Abstract
Objective
To investigate the occurrence of ankylosing spondylitis (AS)-related sick leave (SL) over 6 12 years and explore factors predicting first and recurrent SL.
Methods
Data from employed patients from the Outcome in Ankylosing Spondylitis International Study were used. At each visit, patients indicated the occurrence of SL (yes/no) in the previous inter-assessment period. Cox regressions predicted a first episode of SL. Generalised estimating equations (GEE) explored the association between SL and (time-lagged) predictors. To investigate whether SL predicts new SL, SL in the first year was included as covariate in a separate analysis.
Results
139 patients (76% males, mean (SD) age 38.7 (10.0) years) were at risk for SL for an average period of 7.9 years, of whom 88 (63%) reported any SL. In both the Cox baseline predictors model (HR (95% CI)) and the time-varying GEE models (OR (95% CI)), AS Disease Activity Score (1.67, 1.23 to 2.28 (HR); 1.48, 1.07 to 2.03 (OR)); Bath AS Disease Activity Index (1.33, 1.18 to 1.51 (HR); 1.31, 1.15 to 1.49 (OR)), Bath AS Functional Index (1.17, 1.02 to 1.34 (HR); 1.31, 1.16 to 1.47 (OR)) and comorbidity at baseline (GEE only, 1.52, 1.00 to 2.29 (OR)) were associated with SL in separate models, but only in patients with low educational attainment. SL in the first year was an independent predictor of SL over time (OR: 2.62 to 8.37 in different models, all p<0.05).
Conclusion
Disease activity and physical function predicted first and recurrent SL, but only in patients with low educational attainment. Prior SL results in future SL, and SL should therefore be a signal for support to prevent future adverse work outcome.
Keywords: ankylosing spondylitis, sick leave, absenteeism, longitudinal
Key messages.
What is already known about this subject?
While the adverse impact of ankylosing spondylitis (AS) on employment has been well studied, data on the course of sick leave over time are mainly lacking.
Limited evidence suggests a role of disease-related as well as contextual factors in the occurrence of sick leave in AS.
What does this study add?
Over the course of 12 years, 63% of patients at risk experience at least one episode of sick leave and almost half (45%) experience recurrent sick leave.
Disease-related factors only predict sick leave in patients with low level of education, and recent sick leave independently predicts future sick leave in all patients.
How might this impact on clinical practice?
Patients with lower educational attainment and those who already experienced sick leave require additional support in their work role.
Introduction
Symptoms of ankylosing spondylitis (AS) usually arise in young adulthood, thereby affecting patients’ ability to pursue their professional career and participate sustainably in the labour force.1–6 Previous observational research on worker participation in AS mainly focused on the magnitude and determinants of work disability.3–5 However, understanding sick leave (SL) might be even more important. First, sick leave is in itself a relevant outcome. For society, the indirect costs associated with sick leave and work disability due to AS have been shown to be at least as high as direct costs.7 Besides, patients with a musculoskeletal disease indicated absenteeism had a negative effect on psychological well-being and self-esteem.8 Second, recurrent and/or prolonged sick leave may serve as an indicator of future adverse work outcomes such as reduced career prospects or eventually work loss.
Only few studies have investigated determinants of sick leave in AS.1 9–13 Biomedical factors that have been identified include higher self-reported active disease and depressive symptoms,11 worse functional status,1 13 concomitant peripheral joint disease10 and higher level of pain.13 In addition, contextual factors, defined by the WHO as factors that are outside the disease, can influence outcomes such as sick leave. These can be personal (eg, sex, age, education) and environmental factors (eg, relationships with others, health services, social security).14 Previous studies showed that lower educational attainment, helplessness, job type (physical load) and social security regulations are associated with sick leave.9 10 12 However, a recent review concluded that evidence was weak, as only few studies were available.15 Finally, the role of sick leave itself as a potential predictor of recurrent sick leave has never been explored in AS. If such an association is found, both patients and society could benefit from this signal, reducing repeated or long-term sick leave and perhaps work disability.
In order to support a causal role of potential factors in relation to sick leave, longitudinal data are mandatory, especially when it allows time-dependent variation of potential predictors. This is particularly relevant as some factors (such as disease activity) might have short-term influence on the occurrence of sick leave, while other factors (such as contextual factors) are rather long-term determinants.
The aim of the present study was to investigate patterns in AS-related sick leave over an extended follow-up period and to investigate which factors, disease-related and contextual, can predict or explain sick leave over time. We hypothesised that contextual factors, specifically education, job type and country of residence, predict and explain sick leave independently of disease characteristics and that the association between disease activity and sick leave would emerge when exploring shorter time-intervals between clinical assessment and the occurrence of sick leave. Furthermore, we expected sick leave to be an independent predictor for future sick leave.
Methods
Patient population
Data from the Outcome in AS International Study (OASIS) were used. OASIS is a multinational prevalence cohort, initiated in 1996 and concluded in 2015. In total, 217 consecutive patients with AS who met the modified New York Criteria were recruited from the Netherlands, Belgium and France from September 1996 through March 1997.16 All patients were treated by their rheumatologists according to standard care. Biological treatment was available on indication since 2002. All patients signed informed consent.
Demographic characteristics and outcome assessment
Information about age, gender, highest level of education attained (dichotomised as higher professional/university versus any other (lower) educational level), human leucocyte antigen B27 (HLA-B27) status, duration of symptoms, presence of physician-confirmed extra-articular manifestations (EAMs: psoriasis, inflammatory bowel disease (IBD) and anterior uveitis) and radiographic hip involvement was collected at baseline. Using clinical records, the Rheumatic Disease Comorbidity Index (RDCI) at baseline was calculated with a theoretical score of 0–9, representing a weighted sum score of common comorbidities.17 18
Clinical outcomes were assessed every 6 months during the first 2 years of follow-up, every year until 6 years of follow-up, and every 2 years thereafter. Disease activity was measured with the Bath AS Disease Activity Index (BASDAI),19 the AS Disease Activity Score with C reactive protein (ASDAS-CRP)20 and laboratory tests (erythrocyte sedimentation rate (ESR) and CRP). Physical function was assessed by the Bath AS Functional Index (BASFI).21 Severity of axial- and peripheral pain experienced during the last week was assessed with two single item globals (0–10; higher being worse). The Bath AS Global Score (BAS-G) was used for global assessment of the patient’s well-being.22 Physician’s global assessment of disease activity was assessed by a single item global (0–10; higher being worse). The Bath AS Metrology Index (BASMI, linear algorithm) was used to assess spinal mobility.23 24 Radiographic damage of the spine was evaluated every 2 years with the modified Stoke AS Spine Score (mSASSS),25 26 and scores represent the average of two trained readers.27 Information about pharmacological treatment (use of non-steroidal anti-inflammatory drugs (NSAIDs), conventional synthetic disease-modifying antirheumatic drugs (csDMARDs) and biologicals) was retrieved at every visit. Use of NSAIDs was converted into the Assessment of SpondyloArthritis international Society (ASAS) NSAID score.28
Work-related outcome and job type
Patients completed questionnaires assessing work status, and in those employed job type (eight categories) and work hours per week every 6 months during the first 2 years of follow-up, every year until 6 years of follow-up, and every 2 years thereafter, until year 12. Working 33 hours or more per week was considered full-time work. Job type was dichotomised into two types: white-collar worker (administrative, scientific and managerial professions) and blue-collar workers (industrial, commercial, servicing, transportation and agricultural professions).29 30 No other data on work contextual factors were collected. Patients with paid work could indicate whether they had experienced AS-related sick leave, without a minimum duration, since last visit and this happened every 2 months during the first 2 years of follow-up, annually until 6 years of follow-up and every 2 years thereafter.
Statistical analysis
Analyses included only patients ‘at risk for sick leave’, that is, patients working at baseline as well as those who started or resumed work during follow-up. Patients were considered to be ‘at risk for sick leave’ from the first assessment they reported to be working (which was not necessarily the baseline assessment of OASIS), and this assessment was used as baseline in all analyses. Patients were censored if they stopped working, became fully work disabled, retired or at the end of follow-up. Patients with evidence of long-term sick leave at entry into the cohort, based on their response to the questionnaire, were excluded from all analyses.
Baseline characteristics and description of sick leave
Baseline characteristics of patients with work were described and compared between those reporting ‘ever’ or ‘never’ sick leave during follow-up using independent t-test, Mann-Whitney test or Chi square test, as appropriate. For small samples (expected count<5), Fisher’s exact test was used.
Factors associated with sick leave over time
Both time-to-first-event and recurrent event analyses were performed. Eventually, three models were computed (online supplementary figure 1). Model 1 is a baseline predictor model exploring time-dependent risk for the first event of sick leave (using Cox regression). Model 2 is a ‘time-varying predictor’ model, allowing explanatory factors to vary over time and exploring association with recurrent events of sick leave (using generalised estimating equations (GEE)). Given the number of missing data on sick leave, GEE (which can handle missing data without losing the entire patient from the analysis) with discrete time points was preferred over Cox recurrent event regression.31 Model 3 was an extension of model 2, with the aim of investigating whether sick leave predicts recurrent sick leave. In this model, the baseline was shifted to the assessment after 1 year of being at risk for sick leave, and sick leave in the first year of being at risk was included as a dichotomised covariate.
rmdopen-2018-000766supp002.tif (2.4MB, tif)
In the base-case of the time-varying models, a 1-year time-lag period was chosen for the time-varying variables, as any longer period was considered less plausible to influence sick leave. Consequently, only data for the first 6 years could be used as further assessments took place every 2 years. To check the possible influence of a shorter or longer time-lag period, two additional (sensitivity) analyses were carried out. First, a 6-month time-lag period was used, in which only data for the first 2 years could be used and second, a 2-year time-lag period was used using all available follow-up data, that is, 12 years. Of note, for the main time-lagged analyses, the 2-monthly sick leave assessments during the first 2 years of follow-up were aggregated into periods of 1 year (1 year time-lag analysis) to harmonise with later assessment periods.
Modelling strategy and variable selection
Variables that could potentially explain or predict sick leave were categorised into four variable groups (‘blocks’): (1) sociodemographics (age, gender (male), country of origin, education, job type, part-time work status), (2) disease characteristics (symptom duration, HLA-B27 positivity, presence of each EAM, RDCI, smoking, ASAS NSAID score, csDMARD use), (3) disease activity (BASDAI, CRP, ESR, ASDAS-CRP, physician global, axial pain, peripheral pain) and (4) function and damage (BASFI, BASMI, mSASSS). Exploratory analysis revealed that the number of observations with time-lagged biological use over time was low (less than 1%). Biological use was therefore not included as potential predictor.
Variables in the final models were selected in steps. All variables of interest were first analysed individually, while adjusting for age and gender. Variables with p<0.20 or confounding variables, which changed the coefficient of sex and/or age>10% on inclusion in the model, were retained and subsequently analysed within their variable block using a manual forward method. Variables significantly associated with the outcome (p<0.05) within each variable block were retained and finally all variable blocks were tested together. Variables that lost significance on inclusion of variables from other blocks were removed from the model using a backward manual method, except for age and gender which were always retained in the model. Collinearity between covariates was checked for in each step, and relevant interactions between the variables were explored both within and between variable blocks (p<0.10 used as threshold for interactions). If analyses had to be stratified due to significant interactions, variables as selected in the total sample were used in the strata. This ensured comparability of results between strata. Analyses were performed using SPSS V.23.0 (IBM, Armonk, New York, USA) and Stata SE Release 14.0 (StataCorp, College Station, Texas, USA).
Results
Description of sick leave and baseline characteristics
Of the 216 valid patients in OASIS, 141 (65%) were at risk for sick leave, of which 2 were excluded due to self-reported long-term sick leave at baseline. In the remaining 139 patients, the average age was 38.7 (SD 10.0) years and average symptom duration 16.4 (SD 8.9) years. At inclusion in OASIS, 121 (87%) patients were employed, while 18 (13%) started or resumed work during follow-up.
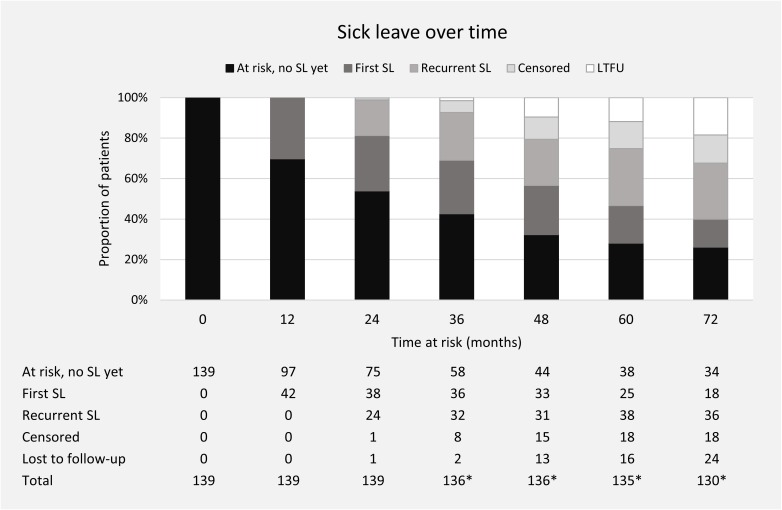
The median time at risk for (recurrent) sick leave among the 139 patients was 84 (IQR 48–144) months. On average, a patient completed 77% of the assessments for sick leave during the period at risk. Among the 88 patients (63%) who ever reported sick leave, 62 (70%) reported sick leave at more than one assessment and 35 (40%) reported sick leave at more than three assessments. The majority of first sick leave events (62/88 [70%]) occurred during the first 2 years of being at risk for sick leave. The number of patients at risk for SL after 2, 4, 6, 8, 10 and 12 years was 137, 108, 88, 68, 63 and 56, respectively. Figure 1 shows the number of patients at risk for sick leave and the occurrence of first and recurrent sick leave over time during the first 6 years.
Figure 1.
Distribution of first and recurrent sick leave episodes over time in the study population at risk. No SL yet=those who are at risk for sick leave, but have not incurred any sick leave (yet). First SL=those who reported SL for the first time during follow-up, in the previous interval or before. Recurrent SL=those who reported SL for the second time during follow-up, in the previous interval or before. Censored=censored from analyses due to reasons of job loss, unemployment, work disability, retirement. Lost to follow-up=patients that were lost to follow-up. *Due to the design of OASIS (annual assessments until month 72, thereafter every 2 years), annual assessments were not always available for those who became at risk for SL during follow-up. AS, ankylosing spondylitis; LTFU, lost to follow-up; OASIS, Outcome in Ankylosing Spondylitis International Study; SL, ankylosing spondylitis-related sick leave.
Compared with patients who never reported sick leave during follow-up, those who ever reported sick leave were more likely to be lower educated and more likely to have a blue collar job type (table 1). There were no other significant differences in baseline characteristics or time at risk for sick leave between these two groups.
Table 1.
Baseline* characteristics of the total study population at risk for sick leave and for the patients with and without sick leave separately
| Variable | Total group | Ever sick leave§ | Never sick leave§ | P values** |
| (n=139) | (n=88) | (n=51) | ||
| Age, years | 38.7 (10.0) | 37.9 (9.6) | 40.3 (10.6) | 0.18 |
| Gender, male (%) | 105 (75.5) | 68 (77.3) | 37 (72.5) | 0.53 |
| Country of origin | 0.23 | |||
| The Netherlands (%) | 74 (53.2) | 51 (58.0) | 23 (45.1) | |
| Belgium (%) | 45 (32.4) | 24 (27.3) | 21 (41.2) | |
| France (%) | 20 (14.4) | 13 (14.8) | 7 (13.7) | |
| Education, high (%) | 49 (36.0) | 23 (27.1) | 26 (51.0) | <0.01 |
| Job type, white collar (%) | 71 (55.9) | 38 (48.1) | 33 (68.8) | 0.02 |
| Part-time worker (%) | 22 (15.9) | 11 (12.6) | 11 (21.6) | 0.17 |
| Partial work disability (%) | 19 (13.8) | 14 (16.1) | 5 (9.8) | 0.30 |
| Age at onset symptoms, years | 22.1 (7.5) | 21.5 (7.4) | 23.1 (7.7) | 0.25 |
| Duration of symptoms, years | 16.4 (8.9) | 16.2 (8.3) | 16.7 (10.1) | 0.79 |
| HLA-B27 positive (%) | 112 (83.6) | 70 (81.4) | 42 (87.5) | 0.36 |
| Comorbidity index (RDCI)† | 0.2 (0.5) | 0.2 (0.5) | 0.1 (0.3) | 0.11 |
| Cardiovascular disease (%) | 7 (5.0) | 6 (6.8) | 1 (2.0) | |
| Diabetes mellitus (%) | 1 (0.7) | 1 (1.1) | 0 (0.0) | |
| Fracture (%) | 5 (3.6) | 4 (4.5) | 1 (2.0) | |
| Depression (%) | 1 (0.7) | 1 (1.1) | 0 (0.0) | |
| Gastrointestinal disease (%) | 6 (4.3) | 5 (5.7) | 1 (2.0) | |
| History of IBD (%) | 7 (5.1) | 5 (5.7) | 2 (4.0) | 1.00 |
| History of psoriasis (%) | 8 (5.8) | 6 (6.8) | 2 (4.0) | 0.71 |
| History of AAU (%) | 22 (15.9) | 14 (15.9) | 8 (16) | 0.99 |
| Hip involvement (%)† | 26 (18.8) | 16 (18.4) | 10 (19.6) | 0.86 |
| Medication use, current‡ | ||||
| NSAID (%) | 101 (72.7) | 66 (75) | 35 (68.6) | 0.42 |
| ASAS NSAID score | 62.5 (53.8) | 64.6 (53.2) | 58.6 (55.3) | 0.45 |
| csDMARDs (%) | 15 (10.8) | 8 (9.1) | 7 (13.7) | 0.40 |
| Smoking, current (%) | 41 (39.4) | 27 (39.7) | 14 (38.9) | 0.94 |
| CRP, mg/L | 15.3 (19.5) | 16.2 (17.6) | 13.9 (22.3) | 0.07 |
| Elevated CRP (%)¶ | 48 (36.1) | 33 (40.2) | 15 (29.4) | 0.21 |
| ESR, mm/hour | 12.3 (12.1) | 11.3 (10.1) | 14.0 (14.7) | 0.42 |
| ASDAS-CRP | 2.5 (0.9) | 2.6 (0.9) | 2.3 (1.0) | 0.06 |
| BASDAI (0–10) | 2.9 (1.8) | 3.0 (1.9) | 2.7 (1.7) | 0.27 |
| BASFI (0–10) | 2.4 (2.0) | 2.6 (2.1) | 2.1 (1.9) | 0.22 |
| Back pain (0–10) | 3.2 (2.2) | 3.4 (2.1) | 2.9 (2.2) | 0.16 |
| BAS-G (0–10) | 3.4 (2.4) | 3.4 (2.3) | 3.5 (2.6) | 0.84 |
| Swollen joint count (0–44) | 0.5 (1.5) | 0.4 (1.5) | 0.5 (1.5) | 0.60 |
| Tender joint count (0–53) | 1.8 (3.3) | 2.0 (3.5) | 1.5 (2.9) | 0.19 |
| BASMI (0–10) | 3.4 (1.5) | 3.5 (1.5) | 3.2 (1.5) | 0.27 |
| mSASSS (0–72) | 7.0 (11.0) | 7.5 (12.0) | 6.0 (9.3) | 0.87 |
Values expressed as mean (SD) unless otherwise stated.
*Data from the first assessment in which patients reported to be working were used as baseline variables.
†Only assessed at baseline.
‡No patients used biologicals at baseline (first assessment in which they reported to be working).
§Ever sick leave; patients who reported sick leave at least once during upto 12 years of follow-up. Never sick leave; patients who never reported sick leave during upto 12 years of follow-up. Note that some of these patients became lost to follow-up or were censored over time (see figure 1).
¶Elevated CRP defined as CRP>10mg/L.
**Two-tailed ever sick leave vs never sick leave.
AAU, acute anterior uveitis; AS, ankylosing spondylitis; ASAS, Assessment of SpondyloArthritis international Society; ASDAS, AS Disease Activity Score; BASDAI, Bath AS Disease Activity Index; BASFI, Bath AS Functional Index; BAS-G, Bath AS Global Score; BASMI, Bath AS Metrology Index; CRP, C reactive protein; ESR, erythrocyte sedimentation rate; HLA-B27, human leucocyte antigen B27; IBD, inflammatory bowel disease; NSAID, non-steroidal anti-inflammatory drug; RDCI, Rheumatic Diseases Comorbidity Index; csDMARD, conventional synthetic disease-modifying antirheumatic drug; mSASSS, modified Stoke Ankylosing Spondylitis Spine Score.
Factors associated with sick leave
Tables 2, 3 and 4 present the results of the multivariable models predicting or explaining SL over time. The results of univariable analyses are shown in online supplementary tables 1& 2. Correlation/collinearity was found between education and job type (variables belonging to group 1), between ASDAS, BASDAI and BASFI (groups 3/4) and between education and BASDAI/ASDAS/BASFI (groups 1/3/4). For the final models, education was selected over job type because of robustness of the association with the outcome. For ASDAS, BASDAI and BASFI, it was decided to perform three separate analyses. As an interaction was observed between education and ASDAS, BASDAI and BASFI, all models were stratified for low and high educational attainment.
Table 2.
Multivariable Cox regression models exploring baseline predictors of first sick leave over 12 years for male patients with AS, stratified by level of education
| Variable* | High educational attainment, male patients only | Low educational attainment, male patients only | ||||||||||
| Model ASDAS (n=34) | Model BASDAI (n=35) | Model BASFI (n=33) | Model ASDAS (n=62) | Model BASDAI (n=65) | Model BASFI (n=64) | |||||||
| HR | 95% CI | HR | 95% CI | HR | 95% CI | HR | 95% CI | HR | 95% CI | HR | 95% CI | |
| Age, years | 0.98 | 0.92 to 1.04 | 0.98 | 0.93 to 1.03 | 1.00 | 0.95 to 1.05 | 1.04 | 1.00 to 1.08 | 1.04 | 1.00 to 1.07 | 1.01 | 0.97 to 1.05 |
| ASDAS-CRP | 0.92 | 0.59 to 1.45 | 1.67 | 1.23 to 2.28 | ||||||||
| BASDAI | 0.81 | 0.60 to 1.10 | 1.33 | 1.18 to 1.51 | ||||||||
| BASFI | 0.59 | 0.32 to 1.07 | 1.17 | 1.02 to 1.34 | ||||||||
Due to correlation/collinearity between ASDAS, BASDAI and BASFI, it was decided to perform three separate analyses for these variables.
Procedure of variable selection: (1) P≥0.20 in univariable analysis and no confounder: country of origin, part-time worker, symptom duration, hip involvement, IBD, uveitis, NSAID index, csDMARD use, CRP, ESR, BAS-G, peripheral pain, swollen joint count. (2) P<0.20 in univariable analysis and/or a confounder for sex or age, but not significant within variable group: (group 1) job type; (group 2) comorbidity index, HLA-B27, psoriasis, smoking; (group 3) axial pain (ASDAS and BASDAI model), physician global, tender joint count; (group 4) BASMI, mSASSS. (3) Statistically significant within variable group, but not when included in final model: axial pain (BASFI model). (4) Excluded from analysis: CRP/ESR (excluded from ASDAS model due to overlap with ASDAS).
*Baseline values were used for all variables in this analysis.
AS, ankylosing spondylitis; ASDAS, AS Disease Activity Score; BASDAI, Bath AS Disease Activity Index; BASFI, Bath AS Functional Index; BAS-G, Bath AS Global Score; CRP, C reactive protein; ESR, erythrocyte sedimentation rate; HLA-B27, human leucocyte antigen B27; IBD, inflammatory bowel disease; NSAID, non-steroidal anti-inflammatory drug; csDMARD, conventional synthetic disease-modifying antirheumatic drug; mSASSS, modified Stoke Ankylosing Spondylitis Spine Score.
Table 3.
Multivariable GEE models exploring determinants of sick leave over 6 years, stratified by level of education
| Variable | High educational attainment | Low educational attainment | ||||||||||
| Model ASDAS (n=46) | Model BASDAI (n=46) | Model BASFI (n=46) | Model ASDAS (n=82) | Model BASDAI (n=85) | Model BASFI (n=85) | |||||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Gender, male | 0.40 | 0.13 to 1.21 | 0.34 | 0.11 to 1.04 | 0.38 | 0.13 to 1.11 | 1.14 | 0.48 to 2.75 | 1.08 | 0.48 to 2.46 | 1.06 | 0.48 to 2.32 |
| Age, years | 0.98 | 0.94 to 1.03 | 0.98 | 0.94 to 1.03 | 0.99 | 0.94 to 1.04 | 1.00 | 0.96 to 1.04 | 0.99 | 0.96 to 1.02 | 0.98 | 0.95 to 1.02 |
| Comorbidity (RDCI) | 1.58 | 0.34 to 7.38 | 1.52 | 1.00 to 2.29 | ||||||||
| ASDAS-CRP* | 0.74 | 0.44 to 1.25 | 1.48 | 1.07 to 2.03 | ||||||||
| BASDAI* | 0.78 | 0.58 to 1.06 | 1.31 | 1.15 to 1.49 | ||||||||
| BASFI* | 0.85 | 0.57 to 1.26 | 1.31 | 1.16 to 1.47 | ||||||||
Due to correlation/collinearity between ASDAS, BASDAI and BASFI, it was decided to perform three separate analyses for these variables.
Procedure of variable selection: (1) P≥0.20 in univariable analysis and no confounder: country of origin, symptom duration, HLA-B27, hip involvement, IBD. (2) P<0.20 in univariable analysis and/or a confounder for sex or age, but not significant within variable group: (group 1) job type; (group 2) psoriasis, uveitis, smoking, NSAID index, csDMARD use; (group 3) BAS-G, axial pain (ASDAS and BASDAI model), peripheral pain, physician global (ASDAS and BASDAI model), swollen joint count, tender joint count (ASDAS and BASDAI model); (group 4) BASMI, mSASSS. (3) Statistically significant when tested within variable group, but not when included in final model: part-time worker, comorbidity index (ASDAS and BASFI model), axial pain (BASFI model), physician global (BASFI model), tender joint count (BASFI model). (4) Excluded from analysis: CRP/ESR (excluded from ASDAS model due to overlap with ASDAS).
*Time-lagged variables (1 year time-lag).
AS, ankylosing spondylitis; ASAS, Assessment of SpondyloArthritis international Society; ASDAS, AS Disease Activity Score; BASDAI, Bath AS Disease Activity Index; BASFI, Bath AS Functional Index; BAS-G, Bath AS Global Score; BASMI, Bath AS Metrology Index; CRP, C reactive protein; ESR, erythrocyte sedimentation rate; GEE, generalised estimating equation; HLA-B27, human leucocyte antigen B27; IBD, inflammatory bowel disease; NSAID, non-steroidal anti-inflammatory drug; RDCI, Rheumatic Diseases Comorbidity Index; csDMARD, conventional synthetic disease-modifying antirheumatic drug; mSASSS, modified Stoke Ankylosing Spondylitis Spine Score.
Table 4.
Multivariable GEE models exploring past sick leave as a predictor for recurrence of sick leave over 6 years, stratified by level of education
| Variable | High educational attainment | Low educational attainment | ||||||||||
| Model ASDAS (n=46) | Model BASDAI (n=46) | Model BASFI (n=46) | Model ASDAS (n=82) | Model BASDAI (n=85) | Model BASFI (n=85) | |||||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Gender, male | 0.93 | 0.23 to 3.82 | 0.88 | 0.21 to 3.72 | 0.85 | 0.20 to 3.49 | 0.79 | 0.27 to 2.31 | 0.73 | 0.25 to 2.10 | 0.70 | 0.25 to 2.01 |
| Age, years | 0.98 | 0.93 to 1.04 | 0.98 | 0.93 to 1.04 | 0.99 | 0.93 to 1.04 | 0.97 | 0.93 to 1.01 | 0.96 | 0.92 to 1.01 | 0.96 | 0.92 to 1.01 |
| Comorbidity (RDCI) | 1.55 | 0.16 to 14.95 | 1.35 | 0.17 to 10.56 | 1.58 | 0.21 to 11.83 | 1.98 | 1.14 to 3.43 | 2.04 | 1.22 to 3.42 | 1.87 | 1.10 to 3.16 |
| ASDAS-CRP* | ‡ | ‡ | ||||||||||
| BASDAI* | 0.77 | 0.46 to 1.28 | 1.27 | 1.07 to 1.51 | ||||||||
| BASFI* | 0.84 | 0.53 to 1.34 | 1.26 | 1.06 to 1.49 | ||||||||
| BAS-G* | 0.93 | 0.64 to 1.35 | 1.20 | 1.04 to 1.39 | ||||||||
| Early SL, yes† | 8.37 | 1.26 to 55.81 | 8.20 | 1.24 to 54.17 | 7.41 | 1.17 to 46.95 | 2.93 | 1.26 to 6.81 | 2.91 | 1.31 to 6.48 | 2.62 | 1.10 to 6.22 |
Due to correlation/collinearity between ASDAS, BASDAI and BASFI, it was decided to perform three separate analyses for these variables.
Procedure of variable selection: (1) P≥0.20 in univariable analysis and no confounder: symptom duration, HLA-B27, IBD, psoriasis, uveitis, NSAID index, CRP, mSASSS. (2) P<0.20 in univariable analysis and/or a confounder for sex or age, but not significant within variable group: (group 1) country of origin, job type; (group 2) hip involvement, smoking, csDMARD use; (group 3) ESR (BASDAI model), axial pain, peripheral pain, physician global, swollen joint count, tender joint count (ASDAS and BASDAI model); (group 4) BASMI. (3) Statistically significant when tested within variable group, but not when included in final model: part-time worker, ESR (BASFI model), tender joint count (BASFI model). (4) Excluded from analysis: ESR (excluded from ASDAS model due to overlap with ASDAS).
*Time-lagged variables (1 year time-lag).
‡Forced into model, but not statistically significant.
†Defined as occurrence of sick leave during the first year of follow-up.
AS, ankylosing spondylitis; ASAS, Assessment of SpondyloArthritis international Society; ASDAS, AS Disease Activity Score; BASDAI, Bath AS Disease Activity Index; BASFI, Bath AS Functional Index; BAS-G, Bath AS Global Score; BASMI, Bath AS Metrology Index; CRP, C reactive protein; ESR, erythrocyte sedimentation rate; GEE, generalised estimating equation; HLA-B27, human leucocyte antigen B27; IBD, inflammatory bowel disease; NSAID, non-steroidal anti-inflammatory drug; RDCI, Rheumatic Diseases Comorbidity Index; SL, ankylosing spondylitis-related sick leave; csDMARD, conventional synthetic disease-modifying antirheumatic drug; mSASSS, modified Stoke Ankylosing Spondylitis Spine Score.
rmdopen-2018-000766supp001.docx (26KB, docx)
In the Cox regression baseline prediction model (model 1, using 12 years of follow-up), an additional interaction between gender and disease activity entailed further stratification for gender (table 2). In view of small sample size of the female subgroups (n=20 for low education, n=14 for high education), only the results for male subgroups (with high vs low education) are presented. While in male patients with a low level of education, higher baseline ASDAS (HR=1.67, 95% CI 1.23 to 2.28), BASDAI (HR=1.33, 95% CI 1.18 to 1.51) and BASFI (HR=1.17, 95% CI 1.02 to 1.34) were associated with increased hazard for first sick leave, in male patients with high level of education, no significant associations with any predictor were observed.
The 1-year time-lag time-varying GEE analyses (model 2, using 6 years of follow-up) revealed for patients with low education an association over time between higher ASDASlag-1yr (OR=1.48, 95% CI 1.07 to 2.03), higher BASDAIlag-1yr (OR=1.31, 95% CI 1.15 to 1.49) or higher BASFIlag-1yr (OR=1.31, 95% CI 1.16 to 1.47) and odds of sick leave during the next year, all in separate analyses (table 3). In addition, in the BASDAI model, higher comorbidity scores at baseline predicted sick leave at any future time point (OR=1.52, 95% CI 1.00 to 2.29). In contrast, in those with high education, no association between either disease activity or physical function and sick leave was seen (table 3). Sensitivity analyses using a 6-month time-lag (using 2 years of follow-up) or 2-year time-lag (using 12 years of follow-up) yielded similar results. Of note, the effect of the association between ASDAS (and to a lesser extent BASDAI and BASFI) and sick leave was stronger when using a shorter (6 month) time-lag and weaker when using a longer (2 year) time-lag (online supplementary tables 3 and 4).
When including sick leave during the first year at risk (SL1st-year) as a covariate in the GEE (model 3, using 6 years of follow-up), SL1st-year was consistently associated with sick leave over time, both in those with low and with high educational attainment. The strength of this association was not significantly different between both educational groups (p value interaction SL1st-year*education=0.63). In addition, only in those with low education, comorbidities at baseline, BASDAIlag-1yr and BASFIlag-1yr, but not ASDASlag-1yr, were significantly associated with future sick leave (table 4). Of note, in the ASDAS model, BAS-G emerged as a significant variable associated with future sick leave, while ASDAS itself was excluded due to non-significance.
As the associations observed between those with low and high educational attainment and sick leave might still be explained by job type (patients with low educational attainment more often were blue-collar workers (62%–67% on the lower educated considered in the GEE analyses), with physically demanding jobs), this was explored in an additional analysis. After adjustment for job type, higher ASDAS/BASDASI/BASFI remained independently associated with sick leave in patients with low educational attainment, while job type itself was not significantly associated with sick leave (data not shown).
Discussion
Among a large number of factors explored, higher disease activity, worse physical function and, to a varying extent, the presence of comorbidities played a role in predicting or explaining sick leave over time. Importantly, most of these effects were dependent on educational level. In addition, the occurrence of sick leave independently of other factors predicts recurrent sick leave.
The association between educational level and sick leave in AS has been investigated previously in one cross-sectional study, which found that a lower educational level was associated with the length of sick leave, but not with the likelihood of incurring any sick leave.9 Our study revealed that education actually modified the association between disease activity or physical function and sick leave. More specifically, only in those with a low level of education higher disease activity or worse physical function increased the risk of sick leave. This role of education is likely multifactorial and might relate to job type, coping ability and self-management skills. While those with lower educational attainment more often were blue-collar worker (about 65%), adjustment for job type did not alter our results and job type did not contribute. As such, educational attainment might reflect more adequate coping with stressors related to disease as well as work, and it is likely that such self-management skills are more important than a specific job type.
The association between higher disease activity and/or worse physical function and sick leave was already highlighted in previous research.1 11 13 As we showed an association in the Cox regression (for male patients with low education attainment) between baseline disease activity and a first episode of sick leave over a period of 12 years, disease activity must have an extended influence on the risk of sick leave. However, the short median time from baseline to first sick leave (1.2 years) should be noted. Results from additional analyses with time-varying models suggest that, in patients with low educational attainment, the effect size of disease activity is clearly larger when time-lag is shorter. Such temporal effect was less clear for BASFI. This suggests that the sick leave in patients with low educational attainment is more sensitive to variation in disease activity over time, while BASFI reflects both underlying disease activity and (irreversible) structural damage,32 therefore being both a short-term and long-term predictor of sick leave in these patients. Neither disease activity nor physical function predicted SL in patients with high educational attainment.
Comorbidities (but not EAMs) at baseline were associated with sick leave over time in the time-varying models. Again, this was only significant in those with low education attainment. Apparently, comorbidities have a long-lasting effect with negative impact on absenteeism in AS. Those with lower educational attainment might be less capable to cope with AS and also with comorbidities. As we used AS-related sick leave as outcome, these results imply that patients attribute the influence of comorbidity on sick leave to AS. It should be noted that, at baseline, only 16 (12%) patients had at least one comorbidity. This is likely the result of the relatively young age at baseline (38.7 years) and also a healthy worker effect (those still working are likely to have a better health state compared with those not working anymore and thus not at risk for SL). In addition, lack of screening for comorbidities in these patients in clinical practice could also have played a role (as awareness of the importance of collecting this was limited at the time of OASIS baseline). The limited number of patients with comorbidities at baseline precluded analysis of the impact of specific comorbidities.
Several studies in AS indicated that country of residence is associated with work disability, and also in the 12-year follow-up study of withdrawal from work in OASIS, a significant influence of country of residence was seen.5 However, in the current analyses of sick leave, no influence of country was observed. This is in line with the analyses of the first 2 years in OASIS, which revealed that the risk of having an episode of sick leave did not depend on country (while length of sick leave did).33 Apparently, the patient's decision to take sick leave is independent of the social security system or cultural aspects related to country of residence but stronger related to health-related and personal factors.
To our best knowledge, this was the first study to investigate whether disease-related sick leave in patients with AS independently predicts recurrent disease-related sick leave, which was confirmed. Previous studies have shown similar results in workers with non-specific musculoskeletal complaints and in general, non-disease specific samples.34–36 Our results emphasise the importance of adequate support for patients who incur sick leave. Prevention of sick leave in AS might reduce short-term costs (for the current period of sick leave) and is likely to prevent future sick leave as well, thereby reducing long-term costs.
The current study had several limitations that need to be addressed. First, the patients in OASIS at risk for SL had long-standing disease with an average symptom duration of 16 years at baseline, thereby limiting the generalisability of the results to patients with short-lasting disease manifestations. Next, a ‘healthy worker effect’ might exist in our study population, as patients with severe disease might have been excluded from the labour force (ie, fully work disabled) before the start of OASIS and would therefore not be included in the analyses. As a result, the population at risk for sick leave in OASIS might be healthier than the overall age-adjusted and gender-adjusted AS population. Third, attrition bias might have occurred. After 12 years, only 56 (40%) patients were still at risk for (recurrent) sick leave. It is unknown whether those who became unemployed or work disabled, or were simply lost to follow-up, would have reported sick leave had they remained. Fourth, although information on the length of sick leave was gathered, this was frequently missing or unreliably reported. Moreover, as longer recall periods are associated with imprecision of the length of self-reported sick leave, we decided not to use the length of sick leave as outcome, limiting the interpretation of our analysis.37 Fifth, the temporal relationship between variables was ensured using time-lagged variables, but the actual period between predictor and sick leave could vary considerably. In sensitivity analyses, we used shorter time-lag periods of 6 months in order to minimise this uncertainty. Finally, as biologicals first became available after several years of follow-up, the number of observations with biological use was low and the effect of biological use on SL over time could not be explored.
The main strength of the current study was the prospective study design, and the length of follow-up allowing to investigate whether sick leave was a predictor for recurrent sick leave. Additionally, all relevant outcomes were systematically measured at regular intervals in a standardised way using validated instruments.
While our findings can be relevant for clinical practice, as we identified factors that could warn rheumatologists a patient is at risk for (upcoming or recurrent) sick leave, it should be noted that occurrence of sick leave is not an outcome with only negative connotations: sick leave could be appreciated as a signal for impending work disability, but it could also serve as a means to recover (thereby preventing work disability in the long term). Even then, AS-related sick leave is still a signal that some form of support is necessary. However, it would be worthwhile to investigate if sick leave should always, and at all costs, be prevented. Further research to determine the exact role of sick leave in sickness and recovery in AS is warranted. Also, we should be careful to not stigmatise patients with chronic disease for having sick leave.
In conclusion, in this prospective cohort study, disease-specific factors (higher disease activity, worse functioning and/or comorbidity) increased the risk for recurrent AS-related sick leave in those with lower education. In addition, AS-related sick leave was an independent and strong predictor of recurrent AS-related sick leave over time. Sick leave seems a signal that support is warranted to prevent future adverse work outcome.
Acknowledgments
The authors thank José Dionisio Castillo-Ortiz for his assistance in recollecting missing data on employment in OASIS.
Footnotes
Contributors: AB and DvdH designed the study. SR, AvT, RL, DvdH, FvdB, MD and AB collected and/or prepared the data. CW, AB and AvT analysed the data. CW, AB, AvT, SR, RL and DvdH critically interpreted the results. CW, AB and AvT were involved in drafting the manuscript. All authors revised the manuscript critically for important intellectual content and approved the final manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent: Not required.
Ethics approval: The ethics committee from all participating hospitals have approved the study.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data statement: No additional data are available.
References
- 1. Boonen A, Brinkhuizen T, Landewé R, et al. . Impact of ankylosing spondylitis on sick leave, presenteeism and unpaid productivity, and estimation of the societal cost. Ann Rheum Dis 2010;69:1123–8. 10.1136/ard.2009.116764 [DOI] [PubMed] [Google Scholar]
- 2. Webers C, Vanhoof L, van Genderen S, et al. . Employment and the role of personal factors among patients with ankylosing spondylitis: a Dutch cross-sectional case-control study. RMD Open 2018;4:e000680 10.1136/rmdopen-2018-000680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Verstappen SM, Watson KD, Lunt M, et al. . Working status in patients with rheumatoid arthritis, ankylosing spondylitis and psoriatic arthritis: results from the British Society for Rheumatology Biologics Register. Rheumatology 2010;49:1570–7. 10.1093/rheumatology/keq131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bakland G, Gran JT, Becker-Merok A, et al. . Work disability in patients with ankylosing spondylitis in Norway. J Rheumatol 2011;38:479–84. 10.3899/jrheum.100686 [DOI] [PubMed] [Google Scholar]
- 5. Castillo-Ortiz JD, Ramiro S, Landewé R, et al. . Work outcome in patients with ankylosing spondylitis: results from a 12-year followup of an international study. Arthritis Care Res 2016;68:544–52. 10.1002/acr.22730 [DOI] [PubMed] [Google Scholar]
- 6. Strömbeck B, Jacobsson LT, Bremander A, et al. . Patients with ankylosing spondylitis have increased sick leave--a registry-based case-control study over 7 yrs. Rheumatology 2009;48:289–92. 10.1093/rheumatology/ken497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Strömbeck B, Englund M, Bremander A, et al. . Cost of illness from the public payers' perspective in patients with ankylosing spondylitis in rheumatological care. J Rheumatol 2010;37:2348–55. 10.3899/jrheum.100099 [DOI] [PubMed] [Google Scholar]
- 8. Floderus B, Göransson S, Alexanderson K, et al. . Self-estimated life situation in patients on long-term sick leave. J Rehabil Med 2005;37:291–9. 10.1080/16501970510034422 [DOI] [PubMed] [Google Scholar]
- 9. Gordeev VS, Maksymowych WP, Schachna L, et al. . Understanding presenteeism in patients with ankylosing spondylitis: contributing factors and association with sick leave. Arthritis Care Res 2014;66:916–24. 10.1002/acr.22253 [DOI] [PubMed] [Google Scholar]
- 10. Guillemin F, Briançon S, Pourel J, et al. . Long-term disability and prolonged sick leaves as outcome measurements in ankylosing spondylitis. Possible predictive factors. Arthritis Rheum 1990;33:1001–6. 10.1002/art.1780330712 [DOI] [PubMed] [Google Scholar]
- 11. Healey EL, Haywood KL, Jordan KP, et al. . Impact of ankylosing spondylitis on work in patients across the UK. Scand J Rheumatol 2011;40:34–40. 10.3109/03009742.2010.487838 [DOI] [PubMed] [Google Scholar]
- 12. Meyer K, Niedermann K, Tschopp A, et al. . Is the work ability index useful to evaluate absence days in ankylosing spondylitis patients? A cross-sectional study. BMJ Open 2013;3:e002231 10.1136/bmjopen-2012-002231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ward MM, Kuzis S. Risk factors for work disability in patients with ankylosing spondylitis. J Rheumatol 2001;28:315–21. [PubMed] [Google Scholar]
- 14. Organization WH International classification of functioning, disability and health. ICF: World Health Organization, 2001. [Google Scholar]
- 15. Stolwijk C, Castillo-Ortiz JD, Gignac M, et al. . Importance of contextual factors when measuring work outcome in ankylosing spondylitis: a systematic review by the OMERACT Worker productivity group. Arthritis Care Res 2015;67:1316–27. 10.1002/acr.22573 [DOI] [PubMed] [Google Scholar]
- 16. van der Linden S, Valkenburg HA, Cats A. Evaluation of diagnostic criteria for ankylosing spondylitis. A proposal for modification of the New York criteria. Arthritis Rheum 1984;27:361–8. [DOI] [PubMed] [Google Scholar]
- 17. Michaud K, Wolfe F. Comorbidities in rheumatoid arthritis. Best Pract Res Clin Rheumatol 2007;21:885–906. 10.1016/j.berh.2007.06.002 [DOI] [PubMed] [Google Scholar]
- 18. Stolwijk C, van Tubergen A, Ramiro S, et al. . Aspects of validity of the self-administered comorbidity questionnaire in patients with ankylosing spondylitis. Rheumatology 2014;53:1054–64. 10.1093/rheumatology/ket354 [DOI] [PubMed] [Google Scholar]
- 19. Garrett S, Jenkinson T, Kennedy LG, et al. . A new approach to defining disease status in ankylosing spondylitis: the Bath Ankylosing Spondylitis Disease Activity Index. J Rheumatol 1994;21:2286–91. [PubMed] [Google Scholar]
- 20. Lukas C, Landewé R, Sieper J, et al. . Development of an ASAS-endorsed disease activity score (ASDAS) in patients with ankylosing spondylitis. Ann Rheum Dis 2009;68:18–24. 10.1136/ard.2008.094870 [DOI] [PubMed] [Google Scholar]
- 21. Calin A, Garrett S, Whitelock H, et al. . A new approach to defining functional ability in ankylosing spondylitis: the development of the Bath Ankylosing Spondylitis Functional Index. J Rheumatol 1994;21:2281–5. [PubMed] [Google Scholar]
- 22. Jones SD, Steiner A, Garrett SL, et al. . The Bath Ankylosing Spondylitis Patient Global Score (BAS-G). Br J Rheumatol 1996;35:66–71. 10.1093/rheumatology/35.1.66 [DOI] [PubMed] [Google Scholar]
- 23. van der Heijde D, Landewé R, Feldtkeller E. Proposal of a linear definition of the Bath Ankylosing Spondylitis Metrology Index (BASMI) and comparison with the 2-step and 10-step definitions. Ann Rheum Dis 2008;67:489–93. 10.1136/ard.2007.074724 [DOI] [PubMed] [Google Scholar]
- 24. Jenkinson TR, Mallorie PA, Whitelock HC, et al. . Defining spinal mobility in ankylosing spondylitis (AS). The Bath AS Metrology Index. J Rheumatol 1994;21:1694–8. [PubMed] [Google Scholar]
- 25. Creemers MC, Franssen MJ, van't Hof MA, et al. . Assessment of outcome in ankylosing spondylitis: an extended radiographic scoring system. Ann Rheum Dis 2005;64:127–9. 10.1136/ard.2004.020503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Ramiro S, van Tubergen A, Stolwijk C, et al. . Scoring radiographic progression in ankylosing spondylitis: should we use the modified Stoke Ankylosing Spondylitis Spine Score (mSASSS) or the Radiographic Ankylosing Spondylitis Spinal Score (RASSS)? Arthritis Res Ther 2013;15:R14 10.1186/ar4144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ramiro S, Stolwijk C, van Tubergen A, et al. . Evolution of radiographic damage in ankylosing spondylitis: a 12 year prospective follow-up of the OASIS study. Ann Rheum Dis 2015;74:52–9. 10.1136/annrheumdis-2013-204055 [DOI] [PubMed] [Google Scholar]
- 28. Dougados M, Simon P, Braun J, et al. . ASAS recommendations for collecting, analysing and reporting NSAID intake in clinical trials/epidemiological studies in axial spondyloarthritis. Ann Rheum Dis 2011;70:249–51. 10.1136/ard.2010.133488 [DOI] [PubMed] [Google Scholar]
- 29. Gaudette LA, Richardson A, Huang S. Which workers smoke? Health Rep 1998;10:35–45. [PubMed] [Google Scholar]
- 30. Schreuder KJ, Roelen CA, Koopmans PC, et al. . Job demands and health complaints in white and blue collar workers. Work 2008;31:425–32. [PubMed] [Google Scholar]
- 31. Twisk JW, Smidt N, de Vente W. Applied analysis of recurrent events: a practical overview. J Epidemiol Community Health 2005;59:706–10. 10.1136/jech.2004.030759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Machado P, Landewé R, Braun J, et al. . A stratified model for health outcomes in ankylosing spondylitis. Ann Rheum Dis 2011;70:1758–64. 10.1136/ard.2011.150037 [DOI] [PubMed] [Google Scholar]
- 33. Boonen A, van der Heijde D, Landewé R, et al. . Work status and productivity costs due to ankylosing spondylitis: comparison of three European countries. Ann Rheum Dis 2002;61:429–37. 10.1136/ard.61.5.429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Lötters F, Hogg-Johnson S, Burdorf A. Health status, its perceptions, and effect on return to work and recurrent sick leave. Spine 2005;30:1086–92. 10.1097/01.brs.0000161484.89398.48 [DOI] [PubMed] [Google Scholar]
- 35. Koopmans PC, Roelen CA, Groothoff JW. Risk of future sickness absence in frequent and long-term absentees. Occup Med 2008;58:268–74. 10.1093/occmed/kqn040 [DOI] [PubMed] [Google Scholar]
- 36. Roelen CA, Koopmans PC, Schreuder JA, et al. . The history of registered sickness absence predicts future sickness absence. Occup Med 2011;61:96–101. 10.1093/occmed/kqq181 [DOI] [PubMed] [Google Scholar]
- 37. Severens JL, Mulder J, Laheij RJ, et al. . Precision and accuracy in measuring absence from work as a basis for calculating productivity costs in The Netherlands. Soc Sci Med 2000;51:243–9. 10.1016/S0277-9536(99)00452-9 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
rmdopen-2018-000766supp002.tif (2.4MB, tif)
rmdopen-2018-000766supp001.docx (26KB, docx)