Abstract
A 65-year-old woman, with valvular heart disease, atrial fibrillation, and depression, presented to the emergency room due to dyspnea with shock state accompanied by agitation. An electrocardiogram showed ST segment elevation in leads II, III, aVF, I, aVL, and V4–6. An echocardiography revealed extensive akinesis in the apex, but hyperkinesis in the base, with apical ballooning appearance. An emergent coronary angiography showed no obstructive disease. The patient required intubation under mechanical ventilator, and an intra-aortic balloon pump to recover from shock state. She had been taking maprotiline, a tetracyclic antidepressant, and had added dextromethorphan, a cough suppressant, just before admission. The patient was diagnosed with takotsubo cardiomyopathy associated with serotonin syndrome due to serotonergic drug interactions. After discontinuation of these drugs and administration of serotonin antagonist under mechanical supportive care, she became hemodynamically stable. Apical ballooning was completely resolved 2 weeks later, and she was discharged well. We diagnosed serotonin syndrome manifesting as excessive serotonin toxicity that resulted in a hyperserotonergic and hyperadrenergic state, causing takotsubo cardiomyopathy. Here, we report a case of takotsubo cardiomyopathy associated with serotonin syndrome. This case suggests that serotonin syndrome should be recognized promptly and complications, including takotsubo cardiomyopathy, need to be treated appropriately.
<Learning objective: We must closely monitor serotonergic agents because serotonin syndrome can occur from a combination some serotonergic drugs, even when each is used at a therapeutic dose. Serotonin syndrome can lead to not only serotonergic but also hyperadrenergic state that may be a trigger of takotsubo cardiomyopathy. Serotonin syndrome should be diagnosed surely to ensure the prompt initiation of the treatment included discontinuation of the precipitating drugs because the disease occasionally progresses rapidly to fatal condition.>
Keywords: Takotsubo cardiomyopathy, Serotonin syndrome, Cardiogenic shock
Introduction
Takotsubo cardiomyopathy, or apical ballooning syndrome, is characterized by transient left ventricular (LV) dysfunction, commonly involving the apex and associated with emotional or physical stress, without any obstructive coronary artery disease. Common clinical presentations of this condition are chest pain and dyspnea mimicking acute myocardial infarction, but pulmonary edema and cardiogenic shock are infrequent [1]. Myocardial stunning mediated by catecholamine excess is the predominant theory explaining the disease mechanism [2]. Serotonin syndrome is a potentially life-threatening condition associated with excessive serotonergic activity in the nervous system caused by overdose with one serotonergic drug or the improper combination of these drugs. Classically, it is characterized by a clinical triad of mental status changes, autonomic instability, and neuromuscular hyperactivity [3]. Overdose with some antidepressants, such as a serotonin–norepinephrine reuptake inhibitor, leads to takotsubo cardiomyopathy independently of serotonin syndrome 4, 5, 6, 7. Only one case has been reported of serotonin syndrome due to overdose of combined antidepressants that induced takotsubo cardiomyopathy [8]. We report the case of a patient who presented with cardiogenic shock due to takotsubo cardiomyopathy associated with serotonin syndrome caused by drug interactions.
Case report
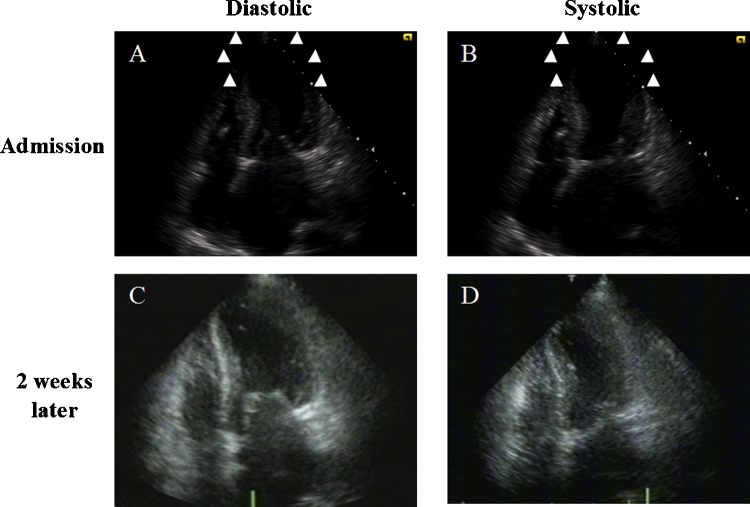
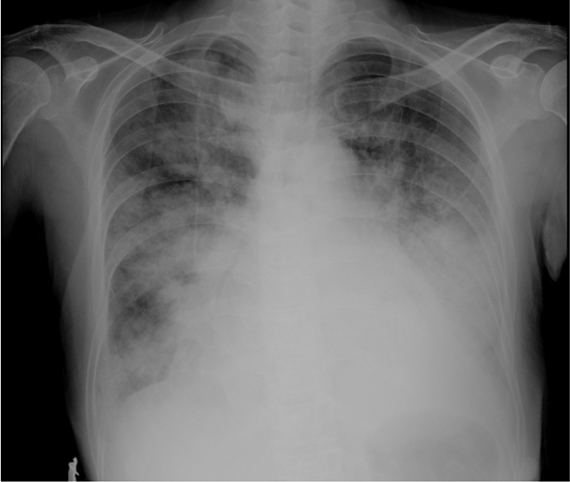
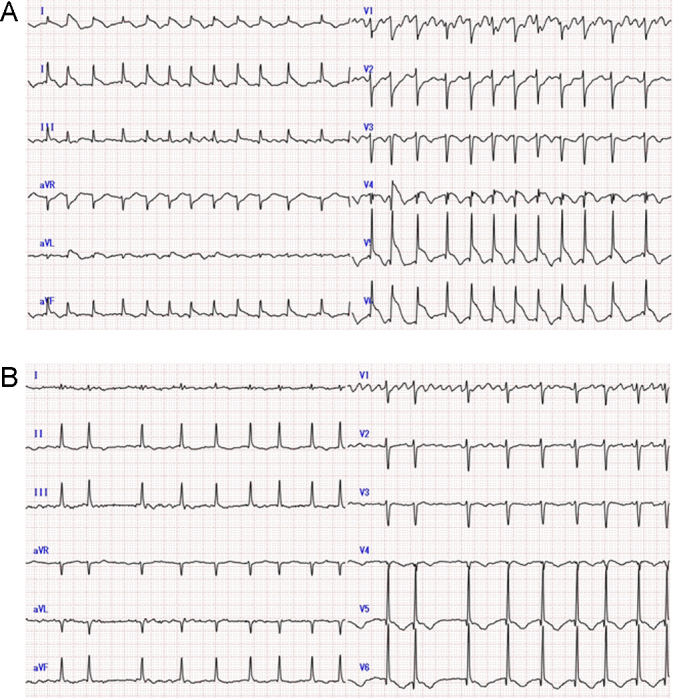
A 65-year-old female with history of depression, valvular heart disease (moderate mitral and aortic valve stenosis), and atrial fibrillation with normal LV function that had been well controlled with verapamil, bisoprolol, and warfarin, presented to our hospital. She had been diagnosed with depression 4 weeks before admission and started maprotiline at that time, gradually increasing from 10 mg to 30 mg once a day. She had noticed cough and fever 3 days prior to admission to our hospital. She went to a local clinic and was diagnosed with acute bronchitis. Amoxicillin and dextromethorphan were prescribed additionally at that time. However she was admitted to the hospital by ambulance because of severe dyspnea and hemosputum. On the patient's arrival, her blood pressure was found to be 83/44 mmHg; her heart rate, 166 beats/min; her oxygen saturation level, 91% on an oxygen mask with reservoir bag at 10 l per minute; her body temperature, 39.8 °C. A chest radiography showed severe pulmonary congestion and consolidation in both lower lobes (Fig. 1). An electrocardiogram showed ST segment elevation in leads II, III, aVF, I, aVL, and V4–6 (Fig. 2A). An echocardiography revealed extensive akinesis in the apex but hyperkinesis in the base, with an apical ballooning appearance (Fig. 3A). Blood tests revealed significant elevation of creatine kinase (CK) 2030 IU/l (normal range, 57–115 IU/l), but CK-MB fraction elevated 28 IU/l (normal range, 4–13 IU/l) slightly, furthermore white blood cell count 13,700/mm3, and C-reactive protein was 25.1 mg/dl. She required intubation under mechanical ventilation support and was started on intravenous catecholamine (dobutamine 8 μg/kg/min and noradrenaline 0.2 μg/kg/min). She underwent emergent coronary angiography to exclude acute coronary syndrome. Her coronary angiogram showed normal coronary arteries without any obstruction. Finally, she was diagnosed with takotsubo cardiomyopathy. For treatment, an intra-aortic balloon pump (IABP) was inserted to maintain her blood pressure. The next day, physical examination showed persistent hypotension, hyperthermia (41.7 °C), muscle rigidity in the extremities, and ocular clonus. As serotonin syndrome was suspected based on her medical history and clinical signs, midazolam was administered intravenously and cyproheptadine was administered via nasogastric tube. On the third day her fever was alleviated and she achieved hemodynamic stability. CK was still high at 607 IU/l with normalized CK-MB 10 IU/l. Electrocardiography showed negative T waves of the prior ST elevated leads (Fig. 2B). On the 7th day, IABP and catecholamine support were withdrawn. Two weeks later echocardiography showed complete resolution of wall-motion abnormalities with an estimated LV ejection fraction of 0.65 (Fig. 3C and D). She was discharged in good health on the 53rd day.
Fig. 1.
Chest radiography on admission shows congestive heart failure with marked cardiomegaly and consolidation in both lower lobes.
Fig. 2.
Electrocardiography (ECG) on and after admission. (A) ECG on admission shows ST segment elevation in leads II, III, aVF, I, aVL, and V4–6. (B) ST elevation resolved and inverted negative T wave in same leads on the third day.
Fig. 3.
Echocardiography on admission and 2 weeks later. Upper: On admission. Triangles indicate the areas of akinesis that appeared as apical ballooning. (A) End-diastolic phase; (B) end-systolic phase on admission. Lower: Two weeks after admission. Abnormalities of left ventricular motion completely resolved with ejection fraction of 0.64. (C) End-diastolic phase; (D) end-systolic phase.
Discussion
We present the case of a patient who suffered potentially fatal cardiogenic shock caused by takotsubo cardiomyopathy due to serotonin syndrome. Takotsubo cardiomyopathy, also known as stress-induced cardiomyopathy or broken-heart syndrome, is characterized by transient dysfunction of the LV apex, concomitant with hyperkinesis of the basal ventricle, with apical ballooning, but no coronary artery obstruction [1]. Several etiologies have been proposed for the condition, such as coronary spasm, sympathetic hyperactivity, microcirculatory failure, and excessive catecholamine-induced myocardial stun [2]. Although the prognosis of takotsubo cardiomyopathy is generally favorable, cardiogenic shock has been found to occur in 4.2% of such cases and in-hospital mortality is 1.1% [1].
Serotonin syndrome manifests as a clinical triad of mental-status changes, autonomic hyperactivity, and neuromuscular abnormalities due to excess serotonergic activity in the central and peripheral nervous system [3]. The present case was diagnosed using the Hunter Serotonin Toxicity Criteria, and the identification of mild muscle rigidity, ocular clonus, and agitation with hyperthermia [3]. Although there are no specific laboratory tests to confirm the diagnosis of the serotonin syndrome, laboratory abnormalities that develop in severe cases include an elevated CK, and inflammatory markers that corresponded with coexisting symptoms with hyperthermia, muscle rigidity, and agitation in this case. Patients with serotonin syndrome usually have vital-sign abnormalities, such as tachycardia, hypertension, and hyperthermia. However the present case presented with shock status due to poor cardiac function except hyperkinetic contraction of the basal ventricle. These findings were compatible with takotsubo cardiomyopathy. 123I-metaiodobenzylguanidine myocardial scintigraphy evaluates cardiac sympathetic nervous function, and the usefulness of imaging has been evaluated in takotsubo cardiomyopathy [9]. However we did not perform myocardial scintigraphy because of the instability of the patient's condition. In the case of cardiogenic shock associated with takotsubo cardiomyopathy, we must exclude LV outflow tract obstruction associated with hyperkinetic movement of sigmoid septum. This is because inotropes and IABP may amplify the intra-ventricular gradient. In the present case, no outflow obstruction was detected by echocardiography.
Patients with stress-induced cardiomyopathy frequently have evidence of exaggerated sympathetic activation, including high levels of plasma catecholamine, serotonin, and other neuronal metabolites [2]. Serotonin syndrome can lead to a hyperadrenergic state and the triggering of takotsubo cardiomyopathy in these cases. Maprotiline is known as a tetracyclic antidepressant with strong selective norepinephrine reuptake inhibitor effects but only weak effects on serotonin and dopamine reuptake. The patient in the present case had received dextromethorphan in addition to maprotiline. Dextromethorphan, a commonly used cough suppressant, is an opioid receptor agonist, N-methyl-d-aspartate (NMDA) glutamase receptor antagonist, and serotonin reuptake inhibitor. It is well-known that this drug can lead to serotonin syndrome [10]. In the present case, the combination of maprotiline and dextromethorphan might have caused serotonin syndrome [3]. The relationship between serotonin syndrome and takotsubo cardiomyopathy has not been clarified to date. Mehta et al. suggested in their case report that serotonin syndrome can lead to physiologic stress due to a hyperadrenergic state, and the hyperadrenergic state can lead to stress-induced cardiomyopathy [8]. Another possibility is that excessive serotonin levels directly overstimulate serotonin receptors in the heart [8]. Furthermore, antidepressant medications have been shown to influence plasma catecholamine levels. Overdose of these drugs or improper combinations of them have led to the development of takotsubo cardiomyopathy independently of serotonin syndrome 4, 5, 6, 7. Elevated serum catecholamine and serotonin levels have been extensively described in stress-induced cardiomyopathy [3].
The management of serotonin syndrome includes discontinuation of the precipitating drugs, provision of supportive care, and control of agitation, autonomic instability, and hyperthermia [3]. In the present case, discontinuation of antidepressants and administration of cyproheptadine, a serotonin antagonist, improved hyperthermia and stabilized hemodynamics on the day after admission. Benzodiazepine was useful in controlling excessive muscle activity. Although serotonin syndrome is a potentially life-threatening condition, more than 85% of clinicians are unaware of the diagnosis [3]. Furthermore, serotonin syndrome does not resolve spontaneously, as long as the precipitating agents continue to be administered. The condition occasionally progresses rapidly to death.
The present patient had received medical treatment for atrial fibrillation with moderate valvular disease for about a decade. Tachyarrhythmia and hyperthermia due to serotonin syndrome, in addition to takotsubo cardiomyopathy, can deteriorate to congestive heart failure following a rapid ventricular response of preexisting atrial fibrillation. The present case suggests that a therapeutic dose of maprotiline, with a concomitant therapeutic dose of dextromethorphan, is required for the occurrence of serotonin syndrome. An irritable condition, characterized by symptoms including agitation, hyperthermia, and tachycardia can result from serotonin syndrome and deteriorate to takotsubo cardiomyopathy associated with continuous adrenergic and serotonergic stimulation. This case study demonstrates that clinicians must closely monitor serotonergic drugs to ensure the prompt initiation of treatment for serotonin syndrome.
References
- 1.Gianni M., Dentali F., Grandi A.M., Sumner G., Hiralal R., Lonn E. Apical ballooning syndrome or takotsubo cardiomyopathy: a systematic review. Eur Heart J. 2006;27:1523–1529. doi: 10.1093/eurheartj/ehl032. [DOI] [PubMed] [Google Scholar]
- 2.Wittstein I.S., Thiemann D.R., Lima J.A., Baughman K.L., Schulman S.P., Gerstenblith G., Wu K.C., Rade J.J., Bivalacqua T.J., Champion H.C. Neurohumoral features of myocardial stunning due to sudden emotional stress. N Engl J Med. 2005;352:539–548. doi: 10.1056/NEJMoa043046. [DOI] [PubMed] [Google Scholar]
- 3.Boyer E.W., Shannon M. The serotonin syndrome. N Engl J Med. 2005;352:1112–1120. doi: 10.1056/NEJMra041867. [DOI] [PubMed] [Google Scholar]
- 4.De Roock S., Beauloye C., De Bauwer I., Vancraynest D., Gurne O., Gerber B., Hantson P. Tako-tsubo syndrome following nortriptyline overdose. Clin Toxicol (Phila) 2008;46:475–478. doi: 10.1080/15563650701519786. [DOI] [PubMed] [Google Scholar]
- 5.Selke K.J., Dhar G., Cohn J.M. Takotsubo cardiomyopathy associated with titration of duloxetine. Tex Heart Inst J. 2011;38:573–576. [PMC free article] [PubMed] [Google Scholar]
- 6.Rotondi F., Manganelli F., Carbone G., Stanco G. Tako-tsubo cardiomyopathy and duloxetine use. South Med J. 2011;104:345–347. doi: 10.1097/SMJ.0b013e318213f3e5. [DOI] [PubMed] [Google Scholar]
- 7.Christoph M., Ebner B., Stolte D., Ibrahim K., Kolschmann S., Strasser R.H., Schon S. Broken heart syndrome: Tako Tsubo cardiomyopathy associated with an overdose of the serotonin–norepinephrine reuptake inhibitor venlafaxine. Eur Neuropsychopharmacol. 2010;20:594–597. doi: 10.1016/j.euroneuro.2010.03.009. [DOI] [PubMed] [Google Scholar]
- 8.Mehta N.K., Aurigemma G., Rafeq Z., Starobin O. Reverse takotsubo cardiomyopathy: after an episode of serotonin syndrome. Tex Heart Inst J. 2011;38:568–572. [PMC free article] [PubMed] [Google Scholar]
- 9.Akashi Y.J., Nakazawa K., Sakakibara M., Miyake F., Musha H., Sasaka K. 123I-MIBG myocardial scintigraphy in patients with “takotsubo” cardiomyopathy. J Nucl Med. 2004;45:1121–1127. [PubMed] [Google Scholar]
- 10.Gillman P.K. Monoamine oxidase inhibitors, opioid analgesics and serotonin toxicity. Br J Anaesth. 2005;95:434–441. doi: 10.1093/bja/aei210. [DOI] [PubMed] [Google Scholar]