Abstract
ABSTRACT: We present the case of an 18-month-old girl, from rural area, admitted to our clinic for fever and cough. The anamnestic data and the clinical and radiological examinations initially suggested the diagnosis of acute interstitial pneumonia. During hospitalization, she repeatedly presented exacerbations with acute respiratory failure, but without fever. Paraclinic examinations revealed anemia, leukocytosis, inflammatory tests with highly increased values, low values of serum iron and serum calcium, hyperproteinemia with hypergammaglobulinemia, the values of IgE and IgG being highly increased. Repeated pulmonary x-rays-peribronchovascular interstitial thickening, at the level of peri-and right infrahilar area. Medullary puncture-increased percentage of eosinophils in several stages of maturity, approximately 20%, normal values for the other medullary series, without atypical cells; the fingertip hemogram showed anemia, leukocytosis, eosinophilia. The diagnosis turned to a possible toxocariasis-atc anti toxocara canis=55.6 NTU. In the third week of hospitalization, the patient presented short crises of nonfebrile seizures. Normal CT and EEG brain. The child was discharged after 5 weeks, the diagnosis being severe toxocariasis with pulmonary and neurological manifestations; she was recommended an antiparasitary treatment and remained in our clinic's records.
Keywords: toxocariasis, child, pulmonary manifestations, seizures
Introduction
Toxocariasis is an infection produced by ingestion of embryonated eggs of Toxocara canis or Toxocara cati, parasites which can be found either in dogs or in cats. The mature parasites live in the intestines of the natural hosts and they eliminate their eggs through faeces. Infection in man occurs after coming into contact with contaminated soil or infected faeces of host animals [1,2].
Case Report
A girl, aged one year and six months, was admitted to the 2nd Pediatric Clinic in February 2015, with fever, cough, and rhinorrhea. The affection had its onset a day before the admission, with cough and rhinorrhea, being treated with Ibalgin. When admitted, she had fever: 38.5°C.
Heredocolateral antecedents: young, healthy parents, 2 healthy sisters of 8 and 7 years, respectively; no chronic diseases in the family.
Physiological antecedents: the third child, born full-term, with a normal evolution within pregnancy, normal birth, birth weight 2150g, L=48cm, no sufferance at birth, naturally fed for one month and a half, then artificially with Lactovit, diversified when 6 months; when 7 months she was fed with goat milk for three months, when 10 months she was given cow milk. When admitted, she received food from adult's meal. Steps were taken to prevent rickets and she was vaccinated according to the Ministry of Health immunization programme. She presented a corresponding psycho-motor development for her age.
Pathological antecedents: hospitalized once when one year of age for acute pneumonia.
Life conditions: a three-room house in the rural area, 5 persons, water from the fountain, wood heating.
When admitted: the patient presented fever (38.2°C), W=8kg, fair general state, pale teguments, perionasal cyanosis, frontal bossing, base-flared thorax, productive cough, mucous rhinorrhea, subcostal indrawing, polipnea (FR=32/min), lung stetacustic: bilateral subcrepitant rales, normal heart beats, AV=120b/min, soft and relaxed abdomen, liver with its lower margin at 2.5cm from the right costal margin, normal stool, hyperemic pharynx, no sign of meningeal irritation.
Investigations when admitted: Hb=8.3g%, T=562000/mm3, L=10800/mm3, NS=50%, Ly=45%, M=5%. VSH=115/130mm at 1/2 hours, protein C reactive=10mg/l, fibrinogen=405mg%. GPT=24U/l, GOT=29U/l, γGT=160U/l, calcemia=7mg%, sideremy=15mg/dl, alkaline phosphatase =163U/l, total serum protein=10.4g/dl, urea=10mg/dl, creatinine=0.44mg/dl, uric acid=2.09mg/dl, normal urine test, negative coproparasitary examination, normal abdominal ECHO.
Pulmonary X-ray (10.02.2015): peribronchovascular interstitial thickening, at the level of peri-and right infrahilar area (1).
Figure 1.
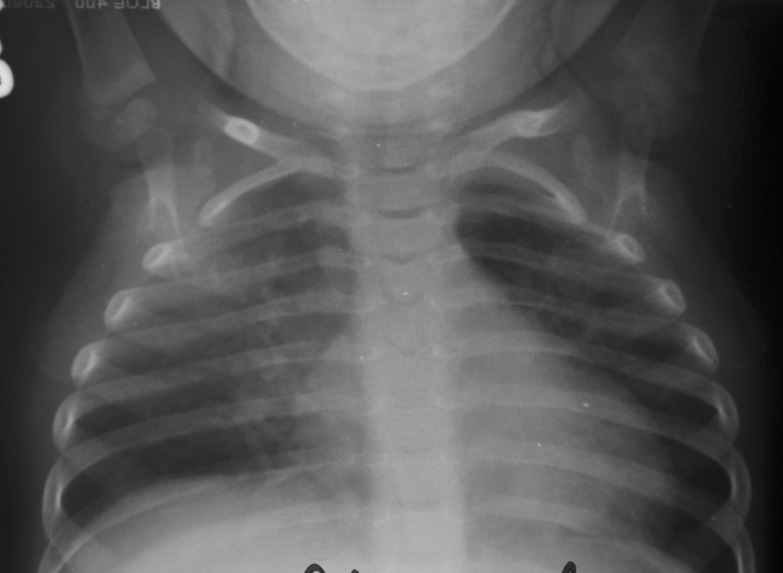
Pulmonary X-ray (10.02.2015)
We established the diagnosis: interstitial acute pneumonia. Acute respiratory failure. Dystrophy. Ferriprive anemia. Carential rickets. We started the treatment based on Sulcef, hydrocortisone hemisuccinate, DNF, and antipyretics.
Because both the inflammatory and the serum protein tests had high values, although the child was dystrophic, we went on with our investigations-electrophoresis of serum protein: total proteins=11.1g%, albumin/globulin=0.41, albumin=29.3g%, α1=2.9%, α2=9%, β=1%, γ=51.7%, monoclonal profile tendency within the gamma migration area. Immunogram: IgA=240.06mg/dl (N=70-400), IgM=214.4mg/dl (N=40-230), Ig G=5822.8mg/dl (N=700-1600), Ig E=4237UI/ml (N1-5 ani <60). The following investigations were repeated: hemogram: Hb=7g%, T=500000/mm3, L=17400/mm3, NS=67%, Ly=31%, M=2%, VSH=145/160mm at 1/2 hours, protein C reactive=90.6mg/dl, fibrinogen=597mg%. Pulmonary x-ray: peribronchovascular interstitial thickening, at the level of peri-and right infrahilar area (2).
Figure 2.
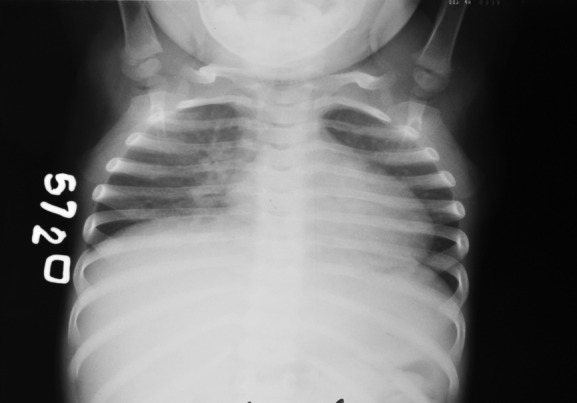
Pulmonary X-ray (16.03.2015)
The hemoglobin had lower values while the leukocytes registered higher values than the ones when admitted; the inflammatory tests also showed higher values. The initial radiologic aspect maintained. The increased values of the serum proteins, hypergammaglobulinemia and the highly increased values of Ig G and Ig E drew our attention.
We discussed the possibility of a malignant affection, of a collagenosis, of an intrauterine infection; therefore we continued our investigations: rheumatoid factor, antinuclear bodies, the absence of LE cells, normal values for the serum complement and the circulating immune complexes. Normal ECHO cord. Sweat test: EC=15mmol/l. Normal ophthalmologic examination and fundus examination, the absence of atg. HBS, atc. anti HVC, atc. anti HIV. Normal TORCH test.
The medullary puncture revealed rich marrow, all the medullary series being present. Normal maturation and differentiation for the granulocytic series, but with an increased percentage of eosinophils in several stages of maturation, 20%. The other series were normal, without atypical cells. The pulp of finger hemogram (performed at the same time with the medullary puncture) revealed Hb=7.9g%, T=420000/mm3, L=14000/mm3, NS=17%, E=36%, Ly=42%, M=5%, anisocytosis, hypochromia, poikilocytosis.
Since we registered increased values of the eosinophils in the marrow and at periphery, we thought of a possible toxocariasis. Therefore, we required an atc. IgG for Toxocara canis and cati, which proved to have highly increased values 55.6 NTU (<9 negative) for Toxocara canis.
At another anamnesis, the mother admitted that her daughter had played with puppies in the courtyard.
During hospitalization, the patient presented repeated cough episodes, expiratory dyspnea, polipnea, subcostal indrawing, groan, maintaining the radiologic aspect, things we considered to be pulmonary manifestations of toxocariasis. In the third week of hospitalization, the child presented brief afebrile seizures. The cranial CT scan and the EEG were normal. After the neurological examination, we considered the seizures as neurological manifestations of toxocariasis. It is possible to have, at neurological level, small lesions, which do not lead to EEG and CT changes.
On the basis of clinical evolution and performed investigations, we established a diagnosis: Severe toxocariasis with pulmonary and neurological manifestations. Ferriprive anemia. Carential rickets. Dystrophy. We started the treatment with Albendozol, hydrocortisone hemisuccinate, Aerius, Liv 52.
The child was discharged after 5 weeks, being recommended to repeat the Albendozol cures, and being given a treatment for the ferriprive anemia and carential rickets; the child remained in our pediatric clinic's records.
Discussion
Toxocariasis is a disease which mainly occurs in the children under five years of age [3]. The prevalence of the disease in children varies considerably around the world, being 1.6-23% in the USA, 57.5% in the Taiwan aboriginal children, while for the young children in Brasil, the frequency varies from 8.7 to 54.8% [4,5].
In man, the egg ingestion is followed by their hatching in the small intestine; then, the larvae migrate via the intestine wall to the liver, where they produce a granulomatous reaction associated with micro-abscess formation [3,5].
If the larvae pass through the filter of the liver, they will invade other organs: lung, kidney, cutaneous tissue [5].
Several factors can contribute to toxocariasis pathogenesis in human: inflammatory reactions caused by the presence of the larvae in tissues, the number of ingested eggs, the immune status of the host, the frequency of the larvae infusion, host getting sensitive to the antigens and the excretory /secretory products of the larvae. These antigens are a mixture of glycoproteins which include an allergic component TBA-1 [6]. In atopic patients, the severity of the disease is higher [6].
During the visceral migration stage, there occur eosinophilia and tissue necrosis. The major response of the host to the antigens at the level of Toxocara canis includes a marked eosinophilia and hypergammaglobulinemia with hyper IgE, as manifestations of the Th2 sublayer of lymphocytes T helper and of the cytokines secreted by these cells: IL5, IL10, Interferon γ [2,3,6].
There is evidence that the chronic presence of the parasitary antigens continuously stimulates the immune system of the host leading to a permanent immune alert, which may constitute the basis of recurrent manifestations at the level of lung or other organs [2,3].
Conclusions
Difficulty in establishing the diagnosis was due to the fact that the values of the sanguine eosinophilia (a constant sign of this affection) were not found in the repeated hemograms.
We considered it a severe form of Toxocariasis because of:
The young age of the child (one year and a half), with carential diseases and a deficiency in the nutritional state;
Severe and persistent pulmonary manifestations;
Afebrile seizures, as a cerebral manifestation of the disease;
Important inflammatory syndrome;
Intense immune response with hypergammaglobulinemia and hyper Ig E.
Acknowledgments
All authors equally contributed in the research and drafting of this paper.
References
- 1.Rodica Hodnea, Corina Constantin, Ioana Iftimie Nastase, Carmen Cretu. Un caz de larve migrans visceralis cu manifestari leucemice la un copil prescolar. Revista Romana de Boli Infectioase. 2011;14(4):223–226. [Google Scholar]
- 2.Ellaine AAC, Regina L. Toxocariasis, visural larva migrans in children. J. Pediatric (Rio J) 2011;87(2):100–110. [Google Scholar]
- 3.D Matei, I Gherghina, Eliza Cinteza. Infestatia cu toxocara canis la copil. Practica Medicala. 2006;1(1-2):35–39. [Google Scholar]
- 4.Despammier D. Toxocariasis clinical aspects, epidemiology, medical, ecology and molecular aspects. Clin. Microbiol. Rev. 2000;16(2):2615–2672. doi: 10.1128/CMR.16.2.265-272.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Santarem V. A., Lole F. N, Rubinsky, Elefant G, Ginfinda R., Protective and risk factors for toxocariasis in children from two diferent social classes et Brazil. Rev. Inst. Med. Txop. Sao-Paulo. 2011;53(2):66–72. doi: 10.1590/s0036-46652011000200002. [DOI] [PubMed] [Google Scholar]
- 6.K Mazur-Melewska, K Jonczyk, A Modlinska-Cwalinska, M Figlerowicz, W Sluzewski. Visceral larva migrans syndrome: analysis of serum cytokine levels in children with hepatic lesions confirmed in radiological findings. Parasite Immunology. 2014;36(12):668–773. doi: 10.1111/pim.12143. [DOI] [PubMed] [Google Scholar]


