: Hayward Medical Series Publications; 2014. Available at: http://tolleyhealthe-conomics.com/wp-content/uploads/2014/09/What-are-health-utilities-Final.pdf. [Google Scholar]
- [23].Patient reported outcomes measurement information system (PROMIS) assessment center. Scoring PROMIS global short form; 2010.
- [24].Hays RD, Bjomer JB, Revicki DA, Spritzer KL, Celia D. Development of physical and mental health summary scores from the patient-reported outcomes measurement information system (PROMIS) global items. Qual Life Res 2009;18:873–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Arias E United States life tables, 2011 National Vital Statistics Reports; vol 64, no 11. Hyattsville, MD: National Center for Health Statistics; 2015. Available at: https://www.cdc.gov/nchs/data/nvsr/nvsr64/nvsr64_l1.pdf. [PubMed] [Google Scholar]
- [26].Shaheen Lindholm R Lindholm L Quality of life among pregnant women with chronic energy deficiency in rural Bangladesh. Health Policy 2006;78: 128–34. [DOI] [PubMed] [Google Scholar]
- [27].Feeny D, Townsend M, Furlong W, et al. Health-related quality-of-life assessment of prenatal diagnosis: chorionic villi sampling and amniocentesis. Genet Test 2002;6:39–46. [DOI] [PubMed] [Google Scholar]
- [28].Burlone S, Edelman AB, Caughey AB, Trussell J, Dantas S, Rodriguez MI. Extending contraceptive coverage under the affordable care act saves public funds. Contraception 2013;87:143–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Washington CI, Jamshidi R,Thung SF Nayeri UA, Caughey AB, Werner EF. Timing of postpartum intrauterine device placement: a cost-effectiveness analysis. Fertil Steril 2015;103:131–7. [DOI] [PubMed] [Google Scholar]
- [30].Pham CT, Crowther CA. Birth outcomes: utility values that postnatal women, midwives and medical staff express. BJOG 2003;110:121–7. [PubMed] [Google Scholar]
- [31].Smith KJ, Tsevat J, Ness RB, Wiesenfeld HC, Roberts MS. Quality of life utilities for pelvic inflammatory disease health states. Sex Transm Dis 2008;35:307–11. [DOI] [PubMed] [Google Scholar]
- [32].Curtin SA, Abma JC, Ventura SJ, Henshaw SK. Pregnancy rates for U.S. women continue to drop NCHS data brief, no 136. National Center for Health Statistics: Hyattsville, MD; 2013. Available at: https://www.cdc.gov/nchs/data/databriefs/dbl36.pdf. [PubMed] [Google Scholar]
- [33].Kolko J ‘Normal America’ is not a small town of white people. FiveThirtyEight 2016. Available at: https://fivethirtyeight.com/features/normal-america-is-not-a-small-town-of-white-people/.
- [34].Ock M, Park JY, Son WS, Lee HJ, Kim SH, Jo MW. Estimation of utility weights for human papilloma virus-related health states according to disease severity. Health Qual Life Outcomes 2016;14: 163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Parkin D, Devlin N. Is there a case for using visual analogue scale valuations in cost-utility analysis? Health Econ 2006;15:653–64. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.