Abstract
A large body of epidemiologic research has concentrated on the 1918 influenza pandemic, but more work is needed to understand spatial variation in pandemic mortality and its effects on natality. We collected and analyzed 35,151 death records from Arizona for 1915–1921 and 21,334 birth records from Maricopa county for 1915–1925. We estimated the number of excess deaths and births before, during, and after the pandemic period, and we found a significant decline in the number of births occurring 9–11 months after peak pandemic mortality. Moreover, excess mortality rates were highest in northern Arizona counties, where Native Americans were historically concentrated, suggesting a link between ethnic and/or sociodemographic factors and risk of pandemic-related death. The relationship between birth patterns and pandemic mortality risk should be further studied at different spatial scales and in different ethnic groups.
Keywords: 1918–1920, Arizona, birth, excess mortality, influenza pandemic, Maricopa county, natality
The Spanish Flu of 1918–1920 was called “the mother of all pandemics” due to its devastating global mortality impact, estimated at 50 million deaths, or 1%–2% of the world population at the time (1, 2). The case fatality rate of this pandemic is estimated at approximately 2.5%—several-fold higher than that of typical seasonal influenza epidemics (1). Another salient feature of this pandemic is the atypical peak of mortality among young adults (3). Multiple pandemic waves occurred during 1918–1920, and areas in the Northern Hemisphere were more likely to experience a “herald wave” in early 1918 (1, 4–6). While our understanding of the mortality impact of this pandemic has improved in recent years, much less is known about the pandemic impact on natality. This is important given that influenza vaccination during pregnancy is currently being promoted. Further, more work is needed to disentangle the local circumstances that shaped pandemic mortality rates across different populations (7).
A lethal influenza pandemic may influence birth rate patterns (8–10) because pregnancy leads to physiological, hormonal, and immunologic changes that are known to heighten the risk of illness and death associated with influenza infection (11, 12). For instance, a cross-sectional study of pregnant women hospitalized during the 1918 influenza pandemic in Maryland, in the United States, found that about half of the pregnant women developed pneumonia, of whom 50% succumbed, with a case fatality rate of 27% (13). Also, a 1957 influenza pandemic study from Minnesota documented that about 50% of deaths among women of reproductive age occurred among pregnant women (14). Furthermore, recent studies have suggested a link between influenza infection in early pregnancy and an increased risk of fetal death (15). Accordingly, US and Scandinavian populations experienced a 5%–15% drop in natality rate 6–7 months after the 1918 pandemic, suggesting an increased risk of miscarriage in the first trimester (9). A similar association was reported during the 1957 pandemic (13, 16). However, prior studies of the 1918 pandemic have focused on highly aggregated national birth statistics, rather than detailed information available from individual birth certificates; further, no study has explored birth patterns in particularly hard hit and low-income populations.
Increasing epidemiologic evidence indicates that the 1918 pandemic was far from a “democratic disease.” Indeed, differences in socioeconomic conditions or residual immunity acquired from prior exposure to related influenza viruses have been hypothesized to drive mortality differences (17–20). A seminal study proposed that national income differences could in part explain an approximately 30-fold variation in 1918 pandemic mortality rates across 20 countries (7). Further work is needed to better understand the spatial heterogeneity in 1918 pandemic mortality impact at finer spatial scales.
In this paper we harness information from 35,151 individual death certificates to analyze differences in pandemic-related excess mortality rates across 13 counties of Arizona. Prior work has shown that the 1918–1920 pandemic killed about 0.8% of the population in Arizona (19), which is one of the highest pandemic mortality rates reported in the United States (21, 22). We also analyzed 21,334 individual birth certificates to quantify the impact of the 1918–1920 influenza pandemic on natality fluctuations in Maricopa county, the most populous county in Arizona state.
METHODS
Study setting
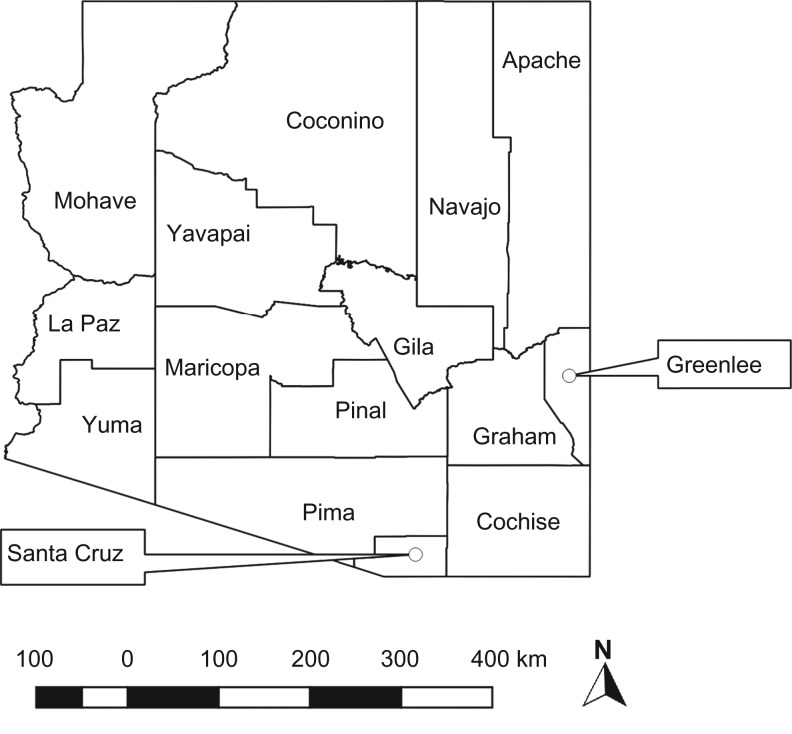
Arizona became a US state in 1912, a few years prior to the 1918 influenza pandemic, and did not become a US vital registration state until 1926 (23); therefore, alternative data sources have to be queried to explore mortality and natality during the pandemic period. Maricopa county is the largest county in this state. In 1920, Maricopa county represented 26.8% of the Arizona population (24). Between 1910 and 1920 the population of Maricopa county increased from 34,488 to 89,576 (see Figure 1 for a county map of Arizona).
Figure 1.
Counties in the US state of Arizona.
Arizona is unique because of its large population of Native Americans and its historical concentration of tuberculosis sanatoriums, due to a dry and arid climate (25). Arizona is one of 4 states with more than 100,000 Native Americans (26). Well-known Native American tribes in Arizona include Apache, Hopi, Maricopa, Navajo, Papago, Pima, Yavapai, and Yuma. More than 20 Native American reservations have covered one-fourth of the state’s surface area. Of these, the Navajo and the Tohono O’odham are the largest reservations in the United States (27). The Navajo reservation include areas in the Apache, Navajo, and Coconino counties, whereas the Tohono O’odham reservation lies in central Pima and includes southwestern Pinal and southeastern Maricopa counties. Overall, the northeastern part of Arizona has a higher residence of Native Americans (28, 29).
The state of Arizona had one of the highest tuberculosis death rates (25), the highest infant mortality rate, and, in its capital city (Phoenix), some of the “worst slums” in the country (30, 31). During 1918–1920, many minority households relied on irrigation canals for drinking water and for bathing (30). Infant mortality rates among black persons, Hispanics, and Native Americans were 2–3 times higher than among white persons (30, 32).
Data sources
The Arizona Genealogy Database (http://genealogy.az.gov/) is a freely available online resource of all birth records generated during the years 1855–1941 and all death certificates recorded during the years 1870–1996 for the state of Arizona. We manually retrieved a total of 21,334 birth records from January 1915 to December 1925 for Maricopa county, Arizona, from this database. For each birth record, we retrieved the date of birth and compiled monthly birth time series, as in a previous study (see Chandra and Yu (10)).
Similarly, to assess the timing and mortality impact of the 1918–1920 influenza pandemic, we manually retrieved a total of 35,151 individual death records from January 1915 to December 1921 for Arizona. For each death record, we compiled date of death, county of death, cause of death, and age at death. We then created weekly and monthly time series of deaths attributed to pneumonia and influenza (P&I) and to all causes, which are traditionally used to monitor the impact of influenza.
We also derived the overall and age-specific population estimates of the 13 Arizona counties from 1915 to 1925 by linear interpolation of estimates available for decennial censuses in 1910, 1920, and 1930 (24, 33). Two counties, Greenlee and Lapaz, were excluded from analysis due to lack of population data.
Statistical analysis
Pandemic period and excess deaths
To define the pandemic period, we determined the most likely period of pandemic influenza activity from the time series of weekly P&I death rates, the most specific indicator of influenza. We first estimated baseline mortality levels by fitting cyclical Serfling regression models to P&I deaths in noninfluenza weeks as in previous studies (19, 34). Periods of pandemic influenza circulation corresponded to those weeks in 1918–1921 where the observed total P&I mortality rate exceeded the upper 95% confidence limit of the baseline level (19, 21, 34). These pandemic periods were used to assess mortality and natality estimation for different counties, sexes, age groups, and causes of death (19). For each county, we estimated excess mortality rates for total population as well as children (<5 years) during the main pandemic wave (October to December) of 1918. We also classified our study period into 3 categories—before the pandemic, during the pandemic, and after the pandemic—based on observed P&I mortality patterns (we return to this later). We added 10 months to the pandemic period to account for the duration of pregnancy, in line with the expected delay between pandemic activity and birth outcomes (10).
Estimation of seasonally and trend-adjusted excess births and deaths
After removing the seasonality and long-term trend components using moving averages, the residual components of the birth and death time series were extracted to capture the corresponding birth and death counts associated with the pandemic. We then estimated the cross-correlation coefficients of P&I deaths and births to identify temporal associations between pandemic influenza and natality at different lags, as in previous studies (10, 35, 36). We estimated these coefficients to identify temporal associations between monthly deaths and births during the pandemic period.
The following definition of cross-correlation coefficient was used (35):
where
where, dt, bt, and k represent deaths in month t, births in month t, and the time difference between the birth and death series (i.e., the number of time lags or leads), respectively. In this study, cross-correlations with lags or leads of up to 12 months (−12 ≤ k ≤ 12) were estimated for the period of 1915–1921. Then, we employed the augmented Dickey-Fuller test for stationarity analysis, Mann-Kendall test for trend analysis, and null hypotheses of zero cross-correlation for each of the estimated correlation coefficients.
All P values reported are 2-sided. Statistical analyses were performed in SAS, version 9.4 (SAS Institute Inc., Cary, North Carolina), and R, version 3.2.3 (R Foundation for Statistical Computing, Vienna, Austria).
RESULTS
Pandemic waves
Based on the time series of P&I deaths, 4 different pandemic waves were identified in Arizona: spring 1918 (April 1918), fall 1918 (October to December 1918), winter 1919 (January to April 1919), and winter 1920 (February to April 1920). Accordingly, we defined our 3 study periods as follows: 1) before the pandemic (January 1915 to March 1918); 2) pandemic (April 1918 to April 1920 plus 10 months); and 3) after the pandemic (March 1921 to December 1925) (Table 1).
Table 1.
Three Study Periods, Maricopa County, Arizona, 1915–1921
| Period | Definition | Dates | t (Month No.)a |
|---|---|---|---|
| 1 | Before the pandemic | January 1915 to March 1918 | 1–39 |
| 2 | Pandemic | April 1918 to April 1920 + 10 months | 40–(64 + 10)b |
| 3 | After the pandemic | March 1921 to December 1925 | 75–132 |
at is a running number for month, starting from January 1915 (t = 1 for January 1915).
b A lag up to 10 months was considered between influenza activity and birth, to fully account for pregnancy.
Seasonally and trend-adjusted excess births and deaths, Maricopa county
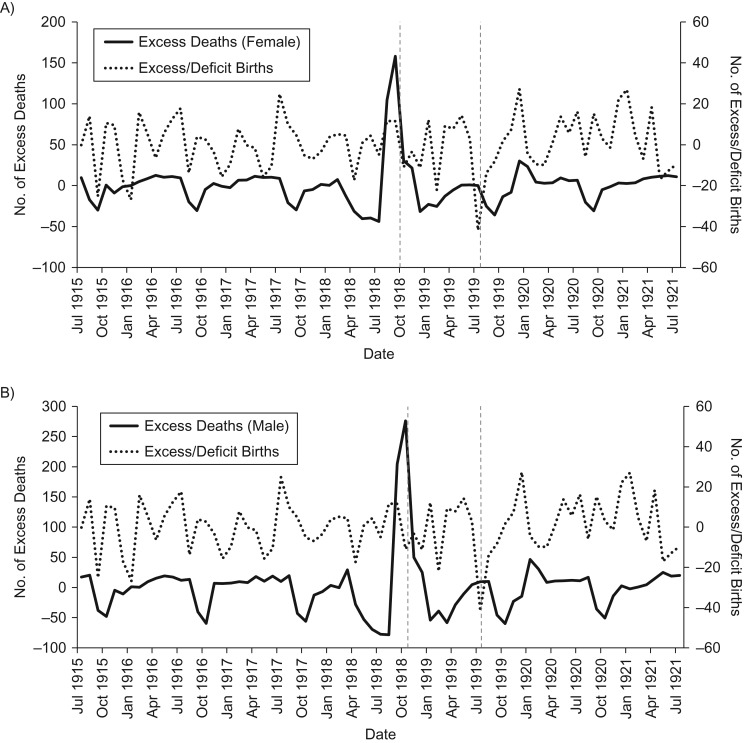
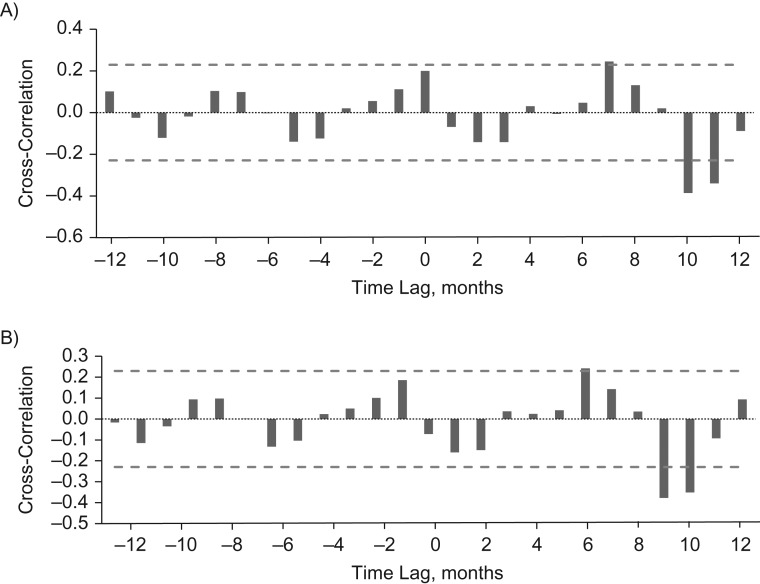
Figure 2 displays the time series of seasonally and trend-adjusted excess births and deaths for Maricopa county, Arizona, between 1915 and 1921, stratified by sex. A small peak in births was observed immediately after pandemic mortality peaked in males and females, while deep troughs in births occurred about 10 months after the peak in pandemic mortality. To formally test the time scale of the association between pandemic activity and births, we calculated the cross-correlation between excess births and sex-specific P&I deaths in individuals aged 10–49 years. We found a significant negative association between influenza deaths in males at time t and births 9–10 months later, and 10–11 months later for female deaths (Figure 3). A natality dip of approximately 43% was observed in July 1919; dips of this size were not seen at any other time point during 1915–1921.
Figure 2.
Excess and deficit births and excess pneumonia and influenza deaths, according to sex, Maricopa County, Arizona, 1915–1921. Time series of seasonally and trend-adjusted variance in births and excess number of pneumonia and influenza deaths is presented for female (A) and male (B) persons. The vertical dashed lines indicate the timing of peak excess deaths and deficit births, respectively.
Figure 3.
Cross-correlations between the excess number of pneumonia and influenza deaths and excess births, Maricopa County, Arizona, 1915–1921. Cross-correlation coefficients were calculated at each lag and lead period (−12 to +12 months); 0 indicates no lag. A) Female persons. B) Male persons. Bars represent cross-correlation coefficients between birth and death time series, and the horizontal dashed lines are the confidence interval (CI) for the null hypothesis of zero correlation between birth and death time series (upper CI = 0.23, lower CI = 0.23).
Spatial analysis of pandemic excess mortality according to time period
The total excess mortality rates according to mortality outcomes, sex, and pandemic waves are shown in Table 2. For the total pandemic period, total P&I excess death rates per 10,000 population were 98.3 for males and 75.9 for females. For both males and females, the highest P&I and all-cause death rates were recorded during the main pandemic wave in fall 1918. In relative terms, during the pandemic period the observed P&I mortality rates were about 5 times and 4 times above the baseline for males and females, respectively (Table 2). The mortality rate ratio of male to female deaths was 1.23.
Table 2.
Estimates of Excess Mortality Rate per 10,000 Population and Rate Ratio Attributable to Pandemic Influenza, According to Time of Pandemic Wave and Sex, Maricopa County, Arizona, 1918–1921
| Cause of Death and Pandemic Wave | Male | Female | ||
|---|---|---|---|---|
| Excess Death Rate per 10,000 Population | RR | Excess Death Rate per 10,000 Population | RR | |
| P&I deaths | ||||
| Spring 1918 (April 1918) | 0.23 | 1.26 | 0.25 | 1.22 |
| Fall 1918 (October to December, 1918) | 63.78 | 10.32 | 48.7 | 7.85 |
| Winter 1919 (January to April 1919) | 20.89 | 3.06 | 18.67 | 2.75 |
| Winter 1920 (February 1st to April 11th, 1920) | 13.42 | 3.13 | 8.26 | 2.53 |
| Total pandemic period | 98.32 | 5.07 | 75.88 | 4.12 |
| All-cause deaths | ||||
| Spring 1918 (April 1918) | 3.5 | 1.21 | 4.77 | 1.40 |
| Fall 1918 (October to December 1918) | 67.45 | 2.22 | 49.08 | 2.22 |
| Winter 1919 (January to April 1919) | 17.17 | 1.25 | 13.0 | 1.26 |
| Winter 1920 (February 1st to April 11th, 1920) | 13.54 | 1.25 | 13.7 | 1.41 |
| Total pandemic period | 101.66 | 1.52 | 80.55 | 1.60 |
Abbreviations: P&I, pneumonia and influenza; RR, rate ratio.
We also estimated county-specific excess mortality rates for all ages and for children aged <5 years for 13 counties in Arizona that provided appropriately stratified data (Table 3). We found that northern counties had higher excess P&I and all-cause mortality overall and for children aged <5 years. Northern counties Apache, Coconino, Mohave, and Navajo had significantly higher excess P&I mortality for children aged <5 years (mean rank = 10.50) compared with other counties (all other counties categorized as “others”; mean rank = 5.44) (Mann-Whitney U test, P < 0.05). However, there was no statistically significant mortality difference in all-age or all-cause deaths (Mann-Whitney U test, P > 0.05).
Table 3.
Country-Specific Excess Pneumonia and Influenza and All-Cause Mortality Rates per 10,000 for Children Aged <5 Years and All Ages, Pandemic Influenza Wave, Arizona, Fall 1918
| County | Excess P&I Mortality Among Ages <5 Years | Excess All-Cause Mortality Among Ages <5 Years | Excess P&I Mortality Among Total Population | Excess All-Cause Mortality Among Total Population |
|---|---|---|---|---|
| Apachea | 150.30 | 86.00 | 82.92 | 76.05 |
| Coconinoa | 225.80 | 168.20 | 131.68 | 120.20 |
| Gilaa | 131.80 | 94.10 | 94.41 | 88.09 |
| Mohavea | 302.60 | 207.70 | 115.02 | 115.98 |
| Navajoa | 88.80 | 72.00 | 25.59 | 24.98 |
| Yavapaia | 121.60 | 109.50 | 80.46 | 82.36 |
| Maricopa | 64.90 | 54.20 | 56.83 | 58.91 |
| Cochiseb | 111.30 | 110.30 | 68.65 | 69.61 |
| Grahamb | 45.50 | 15.20 | 20.94 | 21.02 |
| Pimab | 47.50 | 88.10 | 52.99 | 70.88 |
| Pinalb | 74.30 | 89.30 | 48.05 | 56.91 |
| Santa Cruzb | 62.90 | 48.90 | 28.55 | 34.91 |
| Yumab | 146.70 | 124.90 | 78.20 | 90.66 |
Abbreviation: P&I, pneumonia and influenza.
a Northern Arizona.
b Southern Arizona.
DISCUSSION
In this study, we investigated the impact of the 1918 influenza pandemic on natality fluctuations as well as on county-level mortality in the state of Arizona. We expected a natality decline in the months following peak pandemic activity, as observed in a previous study set in the United States (9). Although the time series of excess/deficit births fluctuated over time in Maricopa County, Arizona, we found a statistically significant dip of approximately 43% in births 9–11 months after peak pandemic mortality. While smaller natality drops were seen in earlier years, a drop of this magnitude was unique to the period after the pandemic, suggesting an effect of the pandemic on natality. We also found higher pandemic-related death rates in northern Arizona counties, where Native Americans were historically concentrated.
Indigenous populations have been disproportionately affected during past influenza pandemics (37, 38). For example, in New Zealand, the death rate among the Maori was at least 7.3 times higher than the corresponding death rate for the rest of the population (38). Similarly, the mortality ratios for indigenous populations relative to European populations in the continental United States and Canada were found to be 3.2 and 4.8 during the 1918 pandemic, respectively (37). Likewise, our results suggest that northern counties in Arizona with high Native American population density (e.g., Apache, Coconino, and Navajo) experienced higher excess pandemic death rates compared with other counties in the state. Anecdotal evidence recorded in the Arizona Bulletin of 1918 indicated that northern cities with a significant proportion of Native Americans (27, 28) (Winslow, Holbrook, and Flagstaff) required assistance in confronting the pandemic (29). We note that quantitative data on the proportion of Native Americans by county was not available; further work should focus on exploring the association between influenza death rates and ethnicity in a more quantitative manner.
We also found high excess mortality rates in the southern mining counties of Cochise and Yuma. Cochise county was one of the counties that had operating copper mines and smelters, and Yuma county had one of the oldest silver and lead mines in the state. Mining activity could be a proxy for lower socioeconomic conditions. We cannot rule out additional within-county variability in socioeconomic factors, including, nutritional status, overall baseline health, and access to hospital care. For instance, some of the lowest pandemic mortality rates were observed in Maricopa county, within which South Phoenix was a rather stigmatized and degraded minority district (30). The study of within-county variation in pandemic mortality calls for more spatially resolved data sets.
It is important to highlight that at the time of the pandemic, the state of Arizona was characterized by significant contamination issues, lack of potable water, crowding, substandard housing, and a lack of health care for minorities (29, 30). On one hand, the state was advertised as a privileged location for health seekers due to its dry climate and pure air, but on the other hand many lived in ill-ventilated buildings and were at high risk of contracting infectious diseases (29). Many minority families in Phoenix were found to be eating and sleeping in a single room, and children were found living in the same room with persons afflicted with tuberculosis (30). Arizona had the highest infant mortality rate of all US states, particularly among minorities (30, 31). In this context, perhaps it is not surprising that the 1918 influenza pandemic disproportionately affected lower socioeconomic groups, including Native American populations geographically concentrated in northern counties.
Our study is subject to several limitations. First, due to lack of laboratory confirmation of influenza infection in the era before virology, our excess mortality approach would not have been able to distinguish elevation in mortality rates associated with noninfluenza respiratory causes and coinciding with the pandemic period. Second, we did not model other factors associated with World War I that could have influenced fertility rates (39). Third, a more refined analysis at the neighborhood level could have revealed more clearly the association of specific risk factors, including tuberculosis, income, occupation, and ethnicity (40).
In summary, we report a significant dip in excess births about 9–11 months following the peak in excess pandemic mortality. This period surpasses the expected 9 months of pregnancy and may be due to delays in reporting births or a stronger impact of influenza on pregnancy in the later part of the fall pandemic wave. Our results also show significant county-level variation in excess mortality rates during the 1918 influenza pandemic. For instance, we found that Arizona counties with relatively higher Native American population located in northern Arizona were disproportionately affected by the pandemic. Future research is needed to disentangle spatial variation in excess mortality and birth rates at finer spatial resolutions (e.g., neighborhood) in relation to demographic and socioeconomic indicators.
ACKNOWLEDGMENTS
Author affiliations: Department of Population Health Sciences, School of Public Health, Georgia State University, Atlanta, Georgia (Sushma Dahal, Kenji Mizumoto, Gerardo Chowell); Graduate School of Medicine, Hokkaido University, Hokkaido, Japan (Kenji Mizumoto); School of Human Evolution and Social Change, Arizona State University, Tempe, Arizona (Bob Bolin); and Division of International Epidemiology and Population Studies, Fogarty International Center, National Institutes of Health, Bethesda, Maryland (Cecile Viboud, Gerardo Chowell).
S.D. acknowledges support from the Fulbright program. This work was funded by the Japanese Society for the Promotion of Science (grants 15K20936 and 18K17368 to K.M.); the Program for Advancing Strategic International Networks to Accelerate the Circulation of Talented (grant G2801 to K.M.); the Multinational Influenza Seasonal Mortality Study (http://www.misms.net), Fogarty International Center, National Institutes of Health (support to G.C. and C.V.); the RAPIDD Program, Science and Technology Directorate, Department of Homeland Security (support to G.C. and C.V.); the National Science Foundation (grant 1414374 to G.C.), as part of the joint National Science Foundation–National Institutes of Health–US Department of Agriculture Ecology and Evolution of Infectious Diseases program; and the United Kingdom Biotechnology and Biological Sciences Research Council (grant BB/M008894/1).
This work does not represent the views of the US Government or the National Institutes of Health.
Conflict of interest: none declared.
Abbreviation
- P&I
pneumonia and influenza
REFERENCES
- 1. Taubenberger JK, Morens DM. 1918 influenza: the mother of all pandemics. Emerg Infect Dis. 2006;12(1):15–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Johnson NP, Mueller J. Updating the accounts: global mortality of the 1918–1920 “Spanish” influenza pandemic. Bull Hist Med. 2002;76(1):105–115. [DOI] [PubMed] [Google Scholar]
- 3. Miller MA, Viboud C, Balinska M, et al. . The signature features of influenza pandemics—implications for policy. N Engl J Med. 2009;360(25):2595–2598. [DOI] [PubMed] [Google Scholar]
- 4. Morens DM, Fauci AS. The 1918 influenza pandemic: insights for the 21st century. J Infect Dis. 2007;195(7):1018–1028. [DOI] [PubMed] [Google Scholar]
- 5. Simonsen L, Chowell G, Andreasen V, et al. . A review of herald pandemic waves in 1918: importance for contemporary pandemic response strategies. Ann Epidemiol. 2018;28(5):281–288. [DOI] [PubMed] [Google Scholar]
- 6. Sattenspiel L. Regional patterns of mortality during the 1918 influenza pandemic in Newfoundland. Vaccine. 2011;29(suppl 2):B33–B37. [DOI] [PubMed] [Google Scholar]
- 7. Murray CJ, Lopez AD, Chin B, et al. . Estimation of potential global pandemic influenza mortality on the basis of vital registry data from the 1918–20 pandemic: a quantitative analysis. Lancet. 2006;368(9554):2211–2218. [DOI] [PubMed] [Google Scholar]
- 8. Mamelund S-E. Can the Spanish influenza pandemic of 1918 explain the baby boom of 1920 in neutral Norway? Population (english edition). 2004;59(2):229–260. [Google Scholar]
- 9. Bloom-Feshbach K, Simonsen L, Viboud C, et al. . Natality decline and miscarriages associated with the 1918 influenza pandemic: the Scandinavian and United States experiences. J Infect Dis. 2011;204(8):1157–1164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Chandra S, Yu YL. Fertility decline and the 1918 influenza pandemic in Taiwan. Biodemography Soc Biol. 2015;61(3):266–272. [DOI] [PubMed] [Google Scholar]
- 11. Rasmussen SA, Jamieson DJ, Bresee JS. Pandemic influenza and pregnant women. Emerg Infect Dis. 2008;14(1):95–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Rasmussen SA, Jamieson DJ, Uyeki TM. Effects of influenza on pregnant women and infants. Am J Obstet Gynecol. 2012;207(3):S3–S8. [DOI] [PubMed] [Google Scholar]
- 13. Harris JW. Influenza occurring in pregnant women: a statistical study of thirteen hundred and fifty cases. J Am Med Assoc. 1919;72(14):978–980. [Google Scholar]
- 14. Freeman DW, Barno A. Deaths from Asian influenza associated with pregnancy. Am J Obstet Gynecol. 1959;78(6):1172–1175. [DOI] [PubMed] [Google Scholar]
- 15. Lieberman RW, Bagdasarian N, Thomas D, et al. . Seasonal influenza A (H1N1) infection in early pregnancy and second trimester fetal demise. Emerg Infect Dis. 2011;17(1):107–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hardy JM, Azarowicz EN, Mannini A, et al. . The effect of Asian influenza on the outcome of pregnancy, Baltimore, 1957–1958. Am J Public Health Nations Health. 1961;51(8):1182–1188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Chowell G, Erkoreka A, Viboud C, et al. . Spatial-temporal excess mortality patterns of the 1918–1919 influenza pandemic in Spain. BMC Infect Dis. 2014;14:371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Noymer A, Garenne M. The 1918 influenza epidemic’s effects on sex differentials in mortality in the United States. Popul Dev Rev. 2000;26(3):565–581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Dahal S, Jenner M, Dinh L, et al. . Excess mortality patterns during 1918–1921 influenza pandemic in the state of Arizona, USA. Ann Epidemiol. 2017;28(5):273–280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Mamelund SE. 1918 pandemic morbidity: the first wave hits the poor, the second wave hits the rich. Influenza Other Respir Viruses. 2018;12(3):307–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Viboud C, Eisenstein J, Reid AH, et al. . Age- and sex-specific mortality associated with the 1918–1919 influenza pandemic in Kentucky. J Infect Dis. 2013;207(5):721–729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Olson DR, Simonsen L, Edelson PJ, et al. . Epidemiological evidence of an early wave of the 1918 influenza pandemic in New York City. Proc Natl Acad Sci U S A. 2005;102(31):11059–11063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Linder FE, Grove RD. Vital Statistics Rates in the United States 1900–1940. Washington, DC: United States Government Printing Office; 1947. https://www.cdc.gov/nchs/data/vsus/vsrates1900_40.pdf. Accessed March 20, 2018. [Google Scholar]
- 24. Forstall RL, ed. Population of States and Counties of the United States: 1790–1990. Washington, DC: US Bureau of the Census; 1996. https://www.census.gov/population/www/censusdata/PopulationofStatesandCountiesoftheUnitedStates1790-1990.pdf. Accessed March 10, 2018. [Google Scholar]
- 25. Grineski SE, Bolin B, Agadjanian V. Tuberculosis and urban growth: class, race and disease in early Phoenix, Arizona, USA. Health Place. 2006;12(4):603–616. [DOI] [PubMed] [Google Scholar]
- 26. Passel JS. The growing American Indian population, 1960–1990: beyond demography. Popul Res Policy Rev. 1997;16(1–2):11–31. [Google Scholar]
- 27. Arizona Edventures Top 10 Indian reservations. http://www.arizonaedventures.com/arizona/blog/things-to-see-do/arizona-top-ten/indian-reservations/. Accessed March 20, 2018.
- 28. Arizona Edventures Arizona tribal and federal lands. http://www.arizonaedventures.com/images/IndianReservationsAZ.pdf. Accessed March 20, 2018.
- 29. State Board of Health Bulletin of the Arizona State Board of Health, Vol. VI, No. 8 Phoenix, AZ: Arizona State Board of Health; October 1918. [Google Scholar]
- 30. Bolin B, Grineski S, Collins T. The geography of despair: environmental racism and the making of South Phoenix, Arizona, USA. Hum Ecol Rev. 2005;12(2):156–168. [Google Scholar]
- 31. McLoughlin E. People’s Padre: An Autobiography. 15th ed Boston, MA: Beacon Press; 1954. [Google Scholar]
- 32. Buck CE. A Survey of Public Health in Arizona Phoenix, AZ: Arizona Statewide Public Health Committee; 1936. [Google Scholar]
- 33. United States Census Bureau Census of population and housing. Washington, DC: United States Census Bureau; 2018. http://www.census.gov/prod/www/decennial.html. Accessed February 20, 2018. [Google Scholar]
- 34. Chowell G, Simonsen L, Flores J, et al. . Death patterns during the 1918 influenza pandemic in Chile. Emerg Infect Dis. 2014;20(11):1803–1811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Bisgaard S, Kulahci M. Time Series Analysis and Forecasting by Example. Hoboken, NJ: John Wiley & Sons; 2011. [Google Scholar]
- 36. Zeger SL, Irizarry R, Peng RD. On time series analysis of public health and biomedical data. Annu Rev Public Health. 2006;27:57–79. [DOI] [PubMed] [Google Scholar]
- 37. Mamelund SE. Geography may explain adult mortality from the 1918–20 influenza pandemic. Epidemics. 2011;3(1):46–60. [DOI] [PubMed] [Google Scholar]
- 38. Wilson N, Barnard LT, Summers JA, et al. . Differential mortality rates by ethnicity in 3 influenza pandemics over a century, New Zealand. Emerg Infect Dis. 2012;18(1):71–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Mamelund SE. Fertility fluctuations in times of war and pandemic influenza. J Infect Dis. 2012;206(1):140–141. [DOI] [PubMed] [Google Scholar]
- 40. Grantz KH, Rane MS, Salje H, et al. . Disparities in influenza mortality and transmission related to sociodemographic factors within Chicago in the pandemic of 1918. Proc Natl Acad Sci U S A. 2016;113(48):13839–13844. [DOI] [PMC free article] [PubMed] [Google Scholar]