Abstract
Although the reasons for immigrating to the U.S. vary by Latino groups, many Latinos cite economic or political motivations for their migration. Once in the United States, Latino immigrants may face many challenges, including discrimination and blocked opportunities for social mobility, and difficulties in obtaining health services and quality health care. The purpose of this study was to explore how changes in social mobility from the country of origin to the U.S. may relate to Latina women’s health care interactions. We examined whether self-reported social mobility among 419 Latina women immigrants is associated with satisfaction with health care.We also examined the association among social mobility and self-rated health, quality of care, and medical mistrust. Upward social mobility was associated with greater number of years lived in the U.S., and downward social mobility was associated with more years of education. Those who reported no changes in social class (stable social mobility) were older and were the most satisfied with their medical care. Multiple regression analyses indicated that downward social mobility was associated with less satisfaction with care when controlling for demographic covariates, quality of care, and medical mistrust. Results suggest that perceived social mobility may differentially predict Latina immigrants’ satisfaction with the health care system, including their trust in U.S. medical institutions. We conclude that perceived social mobility is an important element in exploring the experiences of immigrant Latinas with health care in the United States.
Keywords: social mobility, Latina health, satisfaction with care, medical mistrust, quality of care, immigrant health, Dominicans
1. Introduction
Latinos currently comprise a significant portion (representing 16% of the population) of the United States with subpopulations from various national and regional origins, including Mexican Americans (63.0% of Latinos in the U.S.), mainland Puerto Ricans (9.2%), Cubans (3.5%), and Salvadorans (3.3%). Dominicans, typically categorized as “Other Hispanic”, are the fifth largest Latino group in the U.S. (2.8% of all Latinos) (U.S. Census Bureau, 2011). Further, a little more than one-third of all Latinos in the U.S. are foreign born (34.4%) (Pew Research 2017). Despite their demographic variety and wide-ranging representation in the U.S., Latinos as a whole experience persistent health disparities throughout their life course (OMH 2017). Additionally, Latinos of all sub-ethnic backgrounds disproportionately lack access to health care and are less likely to have a regular source of health care than other groups (Dominguez et al 2015)
Studies that examine patient-provider and general health care setting interactions consistently find that Latinos are more dissatisfied with health care than non-Latino whites (Morales et al 1999). Previous research has examined the correlation of health care access with medical mistrust and satisfaction with care among Latinos (Abraido-Lanza et al., 2011; Jones et al 2018), but no studies to our knowledge have analyzed the role of social mobility and satisfaction with health care among Latina immigrants. In this study, we further explore the role of perceived social mobility in satisfaction with care and examine whether social mobility is associated with self-rated health, quality of care, and medical mistrust.
1.1. Social Mobility, Latino Immigration, and Health
Downward social mobility is associated with poor physical health and negative healthbehaviors (Boyle et al 2009; Osypuk et al 2016; Hallqvist et al 2004; Harding 2003; Power et al 1996). In addition to measures of income and education attainment, changes in Subjective Social Status (SSS) — defined as an individual’s perception of socioeconomic standing in a social hierarchy (Nicklett & Burgard, 2009, p. 4), — are also used to measure social mobility. According to Nicklett & Burgard (2009), the SSS is a robust independent predictor of health that can capture the effects of stress, shame, and distrust (Franzini et al 2006). Euteneuer’s (2014) comprehensive overview of SSS and health outcomes found that SSS is related to stress-related biological risk factors, which highlight SSS’s direct effect on neuroendocrine pathways and behaviors that lead to poor health outcomes.
Although limited, current research suggests that the concepts of social class, social mobility, and social status may be associated with health and quality of life. Among young adults in Australia, downward social mobility was associated with lower life satisfaction compared to upward and stable social mobility, while upward social mobility was associated with similar health outcomes to that of stable social mobility (Brenna & Spencern 2014). The effects of social status seem to be shaped primarily by relative comparison to the context in which individuals find themselves. Simandan (2018) calls this status-based identity. Changes in social class can impact status-based identity and subjective wellbeing; immigrants from disadvantaged backgrounds, for example, although economically upward mobile in host countries, are more susceptible to social isolation and the threat of social exclusion, which may account for the lack of direct association between upward social mobility and improvement in physical health (Simandan 2018). Of yet, there is no research that correlates changes in social standing and its association with perceptions of quality of care and medical mistrust, and we hope to begin to illuminate this topic given the important role of subjective perceptions of identity, host country, and medical treatment among immigrant Latinas.
Given their heterogeneity, Latino subgroups differ in their perceptions of social standing and social mobility in the United States. Franzini et al (2006) demonstrate that objective and subjective social status measures are similar to one another, yet there are disparities in how less acculturated Latino subgroups rank their social status when compared with more acculturated subgroups. For example, whereas mastery of the English language and U.S. nativity are associated with high evaluations of social standing among a Mexican sample, this is not the case for Puerto Ricans who are U.S. citizens and may therefore associate social standing closer to white, and therefore mainstream, American ideals (Franzini et al 2006). There is limited knowledge regarding perceptions of social standing among Dominican women in the U.S. and our aim is to begin to address the association between social standing, social mobility, and health care experiences within this population.
Immigration experiences and patterns also shape opportunities for social mobility, and Latino populations vary greatly in immigration history, patterns, and trajectories. Moreover, economic conditions, labor shortages, and the political climate in the U.S. create different contexts of reception for the various groups at different historical periods (Tienda & Sanchez, 2013). Considering that the motives for moving to the U.S. may be influenced by the social class standing of an individual in her native land, experiences with the health care system and health care interactions in turn may differ along these lines. The heterogeneity in social mobility experiences and perceptions of Latino ethnic subgroups indicates that there are also subgroup differences in the effects of perceived social mobility on health and interactions with health care system based on subgroup demographics, history, and context of comparisons.
Further, although there are over one million Dominicans in the United States (Brown & Patten 2013), — the majority of whom reside in New York City (Rumbaut & Komaie 2010), — there is a paucity of research on the health of Dominicans in the United States. Like other Latino groups, most Dominicans cite economic or political motivations for their migration to the United States. Largely politically motivated, immigration from the Dominican Republic to the U.S. rose in the early 1960s under dictator Rafael Trujillo (Tienda & Sanchez, 2013). Later, immigration took on a more economic character and may have been influenced by perceptions of greater opportunities for upward social mobility in the U.S. (Portes and Rumbaut, 2006).
Only recently has migration theory begun to fully integrate gender into the understanding of migration patterns and outcomes for migrants in receiving countries. Most importantly to thepresent study, a focus on gender and particularly on women migrants allows for a parsing of how their experiences differ from those of men. According to Boyd and Grieco (2003), “women may have different experiences than men because they are frequently segregated into traditional ‘female’ occupations…The gender hierarchies that affect all women in general also handicapimmigrant women in particular, influencing job opportunities, work environment, and wages vis-a-vis their male counterparts” (www.migrationpolicy.org). These elements of women migrants’ experiences may also uniquely define their experiences of social mobility.
The United Nations Population Division estimates that by mid-2017 Dominican women immigrants were almost 56% of the Dominican migrants to the U.S. (United Nations 2018). In fact, the trend in Dominican migration over the past decade (Daviglus, et. al., 2012) indicates that the foreign born Dominican population is “female predominant”, using Donato and Gabaccia’s (2015) typology of gender composition among immigrants. There is also evidence that Dominican migrants are more likely to have lower educational attainment, earn less than other migrants and non-migrants and thus live in poverty, and are more likely than other immigrant groups to be naturalized U.S. citizens (Zong & Batalova, 2018). Yet, this information has not been analyzed by gender despite the fact that the socioeconomic disparities indicated weigh heavier on women, in general, and among black and Latina women in particular, especially when they are heads of household (NWLC, 2018). Therefore, little is known about Dominican women’s immigrant experiences in the U.S., their social trajectories, or how these impact health interactions and health outcomes for this group. By measuring perceived social status changes between their native country and the U.S., length of residence in the U.S., acculturation, and perceptions of health and clinical encounters, this study begins to shed light on the experiences of immigrant Latinas and their interactions with the U.S. health care system.
1.1.1. Acculturation, Social Mobility, and Health Care Interactions
An exploration of social mobility also contributes to the body of work on acculturation processes among Latinos. Although different definitions of acculturation are engaged throughout wide ranging research approaches, in this piece we apply acculturation defined as “the process by which individuals adopt the attitudes, values, customs, beliefs, and behaviors of another culture” (Abraido-Lanza et al 2006, p. 1342). Acculturation, as well as Latino immigration trajectories, are of great interest because of their paradoxical effects on health: recent Latino immigrants to the U.S. demonstrate better health outcomes than non-Hispanic whites in the U.S., but the protective effects of immigration disappear in later generations (Balcazar et al 2015). While researchers point to the association between greater acculturation and unhealthful behavior to explain the differing health outcomes between immigrant and non-immigrant Latinos, ethno/racial discrimination may also play a role (Abraído-Lanza, Echeverría & Flórez, 2016). For example, blocked opportunities for upward social mobility may create difficulties in accessing health services and receiving quality health care. Of note, among Latinos higher acculturation scores and greater English language skills are associated with greater medical mistrust; one explanation for this observation is that increased experiences with health care services may also increase negative experiences related to ethnicity or race in these settings (Hong et al 2017). Nevertheless, greater quality of care can be a mediating factor as it is associated with higher rates of health screenings regardless of levels of acculturation or years living in the United States (Hong et al 2017). These factors have implications for access to health care among Latinos as they are more likely to report fear of being exploited as medical “guinea pigs” in clinical settings compared to whites, and report higher mistrust and unwillingness to participate in health screenings (Davis et al 2012).
Associated with these phenomena are the general assumptions that first generation immigrants to the U.S. might have strong motivation for upward social mobility and less time exposed to U.S. race-based differentiation than second and third generations (Owens & Lynch 2013). Exposure to race-based differentiation may lead to internalization of negative stereotypes, which eventually attenuate expectations and create internalization of race-based differentiation of opportunities for social mobility and status relative to whites (Owens & Lynch 2013). Nevertheless, there has been scarce exploration of the role of perceived social mobility among Latinos and its effect on health and health care experiences.
Given the influence of limited access to care, differing immigration motives and trajectories, as well as acculturation effects on health for Latinos in the U.S., we stem from the work of Alcantara, Chen, and Alegría (2014) to explore the association between perceived social mobility, health, and satisfaction with health care among Dominican women. We examine whether self-reported social mobility is associated with satisfaction with medical care, as well as the associations among social mobility, self-reported mental and physical health, quality of care, and medical mistrust. In light of prior observations on the associations between immigration experiences and health, the primary hypothesis is that compared to stable social mobility, downward social mobility is associated with less satisfaction with care. We also hypothesized that relative to stable social mobility, downward social mobility is associated with poor physical and mental health, worse quality of health care, and greater medical mistrust.
2. Methods
The data in this study are part of a larger study on Dominican women’s health promoting behaviors and cancer screening practices (BLINDED). Participants were recruited from various community sites in New York City, and by flyers posted in designated areas in the target communities (e.g., apartment buildings and community-based agencies and service facilities) predominantly in Washington Heights, Inwood, and a western section of the Bronx. Data were collected during the years 2010 to 2012. Over half of the sample (54%) was recruited from community sites, and the remainder by broader community outreach. Eligibility criteria were: (1) Dominican female aged 40 years or older and (2) no prior diagnosis of any form of cancer. Although they have since been revised, at the time of the study, national guidelines recommended mammogram screening at age 40 (CDC 2007). Informed consent was obtained prior to participation in the study, and the university’s medical center Institutional Review Board approved the research.
A total of 419 women participated in the study. Data were collected by a structured face-to-face interview conducted in Spanish, either in the respondent’s home or a community-based site, based on the participant’s preference. Interviews lasted an average of 55 minutes, and respondents received $20 cash for their participation. Other details on study procedures, including Spanish language translation methods of measures (except for the medical mistrust and acculturation scales, for which Spanish versions already exist) are provided in [BLINDED].
2.1.1. Social Mobility Measures
We assessed the primary independent variable of interest, social mobility, with a validated measure from the National Latino and Asian American Study (NLAAS) that asksparticipants to indicate their perceived social status on a 10-stepped ladder, where one represents the bottom of the ladder and therefore the bottom of the social hierarchy, and 10 represents the top (Guarnaccia et al 2007). This measure assesses an individual’s perspective on her social realities, personal social circumstances, individual perceptions of social class and her definitions for worst and best social positions (Franzini et al 2006). Respondents were instructed:
“Think of this ladder as 10 representing where people stand in the United States. At the op of the ladder are the people who are the best off – those who have the most money,the most education and the most respected jobs. At the bottom are the people who are the worst off – who have the least money, least education, and the least respected jobs or no job. The higher up you are on the ladder, the closer you are to the people at the very top;the lower you are, the closer you are to the people at the very bottom. What is the number to the right of the rung where you think you stand at this time in your life, relative to other people in the United States?”
Participants were asked to assess their social standing twice; once in the United States, currently, and on another ladder, to assess where they would be had they not left the Dominican Republic. To measure social mobility, we followed Alcántara et al’s (2014) method. For each participant, social mobility was calculated by comparing responses to the U.S. ladder compared with the Dominican Republic ladder. We created three social mobility categories. Downward social mobility was calculated as any loss (i.e., any decrease) of 1 to 9 steps in the respondent’s U.S. subjective social standing (SSS) ladder compared to her Dominican Republic ladder score. Stable social mobility was operationalized as no change in SSS, and upward social mobility was calculated as any gain (i.e., increase) of 1–9 steps in SSS.
2.1.2. Sociodemographic and acculturation covariates
Variables measured as potential confounders were: age (assessed in years), education (highest grade completed in years), and acculturation. We assessed length of time living in the United States, measured in years, as a proxy for acculturation. We also used the brief 12-item short form of the Acculturation Rating Scale for Mexican Americans (Brief ARSMA; Cuellar, Bastida, & Braccio, 2004), which is one of the most widely-used measures of acculturation, and can be adapted for use with other Latino populations (Chun et al., 2003). Items include language ability and embeddedness with Anglo-American friends rated on a 5-point scale, with higher scores indicating greater acculturation. The scale’s reliability, assessed with Cronbach’s alpha, was α = .75.
2.1.3. Self-Rated Mental and Physical Health
Physical health and mental health were each measured with one item with standardized questions used in various national surveys. Poor general mental health was assessed as, “In general, would you say your general mental health is?…”. Poor physical health was similarly assessed, “In general, you would say your health is?”. Both items had response options of 1= excellent, 2 = very good, 3 = good, 4 = fair, or 5 = poor. These items were coded as continuous variables, as has been previously done in Abraido-Lanza et al 2011, such that a higher score indicated poorer mental and physical health. We also created dichotomous mental health and physical health variables by combining the fair/poor and excellent/very good/good categories. Analyses with these dichotomous variables yielded similar results.
Although self-rated health items have been previously criticized, especially in light of language differences that emerge in English-to-Spanish translations (Santos-Lozada & Martinez 2018), other studies have demonstrated self-rated health item validity (Pérez-Zepeda et al 2016; Berchick and Lynch 2017). For our study population, self-rated physical health and mental health exhibited internal validity when correlated with patient co-morbidities (p < .000, for both items).
2.1.4. Quality of Care and Medical Mistrust
Quality of care was assessed using a slightly modified version of Saha et al.’s (2003) five-item scale, derived from the Commonwealth Fund’s 2001 Health Care Quality Survey. The scale measures the quality of general patient-physician interactions during the last visit (e.g., “The last time you visited your doctor, did the doctor listen to everything you had to say?,” “Did the doctor involve you in decisions about your care?,” “Did the doctor treat you with respect and dignity?”). We modified the scale slightly to standardize all items to a three-point response scale (as the original scale contained both two- and three-point responses), and recoded items such that greater values indicate higher quality of care. We calculated average scores, which could range from 1 to 3. The modified scale showed good reliability (Cronbach’s α=0.77).
General medical mistrust was measured with the validated Spanish version of the Group Based Medical Mistrust Scale (GBMMS) (Thompson et al 2004). GBMMS contains items that tap suspicion, the perception that race-based medical mistreatment leads to health disparities, and lack of support from health care providers, rated on a scale of 1 = “strongly disagree” to 5 = “strongly agree”. After reverse-scoring appropriate items, we calculated a mean score for each participant, yielding scores ranging from 1 to 5 with higher scores indicating greater mistrust. The measure has been used previously with diverse samples (Thompson et al 2004), including Dominicans (Abraído-Lanza et al., 2011). In this study, the internal consistency of the GBMMS was good (Cronbach’s α=0.87).
2.1.5. Satisfaction with Care
The main dependent variable, satisfaction with care was measured with one item: “How satisfied are you with the quality of your medical care that you received in the place where you went for medical assistance?”. Responses were assessed on a 4-point scale ranging from 4 = “very satisfied” to 1 = “not at all satisfied”, with higher values representing greater satisfaction.This measure has been previously used with diverse samples, including Latinos (Saha, Arbelaez & Cooper, 2003) and Dominicans (Abraído-Lanza et al., 2011).
2.2. Statistical analyses
We examined the association between social mobility and satisfaction with care with hierarchical multiple regression analyses. This analysis is meant to highlight variance in satisfaction with care associated with social mobility, as well as other possible predictors of satisfaction with care such as participant demographics, quality of care, and medical mistrust. Satisfaction with care was treated as a continuous variable following previous research (Abraido-Lanza et al., 2011). Model 1 tested the associated between satisfaction with care and the social mobility dichotomous predictor variables. Stable social mobility was treated as the reference group. In model 2, we entered sociodemographics variables (i.e. age, education), and acculturation variables. In model 3, we added physical and mental health variables. Finally, in model 4, quality of care and medical mistrust were added. All analyses were conducted using SPSS v. 24 and STATA v. 14.2.
3. Results
3.1. Descriptive Statistics
Table 1 one provides demographic descriptive statistics. The mean age of the sample was 60.5 years (SD 11.5). Average years lived in the United States was 24.8 (SD 13.8). Mean years of education for the entire sample was 8.5 (SD 4.5). Finally, the majority of participants were covered by health insurance (93.3%).
Table 1.
Demographics- Descriptive Statistics N=419
| Mean (SD) | |
|---|---|
| Age (M, SD)* | 60.5 (11.5) |
| Years of Education** | 8.5 (4.5) |
| Years in the US | 24.8 (13.8) |
| Health Insurance Type ** n(%) | |
| Any health insurance | 387 (93.3) |
| No health insurance | 28 (6.7) |
| Acculturation (ARSMA) | 20.2 (6.1) |
| Social Mobility Status | |
|
Downward (Loss of 1–9 steps) n (%) |
133 (31.7%) |
| Age (M, SD) | 59.0 (11.6) |
| Years of Education (M, SD) | 10.0 (4.7) |
| Years in the US (M, SD) | 22.27(14.5) |
| Acculturation (ARSMA) (M, SD) | 20.0 (5.8) |
|
Stable (No Change in steps) n (%) |
92 (21.9%) |
| Age (M, SD) | 63.0 (11.5) |
| Years of Education (M, SD) | 7 (4.1) |
| Years in the US (M, SD) | 24.40 (14.9) |
| Acculturation (ARSMA) (M, SD) | 19.6 (6.2) |
|
Upward (Gain of 1–9 steps) n (%) |
192 (45.8%) |
| Age (M, SD) | 60.4, (11.3) |
| Years of Education (M, SD) | 8.2 (4.2) |
| Years in the US (M, SD) | 26.8 (12.5) |
| Acculturation (ARSMA) (M, SD) | 20.8 (6.3) |
402 respondents
415 respondents
Social status data was available for 417 participants; 133 reported downward social mobility and 192 reported upwardly social mobility. The rest, 92 participants, reported no change in their class status and were categorized in the stable social mobility group (Table 1).
Table 2 presents the bivariate intercorrelations of demographic variables and predictor variables, quality of care, medical mistrust, and social mobility. Downward social mobility was associated with living fewer years in the U.S. (p ≤ .05), and more years of education (p ≤ .01). Stable social mobility was associated with older age (p ≤ .05), and fewer years of education (p ≤.001). Of note, poor mental health was significantly associated with less satisfaction with care (p≤ .01), and poor health status correlated with greater age, fewer years of education, and with more years lived in the U.S. (p ≤ .001). Finally, age was negatively associated with years of education (p ≤ .01).
Table 2.
Intercorrelation matrix for model variables with Pearson correlations and p-values (n= 419)
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. | Satisfaction with Care |
|||||||||||
| 2. | Downward Social Mobility |
−.14** | ||||||||||
| 3. | Stable Social Mobility |
.11* | −.36*** | |||||||||
| 4. | Upward Social Mobility |
.04 | −.63*** | −.49*** | ||||||||
| 5. | Age | .10* | −.092 | .11* | −.008 | |||||||
| 6. | Years of Education |
−.12* | .23*** | −.18*** | −.07 | −.42** | ||||||
| 7. | Years in the US | −.041 | −.12* | −.02 | .13** | .41** | −.08 | |||||
| 8. | Acculturation (ARSMA) |
−.08 | −.03 | −.06 | .08 | −.28*** | .35*** | .17*** | ||||
| 9. | Poor Health | −.06 | −.07 | .03 | .04 | .25** | −.20** | .23** | −.16** | |||
| 10. | Poor Mental Health |
−.13** | −.00 | −.02 | .02 | .10* | −.15** | .15** | −.05 | .31** | ||
| 11. | Quality of Care | .52*** | −.10 | .08 | .02 | .14** | −.13** | .04 | −.06 | −.01 | −.11* | |
| 12. | Medical Mistrust |
−.34*** | .10* | −.02 | −.08 | −.06 | .07 | .05 | .09 | .08 | .19*** | −.17*** |
p ≤ 0.05
p ≤ 0.01
p ≤ 0.001
Figure 1 illustrates the distribution of participants’ perceived social class status in the Dominican Republic on the 1–10 stepladder social scale compared with their reported status in the U.S. (downward, stable, or upward). Those who reported downward social mobility in the U.S. were primarily at stepladder 6 and above (higher social status) in the Dominican Republic (n = 93, 70%). The majority of respondents who claimed upward mobility in the U.S. assessed their social standing in the Dominican Republic as 1–4 in the stepladder (lower social status) (n = 173, 90%), whereas those who reported stable social mobility between the Dominican Republic and the U.S. were relatively more evenly distributed across the Dominican Republic social ladder. Nevertheless, a majority of the stable mobility respondents identified being in the 1–5 steps in the Dominican Republic (lower- to middle- social status) (n = 73, 79%).
Figure 1.
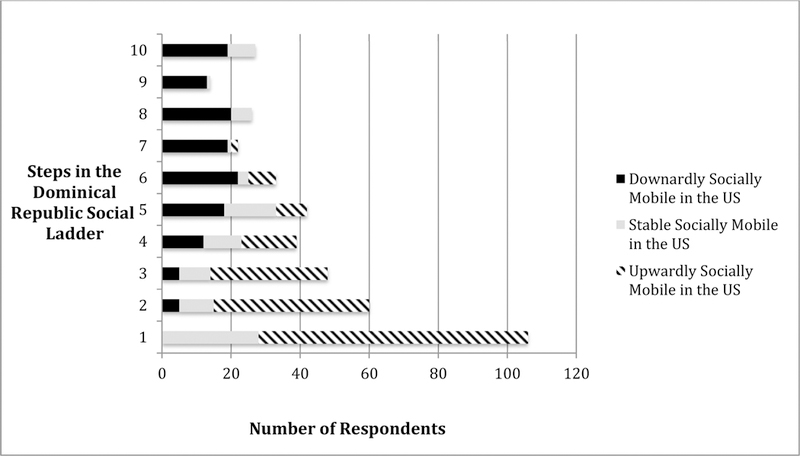
Distribution of perceived social standing in the Dominican Republic, by social status change grouping
3.2. Social Mobility and Dissatisfaction with Care and Medical Mistrust
Table 3 presents the results of the regression equation predicting satisfaction with care, with stable social mobility as the reference group. In all four models, downward social mobility was significantly associated with less satisfaction with care (p ≤ .05). In models 2–4, age, years of education, years living in the U.S., and acculturation were not significant predictors of satisfaction with care. Model 3 shows that self-rated poor general mental health significantly predicted less satisfaction with care (β = −.11). Additionally, quality of care correlated significantly with greater satisfaction with care (β = .47) and medical mistrust was a significant predictor of decreased satisfaction with care (β = −.25).
Table 3.
Regression Analysis with Social Mobility, Sociodemographic Characteristics, Acculturation and Perceived Health as Predictors of Satisfaction with Care
| Model 1 | Model 2 | Model 3 | Model 4 | |||||
|---|---|---|---|---|---|---|---|---|
| Std β | (S.E.) | Std β | (S.E.) | Std β | (S.E.) | Std β | (S.E.) | |
| Stable Social Mobility * | ||||||||
| Downward Social Mobility |
−.20 | (.09) | −.19 | (.10) | −.19 | (.10) | −.12 | (.08) |
| Upward Social Mobility | −.08 | (.09) | −.08 | (.09) | −.08 | (.09) | −.06 | (.07) |
| Age | .06 | (.00) | .09 | (.00) | .00 | (.00) | ||
| Years of Education | −.05 | (.00) | −.05 | (.00) | −.05 | (.00) | ||
| Years Living in the US | .03 | (.00) | .04 | (.00) | .02 | (.00) | ||
| Acculturation (ARSMA) | −.07 | (.01) | −.08 | (.01) | −.04 | (.00) | ||
| Poor Health | −.08 | (.03) | −.04 | (.03) | ||||
| Poor General Mental Health |
−.11 | (.03) | −.02 | (.03) | ||||
| Quality of Care | .47 | (.12) | ||||||
| Medical Mistrust | −.25 | (.03) | ||||||
Reference Group
Bold items are significant, p ≤ 0.05
4. Discussion
We describe how Latina immigrants’ trajectories of social mobility are associated with satisfaction with health care in the United States. Downward social mobility was associated with more years of education, fewer years lived in the U.S., and greater medical mistrust compared to stable or upward social mobility, while upward social mobility associated significantly with more years lived in the U.S. compared to downward and stable social mobility. We had hypothesized that perceptions of downward social mobility would be associated with less satisfaction with care relative to stable social mobility and that downward social mobility would be associated with poor physical and mental health, worse quality of health care, and greater medical mistrust compared to stable social mobility. Our results indicate that subjective perceptions of downward social mobility among Dominican women in New York City correlate with less satisfaction with health care compared to stable and upward social mobility.
The surprising finding that downward social mobility associated with more years of education and fewer years living in the U.S. may reflect the effect of relative newness to the U.S., and may indicate that participants who indicated downward social mobility and higher education received their education in the Dominican Republic. Thus, they may have expected greater potential for upward social mobility post migration. However, there is some suggestion that education attainment might not be as salient a marker of social status for Latinos when compared to years in the U.S. or employment status (Ostrove et al 2000). Further, upward social mobility correlated with more years of living in the U.S., but not satisfaction with care, which aligns with previous research that associates exposure to negative experiences related to ethnicity or race in U.S. health care settings (Hong el al 2017). Stable social mobility was associated with greater age and fewer years of education, factors that should be addressed further in their implications for treatment expectations and experiences.
Contrary to the myth of the “American Dream”, the majority of Dominican women in this study perceived themselves to be of a lower or equal social status standing in the U.S. than they would have been in the Dominican Republic. Among Dominican immigrants — perhaps more than many other Latino ethnic groups — racial identity may play a central role the process of acculturation. Itzigsohn, Giorguli, and Vasquez (2005) find that Dominican immigrants experience a complex process of racial re-identification in the U.S. where choices of racial identity are limited. Their study reports that although a majority of Dominicans’ self-identification remains connected with an indigenous or Hispanic mixed-race identity, the Dominicans interviewed understood that the mainstream perception of themselves in the U.S. racial hierarchy is as black; the subset of Dominicans who identified themselves as black eported experiencing higher rates of discrimination and greater social distance from whites in the U.S, despite holding the highest occupational status among all self-identified racial groups. Similarly, in a study of the self-rated health status among Mexican immigrant and Mexican-American Latinos, Vasquez and Sanchez (2018) note that exposure to the U.S. racial classification system generates worse self-rated health for darker skinned U.S. born Latinos. Both poor self-rated health and perceptions of racial discrimination have been linked to decreased satisfaction with medical care (Weech-Maldonado et. al., 2012). The findings of the present study, combined with prior literature, point to a need to include not only self-reported race but also “mainstream perception of your race” in surveys of Latinos and Hispanics in the United States. Unlike other ethno-racial groups, there may exist an important dichotomy among Latinos between perception and lived reality, which may explain factors such as reduced social mobility, low self-rated health, and lack of satisfaction with medical care.
As previously noted, there are gendered expectations regarding occupational and economic opportunities for recent immigrants. Despite Dominican migrants’ lower rates of education attainment, and consistent relative poverty compared to other migrant and non-migrant groups (Zong & Batalova, 2018), little attention has been given to the impact of perceptions of changes in social position on Dominican women and their interactions with health care institutions and health outcomes. Our study begins to explore perceptions of social mobility with that of satisfaction with care, medical mistrust and quality of care. Paradoxical findings, such as the association between higher education and perception downward social mobility, and the lack of association between upward social mobility and greater satisfaction with care, gives emphasis to a gap in understanding the role of subjective perceptions of social standing on health care interactions and health behaviors among Latina women.
Health care providers can be equipped with resources to help mitigate the negative impacts of immigration policy stressors that affect health care interactions and health outcomes by further understanding risk factors for immigrant patients (Hacker et al 2012). For example, fear and intimidation based on punitive immigration policies affect health behaviors and may restrain the ability of individuals to navigate U.S. institutions with ease, or prevent relocation to different states to pursue employment opportunities (Ardy et al 2012; Salas et al 2013; Amuedo-Dorantes et al 2013). An internalized sense of lower social standing in clinical settings, due to feelings of discrimination, for example, limits the ability of patients to make claims for their well being and legitimize their health concerns. They also constrain immigrants’ access to resources that mitigate negative health outcomes (Briggs 2005). Nguyen et al (2007) find that therapeutic citizenship — the sense of being able to make claims for specific forms of care from health institutions and the government — may influence immigrants who perceive themselves to be downwardly socially mobile to feel they have less of a right to health care. Taking into account these factors, providers are positioned to be aware of these setbacks and to acknowledge the larger contexts that influence health outside of the clinic in order to facilitate healthful behavior. Increasing minority patient satisfaction with care and retention are ways to counter barriers to health found outside of the clinic and both of these factors have been positively associated with clinicians who not only prioritize a therapeutic alliance, but who are also concordant in language or racially/ethnically (Alegría et al 2013; Fernandez et al 2011; Parker et al 2017; Jamarillo et al 2016).
This study is not without limitations. This is a cross sectional analysis of social mobility and its association with satisfaction with health care. Therefore, we cannot make claims to directionality of the associations between social mobility and satisfaction with care. Further, as a secondary analysis of breast cancer screening data, our study participants were middle-aged and older Dominican woman residing in NYC, and therefore represent a subset of the Latino immigration experience. Future studies should examine how social status differences impact health interactions for populations of various ages, states of employment, and at different time points in their immigration to the United States.
Despite these limitations, we find that our research is a novel analysis of the influence of social mobility among Latina immigrants on their interactions with providers. One of the strengths of our study was the focus on an often overlooked population in research: middle-aged Dominican women and their views regarding social mobility. Our findings did not indicate that those who experienced downward social mobility were also likely experience worse health outcomes, but social mobility from country of origin has a relationship with perceptions of clinical interactions such as medical mistrust, perceptions of quality of care and satisfaction with care. A body of research finds that lack of satisfaction with care is associated with decreased adherence to medical treatment and an increased likelihood of loss to follow up (LaVeist et al 2009; LaVeist et al 2000; Jones et al 2018). More research needs to be conducted regarding ethnic immigrant groups and the role of SSS on medical adherence, medical mistrust, satisfaction with care, and health outcomes.
Highlights.
This is a unique analysis of social mobility among Dominican immigrant women
Downward social mobility was associated with lower satisfaction with health care
Downward social mobility was (weakly) associated with poor mental health
Upward and stable social mobility were not associated with better health outcomes
Acknowledgments
Thanks to Raziel D. Valiño, Mariana Martins, Emily Vasquez, Elisa Gonzalez, Evianna Cruz, Milagros Ventura, and Karen R. Flórez for their research assistance. Special thanks to Adolfo Cuevas and Danny Giovenco for their insight during the conceptualization of this work.
Funding
This work was supported by grant R21CA134247 from the National Institutes of Health. The work was also supported, in part by grants R25GM062454, and UL1TR000040 from the National Institutes of Health; and to the first author by the Rowe Family Foundation.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Sonia Mendoza, Columbia University, Mailman School of Public Health, Department of Sociomedical Sciences New York, NY.
Adria N. Armbrister, Columbia University, Mailman School of Public Health, Department of Epidemiology New York, NY.
Ana F. Abraído-Lanza, New York University, College of Global Public Health New York, NY.
References
- Abraído-Lanza AF, Armbrister AN, Flórez KR, Aguirre AN. Toward a theory-driven model of acculturation in public health research. Am J Public Health 2006. August 96(8):1342–6. Epub 2006 Jun 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abraído-Lanza AF, Céspedes A, Daya S, Flórez KR, White K. Satisfaction with health care among Latinas. J Health Care Poor Underserved 2011. May;22(2):491–505. doi: 10.1353/hpu.2011.0042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abraído-Lanza AF, Echeverría SE & Flórez K (2016). Latino immigrants, acculturation, and health: Promising new directions in research. Annual Review of Public Health, 37, 219–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abraído-Lanza AF, Shelton RC, Martins MC, & Crookes DM (2017). Social norms, acculturation, and physical activity among Latina women. Journal of Immigrant and Minority Health, 19(2), 285–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alcántara C, Chen CN, Alegría M. Do post-migration perceptions of social mobility matter for Latino immigrant health? Soc Sci Med 2014. January;101:94–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegría M, Roter DL, Valentine A, Chen CN, Li X, Lin J, Rosen D, Lapatin S, Normand SL, Larson S, Shrout PE. (2013). Patient-clinician ethnic concordance and communication in mental health intake visits. Patient Educ Couns 93(2):188–96. doi:10.1016/j.pec.2013.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amuedo-Dorantes C, Puttitanun T, Martinez-Donate AP. How do tougher immigration measures affect unauthorized immigrants? Demography 2013. June;50(3):1067–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balcazar AJ, Grineski SE, Collins TW. The Hispanic health paradox across generations: the relationship of child generational status and citizenship with health outcomes. Public Health 2015. June;129(6):691–7. doi: 10.1016/j.puhe.2015.04.007. Epub 2015 May 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berchick ER, Lynch SM. Regional Variation in the Predictive Validity of Self-Rated Health for Mortality. SSM Popul Health 2017. December;3:275–282. doi: 10.1016/j.ssmph.2017.01.010. Epub 2017 Jan 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Briggs CL. Communicability, Racial Discourse, and Disease. The Annual Review of Anthropology 2005. 34: 269–91. [Google Scholar]
- Brown A, & Patten E “Hispanics of Dominican Origin in the United States, 2011.” Pew Research Center Hispanic Trends Accessed April 12, 2018. http://www.pewhispanic.org/2013/06/19/hispanics-of-dominican-origin-in-the-united-states-2011/ [Google Scholar]
- Boyd M & Grieco E “Women and Migration: Incorporating Gender into International Migration Theory,” Migration Information Source, March 1, 2003, www.migrationpolicy.org/article/women-and-migration-incorporating-gender-international-migration-theory [Google Scholar]
- Centers for Disease Control (CDC). (2007). Morbidity and Mortality Weekly Report. Use of Mammograms Among Women Aged >40 Years --- United States, 2000—2005 https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5603a1.htm. Accessed July 25,2018. [PubMed] [Google Scholar]
- Chun KM, Organista BP, & Marín G (2003). (Eds.). Acculturation: Advances in theory, measurement and applied research Washington, DC: American Psychological Association. [Google Scholar]
- Cuellar I, Bastida E, Braccio SM. Residency in the United States, subjective well-being, and depression in an older Mexican-origin sample. J Aging Health 2004;16(4):447–66. [DOI] [PubMed] [Google Scholar]
- Daviglus, Martha L,.et al. 2012. Prevalence of Major Cardiovascular Risk Factors and Cardiovascular among Hispanic/Latino Individuals of Diverse Backgrounds in the United States; JAMA; Vol. 308(17): 1775–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis JL, Bynum SA, Katz RV, Buchanan K, Green BL. (2012). Sociodemographic differences in fears and mistrust contributing to unwillingness to participate in cancer screenings. J Health Care Poor Underserved 23(4 Suppl), 67–76. doi: 10.1353/hpu.2012.0148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dominguez K, Penman-Aguilar A, Chang MH, Moonesinghe R, Castellanos T, Rodriguez-Lainz A, Schieber R; Centers for Disease Control and Prevention (CDC). Vital signs: leading causes of death, prevalence of diseases and risk factors, and use of health services among Hispanics in the United States - 2009–2013. MMWR Morb Mortal Wkly Rep 2015. May 8;64(17):469–78. [PMC free article] [PubMed] [Google Scholar]
- Donato and Gabaccia, Gender and International Migration (New York: Russell Sage Foundation, 2015). [Google Scholar]
- Edward J Undocumented Immigrants and Access to Health Care: Making a Case for Policy Reform. Policy Polit Nurs Pract 2014. February;15(1–2):5–14. Epub 2014 May 6. [DOI] [PubMed] [Google Scholar]
- Fernandez A, Schillinger D, Warton EM, Adler N, Moffet HH, Schenker Y, Salgado MV, Ahmed A, Karter AJ. (2011). Language barriers, physician-patient language concordance, and glycemic control among insured Latinos with diabetes: the Diabetes Study of Northern California (DISTANCE). J Gen Intern Med, 26(2), 170–6. doi:10.1007/s11606-010-1507-6. Epub 2010 Sep 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finch BK, Vega W. Acculturation stress, social support, and self-rated health among Latinos in California. Journal of Immigrant Health 2003; 5:109–117. [DOI] [PubMed] [Google Scholar]
- Franzini L, Fernandez-Esquer ME. The association of subjective social status and health in lowincome Mexican-origin individuals in Texas. Social Science & Medicine 2006; 63:788–804. [DOI] [PubMed] [Google Scholar]
- Guarnaccia PJ, Pincay IM, Alegría M, Shrout PE, Lewis-Fernández R, Canino GJ. Assessing diversity among Latinos: results from the NLAAS. Hispanic Journal of Behavioral Sciences 2007;29:510–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hacker K, Chu J, Arsenault L, Marlin RP. Provider’s perspectives on the impact of Immigration and Customs Enforcement (ICE) activity on immigrant health. J Health Care Poor Underserved 2012. May;23(2):651–65. doi: 10.1353/hpu.2012.0052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harding S Social mobility and self-reported limiting long-term illness among West Indian and South Asian migrants living in England and Wales. Social Science & Medicine 2003; 56:355–361. [DOI] [PubMed] [Google Scholar]
- Hong YR, Tauscher J, Cardel M. (2017). Distrust in health care and cultural factors are associated with uptake of colorectal cancer screening in Hispanic and Asian Americans. Cancer 2018. January 15;124(2):335–345. doi: 10.1002/cncr.31052. Epub 2017 Oct 4. [DOI] [PubMed] [Google Scholar]
- Itzigsohn Jose, Giorguli Silvia and Vasquez Obed. Immigrant Incorporation and Racial Identity: Racial Self-identification among Dominican Immigrants. Race and Ethnic Studies 2005;28 (1): 50–78. [Google Scholar]
- Jaramillo J, Snyder E, Dunlap JL, Wright R, Mendoza F, Bruzoni M. (2016). The Hispanic Clinic for Pediatric Surgery: A model to improve parent-provider communication for Hispanic pediatric surgery patients. J Pediatr Surg, 51(4), 670–674. doi: 10.1016/j.jpedsurg.2015.08.065. Epub 2015 Sep 15 [DOI] [PubMed] [Google Scholar]
- Jones AL, Cochran SD, Leibowitz A, Wells KB, Kominski G, Mays VM. Racial, Ethnic, and Nativity Differences in Mental Health Visits to Primary Care and Specialty Mental Health Providers: Analysis of the Medical Expenditures Panel Survey, 2010–2015. Healthcare (Basel) 2018. March 22;6(2). pii: E29. doi: 10.3390/healthcare6020029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaVeist TA, Nickerson KJ, Bowie JV. (2000) Attitudes about racism, medical mistrust, and satisfaction with care among African American and white cardiac patients. Med Care Res Rev 57 Suppl 1:146–61. [DOI] [PubMed] [Google Scholar]
- LaVeist TA, Isaac LA, Williams KP. (2009). Mistrust of health care organizations is associated with underutilization of health services. Health Serv Res, 44(6), 2093–105. doi: 10.1111/j.1475-6773.2009.01017.x. Epub 2009 Sep 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez O Immigration policy and access to health services. J Immigr Minor Health 2014. August;16(4):563–4. doi: 10.1007/s10903-013-9864-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morales LS, Cunningham WE, Brown JA, Liu H, Hays RD. Are Latinos less satisfied with communication by health care providers? J Gen Intern Med 1999. July;14(7):409–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Women’s Law Center, “Women and Poverty, State by State”, Last accessed: July 16, 2018, Available online: nwlc.org/resources/women-and-poverty-state-state/
- Nicklett EJ, Burgard SA. Downward social mobility and major depressive episodes among Latino and Asian-American immigrants to the United States. Am J Epidemiol 2009. September 15; 170 (6):793–801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen VK, Ako CY, Niamba P, Sylla A, Tiendrébéogo I. Adherence as therapeutic citizenship: impact of the history of access to antiretroviral drugs on adherence to treatment. AIDS 2007. October;21 Suppl 5:S31–5. doi: 10.1097/01.aids.0000298100.48990.58. [DOI] [PubMed] [Google Scholar]
- Office of Minority Health (OMH). Profile: Hispanic/Latino Americans. 2017 Sep; https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=3&lvlid=64. [Google Scholar]
- Ostrove JM, Adler NE, Kuppermann M, Washington AE. Objective and subjective assessments of socioeconomic status and their relationship to self-rated health in an ethnically diverse sample of pregnant women. Health Psychol 2000. November;19(6):613–8. [DOI] [PubMed] [Google Scholar]
- Osypuk TL, Slaughter-Acey JC, Kehm RD, Misra DP Life-course Social Mobility and Reduced Risk of Adverse Birth Outcomes. Am J Prev Med 2016. December;51(6):975–982. doi: 10.1016/j.amepre.2016.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Owens J, Lynch SM. Black and Hispanic immigrants’ resilience against negative ability racial stereotypes at selective colleges and universities in the United States. Sociol Educ 2012. October;85(4):303–325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker MM, Fernández A, Moffet HH, Grant RW, Torreblanca A, Karter AJ. (2017). Association of Patient-Physician Language Concordance and Glycemic Control for Limited-English Proficiency Latinos With Type 2 Diabetes. JAMA Intern Med, 177(3), 380–387. doi: 10.1001/jamainternmed.2016.8648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pérez-Zepeda MU, Belanger E, Zunzunegui MV, Phillips S, Ylli A, Guralnik J. Assessing the Validity of Self-Rated Health with the Short Physical Performance Battery: A Cross-Sectional Analysis of the International Mobility in Aging Study. PLoS One 2016. April 18;11(4):e0153855. doi: 10.1371/journal.pone.0153855. eCollection 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Portes A; Rumbaut RG. Immigrant America: A portrait Berkeley, CA: University of California Press; 2006. [Google Scholar]
- Power C, Matthews S, Manor O. Inequalities in self rated health in the 1958 birth cohort: lifetime social circumstances or social mobility? BMJ 1996. August 24;313 (7055):449–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pew Research. 2017 Accessed February 14, 2018. http://www.pewresearch.org/facttank/2017/09/18/how-the-u-s-hispanic-population-is-changing/
- Rumbaut RG, Komaie G. Immigration and adult transitions. Future Child 2010. Spring;20(1):43– 66. [DOI] [PubMed] [Google Scholar]
- Santos-Lozada AR, Martinez MJ. How Have You Been? or ¿Como estás?: Does Language of Interview Influences Self-Rated Health Among Hispanic Subgroups? J Immigr Minor Health 2018. August;20(4):766–775. doi: 10.1007/s10903-017-0606-4. [DOI] [PubMed] [Google Scholar]
- Simandan D Rethinking the health consequences of social class and social mobility. Soc Sci Med 2018. March;200:258–261. doi: 10.1016/j.socscimed.2017.11.037. Epub 2018 Jan 1. [DOI] [PubMed] [Google Scholar]
- Smedley BD, Stith AY, Nelson AR, editors. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Institute of Medicine (US) Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care; Washington (DC): National Academies Press (US); 2003. [PubMed] [Google Scholar]
- Thompson HS, Valdimarsdottir HB, Winkel G, et al. The Group-Based Medical Mistrust Scale: psychometric properties and association with breast cancer screening. Prev Med 2004. February; 38(2):209–18. [PubMed: 14715214] [DOI] [PubMed] [Google Scholar]
- Tienda M & Sanchez S (2013). Latin American Immigration to the United States. Daedalus, 142(3), 48–64. doi:10.1162/DAED_a_00218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United Nations Population Division. N.d. International Migrant Stock by Destination and Origin Accessed July 16, 2018.
- http://www.un.org/en/development/desa/population/migration/data/estimates2/estimates17.shtml.
- U.S. Census Bureau. The Hispanic population 2010. U.S. Department of Commerce Economics and Statistics Administration, 2011. (Accessed January 25, 2014, at http://www.census.gov/prod/cen2010/briefs/c2010br-04.pdf) [Google Scholar]
- Vasquez Cirila Estela and Gabriel R/ Sanchez. The Impact of Acculturation and Racialization on Self-Rated Health Status Among U.S. Latinos. Journal of Immigrant and Minority Health (January 2018): 1–7. [DOI] [PubMed]
- Weech-Maldonado R, Hall A, Bryant T, Jenkins KA, Elliott MN. The relationship between perceived discrimination and patient experiences with health care. Med Care 2012. September;50(9 Suppl 2):S62–8. doi: 10.1097/MLR.0b013e31825fb235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zong J, & Batalova J “Dominican Immigrants in the United States,” Migration Information Source, April 11, 2018, www.migrationpolicy.org/article/dominican-immigrants-united-states [Google Scholar]


