Abstract
Objective
To perform a systematic review and meta-analysis identifying (1) potential modifiable risk factors and (2) associated modifiable factors for patellar tendinopathy in athletes.
Design
A systematic review and meta-analysis was conducted. Risk of bias was assessed using the Newcastle-Ottawa Scale and grouped based on study design. Meta-analytic statistics were performed for items reported by five or more studies. A strength of evidence rating is provided for items not appropriate for meta-analysis.
Data sources
PubMed, Web of Science, Scopus and Cinahl were searched on 14 November 2017.
Eligibility criteria
Quantitative, original research reporting potential modifiable risk factors or associated factors, comparing athletes with patellar tendinopathy to a group without the injury.
Results
862 records were screened and 31 articles were included (6 prospective, 25 cross-sectional). There was a lack of strong evidence for any potential modifiable risk factor or associated factors. There was limited or conflicting evidence that decreased ankle dorsiflexion range-of-motion, decreased posterior thigh and quadriceps flexibility, greater volume of jump training, more volleyball sets played per week, greater counter-movement jump (CMJ) height, and greater activity volume are potential modifiable risk factors. Meta-analysis supported greater activity volume (Cohen’s d=0.22, 95% CI: 0.06–0.39, p=0.008), higher bodyweight (0.36, 0.17–0.55, p<0.001), and greater CMJ height (0.31, 0.07–0.56, p=0.01) as associated modifiable factors.
Conclusions
There is a lack of strong evidence for any potential modifiable risk factors or associated factors. Factors with lower levels of support may be of interest in designing prevention programs but require further research in high-quality, prospective studies.
INTRODUCTION
Patellar tendinopathy is a clinical diagnosis, characterized by focal pain at the inferior pole of the patella and load-dependent symptoms, with increased loads resulting in a greater degree of pain.[1] It most commonly affects athletes participating in jumping sports, where the extensor mechanism experiences high, repetitive loads.[2] The prevalence of patellar tendinopathy is high, with 11.8–14.4% of recreational volleyball and basketball players reporting symptoms.[3] In elite players the prevalence is even higher, with 32% of elite men’s basketball players and 45% of elite men’s volleyball players experiencing symptoms.[2] These players have decreased sports performance[2] and prolonged absences from training and matches.[4] Although many athletes with patellar tendinopathy will seek treatment or modify activity, 49% will experience recurrent symptoms[4] and more than 50% may retire from sports participation due to persistent pain.[5] Therefore, it is of interest to identify ways to prevent patellar tendinopathy so athletes never enter a cycle of recurrent pain and functional limitation.
Identification of risk factors for patellar tendinopathy is essential to development of targeted prevention programs. A previous systematic review by van der Worp et al. identified over 40 potential risk factors for patellar tendinopathy.[6] However, the authors found that many proposed risk factors have not been prospectively investigated, have limited support from low-quality studies or have conflicting evidence. Additionally, not all risk factors were modifiable. Thus, they may assist in identifying athletes at higher risk of injury but do not provide an opportunity for clinicians to intervene to reduce that risk. Building upon the work by van der Worp et al., the purpose of this study was two-fold:
To systematically identify potential modifiable risk factors for patellar tendinopathy in athletes using prospective, longitudinal studies.
To systematically identify associated modifiable factors in athletes, which lack prospective support as potential modifiable risk factors, using cross-sectional studies.
METHODS
The protocol for this review was registered on the International Prospective Register of Systematic Reviews (PROSPERO) (ID #: 42016052904) and conducted according to Preferred Reporting Items for Systemic Reviews and Meta-Analysis (PRISMA) guidelines.[7]
Search strategy
Using the assistance of a research librarian, a search strategy was developed based on two categories of interest: (1) terms related to the patellar tendon or patellar tendinopathy and (2) terms related to modifiable risk factors (Supplementary Material). A human participants restriction was applied. Studies were not limited to a specific time period or language. Preliminary searches were conducted to ensure that the search strategy was comprehensive. Following preliminary searches, articles including the terms “ACL”, “anterior cruciate ligament”, “graft”, “arthroplasty”, “prosthetic” and “fracture” in their title or abstract were excluded to limit the number of irrelevant articles. An online search was performed of PubMed, Web of Science, Scopus and Cinahl. The initial search was conducted on 18 November 2016 and repeated on 14 November 2017. Following the full-text review phase, references of included studies and retained systematic reviews were hand-searched for additional relevant articles not captured by the initial search.
Inclusion and exclusion criteria
All quantitative original research comparing athletes with patellar tendinopathy to a control group without the injury was considered. Patellar tendinopathy is defined as symptoms isolated to the inferior pole of the patella.[1] However, historically, patellar tendinopathy was more broadly defined as “Jumper’s Knee” and included symptoms anywhere along the patellar tendon or quadriceps tendon.[8] Therefore, studies that utilized a broader definition of patellar tendinopathy were included, as symptoms at sites other than the inferior pole of the patella are less common.[8] Studies in which diagnosis was based on imaging alone were excluded since patellar tendon structural changes are common in individuals without clinical signs and symptoms of patellar tendinopathy.[9] Animal, cadaveric or interventional studies were excluded. Abstracts, conference proceeding, editorials, opinion-based papers, reviews (narrative or systematic), letters, case series and case studies were also excluded. However, systematic reviews were retained until the full-text phase so their references could be included in the hand-search. Additionally, studies lacking modifiable potential risk factors or associated factors, or a clear comparison between patellar tendinopathy and a group without the injury were excluded.
Study selection
Prior to record screening, duplicates were removed by the research librarian. Two reviewers (ALS and AHS) completed title, abstract and full-text review independently for all records. Records were screened for inclusion/exclusion criteria. After each phase of the screening process, disagreements regarding record inclusion were discussed and a third reviewer (KGS) was consulted if consensus could not be reached. Included articles were grouped based on study design; prospective, longitudinal, cohort studies (prospective) and cross-sectional or case-control studies (cross-sectional). Prospective studies can identify potential modifiable risk factors, since presence or exposure to the risk factor are determined prior to development of patellar tendinopathy. At best, items identified in cross-sectional studies can only be considered associated modifiable factors, since a temporal relationship cannot be established.
Quality assessment
Studies were independently assessed for risk-of-bias and methodological quality by two reviewers (ALS and PK) using a modified version of the Newcastle-Ottawa Scale (NOS).[10] The NOS is an eight-item checklist, grouped into three domains (selection, comparability, and outcome or exposure) designed for assessing risk-of-bias in non-randomized studies. There are two versions of the instrument, one for case-control (cross-sectional) studies and one for cohort (prospective) studies. For each item assessed, a list of responses is provided and the reviewer must select the response most appropriate for the study. Responses that indicate low risk-of-bias are awarded a star and studies can receive a maximum score of nine stars. For certain items, multiple responses may be appropriate. For example, studies that reported multiple factors of interest may have used independent blind assessment for some factors and self-report for others. In these instances, separate scores are reported. The NOS has been previously used for quality assessment in systematic reviews[11,12] and was deemed appropriate for use in a review of quality assessment instruments.[13] If reviewers disagreed on a quality assessment rating, the inconsistency was discussed and a third reviewer (KGS) was consulted, if necessary, to resolve disputes. Studies were not excluded based on their quality assessment score. However, the quality assessment score was considered for determining the strength of the results.
Data extraction
Data extraction was completed by a single reviewer (ALS) using pre-defined categories and independently verified by a second reviewer (PK). These categories included: study design, potential risk factors investigated, inclusion and exclusion criteria, group allocation, sample size, population age, sports included, competition level, sex distribution, proportion of cases and controls, diagnostic criteria for patellar tendinopathy and study conclusions. For each factor of interest, the method of measurement, reported values, statistical test used and significance level were also recorded. Factors were excluded from analysis if they were used for matching case and control groups, as the distribution of these factors were controlled by the research team and cannot be attributed to the injury. Additionally, factors previously reported in a study using the same or part of the same sample were excluded to prevent data duplication. Ultrasound imaging measures and biomechanical variables were not extracted since these measures were recently explored in other systematic reviews.[14,15] Potential risk factors or factors associated with patellar tendinopathy were categorized into six groups:
Anthropometrics
Joint Range-of-Motion and Muscle Length
Sports and Physical Activity
Functional Test Performance
Muscle Performance
Occupational Demands
Data synthesis and analysis
Cohen’s Kappa values were calculated for inter-rater agreement for each stage of the screening process and for quality assessment ratings.[16] Scores were interpreted using pre-defined cut-off scores.[17]
For potential risk factors or associated factors reported by five or more studies within a study-design grouping, meta-analytic statistics are reported. Cohen’s d with 95% confidence intervals were calculated for each factor using Comprehensive Meta-Analysis software, version 3.3.070 (Engelwood, NJ, USA) with alpha set at 0.05.[18] A positive effect indicates that the measured value was larger in the patellar tendinopathy group and a negative effect indicates the value was smaller in the patellar tendinopathy group. As a follow-up, odds ratios (OR = ((n) exposed cases/(n) unexposed cases)/((n) exposed controls/ (n) unexposed controls)) with 95% confidence intervals are reported for significant effects.[19] For calculation of effect sizes the fixed effects model was used when heterogeneity between studies was low or moderate and random effects model used when it was high. This study followed McAuliffe et al’s[14] criteria for assessing heterogeneity using Higgin’s I2 value,[20] an I2≤30% was considered low and I2>30% was moderate; heterogeneity was high when I2>50%.
Funnel plots[21] were created and analyzed for publication bias using Duval and Tweedie’s Trim and Fill method for all factors reported in the quantitative synthesis.[22] If a factor of interest was reported separately for unilateral and bilateral tendinopathy, sex, or limb then the weighted pooled mean and variance was used in the analysis. In some studies, several measures of the same outcome were reported. In these cases, the weighted pooled mean and variance were also used to obtain a combined measure of effect. If a factor was discussed but insufficient data was reported to calculate a measure of effect, then the authors were contacted to request additional information.
Studies or factors not included in the meta-analysis were included in the qualitative summary. The strength of evidence for factors of interest was assessed using criteria established by Mallows et al. to synthesize non-randomized studies.[11] Each study was assigned a quality assessment score by dividing the stars awarded on the NOS by the number of available stars. Based on these scores, studies were classified as low (0.00–0.44, 1–4 stars), moderate (0.45–0.70, 5 or 6 stars), or high quality (0.71–1.00, 7–9 stars).[11] A rating system, adapted by Mallows et al.[11] from the Cochrane Collaboration Back Review Group,[23] was used to rate the level of evidence for each factor of interest, accounting for the quality and quantity of evidence (Table 1). A study was considered to have positive findings if significance testing was performed and the p-value was less than 0.05.
Table 1.
Levels of Evidence
| Strong evidence | Consistent findings in high-quality studies (n≥2) |
| Moderate evidence | Consistent findings among lower-quality studies (n>2) and/or one high-quality study |
| Limited evidence | (n≤2) relevant lower-quality studies |
| Conflicting evidence | Inconsistent findings among multiple studies |
| No evidence | No studies with significant findings |
RESULTS
Identification of studies
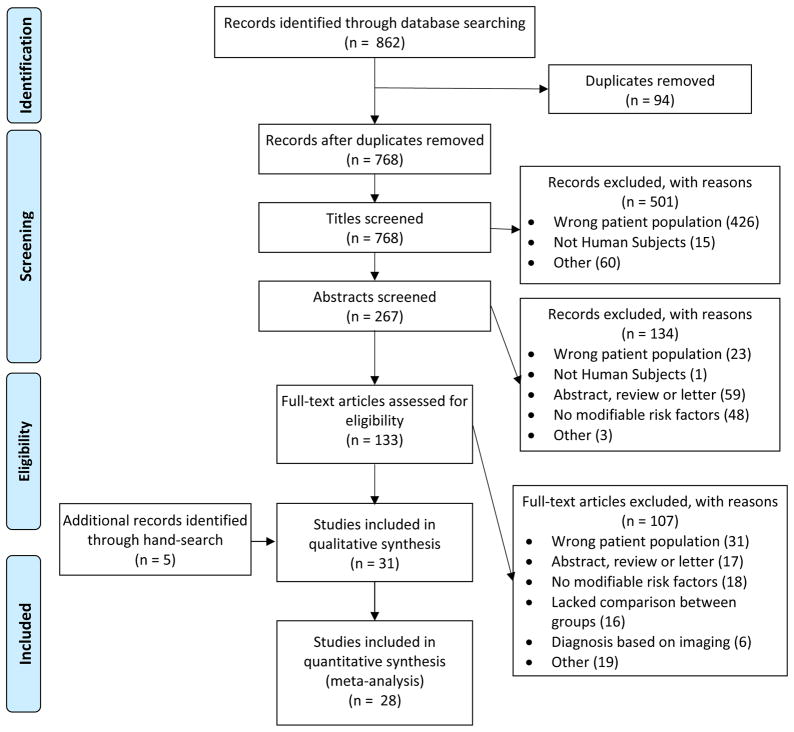
The initial search resulted in 862 studies (Figure 1). After removal of duplicates, 768 records were screened for inclusion and exclusion criteria. Following title and abstract review, 133 studies were appropriate for full-text review. 107 studies were excluded during full-text review, yielding 26 articles for inclusion. Inter-rater agreement ranged from moderate to almost perfect (Supplementary Material). Five additional articles were included after hand-searching references of included articles and retained systematic reviews, resulting in 31 included articles for qualitative review (Figure 1). Of these articles, 28 contained factors that were included in the quantitative synthesis (Figure 1). All included articles were in English. Authors provided additional information for five of eight articles for which additional information was requested.
Figure 1.
PRISMA flow diagram.
From: Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group (2009). Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med 6(7): e1000097. doi:10.1371/journal.pmed1000097
Study characteristics
Of the 31 studies considered, six were prospective. All six included young athletes, with mean ages under 30. The majority, 83% (5/6), played either volleyball or basketball, and consisted of elite athletes competing at the professional, national or international level (67%, 4/6) (Supplementary Material). Twenty-five studies were cross-sectional, and similarly 88% (22/25) had mean ages less than 30 years old. The majority of athletes were volleyball and basketball players (80%, 20/25); however only 32% (8/25) included elite athletes (Supplementary Material). The majority of prospective (86%, 6/7) and cross-sectional (56%, 14/25) studies included both sexes although, 40% (10/25) of cross-sectional studies consisted of only male athletes (Supplementary Material).
Risk-of-bias assessment
Prospective studies and cross-sectional studies each had a median NOS score of 5/9 points but there was greater variability in scores for cross-sectional studies (range: 1–8 points) than prospective studies (range: 4–6 points) (Table 2). All prospective studies used appropriate selection of a non-exposed cohort (Item 2) and had adequate follow-up (Item 7). One prospective study used independent blind assessment or medical record linkage to determine the presence of patellar tendinopathy (Item 6). All cross-sectional studies used the same method to determine the presence of factors of interest for cases and controls (Item 7) and 23 (92%) used community controls (Item 3). Two cross-sectional studies used secure records or a blinded exam to determine the presence of a factor of interest (Item 6). Inter-rater agreement was almost perfect (Supplementary Material). Upon visual inspection, using the Trim and Fill method, there did not appear to be evidence of publication bias for body mass index (BMI), bodyweight or activity volume for cross-sectional studies (Supplementary Material). Other items had too few studies to draw conclusions about publication bias.
Table 2.
Quality assessment scores on the Newcastle-Ottawa Scale (NOS) for included studies.
| Author (Year) | Potential Risk Factor or Associated Factor | Covariates Controlled | Selection | Comparability | Exposure/Outcome | Total Stars | Study Quality | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |||||
| Prospective Studies | ||||||||||||
|
| ||||||||||||
| de Vries et al. (2015)[24] | All investigated risk factors | Sex, Sport, Playing level | * | * | * | ** | * | 6 | Moderate | |||
| Visnes and Bahr (2013)[29] | Bodyweight, Waist Circumference, Skinfold Measurements | Sex | * | * | * | * | * | * | 6 | Moderate | ||
| Witvrouw et al. (2001)[28] | All investigated risk factors | Sex | * | * | * | * | * | * | 6 | Moderate | ||
| Backman et al. (2011)[23] | BMI, Bodyweight, Ankle Dorsiflexion ROM | * | * | * | * | * | 5 | Moderate | ||||
| Visnes and Bahr (2013)[27] | Volleyball Sets Per Week, Beach Volleyball Training Volume, Strength Training Volume, Jump Training Volume, Other Training Volume | Sex | * | * | * | * | * | 5 | Moderate | |||
| Visnes et al. (2013)[24] | All investigated risk factors | Sex | * | * | * | * | * | 5 | Moderate | |||
| Backman et al. (2011)[25] | Activity Volume, Sport-Specific Training Volume | * | * | * | * | 4 | Low | |||||
| Hagglund et al. (2011)[27] | All investigated risk factors | * | * | * | * | 4 | Low | |||||
|
| ||||||||||||
| Cross-Sectional Studies | ||||||||||||
|
| ||||||||||||
| Groot et al. (2016)[31] | All investigated factors | Age, Sex | * | * | * | * | ** | * | * | 8 | High | |
| Lian et al. (1996)[48] | All investigated factors | Age, Position, Playing Position, Training Volume | * | * | * | * | ** | * | * | 8 | High | |
| Lian et al. (2005)[2] | Weight Training Volume, Jump Training Volume | Age, Height, Weight, Experience at the Elite Level, Training Volume | * | * | * | * | ** | * | 7 | High | ||
| Morton et al. (2017)[32] | Activity Volume | Age, Sex | * | * | * | ** | * | * | 7 | High | ||
| Rio et al. (2016)[33] | Peak Knee Extension Isometric Torque, Corticospinal Excitability of the Quadriceps | Age, Activity Level | * | * | ** | * | * | * | 7 | High | ||
| Torres et al. (2016)[34] | All investigated factors | Sex, Playing Position | * | * | ** | * | * | * | 7 | High | ||
| Crossley et al. (2007)[30] | All investigated factors | Age, Height | * | * | ** | * | * | 6 | Moderate | |||
| Lian et al (2003)[42] | All investigated factors | * | * | * | * | * | * | 6 | Moderate | |||
| Rio et al. (2016)[33] | BMI | Age, Activity Level | * | * | ** | * | * | 6 | Moderate | |||
| Rosen et al. (2015)[49] | All investigated factors | Age, Sex Height, Weight | * | * | ** | * | * | 6 | Moderate | |||
| Siegmund et al. (2008)[50] | All investigated factors | Height, Weight, Playing Position, Playing Experience, Frequency of Play | * | * | ** | * | * | 6 | Moderate | |||
| Zhang et al. (2016)[37] | All investigated factors | Age, Sport | * | * | ** | * | * | 6 | Moderate | |||
| Bisseling et al. (2007)[38] | All investigated factors | * | * | * | * | * | 5 | Moderate | ||||
| Cassel et al. (2015)[39] | All investigated factors | * | * | * | * | * | 5 | Moderate | ||||
| Lian et al. (2005)[2] | Bodyweight, Activity Volume | * | * | * | * | * | 5 | Moderate | ||||
| Morton et al. (2017)[32] | BMI | * | * | * | * | * | 5 | Moderate | ||||
| Ferretti et al. (1984)[8] | All investigated factors | * | * | * | * | 4 | Low | |||||
| Longo et al. (2011)[43] | All investigated factors | * | * | * | * | 4 | Low | |||||
| Malliaras et al. (2006)[46] | All investigated factors | * | * | * | * | 4 | Low | |||||
| Scattone Silva et al. (2016)[44] | All investigated factors | * | * | * | * | 4 | Low | |||||
| Van der Worp et al. (2011)[52] | All investigated factors | Age, Sex | * | ** | * | 4 | Low | |||||
| Van der Worp et al. (2012)[35] | All investigated factors | Age, Sex, BMI, Sport | * | ** | * | 4 | Low | |||||
| Van Wilgen et al. (2013)[36] | All investigated factors | * | * | * | * | 4 | Low | |||||
| Zwerver et al. (2011)[3] | All investigated factors | * | * | * | * | 4 | Low | |||||
| Bode et al. (2008)[45] | All investigated factors | * | * | * | 3 | Low | ||||||
| Dauty et al. (2007)[38] | All investigated factors | * | * | * | 3 | Low | ||||||
| Kujala et al. (1986)[40] | All investigated factors | * | * | 2 | Low | |||||||
| Krauss et al. (2007)[51] | All investigated factors | * | 1 | Low | ||||||||
“All investigated (risk) factors” indicates that the quality assessment scores were identical for all factors of interest included in the study. BMI = Body mass index, ROM = Range-of-motion. The cohort-version of the NOS was used for prospective studies and the case-control version was used for cross-sectional studies.
Prospective studies: Potential Risk factors
Quantitative synthesis: Meta-analysis
Anthropometrics
Bodyweight was the only prospectively investigated factor appropriate for meta-analysis. Five studies[24–28] with high heterogeneity (I2=55.7) were included. Bodyweight was not significantly associated with risk of patellar tendinopathy (p=0.08) (Supplementary Material).
Qualitative synthesis
Joint range-of-motion and muscle length
Limited evidence from individual moderate quality studies supported decreased ankle dorsiflexion range-of-motion,[25] posterior thigh flexibility,[28] and quadriceps flexibility[28] as potential risk factors (Table 3).
Table 3.
Strength of evidence for potential risk factors (prospective studies) included in qualitative synthesis.
| Potential Risk Factor | Study | Study Quality | Positive Findings | Level of Evidence |
|---|---|---|---|---|
| Anthropometrics | ||||
|
| ||||
| BMI | Backman et al. (2011) | Moderate | No | No evidence |
| de Vries et al. (2015) | Moderate | No | ||
|
| ||||
| Waist Circumference | Visnes and Bahr (2013) | Moderate | No | No evidence. |
|
| ||||
| Skin-fold Measures | Visnes and Bahr (2013) | Moderate | No | No evidence. |
|
| ||||
| Joint Range-of-Motion and Muscle Length | ||||
|
| ||||
| Ankle dorsiflexion ROM | Backman et al. (2011) | Moderate | Yes | Limited evidence for decreased ankle dorsiflexion ROM. |
|
| ||||
| Posterior Thigh Flexibility | Witvrouw et al. (2001) | Moderate | Yes | Limited evidence for decreased posterior thigh flexibility |
|
| ||||
| Quadriceps Flexibility | Witvrouw et al. (2001) | Moderate | Yes | Limited evidence for decreased quadriceps flexibility. |
|
| ||||
| Sports and Activity Related Factors | ||||
|
| ||||
| Activity Volume | de Vries et al. (2015) | Moderate | No | Conflicting evidence for increased activity volume. |
| Visnes et al. (2013) | Moderate | Yes | ||
| Backman et al. (2011) | Low | No | ||
| Hagglund et al. (2011) | Low | Yes | ||
|
| ||||
| Strength Training Volume | Visnes and Bahr (2013) | Moderate | No | No evidence. |
|
| ||||
| Jump Training Volume | Visnes and Bahr (2013) | Moderate | Yes | Limited evidence for greater volume of jump training per week. |
|
| ||||
| Sport Surface | de Vries et al. (2015) | Moderate | No | No evidence. |
| Hagglund et al. (2011) | Low | No | ||
|
| ||||
| Sport Specific Training Volume | Backman et al. (2011) | Low | No | No evidence. |
|
| ||||
| Volleyball Sets Played Per Week | Visnes and Bahr (2013) | Moderate | Yes | Limited evidence for greater number of volleyball sets played per week. |
|
| ||||
| Beach Volleyball Training Volume | Visnes and Bahr (2013) | Moderate | No | No evidence. |
|
| ||||
| Training Volume in Sports Other Than Primary Sport (Volleyball or Basketball) | de Vries et al. (2015) | Moderate | No | No evidence. |
| Visnes and Bahr (2013) | Moderate | No | ||
|
| ||||
| Training/Match Exposure Ratio | Hagglund et al. (2011) | Low | No | No evidence |
|
| ||||
| Functional Testing | ||||
|
| ||||
| CMJ Height | Visnes et al. (2013) | Moderate | Yes | Limited evidence for greater CMJ height in men. No evidence in women. |
|
| ||||
| Standing Jump Height | Visnes et al. (2013) | Moderate | No | No evidence. |
|
| ||||
| Muscle Performance | ||||
|
| ||||
| Knee Extension Torque | Witvrouw et al. (2001) | Moderate | No | No evidence. |
|
| ||||
| Knee Flexion Torque | Witvrouw et al. (2001) | Moderate | No | No evidence. |
|
| ||||
| Occupational Demands | ||||
|
| ||||
| Occupational Classification | de Vries et al. (2015) | Moderate | No | No evidence. |
|
| ||||
| Knee Loading During Work | de Vries et al. (2015) | Moderate | No | No evidence. |
BMI = Body mass index, ROM = Range-of-motion, CMJ = Counter-movement jump
Sports and activity related factors
Limited evidence from one moderate quality study supported greater volume of jump training and greater number of volleyball sets played per week as potential risk factors.[29] There was conflicting evidence from four moderate to low quality studies for increased activity volume as a potential risk factor (Table 3).[24–27]
Functional testing
There was limited evidence from one moderate quality study supporting greater counter-movement jump height as a potential risk factor in male athletes (Table 3).[26]
Cross-sectional studies: Associated Modifiable Factors
Quantitative synthesis: Meta-analysis
Anthropometrics
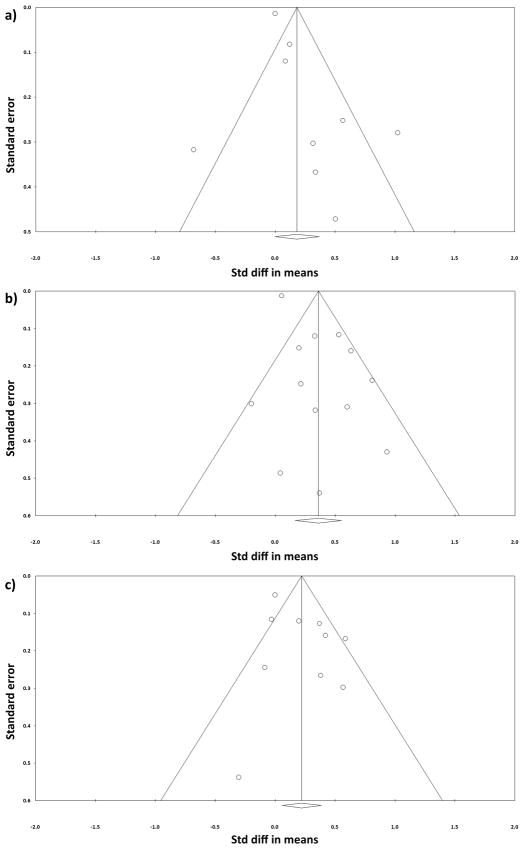
BMI and bodyweight were appropriate for meta-analysis. For BMI, nine studies with high heterogeneity (I2=71.7) were included in the meta-analysis (Supplementary Material).[3,30–37] BMI was not significantly associated with patellar tendinopathy (p=0.06) (Supplementary Material). One low quality study[3] was excluded from the meta-analysis due to insufficient data but the reported results were in agreement with the quantitative synthesis. For bodyweight, 13 studies with high heterogeneity (I2=77.8) were included in the meta-analysis (Figure 2).[2,3,30,35,37–44] There was a small, positive effect for bodyweight, indicating that greater bodyweight is significantly associated with patellar tendinopathy (Figure 2). This effect translates to an odds ratio of 1.92 (95% CI: 1.35 to 2.73). One low quality study was excluded due to insufficient data.[45] In this study, weight did not differ significantly between young elite soccer players with or without patellar tendinopathy.
Figure 2.
Standardized mean difference (Cohen’s d) with 95% CI for a) bodyweight, b) activity volume and c) CMJ height as associated modifiable factors.
Sport and activity related factors
Activity volume was appropriate for meta-analysis. Ten studies with high heterogeneity (I2=67.0) were included (Figure 2).[2,3,8,30,32,35,39,42,44,46] There was a small, positive effect for activity volume, indicating that greater activity volume is significantly associated with patellar tendinopathy (Figure 2). This effect translates to an odds ratio of 1.50 (95% CI: 1.11 to 2.02). Two low quality studies and one high quality study were excluded due to insufficient data. These studies did not find a significant association between hours of weekly sports participation[3] or training[31,45] and patellar tendinopathy.
Functional testing
Counter-movement jump (CMJ) height was appropriate for meta-analysis. The CMJ height included performance on the CMJ, drop CMJ and vertical jump, as these measures allow a counter movement and assess an athlete’s ability to utilize the stretch-shortening cycle.[47] Five studies with moderate heterogeneity (I2=44.2) were included (Figure 2).[42,46,48–50] There was a small, positive effect for CMJ height, indicating that greater CMJ height is associated with patellar tendinopathy (Figure 2). This effect translates to an odds ratio of 1.77 (95% CI: 1.13 to 2.77).
Muscle performance
Knee extension torque production was appropriate for meta-analysis. Five studies with high heterogeneity (I2=89.7) were included (Supplementary Material).[33,40,41,44,51] Knee extension torque production was not significantly associated with patellar tendinopathy (p=0.19) (Supplementary Material).
Qualitative synthesis
Joint range-of-motion and muscle length
There was conflicting evidence from three moderate to low quality studies for decreased ankle dorsiflexion range-of-motion and altered posterior thigh flexibility as associated modifiable factors (Table 4).[30,44,46]
Table 4.
Strength of evidence for associated modifiable factors (cross-sectional studies) included in qualitative synthesis.
| Associated Modifiable Factor | Study | Study Quality | Positive Findings | Level of Evidence |
|---|---|---|---|---|
| Anthropometrics | ||||
|
| ||||
| Waist Circumference | Van der Worp et al. (2012) | Low | No | No evidence. |
|
| ||||
| Hip Circumference | Van der Worp et al. (2012) | Low | No | No evidence. |
|
| ||||
| Waist-to-hip Ratio | Van der Worp et al. (2012) | Low | No | No evidence. |
|
| ||||
| Joint Range-of-Motion and Muscle Length | ||||
|
| ||||
| Ankle Dorsiflexion ROM | Crossley et al. (2007) | Moderate | No | Conflicting evidence for decreased ankle dorsiflexion ROM. |
| Malliaras et al. (2006) | Low | Yes | ||
| Scattone Silva et al. (2016) | Low | Yes | ||
|
| ||||
| Posterior Thigh Flexibility | Crosley et al. (2007) | Moderate | Yes | Conflicting evidence for both increased and decreased posterior thigh flexibility. |
| Malliaras et al. (2006) | Low | No | ||
| Scattone Silva et al. (2016) | Low | Yes | ||
|
| ||||
| Quadriceps Flexibility | Scattone Silva et al. (2016) | Low | No | No evidence. |
|
| ||||
| Knee Extension ROM | Kujala et al. (1986) | Low | No | No evidence. |
|
| ||||
| Sports and Activity Related Factors | ||||
|
| ||||
| Strength Training Volume | Lian et al. (2005) | High | Yes | Moderate evidence for greater volume of strength training per week. |
| Lian et al. (2003) | Moderate | Yes | ||
|
| ||||
| Jump Training Volume | Lian et al. (2005) | High | No | Conflicting evidence for greater volume of jump training per week. |
| Lian et al. (2003) | Moderate | Yes | ||
|
| ||||
| Sport Surface | Bode et al. (2017) | Low | No | No evidence. |
| Ferretti et al. (1984) | Low | Not Tested | ||
| Krauss et al. (2007) | Low | No | ||
| van der Worp et al. (2012) | Low | No | ||
|
| ||||
| Running Workouts per Week | Krauss et al. (2007) | Low | No | No evidence. |
|
| ||||
| Weekly Running Mileage | Krauss et al. (2007) | Low | No | No evidence. |
|
| ||||
| Running Speed | Krauss et al. (2007) | Low | Yes | Limited evidence for running at a slower average pace. |
|
| ||||
| Impact Profile of Sport | Longo et al. (2011) | Low | No | No evidence. |
|
| ||||
| Sport Specific Training Volume | Lian et al. (2003) | Moderate | No | No evidence. |
|
| ||||
| Quantity of Stretching Before or After Training | Lian et al. (2003) | Moderate | No | No evidence. |
|
| ||||
| Shoe Type | Bode et al. (2017) | Low | No | No evidence. |
|
| ||||
| Insole Use | Bode et al. (2017) | Low | No | No evidence. |
|
| ||||
| Functional Testing | ||||
|
| ||||
| Standing Jump Height | Lian et al. (1996) | High | Yes | Conflicting evidence for greater standing jump height with a 20-kg load. No evidence for greater jump height without an external load or with a ½ BW load. |
| Lian et al. (2003) | Moderate | No | ||
|
| ||||
| Standing Jump Work | Lian et al. (1996) | High | Yes | Conflicting evidence for greater work performed during the standing jump. |
| Lian et al. (2003) | Moderate | No | ||
|
| ||||
| Average Force during Standing Jump | Lian et al. (2003) | Moderate | Yes | Limited evidence for greater average force during a standing jump with a ½-BW or a 1-BW load. |
|
| ||||
| Average Power During Standing Jump | Lian et al. (2003) | Moderate | Yes | Limited evidence for greater average power during a standing jump with a ½-BW or a 1-BW load. |
|
| ||||
| Average Velocity During Standing Jump | Lian et al. (2003) | Moderate | No | No evidence. |
|
| ||||
| CMJ Work | Lian et al. (1996) | High | Yes | Conflicting evidence for greater CMJ work. |
| Lian et al. (2003) | Moderate | No | ||
|
| ||||
| Drop CMJ Work | Lian et al. (2003) | Moderate | Yes | Limited evidence for greater drop CMJ work from a 45 cm height. |
|
| ||||
| CMJ-Standing Jump Height | Lian et al. (1996) | High | Yes | Conflicting evidence for greater CMJ-standing jump height. |
| Lian et al. (2003) | Moderate | No | ||
|
| ||||
| Average Power on 15-Second Rebound Test | Lian et al. (1996) | High | Yes | Conflicting evidence for greater average power on the 15-second rebound. |
| Lian et al. (2003) | Moderate | No | ||
|
| ||||
| Jump Test Composite Score | Lian et al. (2003) | Moderate | Yes | Limited evidence for better performance on a battery of jump tests. |
|
| ||||
| 6-Meter Hop Test Time | Crossley et al. (2007) | Moderate | No | No evidence. |
|
| ||||
| Hop for Distance | Crossley et al. (2007) | Moderate | No | No evidence. |
|
| ||||
| Muscle Performance | ||||
|
| ||||
| Knee Flexion Torque | Dauty et al. (2007) | Low | No | No evidence. |
| Krauss et al. (2007) | Low | No | ||
| Kujala et al. (1986) | Low | No | ||
|
| ||||
| Plantarflexion Endurance | Crossley et al. (2007) | Moderate | No | No evidence. |
| Malliaras et al. (2006) | Low | No | ||
|
| ||||
| Normalized Peak Plantarflexion Torque | Scattone Silva et al. (2016) | Low | No | No evidence. |
|
| ||||
| Knee Extension Fatigue Ratio | Dauty et al. (2007) | Low | Yes | Limited evidence for decreased knee extension fatigue ratio. |
|
| ||||
| Knee Flexion Fatigue Ratio | Dauty et al. (2007) | Low | No | No evidence. |
|
| ||||
| Knee Extension Eccentric Endurance Quotient | Krauss et al. (2007) | Low | Not Tested | No evidence. |
|
| ||||
| Knee Flexion Eccentric Endurance Quotient | Krauss et al. (2007) | Low | Not Tested | No evidence. |
|
| ||||
| Concentric Hamstring to Quadriceps Quotient | Krauss et al. (2007) | Low | No | No evidence. |
|
| ||||
| Normalized Peak Hip Extension Torque | Scattone Silva et al. (2016) | Low | Yes | Limited evidence for decreased normalized hip extension torque. |
|
| ||||
| Stimulus Response Curve for the Motor Evoked Potential of the Quadriceps | Rio et al. (2016) | High | Yes | Moderate evidence for a steeper slope to the motor evoked potential curve for the quadriceps. |
|
| ||||
| Occupational Demands | ||||
|
| ||||
| Occupational Classification | van der Worp et al. (2011) | Low | Yes | Limited evidence for heavy physically demanding work. |
|
| ||||
| Knee Loading During Work | van der Worp et al. (2011) | Low | No | No evidence. |
ROM = Range-of-motion, BW = Bodyweight, CMJ = Counter-movement jump
Sport and activity related factors
Moderate evidence from one high and one moderate quality study supported greater volume of strength training per week as an associated modifiable factor (Table 4).[2,42] Limited evidence from one low quality study supported slower average running pace as an associated modifiable factor (Table 4).[51] There was conflicting evidence from one high and one moderate quality study for greater volume of jump training per week as associated modifiable factors (Table 4).[2,42]
Functional testing
Limited evidence from one moderate quality study supported greater average force and power with a ½- or 1-bodyweight load during a standing jump, greater work performed during a drop CMJ, and better performance on a jump test battery as associated modifiable factors (Table 4).[42] There was conflicting evidence from one high quality and one moderate quality study for greater standing jump height with a 20-kg load, work performed during a standing jump or CMJ, difference between CMJ and standing jump height, and average power on 15-second rebound test as associated modifiable factors (Table 4).[42,48]
Muscle performance
Moderate evidence from one high quality study supported a steeper slope for the motor evoked potential curve of the quadriceps, representing altered corticospinal excitability to the quadriceps, as an associated modifiable factor (Table 4).[33] Limited evidence from individual low quality studies supported decreased knee extension fatigue ratio[40] and normalized peak hip extension torque[44] as associated modifiable factors (Table 4).
Occupational demands
Limited evidence from one low quality study supported heavy physically demanding work as an associated modifiable factor (Table 4).[52]
DISCUSSION
Main findings
There is a lack of strong evidence for any prospectively investigated potential modifiable risk factors for patellar tendinopathy. However, there was limited or conflicting evidence that decreased ankle dorsiflexion range-of-motion, decreased posterior thigh and quadriceps flexibility, greater volume of jump training, more volleyball sets played per week, greater CMJ height, and greater activity volume are potential modifiable risk factors for patellar tendinopathy. Additionally, there was a lack of strong evidence for any associated modifiable factor reported in cross-sectional studies. Moderate to conflicting evidence supported greater volume of strength training, better jumping performance, less normalized hip extension torque, decreased knee extension fatigue ratio, and altered corticospinal excitability to the quadriceps as associated modifiable factors.
Risk-of-bias and study quality
In agreement with the findings of van der Worp et al., there were few prospective studies investigating risks factors and none were high quality.[6] Many of the cross-sectional studies were low quality and nearly half failed to control for covariates, which limits the strength of evidence for associated modifiable factors. However, there was no evidence of publication bias in the meta-analysis of BMI, bodyweight or activity volume in cross-sectional studies. In light of these findings, additional high-quality, prospective studies are needed.
Anthropometric measures
A systematic review by Gaida et al.[53] found that adiposity, including the surrogate measures of BMI and body weight, is frequently associated with tendinopathy and may be a risk factor for tendon injuries. In contrast, this study found no evidence supporting anthropometric measures as potential risk factors for patellar tendinopathy. Although a small, positive effect was found for bodyweight in cross-sectional studies, suggesting that greater bodyweight is an associated modifiable factor, bodyweight was not significantly associated with an increased risk of patellar tendinopathy in prospective studies. Patellar tendinopathy is most common in young athletic individuals[3] and the majority of studies included in this review were conducted in elite athletes. Therefore, it is unlikely that the athletes in these studies had high adiposity. Instead, higher body weight likely reflects a taller stature and a build that is more muscular.[54]
Joint range-of-motion and muscle length
Individual moderate quality prospective studies identified decreased ankle dorsiflexion range-of-motion, posterior thigh flexibility and quadriceps flexibility as potential risk factors for patellar tendinopathy. In one prospective and one cross-sectional study, athletes had a higher risk of patellar tendinopathy if their dorsiflexion range-of-motion fell below cut-off scores of 36.5°[25] or 45.0°,[46] respectively. When jumping, adequate ankle joint range-of-motion is of importance since the ankle is responsible for absorbing 37% to 50% of the total kinetic energy during the landing phase.[55] Additionally, decreased dorsiflexion is moderately correlated with higher ground reaction forces during a drop landing task.[56] This increase in ground reaction force, coupled with potentially altered ability to absorb kinetic energy at the ankle, may increase patellar tendon loads. Furthermore, decreased ankle weight-bearing dorsiflexion range-of-motion results in altered knee kinematics during squatting,[57] which may increase patellar tendon loads during athletic activities.[15] It is hypothesized that decreased posterior thigh flexibility may contribute to patellar tendon overload by decreasing the mechanical advantage of the extensor mechanism and increasing the demands placed on the quadriceps during knee extension.[44] Similarly, decreased quadriceps flexibility may contribute to overload by increasing passive tension within the patellar tendon.[37] Based on the limited evidence, clinicians may want to assess for restrictions in these measures but further research using high quality, prospective study designs is warranted.
Sport and activity related factors
Patellar tendinopathy is considered an overuse injury so an association between higher levels of activity or training and injury is expected.[58] Therefore, the limited or conflicting evidence from prospective studies regarding volume of activity or jump training and the small effect from cross-sectional studies for activity volume is surprising. This may be explained in part by the composition of the studies and how activity was defined. The plurality of studies consisted of elite athletes so the participants are likely completing a high volume of training and there is minimal variability between groups. Additionally, activity was typically reported as a duration, with no indication of the intensity, type of activity, or whether activity level had changed. Activity duration alone may not accurately describe the load-placed on the patellar tendon or the tendon’s readiness to accommodate those loads. Thus, future studies should examine patellar tendon load during activity and the relationship between current and previous level of activity to provide a more complete picture of how activity contributes to patellar tendinopathy. Although there was no evidence from the sole prospective study investigating weekly strength training volume, there was moderate evidence from two cross-sectional studies that greater weekly strength training volume may be an associated modifiable factor. In designing prevention or rehabilitation programs, clinicians may want to consider altering the volume of activity, jump or strength training to reduce cumulative tendon load. Additionally, other parameters, such as intensity, activity type and prior activity level, and their relationship to recovery should be considered.
Functional testing
Although greater CMJ height is the only measures with prospective support, limited or conflicting evidence identified higher values on other metrics of jump performance as associated modifiable factors. This suggests that athletes with greater jumping ability are at higher risk of developing patellar tendinopathy. With greater jumping ability, athletes are likely generating greater forces at take-off[59] and must dissipate greater vertical ground reaction forces at landing.[60] As a result, they experience a higher cumulative load on the extensor apparatus for a given jump. These athletes may also be completing a higher quantity or frequency of jumps since they likely have more opportunities to play and are more involved while on the court. A recent systematic review of the relationship between jump biomechanics and patellar tendinopathy identified a “stiff” landing pattern as a potential risk factor for patellar tendinopathy.[15] The authors also emphasized that adequate lower extremity flexibility and range-of-motion are necessary to utilize a more flexible landing pattern, which may be protective against patellar tendinopathy. Since better jumping ability is desirable in an athletic population, clinicians should consider modifying landing biomechanics and lower extremity flexibility and range-of-motion instead to reduce the risk of injury.
Muscle performance
There was no evidence from prospective studies or a meta-analysis of cross-sectional studies that knee extension torque production was associated with patellar tendinopathy. However, there was moderate to limited evidence from individual cross-sectional study that altered corticospinal excitability to the quadriceps and decreased knee extension fatigue ratio may be an associated modifiable factor. This suggests that quadriceps muscle performance may be altered in patellar tendinopathy but this alteration may not be captured by torque production alone. Participation in jumping sports requires rapid force development, high levels of lower extremity power, and multi-joint coordination.[61] Additionally, these muscle performance tests are typically performed in a rested state and do not assess how these measures may change with fatigue. It should be noted that knee extension torque was the only muscle performance measure relating to the quadriceps that was prospectively investigated. Thus, further research is warranted to determine if other measures of quadriceps muscle performance, such as fatigue resistance, endurance, power and muscle activation, are related to the development of patellar tendinopathy.
There was also limited evidence supporting decreased normalized hip extension torque as an associated modifiable factor. During landing tasks, the hip extensors are responsible for dissipating 20 to 25% of the kinetic energy absorbed by the lower extremities.[55] Therefore, decreased hip extensor strength may increase demands placed on the knee extensors. Furthermore, the contribution of the hip extensors to energy dissipation increases when utilizing a softer landing strategy.[55,62] To compensate for decreased hip extension strength, individuals may adopt a stiffer landing strategy, which has been previously identified as a potential risk factor for patellar tendinopathy.[15] Clinicians may want to assess for hip extension strength deficits in prevention programs, although prospective studies are needed to confirm if this deficit is a risk factor for patellar tendinopathy.
Occupational demands
There was no prospective evidence that occupational classification (e.g. heavy vs. light physically demanding work) is a potential risk factor for patellar tendinopathy. However, there was limited evidence from one cross-sectional study that heavy physically demanding work may be an associated modifiable factor. Given the limited evidence and lack of prospective support, it is unlikely that occupational classification is a risk factor for patellar tendinopathy.
Patellar tendinopathy and tendon load
Patellar tendinopathy is considered an overuse injury resulting from repetitive stress to the patellar tendon with insufficient recovery.[63] This is supported by the findings of this systematic review and meta-analysis, as each of the potential modifiable risk factors with support from prospective studies may directly or indirectly increase the loads placed on the patellar tendon. However, some of these risk factors, such as jumping ability, may be beneficial to athletic performance and undesirable to change. Therefore, clinicians may need to manipulate other training parameters to reduce the cumulative load on the tendon or increase recovery time between activities.
Limitations
There were several limitations to our review. First, different versions of the NOS were used for prospective and cross-sectional studies. Therefore, quality assessment ratings are not comparable between study designs. Although certain cross-sectional studies scored higher than prospective studies, the cross-sectional studies are not able to establish a temporal relationship between the factor of interest and patellar tendinopathy. Second, included studies encompassed a variety of populations, methods and research questions, which is reflected in the high heterogeneity between studies. A consequence of high heterogeneity is that the calculated effect may be due to the differences in study design or populations evaluated, not true differences in the outcome of interest.[20] To address this limitation, a random-effects model was used when heterogeneity was high, as this provides a more conservative estimate of the effect size. Third, many potential risk factors or associated factors were investigated by a limited number of studies and many of these, especially for cross-sectional studies, had small sample sizes. This limits the strength of evidence for these items and lack of support does not indicate that an item of interest is definitely not associated with patellar tendinopathy. Therefore, clinicians should use their clinical judgement and not completely disregard other potential risk factors when creating an individualized prevention program. Fourth, a large portion of these studies were conducted in male, elite athletes. Although this is representative of the population most commonly diagnosed with patellar tendinopathy, it may limit generalizability to female and recreational athletes. Finally, there was large variability between definitions of patellar tendinopathy, which was expected, as the definition of patellar tendinopathy has shifted over time. However, this potentially introduces bias by incorporating individuals with other diagnosis. Despite this concern, the decision was made to include broader definitions of patellar tendinopathy, as the prevalence of other diagnosis is typically low compared to true patellar tendinopathy and we did not want to exclude a large body of previous research.[8]
CONCLUSIONS
There was limited or conflicting evidence that decreased ankle dorsiflexion range-of-motion, decreased posterior thigh and quadriceps flexibility, greater volume of jump training, more volleyball sets played per week, greater CMJ height, and greater activity volume are potential modifiable risk factors for patellar tendinopathy. However, this evidence is based on few moderate or low quality prospective studies.
Supplementary Material
Summary Box.
What is already known?
Patellar tendinopathy is extremely common in athletes that participate in jumping sports and many will experience recurrent symptoms after treatment.
Symptoms of patellar tendinopathy are load dependent, with increased loads resulting in a greater degree of pain.
Numerous risk factors have been proposed for patellar tendinopathy but not all are modifiable.
What are the new findings?
There was limited or conflicting evidence that decreased ankle dorsiflexion range-of-motion, decreased posterior thigh and quadriceps flexibility, greater volume of jump training, more volleyball sets played per week, greater CMJ height, and greater activity volume are potential modifiable risk factors for patellar tendinopathy.
Moderate to conflicting evidence supported greater volume of strength training, better jumping performance, less normalized hip extension torque, decreased knee extension fatigue ratio, and altered corticospinal excitability to the quadriceps as associated modifiable factors.
There is a lack of strong evidence for any potential modifiable risk factors or associated modifiable factors for patellar tendinopathy, highlighting the need for high-quality, prospective studies of risk factors for patellar tendinopathy.
Acknowledgments
The authors would like to express their gratitude to Sarah Katz for her assistance in designing the search strategy, Barbara Wondrasch for her assistance in translating articles during the screening process and the authors that were able to provide additional information about their studies.
FUNDING: The research was funded in part by the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institute of Health (#T32HD007490-18) and by a Florence P. Kendall Doctoral Scholarship and a Promotion of Doctoral Studies I Scholarship from the Foundation for Physical Therapy.
Footnotes
CONTRIBUTORS: ALS, AHS and KGS were responsible for the concept and design of this study, as well as the article screening process. ALS and PK conducted the quality assessment and data extraction. RP provided statistical expertise. All authors assisted with interpretation of results and revision of the manuscript.
References
- 1.Malliaras P, Cook J, Purdam C, et al. Patellar tendinopathy: Clinical diagnosis, load management, and advice for challenging case presentations. J Orthop Sport Phys Ther. 2015;45:887–98. doi: 10.2519/jospt.2015.5987. [DOI] [PubMed] [Google Scholar]
- 2.Lian Ø, Refsnes P-E, Engebretsen L, et al. Prevalence of jumper’s knee among elite athletes from different sports. Am J Sports Med. 2005;31:408–13. doi: 10.1177/0363546504270454. [DOI] [PubMed] [Google Scholar]
- 3.Zwerver J, Bredeweg SW, van den Akker-Scheek I. Prevalence of Jumper’s knee among nonelite athletes from different sports: a cross-sectional survey. Am J Sports Med. 2011;39:1984–8. doi: 10.1177/0363546511413370. [DOI] [PubMed] [Google Scholar]
- 4.Cook JL, Khan KM, Harcourt PR, et al. A cross sectional study of 100 athletes with jumper’s knee managed conservatively and surgically. The Victorian Institute of Sport Tendon Study Group. Br J Sports Med. 1997;31:332–6. doi: 10.1136/bjsm.31.4.332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kettunen Ja, Kvist M, Alanen E, et al. Long-term prognosis for jumper’s knee in male athletes. A prospective follow-up study. Am J Sports Med. 2002;30:689–92. doi: 10.1177/03635465020300051001. [DOI] [PubMed] [Google Scholar]
- 6.van der Worp H, van Ark M, Roerink S, et al. Risk factors for patellar tendinopathy: a systematic review of the literature. Br J Sports Med. 2011;45:446–52. doi: 10.1136/bjsm.2011.084079. [DOI] [PubMed] [Google Scholar]
- 7.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62:e1–34. doi: 10.1016/j.jclinepi.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 8.Ferretti A, Puddu G, Mariani PP, et al. Jumper’s knee: An epidemiological study of volleyball players. Phys Sportsmed. 1984;12:97–106. [Google Scholar]
- 9.Cook JL, Khan KM, Kiss ZS, et al. Asymptomatic hypoechoic regions on patellar tendon ultrasound: A 4-year clinical and ultrasound followup of 46 tendons. Scand J Med Sci Sports. 2001;11:321–7. doi: 10.1034/j.1600-0838.2001.110602.x. [DOI] [PubMed] [Google Scholar]
- 10.Wells GA, Shea B, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses. Ottawa Hosp Res Inst. 2013:1–4. [Google Scholar]
- 11.Mallows A, Debenham J, Walker T, et al. Association of psychological variables and outcome in tendinopathy: a systematic review. Br J Sports Med. 2017;51:743–8. doi: 10.1136/bjsports-2016-096154. [DOI] [PubMed] [Google Scholar]
- 12.Toohey LA, Drew MK, Cook JL, et al. Is subsequent lower limb injury associated with previous injury? A systematic review and meta-analysis. Br J Sports Med. 2017 doi: 10.1136/bjsports-2017-097500. bjsports-2017-097500. [DOI] [PubMed] [Google Scholar]
- 13.Deeks JJ, Dinnes J, D’Amico R, et al. Evaluating non-randomised intervention studies. Health Technol Assess (Rockv) 2003:7. doi: 10.3310/hta7270. [DOI] [PubMed] [Google Scholar]
- 14.Mcauliffe S, Mccreesh K, Culloty F, et al. Can ultrasound imaging predict the development of Achilles and patellar tendinopathy? A systematic review and meta-analysis. Br J Sport Med. 2016;50:1516–23. doi: 10.1136/bjsports-2016-096288. [DOI] [PubMed] [Google Scholar]
- 15.van der Worp H, de Poel HJ, Diercks RL, et al. Jumper’s knee or lander’s knee? A systematic review of the relation between jump biomechanics and patellar tendinopathy. Int J Sports Med. 2014;35:714–22. doi: 10.1055/s-0033-1358674. [DOI] [PubMed] [Google Scholar]
- 16.Cohen J. A Coefficient of agreemnet for nominal scales. Educ Psychol Meas. 1960;20:37–46. [Google Scholar]
- 17.Landis JR, Koch GG. The Measurement of Observer Agreement for Categorical Data Published by : International Biometric Society Stable URL : http://www.jstor.org/stable/2529310. Biometrics. 1977;33:159–74. [PubMed] [Google Scholar]
- 18.Cohen J. Statistical power analysis for the behavioral sciences. Stat Power Anal Behav Sci. 1988;2:567. [Google Scholar]
- 19.Szumilas M. Explaining odds ratios. J Can Acad Child Adolesc Psychiatry. 2010;19:227–9. [PMC free article] [PubMed] [Google Scholar]
- 20.Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–58. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 21.Egger M, Davey Smith G, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–34. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Duval S, Tweedie R. Trim and Fill: A Simple Funnel-Plot-Based Method of Testing and Adjusting for Publication Bias in Meta-Analysis. Biometrics. 2000;56:455–63. doi: 10.1111/j.0006-341x.2000.00455.x. [DOI] [PubMed] [Google Scholar]
- 23.van Tulder M, Furlan A, Bombardier C, et al. Updated Method Guidelines for Systematic Reviews in the Cochrane Collaboration Back Review Group. Spine (Phila Pa 1976) 2003;28:1290–9. doi: 10.1097/01.BRS.0000065484.95996.AF. [DOI] [PubMed] [Google Scholar]
- 24.de Vries AJ, van der Worp H, Diercks RL, et al. Risk factors for patellar tendinopathy in volleyball and basketball players: A survey-based prospective cohort study. Scand J Med Sci Sports. 2015;25:678–84. doi: 10.1111/sms.12294. [DOI] [PubMed] [Google Scholar]
- 25.Backman LJ, Danielson P. Low range of ankle dorsiflexion predisposes for patellar tendinopathy in junior elite basketball players: A 1-year prospective study. Am J Sports Med. 2011;39:2626–33. doi: 10.1177/0363546511420552. [DOI] [PubMed] [Google Scholar]
- 26.Visnes H, Aandahl HÅ, Bahr R. Jumper’s knee paradox—jumping ability is a risk factor for developing jumper’s knee: a 5-year prospective study. Br J Sports Med. 2013;47:503–7. doi: 10.1136/bjsports-2012-091385. [DOI] [PubMed] [Google Scholar]
- 27.Hägglund M, Zwerver J, Ekstrand J. Epidemiology of patellar tendinopathy in elite male soccer players. Am J Sports Med. 2011;39:1906–11. doi: 10.1177/0363546511408877. [DOI] [PubMed] [Google Scholar]
- 28.Witvrouw E, Bellemans J, Lysens R, et al. Intrinsic risk factors for the development of patellar tendinitis in an athletic population. A two-year prospective study. Am J Sports Med. 2001;29:190–5. doi: 10.1177/03635465010290021201. [DOI] [PubMed] [Google Scholar]
- 29.Visnes H, Bahr R. Training volume and body composition as risk factors for developing jumper’s knee among young elite volleyball players. Scand J Med Sci Sports. 2013;23:607–13. doi: 10.1111/j.1600-0838.2011.01430.x. [DOI] [PubMed] [Google Scholar]
- 30.Crossley KM, Thancanamootoo K, Metcalf BR, et al. Clinical features of patellar tendinopathy and their implications for rehabilitation. J Orthop Res. 2007;25:1164–75. doi: 10.1002/jor.20415. [DOI] [PubMed] [Google Scholar]
- 31.Groot HE, van der Worp H, Nijenbanning L, et al. Is proprioception diminished in patients with patellar tendinopathy? Gait Posture. 2016;45:224–8. doi: 10.1016/j.gaitpost.2016.02.010. [DOI] [PubMed] [Google Scholar]
- 32.Morton S, Williams S, Valle X, et al. Patellar tendinopathy and potential risk factors: An international database of cases and controls. Clin J Sport Med. 2017;27:468–74. doi: 10.1097/JSM.0000000000000397. [DOI] [PubMed] [Google Scholar]
- 33.Rio E, Kidgell D, Moseley GL, et al. Elevated corticospinal excitability in patellar tendinopathy compared with other anterior knee pain or no pain. Scand J Med Sci Sports. 2016;26:1072–9. doi: 10.1111/sms.12538. [DOI] [PubMed] [Google Scholar]
- 34.Torres R, Ferreira J, Silva D, et al. Impact of patellar tendinopathy on knee proprioception. Clin J Sport Med. 2017;27:31–6. doi: 10.1097/JSM.0000000000000295. [DOI] [PubMed] [Google Scholar]
- 35.van der Worp H, van Ark M, Zwerver J, et al. Risk factors for patellar tendinopathy in basketball and volleyball players: a cross-sectional study. Scand J Med Sci Sports. 2012;22:783–90. doi: 10.1111/j.1600-0838.2011.01308.x. [DOI] [PubMed] [Google Scholar]
- 36.van Wilgen CP, Konopka KH, Keizer D, et al. Do patients with chronic patellar tendinopathy have an altered somatosensory profile? A Quantitative Sensory Testing (QST) study. Scand J Med Sci Sports. 2013;23:149–55. doi: 10.1111/j.1600-0838.2011.01375.x. [DOI] [PubMed] [Google Scholar]
- 37.Zhang ZJ, Ng GYF, Lee WC, et al. Increase in passive muscle tension of the quadriceps muscle heads in jumping athletes with patellar tendinopathy. Scand J Med Sci Sports. 2017;27:1099–104. doi: 10.1111/sms.12749. [DOI] [PubMed] [Google Scholar]
- 38.Bisseling RW, Hof AL, Bredeweg SW, et al. Relationship between landing strategy and patellar tendinopathy in volleyball. Br J Sports Med. 2007;41:e8. doi: 10.1136/bjsm.2006.032565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cassel M, Baur H, Hirschmüller A, et al. Prevalence of Achilles and patellar tendinopathy and their association to intratendinous changes in adolescent athletes. Scand J Med Sci Sports. 2015;25:e310–8. doi: 10.1111/sms.12318. [DOI] [PubMed] [Google Scholar]
- 40.Dauty M, Dupre M, Potiron-Josse M, et al. Identification of mechanical consequences of jumper’s knee by isokinetic concentric torque measurement in elite basketball players. Isokinet Exerc Sci. 2007;15:37–41. [Google Scholar]
- 41.Kujala UM, Osterman K, Kvist M, et al. Factors predisposing to patellar chondropathy and patellar apicitis in athletes. Int Orthop. 1986;10:195–200. doi: 10.1007/BF00266208. [DOI] [PubMed] [Google Scholar]
- 42.Lian Ø, Refsnes P-E, Engebretsen L, et al. Performance characteristics of volleyball players with patellar tendinopathy. Am J Sports Med. 2003;31:408–13. doi: 10.1177/03635465030310031401. [DOI] [PubMed] [Google Scholar]
- 43.Longo UG, Rittweger J, Garau G, et al. Patellar tendinopathy in master track and field athletes: influence of impact profile, weight, height, age and gender. Knee Surg Sports Traumatol Arthrosc. 2011;19:508–12. doi: 10.1007/s00167-010-1314-y. [DOI] [PubMed] [Google Scholar]
- 44.Scattone Silva R, Nakagawa TH, Ferreira ALG, et al. Lower limb strength and flexibility in athletes with and without patellar tendinopathy. Phys Ther Sport. 2016;20:19–25. doi: 10.1016/j.ptsp.2015.12.001. [DOI] [PubMed] [Google Scholar]
- 45.Bode G, Hammer T, Karvouniaris N, et al. Patellar tendinopathy in young elite soccer- clinical and sonographical analysis of a German elite soccer academy. BMC Musculoskelet Disord. 2017;18:344. doi: 10.1186/s12891-017-1690-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Malliaras P, Cook JL, Kent P. Reduced ankle dorsiflexion range may increase the risk of patellar tendon injury among volleyball players. J Sci Med Sport. 2006;9:304–9. doi: 10.1016/j.jsams.2006.03.015. [DOI] [PubMed] [Google Scholar]
- 47.Harman EA, Rosenstein MT, Frykman PN, et al. The effects of arms and countermovement on vertical jumping. Med Sci Sport Exerc. 1990;22:825–33. doi: 10.1249/00005768-199012000-00015. [DOI] [PubMed] [Google Scholar]
- 48.Lian Ø, Engebretsen L, Øvrebø RV, et al. Characteristics of the leg extensors in male volleyball players with jumper’s knee. Am J Sports Med. 1996;24:380–5. doi: 10.1177/036354659602400322. [DOI] [PubMed] [Google Scholar]
- 49.Rosen AB, Ko J, Simpson KJ, et al. Lower extremity kinematics during a drop jump in individuals with patellar tendinopathy. Orthop J Sport Med. 2015;3:2325967115576100. doi: 10.1177/2325967115576100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Siegmund JA, Huxel KC, Swanik CB. Compensatory mechanisms in basketball players with jumper’s knee. J Sport Rehabil. 2008;17:358–71. doi: 10.1123/jsr.17.4.358. [DOI] [PubMed] [Google Scholar]
- 51.Krauss I, Grau S, Rombach S, et al. Association of strength with patellar tendinopathy in female runners. Isokinet Exerc Sci. 2007;15:217–23. [Google Scholar]
- 52.van der Worp H, Zwerver J, Kuijer PPFM, et al. The impact of physically demanding work of basketball and volleyball players on the risk for patellar tendinopathy and on work limitations. J Back Musculoskelet Rehabil. 2011;24:49–55. doi: 10.3233/BMR-2011-0274. [DOI] [PubMed] [Google Scholar]
- 53.Gaida JE, Ashe MC, Bass SL, et al. Is adiposity an under-recognized risk factor for tendinopathy? A systematic review. Arthritis Rheum. 2009;61:840–9. doi: 10.1002/art.24518. [DOI] [PubMed] [Google Scholar]
- 54.Peña J, Moreno-Doutres D, Coma J, et al. Anthropometric and fitness profile of high-level basketball, handball and volleyball players. Rev Andaluza Med del Deport. 2015 Published Online First. [Google Scholar]
- 55.Devita P, Skelly Wa. Effect of landing stiffness on joint kinetics and energetics in the lower extremity. Med Sci Sports Exerc. 1992;24:108–15. [PubMed] [Google Scholar]
- 56.Hoch MC, Farwell KE, Gaven SL, et al. Weight-bearing dorsiflexion range of motion and landing biomechanics in individuals with chronic ankle instability. J Athl Train. 2015;50:833–9. doi: 10.4085/1062-6050-50.5.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Dill KE, Begalle RL, Frank BS, et al. Altered knee and ankle kinematics during squatting in those with limited weight-bearing-lunge ankle-dorsiflexion range of motion. J Athl Train. 2014;49:723–32. doi: 10.4085/1062-6050-49.3.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Khan KM. Time to abandon the ‘tendinitis’ myth. BMJ. 2002;324:626–7. doi: 10.1136/bmj.324.7338.626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Tomioka M, Owings TM, Grabiner MD. Lower extremity strength and coordination are independent contributors to maximum vertical jump height. J Appl Biomech. 2001;17:181–7. [Google Scholar]
- 60.Mcnitt-Gray JL. Kinetics of the lower-extremities during drop landings from 3 heights. J Biomech. 1993;26:1037–46. doi: 10.1016/s0021-9290(05)80003-x. [DOI] [PubMed] [Google Scholar]
- 61.Vanezis A, Lees A. A biomechanical analysis of good and poor performers of the vertical jump. Ergonomics. 2005;48:1594–603. doi: 10.1080/00140130500101262. [DOI] [PubMed] [Google Scholar]
- 62.Zhang SN, Bates BT, Dufek JS. Contributions of lower extremity joints to energy dissipation during landings. Med Sci Sports Exerc. 2000;32:812–9. doi: 10.1097/00005768-200004000-00014. [DOI] [PubMed] [Google Scholar]
- 63.Magnusson SP, Langberg H, Kjaer M. The pathogenesis of tendinopathy: balancing the response to loading. Nat Rev Rheumatol. 2010;6:262–8. doi: 10.1038/nrrheum.2010.43. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.