Abstract
There is paucity of data regarding the geographical distribution, incidence, and phylogenetics of multi-drug resistant (MDR) Salmonella Typhi in sub-Saharan Africa. Here we present a phylogenetic reconstruction of whole genome sequenced 249 contemporaneous S. Typhi isolated between 2008-2015 in 11 sub-Saharan African countries, in context of the 2,057 global S. Typhi genomic framework. Despite the broad genetic diversity, the majority of organisms (225/249; 90%) belong to only three genotypes, 4.3.1 (H58) (99/249; 40%), 3.1.1 (97/249; 39%), and 2.3.2 (29/249; 12%). Genotypes 4.3.1 and 3.1.1 are confined within East and West Africa, respectively. MDR phenotype is found in over 50% of organisms restricted within these dominant genotypes. High incidences of MDR S. Typhi are calculated in locations with a high burden of typhoid, specifically in children aged <15 years. Antimicrobial stewardship, MDR surveillance, and the introduction of typhoid conjugate vaccines will be critical for the control of MDR typhoid in Africa.
Typhoid fever is caused by the bacterium Salmonella Typhi. Here, Park et al. analyse the genomes of 249 S. Typhi isolates from 11 sub-Saharan African countries, identifying genes and plasmids associated with antibiotic resistance and showing that multi-drug resistance is highly pervasive in sub-Saharan Africa.
Introduction
Typhoid fever is a systemic infection primarily caused by the bacterium Salmonella enterica serovar Typhi (S. Typhi). The organism only infects humans, with the disease being contracted by the ingestion of bacteria through contaminated food or water. The vast majority of the global burden of disease (21.7 million estimated cases annually with 217,000 fatalities)1 is thought to arise in urban areas in low-middle income countries (LMICs) in South and Southeast Asia, but more recent data have shown a substantial burden of disease in urban and rural areas of sub-Saharan Africa2. Between 2010 and 2014, the Typhoid Fever Surveillance in Africa Programme (TSAP) conducted population-based surveillance for typhoid fever in thirteen sites in ten sub-Saharan African countries3. The TSAP study, which recruited 13,431 febrile patients, isolated 135 S. Typhi from nine countries and found notably high incidences of typhoid fever in Burkina Faso, Ghana, and Kenya2.
Many antimicrobials remain effective for the treatment of typhoid fever. However, S. Typhi that exhibit resistance to empirical antimicrobials hamper successful therapy4. The phenomenon of antimicrobial resistance (AMR) in S. Typhi has been well described, and resistance to the traditional first-line antimicrobials, ampicillin, chloramphenicol, and trimethoprim-sulfamethoxazole (co-trimoxazole), were associated with large outbreaks in Asia in the 1980s and 1990s5,6. The emergence of resistance to these first-line antimicrobials in Asia, which was dominated by the H58 genotype (now renamed 4.3.1)7,8, led to a change in typhoid treatment guidelines, with fluoroquinolones becoming the empirical choice for MDR infections9,10. However, this shift towards the more common use of fluoroquinolones was inevitably followed by a decline in susceptibility to this group of antimicrobials4,11.
Recent phylogenetic analyses further suggest that the multi-drug resistant (MDR) S. Typhi genotype 4.3.1 dominates and circulates across Southeast (lineage I: Vietnam, Cambodia, and Laos) and South Asia (lineage II: mostly India with clusters in Nepal and Pakistan)12. Additionally, these 4.3.1 S. Typhi have transferred from South Asia into Eastern and Southern Africa (lineages I and II; Kenya, Tanzania, Malawi, South Africa)12–14. The characteristics of 4.3.1 S. Typhi define this genotype as a key driving force in global MDR S. Typhi, as intercontinental transmission, regional circulation, and multiple localised outbreaks over the last three decades are distinct from the evolutionary trends and population structure of other extent S. Typhi genotypes12,15. Despite the known circulation of 4.3.1 S. Typhi in sub-Saharan Africa, there is a paucity of data regarding the geographical distribution of AMR genotypes (MDR and reduced fluoroquinolone susceptibility), their phylogenetic structure, and the incidence of MDR typhoid fever across the African continent. Here, we aimed to investigate the phylogeography and incidence of MDR S. Typhi across sub-Saharan Africa, utilizing organisms generated through the TSAP initiative2,3 and additional typhoid fever studies conducted in Ghana, Uganda, and The Gambia.
Results
Geographical distribution of S. Typhi genotypes in Africa
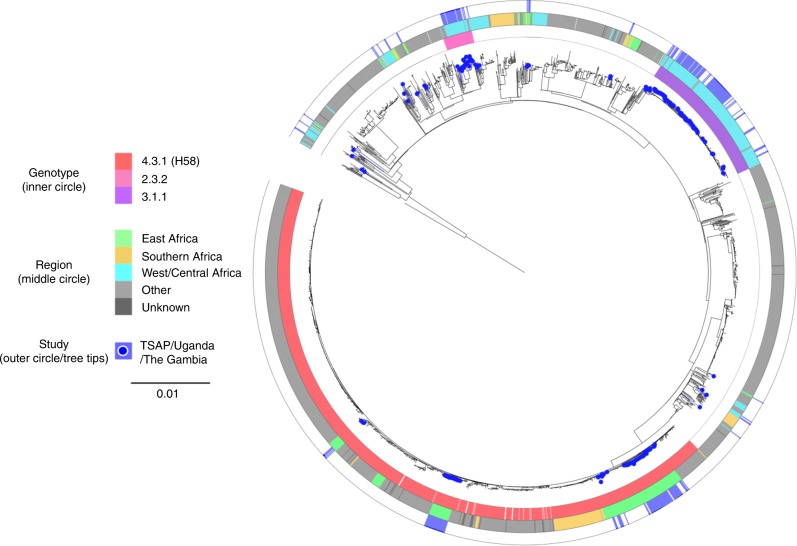
Phylogenetic analysis of 249 contemporary African S. Typhi genome sequences combined with 2,057 existing S. Typhi genome sequences (including 504 from Africa) permitted a visualisation of these new African isolates within a global S. Typhi genomic framework (Fig. 1). The primary observation was that these 249 contemporary African S. Typhi sequences were distributed throughout this framework, with multiple lineages found to be circulating simultaneously across sub-Saharan Africa in the last decade. With TSAP providing expansive sampling across the continent, we observed a substantial degree of genetic diversity, with 12 different S. Typhi genotypes represented in 11 different typhoid endemic countries (Fig. 2). This distribution of genotypes ranged from single organisms in particular countries (for example: The Gambia, Kenya, and Uganda) to numerous closely related organism clusters isolated in several countries (Supplementary Table 1).
Fig. 1.
The phylogenetic context of Salmonella Typhi isolated in sub-Saharan Africa. Maximum likelihood tree outlining the phylogenetic structure of 249 S. Typhi isolates unique to this study (highlighted by the blue points) combined with 2,057 global S. Typhi isolates. The tree is adjacent to three concentric circles highlighting associated metadata. The inner most circle represents the three most predominant genotypes (colour coded according to top of key), the middle circle represents the geographical sub-regions of Africa from where the S. Typhi organisms were isolated (colour coded according to top of key), and the outer circle (blue) again highlights the organisms unique to this study. The scale bar indicates the number of substitutions per variable site
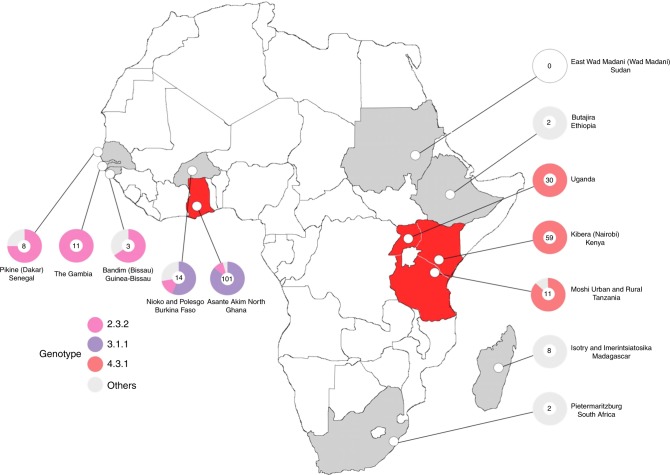
Fig. 2.
The distribution of multi-drug resistant Salmonella Typhi isolated in Africa. Map of the African continent showing the locations of the field sites from where the S. Typhi organisms were isolated for this study. Countries in which multi-drug resistant (MDR) S. Typhi were isolated are coloured in red, countries in which MDR S. Typhi were not isolated are coloured in grey. Pie charts correspond with the proportion of the main genotypes isolated (see key), with the number of isolates from each location in the centre
Despite the apparent broad genetic diversity in the circulating S. Typhi population, the majority of the recently isolated organisms (225/249; 90%) belonged to only three genotypes, 4.3.1 (H58) (99/249; 40%), 3.1.1 (97/249; 39%), and 2.3.2 (29/249; 12%). Organisms belonging to genotype 4.3.1 were found only in East Africa, comprising 100% of the S. Typhi isolates from Kenya (59/59) and Uganda (30/30), and 91% (10/11) of the isolates from Tanzania (Fig. 1 and Fig. 2). Conversely, all of the organisms belonging to genotype 3.1.1 were found only in West African sites, constituting 88% (89/101) and 57% (8/14) of the S. Typhi organisms sequenced from Ghana and Burkina Faso, respectively. Organisms belonging to genotype 2.3.2 were found only in the West African countries of Burkina Faso, The Gambia, Ghana, Guinea-Bissau, and Senegal (Fig. 2 and Supplementary Table 1).
MDR phenotypes restricted to dominant S. Typhi genotypes
The MDR phenotype was prevalent across isolates from the 11 sampled countries, with 129/249 (52%) of all isolates exhibiting the classical S. Typhi MDR phenotypic profile of resistance against ampicillin, chloramphenicol, and co-trimoxazole. MDR organisms were widely distributed in both East and West Africa, and isolated in Ghana (68/101; 67%), Kenya (50/59; 85%), Tanzania (4/11; 36%), and Uganda (7/30; 23%). No MDR organisms were identified in Burkina Faso (0/14), Ethiopia (0/2), The Gambia (0/11), Guinea-Bissau (0/3), Madagascar (0/8), Senegal (0/8), or South Africa (0/2), and none of the organisms in these countries were genotype 4.3.1 or 3.1.1 except for Burkina Faso (8/14; genotype 3.1.1) (Fig. 2 and Table 1).
Table 1.
Genotypes of MDRa S. Typhi and gyrA in four countriesb
| Country (n, all S. Typhi per country) | MDR S. Typhi (n) | MDR S. Typhi (%/out of all S. Typhi per country) | MDR S. Typhi Genotype | Non-susceptible to fluoroquinolones (n, gyrA)c |
|---|---|---|---|---|
| Ghana (101) | 68 | 67 | 3.1.1 | 0 |
| Kenya (59) | 50 | 85 | 4.3.1 (H58) | 9 (Ser83Phe) |
| Tanzania (11) | 4 | 36 | 4.3.1 (H58) | 0 |
| Uganda (30) | 7 | 23 | 4.3.1 (H58) | 30 (Ser83Tyr) |
| Total 201 S. Typhi from 4 countries (out of 249 S. Typhi from 11 countriesd) | 129 | 64% of 201 52% of 249 |
aMDR definition used for the analysis: presence of resistant genes for at least one agent in all three antimicrobial categories of ampicillin/amoxicillin (beta-lactamase: OXA-1, TEM-95/-93) AND chloramphenicol (catA1), AND trimethoprim-sulfamethoxazole (sulfonamide (sul1, sul2) and trimethoprim (dfrA7, dfrA14, dfrA15)
bFour countries with MDR S. Typhi organisms: Ghana, Kenya, Tanzania, and Uganda
cOut of total 249 S. Typhi isolates yielded from this study in 11 countries in sub-Saharan Africa, total 39 isolates were non-susceptible to fluoroquinolone (ciprofloxacin and nalidixic acid (gyrA): 9 of 39 isolates were from Kenya, of which 7 were MDR S. Typhi; and all 30 isolates from Uganda were non-susceptible to fluoroquinolones, of which 7 were MDR S. Typhi. These 39 organisms exhibited the mutations at codon 83 of gyrA; serine (TCC) to phenylalanine (TTC) for all 9 isolates from Kenya (Ser83Phe) and serine (TCC) to TAC (tyrosine) for all 30 Uganda isolates (Ser83Tyr)
dNo MDR S. Typhi from Burkina Faso (14; genotypes 2.2 (2 isolates), 2.3.2 (2 isolates), 3.1.1 (8 isolates), and 4.1.1 (2 isolates)), Ethiopia (2; genotypes 1.2 (1 isolate) and 2.2.2 (1 isolate)), Gambia (11 isolates, all genotype 2.3.2), Guinea-Bissau (3; genotypes 2.3.2 (2 isolates) and 2.3.1 (1 isolate), Madagascar (8; genotypes 2.5 (4 isolates), 2.2 (3 isolates), and 4.1 (1 isolate)), Senegal (8; genotypes 2.3.2 (6 isolates), 3.1 (1 isolate), and 4.1 (1 isolate)), and South Africa (2; all genotypes 3.1.1)
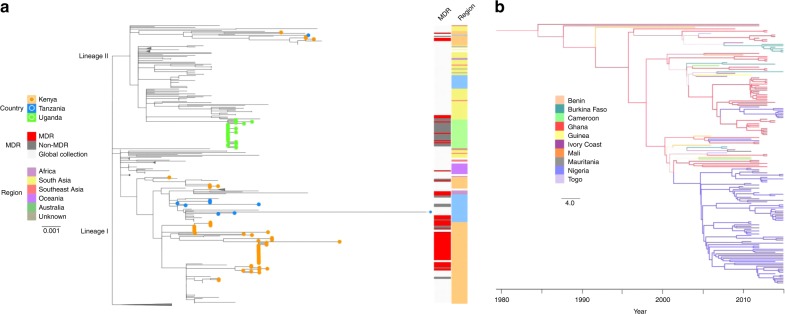
Saliently, MDR phenotypes were confined entirely within the dominant circulating genotypes in East (4.3.1) and West Africa (3.1.1). Overall, 70% (68/97) of 3.1.1 S. Typhi and 62% (61/99) of 4.3.1 S. Typhi were MDR (Supplementary Table 1). Further investigation revealed distinct origins of these MDR S. Typhi genotypes in each region. These contemporary genome sequences were compared to the existing global framework for S. Typhi 4.3.1 using a maximum likelihood phylogeny12 (Fig. 3a). Our Kenyan MDR 4.3.1 organisms (2012–2013) belonged to two distinct clades, one in lineage I and the other in lineage II, indicative of the two distinct introductions from South Asia, as identified in an earlier global study12, followed by the establishment of local populations. The Tanzanian MDR 4.3.1 organisms (2011–2012) clustered within each of these Kenyan clades, providing evidence of historical transfer of 4.3.1 S. Typhi from Kenya into Tanzania; ongoing local expansion was evident in the lineage I group only. The MDR 4.3.1 S. Typhi isolated in Uganda in 2015 formed a monophyletic clade within lineage II that was not closely related to the Kenyan or Tanzanian lineage II organisms, and were characterised by extremely narrow genetic diversity (mean pairwise genetic distance of 1 SNP), indicative of a recent population expansion or an outbreak16. This Ugandan MDR cluster was nested within a clade of 4.3.1 MDR S. Typhi organisms isolated in South Asia between 2007 and 2011, consistent with a third importation of MDR S. Typhi into East Africa from South Asia (Fig. 3a).
Fig. 3.
The phylogenetic structures of the major Salmonella Typhi genotypes in sub-Saharan Africa. a Maximum likelihood tree of genotype 4.3.1 S. Typhi isolates from this study in the context of other global genotype 4.3.1 S. Typhi isolates; the two distinct sub-lineages are labeled at the base of the tree. 4.3.1 S. Typhi isolates from this study (Kenya, Tanzania, and Uganda) are highlighted in corresponding coloured branches and circles at the tip of each tree. The first coloured bar shows the MDR phenotypes of study isolates. The second coloured bar outlines the continents and African regions where 4.3.1 S. Typhi have been detected. Scale bar indicates the number of substitutions per variable site; nodes of the tree have been collapsed for better visualization. b Maximum clade credibility tree (reconstructed using BEAST2) of genotype 3.1.1 S. Typhi isolates from this study in the context of other global genotype 3.1.1 S. Typhi isolates. Tree shows a phylogeographical reconstruction of genotype 3.1.1 S. Typhi isolates in West Africa. Branches are weighted by the support for the location changes; thicker branches have higher support. Branches and nodes are coloured according to the location that had the highest posterior probability values for some nodes of the tree. The scale bar indicates the number of substitutions per variable site per year
In contrast, the 3.1.1 MDR S. Typhi from Ghana (68 isolates) represented a population that was found only in West Africa, with the resulting phylogeny showing no evidence for inter-continental transmission as observed for 4.3.1 (Table 1). Rather, 3.1.1 S. Typhi could be better defined as a repeating pattern of small country specific population expansions with organisms being regularly transferred between countries (Fig. 3b). Phylogeographical reconstruction has not previously been performed for S. Typhi 3.1.1, therefore we conducted a Bayesian spatio-temporal phylodynamics analysis for the subclade using BEAST2 (Fig. 3b). The results suggest that Ghana was the most likely recent source of this 3.1.1 S. Typhi population (posterior probability = 0.66) which emerged de novo, and the corresponding source of three major clusters, which then radiated into other nearby countries on multiple occasions. Notably, Ghanaian S. Typhi appear to have been the probable origin of 3.1.1 S. Typhi in Burkina Faso on at least two separate occasions. Furthermore, existing whole genome sequences of 131 S. Typhi from Nigeria, including two isolates from travellers returning to the United Kingdom from Nigeria, demonstrated that 3.1.1 S. Typhi has been introduced into Nigeria from Ghana on at least two separate occasions. One of these events, estimated to be between 2010 and 2011, formed a major population expansion encompassing the majority (76/86; 88%) of the isolates from Nigeria.
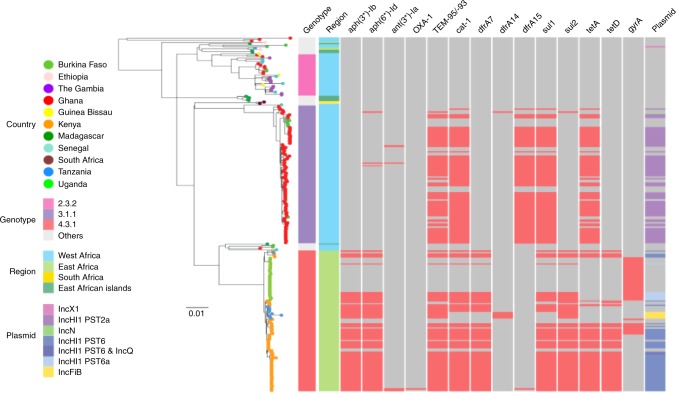
Geographically distinct S. Typhi IncHI1 MDR plasmids
We next investigated the genetic mechanisms associated with the MDR phenotypes by inferring AMR gene content in the 249 contemporaneous African S. Typhi genome sequences. Across the dataset we identified genes encoding resistance to aminoglycosides (aph(3'')-Ib, aph(6)-Id, and ant(3'')-Ia), ampicillin (OXA-1 and TEM-95/-93), chloramphenicol (catA1), trimethoprim (dfrA7, dfrA14 and dfrA15), sulfonamides (sul1 and sul2), and tetracycline (tet(A) and tet(D)). Most AMR genes were associated with IncHI1 plasmids. However, the two MDR S. Typhi genotypes were associated with distinct plasmid lineages. The 3.1.1 MDR S. Typhi from Ghana (68 isolates) carried IncHI1 MDR plasmids of plasmid sequence type (PST) 2a, whilst the 4.3.1 MDR S. Typhi from Kenya (50 isolates) and Uganda (7 isolates), respectively carried ST6 and ST6a IncHI1 MDR plasmids. Minor differences in the specific AMR genes were also evident between these plasmid types (Fig. 4). For example, the class I integron cassette contained dfrA15 in the West African/PST 2a plasmid and dfrA7 in East African/PST 6/6a plasmids, the latter plasmids also contained sul2 and tet(D) which were absent from the West African isolates.
Fig. 4.
The antimicrobial gene distribution within sub-Saharan African Salmonella Typhi. Maximum likelihood phylogenetic tree of 249 S. Typhi isolates from this study with corresponding metadata including genotype, location, antimicrobial resistance genes (AMR), and plasmids (see keys). Countries where S. Typhi isolates were isolated are highlighted by coloured circles at the tip of the branches. The three major genotypes and sub-regions of the Africa continent are shown by the coloured bars; present AMR genes are shown in red. The scale bar indicates the number of substitutions per variable site
Outliers included: non-MDR S. Typhi isolates from Burkina Faso (genotype 2.2) with an IncX1 plasmid containing no resistance genes and Ghana (genotype 3.1.1) with an IncN plasmid displaying resistance against aminoglycosides (aph(6)-Id), ampicillin (TEM-95/-93), trimethoprim (dfrA14), and sulfonamides (sul2) and 5 non-MDR S. Typhi isolates (genotype 4.3.1) from Tanzania with IncFIB plasmid carrying resistant genes aph(3'')-Ib, aph(6)-Id), TEM-95/-93, dfrA14, sul2; and an MDR S. Typhi isolate (genotype 4.3.1) from Kenya with an IncHI1 and IncQ1 plasmid associated with resistance genes against aminoglycosides (aph(3'')-Ib, aph(6)-Id), ampicillin (TEM-95/-93), chloramphenicol (catA1), trimethoprim (dfrA7), sulfonamide (sul1 and sul2), and tetracycline (tet(A) and tet(D)) (Fig. 4). Additionally, none of the four MDR organisms from Tanzania possessed a detectable plasmid backbone. Using Bandage to investigate the location of MDR cassettes, we found that these isolates carried multiple resistance genes (aph(3'')-Ib, aph(6)-Id), TEM-95/-93, catA1, dfrA7, sul1, sul2) on a 24-kb composite chromosomal transposon (Tn2670-like element) inserted between coding sequences STY3618 and STY361912.
In total, 16% (39/249) of the contemporaneous African S. Typhi exhibited reduced susceptibility against ciprofloxacin (9 from Kenya and 30 from Uganda). The Kenyan organisms exhibited the common mutation associated with reduced susceptibility to fluoroquinolones in S. Typhi, a substitution from serine to phenylalanine at codon 83 (Ser83Phe) in gyrA. The Ugandan organisms harboured an alternative serine to tyrosine gyrA mutation also at codon 83 (Ser83Tyr) (Table 1).
The incidence of MDR typhoid fever in African countries
We lastly calculated the incidence of MDR typhoid fever in specific age groups in countries where MDR S. Typhi was isolated: Ghana, Kenya, and Tanzania (Table 2). The incidence of MDR S. Typhi exceeded 100/100,000-person years of observation (PYO) in specific age groups in Ghana (<15 years: 414/100,000 PYO; 95% confidence interval [CI], 333–515) and Kenya (<15 years: 398/100,000 PYO; 95% CI, 291–545), in all age groups in Kenya (263/100,000 PYO; 95% CI, 199–347) and in the urban site in Tanzania (103/100,000 PYO; 95% CI, 61–173). While Burkina Faso had a high overall incidence of typhoid2, no MDR S. Typhi were detected; 2/14 isolates were resistant to chloramphenicol and co-trimoxazole. The highest incidence of MDR S. Typhi in a specific age group in a single location was in children aged 2–4 years in Ghana (747/100,000 PYO; 95% CI, 491–1135), followed by 5–14 year olds in Kenya (507/100,000 PYO; 95% CI, 352–729). In Kenya and Ghana, the only TSAP sites where S. Typhi were isolated from infants (aged 0–1 years), the incidences of MDR S. Typhi in this age group were 148 (95% CI, 48–458) and 60 (95% CI, 17–210) per 100,000 PYO, respectively. Generally, the incidence of MDR S. Typhi was substantially higher in children <15 years than in adults. An exception was in Tanzania, where MDR S. Typhi occurred in higher incidences in those aged ≥15 years than in young children (Table 2).
Table 2.
The incidence of MDR typhoid fever in sub-Saharan Africaa
| Country | Age group in years | PYO estimationb | Recruitment proportionb | Genome-sequenced S. Typhi casesc | Crude MDR S. Typhi cases | Crude MDR S. Typhi incidence per 100,000 PYO | Adjusted MDR S. Typhi cases | Adjusted MDR S. Typhi incidence per 100,000 PYO (95% CI)d | |||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Proportion of catchment population visiting study facility in case of fever (95% CI) | Catchment population | Catchment population adjusted by health-seeking behavior | PYO | ||||||||
| Ghana e | |||||||||||
| AAN | 0–1 | 16% (14–18) | 11222 | 1760 | 4080 | 41% | 1 | 1 | 25 | 2 | 60 (17–210) |
| 2–4 | 16% (13–18) | 8086 | 1268 | 2940 | 41% | 17 | 12 | 306 | 22 | 747 (491–1135) | |
| 0–4 | n.a. | n.a. | n.a. | n.a. | n.a. | 18 | 13 | n.a. | n.a. | n.a. | |
| 5–14 | 16% (15–17) | 34439 | 5415 | 12554 | 623/1657 (38%) | 23 | 16 | 96 | 24 | 252 (177–357) | |
| <15 | n.a. | 53747 | 8443 | 19574 | n.a. | 41 | 29 | 97 | 81 | 414 (333–515) | |
| ≥15 | n.a. | n.a. | n.a. | n.a. | n.a. | 22 | 16 | n.a. | n.a. | n.a. | |
| Non_TSAPe | n.a. | n.a. | n.a. | n.a. | n.a. | 38 | 23 | n.a. | n.a. | n.a. | |
| All | n.a. | n.a. | n.a. | n.a | n.a. | 101 | 68 | n.a. | n.a. | n.a. | |
| Kenya | |||||||||||
| Kibera | 0–1 | 42% (38–47) | 3467 | 1456 | 2031 | 99/99 (100%) | 5 | 3 | 148 | 3 | 148 (48–458) |
| 2–4 | 39% (36–43) | 3070 | 1197 | 2039 | 312/312 (100%) | 11 | 7 | 343 | 7 | 343 (164–720) | |
| 5–14 | 43% (39–47) | 7514 | 3231 | 5722 | 539/539 (100%) | 32 | 29 | 507 | 29 | 507 (352–729) | |
| <15 | n.a. | 14051 | 5884 | 9792 | n.a. | 48 | 39 | 398 | 39 | 398 (291–545) | |
| ≥15 | 35% (32–38) | 15263 | 5342 | 9228 | 301/301 (100%) | 11 | 11 | 119 | 11 | 119 (66–215) | |
| All | n.a. | 29314 | 11227 | 19020 | n.a. | 59 | 50 | 263 | 50 | 263 (199–347) | |
| Tanzania f | |||||||||||
| Moshi Rural | 0–1 | 4% (0–11) | 24289 | 390 | 693 | 79% | 0 | 0 | 0 | 0 | 0 |
| 2–4 | 2% (0–4) | 25281 | 406 | 721 | 79% | 0 | 0 | 0 | 0 | 0 | |
| 5–14 | 13% (10–16) | 118219 | 15487 | 27508 | 79% | 1 (2)f | 0 | 0 | 0 | 0 | |
| <15 | n.a. | 167789 | 16283 | 28922 | n.a. | 1 (2)f | 0 | 0 | 0 | 0 | |
| ≥15 | 2% (1–2) | 298948 | 5172 | 9186 | 79% | 2 (4)f | 0 | 0 | 0 | 0 | |
| All | n.a. | 466737 | 21454 | 38108 | n.a. | 3 (6)f | 0 | 0 | 0 | 0 | |
| Moshi Urban | 0–1 | 7% (0–19) | 10406 | 335 | 595 | 79% | 0 | 0 | 0 | 0 | 0 |
| 2–4 | 2% (0–6) | 10831 | 348 | 618 | 79% | 0 | 0 | 0 | 0 | 0 | |
| 5–14 | 13% (8–19) | 37309 | 4850 | 8615 | 79% | 3 (9)f | 2 (7)f | 12 (81)f | 1 (9)f | 15 (3–84) (103 (54–199)) f | |
| <15 | n.a. | 58546 | 5533 | 9828 | n.a. | 3 (9)f | 2 (7)f | 10 (71)f | 1 (9)f | 10 (1–72) (91 (47–175)) f | |
| ≥15 | n.a. | 125746 | 2138 | 3796 | 79% | 4 (8)f | 2 (4)f | 53 (105)f | 3 (5)f | 67 (19–229) (133 (56–319)) f | |
| All | n.a. | 184292 | 7671 | 13626 | n.a. | 7 (17)f | 4 (11)f | 29 (81)f | 4 (14)f | 29 (11–78) (103 (61–173)) f | |
aThe TSAP study has data from total 10 countries, of which 9 countries (Burkina Faso, Ethiopia, Ghana, Guinea-Bissau, Kenya, Madagascar, Senegal, South Africa, and Tanzania in alphabetical order) found blood culture confirmed S. Typhi isolates circulating in the respective sites. These S. Typhi isolates have been whole-genome sequenced for detection of multidrug resistant (MDR) genes. In addition, S. Typhi isolates yielded from 2 other surveillance activities in Uganda and The Gambia have been added to this analysis. Of these 11 countries, S. Typhi isolates with MDR genes were detected in Ghana from West Africa and Kenya, Tanzania, and Uganda from East Africa. Incidence of MDR S. Typhi in Uganda could not be estimated due to insufficient data on age stratification of patients, catchment population, healthcare seeking behavior and recruitment proportion, which were applied uniformly for the analysis presented in this table for Ghana, Kenya, and Tanzania
bPYO estimation and recruitment proportion have been published in detail in the TSAP typhoid burden paper (Marks et al, Lancet Global Health, 2017).
cGenome sequenced S. Typhi case numbers in this table may not exactly match the crude S. Typhi case numbers reported in the TSAP typhoid burden paper (Marks et al) due to few sequencing failures
dAdjusted incidence rates per 100,000 PYO (95% CI): adjustments for case recruitment and error factors
eGhana samples include non-TSAP projects as outlined in the Supplementary Table 2. AAN: Asante Akim North (Supplementary Table 2)
fTanzania: Enrolment algorithm has been applied to the crude MDR S. Typhi case numbers, that is: recruitment by every 5th patient if enrolled before Nov 11th 2011 and every 2nd patient if enrolled after then. 1 isolate from Tanzania, which was from outside the study catchment area (Supplementary Table 2: “Moshi Other”) is not included in this incidence table due to the insufficient background data required as mentioned in this footnote
Discussion
Here we present a contemporary dataset of S. Typhi genome sequences and AMR data from across sub-Saharan Africa generated through a major population-based surveillance study with data augmented from further locations. We exploited these data to assess the circulation of MDR S. Typhi genotypes and to calculate the incidence of MDR typhoid infections across the continent. Our results have major implications for the use of empirical antimicrobials for treating febrile disease of presumed bacterial origin and future intervention measures for controlling typhoid in Africa.
Despite the broad genetic diversity observed within the continental S. Typhi population, we identified only three principal S. Typhi genotypes. These genotypes were geographically limited to East (genotype 4.3.1) and West (genotypes 3.1.1 and 2.3.2) Africa. MDR S. Typhi in Africa is currently dominated by genotypes 4.3.1 and 3.1.1. S. Typhi 4.3.1 has been previously reported to circulate only in East Africa on the African continent12–14, with 3.1.1 dominating in Nigeria and circulating amongst neighbouring countries in West Africa17. After the likely importation from South Asia within the last 20 years, the extant population of S. Typhi 4.3.1 in Kenya, Tanzania, and Uganda has been formed through multiple introductions from South Asia followed by local expansions. Conversely, S. Typhi 3.1.1, which were isolated in Ghana, Burkina Faso, and Nigeria, do not appear to have recent ancestral roots in Asia, but have undergone localised microevolution within West Africa in recent decades. We speculate that these organisms have been transferred, maintained, and selected through the sustained movement of people and antimicrobial usage in West Africa. The MDR 4.3.1 S. Typhi from Kenya and Uganda also commonly exhibited mutations in gyrA, associated with reduced susceptibility to fluoroquinolones, which has also been reported in Africa in recent years. Conversely, no gyrA mutations were found in the MDR S. Typhi 3.1.1 from Ghana. These data mirror recent reports from Nigeria17, and suggest that first-line antimicrobial agents (ampicillin, chloramphenicol, and co-trimoxazole) for the treatment of febrile diseases are still in common use in West Africa.
The acquisition of an MDR phenotype in S. Typhi is typically associated with IncHI1 plasmids, which have long been considered the main vehicle for resistance to first-line antimicrobials in S. Typhi8. The distinct MDR lineages of S. Typhi found in West and East Africa, each associated with a distinct IncHI1 plasmid sequence type, suggest that S. Typhi and its AMR plasmids have not been transferred laterally across the continent. This may be because genotype 4.3.1 MDR S. Typhi has not been circulating for a sufficient period in Africa to reach the West African region. Furthermore, the four MDR S. Typhi isolates from Tanzania did not harbour plasmid-associated sequences, suggesting that these AMR genes are inserted into the chromosome, as has been observed previously in Asia12,18,19 and Zambia20. The integration of AMR genes into the S. Typhi chromosome is a worrying development, as it provides a mechanism for stable vertical transmission of the MDR phenotype without the potential fitness deficit associated with maintaining large plasmids, increasing the likelihood that MDR will be sustained during the ongoing spread of related S. Typhi across East Africa.
Here we identified specific populations that are most at risk of MDR typhoid, which particularly warrants a reconsideration of current empirical antimicrobial use for treatment of typhoid. Generally, we found that the site incidences of MDR S. Typhi corresponded largely with the overall burden of typhoid in the various study sites2 (that is, countries with high incidences of typhoid also had high incidences of MDR S. Typhi). Consequently, Kenya and Ghana exhibited the highest incidences of MDR typhoid in the sampled countries. Notably, Burkina Faso, which had a high burden of typhoid, had no incidence of MDR S. Typhi in comparison to neighbouring Ghana. Further, we found that children aged <15 years, the highest at-risk age group for typhoid in Africa, also generally exhibited the highest incidence rates of MDR S. Typhi infections. This age distribution of typhoid caused by MDR S. Typhi was not consistent across the continent, as those aged >15 years in Tanzania exhibited a higher incidence of MDR S. Typhi than younger children. Alternatively, some sites with a high burden of typhoid in specific age groups had no MDR infections. We suggest that this distribution is likely to mirror access to, and the generic usage of, specific antimicrobial agents in these locations and age groups, warranting the need for continued country/site-specific surveillance, review of local treatment policies, and the collection of antimicrobial usage data.
The incidence of MDR typhoid varied dramatically between settings and also between age groups in some individual locations. This discrepancy may be due to differing exposures to antimicrobials in different settings and age groups, which could lead to differential selective pressures in local circulating bacterial populations. Our data additionally indicate that AMR/MDR S. Typhi are not only spread through local population movements in East and West Africa but can also arise de novo. This phenomenon can be observed within the microevolution and expansion of 3.1.1 MDR S. Typhi in West Africa. The AMR genes associated with 4.3.1 MDR S. Typhi in East Africa appear to be both plasmid and chromosomally located. This observation, coupled with the acquisition of reduced susceptibility to fluoroquinolones, transmission between East African countries, and the importation of organisms from South Asia, raises further concerns regarding the progression of drug resistant S. Typhi in Africa. 4.3.1 S. Typhi has spread successfully cross South Asia and become increasingly resistant to ciprofloxacin, making treatment options more limited4. The pervasiveness of AMR in 4.3.1 S. Typhi in South Asia has been recently highlighted by an outbreak of a ceftriaxone-resistant 4.3.1 S. Typhi in Hyderabad, Pakistan, which appears to be resistant to commonly available antimicrobial classes21. We predict that new AMR phenotypes that emerge in 4.3.1 S. Typhi in Asia can be periodically introduced into East Africa. Further, the emergence of MDR S. Typhi 4.3.1 in South Africa suggests possible spread from East Africa to Southern Africa through human population movement, however this notion requires further investigation22.
This study highlights locations in sub-Saharan Africa where MDR typhoid is prevalent and where future activities to control its spread from Asia into Africa and also within Africa could be focused. In addition to continuing disease surveillance and investigating the genomic characteristics and phenotypic profiles of MDR S. Typhi, compiling antimicrobial usage data that can be linked with the distribution of AMR/MDR bacterial pathogens across Africa is becoming essential. The World Health Organization (WHO) has prequalified a typhoid conjugate vaccine (TCV) in January 2018 with a recommendation to introduce the vaccine for infants and children older than six months in typhoid endemic countries23. Targeted vaccination programs at sites with a high burden of AMR/MDR S. Typhi could also be considered and may be informed by the age-stratified MDR disease incidence data presented here. New and potentially highly efficacious S. Typhi conjugate vaccines are currently undergoing clinical trials and should become routinely available at the end of this decade23. Until these vaccines become available, countries in Africa with endemic typhoid should structure antimicrobial stewardship policies to control MDR S. Typhi and develop national roadmaps for their deployment.
Methods
Bacterial isolates and antimicrobial susceptibility testing
Between 2010 and 2014, a population-based surveillance of invasive Salmonella infections was conducted in ten sub-Saharan countries (see Supplementary Table 2)2. The research methodology including ethics approvals, sampling framework, and calculation of disease incidence of this programme have been previously reported3. Briefly, over the TSAP sampling period, blood culture-based surveillance was conducted in defined catchment areas. Cultured isolates were assessed for antimicrobial susceptibilities by the disc diffusion method locally and at a central reference laboratory. TSAP recruited 13,558 patients meeting the study inclusion criteria, of which 127 patients were excluded due to incomplete data. This resulted in 13,431 patients and 135 S. Typhi found in 9 countries for analysis2. We also included 114 additional S. Typhi collected from other studies in Africa (Uganda; 2015, Gambia; 2008-2014 and non-TSAP isolates from Ghana; 2010), resulting in a collection of 249 S. Typhi (Supplementary Table 2).
Genome sequencing and SNP calling
Genomic DNA from the 249 S. Typhi isolates was extracted using the Wizard Genomic DNA Extraction Kit (Promega, Wisconsin, USA). Two μg of genomic DNA from each organism was subjected to indexed-tagged pair-end sequencing on an Illumina Hiseq 2000 platform (Illumina, CA, USA) to generate 100 bp paired-end reads. To identify single nucleotide polymorphisms (SNPs), raw Illumina reads were mapped to the reference sequence of S. Typhi CT18 (accession: AL513382) including plasmids pHCM1 (accession: AL513383) and pHCM2 (accession: AL513384), using SMALT version 0.7.4. Candidate SNPs were called against the reference sequence using SAMtools24 and filtered with a minimal phred quality of 30 and minimum consensus base agreement of 75%. The allele at each locus in each isolate was determined by reference to the consensus base in that genome using SAMtools mpileup and removing low confidence alleles with consensus base quality ≤20, read depth ≤5 or a heterozygous base call. SNPs in phage regions, repetitive sequences, or recombinant regions identified previously were excluded12,25. We further identified an additional recombinant region from the whole genome alignment produced by SNP-calling isolates using Gubbins26 and SNPs detected within this region (~20kb from nucleotide 1,439,032-1,459,472) were removed, resulting in a final set of 4,444 chromosomal SNPs. The SNP data were used to assign all isolates to previously defined subclades in the S. Typhi genotyping framework15.
Phylogenetic analysis
A maximum likelihood (ML) phylogenetic tree was constructed from the 4,444 SNP alignment using RAxML version 8.2.8 with a generalized time-reversible model and a Gamma distribution to model the site-specific rate variation (GTR+Γ4 model)27. Branch support for this tree was assessed through a bootstrap analysis with 1,000 pseudo-replicates. To investigate the molecular epidemiology of our African isolates in regional and international context, a secondary ML tree was inferred from a separate alignment of 26,479 SNPs identified across a total of 2,306 S. Typhi isolates (249 from this study, 1,830 from the global collection12, 128 from Nigeria17, and 99 travel-associated S. Typhi organisms isolated in the United Kingdom15) using RAxML with GTRGAMMA substitution model and S. Paratyphi A sequence data to outgroup root the tree. Branch support for this phylogeny was assessed through a 100 bootstrap pseudo-analysis. Annotation of this global tree was visualized using ITOL28. An interactive version of the global phylogeny, with organisms labeled by genotype, country of origin, year of isolation and antimicrobial susceptibility was generated in Microreact29.
Evolutionary timescale and phylogeographic patterns
For genotype 3.1.1 strains, Bayesian phylogenetic analyses was conducted in BEAST2 v2.4.730. The GTR+Γ4 substitution model, an uncorrelated lognormal relaxed-clock model, and the exponential-growth coalescent tree prior were used. Three independent analyses were performed with 5×108 steps, recording samples every 5×104 steps. We assessed sufficient sampling by combining the three independent runs and verifying that the effective sample size of all parameters was at least 500. To calibrate the molecular clock, we used the sampling year of all sequences. This analysis also included an outgroup sequence (CT18) to ensure a biologically meaningful root location. Our selected molecular clock model and tree prior have been shown to perform well even when the data display low rate variation and constant population size dynamics31. This model combination also allows for informal model testing via the coefficient of rate variation and the population growth rate parameters32,33. To determine phylogeographic patterns, we considered the country of sampling as a discrete trait in our analysis in BEAST234. A potential shortcoming of this analysis was that it includes a large number of parameters (transition rates between all locations), therefore the output of these analysis may be affected by the prior distribution. We verified that the prior distribution differed from the posterior by comparing the distributions of all transition rates.
An important consideration when using sampling times as calibrations is that the sampling timespan should capture sufficient genetic variation to allow reliable inferences of evolutionary rates and timescales, such that the data have strong temporal structure. We verified the temporal structure in the data by using a root-to-tip regression and a date-randomisation test35. We conducted a root-to-tip regression for the outgroup-rooted ML tree using TempEst36, and obtained a positive value for the slope, an R2 of 0.12, and a p-value of 3×10-6 (Supplementary Figure 1). For the date-randomisation test we repeated the analysis 20 times while randomising the sampling times. Our expectation was that the randomisations should produce evolutionary rate estimates that were lower and that did not overlap with those obtained with the correct sampling times37, which was the case for our data (Supplementary Figure 2). Finally, we compared our estimate of the time of origin of the 3.1.1 lineage in BEAST with an independent method, LSD v0.338. LSD and BEAST2 produced congruent estimates of the time of origin of the 3.1.1 lineage (Supplementary Figure 3).
Antimicrobial resistance gene and plasmid analyses
ARIBA (Antimicrobial Resistance Identifier by Assembly)39 and CARD (https://card.mcmaster.ca/home) were used to investigate AMR gene content. ARIBA reported the AMR genes and the quality of assemblies and variants detected between the sequencing reads and the reference sequences, including mutations in the quinolone resistance-determining region (QRDR) of the gyrA, gyrB, parC, and parE genes. For plasmid identification, the sequence reads from each isolate were de novo assembled using the short-read assembler Velvet with parameters optimized by Velvet Optimizer40,41. Contigs that were less than 300 bp long were excluded and the assembled contigs were annotated using Prokka41,42. Plasmid typing was performed in silico using PlasmidFinder43. The presence of the IncHI1 plasmid was confirmed by BLASTN searching the assembled sequences in reference to the pHCM1 reference plasmid sequence, and comparative analyses were performed and visualized using ACT44. The IncHI1 plasmid sequence type was identified using SRST2 software45 with the IncHI1 plasmid MLST scheme46. To investigate the isolates with MDR phenotype and without plasmid, raw sequences were subjected to de novo genome assembly using SPAdes47 version 3.11.0, and the resulting assembly graph was visualized in Bandage48 to inspect the location of AMR genes in the genome.
Incidence analyses of MDR S. Typhi
Incidence of MDR S. Typhi was estimated per 100,000 person-years of observation (PYO) for MDR S. Typhi isolates found in Ghana, Kenya and Tanzania. Statistical methodology used previously to calculate the incidence of S. Typhi TSAP isolates2,3 was applied to calculate MDR S. Typhi incidence. Briefly, age-stratified PYO were estimated using available demographic data in HDSS (Health and Demographic Surveillance System) and non-HDSS sites and health-seeking behaviour of randomly selected individuals, representative of the study population, were factored in (denominator). The recruitment proportion was adjusted to the age-stratified crude MDR S. Typhi cases (numerator). Adjusted incidence of MDR S. Typhi per 100,000 PYO was estimated with 95% CIs using these adjustment factors and crude MDR S. Typhi case numbers. The previously established multi-country database (FoxPro software) for TSAP was used for the three countries with MDR S. Typhi. The incidence of MDR S. Typhi in Uganda could not be measured, as data regarding adjustment factors (healthcare seeking behaviour and recruitment proportion) was unavailable at the time of analysis.
Electronic supplementary material
Acknowledgements
This study was supported by the Bill & Melinda Gates Foundation (grant: OPPGH5231). The findings and conclusions contained within are our own and do not necessarily reflect positions or policies of the Bill & Melinda Gates Foundation or the US Centers for Disease Control and Prevention, the International Vaccine Institute. The International Vaccine Institute acknowledges its donors, including the Government of the Republic of Korea and the Swedish International Development Cooperation Agency (SIDA). Research infrastructure at the Moshi site was supported by the US National Institutes of Health (R01TW009237; U01 AI062563; R24 TW007988; D43 PA-03-018; U01 AI069484; U01 AI067854; P30 AI064518), and by the UK Biotechnology and Biological Sciences Research Council (BB/J010367). SB is a Sir Henry Dale Fellow, jointly funded by the Wellcome Trust and the Royal Society (100087/Z/12/Z). KEH is supported by a Senior Medical Research Fellowship from the Viertel Foundation of Australia. Z.A.D. was supported by strategic award #106158 from the Wellcome Trust of Great Britain (106158/Z/14/Z). V.K.W. is supported by NIHR and NIHR Cambridge BRC. We thank staff at the TSAP network countries, the Medical Research Council Unit The Gambia, and the Uganda Public Health Emergency Operations Centre, Kampala, Uganda. We are grateful to Soo-Young Kwon for her invaluable administrative support of the project.
Author contributions
S.E.P., D.P.T., C.B., V.K.W., G.D.P., S.D. and Z.D. contributed in data analysis, interpretation of results under the scientific guidance from S.B. and K.E.H. S.E.P. drafted and edited the paper and S.B. contributed in structuring and editing of the paper. F.M. contributed in project oversight. F.M., S.E.P., V.vK., L.M.C.E., U.P., G.D.P., J.I., H.S-G., J.A.C., R.F.B., Y.A-S., E.O-D., R.R., A.B.S., A.A., N.G., K.H.K., J.M., A.G.S., P.A., H.M.B., J.T.H., J.M.M., L.C., B.O., B.F., N.S., T.J.L.R., T.M.R., L.P.K., E.S., M.T., B.Y., M.A.E.T., A.S., S.P., A.T., A.N., M.B.A., S.V.L., H.J.S., H.J.J., J.F.D., J.K.P., F.K., P.H., J.N.S., T.V., R.D., U.N.I., G.A.M. and S.O. contributed to data acquisition in the field, interpretation of results, and editing of the paper. G.D., J.A.K., A.P., D.M.A., S.A., M.A. and J.D.C. contributed to data interpretation. All authors read and approved the final draft.
Data availability
Raw sequence data are available in the European Nucleotide Archive (projects ERP009684, ERP010763, ERP013866). The Microreact interactive phylogeny of the analysed isolates is available at: https://microreact.org/project/HJWBihsvz. SMALT version 0.7.4 used is available at: http://www.sanger.ac.uk/resources/software/smalt/.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Florian Marks, Stephen Baker
Electronic supplementary material
Supplementary Information accompanies this paper at 10.1038/s41467-018-07370-z.
References
- 1.Crump JA, Luby SP, Mintz ED. The global burden of typhoid fever. Bull. World Health Organ. 2004;82:346–353. [PMC free article] [PubMed] [Google Scholar]
- 2.Marks F, et al. Incidence of invasive salmonella disease in sub-Saharan Africa: a multicentre population-based surveillance study. Lancet Glob. Heal. 2017;5:e310–e323. doi: 10.1016/S2214-109X(17)30022-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Von Kalckreuth V, et al. The typhoid fever surveillance in africa program (TSAP): clinical, diagnostic, and epidemiological methodologies. Clin. Infect. Dis. 2016;62:s9–s16. doi: 10.1093/cid/civ693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Thanh DP, et al. A novel ciprofloxacin-resistant subclade ofh58. Salmonella Typhi is associated with fluoroquinolone treatment failure. eLife. 2016;5:1–13. doi: 10.7554/eLife.14003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rowe Bernard, Ward Linda R., Threlfall E. John. Multidrug-Resistant Salmonella typhi: A Worldwide Epidemic. Clinical Infectious Diseases. 1997;24(Supplement_1):S106–S109. doi: 10.1093/clinids/24.Supplement_1.S106. [DOI] [PubMed] [Google Scholar]
- 6.Mirza S. H., Beechmg N. J., Hart C. A. Multi-drug resistant typhoid: a global problem. Journal of Medical Microbiology. 1996;44(5):317–319. doi: 10.1099/00222615-44-5-317. [DOI] [PubMed] [Google Scholar]
- 7.Roumagnac P., Weill F.-X., Dolecek C., Baker S., Brisse S., Chinh N. T., Le T. A. H., Acosta C. J., Farrar J., Dougan G., Achtman M. Evolutionary History of Salmonella Typhi. Science. 2006;314(5803):1301–1304. doi: 10.1126/science.1134933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Holt KE, et al. Emergence of a globally dominant inchi1 plasmid type associated with multiple drug resistant typhoid. PLoS Negl. Trop. Dis. 2011;5:e1245. doi: 10.1371/journal.pntd.0001245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Akhtar S, et al. Antimicrobial resistance in Salmonella enterica serovar Typhi and paratyphi in South Asia-current status, issues and prospects. Crit. Rev. Microbiol. 2015;41:536–545. doi: 10.3109/1040841X.2014.880662. [DOI] [PubMed] [Google Scholar]
- 10.Emary K, et al. Enteric fever in Cambodian children is dominated by multidrug-resistant H58 Salmonella enterica serovar Typhi with intermediate susceptibility to ciprofloxacin. Trans. R. Soc. Trop. Med. Hyg. 2012;106:718–724. doi: 10.1016/j.trstmh.2012.08.007. [DOI] [PubMed] [Google Scholar]
- 11.Parry Christopher M. Antimicrobial drug resistance in Salmonella enterica. Curr. Opin. Infect. Dis. 2003;16:467–472. doi: 10.1097/00001432-200310000-00014. [DOI] [PubMed] [Google Scholar]
- 12.Wong VK, et al. Phylogeographical analysis of the dominant multidrug-resistant H58 clade of Salmonella Typhi identifies inter-and intracontinental transmission events. Nat. Genet. 2015;47:632–639. doi: 10.1038/ng.3281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Feasey NA, et al. Rapid emergence of multidrug resistant, H58-lineage Salmonella typhi in blantyre, Malawi. PLoS Negl. Trop. Dis. 2015;9:1–13. doi: 10.1371/journal.pntd.0003748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kariuki S, et al. Typhoid in Kenya is associated with a dominant multidrug-resistant salmonella enterica serovar typhi haplotype that is also widespread in Southeast Asia. J. Clin. Microbiol. 2010;48:2171–2176. doi: 10.1128/JCM.01983-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wong VK, et al. An extended genotyping framework for Salmonella enterica serovar Typhi, the cause of human typhoid. Nat. Commun. 2016;7:12827. doi: 10.1038/ncomms12827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kabwama SN, et al. A large and persistent outbreak of typhoid fever caused by consuming contaminated water and street-vended beverages: Kampala, Uganda, January - June 2015. BMC Public. Health. 2017;17:1–9. doi: 10.1186/s12889-016-3954-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wong VK, et al. Molecular surveillance identifies multiple transmissions of Typhoid in West Africa. PLoS Negl. Trop. Dis. 2016;10:1–22. doi: 10.1371/journal.pntd.0004781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chiou CS, Alam M, Kuo JC, Liu YY, Wang PJ. Chromosome-mediated multidrug resistance in Salmonella enterica serovar Typhi. Antimicrob. Agents Chemother. 2015;59:721–723. doi: 10.1128/AAC.04081-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ashton PM, et al. MinION nanopore sequencing identifies the position and structure of a bacterial antibiotic resistance island. Nat. Biotechnol. 2015;33:296–300. doi: 10.1038/nbt.3103. [DOI] [PubMed] [Google Scholar]
- 20.Hendriksen RS, et al. Genomic signature of multidrug-resistant salmonella enterica serovar Typhi isolates related to a massive outbreak in Zambia between 2010 and 2012. J. Clin. Microbiol. 2015;53:262–272. doi: 10.1128/JCM.02026-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Klemm, E. J. et al. Emergence of an extensively drug-resistant Salmonella enterica serovar typhi clone harboring a promiscuous plasmid encoding resistance to fluoroquinolones and third-generation cephalosporins. mBio9, e00105 (2018). [DOI] [PMC free article] [PubMed]
- 22.Keddy Karen H., Sooka Arvinda, Smith Anthony M., Musekiwa Alfred, Tau Nomsa P., Klugman Keith P., Angulo Frederick J. Typhoid Fever in South Africa in an Endemic HIV Setting. PLOS ONE. 2016;11(10):e0164939. doi: 10.1371/journal.pone.0164939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Burki T. Typhoid conjugate vaccine gets WHO prequalification. Lancet Infect. Dis. 2018;18:258. doi: 10.1016/S1473-3099(18)30087-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Li H, et al. The Sequence Alignment/Map format and SAMtools. Bioinformatics. 2009;25:2078–2079. doi: 10.1093/bioinformatics/btp352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Holt KE, et al. High-throughput sequencing provides insights into genome variation and evolution in Salmonella Typhi. Nat. Genet. 2008;40:987–993. doi: 10.1038/ng.195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Croucher NJ, et al. Rapid phylogenetic analysis of large samples of recombinant bacterial whole genome sequences using Gubbins. Nucleic Acids Res. 2015;43:e15. doi: 10.1093/nar/gku1196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stamatakis A. RAxML version 8: aool for phylogenetic analysis and post-analysis of large phylogenies. Bioinformatics. 2014;30:1312–1313. doi: 10.1093/bioinformatics/btu033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Letunic I, Bork P. Interactive Tree Of Life (iTOL): an online tool for phylogenetic tree display and annotation. Bioinformatics. 2007;23:127–128. doi: 10.1093/bioinformatics/btl529. [DOI] [PubMed] [Google Scholar]
- 29.Argimón S, et al. Microreact: visualizing and sharing data for genomic epidemiology and phylogeography. Microb. Genom. 2016;2:e000093. doi: 10.1099/mgen.0.000093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bouckaert R, et al. BEAST 2: a software platform for bayesian evolutionary analysis. PLoS Comput. Biol. 2014;10:1–6. doi: 10.1371/journal.pcbi.1003537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Duchêne S, Geoghegan JL, Holmes EC, Ho SYW. Estimating evolutionary rates using time-structured data: a general comparison of phylogenetic methods. Bioinformatics. 2016;32:3375–3379. doi: 10.1093/bioinformatics/btw005. [DOI] [PubMed] [Google Scholar]
- 32.Duchêne S, et al. Cross-validation to select Bayesian hierarchical models in phylogenetics. BMC Evol. Biol. 2016;16:1–8. doi: 10.1186/s12862-016-0688-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ho SYW, Duchêne S, Duchêne D. Simulating and detecting autocorrelation of molecular evolutionary rates among lineages. Mol. Ecol. Resour. 2015;15:688–696. doi: 10.1111/1755-0998.12320. [DOI] [PubMed] [Google Scholar]
- 34.Lemey P, Rambaut A, Drummond AJ, Suchard MA. Bayesian phylogeography finds its roots. PLoS Comput. Biol. 2009;5:e1000520. doi: 10.1371/journal.pcbi.1000520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rieux A, Balloux F. Inferences from tip-calibrated phylogenies: a review and a practical guide. Mol. Ecol. 2016;25:1911–1924. doi: 10.1111/mec.13586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rambaut A, Lam TT, Max Carvalho L, Pybus OG. Exploring the temporal structure of heterochronous sequences using TempEst (formerly Path-O-Gen) Virus Evol. 2016;2:vew007. doi: 10.1093/ve/vew007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Duchêne Sebastián, Duchêne David, Holmes Edward C., Ho Simon Y.W. The Performance of the Date-Randomization Test in Phylogenetic Analyses of Time-Structured Virus Data. Molecular Biology and Evolution. 2015;32(7):1895–1906. doi: 10.1093/molbev/msv056. [DOI] [PubMed] [Google Scholar]
- 38.To TH, Jung M, Lycett S, Gascuel O. Fast Dating using least-squares criteria and algorithms. Syst. Biol. 2016;65:82–97. doi: 10.1093/sysbio/syv068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hunt, M. et al. ARIBA: rapid antimicrobial resistance genotyping directly from sequencing reads. Microb. Genomics 1–11 (2017). 10.1099/mgen.0.000131 [DOI] [PMC free article] [PubMed]
- 40.Zerbino DR, Birney E. Velvet: Algorithms for de novo short read assembly using de Bruijn graphs. Genome Res. 2008;18:821–829. doi: 10.1101/gr.074492.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Parkhill J, et al. Robust high-throughput prokaryote de novo assembly and improvement pipeline for Illumina data. Microb. Genom. 2016;2:1–7. doi: 10.1099/mgen.0.000083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Seemann T. Prokka: Rapid prokaryotic genome annotation. Bioinformatics. 2014;30:2068–2069. doi: 10.1093/bioinformatics/btu153. [DOI] [PubMed] [Google Scholar]
- 43.Carattoli A, et al. In Silico detection and typing of plasmids using plasmidfinder and plasmid multilocus sequence typing. Antimicrob. Agents Chemother. 2014;58:3895–3903. doi: 10.1128/AAC.02412-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Carver T, et al. Artemis and ACT: Viewing, annotating and comparing sequences stored in a relational database. Bioinformatics. 2008;24:2672–2676. doi: 10.1093/bioinformatics/btn529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Inouye M, et al. SRST2: Rapid genomic surveillance for public health and hospital microbiology labs. Genome Med. 2014;6:90. doi: 10.1186/s13073-014-0090-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Phan MD, et al. Variation in Salmonella enterica serovar typhi IncHI1 plasmids during the global spread of resistant typhoid fever. Antimicrob. Agents Chemother. 2009;53:716–727. doi: 10.1128/AAC.00645-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bankevich A, et al. SPAdes: A New Genome Assembly Algorithm and Its applications to Single-Cell Sequencing. J. Comput. Biol. 2012;19:455–477. doi: 10.1089/cmb.2012.0021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wick RR, Schultz MB, Zobel J, Holt KE. Bandage: Interactive visualization of de novo genome assemblies. Bioinformatics. 2015;31:3350–3352. doi: 10.1093/bioinformatics/btv383. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Raw sequence data are available in the European Nucleotide Archive (projects ERP009684, ERP010763, ERP013866). The Microreact interactive phylogeny of the analysed isolates is available at: https://microreact.org/project/HJWBihsvz. SMALT version 0.7.4 used is available at: http://www.sanger.ac.uk/resources/software/smalt/.