Abstract
Aspiration pneumonia in infants emerges as a result of deglutition disorders, congenital malformations and severe gastroesophageal reflux. Hydrocarbon pneumonitis is caused by the accidental ingestion and aspiration of hydrocarbons into the body. In children, it can be seen as a result of both the lack of monitoring and the tendency for the exploration of the environment. The accidental ingestion of a large quantity is quite rare due to the bad taste of hydrocarbons. Initially, the central nervous system is the one affected, followed by the respiratory system, causing the chemical pneumonia (through direct injury of the lung). Furthermore, we shall present the case of an 18 month infant with severe trauma as a result of the accidental ingestion of diesel, followed by vomiting and who was brought late to the hospital. The pneumothorax that emerged as a complication was remitted after the treatment, but the initially chemical and then mixed pneumonia through bacterial overinfection led to the infant’s death after 12 days of medical attention in the Anesthesia and Intensive Care Unit. The histopathological examination of the analyzed lung fragments did not point out any lipid or foam cells that are characteristic to this type of pathology, but which are not mentioned by the majority of toxicology textbooks and those of pathological anatomy, through the low rate of mortality and numerous factors that can lead to negative false results.
Keywords: pneumonia, aspiration, children
Introduction
Aspiration pneumonia in infants emerges as a result of deglutition disorders, congenital malformations and severe gastroesophageal reflux. Lipid pneumonia is rare and it is produced, more frequently, iatrogenically [1].
The intoxication through the ingestion and aspiration of hydrocarbons in infants can cause pneumonia which very rarely has a fatal evolution. Pneumonitis induced by aspiration of diesel was firstly reported by Laughlen in 1925 [2]. If the anamnesis does not reveal the exposure to hydrocarbons, the diagnosis is very difficult since there are no clinical and radiological particularities of this intoxication. Hydrocarbons are organic substances which contain both carbon and hydrogen. They are liquid in general at ambient temperature and the ingestion of a large quantity of hydrocarbons is unusual because of the bad taste. The intoxication is more frequent in infants who are insufficiently looked after or neglected, it is accidental and it is produced through the exploration of the environment.
The direct injury of the pulmonary parenchyma causes the chemical pneumonia or the hypoxia because of the edema and the bronchial spasm. The general respiratory symptoms appear in the first hours after the exposure and they diminish frequently after an interval between 2 and 8 days [3]. The changes within the chest x-ray occur in the first 2-6 hours from the aspiration; sometimes, it is necessary a second examination. In extreme cases, complications may emerge, leading to severe hypoxia, acute respiratory distress syndrome (ARDS), hypoxic encephalopathy and even death [3]. Respiratory complications refer to pleurisy, pneumothorax, chemical pneumonia and secondary bacterial infections. There may appear other symptoms such as neurological, gastro-intestinal, heart, liver, kidney, and hematologic ones.
Most of the patients who ingest hydrocarbons causing the emergence of chemical pneumonia are cured completely, death occurs very rarely (below 1% of cases) [4], while the prognosis can be influenced by the existence of the bacterial overinfection.
The histopathological changes in lungs (extensive interstitial edema, intra-alveolar fibrin exudate, epithelial desquamation and inflammatory infiltrate) have rarely been pointed out due to the rare cases of death [5,6]. Degenerative and sometimes hemorrhagic lesions were experimentally described at the liver, kidney, spleen and bone marrow levels. The most important characteristic of hydrocarbon aspiration, from an anatomopathological point of view, is the obvious presence of lipid cells in the lung [7]. This fact is not presented in the majority of toxicology textbooks and those of pathological anatomy due to factors that may influence the result of chemical analyses (occurrence of death after more than 4-5 days since the exposure, treatment received by the patient, pathologists’ preference for chromatographic techniques for detecting hydrocarbons, methods for collecting and preparing sampled specimens [3,5].
Clinical case
We present the case of an 18 month-old girl who was admitted to the intensive care unit within Craiova Emergency University Hospital, by transfer from another hospital where she had been previously hospitalized for 2 days after the ingestion of an undetermined quantity of diesel followed by vomiting (the toxic exposure took place after another prior 24 hours). Approximately 36 hours since the admittance, signs of acute respiratory failure had occurred, with a significant drop in the oxygen saturation and the alteration of the sensorium.
The initial thoracic radiography (performed 24 hours since the exposure) did not point out any pathological changes. When the infant was admitted to intensive care, her nutrition level was satisfactory but her condition was extremely serious, with acute respiratory distress syndrome, acute dyspnea, generalized cyanosis, 50% oxygen saturation level, very high respiratory effort (13/minutes respiratory rate), VA=174/minutes, BP=110/50 mmHg, low reactivity, reduced vesicular breath sounds within the area of the left hemithorax, coughing and afebrility. The arterial blood gas tests showed: ph=6.98, PaO2=42.4 mmHg, PaCO2=70.2 mmHg; EKG: sinus tachycardia, the hemogram indicated changed values: Hb=9.2 g/dl, No. erythrocytes (RBC)=3.58x106/mm3, Ht (HCT)=27.4%, leucocytes (WBC)=14.9x103/mm3, with left shift in the leucocyte formula, normal number of thrombocytes. Hepatic tests: GOT=63 U/l, GPT=25 U/l, normal renal function (urea=33 mg/dl, creatinine=0.65 mg/dl).
The orotracheal intubation and mechanical ventilation are decided upon immediately and the drug treatment process is initialized. The saturation level increases to 80% and hardly does it maintain at 90%. The pulmonary radiography (Fig.1) shows the infiltration of the left superior pulmonary lobe in an alveolar shape, with right and left pneumothorax and pneumomediastinum. After 24 hours (Fig.2) a bilateral pneumothorax occurs. The pulmonary parenchyma is collapsed in different degrees from left to the right, of average intensity, with a relatively homogenous structure. After the bilateral pleural drainage, the radiological image shows the remittance of the pneumothorax, but the left superior pulmonary area looks opacified (Fig.3).
Figure 1.

The opacification of the upper left pulmonary area having an alveolar characteristic. Right pneumothorax, mild left pneumothorax and pneumomediastinum
Figure 2.

Bilateral pneumothorax. Pneumomediastinum. The pulmonary parenchyma is colabated in various degrees, of medium intensity, with a relatively homogenous structure
Figure 3.

The opacification of the upper left pulmonary area. Upper pneumomediastinum. Pneumothorax to be remitted
7 days after the admission to intensive care, micronodular opacities are pointed out, grouped in the left pulmonary area adjacent to the left extremity of the cord (Fig.4). The patient was permanently assisted by a mechanical ventilator, she had a fever and despite the intensive general treatment and the intravenous antibiotherapy in accordance with the antibiogram (positive blood culture for staphylococcus aureus) the evolution was unfavorable. Death occurred 12 days since she was admitted to intensive care unit. We performed the autopsy, taking lung samples, and we histopathologically analyzed them through classical techniques, after a paraffin treatment, cutting, and hematoxylin-eosin coloring. We identified lesional polymorphism, with areas of fibroblastic proliferation (Fig.5); some alveoli contain reactive alveocytes, some of them binuclear (Fig.6), alternating with free lumen alveoli; in some of them we noticed the presence of macrophages with hemosiderin, macrophagic reaction (Fig.5); the bronchial lumens contain desquamated cells (Fig.7).
Figure 4.

Grouped, micronodular opacities with a confluence tendency within the left pulmonary area. Absent pneumothorax
Figure 5.
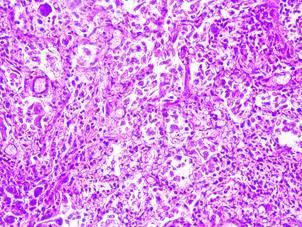
H-E coloring, ob. 20
Figure 6.
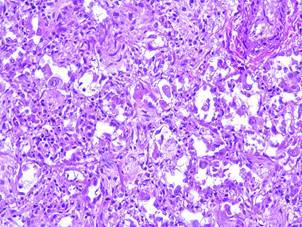
H-E coloring, ob. 20
Figure 7.
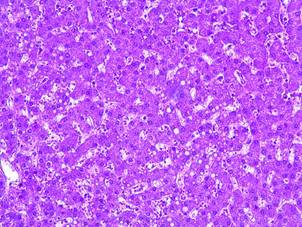
H-E coloring, ob. 40
Discussion
The hydrocarbon intoxication in children is encountered nowadays due to the easy access to these substances. The derivatives from petroleum distillates encompass aromatic hydrocarbons (containing benzene) and aliphatic compounds (with linear catena): methane gas, petrol, and mineral oils. The main toxic effects are given both by tegument irritations or those at the level of digestive or respiratory mucous membranes but also by the depressor character of the central nervous system. Through the aspiration of hydrocarbons the surfactant is inhibited and the alteration of the ventilation-perfusion nexus is produced with direct cytotoxic effect on the pulmonary capillaries and alveoli.
Out of all the toxic manifestations produced by aliphatic hydrocarbons, the most important are the pulmonary ones, having a low absorption in the intestinal tract. The physical properties of toxic products causing the action against organs are viscosity, volatility and the surface tension. The lower the viscosity the higher the risk for aspiration, with easier penetration within the tracheobronchial tract [7]. The increased volatility of the liquid substance produces its light evaporation reducing at the same time the level of oxygen and triggering the emergence of hypoxia.
In case of ingestion, the petroleum derivatives reach directly the lungs, but pneumonia is not given by the quantity of hydrocarbons absorbed at gastro-intestinal level [5]. The oily particles aspired into the airways do not stimulate the coughing reflex and they reach the inferior respiratory tract. The mucociliary clearance is perturbed and this fact prevents the evacuation of particles gathered in the alveolar macrophages [8].
The neurological manifestations are represented by coma in severe cases preceded by somnolence or cephalalgia, dizziness, ataxia and sometimes convulsions [9]. These are explained by both the hematogenous and digestive absorption of toxic substances as well as by the hypoxemia given by the pulmonary disorder.
The characteristic pulmonary lesions are either the hemorrhagic bronchopneumonia with galloping fatal evolution or the acute pulmonary edema. Lesions in general regress with minimum scar changes [10,11].
Among the hydrocarbon intoxication cases, it is considered that diesel fuel aspiration is unusual and less frequent [5]. The accidental ingestion of hydrocarbons accounts for 1-2% of the nondrug intoxications in children below the age of 6, as reported by a medical center in the US, [12] and 10% of the death rate in children, caused by the intoxication with a single substance. Gasoline and engine oil are mostly the ones to blame for. A study published in the US [13] shows that in 2013 out of 31031 cases of hydrocarbon intoxication, 9622 children below the age of 6 were affected, with 18 deaths (0.18%).
The circumstances in which hydrocarbon poisoning takes place in children below the age of 6 are dictated by the lack of monitoring from the family and low socio-economic level. The results of a study carried out at the Aga Khan University Hospital [4] showed that 75% of hospitalized cases belonged to low economic level communities and they were children with more than 3 brothers in a family. In 60% of cases, substances were kept in alcoholic or mineral water bottles. The morbidity and mortality given by the infant’s accidental ingestion exceed the ones given by the adults’ accidental inhaling, cutaneous exposure or suicidal.
With respect to the presented case, the unsupervised infant ingested an undetermined quantity of diesel and initially the family doesn’t go to the doctor for 24 hours. The infant’s admission to intensive care takes place after 36 hours following the emergence of the acute respiratory functional syndrome and the accentuated somnolence. The pulmonary radiography performed 24 hours after the exposure registered no changes but afterwards the acute respiratory symptomatology occurred with multiple complications (pneumothorax, pneumomediastinum) which remitted under pleural. The initially chemical pneumonia became mixed through bacterial overinfection with staphylococcus aureus (analyzed clinically, radiologically and through laboratory exams) leading to death after 12 days of energetic and complex treatment.
Following the autopsy, we did not identify lipidic cells at the lung level, as in most published cases in which death occurred. The little information in this respect suggests that toxic overexposure, received treatment and techniques used, resulted in the impossibility of the identification of lipid cells.
Conclusions
The accidental ingestion and hydrocarbon aspiration (gasoil) produces severe changes by directly affecting the pulmonary parenchyma which causes death. Going immediately to the hospital and initiating as soon as possible the treatment influences the evolution and can prevent death. In our case, death occurred as a result of the bacterial overinfection of an initially chemical pneumonia which resulted in a pneumothorax and pneumomediastinum, both remitted under pleural drainage.
We did not identify pulmonary lipoid cells during the histopathological examination because there passed too many days since the toxic exposure.
Acknowledgments
All authors equally contributed in the research and drafting of this paper.
References
- 1.Oliveira GA, Pessanha LB, Guerra LF, Martins DL, Rondina RG, Silva JR. Aspiration pneumonia in children: an iconographic essay. Radiol Bras. 2015;48(6):391–395. doi: 10.1590/0100-3984.2014.0007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sios SMA, Ferreira AS, Daltro PA, Caetano RL, Moreira JD, Quirico-Santos T. Evolution of exogenous lipoid pneumonia in children: clinical aspects, radiological aspects and the role of bronchoalveolar lavage. J Bras Pneumol. 2009;35:839–845. doi: 10.1590/s1806-37132009000900004. [DOI] [PubMed] [Google Scholar]
- 3.Nityanand Ramnarine. Hidrocarbons Toxicity. West J Emergy Med. 2008;9(3):165–165. [Google Scholar]
- 4.Siddiqui EU, Razzak JA, Naz F, Khan SJE. Factors associated with hydrocarbon ingestion in children. J Pak Med Assoc. 2008;58(11):608–612. [PubMed] [Google Scholar]
- 5.Mogoş Gheorghe, et al., editors. Intoxicaţiile acute – diagnostic şi tratament. Bucureşti: Ed. Medicală ; 1981. pp. 437–440. [Google Scholar]
- 6.Popescu Valeriu, et al., editors. Tratat de pediatrie. Vol. 3. Bucureşti: Ed. Medicală ; 1985. pp. 942–942. [Google Scholar]
- 7.Osterhoudt KC, Burns Ewald M, Shannon M, Henvetig FM, et al., editors. Toxicologie emergencies in Textbook of pediatric emergency medicine. 5. Philadelphia : 2006. pp. 951–951. [Google Scholar]
- 8.Hadda V, Khilnani GC. Lipoid pneumonia: An overview Expert. Rev Respir Med. 2010;4:799–807. doi: 10.1586/ers.10.74. [DOI] [PubMed] [Google Scholar]
- 9.Ulmeanu C, Niţescu Viorela, Ulmeanu Alex, et al., editors. Intoxicaţia cu produse petroliere. 32. Olteniţa: Tipografia Tridone ; 2015. Intoxicaţiile acute la copil şi adolescent; pp. 286–289. [Google Scholar]
- 10.Brander PE, Taskinen E, Stenius –Aarniala B. Fire-eater’s lung. Eur Resir J . 1992;5(1):112–114. [PubMed] [Google Scholar]
- 11.Ewert R, Lindemann I, Romberg B, Petri F, Witt C. the accidental aspiration and ingestion of petroleum in a fire eater. Dtsch Med Wochenschr . 1992;117(42):1594–1598. doi: 10.1055/s-2008-1062481. [DOI] [PubMed] [Google Scholar]
- 12.Watson WA, Litovitz TL, Rodgers GC Jr. Annual report of the American Association of Poison. 2002 [Google Scholar]
- 13.Lee DC. Hydrocarbons . In: Marx JA, Hockberger RS, Walls RM, et al., editors. Rosen’s Emergency Medicine Concepts and Clinical Practice. 8. 158 Philadelphia : Elsevier Saunders; 2014. [Google Scholar]


