Abstract
Biofilms formed by bacterial cells are associated with drastically enhanced resistance against most antimicrobial agents, contributing to the persistence and chronicization of the microbial infections and to therapy failure. The purpose of this study was to combine the unique properties of magnetic nanoparticles with the antimicrobial activity of three essential oils to obtain novel nanobiosystems that could be used as coatings for catheter pieces with an improved resistance to Staphylococcus aureus and Klebsiella pneumoniae clinical strains adherence and biofilm development. The essential oils of ylang ylang, patchouli and vanilla were stabilized by the interaction with iron oxide@C14 nanoparticles to be further used as coating agents for medical surfaces. Iron oxide@C14 was prepared by co-precipitation of Fe+2 and Fe+3 and myristic acid (C14) in basic medium. Vanilla essential oil loaded nanoparticles pelliculised on the catheter samples surface strongly inhibited both the initial adherence of S. aureus cells (quantified at 24 h) and the development of the mature biofilm quantified at 48 h. Patchouli and ylang-ylang essential oils inhibited mostly the initial adherence phase of S. aureus biofilm development. In the case of K. pneumoniae, all tested nanosystems exhibited similar efficiency, being active mostly against the adherence K. pneumoniae cells to the tested catheter specimens. The new nanobiosystems based on vanilla, patchouli and ylang-ylang essential oils could be of a great interest for the biomedical field, opening new directions for the design of film-coated surfaces with anti-adherence and anti-biofilm properties.
Keywords: magnetite, essential oil, adherence, anti-biofilm
1. Introduction
The surface of the biomaterials implanted in the human body is rapidly covered by a proteinaceous conditioning film predisposing to microbial colonization that could lead to biofilm associated infections, produced by a wide range of microorganisms, including Gram-positive cocci and Gram negative bacilli. The biofilm associated infections are characterized by slow onset, middle intensity symptoms, chronic evolution and resistance to antibiotic treatment [1]. In order to overcome this challenging problem, there is an increasing need for the development of new antibiofilm compounds and strategies.
One of the promising approaches to combat biofilms related infections is the coating of medical devices surface with anti-biofilm pellicles releasing antimicrobial agents, able to reduce microbial adhesion and biofilm development.
Plant essential oils are complex, volatile, natural compounds formed by aromatic plants as secondary metabolites [2], largely used against infections produced by bacteria, fungi, and viruses [3,4,5,6,7,8,9]. The antimicrobial activity was attributed to four classes of active compounds represented by terpenes, terpenoids, phenylpropenes, and “others”, that have been shown to act by damaging the cell wall and membrane, inhibition of protein synthesis, or interference with intermediary metabolisms or DNA/RNA synthesis/function and to not exhibit selective pressure for the occurrence of microbial resistance [10,11].
Originating from Indonesia, Malaysia, Philippines, Seychelles Islands, Madagascar, India, Brazil, Japan and China, patchouli (Pogostemon cablin syn. P. patchouli, P. heineanus) essential oils contain almost exclusively bi- and tricyclic sesquiterpenoids, such as 10%–16% α-guaiene, β-caryophyllene, δ-cadinene, pogostol, and respectively 25%–46% (‒)-patchoulol, 6%–11% seychellene, α- and β-patchoulene, α- and β-patchoulene oxide, α-cedrene, (+)-nor-patchoulenol, patchoulenone, isopatchoulenone, patchoulone, and only traces of monoterpenoid hydrocarbons (limonene, α- and β-pinene) are found [12]. Pathchouli essential oil (PEO) is primarily used in cosmetics. Due to its main active sesquiterpenoid compounds, PEO exhibited in vitro antibacterial effects against a wide range of bacteria such as Bacillus sp., Staphylococcus aureus, Streptococcus pyogenes, Proteus sp., Enterobacter aerogenes, Escherichia coli, Klebsiella pneumoniae, Pseudomonas aeruginosa, Salmonella typhi, Shigella dysenteriae [13].
Oleoresin from vanilla (Vanilla planifolia) fruits is obtained by extraction with volatile organic solvents (benzene, petroleum ether, methylene chloride, etc.). Benzene extraction yield is approx. 6%. For use in perfumery, vanilla absolute (or “essential oil”) (VEO) is extracted from oleoresin with ethanol (60%–70% yield). VEO contains mainly aromatic derivatives such as vanillin (85%–87%), 4-hydroxybenzaldehyde (6%–9%), vanillic acid (4%–5%), 4-hydroxybenzyl methyl ether, ethylvanillin, piperonal, methyl anisate [14]. VEO highlighted an inhibitory effect against the quorum-sensing genes expression of the Tn-5 mutant of Chromobacterium violaceum CV026, a soil-borne Gram-negative bacterium [15]. Also, by disc-diffusion technique, VEO demonstrated in vitro antibacterial properties against Enterobacter aerogenes, E. coli, Proteus vulgaris, P. aeruginosa, Streptococcus faecalis [16].
GC-MS analysis of essential oil from the fresh flowers of ylang-ylang (Cananga odorata subsp. genuina) revealed a complex composition consisting mainly of aromatic derivatives (1%–13% benzyl acetate, 5%–10% p-cresyl methyl ether, benzoic acid, cinamyl acetate, methyl benzoate, benzyl benzoate, benzyl salicylate, eugenol, trans-anethole), monoterpenoids (1%–9% linalool, geranyl acetate, geraniol, 1,8-cineole), prenyl derivatives (isoprenyl acetate, prenyl acetate), and sesquiterpenoids (17%–22% germacrene D, 8%–24% α-farnesene, 5%–35% β-caryophyllene, 2%–10% α-humulene) [17]. In vitro, ylang-ylang essential oil inhibited biofilm formed by E. coli ATCC 25922, S. aureus ATCC 6538, S. epidermidis clinical isolated strain and Candida albicans ATCC10231 [18,19].
Recently, magnetic nanoparticles have been reported to be efficient carriers and delivery systems for antibiotics and essential oils [20,21]. The magnetic nanoparticles and antibiotics delivery nanosystems have been shown to improve the therapeutic index of antimicrobial drugs and to diminish their local and systemic side effects [22].
Therefore, the purpose of this study was to combine the unique properties of magnetic nanoparticles with the antimicrobial activity of three essential oils to obtain novel nanobiosystems that could be pelliculised on the surface of catheter pieces exhibiting an improved resistance to microbial adherence and biofilm development by Staphylococcus aureus and Klebsiella pneumoniae clinical strains.
2. Results and Discussion
Iron oxide nanostructures have attracted a lot of attention in the last decade due to their various applications in the medical field [23,24]. Recently, different applications for antimicrobial therapy have been developed, such as anti-biofilm surfaces or drug delivery systems [25,26,27,28,29,30,31,32,33,34,35,36,37]. In this context, nanobiosystems based on iron oxide nanoparticles and essential oils have been prepared in order to create novel anti-adherent surfaces.
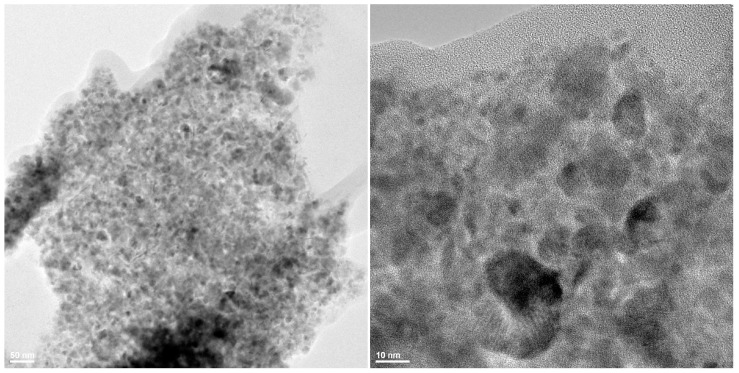
The obtained iron oxide nanoparticles functionalized with myristic acid (C14) have been characterized by TEM, XRD and TGA. TEM results are plotted in Figure 1. The images show that the prepared powder is in the nanometric range, the nanoparticles size is below 20 nm with a low tendency to create aggregates.
Figure 1.
TEM images of Fe3O4@C14 nanostructures.
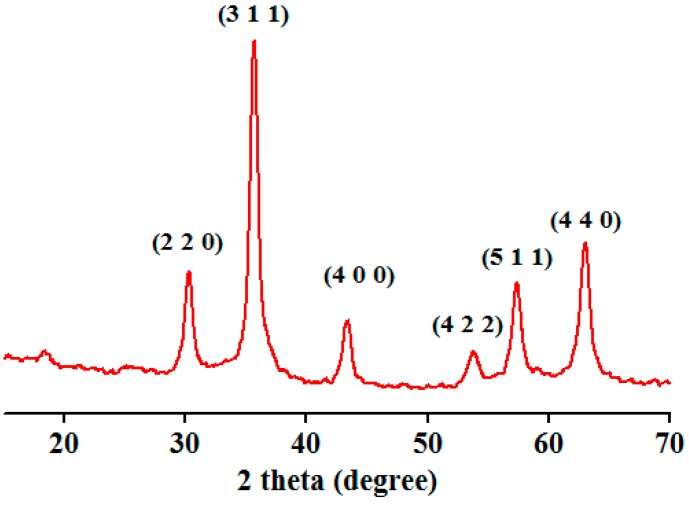
Figure 2 presents the XRD pattern of iron oxide nanostructures. Identified peaks can be assigned to magnetite nanoparticles [35,37]. From the XRD pattern it can be shown that the only crystalline phase presented in the prepared powder is magnetite.
Figure 2.
XRD pattern of Fe3O4@C14.
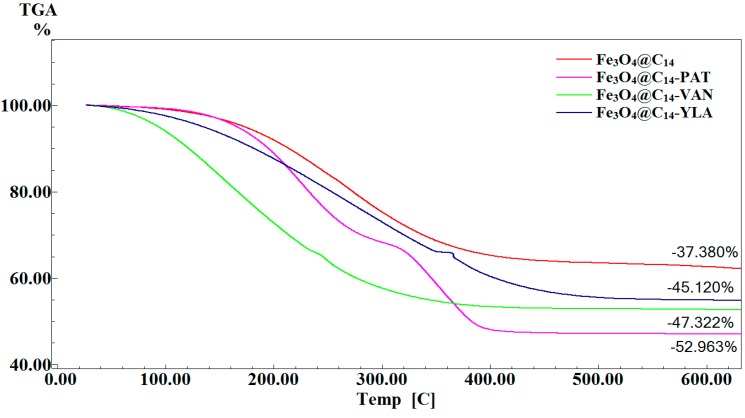
TG analysis (Figure 3) was used in order to estimate the amount of EOs immobilized on the surface of Fe3O4@C14. According to this analysis the amount of PAT, VAN and YLA estimated at 600 °C was 7.74%, 9.94% and 15.583%. The percent of EOs immobilized on the surface of magnetite nanoparticles is strictly dependent on the polarity of EOs.
Figure 3.
TG [C] analysis of Fe3O4@C14 and Fe3O4@C14-EOs.
Despite their frequent presence as commensal bacteria on the human skin and mucous surfaces, staphylococci are also the most frequent causes of biofilm-associated infections, especially in intensive care unit patients [38]. Klebsiella pneumoniae, an important opportunistic pathogen, causes persistent infections associated to biofilms formed on in-dwelling medical devices [39]. Recent studies revealed that numerous plant derived compounds and essential oils exhibit increased antimicrobial properties [40,41,42,43,44,45,46,47,48]. They are relatively easy to obtain, have low mammalian toxicity, and degrade quickly in water and soil, making them relatively environmentally friendly [49]. The development of bacterial resistance toward natural plant products has been thus far documented only in a very limited number of cases (e.g., for reserpine).
Some essential oils have been found to be more effective against biofilm embedded bacteria, probably due to the fact that: (i) the extracellular matrix of the biofilm adsorbs the active components and increases their local concentration; (ii) the cell membrane or cell wall in biofilm cells is different from that in planktonic cells due to differential gene expression in the two cell types [11].
However, the therapeutic effects of the essential oils can be impaired by their high volatility, highlighting the necessity of novel vectoring stabilizing systems [50]. Recent studies have shown that nanoparticles can be used for the delivery of essential oils and for the enhancement of their activity at the site of infection, thus surpassing some of the main drawbacks for conventional antimicrobial agents, which are the development of multiple drug resistance and adverse side effects [51]. During this study we have assessed the antimicrobial activities of three essential oils stabilized by magnetic nanoparticles. Ylang ylang oil has been previously shown to exhibit anti-S. aureus and anti-S. epidermidis activity, in combination with lavender oil and clary sage oil [18], patchouli essential oils have been proved to be active against Listeria monocytogenes, S. aureus biofilms and exhibited repellent properties [18,52,53,54,55], while vanillin, the main flavour component of vanilla showed bacteriostatic activity against Escherichia coli, Lactobacillus plantarum and Listeria innocua, acting primarily by the dissipation of ion gradients and the inhibition of respiration [56].
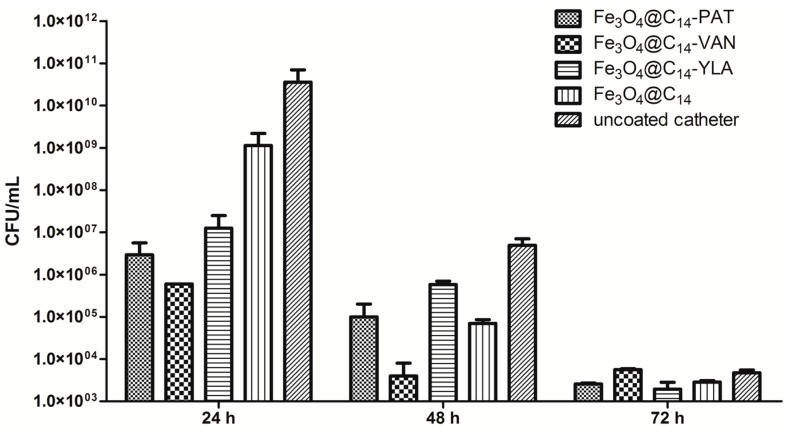
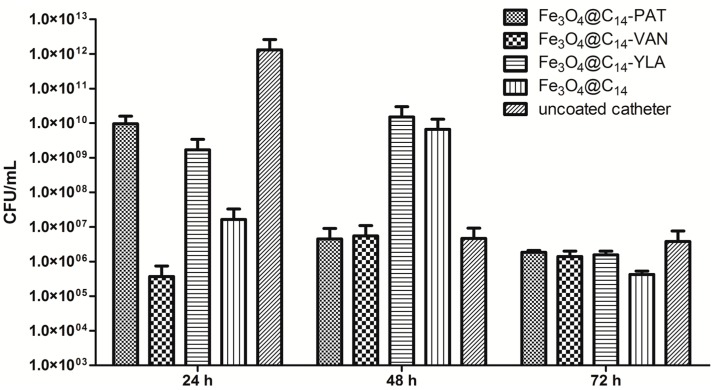
In our study, the observed dynamics of S. aureus and K. pneumoniae biofilms presented a similar growth peak at 24 h, followed by a gradual decrease of bacterial density at 48 h and 72 h (Figure 4 and Figure 5).
Figure 4.
Number of S. aureus viable cells recovered from the biofilms developed on the catheter specimens coated with different essential oils containing nanosystems and on the uncoated catheters tested after 24, 48 and 72 h. Each column represents the average (Av) values of three replicates.
Figure 5.
Number of K. pneumoniae viable cells recovered from the biofilms developed on the catheter specimens coated with different essential oils containing nanosystems and on the uncoated catheters tested after 24, 48 and 72 h. Each column represents the average (Av) values of three replicates.
However, it is to be noticed that the number of K. pneumoniae adhered cells quantified after 24 h has been >one log higher than in case of S. aureus.
The vanilla essential oil coated nanoparticles strongly inhibited both the initial adherence of S. aureus to the coated catheter surface (quantified at 24 h) and the development of the mature biofilm quantified at 48 h (Figure 4).
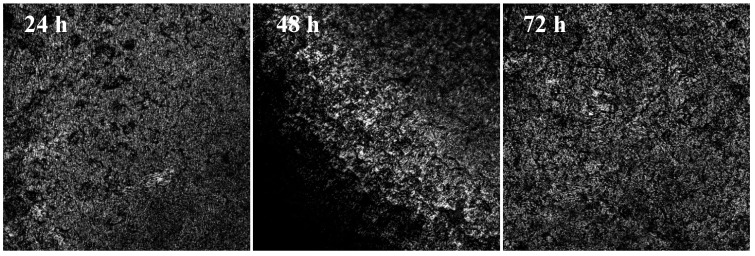
A direct correlation between the viable cell counts and CLSM results was observed. CLSM was used to obtain qualitative images on the distribution of the microbial biofilm on the coated catheteter surfaces vs. the uncoated ones. For example, in case of S. aureus biofilms developed on the catheter specimens coated with Fe3O4@C14-VAN, the CLSM images revealed that the biofilms examined at 24 h and 72 h were better represented than that developed at 48 h and more homogenously distributed on the coated surface (Figure 6).
Figure 6.
CLSM images of S. aureus biofilm developed on Fe3O4@C14-VAN coated substrata at 24 h, 48 h and 72 h; bacteria occur as punctiform, round cells distributed on the coated surface.
The inhibitory effect of the vanilla essential oil loaded nanostructure can be interpreted as significant in accordance with US Pharmacopeia criteria for antimicrobial effectiveness [57], the number of the adherent cells being decreased by more than three/five logs at 24 h and by more than two/three logs at 48 h in comparison with the biofilm embedded cells developed on the catheter samples coated only with the magnetite nanostructures and respectively, on the uncoated catheter. Taking into account that the initial number of the bacterial cells added in the system was 1 × 108–3 × 108 CFU/mL, and the number of the attached bacteria is decreasing over time under the initial value we could state that the vanilla essential oil induced a bactericidal effect and a detachment of the bacterial cells from the biofilm.
The patchouli and ylang-ylang essential oils significantly inhibited the initial adherence phase of S. aureus biofilm development (Figure 4), the number of viable cells being decreased by at least two logs, in comparison with the biofilm developed on the catheter samples coated only with the magnetite nanostructures while at 48 h, the inhibitory effect was less evident, a biofilm inhibition of more than one log being noticed only in comparison with the uncoated catheter.
The tested oils did not exhibit any significant influence on the viability of bacterial cells embedded in biofilms after 72 h. These results demonstrate that the tested oils exhibit a bactericidal effect as long as they are released from the iron based nanocarrier which remains attached to the catheter surface. Thus, after the active compounds are consumed, the remaining viable cells are rebuilding the biofilm.
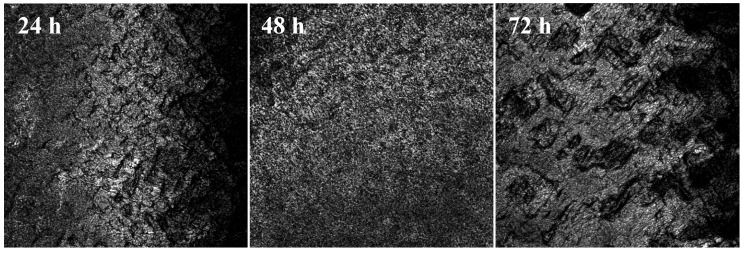
In case of K. pneumoniae biofilms, vanilla oil containing nanostructure proved to be the most potent inhibitor of the initial adherence of K. pneumoniae to the coated catheter specimens (the number of viable cells being decreased by five logs as compared to the uncoated control) (Figure 5), while patchouli and ylang-ylang oils exhibited a lower inhibition of the initial phase of biofilm development (the inhibitory effect being of two to three logs as compared to the uncoated control). However, similar to S. aureus biofilm, the effect seems to be more probably due to the bactericidal effect exhibited by the active compounds released from the coating rather than to the detachment of the adhered cells from the surface (Figure 7).
Figure 7.
CLSM images of K. pneumonia biofilm developed on Fe3O4@C14-VAN coated substrata at 24 h, 48 h and 72 h; bacteria occur as punctiform, round cells distributed on the coated surface.
No significant inhibition of the mature biofilm development quantified at 48 h and 72 h has been observed in the presence of any of the three tested essential oils, the active compounds released from the pellicle being probably more rapidly consumed in their interaction with K. pneumoniae biofilm cells, more dense at 24 h (>1012 CFU/mL) as compared to S. aureus one (<1010 CFU/mL).
3. Experimental Section
3.1. Preparation of Iron Oxide@C14 Nanoparticles
Iron oxide@C14 nanoparticles were prepared according to our previously published papers [58]. Briefly, functionalized iron oxide nanoparticles were prepared by co-precipitation of Fe+2 and Fe3+ in basic aqueous dispersion of C14 (myristic acid).
3.2. Surface Modification of Catheter Pieces with Essential Oils Stabilized by Iron Oxide@C14 Nanoparticles
Surface modification of catheter pieces was performed according to our previously published papers [21,59]. Firstly, the 100 mg of iron oxide@C14 nanoparticles and 100 μL of essential oils (EOs) were dispersed in chloroform and mixed until complete evaporation of chloroform was achieved. This step was repeated for uniform loading of EOs on the surface of iron oxide@C14 nanoparticles. After 7 days prepared Fe3O4@C14-EOs were analyzed by TGA to estimate the amount of EOs immobilized on the surface of Fe3O4@C14. Secondly, after 7 days of drying at ambient temperature the layer of Fe3O4@C14-EOs on the catheter pieces was achieved by submerging the pieces in 10 mL of Fe3O4@C14-EOs fluid (Fe3O4@C14-EOs:CHCl3 = 1 mg/mL) and then the catheter pieces have been extemporaneously dried at room temperature. The rapid drying was facilitated by the convenient volatility of chloroform. The modified specimens were sterilized by ultraviolet irradiation for 20 min [51].
3.3. Characterization
3.3.1. TEM
The transmission electron microscopy (TEM) images were obtained on finely powdered samples using a TecnaiTM G2 F30 S-TWIN high resolution transmission electron microscope from FEI Company (Hillsboro, OR, USA). The microscope was operated in transmission mode at 300 kV with TEM point resolution of 2 Å and line resolution of 1 Å. The fine powder was dispersed into pure ethanol and ultrasonicated for 15 min. After that, diluted sample was put onto a holey carbon-coated copper grid and left to dry before TEM analysis.
3.3.2. XRD
X-ray diffraction analysis was performed on a XRD 6000 diffractometer (Shimadzu, Kyoto, Japan) at room temperature. In all the cases, Cu Kα radiation (λ = 1.5406 Å at 15 mA and 30 kV) was used. The samples were scanned in the Bragg angle 2θ range of 10–80 degree.
3.3.3. TGA
The thermogravimetric (TG) analysis of the Fe3O4@C14 and Fe3O4@C14-EOs was followed with a TG 449C STA Jupiter instrument (Netzsch, Selb, Germany). Samples were screened with 200 mesh prior to analysis, placed in an alumina crucible, and heated at 10 K·min−1 from room temperature to 800 °C, under the flow of 20 mL·min−1 of dried synthetic air (80% N2 and 20% O2).
3.4. Microbial Biofilms Assay
The microbial adherence ability and biofilm development on the functionalized surfaces have been investigated by a culture-based method, using Gram positive (Staphylococcus aureus 246) and Gram-negative (Klebsiella pneumoniae 11) bacterial clinical strains. These strains have been identified using the automatic VITEK II identification system. The specimens of equal area have been distributed in the multi-well plastic plates, and submitted to UV sterilization for 20 min. Thereafter, the liquid culture medium (nutrient broth) was added over the slide specimens. Two wells were inoculated with a microbial inoculum with a density corresponding to 0.5 MacFarland density (1 × 108–3 × 108 CFU/mL) prepared in sterile saline. The obtained microbial strain: culture medium: specimen system was incubated at 37 °C for 24 h, in order to allow microbial strains to multiply and adhere to the samples distributed in each well. The colonized specimen was washed in order to remove the nonadherent bacteria, moved in fresh culture medium and further incubated at 37 °C. After 24 h, 48 h and 72 h, respectively, the specimens were extracted from the culture medium, washed three times in sterile saline, in order to remove the non-adherent bacteria. Ten-fold dilutions were performed from the cultures recovered after the multiplication of microbial cells adhered to the tested substrata in order to count the Colony Forming Units (CFU) and to assess the viable cell counts (VCCs) of the respective cultures. To this purpose, the adhered cells have been removed from samples by vortexing and brief sonication. Serial dilutions ranging from 10−1 to 10−30 of the obtained inocula have been spotted on Muller-Hinton agar, incubated for 24 h at 37 °C and assessed for VCCs. An amount of 5 µL of the chosen dilution was spotted in triplicates on the solid medium. The resulting colonies have been numbered and the average value was submitted to dilution and volume correction. The final value was expressed in CFU/mL. We could assess this way the influence of different tested substrata on the adherence and the dynamics of microbial biofilm development by the selected microbial strains. All experiments were performed on different occasions using three biological replicates. The qualitative examination of biofilm development on the coated catheter surfaces was assessed by CLSM. For our experiments we have used a TCS SP confocal laser scanning microscope (Leica, Wetzlar, Germany) equipped with a He-Ne laser (633 nm) and a PL FLUOTAR40X, NA 0.75 objective. In order to evaluate the biofilm development on the coated vs. control, uncoated catheter surfaces, we have acquired reflection images from each sample surface. No staining of the bacteria was used.
4. Conclusions
The catheter colonization capacity of S. aureus and K. pneumoniae strains, particularly in the initial adherence phase (in case of all three essential oils), but also the development of the mature biofilm (in case of vanilla essential oil) were strongly inhibited by the essential oil-containing nanostructures, suggesting the potential of the obtained nanophytosystems for the design of coatings resistant to microbial colonization with different applications in medicine, food and pharmaceutical industry.
Acknowledgments
This research was financially supported by Sectoral Operational Programme Human Resources Development, financed from the European Social Fund and by the Romanian Government under the contract number POSDRU/156/1.2/G/135764 “Improvement and implementation of universitary master programs in the field of Applied Chemistry and Materials Science-ChimMaster”.
Author Contributions
M.B. performed the microbiological assays, A.M.G., A.E.O., R.C.P. and G.D.M. obtained and characterized the nanosystems, A.M.G., D.F.M and E.B. designed the study, read and approved the manuscript. A.M.G. and M.C.C. drafted the manuscript. R.H. investigated the samples by confocal laser scanning microscopy and G.A.S. and V.L. advised on the sample characterization, read and approved the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Sample Availability: Samples of the nanostructures are available from the authors.
References
- 1.Lazar V. Quorum sensing in biofilms—How to destroy the bacterial citadels or their cohesion/power? Anaerobe. 2001;17:280–285. doi: 10.1016/j.anaerobe.2011.03.023. [DOI] [PubMed] [Google Scholar]
- 2.Bakkali F., Averbeck S., Averbeck D., Waomar M. Biological effects of essential oils—A review. Food Chem. Toxicol. 2008;46:446–475. doi: 10.1016/j.fct.2007.09.106. [DOI] [PubMed] [Google Scholar]
- 3.Hammer K.A., Carson C.F., Riley T.V. Antimicrobial activity of essential oils and other plant extracts. J. Appl. Microbiol. 1999;86:985–990. doi: 10.1046/j.1365-2672.1999.00780.x. [DOI] [PubMed] [Google Scholar]
- 4.Deans S.G., Ritchie G. Antibacterial Properties of Plant Essential Oils. Int. J. Food Microbiol. 1987;5:165–180. [Google Scholar]
- 5.George D.R., Smith T.J., Shiel R.S., Sparagano O.A.E., Guy J.H. Mode of action and variability in efficacy of plant essential oils showing toxicity against the poultry red mite, Dermanyssus gallinae. Vet. Parasitol. 2009;161:276–282. doi: 10.1016/j.vetpar.2009.01.010. [DOI] [PubMed] [Google Scholar]
- 6.Oussalah M., Caillet S., Saucier L., Lacroix M. Inhibitory effects of selected plant essential oils on the growth of four pathogenic bacteria: E-coli O157:H7, Salmonella Typhimurium, Staphylococcus aureus and Listeria monocytogenes. Food Control. 2007;18:414–420. [Google Scholar]
- 7.Astani A., Reichling J., Schnitzler P. Screening for antiviral activities of isolated compounds from essential oils. Evid.-Based Complement. Altern. Med. 2011;2011 doi: 10.1093/ecam/nep187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Silva F., Ferreira S., Duarte A., Mendonca D.I., Domingues F.C. Antifungal activity of Coriandrum sativum essential oil, its mode of action against Candida species and potential synergism with amphotericin B. Phytomedicine. 2011;19:42–47. doi: 10.1016/j.phymed.2011.06.033. [DOI] [PubMed] [Google Scholar]
- 9.Tserennadmid R., Tako M., Galgoczy L., Papp T., Pesti M., Vagvolgyi C., Almassy K., Krisch J. Anti yeast activities of some essential oils in growth medium, fruit juices and milk. Int. J. Food Microbiol. 2011;144:480–486. doi: 10.1016/j.ijfoodmicro.2010.11.004. [DOI] [PubMed] [Google Scholar]
- 10.Burt S. Essential oils: Their antibacterial properties and potential applications in foods—A review. Int. J. Food Microbiol. 2004;94:223–253. doi: 10.1016/j.ijfoodmicro.2004.03.022. [DOI] [PubMed] [Google Scholar]
- 11.Kavanaugh N.L., Ribbeck K. Selected Antimicrobial Essential Oils Eradicate Pseudomonas spp. and Staphylococcus aureus Biofilms. Appl. Environ. Microbiol. 2012;78:4057–4061. doi: 10.1128/AEM.07499-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hussin N., Mondello L., Costa R., Dugo P., Yusoff N.I.N., Yarmo M.A., Ab Wahab A., Said M. Quantitative and Physical Evaluation of Patchouli Essential Oils Obtained from Different Sources of Pogostemon cablin. Nat. Prod. Commun. 2012;7:927–930. [PubMed] [Google Scholar]
- 13.Yang X., Zhang X., Yang S.P., Liu W.Q. Evaluation of the Antibacterial Activity of Patchouli Oil. Iran. J. Pharm. Res. 2013;12:307–316. [PMC free article] [PubMed] [Google Scholar]
- 14.Takahashi M., Inai Y., Miyazawa N., Kurobayashi Y., Fujita A. Identification of the Key Odorants in Tahitian Cured Vanilla Beans (Vanilla tahitensis) by GC-MS and an Aroma Extract Dilution Analysis. Biosci. Biotechnol. Biochem. 2013;77:601–605. doi: 10.1271/bbb.120840. [DOI] [PubMed] [Google Scholar]
- 15.Choo J.H., Rukayadi Y., Hwang J.K. Inhibition of bacterial quorum sensing by vanilla extract. Lett. Appl. Microbiol. 2006;42:637–641. doi: 10.1111/j.1472-765X.2006.01928.x. [DOI] [PubMed] [Google Scholar]
- 16.Subramanian S., Banu H.H., Bai R.M.R., Shanmugavalli R. Biochemical evaluation of antihyperglycemic and antioxidant nature of Psidium guajava leaves extract in streptozotocin-induced experimental diabetes in rats. Pharm. Biol. 2009;47:298–303. [Google Scholar]
- 17.Brokl M., Fauconnier M.L., Benini C., Lognay G., du Jardin P., Focant J.F. Improvement of Ylang-Ylang Essential Oil Characterization by GCxGC-TOFMS. Molecules. 2013;18:1783–1797. doi: 10.3390/molecules18021783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tadtong S., Suppawat S., Tintawee A., Saramas P., Jareonvong S., Hongratanaworakit T. Antimicrobial Activity of Blended Essential Oil Preparation. Nat. Prod. Commun. 2012;7:1401–1404. [PubMed] [Google Scholar]
- 19.Lee K., Lim E.J., Kim K.S., Huang S.L., Veeranagouda Y., Rehm B.H.A. An alginate-like exopolysaccharide biosynthesis gene cluster involved in biofilm aerial structure formation by Pseudomonas alkylphenolia. Appl. Microbiol. Biotechnol. 2014;98:4137–4148. doi: 10.1007/s00253-014-5529-6. [DOI] [PubMed] [Google Scholar]
- 20.Chifiriuc C., Grumezescu V., Grumezescu A.M., Saviuc C., Lazar V., Andronescu E. Hybrid magnetite nanoparticles/Rosmarinus officinalis essential oil nanobiosystem with antibiofilm activity. Nanoscale Res. Lett. 2012;7:1–7. doi: 10.1186/1556-276X-7-209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Grumezescu A.M., Saviuc C., Chifiriuc M.C., Hristu R., Mihaiescu D.E., Balaure P., Stanciu G., Lazar V. Inhibitory Activity of Fe3O4/Oleic Acid/Usnic Acid-Core/Shell/Extra-Shell Nanofluid on S. aureus Biofilm Development. IEEE Trans. Nanobiosci. 2011;10:269–274. doi: 10.1109/TNB.2011.2178263. [DOI] [PubMed] [Google Scholar]
- 22.Zhang L., Pornpattananangkul D., Hu C.M.J., Huang C.M. Development of Nanoparticles for Antimicrobial Drug Delivery. Curr. Med. Chem. 2010;17:585–594. doi: 10.2174/092986710790416290. [DOI] [PubMed] [Google Scholar]
- 23.Schleich N., Sibret P., Danhier P., Ucakar B., Laurent S., Muller R.N., Jerome C., Gallez B., Preat V., Danhier F. Dual anticancer drug/superparamagnetic iron oxide-loaded PLGA-based nanoparticles for cancer therapy and magnetic resonance imaging. Int. J. Pharm. 2013;447:94–101. doi: 10.1016/j.ijpharm.2013.02.042. [DOI] [PubMed] [Google Scholar]
- 24.Philosof-Mazor L., Dakwar G.R., Popov M., Kolusheva S., Shames A., Linder C., Greenberg S., Heldman E., Stepensky D., Jelinek R. Bolaamphiphilic vesicles encapsulating iron oxide nanoparticles: New vehicles for magnetically targeted drug delivery. Int. J. Pharm. 2013;450:241–249. doi: 10.1016/j.ijpharm.2013.04.017. [DOI] [PubMed] [Google Scholar]
- 25.Wang C.H., Qiao L., Zhang Q., Yan H.S., Liu K.L. Enhanced cell uptake of superparamagnetic iron oxide nanoparticles through direct chemisorption of FITC-Tat-PEG(600)-b-poly(glycerol monoacrylate) Int. J. Pharm. 2012;430:372–380. doi: 10.1016/j.ijpharm.2012.04.035. [DOI] [PubMed] [Google Scholar]
- 26.Meenach S.A., Otu C.G., Anderson K.W., Hilt J.Z. Controlled synergistic delivery of paclitaxel and heat from poly(beta-amino ester)/iron oxide-based hydrogel nanocomposites. Int. J. Pharm. 2012;427:177–184. doi: 10.1016/j.ijpharm.2012.01.052. [DOI] [PubMed] [Google Scholar]
- 27.Masoudi A., Hosseini H.R.M., Shokrgozar M.A., Ahmadi R., Oghabian M.A. The effect of poly(ethylene glycol) coating on colloidal stability of superparamagnetic iron oxide nanoparticles as potential MRI contrast agent. Int. J. Pharm. 2012;433:129–141. doi: 10.1016/j.ijpharm.2012.04.080. [DOI] [PubMed] [Google Scholar]
- 28.Lee E.S., Lim C., Song H.T., Yun J.M., Lee K.S., Lee B.J., Youn Y.S., Oh Y.T., Oh K.T. A nanosized delivery system of superparamagnetic iron oxide for tumor MR imaging. Int. J. Pharm. 2012;439:342–348. doi: 10.1016/j.ijpharm.2012.08.054. [DOI] [PubMed] [Google Scholar]
- 29.Jansch M., Stumpf P., Graf C., Ruhl E., Muller R.H. Adsorption kinetics of plasma proteins on ultrasmall superparamagnetic iron oxide (USPIO) nanoparticles. Int. J. Pharm. 2012;428:125–133. doi: 10.1016/j.ijpharm.2012.01.060. [DOI] [PubMed] [Google Scholar]
- 30.Chen X.L., Lv H.Y., Ye M., Wang S.Y., Ni E.R., Zeng F.W., Cao C., Luo F.H., Yan J.H. Novel superparamagnetic iron oxide nanoparticles for tumor embolization application: Preparation, characterization and double targeting. Int. J. Pharm. 2012;426:248–255. doi: 10.1016/j.ijpharm.2012.01.043. [DOI] [PubMed] [Google Scholar]
- 31.Mihaiescu D.E., Grumezescu A.M., Andronescu E., Voicu G., Ficai A., Vasile O.R., Bleotu C., Saviuc C. Prosthetic Devices with Functionalized Anti-biofilm Surface Based NanoAg@C18. Curr. Org. Chem. 2013;17:105–112. [Google Scholar]
- 32.Mihaiescu D.E., Cristescu R., Dorcioman G., Popescu C.E., Nita C., Socol G., Mihailescu I.N., Grumezescu A.M., Tamas D., Enculescu M., et al. Functionalized magnetite silica thin films fabricated by MAPLE with antibiofilm properties. Biofabrication. 2013;5 doi: 10.1088/1758-5082/5/1/015007. [DOI] [PubMed] [Google Scholar]
- 33.Holban A.M., Grumezescu A.M., Ficai A., Chifiriuc C.M., Lazar V., Radulescu R. Fe3O4@C-18-carvone to prevent Candida tropicalis biofilm development. Rev. Rom. Mater. 2013;43:300–305. [Google Scholar]
- 34.Holban A.M., Grumezescu A.M., Andronescu E., Grumezescu V., Chifiriuc C.M., Radulescu R. Magnetite—Usnic Acid Nanostructured Bioactive Material with Antimicrobial Activity. Rev. Rom. Mater. 2013;43:402–407. [Google Scholar]
- 35.Grumezescu A.M., Cotar A.I., Andronescu E., Ficai A., Ghitulica C.D., Grumezescu V., Vasile B.S., Chifiriuc M.C. In vitro activity of the new water-dispersible Fe3O4@usnic acid nanostructure against planktonic and sessile bacterial cells. J. Nanopart. Res. 2013;15 doi: 10.1007/s11051-013-1766-3. [DOI] [Google Scholar]
- 36.Grumezescu A.M., Andronescu E., Holban A.M., Ficai A., Ficai D., Voicu G., Grumezescu V., Balaure P.C., Chifiriuc C.M. Water dispersible cross-linked magnetic chitosan beads for increasing the antimicrobial efficiency of aminoglycoside antibiotics. Int. J. Pharm. 2013;454:233–240. doi: 10.1016/j.ijpharm.2013.06.054. [DOI] [PubMed] [Google Scholar]
- 37.Chifiriuc M.C., Grumezescu A.M., Andronescu E., Ficai A., Cotar A.I., Grumezescu V., Bezirtzoglou E., Lazar V., Radulescu R. Water dispersible magnetite nanoparticles influence the efficacy of antibiotics against planktonic and biofilm embedded Enterococcus faecalis cells. Anaerobe. 2013;22:14–19. doi: 10.1016/j.anaerobe.2013.04.013. [DOI] [PubMed] [Google Scholar]
- 38.Otto M. Staphylococcal biofilms. Curr. Top. Microbiol. 2008;322:207–228. doi: 10.1007/978-3-540-75418-3_10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Magesh H., Kumar A., Alam A., Priyam , Sekar U., Sumantran V.N., Vaidyanathan R. Identification of natural compounds which inhibit biofilm formation in clinical isolates of Klebsiella pneumoniae. Indian J. Exp. Biol. 2013;51:764–772. [PubMed] [Google Scholar]
- 40.Coenye T., Brackman G., Rigole P., de Witte E., Honraet K., Rossel B., Nelis H.J. Eradication of Propionibacterium acnes biofilms by plant extracts and putative identification of icariin, resveratrol and salidroside as active compounds. Phytomedicine. 2012;19:409–412. doi: 10.1016/j.phymed.2011.10.005. [DOI] [PubMed] [Google Scholar]
- 41.Ravichandiran V., Shanmugam K., Anupama K., Thomas S., Princy A. Structure-based virtual screening for plant-derived SdiA-selective ligands as potential antivirulent agents against uropathogenic Escherichia coli. Eur. J. Med. Chem. 2012;48:200–205. doi: 10.1016/j.ejmech.2011.12.015. [DOI] [PubMed] [Google Scholar]
- 42.Abraham S.V.P.I., Palani A., Ramaswamy B.R., Shunmugiah K.P., Arumugam V.R. Antiquorum Sensing and Antibiofilm Potential of Capparis spinosa. Arch. Med. Res. 2011;42:658–668. doi: 10.1016/j.arcmed.2011.12.002. [DOI] [PubMed] [Google Scholar]
- 43.Singh B.N., Singh H.B., Singh A., Singh B.R., Mishra A., Nautiyal C.S. Lagerstroemia speciosa fruit extract modulates quorum sensing-controlled virulence factor production and biofilm formation in Pseudomonas aeruginosa. Microbiology. 2012;158:529–538. doi: 10.1099/mic.0.052985-0. [DOI] [PubMed] [Google Scholar]
- 44.Harjai K., Kumar R., Singh S. Garlic blocks quorum sensing and attenuates the virulence of Pseudomonas aeruginosa. FEMS Immunol. Med. Microbiol. 2010;58:161–168. doi: 10.1111/j.1574-695X.2009.00614.x. [DOI] [PubMed] [Google Scholar]
- 45.Trentin D.D., Giordani R.B., Zimmer K.R., da Silva A.G., da Silva M.V., Correia M.T.D., Baumvol I.J.R., Macedo A.J. Potential of medicinal plants from the Brazilian semi-arid region (Caatinga) against Staphylococcus epidermidis planktonic and biofilm lifestyles. J. Ethnopharmacol. 2011;137:327–335. doi: 10.1016/j.jep.2011.05.030. [DOI] [PubMed] [Google Scholar]
- 46.Carneiro V.A., dos Santos H.S., Arruda F.V.S., Bandeira P.N., Albuquerque M.R.J.R., Pereira M.O., Henriques M., Cavada B.S., Teixeira E.H. Casbane Diterpene as a Promising Natural Antimicrobial Agent against Biofilm-Associated Infections. Molecules. 2011;16:190–201. doi: 10.3390/molecules16010190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Brackman G., Cos P., Maes L., Nelis H.J., Coenye T. Quorum Sensing Inhibitors Increase the Susceptibility of Bacterial Biofilms to Antibiotics in Vitro and in Vivo. Antimicrob. Agents Chemother. 2011;55:2655–2661. doi: 10.1128/AAC.00045-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Jakobsen T.H., van Gennip M., Phipps R.K., Shanmugham M.S., Christensen L.D., Alhede M., Skindersoe M.E., Rasmussen T.B., Friedrich K., Uthe F., et al. Ajoene, a Sulfur-Rich Molecule from Garlic, Inhibits Genes Controlled by Quorum Sensing. Antimicrob. Agents Chemother. 2012;56:2314–2325. doi: 10.1128/AAC.05919-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Isman M.B. Plant essential oils for pest and disease management. Crop. Prot. 2000;19:603–608. [Google Scholar]
- 50.Anghel I., Holban A.M., Andronescu E., Grumezescu A.M., Chifiriuc M.C. Efficient surface functionalization of wound dressings by a phytoactive nanocoating refractory to Candida albicans biofilm development. Biointerphases. 2013;8 doi: 10.1186/1559-4106-8-12. [DOI] [PubMed] [Google Scholar]
- 51.Anghel I., Grumezescu A.M., Holban A.M., Ficai A., Anghel A.G., Chifiriuc M.C. Biohybrid Nanostructured Iron Oxide Nanoparticles and Satureja hortensis to Prevent Fungal Biofilm Development. Int. J. Mol. Sci. 2013;14:18110–18123. doi: 10.3390/ijms140918110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Vázquez-Sánchez D., Cabo M.L., Rodríguez-Herrera J.J. Antimicrobial Activity of Essential Oils against Staphylococcus Aureus Biofilms. Food Sci. Technol. Int. 2014. [(accessed on 28 October 2014)]. in press. Available online: http://www.ncbi.nlm.nih.gov/pubmed/25280938. [DOI] [PubMed]
- 53.Wu H.Q., Li L., Li J., He Z.D., Liu Z.G., Zeng Q.Q., Wang Y.S. Acaricidal Activity of DHEMH, Derived from Patchouli Oil, against House Dust Mite, Dermatophagoides farinae. Chem. Pharm. Bull. 2012;60:178–182. doi: 10.1248/cpb.60.178. [DOI] [PubMed] [Google Scholar]
- 54.Nielsen P.V., Rios R. Inhibition of fungal growth on bread by volatile components from spices and herbs, and the possible application in active packaging, with special emphasis on mustard essential oil. Int. J. Food Microbiol. 2000;60:219–229. doi: 10.1016/s0168-1605(00)00343-3. [DOI] [PubMed] [Google Scholar]
- 55.Shin S. Anti-Aspergillus activities of plant essential oils and their combination effects with ketoconazole or amphotericin B. Arch. Pharm. Res. 2003;26:389–393. doi: 10.1007/BF02976696. [DOI] [PubMed] [Google Scholar]
- 56.Fitzgerald D.J., Stratford M., Gasson M.J., Ueckert J., Bos A., Narbad A. Mode of antimicrobial action of vanillin against Escherichia coli, Lactobacillus plantarum and Listeria innocua. J. Appl. Microbiol. 2004;97:104–113. doi: 10.1111/j.1365-2672.2004.02275.x. [DOI] [PubMed] [Google Scholar]
- 57.U.S. Pharmacopeia. [(accessed on 2 November 2014)]. Available online: http://www.pharmacopeia.cn/v29240/usp29nf24s0_c51.
- 58.Voicu G., Andronescu E., Grumezescu A.M., Huang K.S., Ficai A., Yang C.H., Bleotu C., Chifiriuc M.C. Antitumor Activity of Magnetite Nanoparticles: Influence of Hydrocarbonated Chain of Saturated Aliphatic Monocarboxylic Acids. Curr. Org. Chem. 2013;17:831–840. [Google Scholar]
- 59.Grumezescu A.M., Chifiriuc M.C., Saviuc C., Grumezescu V., Hristu R., Mihaiescu D.E., Stanciu G.A., Andronescu E. Hybrid Nanomaterial for Stabilizing the Antibiofilm Activity of Eugenia carryophyllata Essential Oil. IEEE Trans. Nanobiosci. 2012;11:360–365. doi: 10.1109/TNB.2012.2208474. [DOI] [PubMed] [Google Scholar]