Abstract
Objective:
Emotional overeating and loss-of-control eating are associated with poorer weight- related and psychiatric outcomes, yet our understanding of the relationship between these variables is limited, particularly among individuals in primary care. This study examined the frequency of emotional overeating and relationship with loss-of-control eating among patients with and without binge-eating disorder (BED) seeking weight loss treatment in primary care.
Method:
Participants were 131 adults (n=105 female) with overweight/obesity seeking weight loss treatment in primary care. Participants completed the Eating Disorder Examination (semistructured interview) and Yale Emotional Overeating Scale, which measures emotional overeating episodes. Height and weight were measured. Mean age and BMI were 47.60 years and 35.31 kg/m2, respectively. BED criteria were met by n=35 (26.7%) participants.
Results:
Participants with BED endorsed more frequent emotional overeating episodes compared to those without BED. While total emotional overeating scores were not associated with loss-of- control eating, discrete emotions of emotional overeating (e.g., loneliness) were associated with loss-of-control eating. Emotional overeating was most often reported in response to loneliness, boredom, or anxiety, which varied by BED status.
Conclusions:
Most participants endorsed recent episodes of emotional eating. Future research examining the impact of emotional eating on weight loss treatment outcomes is warranted.
Keywords: emotional eating, binge eating, binge-eating disorder, primary care, obesity, overweight
1. Introduction
Emotional eating is defined as the tendency to eat in response to negative emotions [1–3]. For example, this could include emotional antecedents such as feeling anxious or bored. Previous studies have documented that greater emotional eating is correlated with a higher body mass index (BMI), more weight gain, and increased weight fluctuation [4, 5]. The majority of studies of emotional eating, however, have been conducted with specialty eating disorder clinic samples [6–9], which may not generalize to the larger proportion of individuals with overweight or obesity, such as those seeking weight loss treatment in a primary care setting [10]. To date, only one study has examined emotional eating in a primary care sample and results indicated that emotional eating was common (approximately 50% of the sample of patients with obesity) [10].
The most commonly used assessments of emotional eating (used in the studies described above) possess two major limitations. First, one such measure assesses the ‘urge’ or ‘need’ to eat in response to emotions, as opposed to the actual act of eating itself in response to emotion. This distinction is important as the urge or need to eat may not result in actual emotional eating episodes [11]. Second, research on emotional eating has largely focused on negative affect broadly as an antecedent to eating, and the evidence of specific discrete emotions (e.g., guilt, happiness) and eating has been inconsistent [12]. Notably, a recent investigation found that eating in response to positive emotions (unlike negative emotions) was not associated with negative outcomes (e.g., eating disorder psychopathology, poor psychological well-being) in adults with overweight/obesity [13]. More research is needed, however, to determine whether greater frequency of eating in response to discrete negative emotions (e.g., boredom, anger) are associated with poorer psychiatric comorbidities as this could help inform weight loss treatment. The Yale Emotional Overeating Questionnaire (EOQ) [6] was developed in part to address the aforementioned limitations and was designed to assess the frequency of actual overeating episodes (i.e., as opposed to the urge or need to do so) in response to a variety of discrete emotions, including negative and positive emotions (e.g., anxiety, boredom, happiness). The EOQ was validated in a sample of adults with overweight or obesity and binge-eating disorder (BED) who were seeking treatment for weight loss and binge eating at a specialty clinic [6].
Studies examining individuals with overweight or obesity have also found significantly higher emotional eating among those with BED compared to individuals with subthreshold BED [8] or without BED [7–9, 14, 15]. BED is a recognized eating disorder diagnosis in the Diagnostic and Statistical Manual of Mental Disorders-fifth edition. A diagnosis of BED is defined by eating an unusually large amount of food in a short period of time, paired with a selfreported sense of loss-of-control at least once weekly during the previous three months, accompanied by marked distress related to the binge episodes but without regular compensatory behaviors as with bulimia nervosa [16]. Lifetime estimates of BED rates range from 0.85 to 2.6% [17–19]. BED is associated with obesity, significant medical and psychiatric comorbidities, such as type II diabetes and depression [17, 20], and is common within primary care settings [21]. Despite the prevalence of BED and the fact that BED confers unique health risks beyond obesity alone [20], many primary care physicians lack knowledge regarding the symptoms of BED or are unfamiliar with the diagnosis, and BED is often unrecognized and untreated in primary care [22].
Another possible reason BED may be overlooked in primary care settings could be the inherent subjectivity and difficulty assessing a “binge” episode, such as determining what is considered an “usually large” amount of food [23]. Consequently, recent research has examined loss-of-control eating more broadly. In fact, research suggests that experiencing loss-of-control eating is uniquely associated with distress, impairment, and dysfunctional eating, regardless of a person’s weight status or the amount of food consumed [24, 25]. Moreover, it has been argued that loss-of-control appears to be the most salient binge eating feature [26] and past studies have found that the size of a binge does not distinguish between demographic (e.g., sex) or clinical characteristics (e.g., psychiatric symptoms, eating disorder psychopathology). See Wolfe et al., 2009 for a review. We are unaware of any studies examining the frequency of emotional overeating episodes as it relates to loss-of-control eating or comparing how this potential relationship may differ between individuals with and without BED.
Taken together, both emotional overeating and loss-of-control eating are strongly associated with poorer weight-related and psychiatric outcomes. The relationship between these critical variables, however, is unknown and may have important implications for informing weight loss treatments. Existing literature is limited to specialty clinics, which may not be representative of the general proportion of individuals with overweight or obesity, such as those within primary care settings. Additionally, more research is needed to discern the exact nature of actual emotional overeating (versus urges to do so) and loss-of-control eating in response to discrete emotions. The aims of this investigation were as follows: 1. Examine the frequency of overall and discrete emotional overeating episodes in adults seeking weight loss treatment in a primary care setting. 2. Examine the association between emotional overeating episodes and eating disorder psychopathology. 3. Compare differences in overall and discrete emotional overeating episodes between individuals diagnosed with and without BED. 4. Examine the relationship between overall and discrete emotional overeating episodes and loss-of-control eating and emotional overeating. We hypothesized that emotional overeating episodes would be associated with eating disorder psychopathology and that individuals diagnosed with BED would report more frequent emotional overeating and endorse a greater number of discrete emotions during which they overeat, compared to those without BED. Furthermore, we hypothesized that greater emotional overeating episodes in response to negative emotions would be related to more loss-of-control eating.
2. Method
2.1. Participants
Participants include 131 adults in the overweight or obese range (≥25-≤55) seeking treatment for weight loss in primary care. All participants were recruited within a primary care setting at an urban university-based medical healthcare center (see [27–29] for more detailed procedures). Participants were excluded if they were over the age of 65, had severe psychiatric (e.g., schizophrenia) or medical problems (e.g., cardiac disease), were pregnant/breastfeeding, or had uncontrolled liver or thyroid disease, hypertension, or diabetes. Most participants were female (n=105; 80.2%) and 61.8% identified as non-Hispanic White (n=81). The mean age was 47.60 years old (SD=10.49) and the mean current BMI was 35.31 kg/m2 (SD=6.54). A total of 35 participants (26.7%) of the total sample met BED criteria.
2.2. Measures
Participants were assessed with the Eating Disorder Examination (EDE), a semistructured interview of eating-disorder symptomatology [30]. The EDE is the best-established interview of eating-disorder symptomatology and is used as the primary assessment tool in treatment studies to diagnose BED [31]. Past psychometric studies have demonstrated reliability and validity, including support in differentiating between cases and non-cases of eating disorders [32]. For this investigation, loss-of-control eating frequency (LOC Eating Episodes) was calculated with the sum of eating episodes in the past 28 days during which participants reported experiencing a sense of loss-of-control, regardless of the amount consumed. The subscales of the EDE include Restraint, Eating Concern, Shape Concern, Weight Concern, and a Global Score.
Participants also completed the Yale Emotional Overeating Questionnaire (EOQ) [6], a 9-item self-report measure designed to assess the frequency of emotional overeating. Participants were asked to rate the frequency that they experienced actual Emotional Overeating in response to 9 discrete emotions (i.e., EOQ-Anxiety, EOQ-Sadness, EOQ-Loneliness, EOQ-Tiredness, EOQ-Anger, EOQ-Happiness, EOQ-Boredom, EOQ-Guilt, and EOQ-Pain) during the past 28 days on a 7-point Likert scale (0 = No days, 1 = 1–5 days, 2 = 6–12 days, 3 = 13–15 days, 4 = 1622 days, 5 = 23–27 days, 6 = Every day). For example, “On how many of days out of the past 28 days have you eaten an unusually large amount of food given the circumstances in response to feelings of ANXIETY (worry, stress, nervousness)?” These 9-items are combined and averaged to comprise a total score indicating overall emotional overeating frequency during the past 28 days (EOQ-Total). To replicate the analyses conducted by Gianini et al. [33], we also totaled the 8 negative emotions only (e.g., anger) to create a EOQ-Negative Emotions variable. The current Cronbach’s alpha for the EOQ-Total was 0.89. Height was measured using a wall measure and weight was measured using a large-capacity digital scale. Measured height and weight were used to calculate BMI.
2.3. Procedures
This study received approval from the University Institutional Review Board and all participants provided consent. Participants were assessed for BED by master- or doctoral-level clinicians who were trained in eating/weight disorders using the EDE to diagnose BED (based on DSM-5 criteria).
2.4. Data Analysis
Independent samples t-tests were conducted to compare participants diagnosed with BED to participants without BED (i.e., NBO) for all continuous variables (e.g., age, LOC Eating Episodes) and chi-square analyses were used to compare the groups on sex and race. A series of analyses of covariance (ANCOVAs) were performed to adjust for age and BMI, due to significant differences between individuals with and without BED on these variables. Bivariate correlations were conducted to examine the associations between the EOQ Total and 9 EOQ discrete emotion items that comprise the EOQ-Total, and LOC Eating Episodes, EDE Global and subscales, and BMI.
3. Results
There were no significant group differences based on sex or race/ethnicity; however, participants with BED were significantly younger (t(129) = 2.58, p = .011) and had a significantly higher average BMI (t(129) = −2.94, p = .004) compared to the NBO group (see Table 1 for means and standard deviations). BMI, however, was unrelated to EOQ-Total scores or any of the 9 EOQ discrete emotion items.
Table 1.
Means and standard deviations of Age, BMI, Emotional Overeating, and bivariate correlations with LOC Eating Episodes by group
| Total Sample (N = 129) |
BED (n = 35) |
BED (n = 35) |
NBO (n = 96) |
NBO (n = 96) |
Comparison | Significance | |
|---|---|---|---|---|---|---|---|
| M (SD) | M (SD) | LOC Episodes (r) | M (SD) | LOC Episodes (r) |
ANCOVA (F) |
p-value | |
| Age | 47.60 (10.49) | 43.77 (10.62) | −0.203 | 49.00 (10.14) | −0.018 | - | - |
| BMI | 35.31 (6.54) | 38.01 (7.11) | 0.360* | 34.33 (6.07) | −0.076 | - | - |
| EOQ Total Score | 0.67 (0.86) | 1.12 (0.93) | 0.327 | 0.50 (0.77) | 0.124 | 10.73 | .001 |
| EOQ Negative Emotions | 0.36 (0.31) | 0.53 (0.29) | 0.084 | 0.29 (0.30) | 0.182 | 14.67 | .001 |
| Anxiety | 0.90 (1.37) | 1.46 (1.70) | 0.446** | 0.69 (1.16) | 0.233* | 7.07 | .009 |
| Sadness | 0.80 (1.23) | 1.29 (1.38) | 0.330 | 0.62 (1.13) | 0.250* | 4.88 | .029 |
| Loneliness | 0.85 (1.42) | 1.77 (1.78) | 0.336* | 0.51 (1.10) | 0.023 | 18.61 | <.0001 |
| Tiredness | 0.71 (1.25) | 1.26 (1.52) | 0.396* | 0.51 (1.08) | 0.116 | 6.94 | .01 |
| Anger | 0.47 (0.95) | 0.74 (1.01) | 0.026 | 0.36 (0.91) | 0.153 | 2.41 | .123 |
| Happiness | 0.71 (1.19) | 1.17 (1.58) | 0.011 | 0.54 (0.96) | −0.013 | 5.44 | .021 |
| Boredom | 0.99 (1.41) | 1.57 (1.72) | 0.317 | 0.78 (1.22) | −0.020 | 4.53 | .035 |
| Guilt | 0.45 (1.10) | 0.66 (1.28) | −0.189 | 0.37 (1.03) | 0.038 | 1.77 | .186 |
| Pain | 0.14 (0.43) | 0.17 (0.45) | −0.082 | 0.13 (0.42) | 0.027 | 1.21 | .275 |
Note. BED = patients with binge-eating disorder; NBO = patients without binge-eating disorder; BMI = Body Mass Index; EOQ = Emotional Overeating Questionnaire; EOQ-Negative Emotions = EOQ Negative Emotions items averaged. EOQ scores range from 0 to 6; 0 = No days, 1 = 1–5 days, 2 = 6–12 days, 3 = 12–15 days, 4 = 16–22 days, 5 = 23–27 days, 6 = Every day
p<.05
p<01
3.1. Frequency of Emotional Overeating and Association with Eating Disorder Psychopathology
Most participants reported at least an average of 1–5 days of Emotional Overeating in the past month (n = 97, 75.2%), while approximately 24.8% (n = 32) of participants denied any Emotional Overeating days during the past month (see Table 1). When examining the overall sample, participants reported Emotional Overeating most often in response to feelings of EOQ- Boredom, however, the BED group reported Emotional Overeating most often in response to feelings of EOQ-Loneliness, which was followed by EOQ-Boredom, and EOQ-Anxiety; the NBO group reported Emotional Overeating most often in response to EOQ-Boredom, EOQ- Anxiety, and EOQ-Sadness (See Figure 1 to examine frequencies of participants who endorsed Emotional Overeating in response to the 3 most frequently endorsed emotions).
Figure 1.
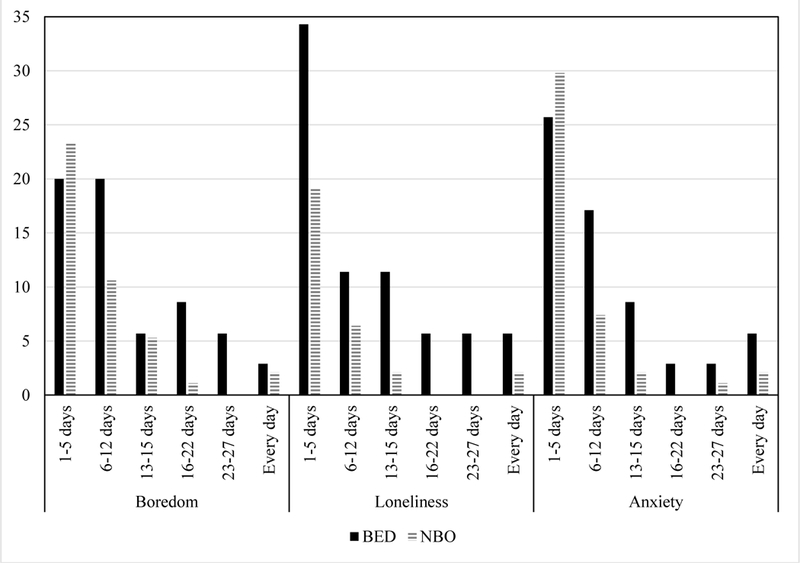
Frequencies of Participants who Endorsed Emotional Overeating in Response to Boredom, Loneliness, and Anxiety During the Past 28 Days
Note. BED=patients with Binge Eating Disorder; NBO=patients without Binge Eating Disorder. Boredom: n = 67; Loneliness: n = 75; Anxiety: n = 69. Participants who reported no days of Emotional Overeating are not included in the above figure.
In the total sample, the EOQ-Total score was significantly positively correlated with EDE-Global scores (see Table 2). Additionally, EOQ-Total scores were significantly positively correlated with several EDE subscales including Eating Concern, Shape Concern, and Weight Concern (correlations ranged from .29-.52). The EOQ-Total score was not associated with EDE Restraint scores.
Table 2.
Bivariate correlations of Emotional Overeating and Eating Disorder Psychopathology
| 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|
| 1 EOQ Total Score | - | |||||
| 2 EDE-Restraint | .07 | - | ||||
| 3 EDE-Eating Concern | .52* | .29* | - | |||
| 4 EDE-Shape Concern | .42* | .28* | .54* | - | ||
| 5 EDE-Weight Concern | .29* | .36* | .48* | .72* | - | |
| 6 EDE-Global | .43* | .60* | .73* | .86* | .85* | - |
Note. EOQ = Emotional Overeating Questionnaire. EDE = Eating Disorder Examination.
p <.01
3.2. Comparison of Emotional Overeating by BED status
Participants with BED reported significantly higher overall EOQ-Total and EOQ- Negative Emotions scores compared to the NBO group (see Table 1). Participants with BED also reported significantly more frequent Emotional Overeating in response to 7 of 9 specific emotions assessed: EOQ-Anxiety, EOQ-Sadness, EOQ-Loneliness, EOQ-Tiredness, EOQ- Anger, EOQ-Happiness, and EOQ-Boredom. No significant differences between groups emerged when examining EOQ-Guilt or EOQ-Pain. After adjusting for age and BMI, the overall pattern of findings did not change, except that there were no longer significant group differences for EOQ-Anger.
3.3. Associations between Emotional Overeating and LOC Eating Episodes by BED status
On average, participants reported 9.68 (SD = 17.39) LOC Eating Episodes in the past month, and individuals with BED (M = 22.14, SD = 28.34) reported a greater frequency of LOC Eating Episodes when compared to the NBO group (M = 5.14, SD = 6.94), t(35.50) = −3.51, p = .001. The correlations between LOC Eating Episodes and the EOQ-Total were not significant for either group (see Table 1). Among participants with BED, greater LOC Eating Episodes were significantly and positively correlated with Emotional Overeating in response to EOQ-Anxiety, EOQ-Loneliness, and EOQ-Tiredness. In the NBO group, greater LOC Eating Episodes were significantly correlated with EOQ-Anxiety and EOQ-Sadness.
4. Discussion
The present investigation examined the frequency of emotional overeating and the relationship with eating disorder psychopathology among patients with and without BED seeking weight loss treatment in primary care. Our findings suggest that most of these individuals experienced emotional overeating in the past month. Overall, participants reported emotional overeating most often in response to boredom, whereas participants diagnosed with BED reported overeating most often in response to feelings of loneliness. Additionally, individuals with BED reported greater frequency of actual emotional overeating when compared to those without BED, similar to previous research reporting more frequent urges to engage in emotional overeating among those with BED [7–9, 14, 15]. More specifically, individuals with BED also reported more episodes of emotional overeating in response to feelings of anxiety, sadness, loneliness, tiredness, happiness, and boredom when compared to those without BED. Finally, the relationship between discrete emotions of emotional overeating and loss-of-control eating frequency varied by group status. Among participants with BED, greater loss-of-control eating was associated with overeating in response to anxiety, loneliness, and tiredness, whereas greater loss-of-control eating was associated with only anxiety and sadness in the NBO group. Our findings add and extend to the existing literature by examining discrete emotional overeating episodes, loss-of-control eating, as well as group differences among those with and without diagnosed BED in primary care.
While most participants reported episodes of emotional overeating in the past month, the overall average frequency of emotional overeating (as assessed with the EOQ-Total) in the current study was lower than reported in previous studies using the EOQ. For instance, the initial validation study of the EOQ was conducted in a sample of patients with an overweight BMI seeking treatment for binge eating, and the overall mean of the sample was 2.29 (SD = 4.44) [6]. Likewise, the mean of the EOQ was much higher (M = 1.46, SD = 1.54) in a sample of Veterans seeking treatment for weight loss [34] and in a sample of post-bariatric surgery patients seeking treatment for loss-of-control eating (M = 1.11, SD = 1.07) [35]. These average differences may be due to variability of the clinical samples. To date, no studies have determined a clinical cutpoint of emotional eating based on the EOQ, which is an important future direction for research.
The frequent occurrence of emotional overeating in response to boredom identified in this study is consistent with prior research findings. The urge to eat in response to boredom was the most common emotion endorsed when compared to other emotions assessed (e.g., anxiety, anger, depression) in a study of undergraduate students [36] and boredom was also the most common antecedent of binge eating identified in a sample of students with subthreshold BED [37]. Results also suggest that overeating in response to loneliness is relatively common among adults diagnosed with BED, consistent with past research on loneliness and social isolation in individuals with BED [6, 38]. This finding is particularly notable given the recent research indicating that experiencing loneliness is associated with poor health-related outcomes [39]. Moreover, a recent meta-analysis suggests that loneliness is a significant risk factor for mortality, finding a 26% increased likelihood of death after controlling for multiple established covariates (e.g., depression, smoking) [40]. This meta-analysis indicated that the risk of mortality related to lack of social relationships was greater than the previously identified mortality risks associated with obesity [40]. Given the established health risks associated with BED, more research is needed to discern whether adults who overeat in response to loneliness are at greater risk for medical or health-related complications.
Interestingly, overeating in response to feelings of happiness was also more frequent in individuals with BED compared to those without. Despite limited research attention, there are several possible reasons to indicate why positive emotions might also be related to the consumption of highly palatable foods or overeating in addition to eating in response to negative emotions. For example, this could include cultural and social factors, as food is often used to celebrate events, such as birthdays and weddings [41]. Additionally, eating in response to positive emotions was not associated with negative outcomes (e.g., eating disorder psychopathology, poor psychological well-being) in adults with overweight/obesity in a previous study [13]. Consistent with these findings, overeating in response to positive emotion (i.e., happiness) was not associated with greater loss-of-control eating in the present investigation.
Similarly, overall EOQ scores (reflecting an average across all the discrete emotions assessed) and overall negative emotions EOQ scores (reflecting an average across only discrete negative emotions assessed) were not associated with greater loss-of-control eating, whereas certain discrete emotional overeating episodes (e.g., anxiety, loneliness) were related to loss-of- control eating depending on BED status. Taken together, these findings highlight the need for examining discrete emotions within research on emotional eating given that overall scores may overlook important findings. Future studies should examine whether greater frequency of emotional eating in response to discrete emotions is associated with poorer treatment outcomes (including weight and binge eating), ideally in a larger sample of patients with BED.
These preliminary results have implications for primary care providers who are tasked with screening for disordered eating. Determining what constitutes a binge episode based on the criteria of an “unusually large” amount of food and a subjective “lack of control” requires extensive clinician training. Given the difficulty in diagnosing BED and that BED often is overlooked in busy primary care environments [23], primary care providers could potentially screen for emotional overeating by asking patients if they overeat when feeling bored, lonely, or anxious, as it might be a signal for more problematic eating behavior, at least among primary care patients interested in weight loss. Patients’ responses could provide clinically useful information to aid in treatment planning and determining if referrals for disordered eating treatment may be needed. It has been argued that brief assessments of disordered eating may be preferable in the primary care setting compared to the exhaustive and comprehensive assessment involved in determining BED diagnosis [23].
The findings of the present study provide preliminary evidence that overeating in response to negative emotions is related to greater eating-disorder psychopathology among individuals in a primary care setting seeking treatment for weight loss. The standard lifestyle treatment for overweight and obesity, behavioral weight loss (BWL), teaches patients skills to achieve weight loss by modifying eating habits and increasing physical activity [42]. While BWL generally produces modest weight loss, many participants do not achieve their goal weight by the end of treatment and weight regain is common [42]. Furthermore, BWL programs have been criticized for not adequately targeting stress management [43] and research suggests that eating in response to internal cues, such as thoughts and emotions is a significant predictor of weight regain [44]. Nascent research suggests that reduction of emotional eating over the course of treatment for weight loss was associated with greater weight loss success [45]. Consequently, more research is needed to explore considerations for tailoring standard treatment approaches for weight loss to more adequately address emotional eating.
There are some limitations worth noting to the present investigation. Given the crosssectional nature of these findings, firm conclusions about directionality cannot be drawn. Additionally, all participants were adults with overweight and obesity seeking weight loss treatment in the primary care setting, and the majority of participants were female and white — thus generalizability is limited. Further, all participants were seeking weight loss treatment and the frequency of emotional eating among primary care patients not seeking treatment is not yet known. Another limitation is the small sample size of patients diagnosed with BED compared to those without BED, and it is possible that null findings for individuals with BED were a result of limited power.
In summary, results of the present investigation suggest that overeating in response to negative and positive emotions is present among most individuals seeking weight loss treatment in primary care. Emotional overeating occurs most often in response to feelings of loneliness, boredom, and anxiety, and appears to be more frequent among individuals with BED. Overall emotional overeating was associated with greater disordered symptoms but not loss-of-control eating. When examining emotional overeating in response to discrete emotions, however, loss- of-control eating was related to anxiety, sadness, loneliness, and tiredness (depending on BED status). Primary care providers may wish to initially briefly assess for emotional eating to determine if referrals may be appropriate. Future research is needed to determine whether reduction in emotional overeating impacts weight loss outcomes in primary care patients.
Acknowledgments
Funding: This work was supported by the National Institutes of Health through the National Institute of Diabetes and Digestive Kidney Diseases [RDB: R03-DK10400801A1 and K23- DK092279]
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- [1].Arnow B, Kenardy J and Agras WS. The Emotional Eating Scale: the development of a measure to assess coping with negative affect by eating. Int J Eat Disord 1995;18:79–90. [DOI] [PubMed] [Google Scholar]
- [2].Macht M How emotions affect eating: a five-way model. Appetite 2008;50:1–11. [DOI] [PubMed] [Google Scholar]
- [3].Van Strien T, Rookus MA, Bergers GP, Frijters JE, Defares PB. Life events, emotional eating and change in body mass index. Int J Obes 1986;10:29–35. [PubMed] [Google Scholar]
- [4].Keller C and Siegrist M. Ambivalence toward palatable food and emotional eating predict weight fluctuations. Results of a longitudinal study with four waves. Appetite 2015;85:138–45. [DOI] [PubMed] [Google Scholar]
- [5].Koenders PG and van Strien T. Emotional eating, rather than lifestyle behavior, drives weight gain in a prospective study in 1562 employees. J Occup Environ Med 2011;53:1287–93. [DOI] [PubMed] [Google Scholar]
- [6].Masheb RM and Grilo CM. Emotional overeating and its associations with eating disorder psychopathology among overweight patients with binge eating disorder. Int J Eat Disord 2006;39:141–6. [DOI] [PubMed] [Google Scholar]
- [7].Pinaquy S, Chabrol H, Simon C, Louvet JP and Barbe P. Emotional eating, alexithymia, and binge-eating disorder in obese women. Obesity research 2003;11:195–201. [DOI] [PubMed] [Google Scholar]
- [8].Ricca V, Castellini G, Lo Sauro C, Ravaldi C, Lapi F, Mannucci E, et al. Correlations between binge eating and emotional eating in a sample of overweight subjects. Appetite 2009;53:418–21. [DOI] [PubMed] [Google Scholar]
- [9].Zeeck A, Stelzer N, Linster HW, Joos A and Hartmann A. Emotion and eating in binge eating disorder and obesity. Eur Eat Disord Rev 2011;19:426–37. [DOI] [PubMed] [Google Scholar]
- [10].Chacko SA, Chiodi SN and Wee CC. Recognizing disordered eating in primary care patients with obesity. Prev Med 2015;72:89–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Opolski M, Chur-Hansen A, Wittert G. The eating-related behaviours, disorders and expectations of candidates for bariatric surgery. Clin Obes 2015;5:165–97. [DOI] [PubMed] [Google Scholar]
- [12].Nicholls W, Devonport TJ and Blake M. The association between emotions and eating behaviour in an obese population with binge eating disorder. Obes Rev 2016;17:30–42. [DOI] [PubMed] [Google Scholar]
- [13].Braden A, Musher-Eizenman D, Watford T and Emley E. Eating when depressed, anxious, bored, or happy: Are emotional eating types associated with unique psychological and physical health correlates? Appetite 2018;125:410–417. [DOI] [PubMed] [Google Scholar]
- [14].Davis C, Levitan RD, Carter J, Kaplan AS, Reid C, Curtis C, et al. Personality and eating behaviors: a case-control study of binge eating disorder. Int J Eat Disord 2008;41:243–50. [DOI] [PubMed] [Google Scholar]
- [15].Schulz S and Laessle RG. Stress-induced laboratory eating behavior in obese women with binge eating disorder. Appetite 2012;58:457–61. [DOI] [PubMed] [Google Scholar]
- [16].American Psychiatric Association. Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Association, 2013. [Google Scholar]
- [17].Hudson JI, Hiripi E, Pope HG Jr. and Kessler RC. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biol Psychiatry 2007;61:348–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Kessler RC, Berglund PA, Chiu WT, Deitz AC, Hudson JI, Shahly V, et al. The prevalence and correlates of binge eating disorder in the World Health Organization World Mental Health Surveys. Biol Psychiatry 2013;73:904–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Udo T, Grilo CM Prevalence and correlates of DSM-5 eating disorder in nationally representative sample of United States adults. Biol Psychiatry in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Hudson JI, Lalonde JK, Coit CE, Tsuang MT, McElroy SL, Crow SJ, et al. Longitudinal study of the diagnosis of components of the metabolic syndrome in individuals with binge-eating disorder. Am J Clin Nutr 2010;91:1568–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Johnson JG, Spitzer RL and Williams JB. Health problems, impairment and illnesses associated with bulimia nervosa and binge eating disorder among primary care and obstetric gynaecology patients. Psychol Med 2001;31:1455–66. [DOI] [PubMed] [Google Scholar]
- [22].Cummins LH, Dunn EC, Rabin L, Russo J, Comtois KA and McCann BS. Primary Care Provider Familiarity with Binge Eating Disorder and Implications for Obesity Management: A Preliminary Survey. Journal of Clinical Psychology in Medical Settings 2003;10:51–56. [Google Scholar]
- [23].Saules KK, Carey J, Carr MM and Sienko RM. Binge-eating disorder: prevalence, predictors, and management in the primary care setting. J Clin Outcome Manag 2015;22. [Google Scholar]
- [24].Colles SL, Dixon JB, O’Brien PE. Loss of control is central to psychological disturbance associated with binge eating disorder. Obesity 2008;16:608–14. [DOI] [PubMed] [Google Scholar]
- [25].Goldschmidt AB. Are loss of control while eating and overeating valid constructs? A critical review of the literature. Obes Rev 2017;18:412–449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Vannucci A, Theim KR, Kass AE, Trockel M, Genkin B, Rizk M, et al. What constitutes clinically significant binge eating? Association between binge features and clinical validators in college-age women. Int J Eat Disord 2013;46:226–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Barnes RD, Ivezaj V, Martino S, Pittman BP and Grilo CM. Back to basics? No weight loss from motivational interviewing compared to nutrition psychoeducation at one-year follow-up. Obesity 2017;25:2074–2078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Barnes RD, Ivezaj V, Martino S, Pittman BP, Paris M and Grilo CM. Examining motivational interviewing plus nutrition psychoeducation for weight loss in primary care. J Psychosom Res 2018;104:101–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Barnes RD, White MA, Martino S, Grilo CM. A randomized controlled trial comparing scalable weight loss treatments in primary care. Obesity 2014;22:2508–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Fairburn CG, Cooper Z. The eating disorder examination (12th edition). New York, NY: Guilford Press, 1993. [Google Scholar]
- [31].Wilfley DE, Schwartz MB, Spurrell EB and Fairburn CG. Using the eating disorder examination to identify the specific psychopathology of binge eating disorder. Int J Eat Disord 2000;27:259–69. [DOI] [PubMed] [Google Scholar]
- [32].Berg KC, Peterson CB, Frazier P and Crow SJ. Psychometric evaluation of the eating disorder examination and eating disorder examination-questionnaire: a systematic review of the literature. Int J Eat Disord 2012;45:428–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Gianini LM, White MA and Masheb RM. Eating pathology, emotion regulation, and emotional overeating in obese adults with Binge Eating Disorder. Eat Behav 2013;14:309–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Godfrey KM, Bullock AJ, Dorflinger LM, Min KM, Ruser CB and Masheb RM. Pain and modifiable risk factors among weight loss seeking Veterans with overweight. Appetite 2018;128:100–105. [DOI] [PubMed] [Google Scholar]
- [35].Wiedemann AA, Ivezaj V and Grilo CM. An examination of emotional and loss-of-control eating after sleeve gastrectomy surgery. Eat Behav 2018;31:48–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Koball AM, Meers MR, Storfer-Isser A, Domoff SE and Musher-Eizenman DR. Eating when bored: revision of the emotional eating scale with a focus on boredom. Health Psychol 2012;31:521–4. [DOI] [PubMed] [Google Scholar]
- [37].Stickney MI and Miltenberger RG. Evaluating direct and indirect measures for the functional assessment of binge eating. Int J Eat Disord 1999;26:195–204. [DOI] [PubMed] [Google Scholar]
- [38].Mason TB, Heron KE, Braitman AL and Lewis RJ. A daily diary study of perceived social isolation, dietary restraint, and negative affect in binge eating. Appetite 2016;97:94–100. [DOI] [PubMed] [Google Scholar]
- [39].Thurston RC, Kubzansky LD. Women, loneliness, and incident coronary heart disease. Psychosom Med 2009;71:836–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Holt-Lunstad J, Smith TB, Baker M, Harris T, Stephenson D. Loneliness and social isolation as risk factors for mortality: A meta-analytic review. Perspect Psychol Sci 2015;10:227–37. [DOI] [PubMed] [Google Scholar]
- [41].Evers C, Adriaanse M, de Ridder DT and de Witt Huberts JC. Good mood food. Positive emotion as a neglected trigger for food intake. Appetite 2013;68:1–7. [DOI] [PubMed] [Google Scholar]
- [42].Butryn ML, Webb V and Wadden TA. Behavioral treatment of obesity. Psychiatr Clin North Am 2011;34:841–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Niemeier HM, Leahey T, Palm Reed K, Brown RA and Wing RR. An acceptance-based behavioral intervention for weight loss: a pilot study. Behav Ther 2012;43:427–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Niemeier HM, Phelan S, Fava JL and Wing RR. Internal disinhibition predicts weight regain following weight loss and weight loss maintenance. Obesity 2007;15:2485–94. [DOI] [PubMed] [Google Scholar]
- [45].Braden A, Flatt SW, Boutelle KN, Strong D, Sherwood NE and Rock CL. Emotional eating is associated with weight loss success among adults enrolled in a weight loss program. J Behav Med 2016;39:727–32. [DOI] [PMC free article] [PubMed] [Google Scholar]


