Abstract
Low neighborhood socioeconomic status has been linked to adverse health outcomes. However, it is unclear whether changing the neighborhood may influence health. We examined 10-year change in neighborhood socioeconomic deprivation in relation to mortality rate among 288,555 participants aged 51–70 years who enrolled in the National Institutes of Health-AARP Diet and Health Study in 1995–1996 (baseline) and did not move during the study. Changes in neighborhood socioeconomic deprivation between 1990 and 2000 were measured by US Census data at the census tract level. All-cause, cardiovascular disease, and cancer deaths were ascertained through annual linkage to the Social Security Administration Death Master File between 2000 and 2011. Overall, our results suggested that improvement in neighborhood socioeconomic status was associated with a lower mortality rate, while deterioration was associated with a higher mortality rate. More specially, a 30-percentile-point reduction in neighborhood deprivation among more deprived neighborhoods was associated with 11% and 19% reductions in the total mortality rate among men and women, respectively. On the other hand, a 30-point increase in neighborhood deprivation in less deprived neighborhoods was associated with an 11% increase in the mortality rate among men. Our findings support a longitudinal association between changing neighborhood conditions and mortality.
Keywords: cancer mortality, cardiovascular disease mortality, mortality, neighborhood characteristics, older adults, socioeconomic deprivation
In recent decades, there has been a growing interest in understanding the impact of neighborhood socioeconomic deprivation on health and health disparities (1). In the United States, investigators in several large prospective cohort studies have consistently reported that more severe neighborhood socioeconomic deprivation at baseline was associated with higher all-cause and cause-specific mortality rates during follow-up (2–5). Although such findings suggest an important role of neighborhood socioeconomic status (SES) in shaping health and health disparities, a crucial remaining question is whether changing neighborhood conditions would lead to changes in health outcomes.
Neighborhood residents may experience changes in neighborhood conditions by moving or by remaining in a neighborhood that changes during their residential tenure. The consequences of moving have been studied by randomizing people to receive relocation vouchers, as in the landmark Moving to Opportunity Study, which found that moving to less disadvantaged neighborhoods may have a positive impact on obesity and diabetes risk, as well as on mental health in girls (6, 7). Moreover, several observational studies also examined the relationship between moving and health outcomes but had mixed findings: In several US studies, authors reported that moving to a better neighborhood was associated with a lower mortality rate (8) and decreased blood pressure in blacks (9), while moving to more deprived neighborhoods was associated with higher weight gain (10, 11). However, studies carried out in Australia and England found no association between moving to a different neighborhood on self-reported health behaviors, overall health status, or multiple diseases (12, 13).
Alternatively, changes in neighborhood conditions can occur by changing the environment surrounding those who continue to live in the same neighborhood. This type of scenario is particularly relevant for the aging population, as residential mobility declines with age (14). However, because conditions in most neighborhoods tend to be stable over a period of time and it may take a long lag time for neighborhood effects on health to emerge (15), conducting such studies would require large populations, geographically diverse neighborhoods, and a sufficiently long follow-up period. Because of such challenges, there has been only limited research on how changing specific aspects of neighborhood environment might affect specific health outcomes. For example, an increase in neighborhood poverty was found to be associated with higher risk of preterm birth (16); improvement in neighborhood safety was linked to a decrease in body mass index (17); and loss of neighborhood supermarkets was related to worsening glycemic control (18). Overall the evidence seems to suggest that improvement in neighborhood conditions might lead to health benefits, while neighborhood deterioration might lead to damaging outcomes. However, although some evidence has suggested that improvements in specific aspects of neighborhood environment are often linked to neighborhood socioeconomic advantages (19, 20), there has been no study that has examined the association between more general improvement in or deterioration of neighborhood socioeconomic conditions and overall health.
In a large cohort of middle-aged to older men and women from diverse areas of the United States who lived in the same neighborhood during the study period, we examined changes in neighborhood socioeconomic deprivation over 11 years of follow-up in relation to rates of total, cardiovascular disease, and cancer mortality. We tested the hypothesis that reductions in relative neighborhood socioeconomic deprivation would be associated with lower all-cause and cause-specific mortality rates, particularly among participants residing in a more deprived neighborhood in 1990. We also examined whether an increase in relative deprivation in more advantaged neighborhoods was associated with an elevated mortality rate.
METHODS
Study population
The National Institutes of Health-AARP Diet and Health Study was established in 1995–1996 by recruiting members of AARP (formerly the American Association of Retired Persons) aged 50–71 years residing in one of 6 US states (California, Florida, Louisiana, New Jersey, North Carolina, and Pennsylvania) and 2 US metropolitan areas (Atlanta, Georgia and Detroit, Michigan). Details of the study have been previously reported (21). In total, 566,399 participants satisfactorily completed the baseline questionnaire, in which they reported their residential address. Addresses of participants were regularly updated using the National Change of Address database. In 2005, in order to prepare for mailing a follow-up questionnaire to the entire cohort, a mailing list was constructed using the most up-to-date addresses for all study participants who were not known to have died. We further extracted address information from the most recent updates for those who died before 2005, which was combined with the mailing list to generate a complete list of updated addresses by 2005. The study was approved by the National Cancer Institute Special Studies Institutional Review Board.
Analytical sample
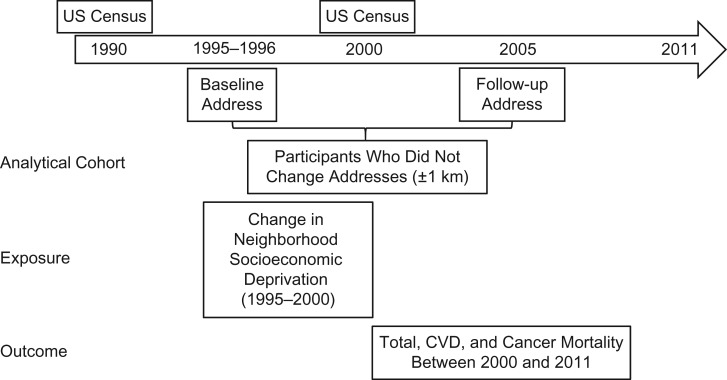
The focus of our study was on participants who reported living in the same neighborhood between baseline and 2000. We compared updated addresses with the baseline addresses and defined nonmovers as those whose updated address was within 1 km of their baseline address. The distance of 1 km was chosen to account for small variations in geocoding over time, as well as local moves within the same neighborhood. A total of 303,174 participants met this criterion and were eligible for this study. Of those, we further excluded participants who died before 2000, which served as the beginning of the mortality follow-up period (n = 14,619), and participants for whom we had missing census information in either 1990 or 2000 (n = 463). The final analytical cohort included 174,994 men and 113,561 women. An outline of the study design is presented in Figure 1.
Figure 1.
Design of a study of the relationship between 10-year change in neighborhood socioeconomic deprivation and total, cardiovascular disease (CVD), and cancer mortality among 288,555 participants aged 51–70 years, National Institutes of Health-AARP Diet and Health Study, 1995–2011.
Neighborhood socioeconomic deprivation
Baseline addresses from 1995 to 1996 were geocoded to latitude/longitude and linked to 1990 and 2000 US Census data at the census tract level. In total, there were 17,850 census tracts in our study. We applied an adapted version of the method developed by Messer et al. (22) and Major et al. (2) to generate an empirical neighborhood socioeconomic deprivation index for both census years, where higher deprivation meant lower SES. In brief, the index was calculated via principal components analysis using 6 variables, and their loadings are presented in Web Table 1 (available at https://academic.oup.com/aje). We also performed sensitivity analyses using 2 additional indicators of neighborhood deprivation: 1) a deprivation index derived from all 14 census variables and 2) percentage of households with an income below the federal poverty level.
We created 2 main variables to characterize changes in neighborhood conditions. First, we created tertiles in both 1990 and 2000 based on the deprivation index and jointly classified the census tracts into 9 categories. Second, to examine the dose-response relationship between changes in neighborhood deprivation and mortality rate, we further calculated the difference in the percentiles for the deprivation index between 1990 and 2000. Changes in individual census variables between the 2 censuses according to different categories of percentile change in the neighborhood deprivation index are presented in Web Table 2. More details on measuring neighborhood socioeconomic deprivation can be found in the Web Appendix.
Mortality ascertainment
The vital status of study participants was ascertained by means of annual linkage to the Social Security Administration’s Death Master File. Cause-of-death information can be obtained through follow-up searches of the National Death Index Plus. In a previous study, Hermansen et al. (23) found that our ascertainment method yielded results that were 95% accurate. The endpoints of our analysis were total mortality, cardiovascular disease mortality (International Classification of Diseases, Tenth Revision, codes I00–I78), and cancer mortality (International Classification of Diseases, Tenth Revision, codes C00–C79). The most recent update on mortality included deaths that occurred through December 31, 2011.
Covariate assessment
At baseline, the National Institutes of Health-AARP Diet and Health Study collected information on a broad range of covariates, including demographic characteristics; lifestyle factors, such as physical activity, smoking, and body mass index; medical history, such as cardiovascular disease, cancer, and diabetes, as well as self-rated health status; and dietary intake, including intakes of total calories, total fat, fruits and vegetables, meat, whole grain, coffee, and alcohol (21).
Statistical analysis
Multivariable-adjusted hazard ratios and 2-sided 95% confidence intervals were calculated using Cox proportional hazards models (SAS 9.3; SAS Institute, Inc., Cary, North Carolina). Person-years were calculated from January 1, 2000, to the date of death or December 31, 2011, whichever occurred first. Robust variance estimation was used for standard error estimation to account for clustering across census tracts (24). Because we detected a statistically significant interaction between sex and changes in neighborhood socioeconomic deprivation (P = 0.01), we conducted our regression analyses for men and women separately.
We performed 2 main analyses: First, we studied rates of total and cause-specific mortality in relation to categories of change in neighborhood deprivation based on tertiles. Second, we further examined the dose-response relationship by using the continuous variable of change in percentile ranking by estimating the association between morality rate and every 5-percentile-change in neighborhood deprivation. Additionally, we examined the relationship between a reduction in neighborhood deprivation (a 2.6%–10.0%, 10.1%–20.0%, 20.1%–30.0%, or >30.0% reduction in deprivation vs. a ≤2.5% reduction or an increase in deprivation (reference group)) and the mortality rate in participants whose neighborhoods were more deprived in 1990 (deprivation index > median), as well as the relationship between an increase in neighborhood deprivation (a 2.6%–10.0%, 10.1%–20.0%, 20.1%–30.0%, or >30.0% increase in deprivation vs. a ≤2.5% increase or a reduction in deprivation (reference group)) and the mortality rate in participants whose neighborhoods were less deprived in 1990 (deprivation index ≤ median).
In all of our models, we adjusted for potentially confounding factors, including demographic characteristics (age and race/ethnicity) and education as an individual-level SES indicator. State of residence was included as a random effect. We further considered the role of neighborhood socioeconomic deprivation in 1990: On the one hand, it may confound the relationship between changes in neighborhood deprivation and mortality rate; on the other hand, as pointed out by Glymour et al. (25), controlling for a baseline variable while studying changes in such a variable may induce bias. Therefore, we present results from models both with and without adjustment for neighborhood deprivation in 1990. Finally, because a large proportion (44%) of baseline cohort participants were excluded, primarily because they moved out of the neighborhood or died before 2000, we compared study characteristics between those who were included in this analysis and those who were excluded (Web Table 3). Although study characteristics appeared to be largely comparable between the two groups, some small differences were noted. Therefore, we conducted sensitivity analysis using inverse probability weighting to account for the potential impact of exclusions (26). More details about model selection and inverse probability weighting can be found in the Web Appendix.
RESULTS
Baseline characteristics are presented in Table 1 according to the 9 categories of neighborhood socioeconomic deprivation in 1990 and 2000. For each of the neighborhood deprivation tertiles in 1990, 75.2% of the respondents lived in census tracts in the same tertile in 2000, 23.8% lived in tracts that changed to an adjacent tertile, and just 0.8% lived in neighborhoods that improved or worsened by 2 tertiles. Overall, when compared with those in less deprived neighborhoods, study participants in the neighborhoods with higher socioeconomic deprivation in 1990 were less likely to be white and more likely to be female. They also exhibited a less healthy lifestyle, with more current smoking, a lower level of physical activity, prolonged television watching, a higher body mass index, and a lower Healthy Eating Index-2005 (27) score, as well as a higher prevalence of chronic conditions. Within each tertile of neighborhood socioeconomic deprivation in 1990, the distribution of these demographic, lifestyle, and medical factors also differed by neighborhood deprivation in 2000, with higher deprivation in 2000 being associated with more women, nonwhite race/ethnicity, an unhealthy lifestyle, and higher prevalence of chronic conditions.
Table 1.
Baseline (1995–1996) Characteristics (%) of 288,555 Participants in the National Institutes of Health-AARP Diet and Health Study According to Tertiles of Neighborhood Socioeconomic Deprivation Index in 1990 and 2000
| Baseline Characteristic | Tertile of Neighborhood Socioeconomic Deprivation Index in 1990 and 2000 | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| T1a (Low Deprivation) | T2 | T3 (High Deprivation) | |||||||
| T1b (n = 76,448; 26.5%) | T2 (n = 17,948; 6.2%) | T3 (n = 1,281; 0.4%) | T1 (n = 17,880; 6.2%) | T2 (n = 62,034; 21.5%) | T3 (n = 16,143; 5.6%) | T1 (n = 1,197; 0.4%) | T2 (n = 16,737; 5.8%) | T3 (n = 78,424; 27.2%) | |
| Age, yearsc | 61.9 (5.3) | 62.2 (5.3) | 62.2 (5.3) | 62.1 (5.4) | 62.4 (5.3) | 62.5 (5.3) | 62.3 (5.3) | 62.5 (5.3) | 62.4 (5.3) |
| Female sex | 34.1 | 38.1 | 41.0 | 36.2 | 39.4 | 41.9 | 35.8 | 38.9 | 45.1 |
| Non-Hispanic white race/ethnicity | 94.4 | 92.1 | 91.9 | 94.7 | 93.5 | 89.4 | 93.3 | 94.0 | 81.5 |
| College graduation or more | 54.4 | 43.6 | 43.7 | 39.5 | 34.1 | 32.3 | 38.4 | 28.3 | 25.8 |
| Married | 78.4 | 73.2 | 66.5 | 75.1 | 71.2 | 67.1 | 73.7 | 72.4 | 63.5 |
| Current smoker | 8.4 | 10.2 | 11.1 | 10.6 | 11.7 | 10.3 | 10.9 | 11.8 | 14.0 |
| Physical activity ≥5 times/week | 20.8 | 20.4 | 22.0 | 20.2 | 19.6 | 19.4 | 20.1 | 20.1 | 18.4 |
| Television viewing ≤2 hours/day | 25.5 | 21.5 | 23.6 | 21.0 | 19.7 | 18.7 | 18.1 | 18.1 | 17.0 |
| Nighttime sleep 7–8 hours/day | 39.9 | 37.8 | 34.4 | 37.6 | 37.1 | 35.1 | 37.2 | 37.0 | 32.4 |
| Body mass indexc,d | 26.5 (4.6) | 26.8 (4.8) | 26.6 (4.6) | 27.0 (5.0) | 27.1 (5.0) | 27.3 (5.4) | 26.9 (4.6) | 27.3 (5.0) | 27.6 (5.4) |
| Alcohol consumption, g/dayc | 14.0 (33.6) | 13.4 (39.3) | 12.4 (32.6) | 14.5 (37.7) | 13.4 (39.1) | 12.1 (35.8) | 13.3 (42.8) | 12.8 (38.9) | 11.9 (41.5) |
| Total HEI-2005 scorec | 67.6 (11.0) | 67.2 (11.2) | 67.2 (11.1) | 66.5 (11.4) | 66.3 (11.5) | 66.6 (11.5) | 67.0 (11.1) | 65.8 (11.6) | 65.7 (11.8) |
| Excellent self-reported health | 21.4 | 17.9 | 19.8 | 17.4 | 15.6 | 14.7 | 16.9 | 14.0 | 12.5 |
| Chronic conditions | |||||||||
| Heart disease | 12.4 | 13.3 | 13.0 | 13.3 | 14.0 | 13.5 | 12.6 | 15.1 | 14.4 |
| Stroke | 1.5 | 1.6 | 2.0 | 1.8 | 2.1 | 2.1 | 2.4 | 2.4 | 2.6 |
| Cancer | 25.5 | 24.3 | 23.3 | 25.4 | 24.9 | 24.4 | 24.8 | 24.1 | 23.4 |
| Diabetes mellitus | 6.7 | 7.9 | 7.9 | 8.0 | 8.8 | 9.9 | 7.6 | 10.0 | 11.2 |
Abbreviations: HEI-2005, Healthy Eating Index-2005; T, tertile.
a Tertile in 1990.
b Tertile in 2000.
c Values are expressed as mean (standard deviation).
d Calculated as weight (kg)/height (m)2.
For both men and women, age-standardized total mortality rates were the lowest among study participants who lived in the neighborhoods with consistently low socioeconomic deprivation in both 1990 and 2000 (14.68 deaths/1,000 and 8.99 deaths/1,000 for men and women, respectively; Table 2). Within each tertile of socioeconomic deprivation in 1990, there appeared to be a trend of an elevated total mortality rate with higher deprivation in 2000. For example, for men who lived in neighborhoods in tertile 1 (the lowest tertile of deprivation) in 1990, the age-standardized total mortality rate was 14.68 deaths/1,000 if the neighborhood remained in tertile 1 in 2000, while the mortality rate increased to 16.59 deaths/1,000 and 18.53 deaths/1,000 if the 2000 neighborhood deprivation index rose to tertile 2 and tertile 3, respectively. Similar trends were observed for other tertiles of 1990 neighborhood deprivation index and for women. Additionally, when we examined cause-specific mortality rates, we found a similar pattern of associations for cardiovascular disease mortality but less consistent and weaker associations for cancer mortality (Table 2).
Table 2.
Total, Cardiovascular Disease, and Cancer Mortality (1995–2011) Among 288,555 Participants in the National Institutes of Health-AARP Diet and Health Study According to Tertiles of Neighborhood Socioeconomic Deprivation Index in 1990 and 2000
| Tertile of Neighborhood Socioeconomic Deprivation Index in 1990 and 2000 | Cause of Death | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total (All Deaths) | Cardiovascular Disease | Cancer | ||||||||||
| No. of Deaths | Age-Standardized Mortality Ratea | Adjusted HRb | 95% CI | No. of Deaths | Age-Standardized Mortality Rate | Adjusted HR | 95% CI | No. of Deaths | Age-Standardized Mortality Rate | Adjusted HR | 95% CI | |
| Men | ||||||||||||
| T1c (low deprivation) | ||||||||||||
| T1d | 10,477 | 14.68 | 1.00 | Referent | 3,050 | 4.28 | 1.00 | Referent | 3,879 | 5.42 | 1.00 | Referent |
| T2 | 2,632 | 16.59 | 1.10 | 1.06, 1.15 | 813 | 5.12 | 1.17 | 1.08, 1.26 | 955 | 6.02 | 1.09 | 1.02, 1.17 |
| T3 | 199 | 18.53 | 1.24 | 1.08, 1.43 | 82 | 7.62 | 1.76 | 1.41, 2.19 | 61 | 5.68 | 1.03 | 0.80, 1.33 |
| T2 | ||||||||||||
| T1 | 2,793 | 17.42 | 1.12 | 1.07, 1.17 | 888 | 5.54 | 1.21 | 1.12, 1.30 | 987 | 6.15 | 1.08 | 1.01, 1.16 |
| T2 | 9,715 | 18.1 | 1.15 | 1.12, 1.18 | 3,034 | 5.65 | 1.21 | 1.15, 1.28 | 3,434 | 6.41 | 1.11 | 1.06, 1.16 |
| T3 | 2,630 | 19.82 | 1.27 | 1.22, 1.33 | 872 | 6.57 | 1.44 | 1.33, 1.55 | 863 | 6.52 | 1.14 | 1.06, 1.23 |
| T3 (high deprivation) | ||||||||||||
| T1 | 199 | 18.18 | 1.18 | 1.03, 1.36 | 60 | 5.47 | 1.22 | 0.95, 1.58 | 68 | 6.22 | 1.10 | 0.87, 1.40 |
| T2 | 2,897 | 19.78 | 1.22 | 1.17, 1.27 | 933 | 6.37 | 1.33 | 1.23, 1.43 | 1,018 | 6.96 | 1.19 | 1.11, 1.27 |
| T3 | 12,658 | 21.12 | 1.31 | 1.27, 1.34 | 4,202 | 7.01 | 1.47 | 1.40, 1.54 | 4,042 | 6.74 | 1.15 | 1.10, 1.20 |
| Women | ||||||||||||
| T1 (low deprivation) | ||||||||||||
| T1 | 3,374 | 8.99 | 1.00 | Referent | 732 | 1.96 | 1.00 | Referent | 1,462 | 3.87 | 1.00 | Referent |
| T2 | 981 | 9.8 | 1.07 | 1.00, 1.15 | 281 | 2.81 | 1.41 | 1.23, 1.61 | 355 | 3.53 | 0.90 | 0.81, 1.02 |
| T3 | 71 | 9.15 | 1.03 | 0.82, 1.31 | 13 | 1.68 | 0.87 | 0.51, 1.51 | 26 | 3.35 | 0.87 | 0.59, 1.28 |
| T2 | ||||||||||||
| T1 | 959 | 10.08 | 1.09 | 1.01, 1.17 | 235 | 2.47 | 1.21 | 1.05, 1.41 | 396 | 4.17 | 1.05 | 0.94, 1.18 |
| T2 | 3,989 | 11.04 | 1.19 | 1.13, 1.24 | 1,066 | 2.95 | 1.44 | 1.31, 1.59 | 1,459 | 4.05 | 1.02 | 0.95, 1.10 |
| T3 | 1,194 | 11.88 | 1.28 | 1.20, 1.37 | 321 | 3.19 | 1.56 | 1.36, 1.78 | 449 | 4.48 | 1.13 | 1.02, 1.26 |
| T3 (high deprivation) | ||||||||||||
| T1 | 67 | 11.06 | 1.16 | 0.91, 1.48 | 17 | 2.76 | 1.34 | 0.83, 2.17 | 20 | 3.26 | 0.82 | 0.53, 1.27 |
| T2 | 1,169 | 12.14 | 1.28 | 1.19, 1.37 | 343 | 3.56 | 1.70 | 1.49, 1.94 | 379 | 3.95 | 0.99 | 0.88, 1.11 |
| T3 | 7,017 | 13.56 | 1.42 | 1.36, 1.48 | 1,991 | 3.84 | 1.78 | 1.63, 1.95 | 2,418 | 4.68 | 1.18 | 1.10, 1.27 |
Abbreviations: CI, confidence interval; HR, hazard ratio; T, tertile.
a Number of deaths per 1,000 participants per year; calculated by direct standardization using 5-year age categories.
b Adjusted for age (50.0–54.9, 55.0–59.9, 60.0–64.9, or ≥65 years), race/ethnicity (non-Hispanic white, non-Hispanic black, or other), and education (<12 years, high school graduation, some college, or college graduation/postgraduate study). State of residence (California, Florida, Georgia, Louisiana, Michigan, North Carolina, New Jersey, or Pennsylvania) was included as a random effect.
c Tertile in 1990.
d Tertile in 2000.
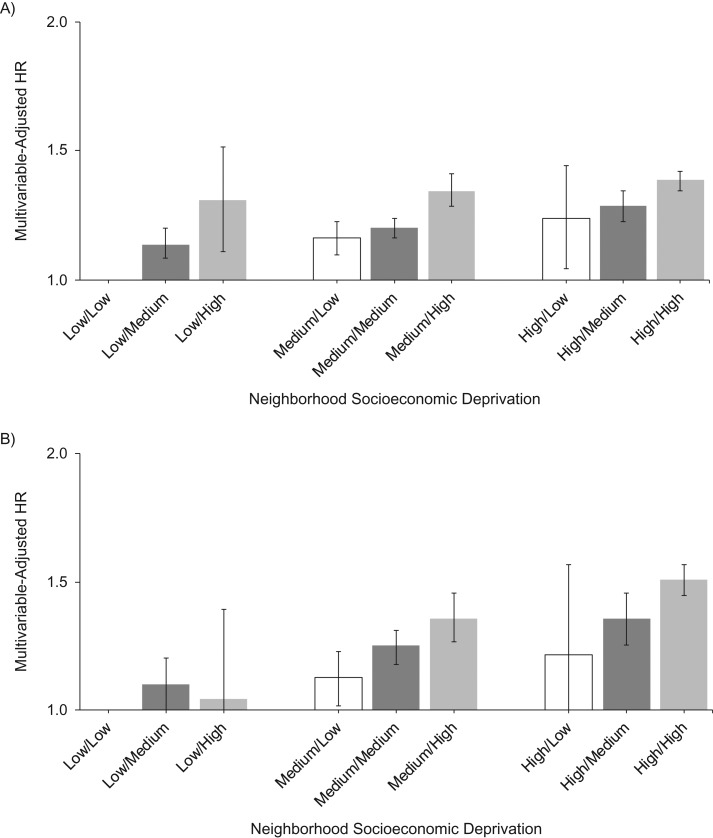
Next, we examined the relationship between changes in neighborhood socioeconomic deprivation and mortality rate after controlling for multiple confounders. Overall, the findings from the multivariable analysis seemed to suggest that in comparison with no change in neighborhood socioeconomic deprivation tertile between 1990 and 2000, a reduction in neighborhood socioeconomic deprivation was associated with a trend of a lower total mortality rate and an increase in neighborhood deprivation was associated with a higher total mortality rate (Table 2, Figure 2, and Web Figure 1). We observed largely similar results using the deprivation index derived from 14 census variables or percentage of households with an income below the poverty level (Web Table 4), or after additionally adjusting for neighborhood deprivation in 1990 (Web Table 5). Use of inverse weighting to control for the probability of being excluded from the analytical sample because of moving or death also had little impact on the results (data not shown).
Figure 2.
Hazard ratios (HRs) for the association between neighborhood socioeconomic deprivation in 1990 and 2000 and total mortality in men (A) and women (B), National Institutes of Health-AARP Diet and Health Study, 1995–2011. The x-axis labels present the neighborhood deprivation groups for 1990/2000; for example, “low/high” indicates low neighborhood deprivation in 1990 and high deprivation in 2000. Results were adjusted for age (50.0–54.9, 55.0–59.9, 60.0–64.9, or ≥65.0 years), race/ethnicity (non-Hispanic white, non-Hispanic black, or other), and education (<12 years, high school graduation, some college, or college graduation/postgraduate study). State of residence (California, Florida, Georgia, Louisiana, Michigan, North Carolina, New Jersey, or Pennsylvania) was included as a random effect. Vertical lines represent 95% confidence intervals. The “low/low” group served as the reference group.
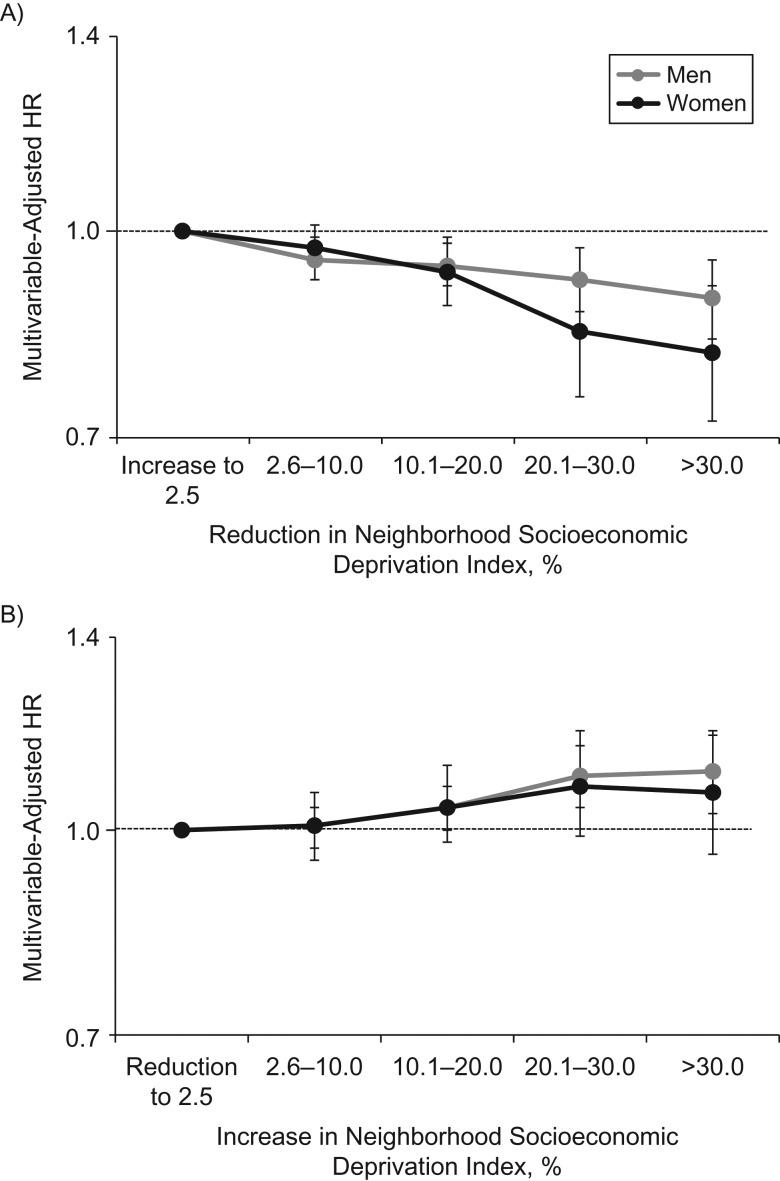
To further investigate the dose-response relationship between changes in neighborhood socioeconomic deprivation and mortality rate, we examined percentile reduction in neighborhood deprivation index between 1990 and 2000 in relation to mortality rate among participants who lived in a more deprived neighborhood in 1990 (Figure 3A, Web Table 6). Overall we found a significant relationship between reduction in neighborhood deprivation and lower total mortality rate. Every 5-percentile-point reduction was associated with 1.1% and 2.0% lower mortality rates in men and women, respectively. Moreover, when compared with neighborhoods with little or no reduction in deprivation or an increase in deprivation, a 30-percentile-point reduction in neighborhood deprivation was associated with 11% and 19% lower risks of mortality in men and women, respectively (hazard ratio (HR) = 0.89 (95% confidence interval (CI): 0.83, 0.95) for men and HR = 0.81 (95% CI: 0.72, 0.91) for women). On the other hand, among people who lived in less deprived neighborhoods in 1990, we found that a relative increase in neighborhood deprivation was associated with a higher mortality rate, but the relationship was significant only in men, among whom a 30-percentile-point increase was associated with 11% greater risk of total mortality (Figure 3B, Web Table 7).
Figure 3.
Sex-specific hazard ratios (HRs) for the association between change in neighborhood socioeconomic deprivation between 1990 and 2000 and total mortality, National Institutes of Health-AARP Diet and Health Study, 1995–2011. Part A shows the association between a reduction in neighborhood deprivation and mortality among participants from a more deprived neighborhood in 1990 (neighborhood socioeconomic deprivation index > median), and the reference group included neighborhoods that had increases in deprivation, no change in deprivation, or a slight reduction in deprivation (up to 2.5%). Part B shows the association between an increase in neighborhood deprivation and mortality among participants from a less deprived neighborhood in 1990 (neighborhood socioeconomic deprivation index ≤ median), and the reference group included neighborhoods that had reductions in deprivation, no change in deprivation, or a slight increase in deprivation (up to 2.5%). Results were adjusted for age (50.0–54.9, 55.0–59.9, 60.0–64.9, or ≥65.0 years), race/ethnicity (non-Hispanic white, non-Hispanic black, or other), and education (<12 years, high school graduation, some college, or college graduation/postgraduate study). State of residence (California, Florida, Georgia, Louisiana, Michigan, North Carolina, New Jersey, or Pennsylvania) was included as a random effect. Vertical lines represent 95% confidence intervals.
Finally, we examined the impact of baseline health status on the association between a reduction in neighborhood socioeconomic deprivation and the mortality rate among participants who lived in more deprived neighborhoods in 1990 (Web Table 8). We found that less healthy women appeared to benefit most from a 30-percentile-point reduction in neighborhood deprivation, with a 21% reduction in total mortality (HR = 0.79, 95% CI: 0.68, 0.90).
DISCUSSION
In this large cohort of middle-aged to older US men and women who lived in the same neighborhoods from the mid-1990s to the mid-2000s, we found that changes in neighborhood socioeconomic deprivation were associated with mortality rates in ways that were consistent with our original hypotheses. Specifically, relative reductions in neighborhood deprivation were associated with a lower total mortality rate among residents of more deprived neighborhoods, and the association was stronger in women, particularly women who were less healthy at baseline. Moreover, a relative increase in deprivation was associated with a higher mortality rate among men living in less deprived neighborhoods.
Research focusing on the associations between health outcomes and changes in neighborhood conditions among the residents could contribute to the current literature in 2 significant ways: First, it would help strengthen or refute the argument for causality for the relationship between neighborhood environment and health; and second, it could provide evidence to better evaluate the potential of interventions that focus on improving conditions which influence health in disadvantaged neighborhoods. Such studies are particularly relevant for the older population, since residential mobility declines with age. In a previous study, Fischer (14) reported that the percentage of the population that moved in 1 year dropped from over 30% for young adults to approximately 5% for people who were 60–80 years of age. Therefore, changing the neighborhood environment may be a more feasible intervention strategy for the older population. There has been sparse evidence suggesting that changing neighborhood conditions may be associated with health outcomes among residents who stay in the same neighborhood. In a recent study, Margerison-Zilko et al. (16) evaluated the trajectory of neighborhood poverty in California and reported that an increase in poverty early in the study period (2003–2009) was associated with a 37% increase in the odds of preterm birth, while a decrease in neighborhood poverty was not associated with changes in preterm birth. In another study, Zhang et al. (18) examined the gain or loss in neighborhood supermarkets in relation to hemoglobin A1c level among patients from the Kaiser Permanente Northern California Diabetes Registry. They found that supermarket loss was consistently associated with worsening hemoglobin A1c status in the study population, while supermarket gain was associated with improvement in hemoglobin A1c levels, but only among people with near-normal levels at baseline (18). Moreover, 2 analyses in the Multi-Ethnic Study of Atherosclerosis found that improvement in neighborhood safety and increase in the number of walking destinations and population density were associated with lower body mass index and waist circumference (17, 28). Overall, findings from these studies and ours support a potentially important impact on public health of changing the neighborhood environment: On the one hand, the evidence consistently identifies deterioration in the neighborhood environment as a risk factor for adverse health outcomes, suggesting that more attention is needed to monitor health problems and reduce disease burden in communities with a worsening condition. On the other hand, there is a suggestion that improvement in neighborhood conditions in more deprived neighborhoods may lead to health benefits, and more studies are needed to explore what types of neighborhood interventions might be most effective.
A unique strength of our study was its large number of participants and neighborhoods, which enabled us to examine the dose-response relationship between changes in neighborhood deprivation and mortality rate to determine the degree of neighborhood change required for health benefits. We found a modest association between changes in neighborhood SES and mortality rate, which suggested that a relatively large change in neighborhood conditions is needed to produce a substantial change in health outcomes. Indeed, using categories of neighborhood change in percentile ranking, we found a substantial (10% or higher) reduction in total mortality risk only when there was a 20-point or greater reduction in neighborhood deprivation.
The large sample size also enabled us to evaluate the relationships by sex and baseline health status, and to our knowledge our study was one of the first to identify subpopulations that are most likely to be affected by changing neighborhood conditions. We found that when compared with men, women from more deprived neighborhoods showed a larger mortality reduction associated with improvements in neighborhood conditions. Interestingly, there has been a growing body of evidence showing that women may benefit more from improvements in their neighborhoods than men. For example, Althoff et al. (29) recently reported that a more walkable built environment was linked to a larger increase in physical activity among women than among men, and Powell-Wiley et al. (17) also reported that an increase in neighborhood safety had a stronger association with decreases in body mass index in women. Moreover, in an analysis of the Southern Community Cohort Study, Warren Andersen et al. (30) also reported that neighborhood disadvantages had a stronger association with mortality in women than in men, although such a sex-specific association was not found in an earlier meta-analysis on neighborhood deprivation and mortality (31). Interestingly, we also found that women who were less healthy seemed to exhibit the biggest reduction in mortality rate associated with improved neighborhood conditions, which supports a potentially large public health benefit of intervention programs that aim at improving neighborhood environment in disadvantaged communities. Taken together, such findings could contribute to the inclusion of individual-level variables in discussions concerning the costs and benefits of investment in neighborhood characteristics.
We also examined the relationship between changes in neighborhood deprivation and cause-specific mortality rate. Interestingly, the associations appeared to be stronger for cardiovascular mortality than for cancer mortality, which may be due to the relatively long latency period needed for most cancers to develop, in comparison with cardiovascular diseases. More studies are needed to examine the potential impact of neighborhood environment on specific health outcomes.
There were also some limitations in our study. First, our population was predominantly white, and most of the participants resided in relatively high-SES neighborhoods. For example, the median percentage of households below the poverty line in our study was 6.0% in 1990 and 6.6% in 2000, as compared with a national average of 13.5% in 1990 and 11.3% in 2000. Therefore, these results may be less generalizable to other populations. We encourage researchers in future studies to utilize cohorts with a more diverse racial/ethnic background to examine the relationship between neighborhood and changes in neighborhood and health in minority populations. Second, we did not have information about specific aspects of the neighborhood, such as the built environment, local businesses, social capital, and access to health care, and we were not able to pinpoint which aspects of the neighborhood were most responsible for the association between mortality and changes in socioeconomic deprivation in the neighborhood. Third, we only had information on residential address at 2 time points (baseline and 2004), while the period of exposure to changing neighborhood deprivation was baseline–2000. If a participant moved out of the neighborhood before 2000 but later moved back into the neighborhood, this may have led to exposure misclassification. Finally, we had only 2 measurements of neighborhood socioeconomic deprivation and they were taken 10 years apart, which limited our ability to assess the impact of short-term fluctuations in neighborhood conditions and may have led to exposure misclassification. For example, we would not be able to differentiate neighborhoods that experienced stable and continuous decline from neighborhoods that experienced multiple rounds of ups and downs if the 2 neighborhoods were at the same level of deprivation in 1990 and 2000.
In conclusion, our findings not only corroborate a relationship between neighborhood environment and health but also suggest that even in an older population, changing neighborhood conditions may have an important impact on health outcomes. We believe our study findings provide further evidence in support of future research to develop and evaluate neighborhood-based interventions that aim to improve health and reduce health disparities.
Supplementary Material
ACKNOWLEDGMENTS
Author affiliations: Department of Health and Human Physiology, College of Liberal Arts and Sciences, University of Iowa, Iowa City, Iowa (Qian Xiao); Department of Epidemiology, College of Public Health, University of Iowa, Iowa City, Iowa (Qian Xiao); Applied Research Program, Division of Cancer Control and Population Sciences, National Cancer Institute, Bethesda, Maryland (David Berrigan); Cardiovascular Branch, Division of Intramural Research, National Heart, Lung, and Blood Institute, Bethesda, Maryland (Tiffany M. Powell-Wiley); Intramural Research Program of the National Institute of Minority Health and Health Disparities, Bethesda, Maryland (Tiffany M. Powell-Wiley); and Metabolic Epidemiological Branch, Division of Cancer Epidemiology and Genetics, National Cancer Institute, Bethesda, Maryland (Charles E. Matthews).
This work was supported by the Division of Intramural Research Programs of the National Cancer Institute, the National Heart, Lung, and Blood Institute, and the National Institute of Minority Health and Health Disparities, National Institutes of Health.
The views expressed in this manuscript are those of the authors and do not necessarily represent the views of the National Cancer Institute; the National Heart, Lung, and Blood Institute; the National Institute of Minority Health and Health Disparities; the National Institutes of Health; or the US Department of Health and Human Services.
Conflict of interest: none declared.
Abbreviations
- CI
confidence interval
- HR
hazard ratio
- SES
socioeconomic status
REFERENCES
- 1. Diez Roux AV. Investigating neighborhood and area effects on health. Am J Public Health. 2001;91(11):1783–1789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Major JM, Doubeni CA, Freedman ND, et al. . Neighborhood socioeconomic deprivation and mortality: NIH-AARP Diet and Health Study. PLoS One. 2010;5(11):e15538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Doubeni CA, Laiyemo AO, Major JM, et al. . Socioeconomic status and the risk of colorectal cancer: an analysis of more than a half million adults in the National Institutes of Health-AARP Diet and Health Study. Cancer. 2012;118(14):3636–3644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Signorello LB, Cohen SS, Williams DR, et al. . Socioeconomic status, race, and mortality: a prospective cohort study. Am J Public Health. 2014;104(12):e98–e107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bethea TN, Palmer JR, Rosenberg L, et al. . Neighborhood socioeconomic status in relation to all-cause, cancer, and cardiovascular mortality in the Black Women’s Health Study. Ethn Dis. 2016;26(2):157–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Osypuk TL, Schmidt NM, Bates LM, et al. . Gender and crime victimization modify neighborhood effects on adolescent mental health. Pediatrics. 2012;130(3):472–481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ludwig J, Sanbonmatsu L, Gennetian L, et al. . Neighborhoods, obesity, and diabetes—a randomized social experiment. N Engl J Med. 2011;365(16):1509–1519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Votruba ME, Kling JR. Effects of neighborhood characteristics on the mortality of black male youth: evidence from Gautreaux, Chicago. Soc Sci Med. 2009;68(5):814–823. [DOI] [PubMed] [Google Scholar]
- 9. Kershaw KN, Robinson WR, Gordon-Larsen P, et al. . Association of changes in neighborhood-level racial residential segregation with changes in blood pressure among black adults: the CARDIA Study. JAMA Intern Med. 2017;177(7):996–1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Powell-Wiley TM, Cooper-McCann R, Ayers C, et al. . Change in neighborhood socioeconomic status and weight gain: Dallas Heart Study. Am J Prev Med. 2015;49(1):72–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Leonard T, Ayers C, Das S, et al. . Do neighborhoods matter differently for movers and non-movers? Analysis of weight gain in the longitudinal Dallas Heart Study. Health Place. 2017;44:52–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Jokela M. Are neighborhood health associations causal? A 10-year prospective cohort study with repeated measurements. Am J Epidemiol. 2014;180(8):776–784. [DOI] [PubMed] [Google Scholar]
- 13. Jokela M. Does neighbourhood deprivation cause poor health? Within-individual analysis of movers in a prospective cohort study. J Epidemiol Community Health. 2015;.69(9):899–904. [DOI] [PubMed] [Google Scholar]
- 14. Fischer CS. Ever-more rooted Americans. City Community. 2002;1(2):177–198. [Google Scholar]
- 15. Powell-Wiley TM, Ayers C, Agyemang P, et al. . Neighborhood-level socioeconomic deprivation predicts weight gain in a multi-ethnic population: longitudinal data from the Dallas Heart Study. Prev Med. 2014;66:22–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Margerison-Zilko C, Cubbin C, Jun J, et al. . Beyond the cross-sectional: neighborhood poverty histories and preterm birth. Am J Public Health. 2015;105(6):1174–1180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Powell-Wiley TM, Moore K, Allen N, et al. . Associations of neighborhood crime and safety and with changes in body mass index and waist circumference: the Multi-Ethnic Study of Atherosclerosis. Am J Epidemiol. 2017;180(3):280–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Zhang YT, Mujahid MS, Laraia BA, et al. . Association between neighborhood supermarket presence and glycated hemoglobin levels among patients with type 2 diabetes mellitus. Am J Epidemiol. 2017:185(12):1297–1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Hirsch JA, Grengs J, Schulz A, et al. . How much are built environments changing, and where?: patterns of change by neighborhood sociodemographic characteristics across seven US metropolitan areas. Soc Sci Med. 2016;169:97–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Hirsch JA, Green GF, Peterson M, et al. . Neighborhood sociodemographics and change in built infrastructure. J Urban. 2017;10(2):181–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Schatzkin A, Subar AF, Thompson FE, et al. . Design and serendipity in establishing a large cohort with wide dietary intake distributions: the National Institutes of Health-American Association of Retired Persons Diet and Health Study. Am J Epidemiol. 2001;154(12):1119–1125. [DOI] [PubMed] [Google Scholar]
- 22. Messer LC, Laraia BA, Kaufman JS, et al. . The development of a standardized neighborhood deprivation index. J Urban Health. 2006;83(6):1041–1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Hermansen SW, Leitzmann MF, Schatzkin A. The impact on National Death Index ascertainment of limiting submissions to Social Security Administration Death Master File matches in epidemiologic studies of mortality. Am J Epidemiol. 2009;169(7):901–908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hosmer DW, Lemeshow S. Applied Logistic Regression. 2nd ed New York, NY: John Wiley & Sons, Inc.; 2000. [Google Scholar]
- 25. Glymour MM, Weuve J, Berkman LF, et al. . When is baseline adjustment useful in analyses of change? An example with education and cognitive change. Am J Epidemiol. 2005;162(3):267–278. [DOI] [PubMed] [Google Scholar]
- 26. Seaman SR, White IR. Review of inverse probability weighting for dealing with missing data. Stat Methods Med Res. 2013;22(3):278–295. [DOI] [PubMed] [Google Scholar]
- 27. Guenther PM, Reedy J, Krebs-Smith SM. Development of the Healthy Eating Index-2005. J Am Diet Assoc. 2008;108(11):1896–1901. [DOI] [PubMed] [Google Scholar]
- 28. Hirsch JA, Moore KA, Barrientos-Gutierrez T, et al. . Built environment change and change in BMI and waist circumference: Multi-Ethnic Study of Atherosclerosis. Obesity (Silver Spring). 2014;22(11):2450–2457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Althoff T, Sosič R, Hicks JL, et al. . Large-scale physical activity data reveal worldwide activity inequality. Nature. 2017;547(7663):336–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Warren Andersen S, Blot WJ, Shu XO, et al. . Associations between neighborhood environment, health behaviors, and mortality. Am J Prev Med. 2018;54(1):87–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Meijer M, Röhl J, Bloomfield K, et al. . Do neighborhoods affect individual mortality? A systematic review and meta-analysis of multilevel studies. Soc Sci Med. 2012;74(8):1204–1212. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.