Abstract
The present paper reviews vasodilator compounds isolated from plants that were reported in the past 22 years (1990 to 2012) and the different mechanisms of action involved in their vasodilator effects. The search for reports was conducted in a comprehensive manner, intending to encompass those metabolites with a vasodilator effect whose mechanism of action involved both vascular endothelium and arterial smooth muscle. The results obtained from our bibliographic search showed that over half of the isolated compounds have a mechanism of action involving the endothelium. Most of these bioactive metabolites cause vasodilation either by activating the nitric oxide/cGMP pathway or by blocking voltage-dependent calcium channels. Moreover, it was found that many compounds induced vasodilation by more than one mechanism. This review confirms that secondary metabolites, which include a significant group of compounds with extensive chemical diversity, are a valuable source of new pharmaceuticals useful for the treatment and prevention of cardiovascular diseases.
Keywords: vasodilator compounds, vascular endothelium, arterial smooth muscle, NO/cGMP pathway, PGI2/cAMP pathway, potassium channel activators, calcium channel blockers, phosphodiesterases inhibitors, PKC inhibitors
1. Introduction
According to the World Health Organization, cardiovascular diseases are the leading cause of death worldwide. Among these, arterial hypertension has a high prevalence and is associated with other conditions, such as myocardial infarction and stroke [1]. Although there are more than 200 drugs that lower blood pressure, less than a third of the hypertension cases are successfully treated due to their low efficacy, detrimental side effects and lack of cardiovascular risk reduction [2]. In addition, the etiology of hypertension has been associated with vascular endothelial dysfunction, which is characterized by an uncoupling between the release of endothelial factors such as nitric oxide (NO), prostacyclin (PGI2) and endothelium-derived hyperpolarization (EDH), as well as effects on endothelium-dependent contractile mechanisms, and the associated change in vascular smooth muscle tone [3].
Some studies have suggested that changes in the bioavailability of endothelium-derived NO may be responsible for endothelial dysfunction and the related altered blood pressure and myocardial infarction [4,5,6,7,8,9,10]. Such altered NO levels can be due to dysfunction of soluble guanylate cyclase protein (sGC), with changes in the levels of this protein likely related to the pathophysiology of pulmonary hypertension and hypoxia [11,12]. With regard to vascular smooth muscle relaxation, various cardiovascular diseases, such as coronary vasospasm [13,14], cardiac ischemia [15] and hypertension [16] have also been associated with altered expression and activation of various potassium channels. Based on the above evidence, we are currently seeking new therapeutic strategies for preventing and treating these conditions that also have relaxing effects on vascular smooth muscle.
In this context, plants are a major source of new biologically active compounds, and the ethnomedical knowledge of traditional medicine from around the world is a useful starting point for determining their efficacy. In addition, due to the multifactorial nature of cardiovascular disease such as hypertension, knowledge of the mechanisms of action of each of the compounds proposed for use in the treatment for this disease is a crucial element for planning and developing different therapeutic strategies. Therefore, the present work reviews the previously reported vasodilator compounds isolated from plants and the different mechanisms of action involved in their vasodilator effects.
2. Search Strategy
The literature review focused on the past 22 years (1990 to 2012), taking into account studies on the vasodilating activity of plant-based treatments and the compounds derived from them. We reviewed more than 450 abstracts on this topic. The search was focused on those metabolites with a vasodilator effect whose mechanism of action involved the vascular endothelium and the arterial smooth muscle vasorelaxation pathways; we did not consider the antioxidant activity or reactive oxygen species scavenging.
3. Types of Compounds with Vasodilator Effects
We identified 207 vasodilator metabolites together with their possible mechanism(s) of action. First, these compounds were classified according to their chemical nature. It is clear that most compounds with vasodilator activity are alkaloids, flavonoids, or terpenoids (Figure 1). The classification of these compounds offers an overview of the types of compounds that present significant vasodilator activity and of the structural diversity exhibited by these bioactive compounds.
Figure 1.
Classification of vasodilator compounds obtained from plants according to their chemical nature.
Some of these compounds have been studied on multiple occasions, and various mechanisms of action have been proposed to explain their vasodilatory activities. These compounds include the flavonoids naringenin [17,18,19], dioclein [20,21,22,23], quercetin [24,25,26,27,28] and (−)-epigallocatechin-3-gallate [29,30,31]; the polyphenols piceatannol [32,33] and resveratrol [34,35,36]; the sesquiterpene polygodial [37,38,39]; the monoterpene rotundifolone [40,41,42] and the alkaloid rutaecarpine [43,44,45,46].
In other cases, mixtures of various compounds obtained from plants or the products generated from them were studied; examples include polyphenols in red wine [47,48], saponins from ginseng [49], proanthocyanidins from persimmon leaf tea [50] and green tea [48,51], as well as the xanthones obtained from Halenia elliptica [52]. In 34 plants, two or more vasodilator compounds were identified, which in some cases had different mechanisms of action. Examples of this are the chalcones isolated from Angelica keiskei [53], the alkaloids obtained from Peganum harmala [54], the glycosides identified in Melaleuca quinquenervia [55] and the macrocyclic bis(bibenzyls) from liverworts [56]. In these examples, the fundamental difference between the mechanisms of action proposed for the isolated compounds is based on their dependence or independence on the endothelium, the involvement of the NO/cGMP pathway and the blockage of voltage-dependent Ca2+ channels.
4. Proposed Mechanisms of Action
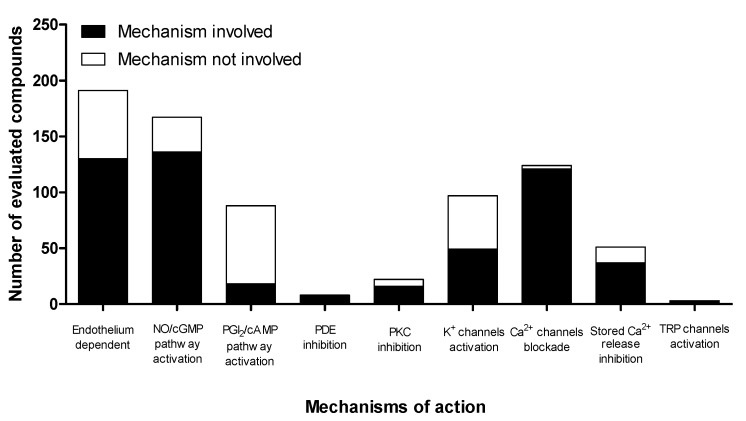
Different mechanisms of action were proposed to explain the vasodilator effect of the 207 compounds derived from plants (Figure 2).
Figure 2.
Classification of compounds obtained from plants according to the main mechanism(s) of action involved in their vasodilator effect.
Analysis of the mechanisms of action of these compounds revealed that, on the one hand, the vasodilator effect of a significant number of compounds (40%) involves two or more mechanisms (Table 1). On the other hand, as shown in Figure 2, over half of the tested compounds have a mechanism of action that requires the participation of the endothelium, at least in part. Therefore, endothelium-derived factors play a key role in the mechanisms of action of these vasodilators. The mechanisms of action most frequently assessed in the vasodilator effects of the plant compounds were activation of the NO/cGMP pathway, blockade of Ca2+ channels, and activation of K+ channels.
Table 1.
Mechanisms of action proposed for vasodilator compounds obtained from plants.
| Compound | Type of artery/vein | EC50 | Endothelium | NO/cGMP | PGI2/cAMP | PDE | PKC | K+ Ch | Ca2+ext /Ca2+int | Ref. | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Allicin | rat pulmonary | 0.8 µg/mL 1 | d | + | x | [65] | ||||
| 2 | Allyl isothiocyanate | rat cerebral | 164 µM 2 | d | x | x | +IKCa, | +TRPA1/ | [66] | ||
| +SKCa, | |||||||||||
| +KIR | |||||||||||
| 3 | Alpha-terpineol | rat mesenteric | NR | + | [67] | ||||||
| 4 | Alpha-zearalanol | rat aorta | NR | d/i | + | +BKCa, | -VOCC/ | [68] | |||
| +KATP | |||||||||||
| 5 | Alpinetin | rat mesenteric | 27.5 µM 1 | d/i | + | x | - | -VOCC/ -IP3R, -RyRs |
[69] | ||
| 6 | Alstonisine | rat aorta | NR | d/i | + | x | -VOCC,- | [70] | |||
| ROCC/ | |||||||||||
| 7 | Amentoflavone | rat aorta | NR | d | + | x | + | -VOCC/ | [71] | ||
| 8 | Angelic ester of 2-β-hydroxy-8α-H-7(11)-eremophilene-12,8-olide | rat mesenteric | 4.74 ± 0.1 §,2 | -VOCCL/ | [72] | ||||||
| rat aorta | 5.43 ± 0.06 §,2 | ||||||||||
| 9 | Angelic ester of 2-β-hydroxy-8β-H-7(11)-eremophilene-12,8-olide | rat mesenteric | 4.11 ± 0.02 §,2 | x | x | -VOCCL/x | [72] | ||||
| rat aorta | 4.92 ± 0.09 §,2 | ||||||||||
| 10 | Apigenin | rat aorta | 3.7 ± 0.5 µM 1 | d/i | + x |
x | x | +IKCa, +SKCa | -VOCC, -ROCC/x +TRPV4/ |
[73] | |
| rat aorta | 63 µM 5 | i | [74] | ||||||||
| rat mesenteric | NR | d | [75] | ||||||||
| 11 | Apocynin | rat aorta | 780 ± 80 µM 1 | d/i | + | x | +KATP | -VOCC,- ROCC/ -IP3R |
[76] | ||
| 12 | Astragaloside IV | rat aorta | NR | d/i | + | + | -VOCC,- ROCC/ -IP3R |
[77] | |||
| 13 | Backebergine | rat aorta | NR | d/i | + | x | -VOCC,- ROCC/ | [78] | |||
| 14 | Baicalin | rat mesenteric | NR | i | + | + | - | +BKCa | -VOCC/ | [79] | |
| 15 | 4-Benzoyl-2-C-β-gluco-pyranosyl-3,5-dihydroxy-6-methylphenyl β-d-glucopyranoside | rat aorta | NR | d | + | [55] | |||||
| 16 | Berberine | rat mesenteric | 1.48 ± 0.16 µM 1 | d/i | + | x | x | +BKCa, +Kv, | x/-RyRs | [80] | |
| +KIR | |||||||||||
| 17 | Betulinic acid | rat aorta | 1.67 µM 1 | d | + | x | [81] | ||||
| 18 | Bilobalide | rat aorta | NR | + | x | -VOCC/ | [82] | ||||
| 19 | Biochanin A | rat aorta | NR | i | +BKCa, +KATP | -VOCC,- ROCC/- | [83] | ||||
| 20 | Brazilin | rat aorta | 183 ± 30 µM 1 | d | + | [84] | |||||
| rat aorta | i | x | [85] | ||||||||
| rat mesenteric | i | x | [85] | ||||||||
| 21 | (−)-Borneol | rat aorta | 4.63 ± 0.15 §,1 | i | +BKCa, +Kv, | -VOCCL/- | [86] | ||||
| +KATP | |||||||||||
| 22 | Butein | rat aorta | 7.4 ± 1.6 µM 1 | d | + | x | - | x | [87] | ||
| 23 | Butylidenephthalide | rat aorta | 4.20 ± 0.07 §,3 | d/i | + | x | - | x | -VOCCL, -ROCC/- |
[88] | |
| 24 | Cadamine | rat aorta | NR | d/i | + | x | -VOCC,- ROCC/ | [89] | |||
| 25 | Caffeic acid | rat aorta | 400 µM 1 | d/i | + | x | [90] | ||||
| 26 | Caffeic acid phenethyl ester | porcine coronary | 4.99 ± 0.17 §,1 | d/i | + | -VOCC/ | [91] | ||||
| rat aorta | 5.15 ± 0.0 §,4 | d | + | x | [92] | ||||||
| 27 | Calycosin | rat aorta | 4.46 ± 0.13 §,3 | i | x | x | -VOCC/x | [93] | |||
| 28 | Capsaicin | rat mesenteric | NR | x | [94] | ||||||
| 29 | Cardamonin | rat mesenteric rat tail |
9.3 µM 1 4.63 ± 0.01 §,1 |
d/i | + | x | - | +BKCa | -VOCC/- IP3R,-RyRs -VOCC/ |
[69] [95] |
|
| 30 | Carvacrol | rat aorta rat cerebral |
145.4 ± 6.07 µM 1 | id | x | x | - | +SKCa, +KIR, +IKCa |
-VOCC/-IP3R +TRPV3/ |
[96] [97] |
|
| 78.8 ± 11.9 µM 2 | |||||||||||
| 4.1 µM | |||||||||||
| 31 | Cassiarin A | rat mesenteric | 6.4 ± 0.8 µM 1 | d/i | + | x | +BKCa | [98] | |||
| 32 | Cathafoline | rat aorta | NR | d/i | + | x | -ROCC/ | [70] | |||
| 33 | Centaureidin | rat orta | 16.7 ± 1.9 µM 5 | i | [99] | ||||||
| 34 | Chrysin | rat orta | 16 ± 4 µM 1 | d | + | [100,101] | |||||
| 35 | Chrysin glucoside | rat aorta | 52 µM 5 | d/i | + | [102] | |||||
| 36 | Cinnamaldehyde | rat aorta | NR | d/i | + | x | x | -VOCC/ | [103] | ||
| 37 | Ethyl cinnamate | rat aorta | 380 ± 40 µM 1 | d/i | + | + | -VOCC/ | [104] | |||
| 38 | 1,8-Cineole | rat aorta | 663.2 ± 63.8 µg/mL 1 | d | + | x | x | [105] | |||
| 39 | (+)-cis-4'-O-Acetyl-3'- O-angeloylkhellactone | rat aorta | NR | d/i | + | x | x | -VOCC/ | [106] | ||
| 40 | Citral | rat aorta | NR | d/i | + | x | -ROCC/- | [102] | |||
| 41 | Citronellol | rat mesenteric | 0.71 ± 0.11 §,1 | i | x | -VOCC/- IP3R, -RyRs |
[107] | ||||
| 42 | Coptisine | rat aorta | 4.49 ± 0.48 §,5 | d/i | + | + | +KV | -VOCC,- ROCC/- | [108] | ||
| 43 | Cornuside | rat aorta | NR | d | + | x | x | [109] | |||
| 44 | Cryptotanshinone | rat coronary | 2.65 ± 0.15 µg/mL 6 | i | x | x | x | -VOCCL/ | [110] | ||
| 45 | Curine | rat mesentericrat aorta | 4.8 ± 1.9 µM 5 7.6 ± 1.6 µM 1 |
i | -VOCC/- - VOCCL/- |
[111] [112] |
|||||
| 46 | Curcumin | porcine coronary | 6.28 ± 0.28 µM 4 | d | + | x | [113] | ||||
| 47 | Cyclosquamosin B | rat aorta | NR | i | -VOCC/ | [114] | |||||
| 48 | Daidzein | rat basilar | 20 ± 7 µM 3 7.4 ± 1.9 µM6 |
ii | x | x | + +BKCa, +KATP |
-VOCC/ | [115] [116] |
||
| 49 | Daidzin | rat basilar | 140 ± 21 µM 3 | i | x | x | +KATP | -VOCC/ | [115] | ||
| 50 | Danshensu | rat coronary | 71.5 ± 11 µg/mL 6 | i | + | -VOCCL/ | [117] | ||||
| 51 | Dehydroevodiamine | rat mesenteric | NR | d/i | + | x | + | -VOCC/ | [118] | ||
| 52 | Demethylpiperitol | rat aorta | NR | d | + | [119] | |||||
| 53 | Denudatin B | rat aorta | 21.2 µg/mL 2 | i | ↑cGMP | x | -VOCC,- ROCC/x | [120] | |||
| 54 | 14-Deoxy-andrographolide | rat aorta | NR | d /i | + | x | x | -VOCC, -ROCC/ |
[121] | ||
| 55 | Dictamnine | rat aorta | 15 µM 2 | i | x | -VOCC,- ROCC/ | [122] | ||||
| 56 | Dihydrotanshinone | rat coronary | 10.39 ± 1.69 µM 6 | i | x | x | x | -VOCCL/ | [123] | ||
| 57 | 3,7-Dihydroxy-2,4-dimethoxyphenanthrene | rat aorta | NR | d/i | + | [124] | |||||
| 58 | Dioclein | rat aorta | 1.3 ± 3.1 µM 1 | d | + | x x |
- | - | +KCa, +KV | -VOCC/-IP3R | [20] |
| rat aorta | 350 ± 80 µM 5 | i | [21] | ||||||||
| rat mesenteric | 0.3 ± 0.06 µM 1 | d/i | [22] | ||||||||
| human saphenous | 7.3 ± 3.1 µM 1 | i | [23] | ||||||||
| 59 | Diosgenin | rat mesenteric | 330 ± 120 µM 1 | d | + | + | +BKCa | [62] | |||
| 60 | Echinacoside | rat aorta | NR | d | + | x | [125] | ||||
| 61 | Ellagic acid | rat aorta | 5.60 ± 0.03 §,1 | d/i | + | x | x | -VOCCL/ | [126] | ||
| 62 | Emodin | rat aorta | NR | i | ↑cGMP | [127] | |||||
| 63 | Ent-18-hydroxy-trachyloban-3-one | rat aorta | 5.7 ± 0.01 §,2 | x | -VOCCL/ | [128] | |||||
| 64 | Ent-8(14), 15-pimaradien-3β-ol | rat aorta | 4.8 ± 0.1 §,1 | d/i | + | x | x | -VOCC/x | [129] | ||
| 65 | Epicatechin | rat aorta | 4.72 ± 0.07 §,1 | d | + | [130] | |||||
| 66 | 7-Epiclusianone | rat aorta | NR | d | + | x | [131] | ||||
| 67 | (−)-Epigallocatechin-3-gallate | rat aorta | 191.8 ± 13 µM 5 | i | - | x +BKCa |
[29] | ||||
| bovine ophtalmic | 6.21 ± 0.06 §,6 | d | + | [31] | |||||||
| rat aorta | 4.76 ± 0.07 §,1 | d | + | [130] | |||||||
| 68 | Equol (daidzein metabolite) | rat aorta | NR | d | + | [132] | |||||
| 69 | Eriodictyol | rat aorta | 61.1 ± 2 µM 5 | i | x | -VOCC/ | [133] | ||||
| 70 | Erythrodiol | rat aorta | 3.38 ± 1.27 µM 1 | d | + | x | [134] | ||||
| 71 | Eudesmin | rat aorta | 10.69 ± 0.77 µg/mL 1 | d | + | + | [135] | ||||
| 72 | Eugenol | rat aorta | x | x | - VOCC,- ROCC/x - VOCC,- ROCC/ |
[136] | |||||
| rat aorta | 1200 µM 1 | d/i | + | [137] | |||||||
| rat mesenteric | d/i | x | [138] | ||||||||
| 73 | Euxanthone | rat aorta | 32.5 ± 2.5 µM 5 | i | x | x | - | x | -VOCC,- ROCC/ -IP3R |
[139] | |
| 74 | Evocarpine | rat aorta | 9.8 µM 2 | -VOCC/ | [140] | ||||||
| 75 | Evodiamine | rat mesenteric | NR | d/i | x | -ROCC/x | [141] | ||||
| 76 | Ferulic acid | rat aorta | NR | i | x | x/ | [142] | ||||
| 77 | Floranol | rat mesenteric | 19.9 ± 2.4 µM 1 | d/i | + | x | x | -VOCC/ | [143] | ||
| rat aorta | i | x | [144] | ||||||||
| 78 | Formononetin | rat aorta | NR | d/ i | + | + | -VOCC/ | [145] | |||
| 79 | Forsythide | rat aorta | NR | i | x | -ROCC/ | [146] | ||||
| 80 | Fraxinellone | rat aorta | 25 µM 2 | -VOCC/ | [122] | ||||||
| 81 | Galangin | rat aorta | NR | d/i | + | x | -VOCC/ | [147] | |||
| 82 | Geissoschizine methyl ether | rat aorta | 0.744 µM 5 | d/i | + | -VOCC/ | [148] | ||||
| 83 | Genistein | rabbit coronary | NR | i | x | x | x | -VOCCL/ | [149] | ||
| human umbilical | -VOCC/- | [150] | |||||||||
| 84 | Gigantol | rat aorta | NR | d/i | + | [124] | |||||
| 85 | Ginsenoside Rg3 | rat aorta | NR | d | + | + | [151] | ||||
| 86 | Gomisin A | rat aorta | NR | d/i | + | [152] | |||||
| 87 | Gymnopusin | rat aorta | 63 µM 5 | i | x | +BKCa, +KATP | -VOCCL/ | [153] | |||
| 88 | Harmaline | rat aorta | 32.8 ± 1.17 µM 2 | d/i | + | + | - | -VOCC/ | [154] | ||
| 89 | Harman | rat aorta | 9 µM 1 | d/i | + | x | x | -VOCCL, -ROCC/ |
[155] | ||
| 90 | Harmine | rat aorta | 3.7 ± 1.2 µM 5 | i | x | x | - | -VOCC/ | [154] | ||
| 91 | Hematoxylin | rat aorta | NR | d | + | [156] | |||||
| 92 | Hesperetin | rat aorta | 62.8 ± 5.0 µM 5 | i | x | - | x | -VOCC,- ROCC/ | [157] | ||
| 93 | Hirsutine | rat aorta | 10.6 µM 5 | i | -VOCC/ | [148] | |||||
| 94 | 4-Hydroxybenzoic acid | rat aorta | 1780 µM 1 | d | + | x | [90] | ||||
| 95 | 4-Hydroxyderricin | rat aorta | NR | d/i | + | -VOCC/ | [53] | ||||
| 96 | 1-Hydroxy-2,3,5-trimethoxyxanthone | rat coronary | 1.67 ± 0.27 µM 6 | d | + | x | - | x | -VOCCL/x | [130] | |
| 97 | Hypogallic acid | rat aorta | 620 µM 1 | d/ i | + | +KATP | [90] | ||||
| 98 | Icariin | rat aorta | NR | + | [158] | ||||||
| canine coronary | d | + | x | x | [159] | ||||||
| 99 | Imperatorin | rat mesenteric mouse aorta |
i | +BKCa | -VOCC,- ROCC/- | [160] | |||||
| 12.2 ± 2.4 µM 1 | d | + | [161] | ||||||||
| 100 | Isoliquiritigenin | rat aorta | 7.4 ± 1.6 µM 1 | i | ↑cGMP | x | x | [162] | |||
| 101 | Isoplagiochin B | rat aorta | NR | i | + | -ROCC/ | [56] | ||||
| 102 | Isoplagiochin D | rat aorta | NR | i | x | -VOCC,- ROCC/ | [56] | ||||
| 103 | Isopropyl 3-(3,4-dihydroxyphenyl) -2-hydroxypropanoate |
rat mesenteric | 7.41 ± 0.08 §,5 | i | +BKCa | -VOCC,- ROCC/- | [123] | ||||
| 104 | Isorhamnetin | rat mesenteric | 5.89 ± 0.11 §,5 | i | x | x | [163] | ||||
| 105 | Isorhynchophylline | rat aorta | 20–30 µM 2 | i | x | -VOCCL/- IP3R | [164] | ||||
| 106 | Iso-S-petasin | rat aorta | NR | i | -VOCCL/ | [165] | |||||
| 107 | Isotirumalin | rat aorta | 4.84 ± 0.24 ǂ,1 | d | + | [166] | |||||
| 108 | Jatrophone | rat aorta | 11.0 µM 5 | d/i | + | -VOCC/- | [167] | ||||
| rat portal vein | 13.54 µM 5 | - | [168] | ||||||||
| 109 | Kaempferol | rat aorta rat aorta rat mesenteric porcine coronary rat aorta |
580 µM 1 4.81 ± 0.13 §,5 5.66 ± 0.06 §,5 |
d/i d/i d |
+ + |
[90] [163] [163] [169] [170] |
|||||
| 110 | Kaurenoic acid | rat aorta | NR | d/i | + | x | +BKCa, +KV | -VOCC/x | [171] | ||
| 111 | Keayanidine B | rat aorta | 23.3 ± 1.3 µM 1 | + | [172] | ||||||
| 112 | Keayanine | rat aorta | 27.5 ± 2.4 µM 1 | + | [172] | ||||||
| 113 | Kolaviron | rat mesenteric | NR | i | +BKCa, +KV | -VOCCL/ - IP3R |
[173] | ||||
| 114 | Labdane-302 | rat mesenteric | 5.4 ± 1.4 µM 1 | d/i | + | + | -VOCCL/ | [174] | |||
| 115 | Labd-8 (17)-en-15-oic acid | rat aorta | 313.6 µg/mL 2 | i | x | [175] | |||||
| 116 | Lectin (of Pisum arvense) | rat aorta | 58.38 ± 1.87 µg/mL 1 | d | + | x | x | [176] | |||
| 117 | Leonurine | rat aorta | 86.4 ± 10.4 µM 1 | - VOCCL/- | [177] | ||||||
| 118 | Leucocyanidol | rat aorta | 2.75 ± 0.15 §,5 | d/i | + | [178] | |||||
| 119 | Ligustilide | rat mesenteric | 3.98 §,2 | i | x | x | -VOCC,- ROCC/ -RyR |
[179] | |||
| rat aorta | 4.39 ± 0.11 §,1 | i | x | x | x | [180] | |||||
| 120 | (−)-limacine | rat aorta | NR | d | + | [78] | |||||
| 121 | Luteolin | rat aorta | NR | i | x | +KIR, +KV | -VOCC/- | [17,181] | |||
| 122 | Machilin D | rat aorta | 17.8 µM | d | + | [182] | |||||
| 123 | Marrubenol | rat aorta | 11.8 ± 0.3 µM 2 | -VOCCL/ | [183] | ||||||
| 124 | Marrubiin | rat aorta | NR | d/i | + | -VOCC/ | [184] | ||||
| 125 | 10-Methoxyaffinisine | rat aorta | NR | d/i | + | x | -VOCC/ | [70] | |||
| 126 | Methyl brevifolincarboxylate | rat aorta | NR | i | -ROCC/x | [185] | |||||
| 127 | Methyleugenol | rat mesenteric | NR | d/i | + | [67] | |||||
| 128 | Methylpaeoniflorin | rat aorta | 10.1 µM 1 | d | + | [186] | |||||
| 129 | Milonine | rat mesenteric | 1.1 µM 1 | d/i | + | x | +BKCa, +SKCa, +KATP | - VOCC,- ROCC/ -IP3R,-RyR |
[187] | ||
| 130 | Mollic acid glucoside | rat aorta | NR | d | + | [188] | |||||
| 131 | Morolic acid | rat aorta | 94.19 µM 5 | d | + | x | [189] | ||||
| 132 | Moronic acid | rat aorta | 16.11 µM 5 | d | + | x | [189] | ||||
| 133 | (+)-Nantenine | rat aorta | NR | i | x | -VOCC/x | [190] | ||||
| 134 | (+/−)-Naringenin | rat aortarat aortarat aorta | 71.2 ± 5.3 µM 1 4.68 µM 5 |
i i i |
- | - | +BKCa | -VDCC, -ROCC/ |
[17] [18] [19] |
||
| 135 | Naucline | rat aorta | 20 µM 1 | i | x | -VOCC, -ROCC/ |
[89] | ||||
| 136 | 1-Nitro-2-phenylethane | rat aorta | 231.5 µM 1 | i | + | x | +KATP, +KV | [191] | |||
| 137 | Norathyriol | rat aorta | NR | i | x | x | -VOCC, -ROCC/ |
[192] | |||
| 138 | Oleanolic acid | rat aorta | 5.58 ± 1.28 µM 1 | d | + | x | [134] | ||||
| 139 | 12-O-Methylcurine | rat aorta | 63.2 ± 8.8 µM 1 | i | - | -VOCC,- ROCC/ -IP3R |
[193] | ||||
| 140 | Orientin | New Zealand rabbit aorta | 2.28 µM 1 | d/i | + | x | x | - VOCC,- ROCC/- | [194] | ||
| 141 | Osthole | rat aorta | NR | i | ↑cGMP | x | - VOCC,- ROCC/- | [195] | |||
| 142 | Paeoniflorin | rat aorta | 19.4 µM 1 | d | + | [186] | |||||
| 143 | Paeonidanin | rat aorta | 7.9 µM 1 | d | + | [186] | |||||
| 144 | Pecrassipine A | rat aorta | NR | d/i | + | x | - VOCC,- ROCC/ | [78] | |||
| 145 | 1,2,3,4,6-Penta-O-galloyl-β-d-glucose | rat aorta | 3.6 µM 1 | d | + | + | x | [196] | |||
| 146 | Perrottetin | rat aorta | NR | i | x | - VOCC,- ROCC/ | [56] | ||||
| 147 | Phlomeoic acid | rat aorta | NR | d/i | + | -VOCC/ | [184] | ||||
| 148 | Phloretin | rabbit coronary | NR | i | [149] | ||||||
| 149 | Piceatannol | rat aorta | 2.4 ± 0.4 µM 1 | d | + | x | +BKCa | [32] | |||
| rat aorta | d | + | [33] | ||||||||
| 150 | Pimaradienoic acid | rat aorta | NR | i | + | + | x | -VOCC/x | [197] | ||
| 151 | Pinocembrin | rat aorta | 4.37 ± 0.02 §,5 | d/i | + | x | +KATP, +KV | - VOCC/- IP3R | [198] | ||
| 152 | Piperitol (sesamin metabolite) | rat aorta | NR | d | + | [119] | |||||
| 153 | Plagiochin A | rat aorta | NR | d | + | [56] | |||||
| 154 | Polygodial | rabbit pulmonary | NR | d | + | x | x | [37] | |||
| rat portal | - | -VOCC/ | [38] | ||||||||
| 155 | Pomolic acid | rat aorta | 2.45 μM 5 | d | + | x | +KATP | [199] | |||
| 156 | (+) Praeruptorin A | rat aorta | 35.4 ± 3.6 µM 1 | d | + | x | - VOCC,- ROCC/ -IP3R |
[200] | |||
| 157 | (−) Praeruptorin A | rat aorta | 45.8 ± 2.5 µM 1 | i | x | x | -VOCC, -ROCC/ -IP3R |
[200] | |||
| 158 | Proanthocyanidins* | rat aorta | NR | d | + | [50] | |||||
| 159 | Procyanidins* | human internal mammary | NR | d | + | + | +KATP, +SKCa, +KV, +KIR |
[201] | |||
| rat aorta | d | + | [202] | ||||||||
| porcine coronary | + | + | [203] | ||||||||
| 160 | Protosappanin D | rat aortarat mesenteric | NR | d/i | + | + | [85] | ||||
| 161 | Puerarin | rat basilar | 304 ± 49 µM 3 | d/i | + | x | + | x/ | [115] | ||
| 162 | Quercetin | rat aorta | NR | i | x + + x |
+ x |
x | - | +BKCa | [24] | |
| rat coronary | 3 mM 7 | d/i | [25] | ||||||||
| pig coronary | NR | i | [27] | ||||||||
| rat aorta | 4.68 ± 0.08 §,5 | i | [163] | ||||||||
| rat mesenteric | 5.35 ± 0.15 §,5 | i | [163] | ||||||||
| rat aorta | 4.36 ± 0.05 §,1 | d | [204] | ||||||||
| rat portal | 59.5 ± 11.1 µM 4 | i | [205] | ||||||||
| 163 | Quercetin 3,7-dimethyl ether | rat aorta | 4.70 ± 0.18 §,1 | d | + | [206] | |||||
| 164 | Quercetine-3-O-galactoside | rat basilar | 20.4 ± 4.49 µM 3 | d/i | + | + | + | [207] | |||
| 165 | Resveratrol | rat aorta | 4.52 ± 0.11 §,1 4.99 ± 0.11 §,1 |
i | + | +KV +KV |
-VOCC/ | [35] | |||
| rat aorta | d/i | [208] | |||||||||
| rat mesenteric | d/i | [209] | |||||||||
| 166 | Reticuline | rat aortarat aorta | 40 ± 10 µM 1 NR |
d/i | + | x | - VOCCL/- IP3R -VOCCL/ |
[63] [210] |
|||
| 167 | Rhynchophylline | rat aorta | 20–30 µM 2 | i | x | - VOCCL/- IP3R,- RyR | [164] | ||||
| 168 | Riccardin A | rat aorta | NR | d | + | [56] | |||||
| 169 | Riccardin C | rat aorta | NR | d | + | [56] | |||||
| 170 | Riccardin F | rat aorta | NR | d | + | [56] | |||||
| 171 | Roseoside | rat aorta | NR | d | + | [55] | |||||
| 172 | Rotundifolone | rat aorta | 184 ± 6 µg/mL 1 | d/i | + | + | +BKCa | - VOCCL/- IP3R -VOCCL/ |
[40] | ||
| rat aorta | NR | i | [41] | ||||||||
| rat mesenteric | 4.0 ± 0.02 §,1 | d/i | [42] | ||||||||
| 173 | Rutaecarpine | rat aorta | NR | d | + | x | -/- - VOCCL/- IP3R |
[43] | |||
| rat aorta | d | + | [44] | ||||||||
| rat aorta | [45] | ||||||||||
| 174 | Rutin | rat mesenteric rat aorta | NR | d | + | + | +KATP | [211] | |||
| 175 | Salvianolic acid B | rat coronary | 147.9 ± 17.4 µg/mL 6 | i | + | -VOCC/ | [212] | ||||
| 176 | Sanguinarine | rat aorta | 3.18 ± 0.37 µM 1 | i | -VOCC, -ROCC/ -IP3R |
[213] | |||||
| 177 | Saponins from Ginseng* | NR | -ROCC/ | [49] | |||||||
| 178 | Sappanchalcone | rat aortarat mesenteric | NR | d | + | + | [85] | ||||
| 179 | Saucerneol | rat aorta | 2.2 µM | d | + | [182] | |||||
| 180 | Saucerneol D | rat aorta | 12.7 µM | d | + | [182] | |||||
| 181 | Scirpusin B | rat aorta | NR | d | + | [214] | |||||
| 182 | Scutellarin | rat aorta | 7.7 ± 0.6 µM 5 | i | x | x | x | x | -VOCC/x | [215] | |
| 183 | Senkyunolide A | rat aorta | 4.32 ± 0.10 §,1 | i | x | x | x | [180] | |||
| 184 | S-petasin | rat mesenteric | 6.01 ± 0.08 §,3 | i i |
x x |
x x |
- VOCCL/ - VOCCL/ |
[72] | |||
| rat aorta | 4.76 ± 0.16 §,3 | [72] | |||||||||
| rat aorta | 6.6 ± 1.4 µM 2 | [216] | |||||||||
| 185 | Tetramethylpyrazine | rat aorta | NR | d/i | + + |
+KATP, +SKCa | -VOCC/ | [217] | |||
| rabbit basilar | NR | [218] | |||||||||
| rat aorta | NR | [219] | |||||||||
| rat pulmonary | 522 µM 1 | [220] | |||||||||
| 186 | Tetrandrine | NR | -VOCCL/ | [217] | |||||||
| 187 | Thaligrisine | rat aorta | 23.0 ± 0.39 µM 5 | -VOCC/ | [221] | ||||||
| 188 | Thymol | rat aorta | 106.4 ± 11.3 µM 1 | i | x | - | -VOCC/-IP3R | [96] | |||
| 189 | Tilianin | rat aorta | 240 µM 5 | d/i | + | x | + KV | [222] | |||
| 190 | Trans-dehydrocrotonin | rat aorta | NR | d | + | [223] | |||||
| 191 | Trans-resveratrol | rat aorta | 3.12 ± 0.26 µM 1 | d | + | [224,225] | |||||
| 192 | Ursolic acid | rat aorta | 44.1 ± 6.1 µM 5 | d | + | x | [64] | ||||
| 193 | Villocarine A | rat aorta | NR | d/i | + | + | -VOCC, -ROCC/ |
[226] | |||
| 194 | Vincamedine | rat aorta | NR | d/i | + | x | -VOCC, -ROCC/ |
[227] | |||
| 195 | Visnadine | rat aortarat portal | NR | - | -VOCCL/ | [228] | |||||
| 196 | Visnagin | rat aorta | 22 ± 4 µM 5 | i | - | -VOCCL, -ROCC/ |
[229] | ||||
| -IP3R,-RyR | |||||||||||
| 197 | Vitisin C | rabbit aorta | NR | d | + | [230] | |||||
| 198 | Vulgarenol | guinea pig heart | NR | d | + | [231] | |||||
| 199 | Wine polyphenolic compounds * | rat aorta | 3.27 ± 0.02 §,5 | d | + | x | + | [47,178] | |||
| 200 | Xanthoangelol | rat aorta | NR | d | + | -VOCC/ | [53] | ||||
| 201 | Xanthoangelol B | rat aorta | NR | i | x | -VOCC/ | [53] | ||||
| 202 | Xanthoangelol E | rat aorta | NR | d | + | -VOCC/ | [53] | ||||
| 203 | Xanthoangelol F | rat aorta | NR | d | + | -VOCC/ | [53] | ||||
| 204 | Xanthone | rat aorta | 60.26 ± 8.43 µM 5 | i | ↑cAMP | -VOCC, -ROCC/x |
[232] | ||||
| 205 | Xanthorrhizol | rat aorta | NR | i | x | x | -VOCC, -ROCC/ |
[233] | |||
| 206 | Zearalanone | rabbit coronary | NR | i | -VOCC/ | [149] | |||||
| 207 | (Z)-3-methylthioacrylic ester of 2beta-hydroxy-8betaH-7(11)-eremophilene-12,8-olide | rat mesentericrat aorta | 5.24 ± 0.13 §,3
4.26 ± 0.17 §,3 |
i | x | x | -VOCCL/ | [72] |
Abbreviations: d, endothelium-dependent; i, endothelium-independent; +, activation; -, inactivation; x, without involvement; EC50, median effective concentration; NO/cGMP, NO/cGMP pathway; PGI2/cAMP, PGI2/cAMP pathway; PDE, phosphodiesterase; PKC, protein kinase C; Ca2+ext, extracellular Ca2+ influx; Ca2+int, Ca2+ release from intracellular stores; ↑cGMP, increased levels of cGMP; ↑cAMP, increased levels of cAMP; BKCa, high-conductance Ca2+ activated K+ channels; IKCa, intermediate-conductance Ca2+-activated K+ channels; SKCa, low-conductance Ca2+-activated K+ channels; KATP, ATP-dependent K+ channels; KIR, inwardly rectifying K+ channels; KV, voltage-dependent K+ channels; VOCC, voltage-operated Ca2+ channels, VOCCL, L-type voltage-operated Ca2+ channels; ROCC, receptor-operated Ca2+ channels; IP3R, inositol triphosphate receptor; RyR, caffeine/ryanodine receptor. EC50 determined in tissues precontracted with 1 phenylephrine, 2 KCl, 3 U46619, 4 prostaglandin F2α, 5 norepinephrine, 6 5-hydroxytryptamine, 7 4-aminopyridine. § pD2 (−log EC50); ǂ pIC30 (−log IC30). NR, not reported; No symbol, not investigated; * Mixtures of compounds obtained from a single plant species.
5. Participation of the Endothelium in the Mechanism of Action
The vascular endothelium synthesizes and releases a broad spectrum of vasoactive substances and plays a fundamental role in the regulation and maintenance of cardiovascular homeostasis [57]. Among the main endothelial-derived factors that relax arterial smooth muscle are NO [58,59], PGI2 [59,60] and the EDH mechanism, which is associated with calcium-activated potassium channel activation [59,61]. Approximately one third of the compounds analyzed utilized both endothelium-dependent and endothelium-independent mechanisms (Table 1). Moreover, among the compounds that produce their vasodilator effect by an endothelium-dependent mechanism, a high percentage (98.4%) involved the NO/cGMP pathway, whereas the PGI2/cAMP pathway was involved in the mechanism used by a low percentage (23%) of the vasodilating compounds (Table 1). Among the 130 compounds whose mechanism of action was endothelium-dependent, assays for evaluating the participation of endothelial muscarinic receptors were performed in only 18. Four of these compounds involved the participation of this kind of receptors: diosgenin [62], reticuline [63], rotundifolone [40] and ursolic acid [64].
6. Compounds Acting on the NO/cGMP Pathway
Although three distinct isoforms of NO synthase (NOS) have been identified (endothelial, eNOS; inducible, iNOS; and neuronal, nNOS), it has generally been accepted that regulation of vascular tone is primarily dependent upon the release of NO from eNOS [234]. However, some studies have suggested that nNOS [235] and iNOS [236] may also be involved in this process. Therefore, NO synthesis can be modulated by regulating the activity or gene expression of the three NOS isoforms [237]. NO, produced by these enzymes, dilates all types of blood vessels by stimulating sGC and increasing cGMP in smooth muscle cells [238].
6.1. Compounds that Regulate eNOS Expression
Although eNOS was initially characterized as a constitutive enzyme of the vascular endothelium, there is evidence to suggest that the expression of this enzyme can be regulated by physiological stimuli or by the actions of certain compounds [239,240]. Some of the compounds obtained from plants that regulate the gene expression of eNOS are betulinic acid, a pentacyclic triterpene isolated from Zizyphi spinosi, a plant used in traditional Chinese medicine for the treatment of cardiovascular diseases [241]; several flavonoids, such as cynaroside and luteolin, which are constituents of the plants Cynara scolymus L. (artichoke) and Prunella vulgaris [242,243]; alkaloids, such as keayanidine B and keayanine, isolated from Microdesmis keayana, an African tropical plant whose roots are used in traditional medicine for treating erectile dysfunction [172]; and other metabolites, such as piceatannol [244].
In general, assays for determining the contributions of these compounds to the regulation of eNOS gene expression have been performed on endothelial cells from the human umbilical cord vein (the EA. hy926 cell line) [244]. For example, in the study of icariin, a flavonoid isolated from Epimedii herba, this cell line was cultured in the presence of different concentrations of it. Subsequently, reverse transcriptase PCR and western blot techniques were used to determine the change in the levels of mRNA and protein of eNOS, respectively. The results indicated that after incubation for 12 h in the presence of icariin, both the mRNA expression and the protein levels of eNOS increased significantly as a function of time and concentration. Additionally, icariin induced a significant relaxation on rat aorta and canine coronary artery [158,159].
6.2. Compounds that Regulate eNOS Activity
In general, assessment of the participation of the NO/cGMP pathway is accomplished through the use of inhibitors of eNOS and sGC. In the case of eNOS, the most commonly inhibitor used is Nω-nitro-L-arginine methyl ester (L-NAME) or some other derivatives, such as NG-monomethyl-L-arginine (L-NMMA) [82,162]. In the case of sGC, 1H-[1,2,4]oxadiazole[4,3-a]quinoxaline-1-one (ODQ) or methylene blue [125] are the most commonly used inhibitors.
The tissues commonly used to test the effects of compounds on the NO/cGMP pathway are isolated rat thoracic aorta rings or arteries from the mesenteric artery bed [126,187]. However, other tissues have been used, such as rat basilar artery [115], rabbit thoracic aorta [230], porcine coronary artery [113], canine coronary artery [159], and bovine ophthalmic artery [31]. An example of a study where both models, the isolated aorta and the mesenteric artery bed, were employed comprises evaluation of the vasodilator effect of alpha-terpineol and methyl eugenol, which were obtained from the essential oil of Croton nepetaefolius. It was found that the NO/cGMP pathway was involved in the vasodilatory activity of these compounds, as the pathway was inhibited in the presence of L-NAME and methylene blue [67].
An example of a compound whose mechanism of action involves activation of eNOS is brazilin, a homoisoflavonoid obtained from Caesalpinia sappan L. This metabolite induced an increase in cGMP levels and vasodilation of the aorta in a concentration-dependent manner. The effect of brazilin has also been studied in cultured endothelial cells from the umbilical cord vein. In these cell cultures, brazilin induced a concentration-dependent increase in eNOS activity by causing an elevation of intracellular Ca2+ in endothelial cells, thus stimulating calmodulin, which in turn activated eNOS [84]. A similar mechanism of action was proposed for gomisin A, a lignane obtained from Schisandra chinensis; however, in this case, human coronary endothelial cells were used to determine the activation of eNOS [245].
Mechanisms that activate eNOS through the phosphatidylinositol-3-kinase/protein kinase B (PIK3/Akt) pathway have also been proposed. The vasodilator effect of epigallocatechin-3-gallate, the most abundant catechin in tea (Camellia sinensis), was dramatically reduced by the PIK3 inhibitor wortmannin and the Akt inhibitor SH6, suggesting that this compound activates the NO/cGMP pathway by inducing the phosphorylation of eNOS [31]. Moreover, this mechanism has also been suggested to account for the vasodilatory activity of proanthocyanidins from the persimmon leaf, quercetin and resveratrol. The effect of these metabolites was studied in diverse cultured endothelial cells and results have pointed out that these compounds induced vasorelaxation through the endothelium-dependent NO/cGMP pathway via sequential phosphorylation of Akt [28,36,50].
6.3. Compounds that Regulate the Activity and Expression of sGC
The results of some studies have suggested that the vasodilator effects of certain compounds produced from plants are mediated by the activation of sGC and, therefore, by an increase in cGMP levels. The levels of sGC have been quantified on rings of isolated rat aortas using immunological techniques [45,162]. In this context, it has been proposed that isoliquiritigenin, a chalcone isolated from Dalbergia odorifera, relaxes the aorta by an endothelium-independent mechanism. Furthermore, incubation of the aorta with this chalcone caused an increase in cGMP levels and a slight increase in cAMP [162]. It has also been proposed that the metabolites emodin and osthole produce their vasodilator effects through a mechanism of action involving increased levels of sGC [127,195].
About 40% of the compounds showed more than one mechanism of action (Table 1). For example, alpinetin and cardamonin exert their relaxing effects through both endothelium-dependent and endothelium-independent mechanisms, the former by activation of the NO/cGMP pathway and the latter through the non-selective inhibition of Ca2+ channels in smooth muscle cells and the inhibition of the contractile mechanism dependent on protein kinase C (PKC) [69]. Similar mechanisms have been proposed for citral and formononetin; both compounds induced relaxation in rat aortic rings through an endothelium-dependent manner via the nitric oxide pathway, and also involving endothelium-independent vasodilatation by the blockade of Ca2+ channels [102,145].
It has also been suggested that the involvement of different mechanisms could depend on the concentration of the metabolite. Low concentrations of caffeic acid phenylethyl ester (CAPE), one of the main components of propolis, induce a relaxing effect on vascular smooth muscle through the activation of the NO/cGMP pathway. In contrast, high concentrations of this compound induce vasodilation in an endothelium-independent manner, likely due to the inhibition of Ca2+ entry into the cytoplasm of muscle cells or due to the inhibition of the release of this cation from intracellular stores [91].
Moreover, the mechanism of action depends on the type of vascular bed and species variations. In this sense it has been demonstrated that vascular relaxation attributable to NO is most prominent in large vessels such as the aorta, while in resistance vessels that regulate blood pressure more directly, NO’s effects are less evident [246]. As an example of the influence of species variations on the action of compounds that affect NO expression, it was shown that resveratrol induced down-regulation of eNOS gene expression in human endothelial cells [247], in contrast, this compound increased eNOS protein expression in bovine endothelial cells [248]. On the other hand, imperatorin, a coumarin obtained from Angelica dahurica var. formosana, induced an endothelium-independent relaxation in rat mesenteric arterial rings by blocking the voltage-dependent calcium channel and the receptor-mediated Ca2+ influx and Ca2+ release [160]. However, in mouse thoracic aorta this coumarin elicited vasodilatation via an endothelium-dependent mechanism involving the nitric oxide pathway [161].
Some studies have conducted in vivo assays in addition to tests on isolated tissues. Chrysin glucoside, isolated from the leaves and flowers of Calycotome villosa, has been observed to have an endothelium-dependent vasodilator effect on isolated rat aortas and a hypotensive effect when administered intravenously to rats [249]. The results of the in vivo assays suggest that the hypotensive effect is probably due to increased vascular relaxation [22,63,76,107,119,136,165].
7. Compounds that Activate the PGI2/cAMP Pathway
Few studies have proposed the activation of the PGI2/cAMP pathway as a mechanism for the vasodilator effects of plant-derived compounds. PGI2 is an endogenous vasoactive eicosanoid produced by cyclooxygenase (COX) from arachidonic acid in endothelial cells; its production is stimulated by endogenous agonists such as serotonine, histamine, bradykinin and acetylcholine. In addition to inhibiting platelet aggregation, PGI2 also causes relaxation of vascular smooth muscle through stimulation of a G-protein-coupled receptor that, in turn, activates adenylyl cyclase (AC) and thus raises cAMP levels, inducing vasodilation as a result [250]. The participation of this pathway is determined by using indomethacin as an inhibitor of the COX enzyme [82,154]. Some compounds whose mechanism of action involves the activation of this pathway at the level of the endothelium are ethyl cinnamate, isolated from the rhizomes of Kaempferia galanga [104]; eudesmin, a lignan obtained from Piper truncatum [135]; labdane-302, a diterpene obtained from Xylopia langsdorffiana [174]; rutin [211]; and procyanidins, derived from grape seeds [201].
The vasodilator activity of procyanidins was evaluated in human internal mammary aortic rings. It was determined that both the NO/cGMP and the PGI2/cAMP pathways were involved in this process through experiments using inhibitors of eNOS (L-NMMA) and sGC (ODQ) for the first pathway and COX (indomethacin) for the second one. The vasodilator effect of procyanidins was eliminated by the removal of the endothelium. Additionally, inhibition of COX produced a 50% decrease in the vasodilatory activity of these compounds, suggesting the involvement of the PGI2/cAMP pathway in their mechanism of action. Subsequent experiments confirmed this finding by observing an increase in PGI2 release, which was dependent on the concentration of procyanidins [201].
Other studies have suggested that some natural compounds produce a vasodilator effect by directly activating AC or increasing cAMP levels in smooth muscle cells. The experimental protocols of these studies aimed to evaluate the effects of both an AC inhibitor (SQ22536) and an inhibitor of cAMP-dependent protein kinase (PKA) (KT5720) on the vasodilation produced by the test compound [79]. Additionally, analogs and antagonists of cyclic nucleotides have been used in the evaluation of these pathways [251]. For example, puerarin, an isoflavone isolated from Radix puerariae that was evaluated using porcine coronary artery rings, was able to shift the dose-response curve of sodium nitroprusside (SNP) to the left. This effect was independent of the endothelium. The SNP-induced relaxation was enhanced by the cAMP analog, 8-Br-cAMP, at a rate similar to that of puerarin, suggesting the involvement of the PGI2/cAMP pathway in the increased vasodilatory activity. Moreover, the cAMP antagonist Rp-8-Br-cAMP decreased the vasoactive effect of this isoflavone. In this case, analogs of cGMP (agonists or antagonists) had no effect on the activity of puerarin. Based on these results, it was suggested that the mechanism of action whereby this isoflavone increases vasodilation in the porcine coronary artery is the activation of the PGI2/cAMP pathway [251].
8. Compounds that Inhibit Phosphodiesterases (PDEs)
Cyclic nucleotide phospodiesterases (PDEs) are enzymes that regulate the cellular levels of cAMP and cGMP by controlling their rates of degradation [252]. The major PDEs in arterial smooth muscle are PDE1, PDE3, PDE4 and PDE5; specifically, PDE5 has been found to be a major cGMP-hydrolizing PDE expressed in smooth muscle cells. The inhibition of PDEs produces vasorelaxant effects by increasing cyclic nucleotide levels [252,253,254].
Several compounds, mostly flavonoids, have been described as PDE inhibitors and vasodilators [18,23,29,157]. The involvement of PDEs in the vasorelaxant effect of these compounds was evaluated by measuring the change on PDE activity. PDEs have been isolated from the cytosolic fraction of bovine aortic smooth muscle [18,23] or rat aorta [87] and their activities were measured by radioenzimatic assays [255].
Specific PDEs were inhibited by different compounds. For example, the vasorelaxant effect of dioclein inhibited PDE1, and to a lesser extent PDE4 and PDE5 [23]; meanwhile, epigallocatechin-3-gallate showed activity over PDE1 and PDE2 [29], while butein, a chalcone obtained from Dalbergia odorifera, inhibited PDE4 only [87].
9. Compounds that Activate K+ Channels
The K+ channels in vascular smooth muscle play an important role in vasodilation because the outflow of K+ through these channels hyperpolarizes the membrane and thereby inhibits the entry of Ca2+. This process eventually results in the relaxation of blood vessels [256]. Four different types of potassium channels have been characterized in arterial smooth muscle: voltage-dependent channels (KV), Ca2+-activated channels (large-conductance, BKCa; intermediate-conductance, IKCa; and small-conductance, SKCa), ATP-dependent channels (KATP) and inwardly rectifying channels (KIR) [257,258,259,260]. It is worth mentioning that there is evidence for cell to cell, segment to segment, and vascular bed to bed diversity of K+ channels that could explain the varying responses of arterial segments or different arteries to stimuli such as hypoxia, vasoactive drugs, or arterial wall injury [261,262,263].
The involvement of different types of K+ channels has been evaluated by the use of channel-specific blockers. The following are the most commonly used blockers of K+ channels: chloride tetraethylammonium (TEA) and BaCl2 as nonselective inhibitors [22,86]; glibenclamide, an inhibitor of KATP channels; aminopyridine (4-AP), which blocks KV channels; and iberiotoxin [35] and charybdotoxin, which block BKCa channels [42,98]. In addition, TEA [82], BaCl2 [22], and apamin [31] have been used to block BKCa, KIR, and SKCa channels, respectively.
BKCa, highly expressed in vascular smooth muscle cells [258], can be activated by both, the NO/cGMP pathway [264] and EDHF [265]. These channels play a key role in blood pressure regulation and therefore, they have been suggested as novel potential drug targets for the treatment of cardiovascular diseases [266]. Recently, a considerable number of natural compounds, especially of the flavonoid type, have been shown to have a vasodilator effect caused, at least in part, by activation of BKCa channels [19,22,198,267,268]. Other compounds with different chemical structures that activate this kind of potassium channels are: diosgenin (steroid sapogenin) [62]; piceatannol (stilbene) [32], isolated from the root of Rheum undulatum; and rotundifolone (monoterpene) [42], the major constituent of the essential oil of Mentha x villosa Hudson.
The study of compounds that activate K+ channels also includes the use of electrophysiological techniques, both to demonstrate these compounds’ role as stimulants and to characterize the type of channels involved in their vasodilator mechanisms. The most common strategy is the patch-clamp technique used on isolated muscle cells [116] or in Xenopus oocytes that express K+ channels from other organisms [269]. For example, the elucidation of the mechanism of action of rotundifolone was carried out in rat superior mesenteric arteries. For investigating the involvement of K+ channels in the vasorelaxant mechanism, several specific channel blockers were used such as TEA, charybdotoxin, 4-AP and glibenclamide. In addition, electrophysiological testing using the patch-clamp technique in mesenteric smooth muscle cells was used to identify the channels activated by rotundifolone. The results indicated that the vasodilator effect of this compound involves the participation of BKCa channels [42]. However, it has been shown that the use of the patch-clamp technique induces apparent phenotypic changes, particularly when it is used on isolated and cultured cells, compared to data derived from intact tissue. Consequently, data gathered in this manner should be interpreted with caution [270].
10. Compounds that Decrease Intracellular Ca2+ Concentration
The mechanism of vascular smooth muscle contraction involves the participation of different signal transduction pathways, all of which converge to increase cytoplasmic Ca2+ concentrations. The concentration of this cation increases both by extracellular Ca2+ entering through voltage-operated Ca2+ channels (VOCCs) and receptor-operated Ca2+ channels (ROCCs), and by the release of Ca2+ from intracellular stores [123]. Therefore, the mechanisms of action associated with vasodilating agents that decrease intracellular Ca2+ concentration involve blocking VOCCs and ROCCs or inhibiting the release of this cation from intracellular stores. The experimental strategy to determine the involvement of Ca2+ channels in the vasodilating effect of test compounds involves incubating aortic rings in a Ca2+-free medium containing a high concentration of K+ and to which CaCl2 is gradually added to induce contraction, both in the absence and presence of the vasodilating compound [79,123].
Different techniques are used to determine the involvement of VOCCs, ROCCs or the release of intracellular calcium. The inhibitory action of vasodilator compounds on VOCCs can be seen as a rightward shift in the dose-response curve for CaCl2, as noted in the case of ligustilide, a compound extracted from Ligusticum chuanxiong, a plant used in traditional Chinese medicine [179], and naucline, an alkaloid derived from Nauclea officinalis [89]. For evaluating the involvement of ROCCs, dose-response curves are performed in the presence of an adrenergic agonist, such as noradrenaline (NA) [123] or phenylephrine (PE) [56] to induce contractions, both in the absence and the presence of the vasodilator compound [89,123]. In addition, the contribution of Ca2+ released from intracellular stores is determined by incubating the tissue in a Krebs solution free of Ca2+ and to which NA is subsequently added to induce phasic contractions with calcium from the sarcoplasmic reticulum. Subsequently, once the contraction is stabilized, CaCl2 is added to induce a tonic contraction. When incubating segments of the aorta with the test compound under these conditions, a decrease of phasic contractions signals that the effect is produced by the outflow of intracellular Ca2+, whereas a decrease in tonic contraction signals that the effect is mediated by Ca2+ entry through ROCCs [185].
The release of Ca2+ from intracellular stores is regulated by the inositol-1,4,5-triphosphate (IP3) system and by the ryanodine receptors (RyRs). RyRs system are a Ca2+ release system where Ca2+ release is induced by the presence of Ca2+ when the receptors are activated by caffeine [179]. For example, isopropyl-3-(3,4-dihydroxyphenyl)-2-hydroxypropanoate has been shown to inhibit both KCl-induced and norepinephrine-induced contractions in the absence and presence of Ca2+ in the rat mesenteric artery. These results suggest that in addition to its activity on VOCCs, this compound also acts on ROCCs and on intracellular calcium stores [123]. In this type of study, blockers of L-type Ca2+ channels, such as nifedipine [271] or diltiazem [154], are used as a positive control. However, calycosin, the main component of Astragali radix, was shown to inhibit CaCl2-induced vasoconstriction in the presence of KCl and PE but did not affect PE-induced contractions in a calcium-free medium. These results indicated the involvement of VOCCs and ROCCs in the vasodilator effect produced by calicosin, excluding the outflow of intracellular Ca2+ [93]. In contrast, low concentrations of euxanthone, a metabolite isolated from Polygala caudate, inhibited the phasic contraction, suggesting that the exit of Ca2+ from the endoplasmic reticulum is involved in the relaxing activity [139]. Moreover, both cardamonin and alpinetin can inhibit the transient contractions produced by PE and caffeine in a Ca2+-free medium and also the contractions induced by K+. The authors suggest that these compounds act through the nonspecific inhibition of Ca2+ entry and the release of intracellular Ca2+ [69].
Other methodologies have been used to elucidate the mechanisms of action of vasoactive compounds. For example, the involvement of VOCCs in the vasodilator mechanism of marrubenol, a diterpene extracted from Marrubium vulgare, was confirmed by recording the inflow current through calcium channels using patch-clamp and fluorescence techniques [183].
11. Compounds that Activate Endothelial Transient Receptor Potential (TRP) Cation Channels
Transient receptor potential (TRP) cation channels are currently considered as the leading candidate proteins mediating diverse non-voltage-gated calcium entry pathways in vascular endothelium and smooth muscle [272,273]. The TRP superfamily contains three major subfamilies based on sequence homology: TRPV (vanilloid), TRPC (canonical), and TRPM (melastatin). Moreover, three additional subfamilies (the “distant TRPs”), TRPP (polycystin), TRPML (mucolipin), and TRPA (ankyrin) have been proposed [274]. In particular, the endothelial TRP channels are exposed to different agonists that enter the blood stream as dietary molecules. Some of these molecules, found in commonly consumed food and plants used in traditional medical practices of several cultures are able to activate these kinds of channels [97,272,273]. Carvacrol, one of the major components of oregano (Origanum vulgare) essential oil, induces an endothelium-dependent vasodilation by activating TRPV3 [97]. Recently, it has been reported that allyl isothiocyanate, which is found in the seeds of mustard (Brassica nigra and B. juncea) causes endothelium-dependent vasodilation of rat cerebral arteries by a mechanism involving TRPA1 activation [66].
12. Compounds that Inhibit Protein Kinase C
The mechanism of vascular smooth muscle contraction evokes the phosphorylation of myosin light chain by increasing intracellular Ca2+ concentration. Additionally, the decrease of the myosin light chain phosphatase (MLCP) increases the sensitivity to Ca2+ [275]. Several pathways have been suggested for the Ca2+ sensing mechanism. One of them is the PKC/CPI-17 pathway [276]. PKC phosporilates CPI-17, enhancing its inhibitory activity over MLCP [276] and producing a sustained contraction. PKC has been found in high concentrations in vascular smooth muscle and can be activated by diacylglicerol [277].
Only a few compounds have been found to evoke their vasorelaxant activity through this mechanism; in all cases, PKC inhibition was not the only mechanism. The participation of PKC in the vasorelaxant mechanism has been evaluated using activators of PKC in smooth muscle cells, such as phorbol esters. 12-O-tetradecanoyl phorbol 13-acetate, phorbol 12-myristate-13-acetate (PMA) and phorbol 12,13-dibutyrate (PDB) were used to evaluate the vasorelaxant mechanisms for dioclein [21], quercetin [24] and euxanthone [139], respectively. This last activator was used also in the characterization of the mechanism of action for thymol and carvacrol: PDB induced a sustained contraction that was attenuated when thymol or carvacrol were added (300 and 1,000 µM) [96].
13. Conclusions
The present review focused on the mechanisms of action responsible for the vasodilator activity of plant-derived compounds. From the information obtained, we identified the main mechanisms of action of most of the vasodilator compounds; these mechanisms are the activation of the NO/cGMP and PGI2/cAMP pathways, the activation of K+ channels and the blockade of voltage-dependent Ca2+ channels.
It should be noted that more than one mechanism of action has been proposed to be involved in the vasodilator effect of almost half of all of the analyzed compounds. This finding suggests that compounds derived from plants may have great therapeutic potential as they involve multiple mechanisms of action in their vascular relaxing activity. In this context, it is critical to emphasize the importance of understanding the different mechanisms of action in order to establish new therapeutic strategies for addressing various cardiovascular diseases.
Finally, given the structural diversity of the active compounds derived from natural products and the diversity of mechanisms of action responsible for their vasodilator activity, it is important to continue the search for new active substances that help in the treatment of cardiovascular diseases.
Acknowledgments
Francisco J. Luna-Vázquez acknowledges Consejo Nacional de Ciencia y Tecnología (CONACYT) for his Ph. D. scholarship.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Nguelefack T.B., Dongmo A.B., Dimo T., Kamanyi A. Phytopharmacology of Some Medicinal Plants Used in Cameroonian Traditional Medicine to Handle Cardiovascular Diseases. In: Capasso A., editor. Recent Developments in Medicinal Plants Research. Research Signpost Publisher; Kerala, India: 2007. [Google Scholar]
- 2.Cogolludo A., Pérez-Vizcaíno F., Tamargo J. New insights in the pharmacological therapy of arterial hypertension. Curr. Opin. Nephrol. Hypertens. 2005;14:423–427. doi: 10.1097/01.mnh.0000168334.09454.1c. [DOI] [PubMed] [Google Scholar]
- 3.Brunner H., Cockcroft J.R., Deanfield J. Endothelial function and dysfunction. Part II: association with cardiovascular risk factors and diseases. A statement by the Working Group on Endothelins and Endothelial factors of the European Society of Hypertension. J. Hypertens. 2005;23:233–246. doi: 10.1097/00004872-200502000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Dominiczak A.F., Bohr D.F. Nitric oxide and its putative role in hypertension. Hypertension. 1995;25:1202–1211. doi: 10.1161/01.hyp.25.6.1202. [DOI] [PubMed] [Google Scholar]
- 5.Miles A.M., Bohle D.S., Glassbrenner P.A., Hansert B., Wink D.A., Grisham M.B. Modulation of superoxide-dependent oxidation and hydroxylation reactions by nitric oxide. J. Biol. Chem. 1996;271:40–47. doi: 10.1074/jbc.271.1.40. [DOI] [PubMed] [Google Scholar]
- 6.Bauersachs J., Bouloumie A., Fraccarollo D., Busse R., Ertl G. Endothelial dysfunction in chronic myocardial infarction despite increased vascular endothelial nitric oxide synthase and soluble guanylate cyclase expression: role of enhanced vascular superoxide production. Circulation. 1999;100:292–298. doi: 10.1161/01.CIR.100.3.292. [DOI] [PubMed] [Google Scholar]
- 7.Vanhoutte P.M., Shimokawa H., Tang E.H.C., Feletou M. Endothelial dysfunction and vascular disease. Acta Physiol. 2009;196:193–222. doi: 10.1111/j.1748-1716.2009.01964.x. [DOI] [PubMed] [Google Scholar]
- 8.Versari D., Daghini E., Virdis A., Ghiadoni L., Taddei S. Endothelium-dependent contractions and endothelial dysfunction in human hypertension. Br. J. Pharmacol. 2009;157:527–536. doi: 10.1111/j.1476-5381.2009.00240.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kloss S., Bouloumie A., Mulsch A. Aging and chronic hypertension decrease expression of rat aortic soluble guanylyl cyclase. Hypertension. 2000;35:43–47. doi: 10.1161/01.HYP.35.1.43. [DOI] [PubMed] [Google Scholar]
- 10.Tsai E.J., Kass D.A. Cyclic GMP signaling in cardiovascular pathophysiology and therapeutics. Pharmacol. Ther. 2009;122:216–238. doi: 10.1016/j.pharmthera.2009.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Crawley D.E., Zhao L., Giembycz M.A., Liu S., Barnes P.J., Winter R.J., Evans T.W. Chronic hypoxia impairs soluble guanylyl cyclase-mediated pulmonary arterial relaxation in the rat. Am. J. Physiol. 1992;263:L325–L332. doi: 10.1152/ajplung.1992.263.3.L325. [DOI] [PubMed] [Google Scholar]
- 12.Tzao C., Nickerson P.A., Russell J.A., Gugino S.F., Steinhorn R.H. Pulmonary hypertension alters soluble guanylate cyclase activity and expression in pulmonary arteries isolated from fetal lambs. Pediatr. Pulmonol. 2001;31:97–105. doi: 10.1002/1099-0496(200102)31:2<97::AID-PPUL1016>3.0.CO;2-K. [DOI] [PubMed] [Google Scholar]
- 13.Marijic J., Li Q., Song M., Nishimaru K., Stefani E., Toro L. Decreased expression of voltage- and Ca (2+)-activated K(+) channels in coronary smooth muscle during aging. Circ. Res. 2001;88:210–216. doi: 10.1161/01.RES.88.2.210. [DOI] [PubMed] [Google Scholar]
- 14.Hibino H., Kurachi Y. A new insight into the pathogenesis of coronary vasospasm. Circ. Res. 2006;98:579–581. doi: 10.1161/01.RES.0000215571.12500.ab. [DOI] [PubMed] [Google Scholar]
- 15.Chan E., Woodman O. Enhanced role for the opening of potassium channels in relaxant responses to acetylcholine after myocardial ischaemia and reperfusion in dog coronary arteries. Br. J. Pharmacol. 1999;126:925–932. doi: 10.1038/sj.bjp.0702376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jepps T.A., Chadha P.S., Davis A.J., Harhun M.I., Cockerill G.W., Olesen S.P., Hansen R.S., Greenwood I.A. Downregulation of Kv7.4 channel activity in primary and secondary hypertension. Circulation. 2011;124:602–611. doi: 10.1161/CIRCULATIONAHA.111.032136. [DOI] [PubMed] [Google Scholar]
- 17.Sánchez de Rojas V.R., Somoza B., Ortega T., Villar A.M. Different mechanisms involved in the vasorelaxant effect of flavonoids isolated from Satureja obovata. Planta Med. 1996;62:554–556. doi: 10.1055/s-2006-957969. [DOI] [PubMed] [Google Scholar]
- 18.Orallo F., Camiña M., Alvarez E., Basaran H., Lugnier C. Implication of cyclic nucleotide phosphodiesterase inhibition in the vasorelaxant activity of the citrus-fruits flavonoid (+/−)-naringenin. Planta Med. 2005;71:99–107. doi: 10.1055/s-2005-837774. [DOI] [PubMed] [Google Scholar]
- 19.Saponara S., Testai L., Iozzi D., Martinotti E., Martelli A., Chericoni S., Sgaragli G., Fusi F., Calderone V. (+/−)-Naringenin as large conductance Ca(2+)-activated K+ (BKCa) channel opener in vascular. Br. J. Pharmacol. 2006;149:1013–1021. doi: 10.1038/sj.bjp.0706951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lemos V.S., Freitas M.R., Muller B., Lino Y.D., Queiroga C.E., Côrtes S.F. Dioclein, a new nitric oxide- and endothelium-dependent vasodilator flavonoid. Eur. J. Pharmacol. 1999;386:41–46. doi: 10.1016/S0014-2999(99)00747-5. [DOI] [PubMed] [Google Scholar]
- 21.Trigueiro F., Cortes S.F., Almeida R.N., Lemos V.S. Endothelium-independent vasorelaxant effect of dioclein, a new flavonoid isolated from Dioclea grandiflora, in the rat aorta. J. Pharm. Pharmacol. 2000;52:1431–1434. doi: 10.1211/0022357001777441. [DOI] [PubMed] [Google Scholar]
- 22.Côrtes S.F., Rezende B.A., Corriu C., Medeiros I.A., Teixeira M.M., Lopes M.J., Lemos V.S. Pharmacological evidence for the activation of potassium channels as the mechanism involved in the hypotensive and vasorelaxant effect of dioclein in rat small resistance arteries. Br. J. Pharmacol. 2001;133:849–858. doi: 10.1038/sj.bjp.0704147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gonçalves R.L., Lugnier C., Keravis T., Lopes M.J., Fantini F.A., Schmitt M., Cortes S.F., Lemos V.S. The flavonoid dioclein is a selective inhibitor of cyclic nucleotide phosphodiesterase type 1 (PDE1) and a cGMP-dependent protein kinase (PKG) vasorelaxant in human vascular tissue. Eur. J. Pharmacol. 2009;620:78–83. doi: 10.1016/j.ejphar.2009.08.008. [DOI] [PubMed] [Google Scholar]
- 24.Duarte J., Pérez-Vizcaíno F., Zarzuelo A., Jiménez J., Tamargo J. Vasodilator effects of quercetin in isolated rat vascular smooth muscle. Eur. J. Pharmacol. 1993;239:1–7. doi: 10.1016/0014-2999(93)90968-N. [DOI] [PubMed] [Google Scholar]
- 25.Kubota Y., Tanaka N., Umegaki K., Takenaka H., Mizuno H., Nakamura K., Shinozuka K., Kunitomo M. Ginkgo biloba extract-induced relaxation of rat aorta is associated with increase in endothelial intracellular calcium level. Life Sci. 2001;69:2327–2336. doi: 10.1016/S0024-3205(01)01303-0. [DOI] [PubMed] [Google Scholar]
- 26.Romero M., Jiménez R., Sánchez M., López-Sepúlveda R., Zarzuelo M.J., O'Valle F., Zarzuelo A., Pérez-Vizcaíno F., Duarte J. Quercetin inhibits vascular superoxide production induced by endothelin-1: Role of NADPH oxidase, uncoupled eNOS and PKC. Atherosclerosis. 2008;202:58–67. doi: 10.1016/j.atherosclerosis.2008.03.007. [DOI] [PubMed] [Google Scholar]
- 27.Suri S., Liu X.H., Rayment S., Hughes D.A., Kroon P.A., Needs P.W., Taylor M.A., Tribolo S., Wilson V.G. Quercetin and its major metabolites selectively modulate cyclic GMP-dependent relaxations and associated tolerance in pig isolated coronary artery. Br. J. Pharmacol. 2010;159:566–575. doi: 10.1111/j.1476-5381.2009.00556.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Li P.G., Sun L., Han X., Ling S., Gan W.T., Xu J.W. Quercetin induces rapid eNOS phosphorylation and vasodilation by an Akt-independent and PKA-dependent mechanism. Pharmacology. 2012;89:220–228. doi: 10.1159/000337182. [DOI] [PubMed] [Google Scholar]
- 29.Alvarez E., Campos-Toimil M., Justiniano-Basaran H., Lugnier C., Orallo F. Study of the mechanisms involved in the vasorelaxation induced by (−)-epigallocatechin-3-gallate in rat aorta. Br. J. Pharmacol. 2006;147:269–280. doi: 10.1038/sj.bjp.0706507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Campos-Toimil M., Orallo F. Effects of (−)-epigallocatechin-3-gallate in Ca2+-permeable non-selective cation channels and voltage-operated Ca2+ channels in vascular smooth muscle cells. Life Sci. 2007;80:2147–2153. doi: 10.1016/j.lfs.2007.04.005. [DOI] [PubMed] [Google Scholar]
- 31.Romano M.R., Lograno M.D. Epigallocatechin-3-gallate relaxes the isolated bovine ophthalmic artery: Involvement of phosphoinositide 3-kinase-Akt-nitric oxide/cGMP signalling pathway. Eur. J. Pharmacol. 2009;608:48–53. doi: 10.1016/j.ejphar.2009.02.034. [DOI] [PubMed] [Google Scholar]
- 32.Oh K.S., Ryu S.Y., Kim Y.S., Lee B.H. Large conductance Ca2+-activated K+ (BKCa) channels are involved in the vascular relaxations elicited by piceatannol isolated from Rheum undulatum rhizome. Planta Med. 2007;73:1441–1446. doi: 10.1055/s-2007-990246. [DOI] [PubMed] [Google Scholar]
- 33.Yoo M.Y., Oh K.S., Lee J.W., Seo H.W., Yon G.H., Kwon D.Y., Kim Y.S., Ryu S.Y., Lee B.H. Vasorelaxant effect of stilbenes from rhizome extract of rhubarb (Rheum undulatum) on the contractility of rat aorta. Phytother. Res. 2007;21:186–189. doi: 10.1002/ptr.2042. [DOI] [PubMed] [Google Scholar]
- 34.Wallerath T., Deckert G., Ternes T., Anderson H., Li H., Witte K., Förstermann U. Resveratrol, a polyphenolic phytoalexin present in red wine, enhances expression and activity of endothelial nitric oxide synthase. Circulation. 2002;106:1652–1658. doi: 10.1161/01.CIR.0000029925.18593.5C. [DOI] [PubMed] [Google Scholar]
- 35.Novakovic A., Bukarica L.G., Kanjuh V., Heinle H. Potassium channels-mediated vasorelaxation of rat aorta induced by resveratrol. Basic Clin. Pharmacol. Toxicol. 2006;99:360–364. doi: 10.1111/j.1742-7843.2006.pto_531.x. [DOI] [PubMed] [Google Scholar]
- 36.Wang N., Ko S.H., Chai W., Li G., Barrett E.J., Tao L., Cao W., Liu Z. Resveratrol recruits rat muscle microvasculature via a nitric oxide-dependent mechanism that is blocked by TNFα. Am. J. Physiol. Endocrinol. Metab. 2011;300:E195–E201. doi: 10.1152/ajpendo.00414.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.André E., Malheiros A., Cechinel-Filho V., Yunes R.A., Calixto J.B. Mechanisms underlying the relaxation caused by the sesquiterpene polygodial in vessels from rabbit and guinea-pig. Eur. J. Pharmacol. 1999;386:47–53. doi: 10.1016/S0014-2999(99)00719-0. [DOI] [PubMed] [Google Scholar]
- 38.El Sayah M., Filho V.C., Yunes R.A., Malheiros A., Calixto J.B. Action of polygodial on agonist-induced contractions of the rat portal vein in vitro. J. Cardiovasc. Pharmacol. 2000;35:670–675. doi: 10.1097/00005344-200004000-00022. [DOI] [PubMed] [Google Scholar]
- 39.André E., Malheiros A., Cechinel-Filho V., Yunes R.A., Calixto J.B. Role of nitric oxide and K+ channels in relaxation induced by polygodial in rabbit corpus cavernosum in vitro. J. Cardiovasc. Pharmacol. 2003;41:300–306. doi: 10.1097/00005344-200302000-00020. [DOI] [PubMed] [Google Scholar]
- 40.Guedes D.N., Silva D.F., Barbosa-Filho J.M., Medeiros I.A. Muscarinic agonist properties involved in the hypotensive and vasorelaxant responses of rotundifolone in rats. Planta Med. 2002;68:700–4. doi: 10.1055/s-2002-33795. [DOI] [PubMed] [Google Scholar]
- 41.Guedes D.N., Silva D.F., Barbosa-Filho J.M., Medeiros I.A. Calcium antagonism and the vasorelaxation of the rat aorta induced by rotundifolone. Braz. J. Med. Biol. Res. 2004;37:1881–1887. doi: 10.1590/s0100-879x2004001200014. [DOI] [PubMed] [Google Scholar]
- 42.Silva D.F., Araújo I.G., Albuquerque J.G., Porto D.L., Dias K.L., Cavalcante K.V., Veras R.C., Nunes X.P., Barbosa-Filho J.M., Araújo D.A., et al. Rotundifolone-induced relaxation is mediated by BK(Ca) channel activation and Ca(v) channel inactivation. Basic Clin. Pharmacol. Toxicol. 2011;109:465–475. doi: 10.1111/j.1742-7843.2011.00749.x. [DOI] [PubMed] [Google Scholar]
- 43.Chiou W.F., Chou C.J., Liao J.F., Sham A.Y., Chen C.F. The mechanism of the vasodilator effect of rutaecarpine, an alkaloid isolated from Evodia rutaecarpa. Eur. J. Pharmacol. 1994;257:59–66. doi: 10.1016/0014-2999(94)90694-7. [DOI] [PubMed] [Google Scholar]
- 44.Chiou W.F., Liao J.F., Chen C.F. Comparative study of the vasodilatory effects of three quinazoline alkaloids isolated from Evodia rutaecarpa. J. Nat. Prod. 1996;59:374–378. doi: 10.1021/np960161+. [DOI] [PubMed] [Google Scholar]
- 45.Wang G.J., Wu X.C., Chen C.F., Lin L.C., Huang Y.T., Shan J., Pang P.K. Vasorelaxing action of rutaecarpine: effects of rutaecarpine on calcium channel activities in vascular endothelial and smooth muscle cells. J. Pharmacol. Exp. Ther. 1999;289:1237–1244. [PubMed] [Google Scholar]
- 46.Hu C.P., Xiao L., Deng H.W., Li Y.J. The depressor and vasodilator effects of rutaecarpine are mediated by calcitonin gene-related peptide. Planta Med. 2003;69:125–129. doi: 10.1055/s-2003-37703. [DOI] [PubMed] [Google Scholar]
- 47.Andriambeloson E., Stoclet J.C., Andriantsitohaina R. Mechanism of endothelial nitric oxide-dependent vasorelaxation induced by wine polyphenols in rat thoracic aorta. J. Cardiovasc. Pharmacol. 1999;33:248–254. doi: 10.1097/00005344-199902000-00011. [DOI] [PubMed] [Google Scholar]
- 48.Schmitt C.A., Dirsch V.M. Modulation of endothelial nitric oxide by plant-derived products. Nitric Oxide. 2009;21:77–91. doi: 10.1016/j.niox.2009.05.006. [DOI] [PubMed] [Google Scholar]
- 49.Kwan C.Y. Vascular effects of selected antihypertensive drugs derived from traditional medicinal herbs. Clin. Exp. Pharmacol. Physiol. Suppl. 1995;22:S297–S299. doi: 10.1111/j.1440-1681.1995.tb02925.x. [DOI] [PubMed] [Google Scholar]
- 50.Kawakami K., Aketa S., Sakai H., Watanabe Y., Nishida H., Hirayama M. Antyhipertensive and vasorelaxant effects of water-soluble proanthocyanidins from persimmon leaf tea in spontaneously hypertensive rats. Biosci. Biotechnol. Biochem. 2011;75:1435–1439. doi: 10.1271/bbb.100926. [DOI] [PubMed] [Google Scholar]
- 51.Yung L.M., Leung F.P., Wong W.T., Tian X.Y., Yung L.H., Chen Z.Y., Yao X.Q., Huang Y. Tea polyphenols benefit vascular function. Inflammopharmacology. 2008;16:230–234. doi: 10.1007/s10787-008-8022-y. [DOI] [PubMed] [Google Scholar]
- 52.Wang Y., Shi J.G., Wang M.Z., Che C.T., Yeung J.H. Vasodilatory actions of xanthones isolated from a Tibetan herb. Halenia elliptica. Phytomedicine. 2009;16:1144–1150. doi: 10.1016/j.phymed.2009.03.015. [DOI] [PubMed] [Google Scholar]
- 53.Matsuura M., Kimura Y., Nakata K., Baba K., Okuda H. Artery relaxation by chalcones isolated from the roots of Angelica keiskei. Planta Med. 2001;67:230–235. doi: 10.1055/s-2001-12011. [DOI] [PubMed] [Google Scholar]
- 54.Shi C.C., Liao J.F., Chen C.F. Comparative study on the vasorelaxant effects of three harmala alkaloids in vitro. Jpn. J. Pharmacol. 2001;85:299–305. doi: 10.1254/jjp.85.299. [DOI] [PubMed] [Google Scholar]
- 55.Lee T.H., Wang G.J., Lee C.K., Kuo Y.H., Chou C.H. Inhibitory effects of glycosides from the leaves of Melaleuca quinquenervia on vascular contraction of rats. Planta Med. 2002;68:492–496. doi: 10.1055/s-2002-32563. [DOI] [PubMed] [Google Scholar]
- 56.Morita H., Zaima K., Koga I., Saito A., Tamamoto H., Okazaki H., Kaneda T., Hashimoto T., Asakawa Y. Vasorelaxant effects of macrocyclic bis(bibenzyls) from liverworts. Bioorg. Med. Chem. 2011;19:4051–4056. doi: 10.1016/j.bmc.2011.05.019. [DOI] [PubMed] [Google Scholar]
- 57.Triggle C.R., Samson M.S., Shalini R., Isra M., Gnanapragasam A., Hong D. The endothelium: influencing vascular smooth muscle in many ways. Can. J. Physiol. Pharmacol. 2012;90:713–738. doi: 10.1139/y2012-073. [DOI] [PubMed] [Google Scholar]
- 58.Palmer R.M., Ferrige A.G., Moncada S. Nitric oxide release accounts for the biological activity of endothelium-derived relaxing factor. Nature. 1987;327:524–526. doi: 10.1038/327524a0. [DOI] [PubMed] [Google Scholar]
- 59.Giles T.D., Sander G.E., Nossaman B.D., Kadowitz P.J. Impaired vasodilation in the pathogenesis of hypertension: Focus on nitric oxide, endohelial-derived hyperpolarizing factors, and prostaglandins. J. Clin. Hypertens. (Greenwich) 2012;14:198–204. doi: 10.1111/j.1751-7176.2012.00606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Gryglewski R.J., Bunting S., Moncada S., Flower R.J., Vane J.R. Arterial walls are protected against deposition of platelet thrombi by a substance (prostaglandin X) which they make from prostaglandin endoperoxides. Prostaglandins. 1976;12:685–713. doi: 10.1016/0090-6980(76)90047-2. [DOI] [PubMed] [Google Scholar]
- 61.Edwards G., Félétou M., Weston A.H. Endothelium-derived hyperpolarising factors and associated pathways: A synopsis. Pflugers Arch. 2010;459:863–879. doi: 10.1007/s00424-010-0817-1. [DOI] [PubMed] [Google Scholar]
- 62.Dias K.L.G., Correia N.A., Pereira K.K.G., Barbosa-Filho J.M., Cavalcante K.V.M., Araújo I.G.A., Silva D.F., Guedes D.N., Neto M.A., Bendhack L.M., et al. Mechanisms involved in the vasodilator effect induced by diosgenin in rat superior mesenteric artery. Eur. J. Pharmacol. 2007;574:172–178. doi: 10.1016/j.ejphar.2007.07.017. [DOI] [PubMed] [Google Scholar]
- 63.Dias K.L., da Silva Dias C., Barbosa-Filho J.M., Almeida R.N., de Azevedo Correia N., Medeiros I.A. Cardiovascular effects induced by reticuline in normotensive rats. Planta Med. 2004;70:328–333. doi: 10.1055/s-2004-818944. [DOI] [PubMed] [Google Scholar]
- 64.Aguirre-Crespo F., Vergara-Galicia J., Villalobos-Molina R., López-Guerrero J., Navarrete-Vázquez G., Estrada-Soto S. Ursolic acid mediates the vasorelaxant activity of Lepechinia caulescens via NO release in isolated rat thoracic aorta. Life Sci. 2006;79:1062–1068. doi: 10.1016/j.lfs.2006.03.006. [DOI] [PubMed] [Google Scholar]
- 65.Ku D.D., Abdel-Razek T.T., Dai J., Kim-Park S., Fallon M.B., Abrams G.A. Garlic and its active metabolite allicin produce endothelium- and nitric oxide-dependent relaxation in rat pulmonary arteries. Clin. Exp. Pharmacol. Physiol. 2002;29:84–91. doi: 10.1046/j.1440-1681.2002.03596.x. [DOI] [PubMed] [Google Scholar]
- 66.Earley S., Gonzales A.L., Crnich R. Endothelium-dependent cerebral artery dilation mediated by TRPA1 and Ca2+-Activated K+ channels. Circ. Res. 2009;104:987–994. doi: 10.1161/CIRCRESAHA.108.189530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Magalhães P.J., Lahlou S., Jucá D.M., Coelho-de-Souza L.N., da Frota P.T., da Costa A.M., Leal-Cardoso J.H. Vasorelaxation induced by the essential oil of Croton nepetaefolius and its constituents in rat aorta are partially mediated by the endothelium. Fundam. Clin. Pharmacol. 2008;22:169–177. doi: 10.1111/j.1472-8206.2008.00571.x. [DOI] [PubMed] [Google Scholar]
- 68.Wang W., Jiang D., Zhu Y., Liu W., Duan J., Dai S. Relaxing effects of phytoestrogen alpha-zearalanol on rat thoracic aorta rings in vitro. Chin. J. Physiol. 2009;52:99–105. doi: 10.4077/CJP.2009.AMH006. [DOI] [PubMed] [Google Scholar]
- 69.Wang Z.T., Lau C.W., Chan F.L., Yao X., Chen Z.Y., He Z.D. Vasorelaxant effects of cardamonin and alpinetin from Alpinia henryi K. Schum. J. Cardiovasc. Pharmacol. 2001;37:596–606. doi: 10.1097/00005344-200105000-00011. [DOI] [PubMed] [Google Scholar]
- 70.Zaima K., Koga I., Iwasawa N., Hosoya T., Hirasawa Y., Kaneda T., Ismail I.S., Lajis N.H., Morita H. Vasorelaxant activity of indole alkaloids from Tabernaemontana dichotoma. J. Nat. Med. 2013;67:9–16. doi: 10.1007/s11418-012-0638-y. [DOI] [PubMed] [Google Scholar]
- 71.Kang D.G., Yin M.H., Oh H., Lee D.H., Lee H.S. Vasorelaxation by amentoflavone isolated from Selaginella tamariscina. Planta Med. 2004;70:718–722. doi: 10.1055/s-2004-827201. [DOI] [PubMed] [Google Scholar]
- 72.Sheykhzade M., Smajilovic S., Issa A., Haunso S., Christensen S.B., Tfelt-Hansen J. S-262 and butterbur lactones dilate vessels through blockage of voltage gated calcium channels and block DNA synthesis. Eur. J. Pharmacol. 2008;593:79–86. doi: 10.1016/j.ejphar.2008.07.004. [DOI] [PubMed] [Google Scholar]
- 73.Zhang Y.H., Park Y.S., Kim T.J., Fang L.H., Ahn H.Y., Hong J.T., Kim Y., Lee C.K., Yun Y.P. Endothelium-dependent vasorelaxant and antiproliferative effects of apigenin. Gen. Pharmacol. 2000;35:341–347. doi: 10.1016/S0306-3623(02)00113-1. [DOI] [PubMed] [Google Scholar]
- 74.Ko F.N., Huang T.F., Teng C.M. Vasodilatory action mechanisms of apigenin isolated from Apium graveolens in rat thoracic aorta. Biochim. Biophys. Acta. 1991;1115:69–74. doi: 10.1016/0304-4165(91)90013-7. [DOI] [PubMed] [Google Scholar]
- 75.Ma X., He D., Ru X., Chen Y., Cai Y., Bruce I.C., Xia Q., Yao X. Apigenin, a plant-derived flavone, activates transient receptor potential vanilloid 4 cation channel. Br. J. Pharmacol. 2012;166:349–358. doi: 10.1111/j.1476-5381.2011.01767.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Senejoux F., Girard-Thernier C., Berthelot A., Bévalot F., Demougeot C. New insights into the mechanisms of the vasorelaxant effects of apocynin in rat thoracic aorta. Fundam. Clin. Pharmacol. 2012 doi: 10.1111/j.1472-8206.2011.01025.x. [DOI] [PubMed] [Google Scholar]
- 77.Zhang C., Wang X.H., Zhong M.F., Liu R.H., Li H.L., Zhang W.D., Chen H. Mechanisms underlying vasorelaxant action of astragaloside IV in isolated rat aortic rings. Clin. Exp. Pharmacol. Physiol. 2007;34:387–392. doi: 10.1111/j.1440-1681.2007.04564.x. [DOI] [PubMed] [Google Scholar]
- 78.Zaima K., Takeyama Y., Koga I., Saito A., Tamamoto H., Azziz S.S., Mukhtar M.R., Awang K., Hadi A.H., Morita H. Vasorelaxant effect of isoquinoline derivatives from two species of Popowia perakensis and Phaeanthus crassipetalus on rat aortic artery. J. Nat. Med. 2012;66:421–427. doi: 10.1007/s11418-011-0600-4. [DOI] [PubMed] [Google Scholar]
- 79.Lin Y.L., Dai Z.K., Lin R.J., Chu K.S., Chen I.J., Wu J.R., Wu B.N. Baicalin, a flavonoid from Scutellaria baicalensis Georgi, activates large-conductance Ca2+-activated K+ channels via cyclic nucleotide-dependent protein kinases in mesenteric artery. Phytomedicine. 2010;17:760–770. doi: 10.1016/j.phymed.2010.01.003. [DOI] [PubMed] [Google Scholar]
- 80.Ko W.H., Yao X.Q., Lau C.W., Law W.I., Chen Z.Y., Kwok W., Ho K., Huang Y. Vasorelaxant and antiproliferative effects of berberine. Eur. J. Pharmacol. 2000;399:187–196. doi: 10.1016/S0014-2999(00)00339-3. [DOI] [PubMed] [Google Scholar]
- 81.Fu J.Y., Qian L.B., Zhu L.G., Liang H.T., Tan Y.N., Lu H.T., Lu J.F., Wang H.P., Xia Q. Betulinic acid ameliorates endothelium-dependent relaxation in L-NAME-induced hypertensive rats by reducing oxidative stress. Eur. J. Pharm. Sci. 2011;44:385–391. doi: 10.1016/j.ejps.2011.08.025. [DOI] [PubMed] [Google Scholar]
- 82.Nishida S., Satoh H. Mechanisms for the vasodilations induced by Ginkgo biloba extract and its main constituent, bilobalide, in rat aorta. Life Sci. 2003;72:2659–2667. doi: 10.1016/S0024-3205(03)00177-2. [DOI] [PubMed] [Google Scholar]
- 83.Wang H.P., Mei R.H., Li X.Y., Zhao M.H., Lu Y., Xia Q., Bruce I. Endothelium-independent vasorelaxant effect of the phyto-oestrogen biochanin a on rat thoracic aorta. Conf. Proc. IEEE Eng. Med. Biol. Soc. 2005;3:2244–2247. doi: 10.1109/IEMBS.2005.1616910. [DOI] [PubMed] [Google Scholar]
- 84.Hu C.M., Kang J.J., Lee C.C., Li C.H., Liao J.W., Cheng Y.W. Induction of vasorelaxation through activation of nitric oxide synthase in endothelial cells by brazilin. Eur. J. Pharmacol. 2003;468:37–45. doi: 10.1016/S0014-2999(03)01639-X. [DOI] [PubMed] [Google Scholar]
- 85.Sasaki Y., Suzuki M., Matsumoto T., Hosokawa T., Kobayashi T., Kamata K., Nagumo S. Vasorelaxant activity of Sappan lignum constituents and extracts on rat aorta and mesenteric artery. Biol. Pharm. Bull. 2010;33:1555–1560. doi: 10.1248/bpb.33.1555. [DOI] [PubMed] [Google Scholar]
- 86.Silva-Filho J.C., Oliveira N.N., Arcanjo D.D., Quintans-Júnior L.J., Cavalcanti S.C., Santos M.R., Oliveira R.D., Oliveira A.P. Investigation of mechanisms involved in (−)-Borneol-induced vasorelaxant response on rat thoracic aorta. Basic Clin. Pharmacol. Toxicol. 2011;110:171–177. doi: 10.1111/j.1742-7843.2011.00784.x. [DOI] [PubMed] [Google Scholar]
- 87.Yu S.M., Cheng Z.J., Kuo S.C. Endothelium-dependent relaxation of rat aorta by butein, a novel cyclic AMP-specific phosphodiesterase inhibitor. Eur. J. Pharmacol. 1995;280:69–77. doi: 10.1016/0014-2999(95)00190-V. [DOI] [PubMed] [Google Scholar]
- 88.Chan S.S., Choi A.O., Jones R.L., Lin G. Mechanisms underlying the vasorelaxing effects of butylidenephthalide, an active constituent of Ligusticum chuanxiong, in rat isolated aorta. Eur. J. Pharmacol. 2006;537:111–117. doi: 10.1016/j.ejphar.2006.03.015. [DOI] [PubMed] [Google Scholar]
- 89.Ishizuka M., Koga I., Zaima K., Kaneda T., Hirasawa Y., Hadi A.H., Morita H. Vasorelaxant effects on rat aortic artery by two types of indole alkaloids, naucline and cadamine. J. Nat. Med. 2013;67:399–403. doi: 10.1007/s11418-012-0689-0. [DOI] [PubMed] [Google Scholar]
- 90.Leeya Y., Mulvany M.J., Queiroz E.F., Marston A., Hostettmann K., Jansakul C. Hypotensive activity of an n-butanol extract and their purified compounds from leaves of Phyllanthus acidus (L.) Skeels in rats. Eur. J. Pharmacol. 2010;649:301–313. doi: 10.1016/j.ejphar.2010.09.038. [DOI] [PubMed] [Google Scholar]
- 91.Cicala C., Morello S., Iorio C., Capasso R., Borrelli F., Mascolo N. Vascular effects of caffeic acid phenethyl ester (CAPE) on isolated rat thoracic aorta. Life Sci. 2003;73:73–80. doi: 10.1016/S0024-3205(03)00235-2. [DOI] [PubMed] [Google Scholar]
- 92.Long Y., Han M., Chen J., Tian X.Z., Chen Q., Wang R. The vasorelaxant effect of caffeic acid phenethyl ester on porcine coronary artery ring segments. Vascul. Pharmacol. 2009;51:78–83. doi: 10.1016/j.vph.2009.03.002. [DOI] [PubMed] [Google Scholar]
- 93.Wu X.L., Wang Y.Y., Cheng J., Zhao Y.Y. Calcium channel blocking activity of calycosin, a major active component of Astragali Radix, on rat aorta. Acta Pharmacol. Sin. 2006;27:1007–1012. doi: 10.1111/j.1745-7254.2006.00349.x. [DOI] [PubMed] [Google Scholar]
- 94.Potenza M.A., De Salvatore G., Montagnani M., Serio M., Mitolo-Chieppa D. Vasodilatation induced by capsaicin in rat mesenteric vessels is probably independent of nitric oxide synthesis. Pharmacol. Res. 1994;30:253–261. doi: 10.1016/1043-6618(94)80107-X. [DOI] [PubMed] [Google Scholar]
- 95.Fusi F., Cavalli M., Mulholland D., Crouch N., Coombes P., Dawson G., Bova S., Sgaragli G., Saponara S. Cardamonin is a bifunctional vasodilator that inhibits Ca(v)1.2 current and stimulates K(Ca)1.1 current in rat tail artery myocytes. J. Pharmacol. Exp. Ther. 2010;332:531–540. doi: 10.1124/jpet.109.161265. [DOI] [PubMed] [Google Scholar]
- 96.Peixoto-Neves D., Silva-Alves K.S., Gomes M.D., Lima F.C., Lahlou S., Magalhães P.J., Ceccatto V.M., Coelho-de-Souza A.N., Leal-Cardoso J.H. Vasorelaxant effects of the monoterpenic phenol isomers, carvacrol and thymol, on rat isolated aorta. Fundam. Clin. Pharmacol. 2010;24:341–350. doi: 10.1111/j.1472-8206.2009.00768.x. [DOI] [PubMed] [Google Scholar]
- 97.Earley S., Gonzales A.L., Garcia Z.I. A dietary agonist of transient receptor potential cation channel V3 elicits endothelium-dependent vasodilation. Mol. Pharmacol. 2010;77:612–620. doi: 10.1124/mol.109.060715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Matsumoto T., Kobayashi T., Ishida K., Hirasawa Y., Morita H., Honda T., Kamata K. Vasodilator effect of Cassiarin A, a novel antiplasmodial alkaloid from Cassia siamea, in rat isolated mesenteric artery. Biol. Pharm. Bull. 2010;33:844–848. doi: 10.1248/bpb.33.844. [DOI] [PubMed] [Google Scholar]
- 99.Orallo F., Lamela M., Camiña M., Uriarte E., Calleja J.M. Preliminary study of the potential vasodilator effects on rat aorta of centaurein and centaureidin, two flavonoids from Centaurea corcubionensis. Planta Med. 1998;64:116–119. doi: 10.1055/s-2006-957386. [DOI] [PubMed] [Google Scholar]
- 100.Villar I.C., Vera R., Galisteo M., O’Valle F., Romero M., Zarzuelo A., Duarte J. Endothelial nitric oxide production stimulated by the bioflavonoid chrysin in rat isolated aorta. Planta Med. 2005;71:829–834. doi: 10.1055/s-2005-871296. [DOI] [PubMed] [Google Scholar]
- 101.Duarte J., Jiménez R., Villar I.C., Pérez-Vizcaíno F., Jiménez J., Tamargo J. Vasorelaxant effects of the bioflavonoid chrysin in isolated rat aorta. Planta Med. 2001;67:567–569. doi: 10.1055/s-2001-16492. [DOI] [PubMed] [Google Scholar]
- 102.Devi R.C., Sim S.M., Ismail R. Effect of Cymbopogon citratus and citral on vascular smooth muscle of the isolated thoracic rat aorta. Evid. Based Complement. Alternat Med. 2012;2012:539475:1–539475:8. doi: 10.1155/2012/539475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Yanaga A., Goto H., Nakagawa T., Hikiami H., Shibahara N., Shimada Y. Cinnamaldehyde induces endothelium-dependent and -independent vasorelaxant action on isolated rat aorta. Biol. Pharm. Bull. 2006;29:2415–2418. doi: 10.1248/bpb.29.2415. [DOI] [PubMed] [Google Scholar]
- 104.Othman R., Ibrahim H., Mohd M.A., Awang K., Gilani A.U., Mustafa M.R. Vasorelaxant effects of ethyl cinnamate isolated from Kaempferia galanga on smooth muscles of the rat aorta. Planta Med. 2002;68:655–657. doi: 10.1055/s-2002-32900. [DOI] [PubMed] [Google Scholar]
- 105.Pinto N.V., Assreuy A.M., Coelho-de-Souza A.N., Ceccatto V.M., Magalhães P.J., Lahlou S., Leal-Cardoso J.H. Endothelium-dependent vasorelaxant effects of the essential oil from aerial parts of Alpinia zerumbet and its main constituent 1,8-cineole in rats. Phytomedicine. 2009;16:1151–1155. doi: 10.1016/j.phymed.2009.04.007. [DOI] [PubMed] [Google Scholar]
- 106.Lee J.W., Roh T.C., Rho M.C., Kim Y.K., Lee H.S. Mechanisms of relaxant action of a pyranocoumarin from Peucedanum japonicum in isolated rat thoracic aorta. Planta Med. 2002;68:891–895. doi: 10.1055/s-2002-34934. [DOI] [PubMed] [Google Scholar]
- 107.Bastos J.F., Moreira I.J., Ribeiro T.P., Medeiros I.A., Antoniolli A.R., De Sousa D.P., Santos M.R. Hypotensive and vasorelaxant effects of citronellol, a monoterpene alcohol, in rats. Basic Clin. Pharmacol. Toxicol. 2010;106:331–337. doi: 10.1111/j.1742-7843.2009.00492.x. [DOI] [PubMed] [Google Scholar]
- 108.Gong L.L., Fang L.H., Qin H.L., Lv Y., Du G.H. Analysis of the mechanisms underlying the vasorelaxant action of coptisine in rat aortic rings. Am. J. Chin. Med. 2012;40:309–320. doi: 10.1142/S0192415X12500243. [DOI] [PubMed] [Google Scholar]
- 109.Kang D.G., Choi D.H., Lee J.K., Lee Y.J., Moon M.K., Yang S.N., Kwon T.O., Kwon J.W., Kim J.S., Lee H.S. Endothelial NO/cGMP-dependent vascular relaxation of cornuside isolated from the fruit of Cornus officinalis. Planta Med. 2007;73:1436–1440. doi: 10.1055/s-2007-990243. [DOI] [PubMed] [Google Scholar]
- 110.Lam F.F., Yeung J.H., Chan K.M., Or P.M. Mechanisms of the dilator action of cryptotanshinone on rat coronary artery. Eur. J. Pharmacol. 2008;578:253–260. doi: 10.1016/j.ejphar.2007.09.040. [DOI] [PubMed] [Google Scholar]
- 111.Dias C.S., Barbosa-Filho J.M., Lemos V.S., Côrtes S.F. Mechanisms involved in the vasodilator effect of curine in rat resistance arteries. Planta Med. 2002;68:1049–1051. doi: 10.1055/s-2002-35662. [DOI] [PubMed] [Google Scholar]
- 112.Medeiros M.A., Pinho J.F., De-Lira D.P., Barbosa-Filho J.M., Araújo D.A., Cortes S.F., Lemos V.S., Cruz J.S. Curine, a bisbenzylisoquinoline alkaloid, blocks L-type Ca2+ channels and decreases intracellular Ca2+ transients in A7r5 cells. Eur. J. Pharmacol. 2011;669:100–107. doi: 10.1016/j.ejphar.2011.07.044. [DOI] [PubMed] [Google Scholar]
- 113.Xu P.H., Long Y., Dai F., Liu Z.L. The relaxant effect of curcumin on porcine coronary arterial ring segments. Vascul. Pharmacol. 2007;47:25–30. doi: 10.1016/j.vph.2007.03.003. [DOI] [PubMed] [Google Scholar]
- 114.Morita H., Iizuka T., Choo C.Y., Chan K.L., Takeya K., Kobayashi J. Vasorelaxant activity of cyclic peptide, cyclosquamosin B, from Annona squamos. Bioorg. Med. Chem. Lett. 2006;16:4609–4611. doi: 10.1016/j.bmcl.2006.06.008. [DOI] [PubMed] [Google Scholar]
- 115.Deng Y., Ng E.S., Yeung J.H., Kwan Y.W., Lau C.B., Koon J.C., Zhou L., Zuo Z., Leung P.C., Fung K.P., et al. Mechanisms of the cerebral vasodilator actions of isoflavonoids of Gegen on rat isolated basilar artery. J. Ethnopharmacol. 2012;139:294–304. doi: 10.1016/j.jep.2011.11.021. [DOI] [PubMed] [Google Scholar]
- 116.Zhang H.T., Wang Y., Deng X.L., Dong M.Q., Zhao L.M., Wang Y.W. Daidzein relaxes rat cerebral basilar artery via activation of large-conductance Ca2+-activated K+ channels in vascular smooth muscle cells. Eur. J. Pharmacol. 2010;630:100–106. doi: 10.1016/j.ejphar.2009.12.032. [DOI] [PubMed] [Google Scholar]
- 117.Lam F.F., Yeung J.H., Chan K.M., Or P.M. Relaxant effects of danshen aqueous extract and its constituent danshensu on rat coronary artery are mediated by inhibition of calcium channels. Vascul. Pharmacol. 2007;46:271–277. doi: 10.1016/j.vph.2006.10.011. [DOI] [PubMed] [Google Scholar]
- 118.Chiou W.F., Liao J.F., Shum A.Y., Chen C.F. Mechanisms of vasorelaxant effect of dehydroevodiamine: A bioactive isoquinazolinocarboline alkaloid of plant origin. J. Cardiovasc. Pharmacol. 1996;27:845–853. doi: 10.1097/00005344-199606000-00012. [DOI] [PubMed] [Google Scholar]
- 119.Nakano D., Kwak C.J., Fujii K., Ikemura K., Satake A., Ohkita M., Takaoka M., Ono Y., Nakai M., Tomimori N., et al. Sesamin metabolites induce an endothelial nitric oxide-dependent vasorelaxation through their antioxidative property-independent mechanisms: Possible involvement of the metabolites in the antihypertensive effect of sesamin. J. Pharmacol. Exp. Ther. 2006;318:328–335. doi: 10.1124/jpet.105.100149. [DOI] [PubMed] [Google Scholar]
- 120.Yu S.M., Chen C.C., Huang Y.L., Tsai C.W., Lin C.H., Huang T.F., Teng C.M. Vasorelaxing effect in rat thoracic aorta caused by denudatin B, isolated from the Chinese herb, magnolia fargesii. Eur. J. Pharmacol. 1990;187:39–47. doi: 10.1016/0014-2999(90)90338-7. [DOI] [PubMed] [Google Scholar]
- 121.Zhang C.Y., Tan B.K. Vasorelaxation of rat thoracic aorta caused by 14-deoxyandrographolide. Clin. Exp. Pharmacol. Physiol. 1998;25:424–429. doi: 10.1111/j.1440-1681.1998.tb02226.x. [DOI] [PubMed] [Google Scholar]
- 122.Yu S.M., Ko F.N., Su M.J., Wu T.S., Wang M.L., Huang T.F., Teng C.M. Vasorelaxing effect in rat thoracic aorta caused by fraxinellone and dictamine isolated from the Chinese herb Dictamnus dasycarpus Turcz: comparison with cromakalim and Ca2+ channel blockers. Naunyn Schmiedebergs Arch. Pharmacol. 1992;345:349–355. doi: 10.1007/BF00168697. [DOI] [PubMed] [Google Scholar]
- 123.Wang S.P., Zang W.J., Kong S.S., Yu X.J., Sun L., Zhao X.F., Wang S.X., Zheng X.H. Vasorelaxant effect of isopropyl 3-(3,4-dihydroxyphenyl)-2-hydroxypropanoate, a novel metabolite from Salvia miltiorrhiza, on isolated rat mesenteric artery. Eur. J. Pharmacol. 2008;579:283–288. doi: 10.1016/j.ejphar.2007.10.009. [DOI] [PubMed] [Google Scholar]
- 124.Estrada-Soto S., López-Guerrero J.J., Villalobos-Molina R., Mata R. Endothelium-independent relaxation of aorta rings by two stilbenoids from the orchids Scaphyglottis livida. Fitoterapia. 2006;77:236–239. doi: 10.1016/j.fitote.2006.02.006. [DOI] [PubMed] [Google Scholar]
- 125.He W.J., Fang T.H., Ma X., Zhang K., Ma Z.Z., Tu P.F. Echinacoside elicits endothelium-dependent relaxation in rat aortic rings via an NO-cGMP pathway. Planta Med. 2009;75:1400–1404. doi: 10.1055/s-0029-1185745. [DOI] [PubMed] [Google Scholar]
- 126.Yılmaz B., Usta C. Ellagic acid-induced endothelium-dependent and endothelium-independent vasorelaxation in rat thoracic aortic rings and the underlying mechanism. Phytother. Res. 2012 doi: 10.1002/ptr.4716. [DOI] [PubMed] [Google Scholar]
- 127.Huang H.C., Lee C.R., Chao P.D., Chen C.C., Chu S.H. Vasorelaxant effect of emodin, an anthraquinone from a Chinese herb. Eur. J. Pharmacol. 1991;205:289–294. doi: 10.1016/0014-2999(91)90912-A. [DOI] [PubMed] [Google Scholar]
- 128.Martinsen A., Baccelli C., Navarro I., Abad A., Quetin-Leclercq J., Morel N. Vascular activity of a natural diterpene isolated from Croton zambesicus and of a structurally similar synthetic trachylobane. Vascul. Pharmacol. 2010;52:63–69. doi: 10.1016/j.vph.2009.11.002. [DOI] [PubMed] [Google Scholar]
- 129.Hipólito U.V., Rodrigues G.J., Lunardi C.N., Bonaventura D., Ambrosio S.R., de Oliveira A.M., Bendhack L.M., da Costa F.B., Tirapelli C.R. Mechanisms underlying the vasorelaxant action of the pimarane ent-8(14),15-pimaradien-3beta-ol in the isolated rat aorta. Eur. J. Pharmacol. 2009;616:183–191. doi: 10.1016/j.ejphar.2009.06.010. [DOI] [PubMed] [Google Scholar]
- 130.Aggio A., Grassi D., Onori E., D'Alessandro A., Masedu F., Valenti M., Ferri C. Endothelium/nitric oxide mechanism mediates vasorelaxation and counteracts vasoconstriction induced by low concentration of flavanols. Eur. J. Nutr. 2013;52:263–272. doi: 10.1007/s00394-012-0320-x. [DOI] [PubMed] [Google Scholar]
- 131.Cruz A.J., Lemos V.S., dos Santos M.H., Nagem T.J., Cortes S.F. Vascular effects of 7-epiclusianone, a prenylated benzophenone from Rheedia gardneriana, on the rat aorta. Phytomedicine. 2006;13:442–445. doi: 10.1016/j.phymed.2005.01.014. [DOI] [PubMed] [Google Scholar]
- 132.Joy S., Siow R.C., Rowlands D.J., Becker M., Wyatt A.W., Aaronson P.I., Coen C.W., Kallo I., Jacob R., Mann G.E. The isoflavone Equol mediates rapid vascular relaxation: Ca2+-independent activation of endothelial nitric-oxide synthase/Hsp90 involving ERK1/2 and Akt phosphorylation in human endothelial cells. J. Biol. Chem. 2006;281:27335–27345. doi: 10.1074/jbc.M602803200. [DOI] [PubMed] [Google Scholar]
- 133.Sánchez de Rojas R., Somoza B., Ortega T., Villar A.M., Tejerina T. Vasodilatory effect in rat aorta of eriodictyol obtained from Satureja obovata. Planta Med. 1999;65:234–238. doi: 10.1055/s-1999-13986. [DOI] [PubMed] [Google Scholar]
- 134.Rodríguez-Rodríguez R., Herrera M.D., Perona J.S., Ruiz-Gutiérrez V. Potential vasorelaxant effects of oleanolic acid and erythrodiol, two triterpenoids contained in ‘orujo’ olive oil, on rat aorta. Br. J. Nutr. 2004;92:635–642. doi: 10.1079/BJN20041231. [DOI] [PubMed] [Google Scholar]
- 135.Raimundo J.M., Trindade A.P., Velozo L.S., Kaplan M.A., Sudo R.T., Zapata-Sudo G. The lignan eudesmin extracted from Piper truncatum induced vascular relaxation via activation of endothelial histamine H1 receptors. Eur. J. Pharmacol. 2009;606:150–154. doi: 10.1016/j.ejphar.2009.01.038. [DOI] [PubMed] [Google Scholar]
- 136.Interaminense L.F., Jucá D.M., Magalhães P.J., Leal-Cardoso J.H., Duarte G.P., Lahlou S. Pharmacological evidence of calcium-channel blockade by essential oil of Ocimum gratissimum and its main constituent, eugenol, in isolated aortic rings from DOCA-salt hypertensive rats. Fundam. Clin. Pharmacol. 2007;21:497–506. doi: 10.1111/j.1472-8206.2007.00514.x. [DOI] [PubMed] [Google Scholar]
- 137.Damiani C.E., Rossoni L.V., Vassallo D.V. Vasorelaxant effects of eugenol on rat thoracic aorta. Vascul. Pharmacol. 2003;40:59–66. doi: 10.1016/S1537-1891(02)00311-7. [DOI] [PubMed] [Google Scholar]
- 138.Criddle D.N., Madeira S.V., Soares de Moura R. Endothelium-dependent and -independent vasodilator effects of eugenol in the rat mesenteric vascular bed. J. Pharm. Pharmacol. 2003;55:359–365. doi: 10.1211/002235702694. [DOI] [PubMed] [Google Scholar]
- 139.Fang L.H., Mu Y.M., Lin L.L., Xiao P.G., Du G.H. Vasorelaxant effect of euxanthone in the rat thoracic aorta. Vascul. Pharmacol. 2006;45:96–101. doi: 10.1016/j.vph.2006.03.011. [DOI] [PubMed] [Google Scholar]
- 140.Yamahara J., Kobayashi G., Matsuda H., Fujimura H. The vasorelaxant effect of evocarpine in isolated aortic strips: Mode of action. Eur. J. Pharmacol. 1988;155:139–143. doi: 10.1016/0014-2999(88)90411-6. [DOI] [PubMed] [Google Scholar]
- 141.Chiou W.F., Chou C.J., Shum A.Y., Chen C.F. The vasorelaxant effect of evodiamine in rat isolated mesenteric arteries: Mode of action. Eur. J. Pharmacol. 1992;215:277–283. doi: 10.1016/0014-2999(92)90039-7. [DOI] [PubMed] [Google Scholar]
- 142.Rhyu M.R., Kim J.H., Kim E.Y. Radix angelica elicits both nitric oxide-dependent and calcium influx-mediated relaxation in rat aorta. J. Cardiovasc. Pharmacol. 2005;46:99–104. doi: 10.1097/01.fjc.0000164092.88821.49. [DOI] [PubMed] [Google Scholar]
- 143.Rezende B.A., Cortes S.F., Lemos V.S. Mechanisms involved in the vasodilator effect of the flavanol floranol in rat small mesenteric arteries. Planta Med. 2004;70:465–467. doi: 10.1055/s-2004-818977. [DOI] [PubMed] [Google Scholar]
- 144.Lemos V.S., Côrtes S.F., dos Santos M.H., Ellena J., Moreira M.E., Doriguetto A.C. Structure and vasorelaxant activity of floranol, a flavonoid isolated from the roots of Dioclea grandiflora. Chem. Biodivers. 2006;3:635–645. doi: 10.1002/cbdv.200690066. [DOI] [PubMed] [Google Scholar]
- 145.Zhao Y., Chen B.N., Wang S.B., Wang S.H., Du G.H. Vasorelaxant effect of formononetin in the rat thoracic aorta and its mechanisms. J. Asian. Nat. Prod. Res. 2012;14:46–54. doi: 10.1080/10286020.2011.628939. [DOI] [PubMed] [Google Scholar]
- 146.Iizuka T., Sakai H., Moriyama H., Suto N., Nagai M., Bagchi D. Vasorelaxant effects of forsythide isolated from the leaves of Forsythia viridissima on NE-induced aortal contraction. Phytomedicine. 2009;16:386–390. doi: 10.1016/j.phymed.2008.09.011. [DOI] [PubMed] [Google Scholar]
- 147.Morello S., Vellecco V., Alfieri A., Mascolo N., Cicala C. Vasorelaxant effect of the flavonoid galangin on isolated rat thoracic aorta. Life Sci. 2006;78:825–830. doi: 10.1016/j.lfs.2005.05.072. [DOI] [PubMed] [Google Scholar]
- 148.Yuzurihara M., Ikarashi Y., Goto K., Sakakibara I., Hayakawa T., Sasaki H. Geissoschizine methyl ether, an indole alkaloid extracted from Uncariae Ramulus et Uncus, is a potent vasorelaxant of isolated rat aorta. Eur. J. Pharmacol. 2002;444:183–189. doi: 10.1016/S0014-2999(02)01623-0. [DOI] [PubMed] [Google Scholar]
- 149.Figtree G.A., Griffiths H., Lu Y.Q., Webb C.M., MacLeod K., Collins P. Plant-derived estrogens relax coronary arteries in vitro by a calcium antagonistic mechanism. J. Am. Coll. Cardiol. 2000;35:1977–1985. doi: 10.1016/S0735-1097(00)00645-8. [DOI] [PubMed] [Google Scholar]
- 150.Speroni F., Rebolledo A., Salemme S., Roldán-Palomo R., Rimorini L., Añón M.C., Spinillo A., Tanzi F., Milesi V. Genistein effects on Ca2+ handling in human umbilical artery: Inhibition of sarcoplasmic reticulum Ca2+ release and of voltage-operated Ca2+ channels. J. Physiol. Biochem. 2009;65:113–124. doi: 10.1007/BF03179062. [DOI] [PubMed] [Google Scholar]
- 151.Kim N.D., Kang S.Y., Park J.H., Schini-Kerth V.B. Ginsenoside Rg3 mediates endothelium-dependent relaxation in response to ginsenosides in rat aorta: role of K+ channels. Eur. J. Pharmacol. 1999;367:41–49. doi: 10.1016/S0014-2999(98)00898-X. [DOI] [PubMed] [Google Scholar]
- 152.Park J.Y., Lee S.J., Yun M.R., Seo K.W., Bae S.S., Park J.W., Lee Y.J., Shin W.J., Choi Y.W., Kim C.D. Gomisin A from Schisandra chinensis induces endothelium-dependent and direct relaxation in rat thoracic aorta. Planta Med. 2007;73:1537–1542. doi: 10.1055/s-2007-993757. [DOI] [PubMed] [Google Scholar]
- 153.Rendón-Vallejo P., Hernández-Abreu O., Vergara-Galicia J., Millán-Pacheco C., Mejía A., Ibarra-Barajas M., Estrada-Soto S. Ex vivo study of the vasorelaxant activity induced by phenanthrene derivatives isolated from Maxillaria densa. J. Nat. Prod. 2012;75:2241–2245. doi: 10.1021/np300508v. [DOI] [PubMed] [Google Scholar]
- 154.Berrougui H., Martín-Cordero C., Khalil A., Hmamouchi M., Ettaib A., Marhuenda E., Herrera M.D. Vasorelaxant effects of harmine and harmaline extracted from Peganum harmala L. seeds in isolated rat aorta. Pharmacol. Res. 2006;54:150–157. doi: 10.1016/j.phrs.2006.04.001. [DOI] [PubMed] [Google Scholar]
- 155.Shi C.C., Chen S.Y., Wang G.J., Liao J.F., Chen C.F. Vasorelaxant effect of harman. Eur. J. Pharmacol. 2000;390:319–325. doi: 10.1016/s0014-2999(99)00928-0. [DOI] [PubMed] [Google Scholar]
- 156.Xie Y.W., Ming D.S., Xu H.X., Dong H., But P.P. Vasorelaxing effects of Caesalpinia sappan involvement of endogenous nitric oxide. Life Sci. 2000;67:1913–1918. doi: 10.1016/S0024-3205(00)00772-4. [DOI] [PubMed] [Google Scholar]
- 157.Orallo F., Alvarez E., Basaran H., Lugnier C. Comparative study of the vasorelaxant activity, superoxide-scavenging ability and cyclic nucleotide phosphodiesterase-inhibitory effects of hesperetin and hesperidin. Naunyn Schmiedebergs Arch. Pharmacol. 2004;370:452–463. doi: 10.1007/s00210-004-0994-6. [DOI] [PubMed] [Google Scholar]
- 158.Xu H.B., Huang Z.Q. Icariin enhances endothelial nitric-oxide synthase expression on human endothelial cells in vitro. Vascul. Pharmacol. 2007;47:18–24. doi: 10.1016/j.vph.2007.03.002. [DOI] [PubMed] [Google Scholar]
- 159.Xu H.B., Huang Z.Q. Vasorelaxant effects of icariin on isolated canine coronary artery. J. Cardiovasc. Pharmacol. 2007;49:207–213. doi: 10.1097/FJC.0b013e3180325abe. [DOI] [PubMed] [Google Scholar]
- 160.He J.Y., Zhang W., He L.C., Cao Y.X. Imperatorin induces vasodilatation possibly via inhibiting voltage dependent calcium channel and receptor-mediated Ca2+ influx and release. Eur. J. Pharmacol. 2007;573:170–175. doi: 10.1016/j.ejphar.2007.06.043. [DOI] [PubMed] [Google Scholar]
- 161.Nie H., Meng L.Z., Zhou J.Y., Fan X.F., Luo Y., Zhang G.W. Imperatorin is responsible for the vasodilatation activity of Angelica Dahurica var. Formosana regulated by nitric oxide in an endothelium-dependent manner. Chin. J. Integr. Med. 2009;15:442–447. doi: 10.1007/s11655-009-0442-z. [DOI] [PubMed] [Google Scholar]
- 162.Yu S.M., Kuo S.C. Vasorelaxant effect of isoliquiritigenin, a novel soluble guanylate cyclase activator, in rat aorta. Br. J. Pharmacol. 1995;114:1587–1594. doi: 10.1111/j.1476-5381.1995.tb14943.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Pérez-Vizcaíno F., Ibarra M., Cogolludo A.L., Duarte J., Zaragozá-Arnáez F., Moreno L., López-López G., Tamargo J. Endothelium-independent vasodilator effects of the flavonoid quercetin and its methylated metabolites in rat conductance and resistance arteries. J. Pharmacol. Exp. Ther. 2002;302:66–72. doi: 10.1124/jpet.302.1.66. [DOI] [PubMed] [Google Scholar]
- 164.Zhang W.B., Chen C.X., Sim S.M., Kwan C.Y. In vitro vasodilator mechanisms of the indole alkaloids rhynchophylline and isorhynchophylline, isolated from the hook of Uncaria rhynchophylla (Miquel) Naunyn Schmiedebergs Arch. Pharmacol. 2004;369:232–238. doi: 10.1007/s00210-003-0854-9. [DOI] [PubMed] [Google Scholar]
- 165.Wang G.J., Wu X.C., Lin Y.L., Ren J., Shum A.Y., Wu Y.Y., Chen C.F. Ca2+ channel blocking effect of iso-S-petasin in rat aortic smooth muscle cells. Eur. J. Pharmacol. 2002;445:239–245. doi: 10.1016/S0014-2999(02)01764-8. [DOI] [PubMed] [Google Scholar]
- 166.Mendes L.J., Capettini L.S., Lôbo L.T., da Silva G.A., Arruda M.S., Lemos V.S., Côrtes S.F. Endothelial nitric oxide-dependent vasorelaxant effect of isotirumalin, a dihydroflavonol from Derris urucu, on the rat aorta. Biol. Pharm. Bull. 2011;34:1499–1500. doi: 10.1248/bpb.34.1499. [DOI] [PubMed] [Google Scholar]
- 167.Duarte D.F., Sant'Ana A.E., Calixto J.B. Analysis of the vasorelaxant action of jatrophone in the isolated aorta of the rat: Influence of potassium channel blockers. Eur. J. Pharmacol. 1992;215:75–81. doi: 10.1016/0014-2999(92)90611-7. [DOI] [PubMed] [Google Scholar]
- 168.Silva A.M., Brum R.L., Calixto J.B. The relaxant action of jatrophone in rat portal vein. A comparison with protein kinase C inhibitors. Life Sci. 1995;57:863–871. doi: 10.1016/0024-3205(95)02019-F. [DOI] [PubMed] [Google Scholar]
- 169.Xu Y.C., Yeung D.K., Man R.Y., Leung S.W. Kaempferol enhances endothelium-independent and dependent relaxation in the porcine coronary artery. Mol. Cell. Biochem. 2006;287:61–67. doi: 10.1007/s11010-005-9061-y. [DOI] [PubMed] [Google Scholar]
- 170.Padilla E., Ruiz E., Redondo S., Gordillo-Moscoso A., Slowing K., Tejerina T. Relationship between vasodilation capacity and phenolic content of Spanish wines. Eur. J. Pharmacol. 2005;517:84–91. doi: 10.1016/j.ejphar.2005.04.044. [DOI] [PubMed] [Google Scholar]
- 171.Tirapelli C.R., Ambrosio S.R., da Costa F.B., Coutinho S.T., de Oliveira D.C., de Oliveira A.M. Analysis of the mechanisms underlying the vasorelaxant action of kaurenoic acid in the isolated rat aorta. Eur. J. Pharmacol. 2004;492:233–241. doi: 10.1016/j.ejphar.2004.04.003. [DOI] [PubMed] [Google Scholar]
- 172.Zamblé A., Martin-Nizard F., Sahpaz S., Reynaert M.L., Staels B., Bordet R., Duriez P., Gressier B., Bailleul F. Effects of Microdesmis keayana alkaloids on vascular parameters of erectile dysfunction. Phytother. Res. 2009;23:892–895. doi: 10.1002/ptr.2717. [DOI] [PubMed] [Google Scholar]
- 173.Adaramoye O.A., Medeiros I.A. Endothelium-independent vasodilation induced by kolaviron, a biflavonoid complex from Garcinia kola seeds, in rat superior mesenteric arteries. J. Smooth Muscle Res. 2009;45:39–53. doi: 10.1540/jsmr.45.39. [DOI] [PubMed] [Google Scholar]
- 174.De Oliveira A.P., Furtado F.F., da Silva M.S., Tavares J.F., Mafra R.A., Araújo D.A., Cruz J.S., de Medeiros I.A. Calcium channel blockade as a target for the cardiovascular effects induced by the 8 (17), 12E, 14-labdatrien-18-oic acid (labdane-302) Vascul. Pharmacol. 2006;44:338–344. doi: 10.1016/j.vph.2006.01.009. [DOI] [PubMed] [Google Scholar]
- 175.Lahlou S., de Barros Correia C.A., Vasconcelos Dos Santos M., David J.M., David J.P., Duarte G.P., Magalhães P.J. Mechanisms underlying the cardiovascular effects of a labdenic diterpene isolated from Moldenhawera nutans in normotensive rats. Vascul. Pharmacol. 2007;46:60–66. doi: 10.1016/j.vph.2006.06.010. [DOI] [PubMed] [Google Scholar]
- 176.Assreuy A.M., Pinto N.V., Lima Mota M.R., Passos Meireles A.V., Cajazeiras J.B., Nobre C.B., Soares P.M., Cavada B.S. Vascular smooth muscle relaxation by a lectin from Pisum arvense: Evidences of endothelial NOS pathway. Protein Pept. Lett. 2011;18:1107–1111. doi: 10.2174/092986611797201011. [DOI] [PubMed] [Google Scholar]
- 177.Chen C.X., Kwan C.Y. Endothelium-independent vasorelaxation by leonurine, a plant alkaloid purified from Chinese motherwort (Leonurus artemisiae) Life Sci. 2001;68:953–960. doi: 10.1016/S0024-3205(00)00987-5. [DOI] [PubMed] [Google Scholar]
- 178.Andriambeloson E., Kleschyov A.L., Muller B., Beretz A., Stoclet J.C., Andriantsitohaina R. Nitric oxide production and endothelium-dependent vasorelaxation induced by wine polyphenols in rat aorta. Br. J. Pharmacol. 1997;120:1053–1058. doi: 10.1038/sj.bjp.0701011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Cao Y.X., Zhang W., He J.Y., He L.C., Xu C.B. Ligustilide induces vasodilatation via inhibiting voltage dependent calcium channel and receptor-mediated Ca2+ influx and release. Vascul. Pharmacol. 2006;45:171–176. doi: 10.1016/j.vph.2006.05.004. [DOI] [PubMed] [Google Scholar]
- 180.Chan S.S., Cheng T.Y., Lin G. Relaxation effects of ligustilide and senkyunolide A, two main constituents of Ligusticum chuanxiong, in rat isolated aorta. J. Ethnopharmacol. 2007;111:677–680. doi: 10.1016/j.jep.2006.12.018. [DOI] [PubMed] [Google Scholar]
- 181.Jiang H., Xia Q., Wang X., Song J., Bruce I.C. Luteolin induces vasorelaxion in rat thoracic aorta via calcium and potassium channels. Pharmazie. 2005;60:444–447. [PubMed] [Google Scholar]
- 182.Oh K.S., Choi Y.H., Ryu S.Y., Oh B.K., Seo H.W., Yon G.H., Kim Y.S., Lee B.H. Cardiovascular effects of lignans isolated from Saururus chinensis. Planta Med. 2008;74:233–238. doi: 10.1055/s-2008-1034310. [DOI] [PubMed] [Google Scholar]
- 183.El-Bardai S., Wibo M., Hamaide M.C., Lyoussi B., Quetin-Leclercq J., Morel N. Characterization of marrubenol, a diterpene extracted from Marrubium vulgare, as an L-type calcium channel blocker. Br. J. Pharmacol. 2003;140:1211–1216. doi: 10.1038/sj.bjp.0705561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Khan A.U., Ullah R., Khan A., Mustafa M.R., Hussain J., Murugan D.D., Hadi A.H. Vasodilator effect of Phlomis bracteosa constituents is mediated through dual endothelium-dependent and endothelium-independent pathways. Clin. Exp. Hypertens. 2012;34:132–139. doi: 10.3109/10641963.2011.601383. [DOI] [PubMed] [Google Scholar]
- 185.Iizuka T., Moriyama H., Nagai M. Vasorelaxant effects of methyl brevifolincarboxylate from the leaves of Phyllanthus niruri. Biol. Pharm. Bull. 2006;29:177–179. doi: 10.1248/bpb.29.177. [DOI] [PubMed] [Google Scholar]
- 186.Yoo M.Y., Lee B.H., Choi Y.H., Lee J.W., Seo J.H., Oh K.S., Koo H.N., Seo H.W., Yon G.H., Kwon D.Y., et al. Vasorelaxant effect of the rootbark extract of Paeonia moutan on isolated rat thoracic aorta. Planta Med. 2006;72:1338–1341. doi: 10.1055/s-2006-951678. [DOI] [PubMed] [Google Scholar]
- 187.Cavalcante H.M., Ribeiro T.P., Silva D.F., Nunes X.P., Barbosa-Filho J.M., Diniz M.F., Correia N.A., Braga V.A., Medeiros I.A. Cardiovascular effects elicited by milonine, a new 8,14-dihydromorphinandienone alkaloid. Basic Clin. Pharmacol. Toxicol. 2011;108:122–130. doi: 10.1111/j.1742-7843.2010.00631.x. [DOI] [PubMed] [Google Scholar]
- 188.Ojewole J.A. Cardiovascular effects of mollic acid glucoside, a 1alpha-hydroxycycloartenoid saponin extractive from Combretum molleR Br ex G Don (Combretaceae) leaf. Cardiovasc. J. Afr. 2008;19:128–134. [PMC free article] [PubMed] [Google Scholar]
- 189.Rios M.Y., López-Martínez S., López-Vallejo F., Medina-Franco J.L., Villalobos-Molina R., Ibarra-Barajas M., Navarrete-Vazquez G., Hidalgo-Figueroa S., Hernández-Abreu O., Estrada-Soto S. Vasorelaxant activity of some structurally related triterpenic acids from Phoradendron reichenbachianum (Viscaceae) mainly by NO production: Ex vivo and in silico studies. Fitoterapia. 2012;83:1023–1029. doi: 10.1016/j.fitote.2012.05.014. [DOI] [PubMed] [Google Scholar]
- 190.Orallo F., Alzueta A.F. Preliminary study of the vasorelaxant effects of (+)-nantenine, an alkaloid isolated from Platycapnos spicata, in rat aorta. Planta Med. 2001;67:800–806. doi: 10.1055/s-2001-18848. [DOI] [PubMed] [Google Scholar]
- 191.Brito T.S., Lima F.J., Aragão K.S., de Siqueira R.J., Sousa P.J., Maia J.G., Filho J.D., Lahlou S., Magalhães P.J. The vasorelaxant effects of 1-nitro-2-phenylethane involve stimulation of the soluble guanylate cyclase-cGMP pathway. Biochem. Pharmacol. 2013;85:780–788. doi: 10.1016/j.bcp.2012.12.012. [DOI] [PubMed] [Google Scholar]
- 192.Ko F.N., Lin C.N., Liou S.S., Huang T.F., Teng C.M. Vasorelaxation of rat thoracic aorta caused by norathyriol isolated from Gentianaceae. Eur. J. Pharmacol. 1991;192:133–139. doi: 10.1016/0014-2999(91)90079-6. [DOI] [PubMed] [Google Scholar]
- 193.Guedes D.N., Barbosa-Filho J.M., Lemos V.S., Côrtes S.F. Mechanism of the vasodilator effect of 12-O-methylcurine in rat aortic rings. J. Pharm. Pharmacol. 2002;54:853–858. doi: 10.1211/0022357021779032. [DOI] [PubMed] [Google Scholar]
- 194.Fu X.C., Wang M.W., Li S.P., Zhang Y., Wang H.L. Vasodilatation produced by orientin and its mechanism study. Biol. Pharm. Bull. 2005;28:37–41. doi: 10.1248/bpb.28.37. [DOI] [PubMed] [Google Scholar]
- 195.Ko F.N., Wu T.S., Liou M.J., Huang T.F., Teng C.M. Vasorelaxation of rat thoracic aorta caused by osthole isolated from Angelica pubescens. Eur. J. Pharmacol. 1992;219:29–34. doi: 10.1016/0014-2999(92)90576-P. [DOI] [PubMed] [Google Scholar]
- 196.Kang D.G., Moon M.K., Choi D.H., Lee J.K., Kwon T.O., Lee H.S. Vasodilatory and anti-inflammatory effects of the 1,2,3,4,6-penta-O-galloyl-beta-D-glucose (PGG) via a nitric oxide-cGMP pathway. Eur. J. Pharmacol. 2005;524:111–119. doi: 10.1016/j.ejphar.2005.08.061. [DOI] [PubMed] [Google Scholar]
- 197.Tirapelli C.R., Ambrosio S.R., da Costa F.B., de Oliveira A.M. Evidence for the mechanisms underlying the effects of pimaradienoic acid isolated from the roots of Viguiera arenaria on rat aorta. Pharmacology. 2004;70:31–38. doi: 10.1159/000074240. [DOI] [PubMed] [Google Scholar]
- 198.Zhu X.M., Fang L.H., Li Y.J., Du G.H. Endothelium-dependent and -independent relaxation induced by pinocembrin in rat aortic rings. Vascul. Pharmacol. 2007;46:160–165. doi: 10.1016/j.vph.2006.09.003. [DOI] [PubMed] [Google Scholar]
- 199.Estrada O., González-Guzmán J.M., Salazar-Bookaman M., Fernández A.Z., Cardozo A., Alvarado-Castillo C. Pomolic acid of Licania pittieri elicits endothelium-dependent relaxation in rat aortic rings. Phytomedicine. 2011;18:464–469. doi: 10.1016/j.phymed.2010.10.008. [DOI] [PubMed] [Google Scholar]
- 200.Xu Z., Wang X., Dai Y., Kong L., Wang F., Xu H., Lu D., Song J., Hou Z. Praeruptorin A enantiomers exert distinct relaxant effects on isolated rat aorta rings dependent on endothelium and nitric oxide synthesis. Chem. Biol. Interact. 2010;186:239–246. doi: 10.1016/j.cbi.2010.04.024. [DOI] [PubMed] [Google Scholar]
- 201.Aldini G., Carini M., Piccoli A., Rossoni G., Facino R.M. Procyanidins from grape seeds protect endothelial cells from peroxynitrite damage and enhance endothelium-dependent relaxation in human artery: new evidences for cardio-protection. Life Sci. 2003;73:2883–2898. doi: 10.1016/S0024-3205(03)00697-0. [DOI] [PubMed] [Google Scholar]
- 202.Matsui T., Korematsu S., Byun E.B., Nishizuka T., Ohshima S., Kanda T. Apple procyanidins induced vascular relaxation in isolated rat aorta through NO/cGMP pathway in combination with hyperpolarization by multiple K+ channel activations. Biosci. Biotechnol. Biochem. 2009;73:2246–2251. doi: 10.1271/bbb.90334. [DOI] [PubMed] [Google Scholar]
- 203.Tokoudagba J.M., Auger C., Bréant L., N'gom S., Chabert P., Idris-Khodja N., Gbaguidi F., Gbenou J., Moudachirou M., Lobstein A., et al. Procyanidin-rich fractions from Parkia biglobosa (Mimosaceae) leaves cause redox-sensitive endothelium-dependent relaxation involving NO and EDHF in porcine coronary artery. J. Ethnopharmacol. 2010;132:246–250. doi: 10.1016/j.jep.2010.08.031. [DOI] [PubMed] [Google Scholar]
- 204.Ajay M., Gilani A.U., Mustafa M.R. Effects of flavonoids on vascular smooth muscle of the isolated rat thoracic aorta. Life Sci. 2003;74:603–612. doi: 10.1016/j.lfs.2003.06.039. [DOI] [PubMed] [Google Scholar]
- 205.Chiwororo W.D., Ojewole J.A. Dual effect of quercetin on rat isolated portal vein smooth muscle contractility. Cardiovasc. J. Afr. 2010;21:132–136. [PMC free article] [PubMed] [Google Scholar]
- 206.Guerrero M.F., Puebla P., Carrón R., Martín M.L., San Román L. Quercetin 3,7-dimethyl ether: A vasorelaxant flavonoid isolated from Croton schiedeanus Schlecht. J. Pharm. Pharmacol. 2002;54:1373–1378. doi: 10.1211/002235702760345455. [DOI] [PubMed] [Google Scholar]
- 207.Fan Y.F., Chen Z.W., Guo Y., Wang Q.H., Song B. Cellular mechanisms underlying hyperin-induced relaxation of rat basilar artery. Fitoterapia. 2011;82:626–631. doi: 10.1016/j.fitote.2011.01.023. [DOI] [PubMed] [Google Scholar]
- 208.Chen C.K., Pace-Asciak C.R. Vasorelaxing activity of resveratrol and quercetin in isolated rat aorta. Gen. Pharmacol. 1996;27:363–366. doi: 10.1016/0306-3623(95)02001-2. [DOI] [PubMed] [Google Scholar]
- 209.Gojkovic-Bukarica L., Novakovic A., Kanjuh V., Bumbasirevic M., Lesic A., Heinle H. A role of ion channels in the endothelium-independent relaxation of rat mesenteric artery induced by resveratrol. J. Pharmacol. Sci. 2008;108:124–130. doi: 10.1254/jphs.08128FP. [DOI] [PubMed] [Google Scholar]
- 210.Medeiros M.A., Nunes X.P., Barbosa-Filho J.M., Lemos V.S., Pinho J.F., Roman-Campos D., de Medeiros I.A., Araújo D.A., Cruz J.S. (S)-reticuline induces vasorelaxation through the blockade of L-type Ca(2+) channels. Naunyn Schmiedebergs Arch. Pharmacol. 2009;379:115–125. doi: 10.1007/s00210-008-0352-1. [DOI] [PubMed] [Google Scholar]
- 211.Xia M.L., Zhou X.M., Yao H., Jiang H.D., Bruce I.C., Wei E.Q., Xia Q. Rutin-induced endothelium-dependent vasorelaxation in rat aortic rings and the underlying mechanism. Conf. Proc. IEEE Eng. Med. Biol. Soc. 2005;6:5595–5597. doi: 10.1109/IEMBS.2005.1615754. [DOI] [PubMed] [Google Scholar]
- 212.Lam F.F., Yeung J.H., Kwan Y.W., Chan K.M., Or P.M. Salvianolic acid B, an aqueous component of danshen (Salvia miltiorrhiza), relaxes rat coronary artery by inhibition of calcium channels. Eur. J. Pharmacol. 2006;553:240–245. doi: 10.1016/j.ejphar.2006.09.030. [DOI] [PubMed] [Google Scholar]
- 213.Hu C.M., Cheng H.W., Cheng Y.W., Kan J.J. Mechanisms underlying the induction of vasorelaxation in rat thoracic aorta by sanguinarine. Jpn. J. Pharmacol. 2001;85:47–53. doi: 10.1254/jjp.85.47. [DOI] [PubMed] [Google Scholar]
- 214.Sano S., Sugiyama K., Ito T., Katano Y., Ishihata A. Identification of the strong vasorelaxing substance scirpusin B, a dimer of piceatannol, from passion fruit (Passiflora edulis) seeds. J. Agric. Food Chem. 2011;59:6209–6213. doi: 10.1021/jf104959t. [DOI] [PubMed] [Google Scholar]
- 215.Pan Z., Feng T., Shan L., Cai B., Chu W., Niu H., Lu Y., Yang B. Scutellarin-induced endothelium-independent relaxation in rat aorta. Phytother. Res. 2008;22:1428–1433. doi: 10.1002/ptr.2364. [DOI] [PubMed] [Google Scholar]
- 216.Wang G.J., Shum A.Y., Lin Y.L., Liao J.F., Wu X.C., Ren J., Chen C.F. Calcium channel blockade in vascular smooth muscle cells: Major hypotensive mechanism of S-petasin, a hypotensive sesquiterpene from Petasites formosanus. J. Pharmacol. Exp. Ther. 2001;297:240–246. [PubMed] [Google Scholar]
- 217.Kwan C.Y. Plant-derived drugs acting on cellular Ca2+ mobilization in vascular smooth muscle: Tetramethylpyrazine and tetrandrine. Stem Cells. 1994;12:64–67. doi: 10.1002/stem.5530120111. [DOI] [PubMed] [Google Scholar]
- 218.Shao Z., Li J., Zhao Z., Gao C., Sun Z., Liu X. Effects of tetramethylpyrazine on nitric oxide/cGMP signaling after cerebral vasospasm in rabbits. Brain Res. 2010;1361:67–75. doi: 10.1016/j.brainres.2010.09.011. [DOI] [PubMed] [Google Scholar]
- 219.Kim E.Y., Kim J.H., Rhyu M.R. Endothelium-independent vasorelaxation by Ligusticum wallichii in isolated rat aorta: Comparison of a butanolic fraction and tetramethylpyrazine, the main active component of Ligusticum wallichii. Biol. Pharm. Bull. 2010;33:1360–1363. doi: 10.1248/bpb.33.1360. [DOI] [PubMed] [Google Scholar]
- 220.Peng W., Hucks D., Priest R.M., Kan Y.M., Ward J.P. Ligustrazine-induced endothelium-dependent relaxation in pulmonary arteries via an NO-mediated and exogenous L-arginine-dependent mechanism. Br. J. Pharmacol. 1996;119:1063–1071. doi: 10.1111/j.1476-5381.1996.tb15778.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Tur R., Magraner J., Catret M., Elorriaga M., Ivorra M.D., D'Ocon P., Bermejo A., Cabedo N., Cortes D., Anselmi E. Mechanism of vascular relaxation by thaligrisine: Functional and binding assays. Life Sci. 2000;67:1535–1548. doi: 10.1016/S0024-3205(00)00752-9. [DOI] [PubMed] [Google Scholar]
- 222.Hernández-Abreu O., Castillo-España P., León-Rivera I., Ibarra-Barajas M., Villalobos-Molina R., González-Christen J., Vergara-Galicia J., Estrada-Soto S. Antihypertensive and vasorelaxant effects of tilianin isolated from Agastache mexicana are mediated by NO/cGMP pathway and potassium channel opening. Biochem. Pharmacol. 2009;78:54–61. doi: 10.1016/j.bcp.2009.03.016. [DOI] [PubMed] [Google Scholar]
- 223.Silva R.M., Oliveira F.A., Cunha K.M., Maia J.L., Maciel M.A., Pinto A.C., Nascimento N.R., Santos F.A., Rao V.S. Cardiovascular effects of trans-dehydrocrotonin, a diterpene from Croton cajucara in rats. Vascul. Pharmacol. 2005;43:11–18. doi: 10.1016/j.vph.2005.02.015. [DOI] [PubMed] [Google Scholar]
- 224.Orallo F., Alvarez E., Camiña M., Leiro J.M., Gómez E., Fernández P. The possible implication of trans-Resveratrol in the cardioprotective effects of long-term moderate wine consumption. Mol. Pharmacol. 2002;61:294–302. doi: 10.1124/mol.61.2.294. [DOI] [PubMed] [Google Scholar]
- 225.Elíes J., Cuíñas A., García-Morales V., Orallo F., Campos-Toimil M. Trans-resveratrol simultaneously increases cytoplasmic Ca(2+) levels and nitric oxide release in human endothelial cells. Mol. Nutr. Food Res. 2011;55:1237–1248. doi: 10.1002/mnfr.201100240. [DOI] [PubMed] [Google Scholar]
- 226.Matsuo H., Okamoto R., Zaima K., Hirasawa Y., Ismail I.S., Lajis N.H., Morita H. New vasorelaxant indole alkaloids, villocarines A-D from Uncaria villosa. Bioorg. Med. Chem. 2011;19:4075–4079. doi: 10.1016/j.bmc.2011.05.014. [DOI] [PubMed] [Google Scholar]
- 227.Arai H., Zaima K., Mitsuta E., Tamamoto H., Saito A., Hirasawa Y., Rahman A., Kusumawati I., Zaini N.C., Morita H. Alstiphyllanines I-O, ajmaline type alkaloids from Alstonia macrophylla showing vasorelaxant activity. Bioorg. Med. Chem. 2012;20:3454–3459. doi: 10.1016/j.bmc.2012.04.013. [DOI] [PubMed] [Google Scholar]
- 228.Duarte J., Vallejo I., Pérez-Vizcaino F., Jiménez R., Zarzuelo A., Tamargo J. Effects of visnadine on rat isolated vascular smooth muscles. Planta Med. 1997;63:233–236. doi: 10.1055/s-2006-957660. [DOI] [PubMed] [Google Scholar]
- 229.Duarte J., Pérez-Vizcaíno F., Torres A.I., Zarzuelo A., Jiménez J., Tamargo J. Vasodilator effects of visnagin in isolated rat vascular smooth muscle. Eur. J. Pharmacol. 1995;286:115–122. doi: 10.1016/0014-2999(95)00418-K. [DOI] [PubMed] [Google Scholar]
- 230.Seya K., Furukawa K., Taniguchi S., Kodzuka G., Oshima Y., Niwa M., Motomura S. Endothelium-dependent vasodilatory effect of vitisin C, a novel plant oligostilbene from Vitis plants (Vitaceae), in rabbit aorta. Clin. Sci. 2003;105:73–79. doi: 10.1042/CS20020288. [DOI] [PubMed] [Google Scholar]
- 231.Del Valle-Mondragón L., Tenorio-López F.A., Torres-Narváez J.C., Zarco-Olvera G., Pastelín-Hernández G. Coronary vasodilator activity of vulgarenol, a sesquiterpene isolated from Magnolia grandiflora, and its possible mechanism. Phytother. Res. 2009;23:666–671. doi: 10.1002/ptr.2696. [DOI] [PubMed] [Google Scholar]
- 232.Cheng Y.W., Kang J.J. Mechanism of vasorelaxation of thoracic aorta caused by xanthone. Eur. J. Pharmacol. 1997;336:23–8. doi: 10.1016/S0014-2999(97)01224-7. [DOI] [PubMed] [Google Scholar]
- 233.Campos M.G., Oropeza M.V., Villanueva T., Aguilar M.I., Delgado G., Ponce H.A. Xanthorrhizol induces endothelium-independent relaxation of rat thoracic aorta. Life Sci. 2000;67:327–333. doi: 10.1016/S0024-3205(00)00619-6. [DOI] [PubMed] [Google Scholar]
- 234.Moncada S., Higgs E.A. The discovery of nitric oxide and its role in vascular biology. Br. J. Pharmacol. 2006;147(Suppl. 1):S193–S201. doi: 10.1038/sj.bjp.0706458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Melikian N., Seddon M.D., Casadei B., Chowienczyk P.J., Shah A.M. Neuronal nitric oxide synthase and human vascular regulation. Trends Cardiovasc. Med. 2009;19:256–262. doi: 10.1016/j.tcm.2010.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Shah M.R., Wedgwood S., Czech L., Kim G.A., Lakshminrusimha S., Schumacker P.T., Steinhorn R.H., Farrow K.N. Cyclic stretch induces inducible nitric oxide synthase and soluble guanylate cyclase in pulmonary artery smooth muscle cells. Int. J. Mol. Sci. 2013;14:4334–4348. doi: 10.3390/ijms14024334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Li H., Fosterman U. Nitric oxide in the pathogenesis of vascular disease. J. Pathol. 2000;190:244–254. doi: 10.1002/(SICI)1096-9896(200002)190:3<244::AID-PATH575>3.0.CO;2-8. [DOI] [PubMed] [Google Scholar]
- 238.Förstermann U., Sessa W.C. Nitric oxide synthases: regulation and function. Eur. Heart J. 2012;33:829–837. doi: 10.1093/eurheartj/ehr304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Li H., Wallerath T., Munzel T., Forstermann U. Regulation of endothelial-type NO synthase expression in pathophisiology and in response to drugs. Nitric Oxide. 2002;7:149–164. doi: 10.1016/S1089-8603(02)00111-8. [DOI] [PubMed] [Google Scholar]
- 240.Fleming I., Busse R. Molecular mechanisms involved in the regulation of the endothelial nitric oxide synthase. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2003;284:R1–R12. doi: 10.1152/ajpregu.00323.2002. [DOI] [PubMed] [Google Scholar]
- 241.Steinkamp-Fenske K., Bollinger L., Xu H., Yao Y., Horke S., Förstermann U., Li H. Reciprocal regulation of endothelial nitric-oxide synthase and NADPH oxidase by betulinic acid in human endothelial cells. J. Pharmacol. Exp. Ther. 2007;322:836–842. doi: 10.1124/jpet.107.123356. [DOI] [PubMed] [Google Scholar]
- 242.Li H., Xia N., Brausch I., Yao Y., Forstermann U. Flavonoids from artichoke (Cynara scolymus L.) up-regulate endothelial-type nitric-oxide synthase gene expression in human endothelial cells. J. Pharmacol. Exp. Ther. 2004;310:926–932. doi: 10.1124/jpet.104.066639. [DOI] [PubMed] [Google Scholar]
- 243.Xia N., Bollinger L., Steinkamp-Fenske K., Förstermann U., Li H. Prunella vulgaris L. Upregulates eNOS expression in human endothelial cells. Am. J. Chin. Med. 2010;38:599–611. doi: 10.1142/S0192415X10008081. [DOI] [PubMed] [Google Scholar]
- 244.Kinoshita Y., Kawakami S., Yanae K., Sano S., Uchida H., Inagaki H., Ito T. Effect of long-term piceatannol treatment on eNOS levels in cultured endothelial cells. Biochem. Biophys. Res. Commun. 2012 doi: 10.1016/j.bbrc.2012.12.017. [DOI] [PubMed] [Google Scholar]
- 245.Park J.Y., Shin H.K., Choi Y.W., Lee Y.J., Bae S.S., Han J., Kim C.D. Gomisin A induces Ca2+-dependent activation of eNOS in human coronary artery endothelial cells. J. Ethnopharmacol. 2009;125:291–296. doi: 10.1016/j.jep.2009.06.028. [DOI] [PubMed] [Google Scholar]
- 246.Brandes R.P., Schmitz-Winnenthal F.H., Félétou M., Gödecke A., Huang P.L., Vanhoutte P.M., Fleming I., Busse R. An endothelium-derived hyperpolarizing factor distinct from NO and prostacyclin is a major endothelium-dependent vasodilator in resistance vessels of wild-type and endothelial NO synthase knockout mice. Proc. Natl. Acad. Sci. USA. 2000;97:9747–9752. doi: 10.1073/pnas.97.17.9747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Hsieh T.C., Lu X., Guo J., Wu J.M. Differential regulation of proliferation, cell cycle control and gene expression in cultured human aortic and pulmonary artery endothelial cells by resveratrol. Int. J. Mol. Med. 2010;26:743–749. doi: 10.3892/ijmm_00000521. [DOI] [PubMed] [Google Scholar]
- 248.Bruder J.L., Hsieh T., Lerea K.M., Olson S.C., Wu J.M. Induced cytoskeletal changes in bovine pulmonary artery endothelial cells by resveratrol and the accompanying modified responses to arterial shear stress. BMC Cell Biol. 2001;2:10–1186. doi: 10.1186/1471-2121-2-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Cherkaoui-Tangi K., Lachkar M., Wibo M., Morel N., Gilani A.H., Lyoussi B. Pharmacological studies on hypotensive, diuretic and vasodilator activities of chrysin glucoside from Calycotome villosa in rats. Phytother. Res. 2008;22:356–361. doi: 10.1002/ptr.2322. [DOI] [PubMed] [Google Scholar]
- 250.Tanaka Y., Yamaki F., Koike K., Toro L. New insights into the intracellular mechanisms by which PGI2 analogues elicit vascular relaxation: Cyclic AMP-independent, Gs-protein mediated-activation of maxiK Channel. Curr. Med. Chem. Cardiovasc. Hematol. Agents. 2004;2:257–265. doi: 10.2174/1568016043356273. [DOI] [PubMed] [Google Scholar]
- 251.Yeung D.K., Leung S.W., Xu Y.C., Vanhoutte P.M., Man R.Y. Puerarin, an isoflavonoid derived from Radix puerariae, potentiates endothelium-independent relaxation via the cyclic AMP pathway in porcine coronary artery. Eur. J. Pharmacol. 2006;552:105–111. doi: 10.1016/j.ejphar.2006.08.078. [DOI] [PubMed] [Google Scholar]
- 252.Bender A.T., Beavo J.A. Cyclic nucleotide phosphodiesterases: molecular regulation to clinical use. Pharmacol. Rev. 2006;58:488–520. doi: 10.1124/pr.58.3.5. [DOI] [PubMed] [Google Scholar]
- 253.Pauvert O., Lugnier C., Keravis T., Marthan R., Rousseau E., Savineau J.P. Effect of sildenafil on cyclic nucleotide phosphodiesterase activity, vascular tone and calcium signaling in rat pulmonary artery. Br. J. Pharmacol. 2003;139:513–522. doi: 10.1038/sj.bjp.0705277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Rybalkin S.D., Yan C., Bornfeldt K.E., Beavo J.A. Cyclic GMP phosphodiesterases and regulation of smooth muscle function. Circ. Res. 2003;93:280–291. doi: 10.1161/01.RES.0000087541.15600.2B. [DOI] [PubMed] [Google Scholar]
- 255.Keravis T., Thaseldar-Roumie R., Lugnier C. Assessment of phosphodiesterase isozyme contribution in cell and tissue extracts. Methods Mol. Biol. 2005;307:63–74. doi: 10.1385/1-59259-839-0:063. [DOI] [PubMed] [Google Scholar]
- 256.Ko E.A., Han J., Jung I.D., Park W.S. Physiological roles of K+ channels in vascular smooth muscle cells. J. Smooth Muscle Res. 2008;44:65–81. doi: 10.1540/jsmr.44.65. [DOI] [PubMed] [Google Scholar]
- 257.Hayabuchi Y., Nakaya Y., Mawatari K., Inoue M., Sakata M., Kagami S. Cell membrane stretch activates intermediate-conductance Ca2+-activated K+ channels in arterial smooth muscle cells. Heart Vessels. 2011;26:91–100. doi: 10.1007/s00380-010-0025-0. [DOI] [PubMed] [Google Scholar]
- 258.Hill M.A., Yang Y., Ella S.R., Davis M.J., Braun A.P. Large conductance, Ca2+-activated K+ channels (BKCa) and arteriolar myogenic signaling. FEBS Lett. 2010;584:2033–2042. doi: 10.1016/j.febslet.2010.02.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Jackson W.F. Potassium channels in the peripheral microcirculation. Microcirculation. 2005;12:113–127. doi: 10.1080/10739680590896072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Gebremedhin D., Kaldunski M., Jacobs E.R., Harder D.R., Roman R.J. Coexistence of two types of Ca (2+)-activated K+ channels in rat renal arterioles. Am. J. Physiol. 1996;270:F69–F81. doi: 10.1152/ajprenal.1996.270.1.F69. [DOI] [PubMed] [Google Scholar]
- 261.Michelakis E.D., Reeve H.L., Huang J.M., Tolarova S., Nelson D.P., Weir E.K., Archer S.L. Potassium channel diversity in vascular smooth muscle cells. Can. J. Physiol. Pharmacol. 1997;75:889–897. doi: 10.1139/y97-111. [DOI] [PubMed] [Google Scholar]
- 262.Hill C.E., Phillips J.K., Sandow S.L. Heterogeneous control of blood flow amongst different vascular beds. Med. Res. Rev. 2001;21:1–60. doi: 10.1002/1098-1128(200101)21:1<1::aid-med1>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 263.Shao Y., Liew R., Guan B., Wong P.E., Shim W.S., Chua Y., He G. Different expression of large-conductance calcium-activated K+ channels in human internal mammary and radial arteries. Cardiovasc Res. 2011;89:329–335. doi: 10.1093/cvr/cvq304. [DOI] [PubMed] [Google Scholar]
- 264.Eichhorn B., Dobrev D. Vascular large conductance calcium-activated potassium channels: functional role and therapeutic potential. Naunyn Schmiedebergs Arch. Pharmacol. 2007;376:145–155. doi: 10.1007/s00210-007-0193-3. [DOI] [PubMed] [Google Scholar]
- 265.Félétou M., Vanhoutte P.M. Endothelium-derived hyperpolarizing factor: Where are we now? Arterioscler. Thromb. Vasc. Biol. 2006;26:1215–1225. doi: 10.1161/01.ATV.0000217611.81085.c5. [DOI] [PubMed] [Google Scholar]
- 266.Cogolludo A., Frazziano G., Briones A.M., Cobeño L., Moreno L., Lodi F., Salaices M., Tamargo J., Perez-Vizcaino F. The dietary flavonoid quercetin activates BKCa currents in coronary arteries via production of H2O2. Role in vasodilatation. Cardiovasc. Res. 2007;73:424–431. doi: 10.1016/j.cardiores.2006.09.008. [DOI] [PubMed] [Google Scholar]
- 267.Calderone V., Chericoni S., Martinelli C., Testai L., Nardi A., Morelli I., Breschi M.C., Martinotti E. Vasorelaxing effects of flavonoids: Investigation on the possible involvement of potassium channels. Naunyn Schmiedebergs Arch. Pharmacol. 2004;370:290–298. doi: 10.1007/s00210-004-0964-z. [DOI] [PubMed] [Google Scholar]
- 268.Dong K., Tao Q.M., Shan Q.X., Jin H.F., Pan G.B., Chen J.Z., Zhu J.H., Xia Q. Endothelium-independent vasorelaxant effect of puerarin on rat thoracic aorta. Conf. Proc. IEEE Eng. Med. Biol. Soc. 2004;5:3757–3760. doi: 10.1109/IEMBS.2004.1404054. [DOI] [PubMed] [Google Scholar]
- 269.Li Y., Johnson G., Romine J.L., Meanwell N.A., Martin S.W., Dworetzky S.I., Boissard C.G., Gribkoff V.K., Starrett J.E., Jr. Novel openers of Ca2+-dependent large-conductance potassium channels: Symmetrical pharmacophore and electrophysiological evaluation of bisphenols. Bioorg. Med. Chem. Lett. 2003;13:1437–1439. doi: 10.1016/s0960-894x(03)00156-2. [DOI] [PubMed] [Google Scholar]
- 270.Sandow S.L., Grayson T.H. Limits of isolation and culture: Intact vascular endothelium and BKCa. Am. J. Physiol. Heart Circ. Physiol. 2009;297:H1–H7. doi: 10.1152/ajpheart.00042.2009. [DOI] [PubMed] [Google Scholar]
- 271.Lam F.F., Yeung J.H., Chan K.M., Or P.M. Dihydrotanshinone, a lipophilic component of Salvia miltiorrhiza (danshen), relaxes rat coronary artery by inhibition of calcium channels. J. Ethnopharmacol. 2008;119:318–321. doi: 10.1016/j.jep.2008.07.011. [DOI] [PubMed] [Google Scholar]
- 272.Zholos A. Pharmacology of transient receptor potential melastatin channels in the vasculature. Br. J. Pharmacol. 2010;159:1559–1571. doi: 10.1111/j.1476-5381.2010.00649.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Earley S. TRPA1 channels in the vasculature. Br. J. Pharmacol. 2012;167:13–22. doi: 10.1111/j.1476-5381.2012.02018.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Earley S., Reading S., Brayden J.E. Functional Significance of Transient Receptor Potential Channels in Vascular Function. In: Liedtke W.B., Heller S., editors. TRP Ion Channel Function in Sensory Transduction and Cellular Signaling Cascades. CRC Press; Boca Raton, FL, USA: 2007. pp. 361–376. [PubMed] [Google Scholar]
- 275.Cole W.C., Welsh D.G. Role of myosin light chain kinase and myosin light chain phosphatase in the resistance arterial myogenic response to intravascular pressure. Arch. Biochem. Biophys. 2011;510:160–173. doi: 10.1016/j.abb.2011.02.024. [DOI] [PubMed] [Google Scholar]
- 276.Li L., Eto M., Lee M.R., Morita F., Yazawa M., Kitazawa T. Possible involvement of the novel CPI-17 protein in protein kinase C signal transduction of rabbit arterial smooth muscle. J. Physiol. 1998;508:871–881. doi: 10.1111/j.1469-7793.1998.871bp.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Nishimura J., Khalil R.A., Drenth J.P., van Breemen C. Evidence for increased myofilament Ca2+ sensitivity in norepinephrine-activated vascular smooth muscle. Am. J. Physiol. 1990;259:H2–H8. doi: 10.1152/ajpheart.1990.259.1.H2. [DOI] [PubMed] [Google Scholar]