Abstract
Individuals with autism spectrum disorder (ASD) are generally less physically active than individuals without disability due to factors such as lack of motor coordination and inadequate transportation resources that can result in various barriers to participation. This affects their independence and may interfere with expectations (e.g., employment) during adulthood. It is essential to explore ways to teach physical activity so people with ASD can generalize skills in community settings. This study examined the effect of a multicomponent behavioral intervention that included (a) the Exercise Buddy application, (b) a system of least prompts, (c) an incremental increase of criteria, and (d) reinforcement to teach three adolescents with ASD functional movement exercises (e.g., squat). All participants increased their mastery of performing these exercises compared to baseline and generalized these skills across two community settings.
Keywords: Young adults with autism spectrum disorder, Physical activity, Technology, Inclusive community fitness
Regular physical activity (PA) is clearly beneficial as indicated by improved overall physical and psychological health, stamina, endurance, and physical fitness; however, 47%–51% of individuals with autism spectrum disorders (ASD) seldom meet the daily recommended guidelines for PA (Lang et al., 2010; Srinivasan, Pescatello, & Bhat, 2014), are more likely to be overweight and obese, and are less likely to voluntarily participate in PA (McCoy, Jakicic, & Gibbs, 2016). Although social and communication impairments are a significant concern for people with ASD, these individuals also display challenges related to the acquisition of PA skills and functional exercising due to factors such as delayed motor development, low levels of interest in daily living activities (Pan, Tsai, Chu, & Hsieh, 2011), and a lack of motivation to participate in PA. Disparities in weight between children with and without ASD have also recently been observed; 42.4% of children with ASD are overweight and 21.4% are considered obese, whereas only 26.1% of children without ASD are considered overweight and 12% are considered obese (Criado et al., 2017). Furthermore, adolescents with ASD are especially vulnerable to living sedentary lives (McCoy et al., 2016), which frequently persists into adulthood and can lead to related health concerns (Bodde & Seo, 2009).
PA has been linked to benefits in physical, social, and emotional functioning in adolescents with ASD. Several studies have shown that engagement in regular PA can decrease rates of stereotypic behavior, off-task behavior, and aggression and improve cognitive performance, appropriate motor behavior, academic responding, social/emotional functioning, independence, and quality of life (LaLonde, MacNeill, Eversole, Ragotzy, & Poling, 2014; Sarol & Çimen, 2015; Sorensen & Zarrett, 2014). Additionally, individuals who fail to meet the daily recommended guidelines for PA during adolescence commonly continue this trajectory into adulthood (Stodden et al., 2008). Identifying strategies to effectively teach exercise skills to adolescents with ASD may assist in preventing or reducing comorbid medical conditions (e.g., heart disease; Sarol & Çimen, 2015).
Although the benefits of regular PA are extensive, the research on successful interventions to increase PA skills in individuals with ASD is limited. It is vitally important to develop a greater understanding of the mechanisms that promote and maintain PA skills in individuals with ASD across the life span to help reduce symptomology of ASD and foster independence.
It is essential to identify PA interventions that teach transition-aged youths with ASD how to access and participate in PA in inclusive settings (e.g., YMCA). Specifically, interventions should identify how individuals with ASD can access and acquire skills related to health and fitness in order to ensure continuation into adulthood (Walker, 2015). However, these types of activities may be challenging for individuals with ASD due to a lack of structure and predictability, the social demands needed to create effective workout routines, and the knowledge needed to use exercise equipment and facilities appropriately (Menear & Neumeier, 2015).
The use of behavioral-based strategies that simultaneously address motivation and skill deficits holds promise for teaching PA skills to adolescents with ASD. Antecedent- and consequence-based interventions using known principles of applied behavior analysis (ABA) were previously found to promote PA in people with ASD (Sorensen & Zarrett, 2014). For example, antecedent strategies (i.e., goal setting) and consequence strategies (e.g., praise) increased steps walked by participants wearing a Fitbit (LaLonde et al., 2014). Todd and Reid (2006) found that self-monitoring, verbal prompting, and praise increased PA (e.g., jogging) in participants with ASD and intellectual disabilities, and self-efficacy increased as a result of a goal-setting intervention (Todd, Reid, & Butler-Kisber, 2010). Additionally, the use of reinforcement to address motivation along with baseline levels of PA skills should be considered prior to intervention. Reinforcing incremental increases in the level of PA may help reduce fatigue, soreness, and frustration when beginning an exercise program. Although the previous research is promising, it is limited in regard to promoting PA skills in people with ASD in inclusive community settings.
Technological interventions may be useful in facilitating the delivery of behavioral-based interventions related to PA. Exercise Buddy is a commercially available application that was developed to teach PA skills to individuals with ASD. The app includes several features known to benefit instruction for adolescents with ASD, including video models of adolescents with ASD, which may help increase attendance to the model (Bellini & Akullian, 2007); visual schedules (i.e., “first/then” and “start/finish” workout schedule options; Fittipaldi-Wert & Mowling, 2009); and audio feedback (e.g., the app tells the participant to “keep it up”). Additionally, the inclusion of premade video models may help reduce barriers for practitioners who lack the technical expertise needed to design video models of common exercises (e.g., squat; Rosenberg, Schwartz, & Davis, 2010).
The purpose of the current study was to explore if a multicomponent behavioral intervention (i.e., the Exercise Buddy application, a system of least prompts, an incremental increase of criteria, and reinforcement) impacted acquisition of PA skills of adolescents with ASD. Additionally, this study examined if the participants were able to successfully chain exercises together to create a workout circuit and generalize the skills across inclusive community settings. This study extends the existing research by exploring if a multicomponent treatment package based in behavior principles can be used to teach PA skills to adolescents and young adults with ASD. The research questions were the following: (a) Is the multicomponent treatment package effective for increasing PA skills in adolescents and young adults with ASD, and (b) to what extent will the PA skills learned generalize to a novel and inclusive community setting?
Method
Participants
This project received approval from an institutional review board prior to recruiting participants, and participants were recruited through a convenience sample. To be included in the study, participants needed to be between the ages of 14 and 22, have a diagnosis of ASD verified through medical or educational records, have a primary sedentary lifestyle or low level of PA based on anecdotal parent/guardian reports, and have an IQ of 55 or higher. Participants also completed a preassessment screening to ensure interest in the types of exercises they would be completing during the study and to determine their ability to attend to and imitate the video model. Individuals that were unable to function independently in the community due to health or behavioral concerns (e.g., risk to self or others) were excluded from the study. Initially, five participants were recruited; however, two withdrew from the study due to health concerns unrelated to the study. Ultimately, three participants met the inclusion criteria and completed the study (see Table 1 for demographic information). Pseudonyms were used to protect the confidentiality and autonomy of the participants.
Table 1.
Participants’ demographic information
| Participant/Gender | Age | Current Education Setting | Ethnicity | IQ | Secondary Disability |
|---|---|---|---|---|---|
| Tess/female | 20 | Aged out of school at 18 | Caucasian | 71a | None |
| Jim/male | 18 | Senior in high school | Caucasian | 85b | Language impairment |
| Jen/female | 21 | Aged out of public school and attended ABA center and day program | Caucasian | 71b | Anxiety disorder |
Tess
Tess was a 20-year-old female diagnosed with ASD. She aged out of public school at age 18 and lived at home with her aunt and was not employed. In addition to her ASD diagnosis, Tess was diagnosed with coloboma in her left eye and had open heart surgery when she was 3 weeks old. Prior to the study, Tess attended a workshop program for adults with disabilities; however, behavioral concerns precluded her attendance. Tess communicated verbally using simple sentences and would engage in conversations on her preferred topics (e.g., music, newborn babies). Tess was typically compliant with task demands but would occasionally hit herself in the face and throw her glasses off of her face to escape nonpreferred activities. At the start of the study, her aunt reported Tess did not currently engage in any structured exercise and did not have any goals related to PA. When asked about previous PA, Tess indicated she used to enjoy going on walks and swimming. Preferred activities for Tess included short walks and listening to music on YouTube. Going to the pool at the YMCA was used as reinforcement for completing Phase 2.
Jim
Jim was an 18-year-old male who was diagnosed with ASD. He lived at home with his parents and was a senior in high school. Jim was eligible for special education and primarily received services in a life skills curriculum; however, he was also in inclusive educational settings for 3 h per day. Previously, Jim had been a member of his school’s extracurricular Unified Track team, where he participated in track events alongside peers without disabilities. He participated in a weight-lifting class at school, but his father anecdotally reported that Jim had an overall low PA level at the start of the study and he did not have specific individualized education program goals related to PA. In general, Jim complied with task demands but would intermittently become distracted and have difficulty focusing. He communicated verbally, was able to imitate others, and followed simple multistep commands. During his free time, Jim preferred activities that included watching YouTube videos of the pop artist Lorde and truck (e.g., mud bogging) videos.
Jen
Jen was a 21-year-old female diagnosed with ASD. At the start of the study, Jen had aged out of public school and was attending an ABA center 3 days per week and a group recreational day program 1 day per week and received one-on-one recreational therapy 1 day per week. As part of her ABA and recreational therapy, Jen would go to the local YMCA at least two times per week and completed exercise circuits using various exercise machines (e.g., leg press) and walked on the treadmill. Despite these opportunities, her mother reported, she still had an overall low level of PA and preferred to engage in sedentary activities (e.g., computer games). Goals related to PA included increasing muscle strength, increasing walking speed, and improving overall stamina. Jen was typically compliant with task demands but would use bathroom requests to escape or delay demands. Jen was able communicate conversationally using short sentences, would follow multistep directions, and could imitate motor actions of others around her. Leisure activities for Jen included watching videos on YouTube and playing computer games.
Setting
The study took place over 4 months and across multiple settings for each participant. Phase 1 sessions were conducted in various teaching trial settings, Phase 2 was at a local YMCA (first community fitness site), and Phase 3 was in the participant’s preferred community fitness location (second community fitness site). Specifically, baseline and Phase 1 (teaching trial settings) sessions were conducted in the living rooms at participants’ homes, but Jen also completed sessions in the conference room at her ABA center and the sensory and break rooms at her day program. During all baseline and Phase 1 sessions, the exercise mat and dumbbells were laid out for participants at the start of each session. During Phase 2, exercise mats and dumbbells available at the YMCA were used. Phase 3 settings were selected by parents/guardians based on interest in potentially obtaining memberships at facilities, cost, availability, and proximity. PA was evaluated in different settings to evaluate generalization of skills in novel settings.
Materials
Exercise Buddy App
An Apple iPad Mini (19.99 cm tall × 13.46 cm wide × 0.64 cm thick) was used in the study to access the commercially available app Exercise Buddy (http://www.exercisebuddy.com/). The Exercise Buddy app included an inventory of various exercises (e.g., yoga, strength training), and selected exercises could be set up based on time or repetitions (referred to as reps) in a start/finish or first/then workout schedule. During the study, the start/finish workout feature of the app was used, and participants created a workout for each exercise (e.g., squats) at the start of each session. The app also provided premade video models of adolescents with ASD completing the majority of exercises included in the app. The exercises in the app were organized into categories according to the type of exercise (e.g., under “Muscular Fitness,” there were 19 premade exercises, such as the squat, dumbbell lateral raise, and dumbbell push-up row).
Four exercises (Table 2) were selected as intervention targets. The exercises were chosen because they worked different muscle groups (i.e., core, legs, and shoulders/back) to avoid fatiguing certain muscle groups while teaching students how to perform different types of exercises, focused on functional movement training, required minimal equipment, could be counted in reps, and had a similar number of critical components (steps) in the video models in the Exercise Buddy app. The squat exercise video was 23 s and displayed an adolescent girl with ASD demonstrating the steps with a series of concurrent verbal instructions. The dumbbell push-up row video was also 23 s and displayed an adolescent boy with ASD demonstrating the steps. The dumbbell lateral raise video was 26 s and displayed the same adolescent boy with ASD performing the steps. The hip extension video was 34 s and displayed a second adolescent boy with ASD. In addition to the visual model, auditory prompts detailing the steps of the task analysis were included. Participants only had access to the videos when watching them during intervention sessions.
Table 2.
Exercise assignments by participant
| Exercise | Tess | Jim | Jen |
|---|---|---|---|
| Squat | X | X | X |
| Hip extension | X | X | X |
| Dumbbell lateral raise | X | ||
| Dumbbell push-up row | X |
Exercise Equipment
One pair of 0.91-kg handheld dumbbells were used in the study to perform the dumbbell lateral raise and dumbbell push-up row exercises. An exercise mat (1.827-m long) was provided for participants to use during the hip extension exercise and cooldown. During Phases 2 and 3, equipment (e.g., mat and dumbbells) available at the community fitness sites was used.
Design, Variables, and Data Collection
A concurrent multiple-probe design across participants was used to determine the effect of the multicomponent treatment package (i.e., Exercise Buddy app in conjunction with prompting and reinforcement) to teach the participants PA skills. This design allowed the researchers to determine if a functional relationship existed between the independent and dependent variables while controlling for carry-over effects (Kennedy, 2005).
The independent variable was the multicomponent treatment package. The package used the components of the Exercise Buddy app (e.g., video models). Prompts were delivered in the following order: verbal only, verbal and gestural, verbal and model, verbal and partial physical, and verbal and full physical. The number of repetitions participants initially completed were determined by baseline performance and were incrementally increased across the intervention. Individualized reinforcement was identified based on participants’ verbal requests prior to sessions (e.g., YouTube music videos). The dependent variable was the percentage of steps of each exercise performed correctly. Six discrete task analysis steps were identified for each of the exercises, and event recording was used to determine the number of steps of the task analyses that participants completed independently for each exercise or the type of prompt required during intervention phases (Table 3).
Table 3.
Steps of task analysis for exercises
| Squat | Hip extension | Dumbbell lateral raise | Dumbbell push-up row |
|---|---|---|---|
|
1. Place your feet shoulder width apart with toes pointed forward. 2. Keep good posture: stand up tall, with shoulders back, and draw your tummy in. 3. Extend your arms out in front of you. 4. Bend your knees down until your hips get slightly above knee level. 5. Keep your eyes forward, back flat, and hips back. 6. Stand up straight. |
1. Lay on the ground with your back on the mat. 2. Make sure your feet are shoulder width apart with toes pointed forward and feet flat on the ground. 3. Keep your knees bent. 4. Keep your arms out at your sides with your palms facing down. 5. Extend your hips and tummy up as high as you can. 6. Control on the way down to lower your hips back down to the mat. |
1. Pick up your dumbbells. 2. Keep your arms to your sides. 3. Extend your arms out. 4. Keep your arms to your sides. 5. Keep good posture and your eyes forward. 6. Control the dumbbells on the way down. |
1. Begin on your hands and knees. 2. Place your hands on the dumbbells. 3. Extend your legs straight. 4. Roll one arm with dumbbell up with elbow bent. 5. Place the dumbbell back on the ground. 6. Keep control of your hips to prevent rocking from side to side. |
All data were collected by the primary investigator and/or two trained research assistants. The primary investigator was a doctoral-level Board Certified Behavior Analyst and a faculty member in ABA with multiple years of experience developing and implementing behavioral interventions for people with disabilities. The research assistants included a 2nd-year doctoral student in school psychology and a 2nd-year speech language pathology student. Both research assistants were trained by the first author on all aspects of the intervention, piloted the treatment package with a different group of students prior to this study, and demonstrated mastery for delivering the intervention during training.
Procedures
Preassessment
Prior to baseline sessions, participants were assessed on their ability to attend to and imitate video models that displayed exercises in the Exercise Buddy app that were similar but not the same as the targeted exercises for the study (e.g., the bridge hold exercise was used as it was similar to the hip extension). Baseline probes were used to assess participants’ ability to complete selected targeted exercises. Any exercises performed at mastery criterion (i.e., 100% of the steps completed independently) or any that were excessively challenging (i.e., the participant was physically unable to perform the exercise as demonstrated in the video in the app) were excluded as targeted exercises.
Warm-Up
Prior to all sessions across phases, all participants completed a brief warm-up led by the researcher. The warm-up consisted of the researcher saying and modeling the activity. The warm-up consisted of reaching both arms overhead toward the ceiling, stretching both arms down toward one’s toes, and arm circles. The cooldown was conducted at the end and consisted of the participant lying down on his or her back, bending one knee, and reaching behind the other leg (above or below the knee) for a hamstring stretch and then switching legs. Participants would perform each movement/stretch for 5–10 s.
Baseline
During baseline, participants were asked to review pictures of the exercises that mirrored the videos from the Exercise Buddy app. After reviewing the pictures for 1 min, the participants were given the instructional cue “Show me how you do 10 reps of [targeted exercise],” depending on the targeted exercise for the session. Participants completed baseline sessions on the targeted exercises in teaching trial settings, and Jim and Tess completed one generalization probe at the YMCA. No videos or prompting were available, participants were only provided with the instructional cue, and an explanation of “reps” was not provided. The dependent variable was the number of steps accurately completed on a task analysis. The task analysis was based on the steps depicted in the app’s video (i.e., 10 reps with 6 steps per rep for a total of 60 possible steps). During all phases, the order of the targeted exercises was predetermined and randomly assigned and included no more than two consecutive sessions of the same exercise. Access to preferred activities (e.g., YouTube videos) and/or monetary reinforcement was given for task compliance throughout the study.
Phase 1: Intervention in Teaching Trial Settings
Following baseline, Phase 1 intervention was implemented in teaching trial settings easily accessible to the participants (e.g., living room at home). During Phase 1, participants viewed how to do each exercise on an iPad (i.e., watched the video model on the Exercise Buddy app complete the exercise). To avoid fatigue and muscle soreness, Phase 1 sessions were intentionally short in duration (i.e., 1–5 min) and participants initially only completed two reps of each exercise. Reps were incrementally increased by two until participants could complete 10 reps of each exercise. The exercise was initiated after participants viewed the video model of the exercise in the app and when the researcher gave the instructional cue “Show me how you do [n] reps of [targeted exercise],” depending on the number of reps per exercise. Mastery criterion was achieved when a participant independently completed 80% of the six steps of each rep of an individual exercise (i.e., squats, hip extension, dumbbell lateral raise, dumbbell push-up row) across three sessions (e.g., the participant completed 80% of the six steps of each of the two squat reps independently across three sessions). Once mastery was achieved, the criterion increased and participants then needed to complete two additional reps. This continued until participants completed 10 reps of each exercise at the mastery criterion. Participants did not begin working on the new rep criterion for an exercise until they reached the rep mastery criteria for all of their specific targeted exercises. For example, Jim worked on squats, hip extensions, and dumbbell lateral raises. When he reached mastery on four reps of squats, he would not begin working on six reps of squats until he also reached mastery criterion on four reps of the hip extension and dumbbell lateral raise exercises. If a participant did not complete a step independently, the system of least prompts was implemented and the most intrusive prompt required for each step of each rep was recorded. As the criteria increased, participants were verbally instructed on how to manipulate the app to set the number of reps in the start/finish setting in the workout to the new value (e.g., change the reps from two to four). Once a participant independently completed 80% of the steps for each of the 10 reps of all three exercises across three sessions, the participant moved to Phase 2.
Phase 2: Generalization to the YMCA
During this phase, participants completed exercises at mastery criteria (i.e., the termination criteria for Phase 1: 10 reps) in a YMCA setting. The same procedures from Phase 1 were used during Phase 2, and sessions took approximately 5 min. Once participants reached mastery criteria at the YMCA, they entered Phase 3.
Phase 3: Generalization to Community Fitness Sites
Generalization data were collected 1–4 weeks following the completion of Phase 2 data collection and were collected at a new community site (i.e., not a YMCA) that was preferred by the participant and his or her family due to personal interest and/or proximity. Tess selected a personal training facility close to her home, Jim selected a community fitness center close to his home that he and his family were interested in getting a membership at, and Jen completed Phase 3 sessions in the community fitness center located in the hotel she was residing at. None of the participants had previous experience working out in the Phase 3 settings prior to the study.
During Phase 3, participants learned to use the Exercise Buddy app to chain their targeted exercises together to create a workout schedule using verbal prompting. After participants used the app to create their workout schedules, their ability to perform the workout schedule (i.e., behavioral chain of the exercises) in the community setting was assessed. Procedures used in Phase 3 were similar to Phases 1 and 2 (e.g., participants set the start/finish workout setting in the Exercise Buddy app for 10 reps for their targeted exercises, checked off reps as they completed them, and received reinforcement); however, there were two notable differences. First, participants were not required to watch the video model and chose to do so or not. Second, because participants completed multiple exercises per session, they chose the order of the targeted exercises in the workout schedule. Phase 3 sessions took approximately 15–20 min. Mastery criteria were set at correctly completing 80% of the total steps of the 10 reps of the targeted exercises across three sessions. The level of prompting to complete any steps of each of the reps of each of the exercises was recorded.
Social Validity Questionnaire
Twice during this investigation (i.e., prior to baseline and after the generalization phase), participants and their caregivers were interviewed to determine the social validity of using the intervention to address PA behavior (Table 4). Participants and parents/guardians were interviewed individually and responded to questions created for the study. Responses from parents/guardians were recorded using paper and pencil, and any personally identifying participant information was omitted to maintain confidentiality.
Table 4.
Social validity questionnaires
| Preintervention participant | Postintervention participant | Preintervention parent/guardian | Postintervention parent/guardian |
|---|---|---|---|
|
1. Do you think it is important to exercise and learn new PA skills? Why? 2. Do you think you will like exercising and learning new PA skills? Why or why not? 3. What do you think about using an iPad and the Exercise Buddy app to help you learn PA? 4. How do you think the Exercise Buddy app might help you to learn new exercises? 5. Do you struggle with anything when exercising? |
1. Did you like watching the videos on the Exercise Buddy app to learn new PA skills? 2. Did you feel more capable with your ability to perform the PA skills you learned? 3. Did using the Exercise Buddy app help you to learn these skills? a. If it did, how do you think it helped? b. If it did not, why do you think it did not? 4. Do you think you will use these new PA skills in the future? 5. Would you want your parent/guardian to let you keep using this app? 6. Would you like to have other opportunities to continue to use this app (e.g., at the YMCA)? 7. Did you feel comfortable using the Exercise Buddy app? 8. Was there anything you did not like about using it? 9. Do you think other people would like to use the app to learn new PA skills? |
1. Do you think your child will like using the Exercise Buddy app to learn new PA skills? 2. Do you think watching videos of the exercises will assist your child in learning the skills? 3. What do you think the effects of having your child use the app in the community will be? 4. What are your concerns about having your child use the Exercise Buddy app to learn new PA skills? 5.What benefits do you foresee in having your child use the Exercise Buddy app? 6. Do you think you might want to continue to allow your child to use the app in the future to learn additional skills? |
Likert Scale Questions: 5 = strongly agree, 4 = agree, 3 = neutral, 2 = disagree, 1 = strongly disagree 1. Commercially available apps with video can be an effective tool for teaching PA skills to young adults with ASD. 2. The app Exercise Buddy (with video modeling) costs US$29.99 and I would choose to pay this to have my child use the program. 3. Commercially available apps such as Exercise Buddy can help my child facilitate generalization of PA skills to inclusive community settings. 4. Commercially available apps such as Exercise Buddy can help my child increase his/her ability to know how to exercise independently in inclusive community settings. Open-Ended Questions 1. What did you think about having your child use video modeling through the app to learn new PA skills? 2. Do you think the video modeling instruction was effective in teaching the skills to your child? 3. Do you think your child is more confident in his/her PA skills now? 4. Do you think it was better, worse, or equivalent to traditional methods of teaching new PA skills (i.e., without video modeling or prompting)? 5. What did you like most and least about having your child participate in this study? 6. Would you have your child use the Exercise Buddy app in the future? 7. Have you thought of any other ways you may want to use the Exercise Buddy app in the future? 8. Do you think the use of the Exercise Buddy app helped facilitate new skills in inclusive community settings? 9. Was there anything you did not like about having your child use the app? 10. Do you plan for your child to continue to participate in PA/exercise after the study? In what ways? |
Initially, all three participants indicated they wanted to be healthier and believed that leaning how to exercise is an important skill. Jim mentioned that he wanted to prevent heart disease and reduce joint pain, and Jen indicated she wanted to lose weight. At the end of the study, all of the participants indicated they liked using the app to learn new exercises. Jim and Tess mentioned that they liked having the videos available in case they forgot what to do and Jen indicated that she felt healthier after learning how to exercise using the app.
Results from the initial questionnaire indicated that all parents/guardians believed that the videos in the app would help their children learn how to perform PA skills and assist them in improving their health and overall activity level. Two of the parents indicated they thought the videos would be beneficial because they provided visual aids and assisted in maintaining focus. Responses on the postintervention questionnaire indicated that parents/guardians believed the intervention increased their child’s ability to exercise in various settings. The parents/guardians reported that components of the app (e.g., use of visuals) and instruction by the researcher (e.g., prompting) were important for the intervention. The parents/guardians also appreciated that the intervention provided systematic instruction on how to exercise, focused on increasing independence, and incrementally increased the required number of reps, which eased response effort and assisted in skill acquisition. All parents/guardians reported that they planned to have their child continue to exercise after the study. Specifically, two parents/guardians indicated they were looking into gym memberships, and one parent purchased the app and planned to use it at the YMCA.
Interobserver Agreement (IOA) and Treatment Integrity
IOA data were collected independently and simultaneously by a second trained observer and the primary investigator. Agreement was determined when both observers recorded a step of a rep independently or recorded the same type of prompt used. IOA was calculated by dividing the number of agreements by the number of agreements plus disagreements and multiplying by 100. IOA data were collected for 33%–45% of sessions across all phases for all participants. IOA ranged from 93% to 100% across sessions for the three participants. Average agreement was 98.1% across all phases for Tess, 93% for Jim, and 96% for Jen.
Treatment fidelity was assessed during 25%–40% of baseline and intervention sessions. A checklist that indicated the procedures for each phase was developed to ensure appropriate steps were followed (e.g., “Participant views video for exercise based on schedule,” “Researcher tells participant, ‘Show me how you do n reps of [specific exercise for that session based on current criteria for the exercise: squat, hip extension, dumbbell lateral raise, or dumbbell push-up row].’”). Using the checklist, a second trained observer noted whether each step was followed. Treatment fidelity data were collected during the same sessions as IOA identified previously, and treatment fidelity was 100% for all three participants.
Results
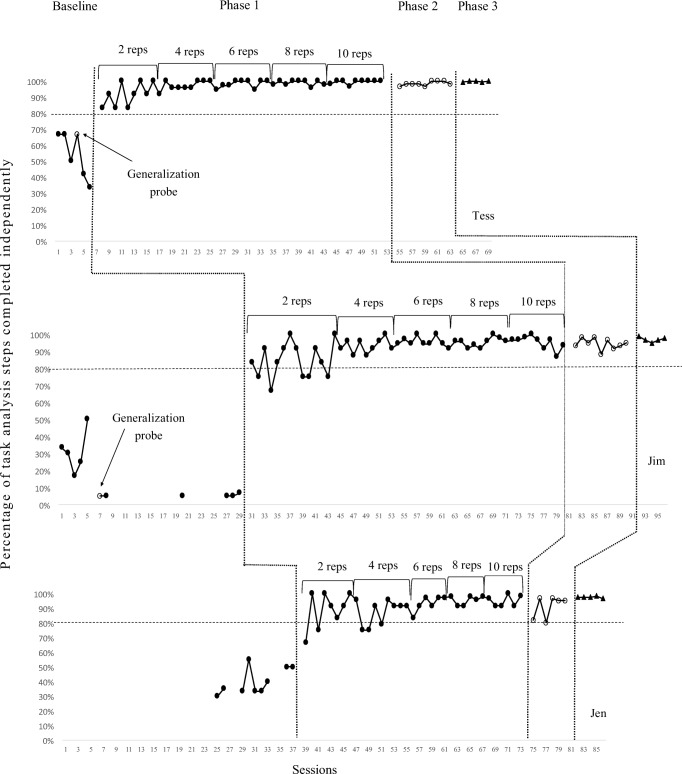
Results indicate an increase in participants’ ability to perform PA skills independently across phases. All of the participants showed an increase in independence between baseline and intervention phases, and improvements were maintained during the generalization phases. Figure 1 illustrates the percentage of steps completed independently when using the Exercise Buddy app during each phase of the study.
Fig. 1.
Percentage of steps of each rep completed independently during baseline, Phase 1 (teaching trial settings), Phase 2 (YMCA), and Phase 3 (preferred community fitness sites)
Tess
Based on the preassessments, Tess displayed mastery of the dumbbell lateral raise, and therefore her targeted exercises were identified as the squat, hip extension, and dumbbell push-up row. Initially, Tess displayed an average of 54.2% of the steps of these exercises independently during baseline. Visual analysis of the data indicates variability during baseline; however, a decreasing trend was reached after six sessions. Further visual analysis of the data indicates that once Phase 1 intervention began, Tess’s performance immediately increased and stability improved. Tess met mastery criterion during each session and the mastery criterion was reached for the three targeted exercises in 45 sessions. The mean number of steps of reps completed independently was 97.1%. During Phase 2, the mean number of steps of reps completed independently was 98.5%. She also met mastery criterion during each session and completed Phase 2 in nine sessions. Last, during Phase 3, Tess completed 99.8% of the steps of the reps for the three exercises chained together independently and met mastery criteria across all five sessions. Results indicated the skills acquired during Phase 1 generalized across both community settings in Phases 2 and 3.
Jim
Based on preassessment results, it was determined Jim would target three exercises: squats, hip extensions, and dumbbell lateral raises. Visual analysis of baseline data reveals initial variability with greater stability during the last six sessions, and Jim completed 16.9% of the steps of the 10 reps independently. During Phase 1 intervention, Jim was able to independently perform 91.9% of the steps of the reps independently. Phase 1 for Jim consisted of 50 sessions. When working on completing two reps, there were five sessions (i.e., Sessions 32, 39, 40, and 43 when working on the squat and Session 34 when working on the dumbbell lateral raise) that Jim did not meet mastery criteria. After mastering two reps for the three exercises, he then met mastery criteria during all of the remaining sessions of Phase 1 and his data show less variability. During Phase 2, Jim completed an average of 94.4% of the steps of the reps independently and he met mastery criteria during each session. Last, during Phase 3, Jim was able to independently complete an average of 97.0% of the steps and met mastery criteria during all five sessions. Results demonstrate the skills were generalized across the community settings.
Jen
Preassessment results indicated that Jen displayed mastery of the dumbbell lateral raise and excessive challenge with the dumbbell push-up row (i.e., she was not able to hold the plank position); therefore, only two targeted exercises were identified for her (i.e., squat and hip extension). Visual analysis of the data indicates that during baseline Jen was able to complete an average of 40.0% of the steps of the reps independently and stability was reached after nine sessions. During Phase 1, accuracy increased and she was able to complete an average of 91.4% of the steps of the reps independently. Initially, there was high variability in Phase 1; however, her ability to perform the reps more independently became more stable halfway through the phase, around Session 58. Jen completed Phase 1 in 35 sessions, and there were five sessions (Sessions 39, 41, 48, 49, and 51) where she did not meet mastery criteria when working on the squat. After progressing to Phase 2, Jen completed all sessions at mastery criteria with an average of 90.8% of the steps of the reps completed independently. During Phase 3, Jen’s performance increased and became more stable. She met mastery criteria in all sessions with an average of 97.5% of the steps of the reps completed independently. Results indicate the intervention was effective in helping Jen learn to complete and generalize the exercises.
Discussion
The purpose of the study was to explore the effectiveness of using a multicomponent, behaviorally based intervention package to facilitate PA skills in inclusive community settings for people with ASD. The results of the study demonstrate a functional relationship between the treatment package and the participants’ independence in performing the PA skills. All three participants’ levels of independence also remained stable when probed to complete the exercises in community settings. These results support previous research indicating that interventions using behavioral principles delivered through a technological device (e.g., an app on an iPad) can be effective in teaching students with ASD socially valid skills (King, Thomeczek, Voreis, & Scott, 2014) and expand this research to PA interventions.
The treatment package included components that provided antecedent instruction through the app (i.e., video model, visual schedule, incremental increase of reps), immediate feedback on errors (i.e., prompting by the researcher), and reinforcement to address motivational deficits (i.e., delivered contingently upon completing sessions). Given the use of the treatment package, the individual impact of each component of the intervention on PA skills cannot be determined. The participants indicated they enjoyed using the Exercise Buddy app to learn how to exercise, and by Phase 3, all participants learned to manipulate the app to design a workout schedule and maintained high levels of independence when exercising at their preferred community fitness sites. It appeared that the instruction provided by the video models in the app contributed to teaching the participants the skills; however, additional prompting by the researchers was required to assist participants in meeting mastery criteria. The most intrusive prompt needed to assist participants in learning the exercises was a partial physical prompt; however, verbal prompts were primarily all that was required during Phase 3.
Implications for Practice
Strategies to promote PA skills in young adults with ASD are greatly needed given the concerns with obesity and lack of PA (McCoy et al., 2016). It is also critical that adolescents with ASD have access to meaningful activities alongside peers without disabilities in inclusive settings outside of school (Platos & Wojaczek, 2017). Previous researchers demonstrated that visual cues (e.g., pictures) were effective in teaching PA skills; however, this research did not focus on generalizing skills to community sites (Menear & Neumeier, 2015). The results of this study provide initial support of a treatment package that helped facilitate increased independence of PA skills in community settings.
Access to the community is particularly important for young adults with ASD who exit the K–12 school system and no longer receive structured educational programming or community-based instruction. PA interventions for people with ASD need to focus on removing barriers to PA while simultaneously promoting meaningful PA across the life span. Identification of salient establishing operations (e.g., preferred workout locations) are critical given the impact these have on the reinforcing value of PA and the motivation to continue to exercise (Todd & Reid, 2006). This study provided an initial exploration by incorporating various settings (e.g., home, YMCA, other community fitness sites) that adults may choose to exercise in, as well as exposing participants to options for beginning an exercise program (e.g., use of the Exercise Buddy app, incrementally increase reps). It is important for secondary special education teachers, behavior analysts, adult service providers, parents/guardians, and others who are concerned about the activity levels of young adults with ASD to consider how to effectively ensure exercising becomes a lifelong activity. Through the various sites embedded within the study, the parents/guardians and participants increased their awareness of the fitness facilities and options available to them.
The primary focus of this study was to explore the use of the treatment package to monitor progress toward PA goals; however, during Phase 3, participants chose whether or not they wanted to watch the video models and could pick the order they completed their targeted exercises as way to facilitate self-determination. Tess always chose to watch all the videos for all three of her targeted exercises during Phase 3. However, Jen and Jim varied; sometimes they chose to watch the videos and other times they did not. For example, during Session 86, Jen chose to watch the video for the squat but not the hip extension. These variations might indicate that, at times, participants were confident in their ability to perform certain exercises without the video model. Additionally, during Phase 3, the participants indicated they enjoyed being able to decide the order they would complete exercises and typically created workouts where the order of the exercises differed.
Limitations and Future Directions
There are a number of limitations in this study that are important to note. To begin, as part of the treatment package, the participants incrementally increased the reps during the initial phase and received reinforcement and prompting across all phases. An informal preference assessment (i.e., participants were asked what they wanted to do after working out) was used to identify reinforcement for participants, and following sessions, participants received intermittent monetary reinforcement (a total of $40 distributed across sessions) and access to preferred activities (e.g., watching a YouTube video). The study did not explore if participants would maintain the skills outside of the treatment package. During Phase 3, the option of watching the video model was included as a way to begin fading one component of the intervention; however, it would be of interest for future research to more systematically explore fading of components to determine which are critical.
As a result of the intervention, participants incrementally increased the intensity of their workout by increasing the reps and the number of exercises they performed; however, exploring the features of the app alone, without the additional treatment components (e.g., prompting, reinforcement), would be of interest for future researchers seeking to increase PA skills. The app component capitalized on behavioral principles given that it permitted participants to set the number of reps for each workout to a specific number that could be incrementally increased, allowed participants to create a workout that only consisted of one exercise (e.g., squat) during Phase 1 and multiple exercises during Phase 3, contained video models that included both visual and audio instructions, provided verbal praise for completion of each exercise and the entire workout when multiple exercises where used, enabled participants to check off reps as they completed them, and was delivered on an easily portable and socially acceptable device (i.e., iPad). It would also be of interest for future research to explore the motivational deficits of exercise for people with ASD and strategies to teach people with ASD ways to facilitate how exercise can serve as a primary reinforcer in and of itself.
Another limitation is that this study only focused on a few targeted exercises (i.e., two or three exercises) for the participants, leaving out a number of other types of exercises that may have been of greater interest or more motivating to the participants. Furthermore, participants did not get to pick the types of exercises they worked on, and it could be they would have been more motivated to learn other types of exercises that were not included in the study. Future research that facilitates increased opportunities for self-determination in PA skills for young adults with ASD in inclusive community settings is needed. Self-determination in adolescents with disabilities has been correlated with greater community access in adulthood and more positive postschool outcomes (Shogren, Wehmeyer, Palmer, Rifenbark, & Little, 2015). Furthermore, self-determination was found to impact motivation in physical education classes at school in adolescent males with ASD (Pan et al., 2011). Self-determination was not systematically explored in this study; however, following Session 62 (Phase 3), Tess demonstrated an act of self-determination and requested to watch the video of the butterfly yoga exercise (an exercise not included as part of the study). She then performed the exercise while watching it and indicated she enjoyed doing the additional exercise even though it was not required. It would be of interest for future research to explore preference and choices during PA and the impact on motivation and acquisition within community fitness sites.
This study involved an investigation of one commercial app for one set of participants to teach specific exercises. The findings of this study should be considered preliminary, and future research should explore the ability of the app to teach other exercises, as well as investigate other apps or technological interventions. Further research should seek to replicate this methodology and results with other participants with ASD (e.g., other age cohorts). Additionally, during the intervention phases, the participants were required to set the number of reps for their exercises during sessions and put together their workout schedule in Phase 3; however, these data were not systematically recorded. Jim struggled the most with navigating the app, whereas Jen and Tess quickly learned how to use it to set up their reps in Phase 1 and workouts in Phase 3. Future research should explore participants’ ability to navigate the app in addition to completing the exercises. Last, the participants in this study generally responded well to the premade videos provided in the Exercise Buddy app; however, other individuals with more severe forms of ASD may benefit from custom-made videos that provide video prompts of exercises.
The focus of this study was on skill acquisition and independence of skills in community settings; therefore, another limitation is the lack of focus on physiological effects (e.g., heart rate), weight loss, or strength building. It would be of interest for future research to explore if a similar type of intervention can not only impact independence in skills but also assess the effectiveness of interventions on physical changes, weight loss, and/or other health-related measures.
Conclusions
In conclusion, this study supports previous research demonstrating the benefits of incorporating behaviorally based interventions to promote skill acquisition in people with ASD through an important examination of PA. The study provides preliminary evidence to support how a PA treatment package can apply behavioral principles and assist people with ASD in learning PA skills and generalize skills across inclusive community sites. The participants learned to create a workout schedule and perform it using the technology in their preferred community fitness sites. The use of the app on the iPad facilitated a socially acceptable way to get people with ASD to engage in PA; however, future research is needed to more thoroughly understand potential benefits of the various components of the treatment package.
Implications for Practice
Physical activity is a socially valid behavior that is critical to increasing access to health for people with autism spectrum disorders (ASD).
Instruction in community settings promotes generalization, access, and advocacy for people with ASD.
Behavioral interventions delivered through everyday technologies (i.e., iPad) are socially acceptable for people with ASD to use in inclusive community settings.
Exercise Buddy is a commercially available app that includes premade video models; this can help minimize the response effort of clinicians seeking to use these types of interventions with clients.
Funding
This study was funded by Ball State University’s Aspire Start-Up grant.
Compliance with Ethical Standards
Conflict of Interest
The authors declare they have no conflicts of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Footnotes
Laura Bassette, Department of Special Education, Ball State University; Jessica Kulwicki, Department of Educational Psychology, Ball State University; Shannon Titus Dieringer, Department of Special Education, Ball State University; Kimberly A. Zoder-Martell, Department of Special Education, Ball State University; Ryan Heneisen, Department of Speech Pathology and Audiology, Ball State University
References
- Bellini S, Akullian J. A meta-analysis of video modeling and video self-modeling interventions for children and adolescents with autism spectrum disorders. Exceptional Children. 2007;73:264–287. doi: 10.1177/001440290707300301. [DOI] [Google Scholar]
- Bodde A, Seo D. A review of social and environmental barriers to physical activity for adults with intellectual disabilities. Disability and Health Journal. 2009;2:57–66. doi: 10.1016/j.dhjo.2008.11.004. [DOI] [PubMed] [Google Scholar]
- Criado, K.K., Sharp, W.G., McCracken, C.E., De Vinck-Baroody, O., Dong, L., Aman, M.G., et al. (2017). Overweight and obese status in children with autism spectrum disorder and disruptive behavior. Autism, 22(4), 1–10. 10.1177/1362361316683888. [DOI] [PMC free article] [PubMed]
- Fittipaldi-Wert J, Mowling CM. Using visual supports for students with autism in physical education. Journal of Physical Education, Recreation and Dance. 2009;80:39–43. doi: 10.1080/07303084.2009.10598281. [DOI] [Google Scholar]
- Kennedy, C. H. (2005). Single-case designs for educational research. Boston: Pearson/Allyn and Bacon.
- King AM, Thomeczek M, Voreis G, Scott V. iPad® use in children and young adults with autism spectrum disorder: An observational study. Child Language Teaching and Therapy. 2014;30:159–173. doi: 10.1177/0265659013510922. [DOI] [Google Scholar]
- LaLonde KB, MacNeill BR, Eversole LW, Ragotzy SP, Poling A. Increasing physical activity in young adults with autism spectrum disorders. Research in Autism Spectrum Disorders. 2014;8:1679–1684. doi: 10.1016/j.rasd.2014.09.001. [DOI] [Google Scholar]
- Lang R, Koegel LK, Ashbaugh K, Regester A, Ence W, Smith W. Physical exercise and individuals with autism spectrum disorders: A systematic review. Research in Autism Spectrum Disorders. 2010;4:565–576. doi: 10.1016/j.rasd.2010.01.006. [DOI] [Google Scholar]
- McCoy SM, Jakicic JM, Gibbs BB. Comparison of obesity, physical activity, and sedentary behaviors between adolescents with autism spectrum disorders and without. Journal of Autism and Developmental Disorders. 2016;46:2317–2326. doi: 10.1007/s10803-016-2762-0. [DOI] [PubMed] [Google Scholar]
- Menear KS, Neumeier WH. Promoting physical activity for students with autism spectrum disorder: Barriers, benefits, and strategies for success. Journal of Physical Education, Recreation and Dance. 2015;86:43–48. doi: 10.1080/07303084.2014.998395. [DOI] [Google Scholar]
- Pan C, Tsai C, Chu C, Hsieh K. Physical activity and self-determined motivation of adolescents with and without autism spectrum disorders in inclusive physical education. Research in Autism Spectrum Disorders. 2011;5:733–741. doi: 10.1016/j.rasd.2010.08.007. [DOI] [Google Scholar]
- Platos M, Wojaczek K. Broadening the scope of peer-mediated intervention for individuals with autism spectrum disorders. Journal of Autism and Developmental Disorders. 2017;48:747–750. doi: 10.1007/s10803-017-3429-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roid, G. H. (2003). Stanford–Binet intelligence scales. Itasca: Riverside Publishing.
- Rosenberg NE, Schwartz IS, Davis CA. Evaluating the utility of commercial videotapes for teaching hand washing to children with autism. Education and Treatment of Children. 2010;33:443–455. doi: 10.1353/etc.0.0098. [DOI] [Google Scholar]
- Sarol H, Çimen Z. The effects of adapted recreational physical activity on the life quality of individuals with autism. Anthropologist. 2015;21:522–527. doi: 10.1080/09720073.2015.11891842. [DOI] [Google Scholar]
- Shogren KA, Wehmeyer ML, Palmer SB, Rifenbark GG, Little TD. Relationships between self-determination and postschool outcomes for youth with disabilities. Journal of Special Education. 2015;48:256–267. doi: 10.1177/0022466913489733. [DOI] [Google Scholar]
- Sorensen C, Zarrett N. Benefits of physical activity for adolescents with autism spectrum disorders: A comprehensive review. Review Journal of Autism and Developmental Disorders. 2014;1:344–353. doi: 10.1007/s40489-014-0027-4. [DOI] [Google Scholar]
- Srinivasan SM, Pescatello LS, Bhat AN. Current perspectives on physical activity and exercise recommendations for children and adolescents with autism spectrum disorders. Physical Therapy. 2014;94:1–16. doi: 10.2522/ptj.20130157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stodden, D. F., Goodway, J. D., Langendorfer, S. J., Roberton, M., A., Rudisill, M. E., Garcia, C., & Garcia, J. E. (2008). A developmental perspective on the role of motor skill competence in physical activity: An emergent relationship. Quest, 60, 290–306.
- Todd T, Reid G. Increasing physical activity in individuals with autism. Focus on Autism and Other Developmental Disabilities. 2006;21:167–176. doi: 10.1177/10883576060210030501. [DOI] [Google Scholar]
- Todd T, Reid G, Butler-Kisber L. Cycling for students with ASD: Self-regulation promotes sustained physical activity. Adapted Physical Activity Quarterly. 2010;27:226–241. doi: 10.1123/apaq.27.3.226. [DOI] [PubMed] [Google Scholar]
- Walker, B. (2015). Growing up on the spectrum: How high-functioning young adults with autism transition to independence (Unpublished honors thesis). University of Puget Sound, Tacoma.
- Wechsler, D. (2014). Wechsler adult intelligence scale (4th ed.). San Antonio: Psychological Corporation.