The congenital sideroblastic anemias (CSAs) share the common feature of pathological intramitochondrial iron deposits in erythroid precursors. Nearly two-thirds of CSA can be attributed to a mutation in a specific nuclear-encoded gene or to mitochondrial DNA deletions,1 each of which involves one of three distinct pathways: iron-sulfur cluster biogenesis, heme biosynthesis, or mitochondrial translation/respiration.2 The most common form of the latter group is Pearson-Marrow-Pancreas syndrome (PMPS), which is a multisystem disorder characterized by sideroblastic anemia, exocrine pancreas insufficiency, and failure to thrive along with other, protean pathologies including in the neuromuscular, hepatic and gastrointestinal systems.3 PMPS is due to heteroplasmy for diverse incompletely overlapping, large (~2–10 kb) deletions in the mitochondrial genome (MT-DNA).4 No one protein-coding MT-gene is uniformly deleted in PMPS, but in all cases, at least one mitochondrial transfer RNA (MT-tRNA) is deleted, suggesting that the underlying pathogenesis involves mitochondrial protein synthesis rather than the deficiency of a single mitochondrially encoded protein per se. Mitochondrial translational/respiratory insufficiency as a common mechanism underlying the pathogenesis of syndromic CSA is further supported by the association of pseudouridine synthase 1 (PUS1) and mitochondrial tyrosyl-tRNA synthase mutations in patients with mitochondrial myopathy with lactic acidosis and sideroblastic anemia (MLASA), which overlap clinically with PMPS.5,6 An “MLASA-plus” phenotype in one patient was recently attributed to a missense mutation (m.8969G>A, c.443G>A, p.Ser148Asn) in the mitochondrial gene MT-ATP6,7 which encodes the F0 domain of complex V, the ATP synthase of the oxidative phosphorylation (OXPHOS) system, marking the first time that a mutation in an individual OXPHOS component has been linked to the pathogenesis of CSA. Subsequently, a recurring mutation in the respiratory complex I protein, NDUFB11,8 was reported in patients with syndromic CSA. Here, we describe three syndromic CSA patients carrying the m.8969 MT-ATP6 variant, defining the clinical spectrum of ATP6-mutation associated sideroblastic anemias (ATP6-SA), and distinguishing it from MLASA.
We studied 102 probands with CSA in whom MT-DNA deletion screening and candidate gene sequencing and/or whole exome sequencing (~100X median depth, >95% exonic coverage at 20X) did not reveal a MT-DNA deletion or a mutation in a published CSA disease-associated gene. We identified three patients from three families with varying degrees of heteroplasmy for the m.8969G>A allele by Sanger sequencing and evaluated the extent of heteroplasmy by next generation sequencing (http://dx.doi.org/10.1101/222109) (Table 1). No other heteroplasmic MT-ATP6 variants were identified. Investigation was performed with consent under a human subjects research protocol approved by Boston Children’s Hospital.
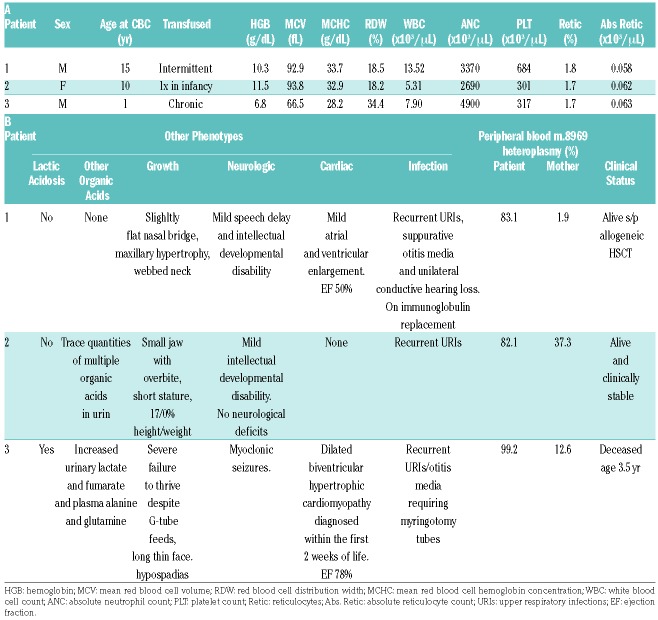
Table 1.
Hematological phenotype (A) and other phenotypes and genotypes (B) of m.8969G>A patients with congenital sideroblastic anemia.
Patient 1, a Caucasian male, was diagnosed with anemia in utero and underwent multiple transfusions starting at 20 weeks of gestation. After birth, his clinical course was complicated by jaundice requiring phototherapy and exchange transfusion, and persistent anemia. There was a maternal family history of hereditary xerocytosis (HX) due to a PIEZO1 mutation (c.7479_7484dup); the patient also carried this variant.9 As his phenotype was incompletely compatible with HX, he underwent a bone marrow aspiration, which was diagnostic of sideroblastic anemia. His blood lactic acid was normal and urine organic acids were unremarkable. He received intermittent transfusions and his clinical course was complicated by cardiomegaly and hepatic iron overload. He suffered from recurrent viral illnesses and acute suppurative otitis media with perforation, so severe that he was referred to immunology, and given subcutaneous immunoglobulin injections. Other than a mild cognitive developmental delay, no other neurological symptoms were present. He has a unilateral webbed neck and a flat nasal bridge with maxillary hypertrophy. Because of a persistent normocytic sideroblastic anemia and concern for a primary immunodeficiency, at age 14 years he underwent a matched unrelated donor peripheral blood stem cell transplant complicated by drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome, Epstein-Barr virus reactivation, and chronic graft-versus-host disease of the skin. Subsequently, 11/2 years following transplantation, a retrospective analysis of banked pre-transplant peripheral blood DNA showed 81.3%, 1.9%, 0.1%, and 0.1% m.8969G>A heteroplasmy in the patient, his mother, his father, and clinically unaffected male sibling, respectively.
Patient 2, a Caucasian Hispanic female, was small for gestation and required a transfusion several weeks after birth. Her anemia was initially microcytic. A bone marrow aspiration at age 2 months revealed ring sideroblasts. Her clinical course has been complicated by growth failure and persistent mild normocytic anemia associated with marrow ring sideroblasts. She has dysmorphic facies, including maxillary hypertrophy, a small jaw and a beaked nose. Other than mild intellectual disability, she has no neurological deficits. Urine organic acid analysis at age 10 years was remarkable for trace quantities of lactic, pyruvic, ethylmalonic and fumaric acids. MT-DNA analysis showed 82.1%, 37.3%, 0.2%, 0.0%, and 0.1% heteroplasmy for m.8969G>A in the patient, her mother, her father, and two full siblings, respectively. The mother is asymptomatic, non-dysmorphic, and has a normal CBC.
Patient 3, a male born of a Caucasian mother and African American father, presented with facial dysmorphism and failure to thrive soon after birth. An arterial blood gas analysis showed metabolic acidosis, with an elevated lactic acid level (8.9 mmol/L). Lactic and fumaric acid levels were also increased in the urine, and alanine and glutamine levels were increased in the plasma. There was marked cardiomegaly on chest X-ray and biventricular dilated hypertrophic cardiomyopathy by echocardiography. Neurological dysfunction, including hypotonia, myotonic seizures, gross motor and developmental delay, and visual and auditory deficits were also evident. A muscle biopsy to evaluate for a mitochondrial cytopathy was unrevealing. Microcytic anemia became evident by 2 weeks of life. Bone marrow examination disclosed sideroblastic anemia. He was trialed with erythropoietin and pyridoxine with no response, and was subsequently maintained on chronic transfusions in combination with iron chelation therapy. His clinical status was also complicated by recurrent upper respiratory infections and acute otitis media requiring myringotomy. He expired from aspiration pneumonia at age 3½ years. More than a decade after his death, he was found to be 99.2% heteroplasmic for the m.8969G>A mutation in peripheral blood; the patient’s asymptomatic mother’s peripheral blood DNA was 12.6% heteroplasmic.
In addition to the patient with “MLASA-plus” the m.8969G>A mutation in MT-ATP6 has been reported previously,10–12 but was not associated with CSA, despite a relatively high mutation burden in the peripheral blood of most of the other patients. The “MLASA-plus” index case, described Burrage et al., was a child with a complex multisystem disorder including failure to thrive, developmental delay, mitochondrial myopathy, lactic acidosis, sideroblastic anemia, a cardiac conduction defect, sensorineural hearing loss, epilepsy, agenesis of the corpus callosum, and stroke-like episodes.7 This patient was 96%, 85%, and 88% heteroplasmic for m.8969G>A in leukocytes, fibroblasts, and muscle, respectively. Importantly, they demonstrated a specific mitochondrial complex V (ATP synthase) defect in primary patient cells. Isohanni et al. reported a pair of siblings with failure to thrive, neuro-cognitive delays and elevated cerebrospinal fluid lactate levels.10 The more severely affected sibling, who was ~95% heteroplasmic in fibroblasts and skeletal muscle, required a single transfusion for neonatal anemia and had organic aciduria and an ATP synthesis defect in skeletal muscle. The less severely affected sibling was 79% heteroplasmic in blood. Wen et al. presented a female with neuro-motor deficits and IgA nephropathy with an m.8969G>A mutation heteroplasmy of 61% in peripheral blood, 79% in urine, and 89% in renal tissue; a blood phenotype was not described.11 Sallevelt et al. briefly mentioned a patient who died at age 7½ months with 95% m.8969G>A heteroplasmy in blood, fibroblasts and skeletal muscle, but did not comment on the infant’s phenotype.12 Overall, these combined data would suggest that an allele burden of at least 80% in peripheral blood leukocytes is required to manifest an overt CSA phenotype. Alternatively, as is true of other diseases attributable to mutations in the mitochondrial genome, the phenotype may be influenced by coinheritance of other variants, including those in nuclear-encoded mitochondrial proteins.13
Other mutations in MT-ATP6 lead to diverse phenotypes, including Leber’s Hereditary Optic Neuropathy (LHON), neuropathy, ataxia, and retinitis pigmentosa (NARP), maternally inherited Leigh syndrome (MILS), and mitochondrial spinocerebellar ataxia (MT-SCA). NARP and MILS patients most often carry variants in the active site, p.155-164, but some patients with MILS have C-terminal variants, and other individuals with NARP may have mutations throughout the gene, similar to patients with LHON.14 Other phenotypes, such as MT-SCA are uniquely associated with specific variants (i.e., m.9035T>C); this also appears to be true of ATP6-CSA. Nevertheless, as evidenced by a number of patients, CSA is not an inevitable complication of the m.8969G>A mutation. This suggests that the p.Ser148Asn variant has properties distinct from most other MT-ATP6 mutations. Indeed, a comprehensive study of a mutant orthologous to p.Ser148Asn in yeast indicates that the loss of complex V function is attributable to a unique mutation-specific hydrogen bond with p.Glu145.15 Consequently, p.Ser148Asn, may have neomorphic properties that alter mitochondrial metabolism in a manner permissive for the development of ring sideroblasts. Unfortunately, the fundamental biochemical pathogenesis of altered metabolism and the ontogeny of ring sideroblasts in this, and all, sideroblastic anemias is obscure.
While the initial reported case of CSA due to m.8969G>A heteroplasmy had a severe, MLASA-like phenotype,7 this is not true of all of the cases we report here; one of three patients did have a complex metabolic phenotype, whereas the other two had milder CSA with the only syndromic features being mild facial dysmorphism, mild neuro-cognitive dysfunction and/or organic aciduria. For this reason, rather than classify the disorder within the rubric of MLASA, it may be best viewed within the spectrum of other mitochondrial cytopathies, like PMPS, that demonstrate pleiotropy dependent upon tissue-specific heteroplasmy. Thus we propose the more encompassing name of ATP6-SA.
Supplementary Material
Acknowledgments
The authors thank the families described in this work for their participation. Susan Wong is gratefully acknowledged for administrative support of the research protocol. This work was supported by R01 DK087992 to M.D.F. S.B. was supported by the German National Academic Foundation and German Academic Exchange Service. S.S.B. was supported by the US Department of Veterans Affairs and the Oklahoma Center for Advancement of Science and Technology. J.F.T. E.J.W., and T.R. were employees of Claritas Genomics at the time this work was performed.
Footnotes
Information on authorship, contributions, and financial & other disclosures was provided by the authors and is available with the online version of this article at www.haematologica.org.
References
- 1.Bergmann AK, Campagna DR, McLoughlin EM, et al. Systematic molecular genetic analysis of congenital sideroblastic anemia: evidence for genetic heterogeneity and identification of novel mutations. Pediatr Blood Cancer. 2010;54(2):273–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bottomley SS, Fleming MD. Sideroblastic anemia: diagnosis and management. Hematol Oncol Clin North Am. 2014;28(4):653–670. [DOI] [PubMed] [Google Scholar]
- 3.Pearson HA, Lobel JS, Kocoshis SA, et al. A new syndrome of refractory sideroblastic anemia with vacuolization of marrow precursors and exocrine pancreatic dysfunction. J Pediatr. 1979;95(6):976–984. [DOI] [PubMed] [Google Scholar]
- 4.Rotig A, Cormier V, Blanche S, et al. Pearson’s marrow-pancreas syndrome. A multisystem mitochondrial disorder in infancy. J Clin Invest. 1990;86(5):1601–1608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zeharia A, Fischel-Ghodsian N, Casas K, et al. Mitochondrial myopathy, sideroblastic anemia, and lactic acidosis: an autosomal recessive syndrome in Persian Jews caused by a mutation in the PUS1 gene. J Child Neurol. 2005;20(5):449–452. [DOI] [PubMed] [Google Scholar]
- 6.Riley LG, Cooper S, Hickey P, et al. Mutation of the mitochondrial tyrosyl-tRNA synthetase gene, YARS2, causes myopathy, lactic acidosis, and sideroblastic anemia--MLASA syndrome. Am J Hum Genet. 2010;87(1):52–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Burrage LC, Tang S, Wang J, et al. Mitochondrial myopathy, lactic acidosis, and sideroblastic anemia (MLASA) plus associated with a novel de novo mutation (m.8969G>A) in the mitochondrial encoded ATP6 gene. Mol Genet Metab. 2014;113(3):207–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lichtenstein DA, Crispin AW, Sendamarai AK, et al. A recurring mutation in the respiratory complex 1 protein NDUFB11 is responsible for a novel form of X-linked sideroblastic anemia. Blood. 2016;128(15):1913–1917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Albuisson J, Murthy SE, Bandell M, et al. Dehydrated hereditary stomatocytosis linked to gain-of-function mutations in mechanically activated PIEZO1 ion channels. Nat Commun. 2013;4:1884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Isohanni P, Carroll CJ, Jackson CB, et al. Defective mitochondrial ATPase due to rare mtDNA m.8969G>A mutation-causing lactic acidosis, intellectual disability, and poor growth. Neurogenetics. 2018;19(1):49–53. [DOI] [PubMed] [Google Scholar]
- 11.Wen S, Niedzwiecka K, Zhao W, et al. Identification of G8969>A in mitochondrial ATP6 gene that severely compromises ATP synthase function in a patient with IgA nephropathy. Sci Rep. 2016;6:36313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sallevelt SC, de Die-Smulders CE, Hendrickx AT, et al. De novo mtDNA point mutations are common and have a low recurrence risk. J Med Genet. 2017;54(2):73–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jiang P, Jin X, Peng Y, et al. The exome sequencing identified the mutation in YARS2 encoding the mitochondrial tyrosyl-tRNA synthetase as a nuclear modifier for the phenotypic manifestation of Leber’s hereditary optic neuropathy-associated mitochondrial DNA mutation. Hum Mol Genet. 2016;25(3):584–596. [DOI] [PubMed] [Google Scholar]
- 14.Dautant A, Meier T, Hahn A, et al. ATP synthase diseases of mitochondrial genetic origin. Front Physiol. 2018;9:329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Skoczen N, Dautant A, Binko K, et al. Molecular basis of diseases caused by the mtDNA mutation m.8969G>A in the subunit a of ATP synthase. Biochim Biophys Acta. 2018;1859(8):602–611. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.