Abstract
Procedural flow disruptions secondary to interruptions play a key role in error occurrence during complex medical procedures, mainly because they increase mental workload among team members, negatively impacting team performance and patient safety. Since certain types of interruptions are unavoidable, and consequently the need for multitasking is inherent to complex procedural care, this field can benefit from an intelligent system capable of identifying in which moment flow interference is appropriate without generating disruptions. In the present study we describe a novel approach for the identification of tasks imposing low cognitive load and tasks that demand high cognitive effort during real-life cardiac surgeries. We used heart rate variability analysis as an objective measure of cognitive load, capturing data in a real-time and unobtrusive manner from multiple team members (surgeon, anesthesiologist and perfusionist) simultaneously. Using audio-video recordings, behavioral coding and a hierarchical surgical process model, we integrated multiple data sources to create an interactive surgical dashboard, enabling the identification of specific steps, substeps and tasks that impose low cognitive load. An interruption management system can use these low demand situations to guide the surgical team in terms of the appropriateness of flow interruptions. The described approach also enables us to detect cognitive load fluctuations over time, under specific conditions (e.g. emergencies) or in situations that are prone to errors. An in-depth understanding of the relationship between cognitive overload states, task demands, and error occurrence will drive the development of cognitive supporting systems that recognize and mitigate errors efficiently and proactively during high complex procedures.
Keywords: cognitive load, cardiac surgery, heart rate variability, process model
1. Introduction
Recent estimates rank medical errors leading to preventable patient harm as the third cause of death in the U.S. Fifty to 65% of complications experienced by hospitalized patients are procedural in nature and 75% of adverse events occur in the procedure/operating room.[1] Preventable errors leading to error cycles precede 80% of deaths in complex interventional care, and understanding and managing conditions leading to errors is critical to eliminate preventable patient harm.[2] The U.S. Institute of Medicine identified workflow disruptions during complex procedures as a leading contributing factor to medical errors.[3] Procedural flow disruptions secondary to interruptions have been proposed as surrogates for errors, because they increase mental workload and stress of interventional team members, negatively affect mental readiness, impair situational awareness and increase fatigue and frustration. [4]
Surgical flow disruptions play a key role in preventable error generation during complex surgical procedures (e.g. robotic surgery). Wiegmann et al. found a linear relationship between surgical flow disruptions and errors; as the number of disruptions increased, so did the number of errors (r=0.47, p<0.05).[5] A growing body of research in complex systems is aiming at manipulating the timing of information notifications in relationship to the ongoing task to minimize the preventable errors and surgical flow disruptions. [6, 7] Distractions and interruptions decrease focus and divert attention from the current task. The cost of distractions and interruptions have been widely studied in the aviation and transportation industry where it has been shown that interruption decrease performance [8, 9] and increase stress and perceived workload. [10]
In a complex medical procedural environment, the smooth execution of multi-party dependencies often depends on the perfect synchronized coordination among the various members of the healthcare team, the cost of interruptions or distractions can be extremely high. Proper communication and coordination is extremely essential for the successful execution of a complex procedure. Breakdown in the communication workflow, or disruption of the smooth execution of the individual sub-steps can become critical. Therefore, there is a need to decrease peri-procedural distractions and interruptions which can increase the perceived workload among surgeons and impair team performance.[11, 12]
Increase in stress levels increases the probability of making mistakes that can have potentially serious consequences to patient safety.[13] While some distractions such as noise, interruptions from communication devices and external staff may be avoidable, certain interruptions such as clinical clarifications, questions, and requests by the OR staff, may be necessary. For the essential interruptions, unless they are critical, it is important to be able to present them in between the operation steps, when the surgical workload and stress is low. From a Human Computer Interaction perspective this presents new challenges in deciding which machine generated notifications are absolutely critical, and when and how to present them without causing major disruption in the clinical workflow.
In the present study we describe a novel approach for the identification of surgical tasks imposing low vs high cognitive load during real-life cardiac surgeries. We hypothesize that timing interruptions during moments of low mental workload will be less likely to cause flow disruptions vs. interruptions during high workload moments.
2. Methods
In an initial cohort of 10 cardiac surgery cases, we have investigated the cardiac surgery team performing two different complex procedures: coronary artery bypass grafting (CABG) and aortic valve replacement (AVR). Regulatory approvals were obtained by the local Institutional Review Board (IRB), including additional protections for employees as vulnerable subjects. Both patients and staff signed an IRB approved informed consent form and separate authorization for the release of information due to audio/video recording of the procedures.
2.1. Surgical Process Modeling
A surgical team process model for two common cardiac surgery procedures (CABG and AVR) was developed by our group and described in a previous study.[14] Each procedure was segmented in 3 stages, 13-14 steps, 160-180 sub-steps, and approximately 200 tasks. The cardiac surgery process model uses a 4-level hierarchical structure involving four sub(teams): surgeon, anesthesiologist, perfusionist and nurse.
2.2. Audio and Video Recording
Two GoPro cameras (HERO4) were placed in the OR at the room corner and surgical light head, and configured to record an ultra-wide (entire team) and a narrow (surgical field) field of view at 30 frames per second and 960 pixels of video resolution. Three stereo digital voice recorders (Sony ICD-PX440) captured audio at 44.1 KHz/192 Kbps from three team members (surgeon, anesthesiologist and perfusionist) via a lapel microphone. Video and audio files were recorded in MP4 and MP3 formats respectively and synchronized during post-production.
2.3. Heart Rate Variability Analysis (HRV)
HRV is a validated measure of cognitive workload. [15, 16] A heart rate sensor (Polar H7 chest strap) was used to capture beat-to-beat (R-R) intervals from three team members (surgeon, anesthesiologist and perfusionist). We used an ultra-short-term analysis of HRV, calculating the LF/HF ratio for each 1 minute epoch, as validated by previous studies. [17] We have also assessed self-reported cognitive load by applying the SURG-TLX questionnaire immediately after the procedure. [18]
2.4. Dashboard for Interactive Task Analysis
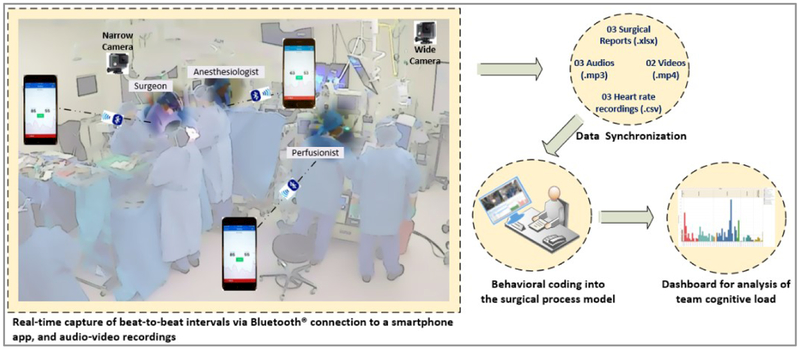
A multisource database was created in Excel (format .xlsx) and connected to a data analytics software (Tableau Desktop, version 10.4), allowing us to build an interactive dashboard. Fig. 1 illustrates our multimodal approach to capture, integrate, synchronize and display data for analysis.
Fig. 1.
Multimodal data embed into the surgical process model.
3. Results
In our initial cohort of 10 cardiac surgery procedures (8 CABG and 2 AVR), HRV parameters presenting statistically significant correlation with the SURG-TLX score were: standard deviation of normal to normal R-R intervals (SDNN) (r = −0.61, p < 0.001), HRV triangulation index (r = −0.69, p < 0.001), maximum low frequency (LF)/ high frequency (HF) ratio (r = 0.55, p < 0.027), and number of episodes that LF/HF ratio was > 2.0 (r = 0.80, p < 0.001).
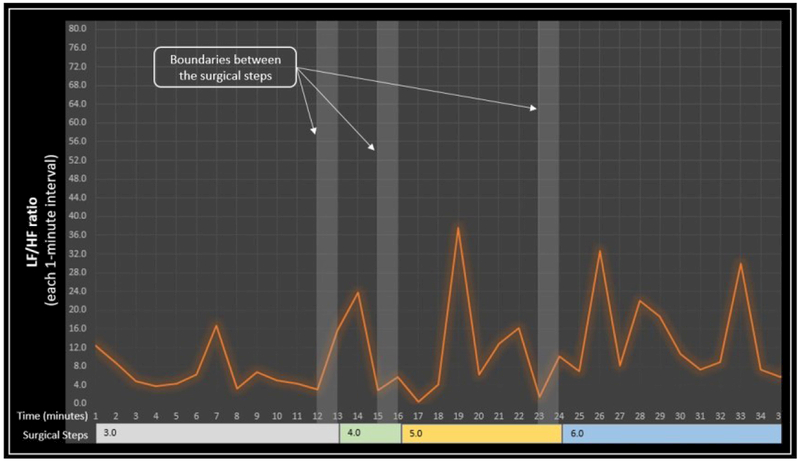
Using HRV LF/HF ratio, we identified multiple moments of low cognitive workload throughout the recorded procedures; these moments seem to coincide with boundaries between tasks (Fig. 2). An interruption management system can time the interruptions required to exchange critical information during moments of low workload. The approach herby described also enables us to detect cognitive load fluctuations over time or in situations that are prone to errors.
Fig. 2.
Identification of moments of low cognitive workload at the boundaries between steps during cardiac surgery.
4. Discussion
Complex procedural care is associated with high need for constant communication and coordination. In a recent systematic review, Rivera-Rodriguez and associates found that interruptions occur frequently in all healthcare settings but especially in complex procedural care and that only relatively few studies examined the cognitive implications of interruptions. [19] Monk et al. have proposed to manipulate the time at which the notification of an information is delivered, relative to the execution of the ongoing task; these Authors proposed that this timing impacts on the cost of the interruption. [20] Bailey and associates have examined changes in mental workload during execution of interactive tasks. [6] They observed that workload exhibits transient decreases at subtask boundaries, corresponding to the completion of large chunks of the task. The majority of disrupting events in complex procedural care are related to information exchanges through communication. Since certain types of interruptions are inherent to complex procedural care, the patient safety field can benefit from an intelligent system capable of identifying in which moment workflow interference has the lowest cost.
There is lack of data describing patterns and distribution of cognitive workload among members of teams engaged in complex surgical procedural care and our ongoing research program is aimed at closing this knowledge gap and enabling new safety approaches. Procedural flow disruptions secondary to interruptions have been proposed as surrogates for errors, because they increase mental workload and stress of interventional team members, negatively affect mental readiness, impair situational awareness and increase fatigue and frustration. Awareness of the critical importance of flow interruptions on the quality of teamwork and their impact on patient outcomes has considerably increased in the last decade. Currently no interruption management system is available to the interventional team. Optimal management of flow interruptions that are required for the acquisition or notification of mission-critical information, may avoid disrupting the workflow and may lead to fewer error cycles and improved patient safety. Influential cyber-human systems research suggests that interrupting tasks during moments of lower mental workload minimizes interruption cost, as transient decrements of mental workload are present at the boundary between tasks, especially after completion of large chunks of the task. This improved understanding of variations in mental workload during complex processes offers a solution to optimally time interruptions of complex medical procedures while minimizing the cost.
Our group has demonstrated that cognitive workload during cardiac surgery procedures can be monitored in near-real time and changes throughout the procedure, alternating peaks of high workload with valleys of low workload. We have also described a context-aware cognitive interface that can predict mental workload in real-time based on physiological data. Fifty-two percent of disrupting events in complex procedural care are related to communication; [5] when individuals are disrupted by an interruption, their attention is shifted away from the primary task to the interruption task. [21] Once this shift of working memory occurs, situation awareness of the primary task begins to decay to “make room” for the process required to deal with the interrupting task; once the primary task is resumed, it is easy for the individual not to remember which part of the primary task was last completed. When attention is shifted away from the primary task, the likelihood of an error occurring upon return to the primary task is increased. Many interruptions however are required to maintain system performance and their high frequency is indicative of the high need for constant communication and coordination in healthcare.
5. Conclusions
We maintain that many medical errors are mental workload problems, that workflow disruptions are surrogates for errors and that, by timing interruptions during moments of low mental workload, the cost of the interruption (i.e. errors) can be minimized
We therefore hypothesize that a context-aware cognitive system could help manage the information flow in the procedural suite and avoid flow disruptions and error cycles leading to patient harm; such system is predicated upon monitoring changes in mental workload in real-time and delivering interruptions and notifications at the appropriate time.
Acknowledgements.
The authors wish to acknowledge the contribution, dedication and commitment to excellence of the cardiac surgery team and operating room staff at the VA Boston Healthcare System. Research reported in this publication was supported by the National Heart, Lung, and Blood Institute of the National Institutes of Health under award number 1R01HL126896-01A1. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- 1.Makary MA, Daniel M: Medical error-the third leading cause of death in the US. BMJ 2016, 353:i2139. [DOI] [PubMed] [Google Scholar]
- 2.Gawande AA, Zinner MJ, Studdert DM, Brennan TA: Analysis of errors reported by surgeons at three teaching hospitals. Surgery 2003, 133(6):614–621. [DOI] [PubMed] [Google Scholar]
- 3.Stefl ME: To Err is Human: Building a Safer Health System in 1999. Front Health Serv Manage 2001, 18(1): 1–2. [PubMed] [Google Scholar]
- 4.Weigl M, Stefan P, Abhari K, Wucherer P, Fallavollita P, Lazarovici M, Weidert S, Euler E, Catchpole K: Intra-operative disruptions, surgeon’s mental workload, and technical performance in a full-scale simulated procedure. Surg Endosc 2016, 30(2):559–566. [DOI] [PubMed] [Google Scholar]
- 5.Wiegmann DA, ElBardissi AW, Dearani JA, Daly RC, Sundt TM: Disruptions in surgical flow and their relationship to surgical errors: an exploratory investigation. Surgery 2007, 142(5):658–665. [DOI] [PubMed] [Google Scholar]
- 6.Bailey BP, Iqbal ST: Understanding changes in mental workload during execution of goal-directed tasks and its application for interruption management. ACM Trans Comput-Hum Interact 2008, 14(4): 1–28. [Google Scholar]
- 7.Miyata Y, Norman DA: Psychological issues in support of multiple activities In: User centered system design. Hillsdale, NJ: Lawrence Erlbaum Associates, INC; 1986: 265–284. [Google Scholar]
- 8.Latorella KA: Effects of Modality on Interrupted Flight Deck Performance: Implications for Data Link. Proceedings of the Human Factors and Ergonomics Society Annual Meeting 1998, 42(1):87–91. [Google Scholar]
- 9.Oulasvirta A, Saariluoma P: Surviving task interruptions: Investigating the implications of long-term working memory theory. International Journal of Human-Computer Studies 2006, 64(10):941–961. [Google Scholar]
- 10.Chen Y: Stress State of Driver: Mobile Phone Use While Driving. Procedia - Social and Behavioral Sciences 2013, 96:12–16. [Google Scholar]
- 11.Wheelock A, Suliman A, Wharton R, Babu ED, Hull L, Vincent C, Sevdalis N, Arora S: The Impact of Operating Room Distractions on Stress, Workload, and Teamwork. Ann Surg 2015, 261(6):1079–1084. [DOI] [PubMed] [Google Scholar]
- 12.Arora S, Hull L, Sevdalis N, Tierney T, Nestel D, Woloshynowych M, Darzi A, Kneebone R: Factors compromising safety in surgery: stressful events in the operating room. Am JSurg 2010, 199(1):60–65. [DOI] [PubMed] [Google Scholar]
- 13.Arora S, Sevdalis N, Nestel D, Woloshynowych M, Darzi A, Kneebone R: The impact of stress on surgical performance: a systematic review of the literature. Surgery 2010, 147(3):318–330, 330.e311–316. [DOI] [PubMed] [Google Scholar]
- 14.Dias R, Zenati M, Conboy H, Gabany J, Arney D, Goldman J, Osterweil L, Avrunin G, Clarke L, Yule S: Embedding Real-Time Measure of Surgeons’ Cognitive Load into Cardiac Surgery Process Modeling In: Academic Surgical Congress: 2018; Jacksonville, FL, USA; 2018. [Google Scholar]
- 15.Dias RD, Ngo-Howard MC, Boskovski MT, Zenati MA, Yule SJ: Systematic review of measurement tools to assess surgeons’ intraoperative cognitive workload. British Journal of Surgery 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Thayer JF, Hansen AL, Saus-Rose E, Johnsen BH: Heart rate variability, prefrontal neural function, and cognitive performance: the neurovisceral integration perspective on self-regulation, adaptation, and health. Ann Behav Med 2009, 37(2):141–153. [DOI] [PubMed] [Google Scholar]
- 17.Baek HJ, Cho CH, Cho J, Woo JM: Reliability of ultra-short-term analysis as a surrogate of standard 5-min analysis of heart rate variability. Telemed J E Health 2015, 21(5):404–414. [DOI] [PubMed] [Google Scholar]
- 18.Wilson MR, Poolton JM, Malhotra N, Ngo K, Bright E, Masters RS: Development and validation of a surgical workload measure: the surgery task load index (SURG-TLX). World J Surg 2011, 35(9):1961–1969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rivera-Rodriguez AJ, Karsh BT: Interruptions and distractions in healthcare: review and reappraisal. Qual Saf Health Care 2010, 19(4):304–312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Monk CA, Boehm-Davis DA, Trafton JG: The Attentional Costs of Interrupting Task Performance at Various Stages. Proceedings of the Human Factors and Ergonomics Society Annual Meeting 2002, 46(22):1824–1828. [Google Scholar]
- 21.Flin R, Youngson G, Yule S: Enhancing Surgical Performance. Boca Raton, FL, US: CRC Press; 2016. [Google Scholar]