Abstract
Accurate quantification of minimal residual disease (MRD) during treatment of chronic myeloid leukemia (CML) guides clinical decisions. The conventional MRD method, RQ-PCR for BCR-ABL1 mRNA, reflects a composite of the number of circulating leukemic cells and the BCR-ABL1 transcripts per cell. BCR-ABL1 genomic DNA only reflects leukemic cell number. We used both methods in parallel to determine the relative contribution of the leukemic cell number to molecular response. BCR-ABL1 DNA PCR and RQ-PCR were monitored up to 24 months in 516 paired samples from 59 newly-diagnosed patients treated with first-line imatinib in the TIDEL-II study. In the first three months of treatment, BCR-ABL1 mRNA values declined more rapidly than DNA. By six months, the two measures aligned closely. The expression of BCR-ABL1 mRNA was normalized to cell number to generate an expression ratio. The expression of e13a2 BCR-ABL1 was lower than that of e14a2 transcripts at multiple time points during treatment. BCR-ABL1 DNA was quantifiable in 48% of samples with undetectable BCR-ABL1 mRNA, resulting in MRD being quantifiable for an additional 5-18 months (median 12 months). These parallel studies show for the first time that the rapid decline in BCR-ABL1 mRNA over the first three months of treatment is due to a reduction in both cell number and transcript level per cell, whereas beyond three months, falling levels of BCR-ABL1 mRNA are proportional to the depletion of leukemic cells.
Introduction
Real-time reverse transcriptase quantitative PCR (RQ-PCR) for BCR-ABL1 mRNA is widely used for the routine monitoring of chronic myeloid leukemia (CML) patients receiving tyrosine kinase inhibitor (TKI) therapy. The achievement of molecularly-defined therapeutic targets during TKI treatment is associated with superior progression-free and overall survival.1 The BCR-ABL1 mRNA level is a composite measurement that reflects both the proportion of leukemic cells in the sample, and the expression of BCR-ABL1 relative to its control gene. Pre-analytical factors, such as the rate of degradation of the target mRNA, and methodological factors, such as the efficiency of reverse transcription or the choice of control gene, may have a significant influence on the final result of RQ-PCR.2,3 Substantial effort has been invested to minimize variation due to such factors through the development of an International Scale (IS) for BCR-ABL1.4
An alternative approach to overcome the variability in RQ-PCR is to measure BCR-ABL1 genomic DNA, since the overwhelming majority of chronic phase CML patients will have a single copy of BCR-ABL1 and two copies of an autosomal control gene in each leukemic cell. In the past, this approach was not practical due to the complexity of sequencing individual genomic breakpoints. Almost all CML patients express one or both of the two common BCR-ABL1 mRNA transcripts (e13a2, e14a2), whereas the genomic fusion sequences involve introns that are spliced out from the mRNA, and are essentially unique to each individual patient.5 Advances in sequencing technology have made it relatively simple to detect BCR-ABL1 genomic breakpoints, and several methods have been published.6,7
It should be emphasized that DNA PCR and RQ-PCR are not expected to yield identical results. This is perhaps best exemplified by the comparison of RQ-PCR with metaphase karyotyping in CML, which shows that a partial cytogenetic response [≤35% Philadelphia-positive (Ph+) cells] is roughly equivalent to BCR-ABL1IS ≤10%.8 Whereas both techniques are clinically useful, measures of the size of the CML clone the end point of each assay is qualitatively different. BCR-ABL1 DNA PCR is analogous to fluorescence in situ hybridization, in that both methods measure the simple proportion of cells in a sample that carry the Philadelphia rearrangement.
We used quantitative BCR-ABL1 DNA techniques, Q-PCR and digital PCR (dPCR), to monitor a cohort of patients in the Australasian Leukaemia and Lymphoma Group (ALLG) CML9 study (TIDEL-II).9 These results were compared with routine RQ-PCR monitoring. Since the number of copies of BCR-ABL1 DNA is directly related to the number of leukemic cells in a sample, we used DNA and mRNA-based methods in order to determine the relative contribution of cell number and expression changes to molecular response in CML. Secondly, where there were differences between RQ-PCR and DNA PCR, we explored whether these differences might provide additional predictive information concerning treatment response.
Methods
Patients’ characteristics and samples
Fifty-nine newly diagnosed chronic phase CML patients from the TIDEL-II clinical trial9 were included in our study. Details of these patients and of the samples analyzed are presented in the Online Supplementary Appendix and Online Supplementary Tables S1 and S2. The overall clinical characteristics and treatment responses of the selected cohort were not significantly different from those of the overall study population. The subset of patients included here were selected in three categories: undetectable MRD (UMRD) achieved within the first 2 years (n=26); treatment failure (n=9); and 24 additional patients not falling into either of the first two categories. Treatment failure was defined following the European LeukemiaNet (ELN) criteria as loss of complete hemato-logic response, loss of complete cytogenetic response, loss of major molecular response (MMR; BCR-ABL1IS ≤0.1%), kinase domain mutations, or progression to accelerated phase/blast crisis).10
Peripheral blood samples for molecular analysis were collected prior to commencing TKI treatment (baseline); at one, two, and three months; and every three months thereafter up to 24 months. RQ-PCR was performed centrally in the diagnostic laboratory of SA Pathology, Adelaide, Australia, using the BCR control gene.11 The results were reported as BCR-ABL1/BCR% applying an IS conversion factor (Online Supplementary Appendix).4 Chromosome banding analysis was routinely performed at diagnosis in the respective local laboratories. Samples with fewer than 10 metaphases were excluded from this analysis.
All samples were collected with informed consent in accordance with the Institutional Ethics-approved protocols and with reference to the Declaration of Helsinki.
Breakpoint detection
The BCR-ABL1 genomic DNA breakpoint was determined, as previously described, in blood samples collected at diagnosis using long range PCR with a single forward primer in BCR and multiple reverse primers in ABL1 to amplify the breakpoint (Online Supplementary Appendix).12,13
Quantification of BCR-ABL1 DNA
Genomic DNA was extracted from peripheral blood leukocytes. The amount of amplifiable DNA in each sample was measured using the GUSB control gene. The earlier assays were performed using real-time Q-PCR with standard curves for both BCR-ABL1 (patient’s diagnostic DNA assigned a value of 100%) and GUSB (plasmid) diluted in non-human DNA. Later assays used digital PCR (dPCR) for both BCR-ABL1 and GUSB with the aim of improving precision. Results were reported as BCR-ABL1/GUSB% (corrected for the two copies of GUSB per cell) normalized against the individual patient’s diagnostic sample. Further details are provided in the Online Supplementary Appendix and Online Supplementary Figures S1-S3.
Statistical analysis
Statistical analysis was performed using the GraphPad Prism 7 statistical software (GraphPad Prism Inc., La Jolla, CA, USA). Agreement between assays was assessed using the method of Bland and Altman.14 Correlation between non-parametric values was assessed using Spearman rank coefficient. Differences between BCR-ABL1 DNA and mRNA measurements were compared using a Mann-Whitney test. The cumulative incidence of MMR and MR4.5 was calculated using the Fine and Gray regression method in R. Any event leading to the permanent discontinuation of imatinib/nilotinib (including treatment failure, intolerance, and death) was treated as a competing risk. P<0.05 was considered statistically significant.
Results
Comparison between DNA and mRNA before treatment
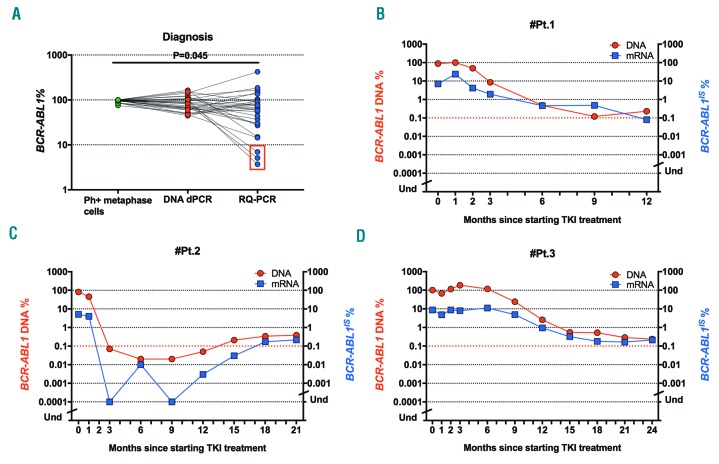
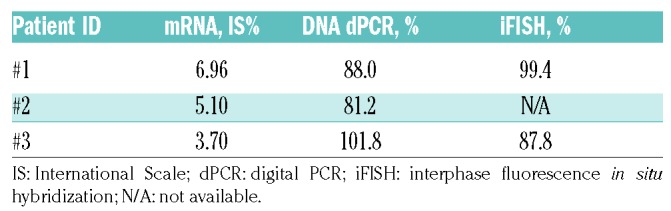
Since DNA Q-PCR quantifies BCR-ABL1 relative to the diagnostic DNA, we considered only the absolute dPCR values at diagnosis (n=29) and compared these values with the corresponding mRNA levels and the percentage of Ph+ bone marrow metaphase cells. The median value of BCR-ABL1 DNA prior to TKI treatment was 100% by karyotyping (range, 85-100%) and 84% (range, 45-164%) by dPCR. The corresponding median BCR-ABL1IS value was 70%, with values ranging from 3.7% to 425% (Figure 1A). Two of the 3 patients (#1 and #3) with low BCR-ABL1IS mRNA had stored peripheral blood cells available for interphase fluorescence in situ hybridization, which showed excellent agreement with the BCR-ABL1 DNA values obtained by dPCR (Table 1). Two of these 3 patients experienced treatment failure (blast crisis/secondary resistance with a kinase domain mutation) and the third patient had ELN warning features at baseline (high Sokal score and additional clonal chromosomal abnormalities in Ph+ cells) and failed to reach MMR by 12 months and MR4.5 by 24 months. All 3 of these patients expressed e13a2 BCR-ABL1 transcripts (one expressed both e13a2 and e14a2) and all had unusually low white blood cell counts at study entry (<20×109/L) (Online Supplementary Table S3). The post-treatment molecular responses of these 3 patients are shown in Figure 1B-D.
Figure 1.
DNA and mRNA prior to treatment. (A) Proportion of leukemic cells and BCR-ABL1 expression before treatment assessed by conventional cytogenetic analysis (green), DNA dPCR (red) and RQ-PCR (blue). Three patients with discrepant DNA and mRNA values are highlighted (red square). (B-D) Molecular response of patients (pts) with BCR-ABL1IS <10% despite DNA values close to 100%. Absolute DNA dPCR values are represented at diagnosis. TKI: tyrosine kinase inhibitor; Ph+: Philadelphia positive; Und: undetectable.
Table 1.
BCR-ABL1 values in patients with low mRNA values relative to DNA values.
Agreement of Q-PCR and dPCR for BCR-ABL1 DNA
Forty-six serial samples from 9 patients on TKI treatment were quantified by both Q-PCR and dPCR for BCR-ABL1 DNA. The results were highly correlated (r=0.94, P<0.0001). Agreement between the two methods was further assessed using a Bland-Altman plot (Online Supplementary Figure S4). The mean bias was -0.11-log with the 95% limits of agreement ranging from -1.02-log to 0.80-log (±8.1 fold) indicating that there was no systematic difference between the results obtained by the two DNA PCR methods after diagnosis. In subsequent analyses of BCR-ABL1 DNA during treatment the two sets of data were combined.
Faster reduction in BCR-ABL1 mRNA than DNA early in treatment
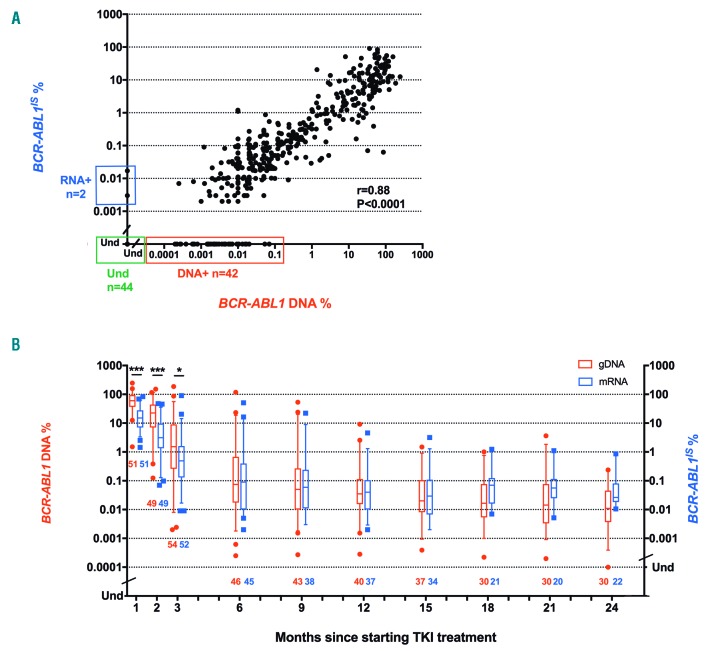
In our cohort of 59 patients, the quantified BCR-ABL1 mRNA and DNA results (undetectable values excluded) were highly correlated across the range of values during TKI treatment (r=0.88; P<0.0001) (Figure 2A). However, during the first three months of therapy BCR-ABL1 DNA values were significantly higher than mRNA, whereas from six months onwards there was good agreement between methods (Figure 2B). The median reduction in BCR-ABL1IS from baseline to three months was 2.05-log versus 1.75-log for BCR-ABL1 DNA (Online Supplementary Figure S5). This bias was independent of the BCR-ABL1 DNA quantification method (seen with both dPCR and Q-PCR; see Online Supplementary Figure S6).
Figure 2.
Comparison between mRNA and DNA quantification of BCR-ABL1. (A) Positive values from DNA (red) and mRNA (blue) were compared during treatment until 24 months. The quantifiable mRNA and DNA values were highly correlated, but at very low levels 42 samples were positive by DNA PCR only (red square). (B) The mRNA and DNA values (number, median and interquartile range) are shown for individual time points up to 24 months. Note that the apparent increase in RQ-PCR after 18 months is due to the exclusion of RQ-PCR samples in which there was undetectable BCR-ABL1. *P<0.05; ***P<0.0001; Und.: undetectable.
Early molecular response assessment by BCR-ABL1 mRNA and DNA
A reduction in BCR-ABL1IS to ≤10% at three months [early molecular response (EMR)] has emerged as an early treatment milestone that is strongly associated with later achievement of optimal response and progression-free survival.15,16 The predictive effect of EMR was confirmed in the overall TIDEL-II study population of 210 patients.9 In this smaller subgroup, no patient with BCR-ABL1IS levels >10% at three months went on to achieve MMR or MR4.5. We tested the predictive value of BCR-ABL1 levels by both mRNA and DNA at the 3-month landmark using the established BCR-ABL1 transcript IS cut-offs of 10% and 1%. Both mRNA and DNA levels were predictive of later MMR and MR4.5, and the BCR-ABL1 DNA level did not improve the predictive value of conventional RQ-PCR (Online Supplementary Figure S7). The optimal BCR-ABL1 DNA cut-off for prediction of later molecular response could not be determined in this study due to the small number of patients and the potential bias due to the selection of patients on the basis of response.
Transcript type and molecular response
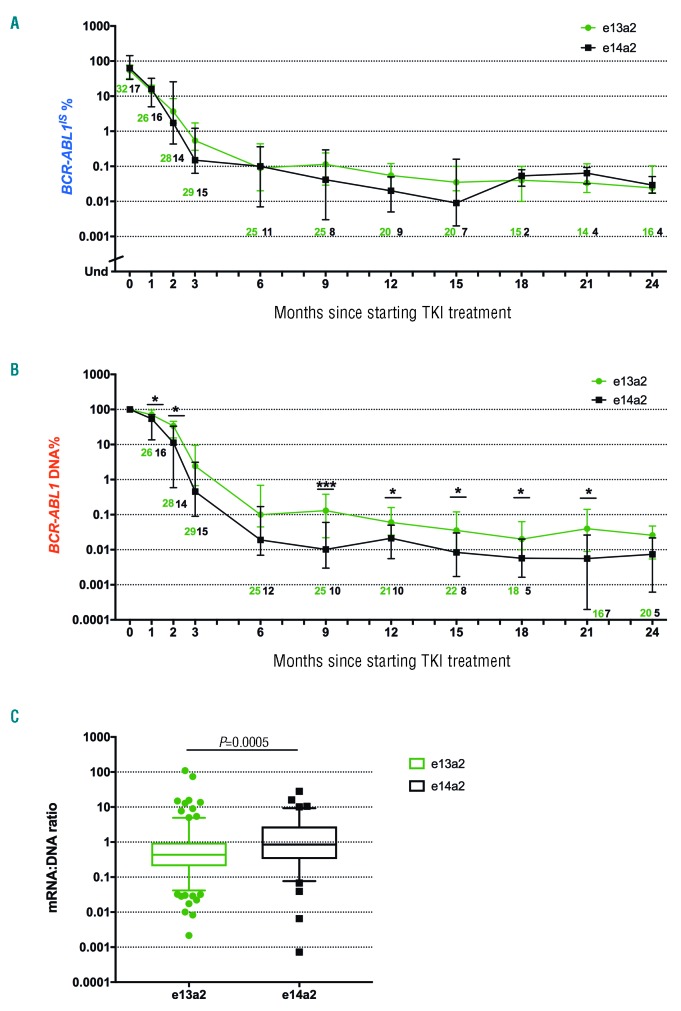
It has previously been reported that the BCR-ABL1 transcript type may influence treatment outcomes (reviewed by Marum and Branford17). Consequently, we compared molecular responses in patients having only e13a2 transcripts (n=32) or only e14a2 transcripts (n=17). There was no significant difference between BCR-ABL1IS levels according to transcript type at any individual time point (Figure 3A). However, BCR-ABL1 DNA was significantly higher in e13a2 patients at multiple time points during treatment (Figure 3B). The median BCR-ABL1 expression ratio (mRNA%:DNA%) was 0.5 for e13a2 versus 1.09 for e14a2 (P=0.0005) (Figure 3C). This analysis was repeated using BCR-ABL1 DNA values from dPCR and Q-PCR separately and a similar pattern was observed (Online Supplementary Figure S8).
Figure 3.
BCR-ABL1 transcript type and molecular response. (A) Comparison of the BCR-ABL1IS values during the first two years of tyrosine kinase inhibitor (TKI) treatment (e13a2 shown in green and e14a2 shown in black). (B) Comparison of e13a2 and e14a2 BCR-ABL1 DNA values in the same patients. Diagnostic values were assigned a value of 100%. Note that at later time points the proportion of e14a2 patients with undetectable BCR-ABL1 DNA was higher than for e13a2, which may result in an underestimation of the difference between the two transcript types. (C) Box and whiskers plot comparing BCR-ABL1 expression ratio (mRNA:DNA) for e13a2 and e14a2 transcripts. *P<0.05; ***P<0.001.
Sensitivity of RQ-PCR and DNA PCR
The median limit of detection achieved by RQ-PCR was MR4.6 (range, 3.2-5.1 log) in comparison with MR5.2 (range, 4.6-5.7 log) for DNA PCR. BCR-ABL1 DNA was detected in 42 of 86 samples with undetectable mRNA (49%) with a median value of 0.002% (range, 0.0002-0.07%). Two samples were mRNA-positive, DNA-negative with BCR-ABL1IS values of 0.003 and 0.02% (Figure 2A). The remaining 44 samples had undetectable BCR-ABL1 by both methods. The higher degree of sensitivity using BCR-ABL1 DNA led to MRD being quantifiable for an additional 5-18 months (median 12 months) of follow up. Samples collected after 24 months were not analyzed, so in some patients the duration of quantifiable MRD may have been longer than this estimate.
Discussion
BCR-ABL1 molecular monitoring by RQ-PCR is relied upon to ensure that TKI-treated patients are on track to achieve an optimal response, to define the end points of clinical trials, and to determine criteria for a safe trial of cessation of TKI therapy after having sustained a deep molecular response.18–20 Molecular responses defined by RQ-PCR have been shown to be robust indicators of clin ical outcome, yet the biology of BCR-ABL1 molecular response is relatively complex. Key to this complexity is the composite nature of the response: a reduction in the ratio of BCR-ABL1 mRNA to a control gene could be due to a reduction in the proportion of CML cells in the sample, a reduction in the expression of BCR-ABL1, an increase in the expression of the control gene, or even a change in the relative stability of these mRNA transcripts. Since the number of copies of genomic BCR-ABL1 is directly proportional to the number of leukemic cells, we reasoned that measuring both BCR-ABL1 DNA and mRNA would lead to a better understanding of the main determinants of variation in molecular response.
During the first three months of treatment, the BCR-ABL1 DNA values were significantly higher than the corresponding BCR-ABL1IS values. After three months, the reduction in BCR-ABL1IS levels (2.05-log) was primarily due to depletion of CML cells (1.75-log), with only a small contribution from expression changes (0.3-log reduction; 2-fold decrease). A proportionally greater decline in expression than in cell number is likely due to the early depletion of higher expressing cells. From six months of treatment onwards, there was generally excellent agreement between the level of MRD measured by BCR-ABL1 DNA and by RQ-PCR, indicating that the decline in BCR-ABL1IS is closely paralleled by declining numbers of BCR-ABL1-positive cells, as has been predicted using mathematical models based on RQ-PCR data.21,22
Several studies dating back at least two decades have reported inferior treatment responses among CML patients with e13a2 BCR-ABL1 transcripts.17,23 Differences in molecularly-defined end points might simply reflect differing amplification efficiency in the BCR-ABL1 assay, especially in those systems that use a common forward primer in BCR e13, resulting in a 76 bp difference in amplicon length between the two transcripts.24 In BCR-ABL1 DNA PCR, every patient-specific assay will have differing properties due to varying amplicon size and nucleotide composition. These differences are determined by factors related to the precise intronic location of the breakpoints, and therefore independent of the transcript type (Online Supplementary Figure S3). We took advantage of this to compare the relative expression of e13a2 and e14a2 BCR-ABL1 transcripts by normalizing the BCR-ABL1IS value against BCR-ABL1 DNA. Patients expressing both e13a2 and e14a2 transcripts were excluded from this analysis; in those cases the genomic BCR breakpoint is after exon 14, so e14a2 is the dominant transcript with a fraction of e13a2 expressed due to alternative splicing.25 Despite the small number of patients with each transcript type, we were able to show a significant difference in expression per cell at multiple time points during treatment. These findings require independent confirmation in a larger cohort. When treatment decisions are made according to molecular landmark responses, this may lead to incorrect classification of some e13a2 patients as optimal responders, and could contribute to adverse outcomes. Intriguingly, we identified 3 e13a2 patients who at diagnosis had discordant low BCR-ABL1 mRNA values (<10%) despite having close to 100% BCR-ABL1I-positive cells by DNA PCR and metaphase karyotyping. All 3 of these patients experienced treatment failure or warning by ELN criteria. The significance of this finding is unclear, given the small number of patients in this subgroup. It is, however, consistent with the experimental observation that imatinib sensitivity was reduced in BCR-ABL1-trans- duced murine cells selected for low BCR-ABL1 expression.26
The median limit of detection of BCR-ABL1 DNA was MR5.2 versus MR4.6 for conventional RQ-PCR. This improvement in sensitivity led to around half of the samples with undetectable BCR-ABL1 mRNA having measurable MRD and extended the period of time in which there was detectable BCR-ABL1 by around a year. The median limit of detection for dPCR was MR5.2. These results are similar to those obtained by Alikian et al., who used dPCR for both BCR-ABL1 DNA and mRNA, and found higher sensitivity with the DNA-based assay.6 Whilst the comparison of PCR methods was not the aim of this study, we found that dPCR was more precise, especially at diagnosis, but the Fluidigm® system has the disadvantage that more than 80% of the input DNA is lost in the dead space of the microfluidic circuit.
More sensitive mRNA-based methods have also been developed,6,17,27 and comparisons using different technology may yield different results. Nevertheless, genomic DNA-based methods have the advantage of greater specificity since cross-contamination between samples from different patients cannot cause false-positive results when the assays are patient-specific. A previous study showed that some patients with undetectable BCR-ABL1 mRNA by RQ-PCR had MRD detected by dPCR, and that these patients had a lower probability of successful treatment-free remission (TFR) after imatinib discontinuation.27 In the ENESTfreedom study of discontinuation of first-line nilotinib, patients with MR4.5 on every measurement for 12 months prior to stopping nilotinib were more likely to maintain TFR at 12 months than patients with one or more results above the MR4.0 threshold.28 More sensitive PCR methods might, therefore, have clinical utility as a means of refining estimates of the probability of TFR.
Miminal residual disease measurement by genomic DNA PCR provides insights into the kinetics of molecular response that are not provided by conventional RQ-PCR. The strong correlation between RQ-PCR and DNA-based PCR in follow-up samples beyond three months indicates that the major determinant of RQ-PCR values is the number of circulating leukemic cells, rather than variable expression of BCR-ABL1.
Supplementary Material
Acknowledgments
The authors wish to thank the patients, investigators, study coordinators, and ALLG staff who provided the samples and clinical data for this study, and acknowledge the ALLG as the sponsor of the TIDEL-II clinical trial. Novartis Pharmaceuticals provided a research grant for this project and additional funding was obtained from the South Australian Health Services Charitable Gifts Board.
Footnotes
Check the online version for the most updated information on this article, online supplements, and information on authorship & disclosures: www.haematologica.org/content/103/12/2026
References
- 1.Hughes TP, Kaeda J, Branford S, et al. Frequency of major molecular responses to imatinib or interferon alfa plus cytarabine in newly diagnosed chronic myeloid leukemia. N Engl J Med. 2003;349(15):1423–1432. [DOI] [PubMed] [Google Scholar]
- 2.van der Velden VH, Boeckx N, Gonzalez M, et al. Differential stability of control gene and fusion gene transcripts over time may hamper accurate quantification of minimal residual disease--a study within the Europe Against Cancer Program. Leukemia. 2004;18(4):884–886. [DOI] [PubMed] [Google Scholar]
- 3.Hughes T, Deininger M, Hochhaus A, et al. Monitoring CML patients responding to treatment with tyrosine kinase inhibitors: review and recommendations for harmonizing current methodology for detecting BCR-ABL transcripts and kinase domain mutations and for expressing results. Blood. 2006;108(1):28–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Branford S, Fletcher L, Cross NC, et al. Desirable performance characteristics for BCR-ABL measurement on an international reporting scale to allow consistent interpretation of individual patient response and comparison of response rates between clinical trials. Blood. 2008;112(8):3330–3338. [DOI] [PubMed] [Google Scholar]
- 5.Ross DM, O’Hely M, Bartley PA, et al. Distribution of genomic breakpoints in chronic myeloid leukemia: analysis of 308 patients. Leukemia. 2013;27(10):2105–2107. [DOI] [PubMed] [Google Scholar]
- 6.Alikian M, Ellery P, Forbes M, et al. Next-Generation Sequencing-Assisted DNA-Based Digital PCR for a Personalized Approach to the Detection and Quantification of Residual Disease in Chronic Myeloid Leukemia Patients. J Mol Diagn. 2016;18(2):176–189. [DOI] [PubMed] [Google Scholar]
- 7.Linhartova J, Hovorkova L, Soverini S, et al. Characterization of 46 patient-specific BCR-ABL1 fusions and detection of SNPs upstream and downstream the breakpoints in chronic myeloid leukemia using next generation sequencing. Mol Cancer. 2015;14:89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ross DM, Branford S, Moore S, Hughes TP. Limited clinical value of regular bone marrow cytogenetic analysis in imatinib-treated chronic phase CML patients monitored by RQ-PCR for BCR-ABL. Leukemia. 2006;20(4):664–670. [DOI] [PubMed] [Google Scholar]
- 9.Yeung DT, Osborn MP, White DL, et al. TIDEL-II: first-line use of imatinib in CML with early switch to nilotinib for failure to achieve time-dependent molecular targets. Blood. 2015;125(6):915–923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Baccarani M, Deininger MW, Rosti G, et al. European LeukemiaNet recommendations for the management of chronic myeloid leukemia: 2013. Blood. 2013;122(6):872–884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Branford S, Hughes TP, Rudzki Z. Monitoring chronic myeloid leukaemia therapy by real-time quantitative PCR in blood is a reliable alternative to bone marrow cytogenetics. Br J Haematol. 1999;107(3):587–599. [DOI] [PubMed] [Google Scholar]
- 12.Score J, Calasanz MJ, Ottman O, et al. Analysis of genomic breakpoints in p190 and p210 BCR-ABL indicate distinct mechanisms of formation. Leukemia. 2010;24(10):1742–1750. [DOI] [PubMed] [Google Scholar]
- 13.Ross DM, Branford S, Seymour JF, et al. Patients with chronic myeloid leukemia who maintain a complete molecular response after stopping imatinib treatment have evidence of persistent leukemia by DNA PCR. Leukemia. 2010;24(10):1719–1724. [DOI] [PubMed] [Google Scholar]
- 14.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1(8476):307–310. [PubMed] [Google Scholar]
- 15.Hanfstein B, Muller MC, Hehlmann R, et al. Early molecular and cytogenetic response is predictive for long-term progression-free and overall survival in chronic myeloid leukemia (CML). Leukemia. 2012;26(9):2096–2102. [DOI] [PubMed] [Google Scholar]
- 16.Hughes TP, Saglio G, Kantarjian HM, et al. Early molecular response predicts outcomes in patients with chronic myeloid leukemia in chronic phase treated with frontline nilotinib or imatinib. Blood. 2014;123(9):1353–1360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Marum JE, Branford S. Current developments in molecular monitoring in chronic myeloid leukemia. Ther Adv Hematol. 2016;7(5):237–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hughes TP, Ross DM. Moving treatment-free remission into mainstream clinical practice in CML. Blood. 2016;128(1):17–23. [DOI] [PubMed] [Google Scholar]
- 19.Mahon FX, Etienne G. Deep molecular response in chronic myeloid leukemia: the new goal of therapy? Clin Cancer Res. 2014;20(2):310–322. [DOI] [PubMed] [Google Scholar]
- 20.Saussele S, Richter J, Hochhaus A, Mahon FX. The concept of treatment-free remission in chronic myeloid leukemia. Leukemia. 2016;30(8):1638–1647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Michor F, Hughes TP, Iwasa Y, et al. Dynamics of chronic myeloid leukaemia. Nature. 2005;435(7046):1267–1270. [DOI] [PubMed] [Google Scholar]
- 22.Roeder I, Horn M, Glauche I, Hochhaus A, Mueller MC, Loeffler M. Dynamic modeling of imatinib-treated chronic myeloid leukemia: functional insights and clinical implications. Nat Med. 2006;12(10):1181–1184. [DOI] [PubMed] [Google Scholar]
- 23.Jain P, Kantarjian H, Patel KP, et al. Impact of BCR-ABL transcript type on outcome in patients with chronic-phase CML treated with tyrosine kinase inhibitors. Blood. 2016;127(10):1269–1275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gabert J, Beillard E, van der Velden VH, et al. Standardization and quality control studies of ‘real-time’ quantitative reverse transcriptase polymerase chain reaction of fusion gene transcripts for residual disease detection in leukemia - a Europe Against Cancer program. Leukemia. 2003;17(12):2318–2357. [DOI] [PubMed] [Google Scholar]
- 25.Branford S, Hughes TP, Rudzki Z. Dual transcription of b2a2 and b3a2 BCR-ABL transcripts in chronic myeloid leukaemia is confined to patients with a linked polymorphism within the BCR gene. Br J Haematol. 2002;117(4):875–877. [DOI] [PubMed] [Google Scholar]
- 26.Kumari A, Brendel C, Hochhaus A, Neubauer A, Burchert A. Low BCR-ABL expression levels in hematopoietic precursor cells enable persistence of chronic myeloid leukemia under imatinib. Blood. 2012;119(2):530–539. [DOI] [PubMed] [Google Scholar]
- 27.Mori S, Vagge E, le Coutre P, et al. Age and dPCR can predict relapse in CML patients who discontinued imatinib: the ISAV study. Am J Hematol. 2015;90(10):910–914. [DOI] [PubMed] [Google Scholar]
- 28.Ross DM, Masszi T, Gomez Casares MT, et al. Durable treatment-free remission in patients with chronic myeloid leukemia in chronic phase following frontline nilotinib: 96-week update of the ENESTfreedom study. J Cancer Res Clin Oncol. 2018;144(5):945–954. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.