Abstract
Icariin is effective in the treatment of hyperlipidemia. To understand the effect of icariin on lipid metabolism, effects of icariin on PPARα and its target genes were investigated. Mice were treated orally with icariin at doses of 0, 100, 200, and 400 mg/kg, or clofibrate (500 mg/kg) for five days. Liver total RNA was isolated and the expressions of PPARα and lipid metabolism genes were examined. PPARα and its marker genes Cyp4a10 and Cyp4a14 were induced 2-4 fold by icariin, and 4-8 fold by clofibrate. The fatty acid (FA) binding and co-activator proteins Fabp1, Fabp4 and Acsl1 were increased 2-fold. The mRNAs of mitochondrial FA β-oxidation enzymes (Cpt1a, Acat1, Acad1 and Hmgcs2) were increased 2-3 fold. The mRNAs of proximal β-oxidation enzymes (Acox1, Ech1, and Ehhadh) were also increased by icariin and clofibrate. The expression of mRNAs for sterol regulatory element-binding factor-1 (Srebf1) and FA synthetase (Fasn) were unaltered by icariin. The lipid lysis genes Lipe and Pnpla2 were increased by icariin and clofibrate. These results indicate that icariin is a novel PPARα agonist, activates lipid metabolism gene expressions in liver, which could be a basis for its lipid-lowering effects and its beneficial effects against diabetes.
Keywords: icariin, clofibrate, mouse live, PPARα, Cyp4a14, lipid-lowering effect
1. Introduction
The peroxisome proliferator activated receptor-α (PPAR-α) plays a pivotal role in the regulation of lipid metabolism and fatty acid oxidation, and is beneficial in protecting against metabolic disorders associated with type-II diabetes and obesity [1,2]. PPARα agonists, such as the fibrates, are used to correct dyslipidemia and decrease risks of cardiovascular diseases [2,3]. PPARα-null mice develop obesity and high plasma triglyceride levels [4], and they are more vulnerable to high-fat diet-induced nonalcoholic fatty liver disease (NASH) [5]. PPARα is expressed highly in liver [6] and is a key regulator for lipid metabolism. Pharmacological activation of PPARα has anti-inflammatory activities in liver, adipose, and vascular tissues [7] and PPARα agonists are proposed to be promising candidates for metabolic disorders [2].
Icariin is a flavonol glycoside isolated from Epimedium genus, which has been used in traditional Chinese medicine for thousands of years. The origination and chemical structure of icariin, its antioxidative properties and medicinal applications have been reviewed [8,9]. Our Laboratory has shown that icariin protects against cerebral ischemia/reperfusion injury [10], improves learning and memory deficit in rats induced by aluminum [11], chronic cerebral hypoperfusion [12], and by D-galactose [13]. The beneficial effects of icariin appear to be related to inhibition of beta-amyloid peptide segments [14], and the protection against lipopolysaccharide-induced neuroinflammation [15]. We have recently shown that icariin improves learning and memory functions in APP/PS1 transgenic mice through the stimulation of NO/cGMP signaling [16].
The beneficial effects of icariin on metabolic syndrome are recently recognized [17,18]. In rabbits fed a high-cholesterol diet, icariin reduced the levels of serum total cholesterol and low-density lipoprotein cholesterol [18]. In streptozocin-induced diabetes rats, icariin ameliorates streptozocin-increased activities of lactate dehydrogenase, acid phosphatase, gamma-glutamyltranspeptidase and alpha-glucosidase in the epididymis and reduces serum lipid and fructose levels [17]. Icariin also ameliorates streptozocin-induced rat diabetic retinopathy [19] and nephropathy [20]. More interestingly, icariin has been shown to induce peroxisome proliferator-activated receptor gamma coactivator-1 alpha (PGC-1alpha), peroxisome proliferator-activated receptor alpha (PPARα) during cardiomyocyte differentiation in murine embryonic stem (ES) cells [21]. In our recent studies, we found that icariin is effective in inducing Cyp4a14, a PPARα-target gene in mouse livers [22], which arouses our interest to examine whether icarriin is a PPARα activator. PPARα regulates genes encoding enzymes and transporters of fatty acid oxidation [1,2,3,4,5,6,23]. We further examined the effects of icariin on the mRNAs of lipid metabolic enzyme genes, using PPARα agonist clofibrate as a positive control. The results revealed that icariin is a novel PPARα activator and provides the molecular basis for its beneficial lipid-lowering effects by inducing fatty acid (FA) β-oxidation enzyme genes.
2. Results and Discussion
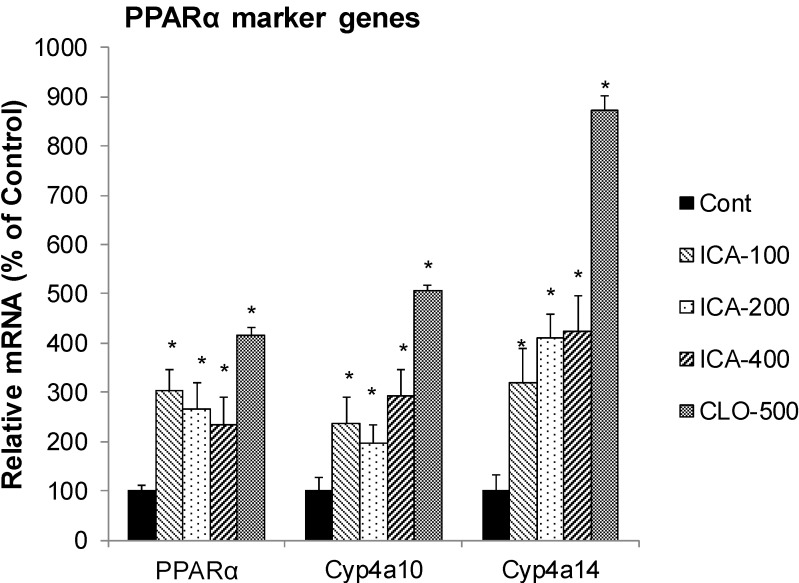
2.1. Effect of Icariin on the mRNA of PPARα and Marker Enzymes
Figure 1 illustrates the effects of icariin and clofibrate (CLO) on the expression of PPARα and PPARα-target marker genes Cyp4a10 and Cyp4a14. CLO is a well-known PPARα activator, and increased the mRNA of PPARα 4-fold, Cyp4a10 5-fold, and Cyp4a14 8.7-fold. In comparison, icariin also increased PPARα 2.3-fold, Cyp4a10 2.9-fold, and Cyp4a14 4.2-fold. Administration of icarriin and/or CLO did not affect animal body weight, animal general health and did not produce histopathological alterations (Data not shown).
Figure 1.
Effects of Icariin (ICA) on expression of PPARα and PPARα marker enzymes. Data are expressed as mean ± SEM (n = 5). * Significantly different from CMC-treated mice (p < 0.05).
In our preliminary studies, icariin induced Cyp4a14 in Kunming mice [22], and this effect is now further verified in C57BL/6 mice in the present study, with clofibrate as a positive control. The induction of Cyp4a14 suggests that icariin could affect lipid metabolism, as icariin has recently been shown to have lipid-lowering effects in rabbits [18] and in rats [17]. In cultured cells, icariin has been shown to induce PPARα [21]. In the present study, icariin not only induced PPARα, but also PPARα activation marker enzyme gene Cyp4a10 and Cyp4a14. The results indicate that icariin is a novel PPARα activator and provides the molecular basis for its beneficial lipid-lowering effects by inducing FA β-oxidation enzyme genes.
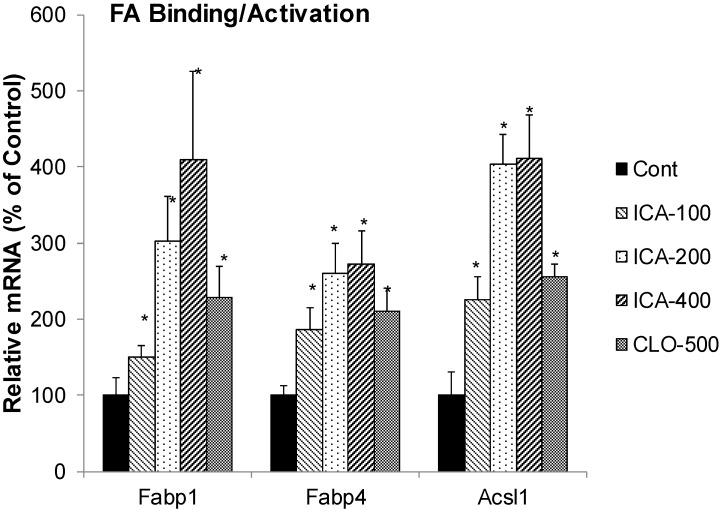
2.2. Effect of Icariin on the mRNA of Fatty Acid Binding Protein and Activation
Figure 2 illustrates the effects of ICA and CLO on the expression of FA binding protein Fabp1, Fabp4 and long chain acyl-CoA synthetase 1 (Acsl1). CLO increased the mRNA of Fabp1 2.2-fold, Fabp4 2.3-fold, and Acsl1 2.6-fold. In comparison, icariin dose-dependently increased Fabp1 4-fold, Fabp4 2.7-fold, and Acsl1 4-fold.
Figure 2.
Effects of Icariin (ICA) on expression of fatty acid binding proteins and coactivators. Data are expressed as mean ± SEM (n = 5). * Significantly different from CMC-treated mice (p < 0.05).
Many drugs could reprogram the liver to adapt various stimuli and maintain homeostasis [24]. For example, PPARα regulates genes encoding enzymes and transporters of fatty acid oxidation [1,2,3,4,5,6,23]. Liver FA binding protein (FABP1) prevents lipotoxicity of free fatty acids and regulates FA trafficking and partition, and is activated by PPARα [25]. FABPs are the major soluble protein that binds very-long-chain n-3 polyunsaturated fatty acids (n-3 PUFAs) in hepatocytes [26]. Mice deficient in liver FA binding protein (L-FABP-/-) exacerbated diet-induced weight gain and fat tissue mass gain when fed high-fat diet [27]. Acyl-CoA synthetase is a family of enzymes that catalyze the esterification of FA with CoA. Long-chain acyl CoA synthetase 1 (Acsl1) plays an important role in fatty acid metabolism and triacylglycerol synthesis and increased fatty acid uptake into hepatocytes for esterification [28], and is a PPARα target or co-activator [29]. In the present study the expression of FA binding protein Fabp1 and Fabp4, as well as Acsl1 were increased by icarriin and clofibrate, implying that icarriin activation of PPARα could enhance FA metabolism by increasing FA binding and co-activation.
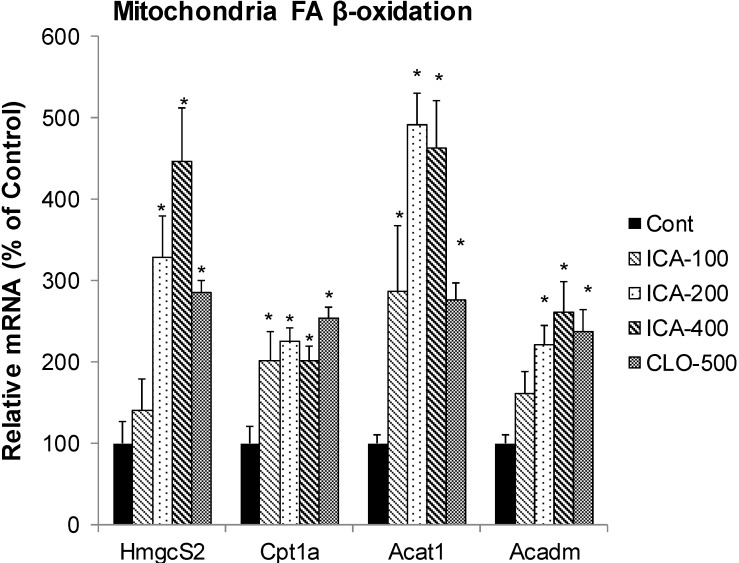
2.3. Effect of Icariin on the mRNA of Mitochondria FA β-Oxidation
Figure 3 shows the effects of icariin and CLO on FA mitochondria β-oxidation, including Cpt1a (carnitine palmitoyltransferase 1a, rate-limiting enzyme of mitochondria FA oxidation), Acat1 (acetyl-CoA acetyltransferase 1, an enzyme central to multiple metabolic pathways), Acadm (Acad1) (Acyl-coenzyme A dehydrogenase 1, catalyzes mitochondrial fatty acid beta-oxidation), and Hmgcs2 (Mitochondrial HMG-CoA synthase, the rate-limiting enzyme in ketogenesis). CLO increased the mRNA of Cpt1a 2.8-fold, Acat1 2.5-fold, Acadm 2.4-fold, and Hmgcs2 2.9-fold. In comparison, icariin dose-dependently increased Cpt1a 4.6-fold, Acat1 2.3-fold, Acadm 2.6-fold and Hmgcs2 4.5-fold.
Figure 3.
Effects of Icariin (ICA) on expression of mitochondrial fatty acid β-oxidation enzymes. Data are expressed as mean ± SEM (n = 5). * Significantly different from CMC-treated mice (p < 0.05).
Mitochondria FA β-oxidation and ketone body formation is important in lipid metabolism [30]. Hmgcs2 encodes the key enzyme for ketone-body synthesis, the mitochondrial HMG-CoA synthase [31] and is the rate-limiting enzyme in ketogenesis. Hmgcs2 has been shown to interact with PPARα and acts as a co-activator to up-regulate transcription of genes of lipid metabolism [32]. Cpt1a is a rate-limiting enzyme of mitochondria FA oxidation, which is co-localized with Acsl1 in the liver mitochondrial outer membrane as a part of FA transfer complex [33]. Acat1 is an enzyme central to multiple metabolic pathways [34], and Acadm catalyzes mitochondrial FA β-oxidation [35]. Several compounds such as fenofibrate [35], gemfibrozil analogues [36], inhibitors of FA synthesis [37] and herbal medicine oxymatrine [38], all increase Cpt1a, and/or Acat1, Acadm, Hmgcs2 as a mechanism of their lipid-lowering effects, thus, up-regulation of mitochondrial FA β-oxidation could be a mechanism for lipid lowering effects of icariin.
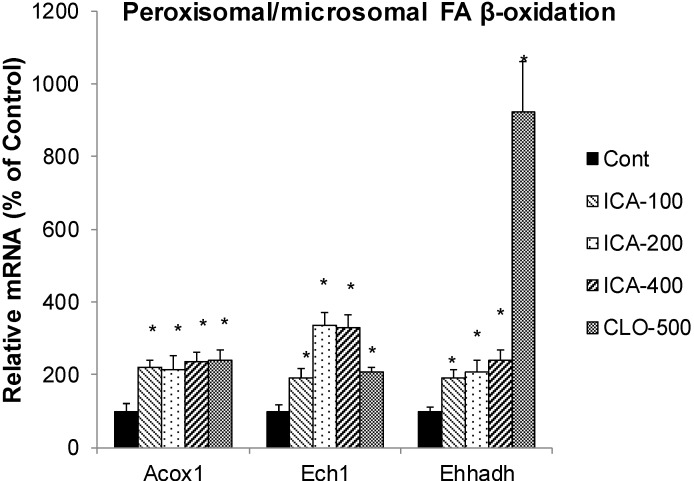
2.4. Effect of Icariin on the mRNA of Peroxisome FA Oxidation
Figure 4 shows the effects of icariin and CLO on peroxisome FA oxidation, including Acox1 (acyl-CoA oxidase 1, a key enzyme involved in peroxisome β-oxidation), Ech1 (enoyl coenzyme A hydratase 1, peroxisome FA oxidation), and Ehhadh (Enoyl-CoA, 3-hydroxyacyl CoA Dehydrogenase, a proximal L-bifunctional protein). CLO increased the mRNA of Acox1 2.4-fold, Ech1 2.1-fold, but markedly increased Ehhadh 11-fold. In comparison, icariin increased Acox1 2.4-fold, Ech1 3.3-fold (in dose-dependent manner), and Ehhadh 2.4-fold.
Figure 4.
Effects of Icariin (ICA) on expression of peroxisome fatty acid β-oxidation enzymes. Data are expressed as mean ± SEM (n = 5). * Significantly different from CMC-treated mice (p < 0.05).
Peroxisomal FA β-oxidation is another important route of FA metabolism and is regulated by PPARα. Acox1, Ech1, and Ehhadh are key enzymes involved in peroxisomal β-oxidation [39,40,41,42]. Green tea polyphenols [40] and Compound K [42] alleviate obesity by induction of Acox1. Ech1 is an important component of enhanced peroxisomal β-oxidation in C57 mice [39]. Ehhadh is indispensable for the production of medium-chain dicarboxylic acids, providing an explanation for the coordinated induction of mitochondrial and peroxisomal oxidative pathways during fasting [41]. In the present study, the mRNAs of these enzymes were increased by icariin and clofibrate, and marked increase of Ehhadh was seen with clofibrate. The increased peroxisomal FA oxidation together with mitochondrial FA oxidation would enhance FA metabolism and turn over via PPARα activation pathway.
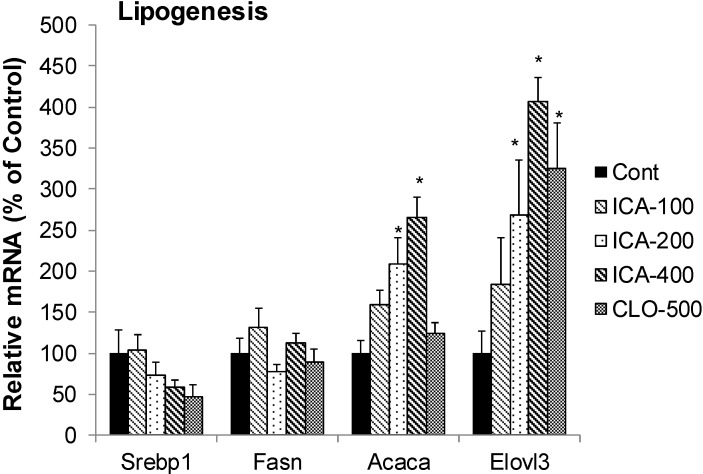
2.5. Effect of Icariin on the mRNA of Lipogenesis
Figure 5 shows the effects of icariin and CLO on mRNAs of lipogenesis enzymes, including Srebp1 (sterol regulatory element-binding protein 1, a transcription factor for lipogenesis), Fasn (fatty acid synthase, a key enzyme in lipogenesis), Acaca (Acetyl-CoA carboxylase 1), a rate-limiting enzyme in FA synthesis, and Elovl3 (elongation of very long chain fatty acids 3, involved in the regulation of the progression of adipogenesis). CLO decreased the mRNA of Srebp1 50%, had no effects on mRNA levels of Fasn and Acaca, but increased Elovl3 3.3-fold. In comparison, icariin also decreased the mRNA of Srebp1 40%, had no effects on mRNA levels of Fasn, but increased the expression of Acaca (2.6-fold) and Elovl3 (4-fold).
Figure 5.
Effects of Icariin (ICA) on Expression of lipogenesis enzymes. Data are expressed as mean ± SEM (n = 5). * Significantly different from CMC-treated mice (p < 0.05).
Srebp1 is a key transcription factor and Fasn is the key enzyme of lipogenesis [30,43]. The expression of the Elovl3 is under the control of PPARα [44]. Inhibition of Srebp1 and/or Fasn is proposed as a mechanism of lipid-lowering effects of resveratrol [45], betulinic acid [46], and oxymatrine [38]. In the present study, both icariin and clofibrate did not show apparent effects on the mRNA of Srebp1 and Fasn. However, they increased the lipogenesis enzyme Acaca and Elovl3.
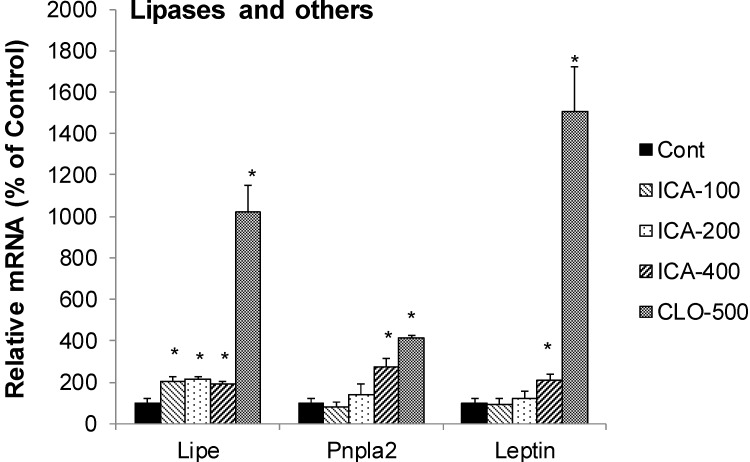
2.6. Effect of Icariin on the mRNA of Lipolysis
Figure 6 shows the effects of icariin and CLO on mRNAs of lipolysis enzymes, including Lipe (hormone-sensitive lipase), Pnpla2 (adipose triglyceride lipase, also known as ATGL) and Leptin. CLO increased the mRNA of Lipe 10-fold, Pnpla2 4-fold, but markedly increased the mRNA of leptin (15-fold). In comparison, icariin increased Lipe 2-fold, Pnpla2 (7-fold), and leptin (2-fold).
Figure 6.
Effects of Icariin (ICA) on expression of lipolytic enzymes. Data are expressed as mean ± SEM (n = 5). * Significantly different from CMC-treated mice (p < 0.05).
Another interesting observation in this study is the increased mRNA levels of lipolysis, namely Pnpla2 and Lipe. Lipe is a hormone-sensitive lipase, and Pnpla2 is a members of the Patatin-like Phospholipase Domain containing Protein A (PNPLA) family playing key roles in triglyceride hydrolysis and energy metabolism, particular Pnpla2 (also called ATGL) [47]. Increased expression of Pnpla2 plays a role in protecting steatohepatitis [48]. Thus, the increase of Pnpla2 and Lipe by icariin and clofibrate is related to PPARα activation and would be beneficial and related to their lipid-lowering effects.
3. Experimental Section
3.1. Chemicals
Icariin was obtained from Zelang Medical Technology CO., LTD (Nanjing, China) with a purity of 98%. Clofibrate was from Sigma (St. Louis, MO, USA) and other chemicals were reagent grade.
3.2. Animals and Treatments
Adult 8-week old male C57BL/6 mice were obtained from the Animal Breeding Center (Chongqing, China), and maintained in the SPF-grade animal facilities (Certificate #SYXK2011-004). Mice were acclimated for 1-week in a temperature- and humidity-controlled facility with a standard 12-h light schedule. Mice had free access to SPF-grade rodent chow (Chongqing, China) and purified drinking water. Mice were treated with icariin (100, 200, and 400 mg/kg, dissolved in 2% carboxymethylcellulose sodium (CMC, as a vehicle) for 5 days. Clofibrate (CLO, 500 mg/kg, po for 5 days) was used as a positive control, for negative controls, mice were given 2% CMC (10 mL/kg). 24 h after the last dose, livers were collected for analysis. All animal procedures follow the NIH guide of Humane Use and Care Animals, and approved by Institutional Animal Use and Care Committee of Zunyi Medical College.
3.3. Animal General Health and Histopathology
Mice were monitored daily, the body weight were recorded. Liver weight was recorded at sacrifice. Liver samples were fixed in 10% formalin prior to routine processing and paraffin embedding. Liver sections (5 µm in thickness) were stained with hematoxylin and eosin and evaluated for hepatocellular necrosis.
3.4. RNA Isolation
Total RNA was isolated using RNAiso Plus (TaKaRa Biotechnology, Dalian, China), according to the manufacturer’s protocol. Total RNA was further purified with RNAeasy Mini Kit (Qiagen, Valencia, CA, USA). The concentration of total RNA in each sample was quantified spectrophotometrically at 260 nm. The integrity of each RNA sample was evaluated by formaldehyde-agarose gel electrophoresis and 260/280 nm ratio (>1.8).
3.5. Real-Time RT-PCR Analysis
Total RNA in mouse livers was reverse-transcribed into cDNA by High Capacity cDNA Reverse Transcription Kit (Applied Biosystems, Foster City, CA, USA), and the resulting cDNA was used for real-time PCR analysis using Power SYBR® Green PCR Master Mix (Applied Biosystems). Oligonucleotide primers were designed with Primer3 software and listed in Table 1. Relative expression of genes was calculated by the 2-ΔΔCt method and normalizing to the house-keeping gene GAPDH, and the relative transcript levels were calculated as percentage of GAPDH.
Table 1.
Primer sequences for real-time RT-PCR analysis.
| Gene | GenBank No. | Forward | Reverse |
|---|---|---|---|
| Acaca | NM_133360 | AGAAACCCGAACAGTGGAACT | AGGTAGCCCTTCACGGTTAAA |
| Acadm | NM_007382 | GAGCCCGGATTAGGGTTTAG | TCCCCGCTTTTGTCATATTC |
| Acat1 | NM_009230 | TCGATGACTTTGTGACCAACC | TCCACTTCAAACAGCTCGTCT |
| Acox1 | NM_015729 | CTTGGATGGTAGTCCGGAGA | TGGCTTCGAGTGAGGAAGTT |
| Acsl | NM_007981 | CAGGCAAAGCATGTCTTCAA | TCCCAGATTTTTGGCTTGTC |
| Cpt1a | NM_013495 | TGATGACGGCTATGGTGTTTC | CAAACAAGGTGATAATGTCCATC |
| Cyp410 | NM_010011 | CACACCCTGATCACCAACAG | TCCTTGATGCACATTGTGGT |
| Cyp4a14 | NM_007822 | CTGGGTGATGGAACCTCTGT | CATCTGGGAAGGTGACAGGT |
| Ech1 | NM_016772 | CGCGATGACAGTTTCCAGTA | TGTGCAGAGGAGCTCAGAGA |
| Ehhadh | NM_023737 | TGGATGTGGATGACATTGCT | GGGGAAGAGTATCGGCTAGG |
| Elovl3 | NM_007703 | GAGACCCTGCTTCCCTATCC | CTCCTTCCCTTCATCCTTCC |
| Fabp1 | NM_017399 | ATGAACTTCTCCGGCAAGTAC | ACTTTTTCCCCAGTCATGGTC |
| Fabp4 | NM_024406 | TCACCTGGAAGACAGCTCCT | AAGCCCACTCCCACTTCTTT |
| Fasn | NM_007988 | GACCTTCATGGACACAATGCT | ATACCACCAGAGACCGTTATG |
| GAPDH | M32599 | AACTTTGGCATTGTGGAAGG | GGATGCAGGGATGATGTTCT |
| Hmgcs2 | NM_008256 | CCTCTGTGAATCCTGGGTGT | CTGTGGGGAAAGATCTGCAT |
| Lipe | NM_010719 | ACGCTACACAAAGGCTGCTT | TCGTTGCGTTTGTAGTGCTC |
| Leptin | NM_008493 | CTATGCCACCTTGGTCACCT | ACCAAACCAAGCATTTTTGC |
| Pnpla2 | NM_025802 | TCATGTGACACAGCGAGTGA | AAAGAGGAGCCAAGCACAAA |
| PPARα | NM_011144 | GTCCTCAGTGCTTCCAGAGG | GGTCACCTACGAGTGGCATT |
| Srebp1 | AF374266 | GTGAGCCTGACAAGCAATCA | GGTGCCTACAGAGCAAGAGG |
3.6. Statistical Analysis
Data were analyzed using a one-way ANOVA, followed by Duncan’s multiple range test (p ≤ 0.05) utilizing SPSS 13 Software (SAS, Cary, NC, USA). Data are expressed as mean ± SEM.
4. Conclusions
The present study clearly demonstrated that icariin is a PPARα activator, induces Cyp4a10 and Cyp4a14, and regulates the mRNA levels of lipid metabolism enzymes and proteins, including fatty acid binding protein, fatty acid oxidation in mitochondria and in peroxisome. Icarriin also had effects on lipolysis and differential effects on lipogenesis, and these effects were similar to well-known PPARα activator clofibrate. These findings are novel in revealing the molecular basis for lipid-lowering effects of icariin in laboratory animals.
Acknowledgments
This study was supported by National Natural Science Foundation of China (No. 81160415), Guizhou Education Department (KY-2012-055, (2013)92) and Guizhou Administration of traditional Chinese Medicine (QZYY2013-D402).
Author Contributions
Conceived and designed the experiments: Y.-F.L., J.-S.S. and J.L. Performed the experiments: Y.-F.L., Y.-Y.X., F.J. and J.L. Analyzed the data: Y.-F.L., Y.-Y.X. and J.L. Contributed reagents/materials/analysis tools: Q.W. and J.-S.S. Wrote the paper: Y.-F.L., Y.-Y.X. and J.L.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Sample Availability: Samples of the icarriin are available from the authors as well as from commercial resources (Sigma or Chinese Pharmaceutical companies).
References
- 1.Fruchart J.C. Peroxisome proliferator-activated receptor-alpha (PPARalpha): At the crossroads of obesity, diabetes and cardiovascular disease. Atherosclerosis. 2009;205:1–8. doi: 10.1016/j.atherosclerosis.2009.03.008. [DOI] [PubMed] [Google Scholar]
- 2.Seok H., Cha B.S. Refocusing peroxisome proliferator activated receptor-α: A new insight for therapeutic roles in diabetes. Diabetes Metab. J. 2013;37:326–332. doi: 10.4093/dmj.2013.37.5.326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Duval C., Müller M., Kersten S. PPARalpha and dyslipidemia. Biochim. Biophys. Acta. 2007;1771:961–971. doi: 10.1016/j.bbalip.2007.05.003. [DOI] [PubMed] [Google Scholar]
- 4.Costet P., Legendre C., Moré J., Edgar A., Galtier P., Pineau T. Peroxisome proliferator-activated receptor alpha-isoform deficiency leads to progressive dyslipidemia with sexually dimorphic obesity and steatosis. J. Biol. Chem. 1998;273:29577–29585. doi: 10.1074/jbc.273.45.29577. [DOI] [PubMed] [Google Scholar]
- 5.Abdelmegeed M.A., Yoo S.H., Henderson L.E., Gonzalez F.J., Woodcroft K.J., Song B.J. PPARalpha expression protects male mice from high fat-induced nonalcoholic fatty liver. J. Nutr. 2011;141:603–610. doi: 10.3945/jn.110.135210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Seedorf U., Assmann G. The role of PPAR alpha in obesity. Nutr. Metab. Cardiovasc. Dis. 2001;11:189–194. [PubMed] [Google Scholar]
- 7.Gervois P., Fruchart J.C., Staels B. Inflammation, dyslipidaemia, diabetes and PPars: Pharmacological interest of dual PPARalpha and PPARgamma agonists. Int. J. Clin. Pract. Suppl. 2004;143:22–29. doi: 10.1111/j.1368-504X.2004.00376.x. [DOI] [PubMed] [Google Scholar]
- 8.Sze S.C., Tong Y., Ng T.B., Cheng C.L., Cheung H.P. Herba epimedii: Anti-oxidative properties and its medical implications. Molecules. 2010;15:7861–7670. doi: 10.3390/molecules15117861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kapoor S. Icariin and its emerging role in the treatment of osteoporosis. Chin. Med. J. 2013;126:400–404. [PubMed] [Google Scholar]
- 10.Li L., Zhou Q.X., Shi J.S. Protective effects of icariin on neurons injured by cerebral ischemia/reperfusion. Chin. Med. J. 2005;118:1637–1643. [PubMed] [Google Scholar]
- 11.Luo Y., Nie J., Gong Q.H., Lu Y.F., Wu Q., Shi J.S. Protective effects of icariin against learning and memory deficits induced by aluminium in rats. Clin. Exp. Pharmacol. Physiol. 2007;34:792–795. doi: 10.1111/j.1440-1681.2007.04647.x. [DOI] [PubMed] [Google Scholar]
- 12.Xu R.X, Wu Q., Luo Y., Gong Q.H., Yu L.M., Huang X.N., Sun A.S., Shi J.S. Protective effects of icariin on cognitive deficits induced by chronic cerebral hypoperfusion in rats. Clin. Exp. Pharmacol. Physiol. 2009;36:810–815. doi: 10.1111/j.1440-1681.2009.05149.x. [DOI] [PubMed] [Google Scholar]
- 13.Li F., Gong Q.H., Wu Q., Lu Y.F., Shi J.S. Icariin isolated from epimedium brevicornum maxim attenuates learning and memory deficits induced by d-galactose in rats. Pharmacol. Biochem. Behav. 2010;96:301–305. doi: 10.1016/j.pbb.2010.05.021. [DOI] [PubMed] [Google Scholar]
- 14.Nie J., Luo Y., Huang X.N., Gong Q.H., Wu Q., Shi J.S. Icariin inhibits beta-amyloid peptide segment 25–35 induced expression of beta-secretase in rat hippocampus. Eur. J. Pharmacol. 2010;626:213–218. doi: 10.1016/j.ejphar.2009.09.039. [DOI] [PubMed] [Google Scholar]
- 15.Guo J., Li F., Wu Q., Gong Q., Lu Y., Shi J. Protective effects of icariin on brain dysfunction induced by lipopolysaccharide in rats. Phytomedicine. 2010;17:950–955. doi: 10.1016/j.phymed.2010.03.007. [DOI] [PubMed] [Google Scholar]
- 16.Jin F., Gong Q.H., Xu Y.S., Wang L.N., Jin H., Li F., Li L.S., Ma Y.M., Shi J.S. Icariin, a phoshphodiesterase-5 inhibitor, improves learning and memory in APP/PS1 transgenic mice by stimulation of NO/cGMP signalling. Int. J. Neuropsychopharmacol. 2014;11:1–11. doi: 10.1017/S1461145713001533. [DOI] [PubMed] [Google Scholar]
- 17.Gong Y., Shi J., Xie G.Y., Liu H.R., Qi M.Y. Amelioration of icariin for the epididymis impairment induced by streptozocin (STZ) in rats. Chin. J. Appl. Physiol. 2013;29:47–50. [PubMed] [Google Scholar]
- 18.Zhang W.P., Bai X.J., Zheng X.P., Xie X.L., Yuan Z.Y. Icariin attenuates the enhanced prothrombotic state in atherosclerotic rabbits independently of its lipid-lowering effects. Planta Med. 2013;79:731–736. doi: 10.1055/s-0032-1328551. [DOI] [PubMed] [Google Scholar]
- 19.Xin H., Zhou F., Liu T., Li G.Y., Liu J., Gao Z.Z., Bai G.Y., Lu H., Xin Z.C. Icariin ameliorates streptozotocin-induced diabetic retinopathy in vitro and in vivo. Int. J. Mol. Sci. 2012;13:866–878. doi: 10.3390/ijms13010866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Qi M.Y., Chen K., Liu H.R., Su Y.H., Yu S.Q. Protective effect of Icariin on the early stage of experimental diabetic nephropathy induced by streptozotocin via modulating transforming growth factor β1 and type IV collagen expression in rats. J. Ethnopharmacol. 2011;138:731–736. doi: 10.1016/j.jep.2011.10.015. [DOI] [PubMed] [Google Scholar]
- 21.Ding L., Liang X.G., Zhu D.Y., Lou Y.J. Icariin promotes expression of PGC-1alpha, PPARalpha, and NRF-1 during cardiomyocyte differentiation of murine embryonic stem cells in vitro. Acta Pharmacol. Sin. 2007;28:1541–1549. doi: 10.1111/j.1745-7254.2007.00648.x. [DOI] [PubMed] [Google Scholar]
- 22.Xu S.F., Jin T., Lu Y.F., Li L.S., Liu J., Shi J.S. Effect of icariin on UDP-glucuronosyltransferases in mouse liver. Planta Med. 2014;80:387–392. doi: 10.1055/s-0034-1368265. [DOI] [PubMed] [Google Scholar]
- 23.Patsouris D., Reddy J.K., Müller M., Kersten S. Peroxisome proliferator-activated receptor alpha mediates the effects of high-fat diet on hepatic gene expression. Endocrinology. 2006;147:1508–1516. doi: 10.1210/en.2005-1132. [DOI] [PubMed] [Google Scholar]
- 24.Klaassen C.D. Learning to program the liver. Annu. Rev. Pharmacol. Toxicol. 2014;54:1–8. doi: 10.1146/annurev-pharmtox-011112-140312. [DOI] [PubMed] [Google Scholar]
- 25.Guzmán C., Benet M., Pisonero-Vaquero S., Moya M., García-Mediavilla M.V., Martínez-Chantar M.L., González-Gallego J., Castell J.V., Sánchez-Campos S., Jover R. The human liver fatty acid binding protein (FABP1) gene is activated by FOXA1 and PPARα; and repressed by C/EBPα: Implications in FABP1 down regulation in nonalcoholic fatty liver disease. Biochim. Biophys. Acta. 2013;1831:803–818. doi: 10.1016/j.bbalip.2012.12.014. [DOI] [PubMed] [Google Scholar]
- 26.Petrescu A.D., Huang H., Martin G.G., McIntosh A.L., Storey S.M., Landrock D., Kier A.B., Schroeder F. Impact of L-FABP and glucose on polyunsaturated fatty acid induction of PPARα-regulated β-oxidative enzymes. Am. J. Physiol. Gastrointest. Liver Physiol. 2013;304:G241–G256. doi: 10.1152/ajpgi.00334.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McIntosh A.L., Atshaves B.P., Landrock D., Landrock K.K., Martin G.G., Storey S.M., Kier A.B., Schroeder F. Liver fatty acid binding protein gene-ablation exacerbates weight gain in high-fat fed female mice. Lipids. 2013;48:435–448. doi: 10.1007/s11745-013-3777-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Krammer J., Digel M., Ehehalt F., Stremmel W., Füllekrug J., Ehehalt R. Overexpression of CD36 and acyl-CoA synthetases FATP2, FATP4 and ACSL1 increases fatty acid uptake in human hepatoma cells. Int. J. Med. Sci. 2011;8:599–614. doi: 10.7150/ijms.8.599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Thering B.J., Bionaz M., Loor J.J. Long-chain fatty acid effects on peroxisome proliferator-activated receptor-alpha-regulated genes in Madin-Darby bovine kidney cells: Optimization of culture conditions using palmitate. J. Dairy Sci. 2009;92:2027–2037. doi: 10.3168/jds.2008-1749. [DOI] [PubMed] [Google Scholar]
- 30.Rakhshandehroo M., Sanderson L.M., Matilainen M., Stienstra R., Carlberg C., de Groot P.J., Müller M., Kersten S. Comprehensive analysis of PPARalpha-dependent regulation of hepatic lipid metabolism by expression profiling. PPAR Res. 2007:26839. doi: 10.1155/2007/26839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lee K., Kerner J., Hoppel C.L. Mitochondrial carnitine palmitoyltransferase 1a (CPT1a) is part of an outer membrane fatty acid transfer complex. J. Biol. Chem. 2011;286:25655–25662. doi: 10.1074/jbc.M111.228692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Puisac B., Ramos M., Arnedo M., Menao S., Gil-Rodríguez M.C., Teresa-Rodrigo M.E., Pié A., de Karam J.C., Wesselink J.J., Giménez I., et al. Characterization of splice variants of the genes encoding human mitochondrial HMG-CoA lyase and HMG-CoA synthase, the main enzymes of the ketogenesis pathway. Mol. Biol. Rep. 2012;39:4777–4785. doi: 10.1007/s11033-011-1270-8. [DOI] [PubMed] [Google Scholar]
- 33.Kostiuk M.A., Keller B.O., Berthiaume L.G. Palmitoylation of ketogenic enzyme HMGCS2 enhances its interaction with PPARalpha and transcription at the Hmgcs2 PPRE. FASEB J. 2010;24:1914–1924. doi: 10.1096/fj.09-149765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Still A.J., Floyd B.J., Hebert A.S., Bingman C.A., Carson J.J., Gunderson D.R., Dolan B.K., Grimsrud P.A., Dittenhafer-Reed K.E., Stapleton D.S., et al. Quantification of mitochondrial acetylation dynamics highlights prominent sites of metabolic regulation. J. Biol. Chem. 2013;288:26209–26219. doi: 10.1074/jbc.M113.483396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Harano Y., Yasui K., Toyama T., Nakajima T., Mitsuyoshi H., Mimani M., Hirasawa T., Itoh Y., Okanoue T. Fenofibrate, a peroxisome proliferator-activated receptor alpha agonist, reduces hepatic steatosis and lipid peroxidation in fatty liver Shionogi mice with hereditary fatty liver. Liver Int. 2006;26:613–620. doi: 10.1111/j.1478-3231.2006.01265.x. [DOI] [PubMed] [Google Scholar]
- 36.De Filippis B., Giancristofaro A., Ammazzalorso A., D’Angelo A., Fantacuzzi M., Giampietro L., Maccallini C., Petruzzelli M., Amoroso R. Discovery of gemfibrozil analogues that activate PPARα and enhance the expression of gene CPT1A involved in fatty acids catabolism. Eur. J. Med. Chem. 2011;46:5218–5224. doi: 10.1016/j.ejmech.2011.08.022. [DOI] [PubMed] [Google Scholar]
- 37.Huang H., McIntosh A.L., Martin G.G., Petrescu A.D., Landrock K.K., Landrock D., Kier A.B., Schroeder F. Inhibitors of Fatty Acid Synthesis Induce PPAR α-Regulated fatty acid β-oxidative genes: Synergistic roles of L-FABP and glucose. PPAR Res. 2013;2013:865604. doi: 10.1155/2013/865604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shi L., Shi L., Zhang H., Hu Z., Wang C., Zhang D., Song G. Oxymatrine ameliorates non-alcoholic fatty liver disease in rats through peroxisome proliferator-activated receptor-α activation. Mol. Med. Rep. 2013;8:439–445. doi: 10.3892/mmr.2013.1512. [DOI] [PubMed] [Google Scholar]
- 39.Xie W.D., Wang H., Zhang J.F., Li J.N., Can Y., Qing L., Kung H.F., Zhang Y.O. Enhanced peroxisomal β-oxidation metabolism in visceral adipose tissues of high-fat diet-fed obesity-resistant C57BL/6 mice. Exp. Ther. Med. 2011;2:309–315. doi: 10.3892/etm.2011.208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Huang J., Zhang Y., Zhou Y., Zhang Z., Xie Z., Zhang J., Wan X. Green tea polyphenols alleviate obesity in broiler chickens through the regulation of lipid-metabolism-related genes and transcription factor expression. J. Agric. Food Chem. 2013;61:8565–8572. doi: 10.1021/jf402004x. [DOI] [PubMed] [Google Scholar]
- 41.Houten S.M., Denis S., Argmann C.A., Jia Y., Ferdinandusse S., Reddy J.K., Wanders R.J. Peroxisomal L-bifunctional enzyme (Ehhadh) is essential for the production of medium-chain dicarboxylic acids. J. Lipid Res. 2012;53:1296–1303. doi: 10.1194/jlr.M024463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kim M.S., Lee K.T., Iseli T.J., Hoy A.J., George J., Grewal T., Roufogalis B.D. Compound K modulates fatty acid-induced lipid droplet formation and expression of proteins involved in lipid metabolism in hepatocytes. Liver Int. 2013;33:1583–1593. doi: 10.1111/liv.12287. [DOI] [PubMed] [Google Scholar]
- 43.Yu H.L., Miao H.T., Gao L.F., Li L., Xi Y.D., Nie S.P., Xiao R. Adaptive responses by mouse fetus to a maternal HLE diet by downregulating SREBP1: A microarray- and bio-analytic-based study. J. Lipid Res. 2013;54:3269–80. doi: 10.1194/jlr.M037416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jakobsson A., Jörgensen J.A., Jacobsson A. Differential regulation of fatty acid elongation enzymes in brown adipocytes implies a unique role for Elovl3 during increased fatty acid oxidation. Am. J. Physiol. Endocrinol. Metab. 2005;289:E517–E526. doi: 10.1152/ajpendo.00045.2005. [DOI] [PubMed] [Google Scholar]
- 45.Lin H.C., Chen Y.F., Hsu W.H., Yang C.W., Kao C.H., Tsai T.F. Resveratrol helps recovery from fatty liver and protects against hepatocellular carcinoma induced by hepatitis B virus X protein in a mouse model. Cancer Prev. Res. 2012;5:952–962. doi: 10.1158/1940-6207.CAPR-12-0001. [DOI] [PubMed] [Google Scholar]
- 46.Quan H.Y., Kim D.Y., Kim S.J., Jo H.K., Kim G.W., Chung S.H. Betulinic acid alleviates non-alcoholic fatty liver by inhibiting SREBP1 activity via the AMPK-mTOR-SREBP signaling pathway. Biochem. Pharmacol. 2013;85:1330–1340. doi: 10.1016/j.bcp.2013.02.007. [DOI] [PubMed] [Google Scholar]
- 47.Murugesan S., Goldberg E.B., Dou E., Brown W.J. Identification of diverse lipid droplet targeting motifs in the PNPLA family of triglyceride lipases. PLoS One. 2013;8:e64950. doi: 10.1371/journal.pone.0064950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Jha P., Claudel T., Baghdasaryan A., Mueller M., Halilbasic E., Das S.K., Lass A., Zimmermann R., Zechner R., Hoefler G., et al. Role of adipose triglyceride lipase (PNPLA2) in protection from hepatic inflammation in mouse models of steatohepatitis and endotoxemia. Hepatology. 2014;59:858–869. doi: 10.1002/hep.26732. [DOI] [PubMed] [Google Scholar]