Abstract
An update to the 2007 American College of Veterinary Internal Medicine (ACVIM) consensus statement on the identification, evaluation, and management of systemic hypertension in dogs and cats was presented at the 2017 ACVIM Forum in National Harbor, MD. The updated consensus statement is presented here. The consensus statement aims to provide guidance on appropriate diagnosis and treatment of hypertension in dogs and cats.
Keywords: blood pressure, cardiology, cardiovascular, chronic renal failure, hemodynamics, hypertension, kidney, proteinuria, renal/urinary tract
Abbreviations
- ACEi
angiotensin converting enzyme inhibitor
- ARB
angiotensin II receptor blockers
- BP
blood pressure
- CCB
calcium channel blockers
- CKD
chronic kidney disease
- GFR
glomerular filtration rate
- LVH
left ventricular hypertrophy
- RAAS
renin‐angiotensin‐aldosterone system
- SBP
systolic blood pressure
- SDMA
symmetric dimethylarginine
- TOD
target organ damage
- UPC
urine protein to creatinine ratio
- MRI
magnetic resonance imaging
- IRIS
International Renal Interest Society
- CNS
central nervous system
- CRI
constant rate infusion
1. INTRODUCTION
In 2000, a group of experts was convened to develop comprehensive guidelines for the identification and treatment of systemic hypertension in cats and dogs. In 2007, the recommendations of this expert panel were published as the American College of Veterinary Internal Medicine (ACVIM) consensus statement on hypertension. Over the past 10 years, our understanding of normal systemic arterial blood pressure (BP) and systemic hypertension has expanded, but much remains to be discovered. It is our hope that these revised guidelines, based on the latest available research, will assist practitioners in the development of a rational approach to the diagnosis and treatment of hypertension in companion animals.
2. BP MEASUREMENT
Diagnosing and treating hypertension in the clinical patient necessitate accurate measurement of the patient's BP. Direct BP determination entails catheterization of a suitable artery and assessing arterial pressure using an electronic transducer.1, 2, 3 Although this is the gold standard, it is not practical for hypertension screening and treatment. Clinically, noninvasive indirect estimations of BP such as Doppler and oscillometric devices are commonly used.4, 5, 6
Ideally, BP should be measured using devices that have been validated in the species of interest and under the circumstances in which the patient is being tested. Standards for the validation of indirect BP measuring devices in people are well established,7 but no device has met these criteria in conscious dogs or cats. For this reason, a set of standards for validating indirect BP devices in awake dogs and cats has been proposed and accepted.8 Although many studies have attempted to validate indirect BP devices in anesthetized patients, only a few have been performed in conscious animals.9, 10, 11, 12 In the devices studied to date in awake animals, either a different validation standard was used9, 11, 12 or the device failed to meet the previously established criteria.10
Until devices that can meet the guidelines for measuring BP in conscious animals have been validated, it is our recommendation that currently available devices be used with a degree of caution. Because estimates of BP obtained using an indirect device can only be interpreted in light of results of appropriate validation testing in conscious animals, devices that have not been subjected to appropriate testing in conscious animals should not be used. Nonetheless, studies that have relied upon indirect estimation of BP using available devices have identified adverse effects of increased BP and benefits of intervention, indicating that some of these devices can provide clinically useful information.13, 14 Therefore, we recommend that, once commercially available, only devices that meet the established validation standards in conscious cats and dogs be used.
To obtain reliable results in the measurement of BP, it is important to follow a standard protocol (Table 1). The individual taking the measurements should be skilled and experienced in the handling of animals and the equipment. Studies have shown that operator experience can have a significant impact on BP measurements.1, 15 Often the most skilled individual is a well‐trained technician and not a veterinarian. Anxiety‐ or excitement‐induced situational hypertension can be marked,16, 17 but can be minimized by measuring BP in a quiet area, away from other animals, before other procedures and only after the patients have been acclimated to their surroundings for 5‐10 minutes. Whenever possible, the owner should be present and restraint should be kept to a minimum. The selection of a correctly sized cuff is critical in obtaining accurate measurements.1 Some veterinary‐specific oscillometric devices have specially designed cuffs and these should always be used. When using Doppler and many oscillometric units, the width of the cuff should be 30%‐40% of the circumference of the extremity at the site of cuff placement. The first measurement should be discarded and the average of 5‐7 consecutive consistent indirect measurements should be obtained. If there is substantial variation, the readings should be discarded and the process repeated. In some patients, BP trends downward as the measurement process continues. In these animals, measurements should continue until a plateau is reached and then 5‐7 consecutive consistent values should be recorded. Conversely in some patients, measurement of systolic blood pressure (SBP) may result in a progressive increase in readings. When this occurs, results must be interpreted in the clinical context of the individual patient. The animal's position and attitude, cuff size and site, cuff site circumference (cm), and name of the individual making the measurements should be carefully recorded and used for future pressure measurements. Individual patients may be noise‐sensitive, but, in general, use of headphones by the measurer does not result in lower BP measurements.18
Table 1.
Protocol for accurate blood pressure (BP) measurement
|
3. NORMAL VALUES FOR CANINE AND FELINE BP
Various studies have reported values for BP in normal dogs and cats (Table 2). These values vary, reflecting differences in subject populations, measurement techniques, and animal handling. This variability emphasizes the importance of standardization of technique in veterinary practice. Additional factors affect what is considered “normal” BP. In people, age‐related increases in SBP and pulse pressure have been well characterized.19 The effect of age is less clear in dogs and cats. A small increase in BP of 1‐3 mm Hg/year has been noted with aging in dogs,20, 21 but such an age effect has not been observed in all studies.22, 23 In 1 study, BP increased with age in a heterogeneous population of cats,24 but no age effect was observed in 2 other studies of normal cats.4, 25 In an additional study of apparently healthy cats, a comparatively small increase of 1.5 mm Hg/year was noted for mean BP.26 More recently, a larger study identified an increase in BP over time in cats aged >9 years of age with repeated BP measurements, but the risk of developing hypertension was lower in apparently healthy cats than in those with azotemic chronic kidney disease (CKD).27 A large cross‐sectional study also has identified an increase in BP with age in apparently healthy cats,28 but the cats were not screened for concurrent disease.
Table 2.
Arterial blood pressure (mm Hg) values obtained from normal, conscious, dogs and cats
| Measurement method | n | Systolic | Mean | Diastolic | Nonparametric |
|---|---|---|---|---|---|
|
DOGS:
Intra‐arterial: | |||||
| Anderson et al (1968)191 | 28 | 144 ± 156 | 104 ± 13 | 81 ± 9 | |
| Cowgill et al (1983)192 | 21 | 148 ± 16 | 102 ± 9 | 87 ± 8 | |
| Chalifoux et al (1985)193 | 12 | 154 ± 31 | 115 ± 16 | 96 ± 12 | |
| Stepien et al (1999)194 | 27 | 154 ± 20 | 107 ± 11 | 84 ± 9 | |
| Oscillometry: | |||||
| Bodey and Michell20 | 1267 | 131 ± 20 | 97 ± 16 | 74 ± 15 | |
| Coulter et al (1984)6 | 51 | 144 ± 27 | 110 ± 21 | 91 ± 20 | |
| Kallet et al, 199751 | 14 | 137 ± 15 | 102 ± 12 | 82 ± 14 | |
| Stepien et al (1999)194 | 28 | 150 ± 20 | 108 ± 15 | 71 ± 18 | |
| Meurs et al (2000)23 | 22 | 136 ± 16 | 101 ± 11 | 81 ± 9 | |
| Hoglund et al (2012)36 | 89 | 139 ± 16 | 71 ± 13 | ||
| Doppler ultrasonography: | |||||
| Chalifoux et al (1997)193 | 12 | 145 ± 23 | |||
| Stepien et al (1999)194 | 28 | 151 ± 27 | |||
| Rondeau et al (2013)46 | 51 | 147 ± 25 | |||
|
CATS:
Intra‐arterial: | |||||
| Brown et al (1997)195 | 6 | 125 ± 11 | 105 ± 10 | 89 ± 9 | |
| Belew et al (1999)16 | 6 | 126 ± 9 | 106 ± 10 | 91 ± 11 | |
| Slingerland et al (2007)196 | 20 | 132 ± 9 | 115 ± 8 | 96 ± 8 | |
| Zwijnenberg et al (2011)197 | 6 | 160 ± 12 | 138 ± 11 | 116 ± 8 | |
| Jenkins et al (2014)198 | 6 | 111 ± 4 | 75 ± 2 | ||
| Oscillometry: | |||||
| Bodey et al (1998)24 | 104 | 139 ± 27 | 99 ± 27 | 77 ± 25 | |
| Mishina et al (1998)26 | 60 | 115 ± 10 | 96 ± 12 | 74 ± 11 | |
| Doppler ultrasonography: | |||||
| Kobayashi et al (1990)4 | 33 | 118 ± 11 | |||
| Sparkes et al (1999)25 | 50 | 162 ± 19 | |||
| Lin et al (2006)199 | 53 | 134 ± 16 | |||
| Dos Reis et al (2014)200 | 30 | 125 ± 16 | |||
| Taffin et al (2016)201 | 113a | 133 ± 20 | |||
| Quimby et al (2011)202 | 30 | 137 ± 16b | Median 138 (range 106‐164) | ||
| Paige et al (2009)203 | 87 | 131 ± 18 | |||
| Chetboul et al (2014)133 | 20 | 151 ± 5 | 78 ± 3 | ||
| Payne et al (2017)28 | 780 | 122 ± 16b | Median 121 (IQR 110‐132) | ||
Includes 3 cats with renal azotemia.
Data not included in original publication but obtained after a direct approach to the authors interquartile range (IQR).
An effect of sex on BP was identified in 1 study of dogs20 in which intact males had higher BP and intact females had lower BP as compared to neutered dogs; in all cases, differences among groups were <10 mm Hg. In other studies, no association between sex and higher or lower BP was found.29, 30 Most cats evaluated by veterinarians are neutered and in most studies an effect of sex has not been evident in this species.24, 26 In a recent large study, males had higher BP than females and neutered cats had higher BP than intact animals, but the differences were very small.28
There are substantial interbreed differences in canine BP, most notably for hounds (eg, Greyhounds, Deerhounds) in which BP is higher than in mongrels31 by approximately 10‐20 mm Hg.20, 29, 31, 32 The BP among other breeds varies by 7‐10 mm Hg20, 33 perhaps based on temperament.34, 35, 36 The panel recognizes the need for breed‐specific BP ranges to be developed. In cats, no effect of breed has been observed on BP.24, 28
Obesity is associated with increases in BP in several species.37, 38, 39, 40, 41, 42 This effect has been studied experimentally in dogs.37, 43 A small (<5 mm Hg) increase in BP was noted in obese dogs by oscillometry20 but not by Doppler sphygmomanometry.22 The relationship between obesity and higher BP in dogs may be related to the prevalence of underlying disease.30 In cats, no effect of obesity on BP was observed by oscillometry,24 but cats that were underweight had slightly lower BP when measured with Doppler than those that were of ideal body weight or obese.28 Recent studies suggested no association among body condition score, body weight, and SBP measurements in dogs or cats, but muscle condition score and sarcopenia have been reported to affect radial but not coccygeal BP measurements in the cat.44, 45
Blood pressure measurement results in normal animals are highly variable based on breed, temperament, patient position, measurement method, operator experience, and intrapatient variability,15, 17, 29, 46, 47 and it is difficult to determine a single value and range that might be applicable to all dogs or cats. Ranges of expected values in many studies of normal dogs and cats using various measurement techniques are presented in Table 2. In disease‐free patient populations, in which the BP values typically are expected to be distributed normally, expected normal values are presented as mean ± SD, but in hypertensive patients, the frequency distribution of BP measurements tends to be skewed with fewer patients having very high measurements.48 For this reason, the panel recommends that data from future studies of abnormal populations be presented as median and interquartile range.
4. HYPERTENSION DEFINITIONS
The term systemic hypertension is applied to sustained increases in SBP, and generally can be categorized into 1 of 3 types. It may be caused by environmental or situational stressors, it may occur in association with other disease processes that increase BP (ie, secondary hypertension), or it may occur in the absence of other potentially causative disease processes (ie, idiopathic hypertension). Accordingly, we suggest the definitions and criteria described below.
4.1. Situational hypertension
Increases in BP that occur as a consequence of the in‐clinic measurement process in an otherwise normotensive animal are termed situational hypertension. Situational hypertension is caused by autonomic nervous system alterations that arise from the effects of excitement or anxiety on higher centers of the central nervous system. This type of hypertension resolves under conditions that decrease or eliminate the physiologic stimulus (eg, altering measurement conditions to decrease the animal's anxiety and measuring BP in the animal's home environment). In people, there is question as to whether the so‐called “white coat hypertension” actually represents a risk factor for subsequent hypertensive damage, with some evidence suggesting increased long‐term cardiovascular risk in these, as compared to normotensive, patients.49, 50 There presently is no justification to treat situational hypertension in dogs or cats. More importantly, anxiety‐ or excitement‐induced increases in BP can lead to an erroneous diagnosis of true pathologic systemic hypertension.22, 51
Unfortunately, the effects of anxiety on BP are not predictable, and some animals exhibit a marked increase in BP whereas others do not. Some animals even may exhibit a decrease in BP as a result of the measurement process.16 In human patients, awareness of the phenomena of “white coat” hypertension and of “masked hypertension” (the latter term applied to cases in which in‐clinic BP measurements are normal for a patient who is hypertensive in the nonmedical environment) has encouraged the evaluation of ambulatory or at‐home BP as a complement to conventional in‐clinic BP measurements.52, 53 Whether masked hypertension is important in veterinary species is unclear, and the use of ambulatory BP monitoring has not been systematically evaluated in veterinary medicine.
4.2. Secondary hypertension
Secondary hypertension represents persistent, pathologically increased BP concurrent with a disease or condition known to cause hypertension (Table 3), or hypertension associated with the administration of a therapeutic agent or ingestion of a toxic substance known to cause an increase in BP (Table 4). Hypertension may persist despite effective treatment of the primary condition54, 55, 56 and BP may increase after treatment is initiated.57 The presence of a condition known to cause secondary hypertension, even if effectively resolved by therapeutic intervention, should prompt serial follow‐up evaluations.
Table 3.
Diseases associated with secondary hypertension in dogs and cats
| Disease or condition | Prevalence of hypertension (%) | Reference(s) |
|---|---|---|
| DOGS: | ||
| Chronic kidney disease | 93 | 191 |
| 60 | 192 | |
| 80 | 192 | |
| 79 | 204 | |
| 9 | 20 | |
| 62 | 81 | |
| 19 | 205 | |
| 28.8 | 79 | |
| 14 | 206 | |
| 47 | Jacob et al (1999) (ACVIM abstract) | |
| Acute kidney disease | 87 | 207 |
| 15%‐37% (at admission) | 208 | |
| 62%‐81% (during hospitalization) | ||
| Hyperadrenocorticism (naturally occurring or iatrogenic) | 73 | 55 |
| 80 | 204 | |
| 35 | 209 | |
| 36.8 | 210 | |
| 20‐46.7 | 211 | |
| Diabetes mellitus | 46 | 212 |
| 24 | 204 | |
| 67 | 213 | |
| 55 | 214 | |
| Obesity | Small effect | 20, 22, 30, 37, 43 215, 216 |
| Primary hyperaldosteronism | Rare disease | 217 |
| 218 | ||
| Pheochromocytoma | 43% | 219 |
| 86% | 220 | |
| 54.5‐65% | 221 | |
| Hypothyroidism | Uncommon | 222 |
| Brachycephalic | No prevalence data | 223 |
| CATS: | ||
| Chronic kidney disease | 46 | 4 |
| 65 | 85 | |
| 19 | 48 | |
| 39.6% at diagnosis of CKD | 27 | |
| If normotensive at diagnosis of CKD 17% develop | ||
| Hypertension >3 months after diagnosis | ||
| 29% (stable CKD over 12 months) | 74 | |
| 40% (progressive CKD over 12 months) | ||
| Diabetes mellitus | 0 | 111 |
| No increase of BP | 224 | |
| 15% | 225 | |
| Hyperthyroidism | 87 | 4 |
| 23 | 85 | |
| 5 pretreatment and | 56 | |
| 25 posttreatment | ||
| 10% pretreatment | ||
| 12.8% (pre) and 22% (post) | 226 | |
| 22% (pre) and 24% (post) | 227 | |
| 228 | ||
| Obesity | Hypertension uncommon | 24 |
| Primary hyperaldosteronism | 50%‐100% | 63, 229, 230, 231, 232, 233, 234, 235 |
| Uncommon disease | ||
| Pheochromocytoma | Unusual disease | 236 |
| 237 | ||
| 181 | ||
| Hyperadrenocorticism | 19% | 238, 239 |
Variability in inclusion criteria, measurement techniques, and definition of hypertension makes direct comparison of prevalence data difficult.
Table 4.
Therapeutic agents and intoxicants associated with secondary hypertension in dogs and cats
| Agent | Species | Notes |
|---|---|---|
| Glucocorticoids | Dog | • Statistically significant, mild to moderate, dose‐dependent increases in BP noted at dosages sufficient to induce signs of iatrogenic hyperadrenocorticism.240, 241, 242
• Systemic hypertension (ie, SBP ≥160) is uncommon in dogs administered agents with pure glucocorticoid activity at clinically relevant dosages.240, 242, 243, 244 |
| Mineralocorticoids | Dog | • At high dosages and in normal dogs, administration of desoxycorticosterone (DOC) is associated with statistically significant increases in BP,245, 246 most especially when combined with unilateral nephrectomy or high dietary sodium intake.247, 248
• Desoxycorticosterone pivalate (DOCP), administered at clinically relevant dosage rate (2.2 mg/kg IM q 30 days) to dogs with naturally occurring hypoadrenocorticism was not associated with significant increase in BP.249 |
| Erythropoiesis‐stimulating agents | Dog, cat | • Worsening or onset of systemic HT is common in animals with CKD related anemia when treated with recombinant human erythropoietin,250 recombinant canine or feline erythropoietin,251, 252 or darbepoetin alfa.253, 254
• 96% of dogs administered darbepoetin alfa experienced an increase in BP253 • 37% of previously normotensive cats developed HT during darbepoetin alfa treatment254 • HT noted in 40% and 50% of dogs and cats, respectively, treated with rhEPO250 • It is difficult to know to what degree disease progression alone contributes to observed BP increases. |
| Phenylpropanolamine (PPA) | Dog | • Normal dogs administered PPA (1.5‐12.5 mg/kg PO), experience transient, significant increases in BP peak 30‐120 minutes post‐dose and last approximately 3‐5 hours.255
• Persistent HT is uncommon when administered long‐term at recommended dosage (1.5 mg/kg PO q8h) in incontinent dogs.256, 257 • At high doses, acute intoxication may cause severe systemic HT.258, 259 |
| Phenylephrine hydrochloride | Dog | Systemic HT reported in normal dogs,260 and those scheduled for cataract surgery,261 administered topical ocular phenylephrine hydrochloride. |
| Ephedrine | Dog | Significant increases in direct BP were noted in normal dogs administered ephedrine (1.5 mg/kg PO q12h).262 |
| Pseudoephedrine | Dog | • At high doses, acute intoxication may cause systemic HT.263
• When administered for long term to dogs with urinary incontinence, significant increases in indirect BP were not noted.257 |
| Toceranib phosphate | Dog | Systemic HT documented in 28% of previously normotensive dogs treated for various neoplastic diseases for 14 days.264 |
| Chronic, high‐dose sodium chloride | • BP in normal cats and dogs appears to be relatively salt‐insensitive.134, 265, 266, 267
• High‐sodium diets do not appear to promote HT in cats with reduced renal function,131, 266 and salt‐induced HT in the dog seems to be limited to experimental models that also involve nephrectomy268, 269 or mineralocorticoid administration.248 • BP effects of high‐sodium intake in cats and dogs with pre‐existing naturally occurring systemic HT, have not been systematically evaluated. |
|
| Intoxicants with which systemic hypertension has been reported/associated: | ||
| Cocaine270, 271 | Dog | |
| Methamphetamine/amphetamine272, 273, 274 | Dog | |
| 5‐hydroxytryptophan275 | Dog | |
| Agents associated with systemic hypertension in people, but whose BP effects have not been well characterized in dogs and cats: guarana (caffeine), ma huang (ephedrine), tacrolimus, licorice, and bitter orange.276, 277 | ||
4.3. Idiopathic hypertension
The term “primary” or “essential” hypertension often is used in people to describe persistent pathological hypertension in the absence of any identifiable underlying cause and represents a complex multifactorial disorder involving genetic, lifestyle, and environmental factors. Essential hypertension has been reported in dogs.58, 59, 60, 61, 62 Because subclinical kidney disease is present frequently in people and animals with hypertension, a valid diagnosis of primary or essential hypertension can be difficult to establish. Furthermore, the presence of chronically increased BP suggests that one or more of the neurohumoral and renal systems responsible for regulating BP is abnormal. Thus, the panel recommends the use of the term “idiopathic” in place of “essential” for animals in which high BP occurs in the absence of an overt clinically apparent disease that is known to cause secondary hypertension.
A diagnosis of idiopathic hypertension is suspected when reliable BP measurements demonstrate a sustained increase in BP concurrent with normal CBC, serum biochemistry, and urinalysis results. Unfortunately, increased BP may induce polyuria (the so‐called pressure diuresis), and thus the presence of low urine‐specific gravity (<1.030) in a patient with high BP does not establish that kidney disease is present. On the other hand, the presence of concentrated urine (>1.030) makes kidney disease less likely. Because subclinical kidney disease or other conditions known to cause secondary hypertension may be present in animals with idiopathic hypertension, the panel recommends that diagnostic tests in addition to CBC, serum biochemistry, and urinalysis be considered in affected animals. Depending on the clinical findings, these tests may include renal ultrasound examination (dog, cat), evaluation of serum symmetric dimethylarginine (SDMA) concentrations (dog, cat), measurement of glomerular filtration rate (GFR) (dog, cat), quantitative assessment of proteinuria (dog, cat), serum thyroxine hormone concentration (cat), and serum cortisol concentrations (dog). Additional tests to consider in individual patients include serum and urine aldosterone and catecholamine concentrations as well as adrenal ultrasound examination.
Although secondary hypertension is most common in dogs and cats, idiopathic hypertension is more common than previously recognized, accounting for approximately 13%‐20% of cases in cats.13, 63, 64 Approximately 12% of nonazotemic nonhyperthyroid cats were hypertensive at baseline in one report,65 and in a more recent study of 133 apparently healthy initially normotensive cats aged ≥9 years, 7% developed idiopathic hypertension over the study's follow‐up period.27
5. TARGET ORGAN DAMAGE (TOD)
Systemic hypertension is problematic only because chronically sustained increases in BP cause injury to tissues; the rationale for treatment of hypertension is prevention of this injury. Damage that results from the presence of sustained high BP is commonly referred to as end organ or TOD (Table 5) and the presence of TOD generally is a strong indication for antihypertensive treatment.
Table 5.
Evidence of target organ damage (TOD)
| Tissue | Hypertensive injury (TOD) | Clinical findings indicative of TOD | Diagnostic test(s) |
|---|---|---|---|
| Kidney | Progression of chronic kidney disease | Serial increases in SCr, SDMA, or decrease in GFR Persistent proteinuria, microalbuminuria |
Serum creatinine, SDMA and BUN Urinalysis with quantitative assessment of proteinuria and/or albuminuria GFR measurement |
| Eye | Retinopathy/choroidopathy | Acute onset blindness Exudative retinal detachment Retinal hemorrhage/edema Retinal vessel tortuosity or perivascular edema Papilledema Vitreal hemorrhage Hyphema Secondary glaucoma Retinal degeneration |
Ophthalmic evaluation including a funduscopic examination |
| Brain | Encephalopathy Stroke |
Centrally localizing neurological signs (brain or spinal cord) | Neurological exam Magnetic resonance or other imaging |
| Heart and blood vessels | Left ventricular hypertrophy Left‐sided congestive heart failure (uncommon) Aortic aneurysm/dissection (rare) |
Left ventricular concentric hypertrophy Gallop sound Arrhythmias Systolic heart murmur Evidence of left‐sided congestive failure Hemorrhage (eg, epistaxis, stroke, and aortic rupture) |
Auscultation Thoracic radiography Echocardiography Electrocardiogram |
BUN, blood urea nitrogen concentration; GFR, glomerular filtration rate; SCR, serum creatinine concentration; SDMA, symmetric dimethylarginine.
Hypertension has been associated with proteinuria and histological renal injury in both experimental studies and in naturally occurring disease, an effect that has been identified in several species including humans,66, 67 dogs,14, 68, 69 and cats.70, 71 Proteinuria, in turn, has been associated with more rapid progression of renal disease and increased all‐cause mortality in numerous clinical settings, including CKD and hypertension.70, 72 Antihypertensive treatment generally decreases the severity of proteinuria, at least if the hypertension is severe.13, 72, 73, 74 What remains unproven, at least in dogs and cats, is whether or not this decrease in proteinuria with antihypertensive drug treatment mitigates renal injury, or is simply a surrogate for improved renal outcomes, such as rate of decrease in GFR (usually assessed by measurement of serum creatinine concentration) or renal‐related mortality.13, 72 Although the benefit is unproven, hypertension‐induced or hypertension‐exacerbated proteinuria currently remains an attractive target for treatment in veterinary patients.
Several epidemiological studies have associated hypertension with proteinuria (and in some studies specifically albuminuria) in cats with naturally occurring diseases.70, 72, 74 In addition, albuminuria has been related to an increase in BP in experimental studies of induced renal disease in cats.75 A recent study of cats found that even with anti‐hypertensive treatment, higher time‐averaged SBP was associated with glomerulosclerosis and hyperplastic arteriolosclerosis lesions after the patient's death.71 However, this effect was not replicated in a second, smaller, study.76
In dogs with azotemic CKD, magnitude of BP has been associated with proteinuria, and this has been associated with shortened survival times.14, 77 Hypertension also was associated with shorter renal survival, but only if proteinuria was excluded from the analysis.14 Proteinuria was directly related to the extent of increase in BP and to the rate of decrease in GFR in an experimental study in dogs.78 Dogs with leishmaniasis frequently have proteinuria and systemic hypertension, even when nonazotemic, although in this setting the proteinuria is thought to relate mainly to immune‐mediated glomerular lesions, rather than occurring as a consequence of the hypertension.68, 79 Hypertensive greyhounds have an increased prevalence of microalbuminuria, although most dogs do not have histological evidence of renal injury.29 Hypertension may be present in any stage of CKD, and serum creatinine concentration is not directly related to BP.4, 80 Hypertensive cats and dogs often have minimal or no azotemia.81
Ocular lesions are observed in many cats with hypertension and although prevalence rates for ocular injury vary, the frequency of ocular lesions has been reported to be as high as 100%.60, 63, 64, 82, 83, 84, 85, 86, 87, 88, 89 Ocular lesions also are common in hypertensive dogs.14, 59, 60, 90, 91 The syndrome91 is commonly termed hypertensive retinopathy and choroidopathy and has been frequently reported in dogs14, 59, 60, 92 and cats.63, 64, 84, 85, 93, 94, 95, 96 Exudative retinal detachment is the most commonly observed finding. Other lesions include retinal hemorrhage, multifocal retinal edema, retinal vessel tortuosity, retinal perivascular edema, papilledema, vitreal hemorrhage, hyphema, secondary glaucoma, and retinal degeneration.92 Acute onset of blindness from complete bilateral exudative retinal detachment may be a presenting complaint in both species.60, 93, 94 Effective antihypertensive treatment can lead to retinal reattachment, but restoration of vision87 generally occurs in only a minority63 of patients, and successful treatment of hypertension may not resolve ocular abnormalities.92 Hypertensive ocular injury has been reported in patients with SBP as low as 168 mm Hg,86 and there is a substantially increased risk of occurrence when SBP exceeds 180 mm Hg.60, 82, 93, 95
Hypertensive encephalopathy97 has been reported in dogs14 and cats,63, 94, 98 and it occurs in people as a well‐described entity characterized by white matter edema and vascular lesions.99, 100 Neurologic signs were reported in 29%63 and 46%94 of hypertensive cats. Hypertensive encephalopathy also occurs after renal transplantation in people101 and is a cause of otherwise unexplained death in this setting in cats.98, 102, 103 This syndrome, in its early phases, is responsive to antihypertensive treatment.75, 98 Hypertensive encephalopathy is more likely to occur in cats with a sudden increase in BP, a SBP that exceeds 180 mm Hg, or both.75 Observed clinical signs are typical of intracranial disease and include lethargy, seizures, acute onset of altered mentation, altered behavior, disorientation, balance disturbances (eg, vestibular signs, head tilt, and nystagmus), and focal neurologic defects because of stroke‐associated ischemia. Other central nervous system abnormalities, including hemorrhage and infarction, which occur with chronic hypertension in people,104 also are observed in dogs and cats.105 A recent study described lesions on magnetic resonance imaging consistent with vasogenic edema in the occipital and parietal lobes of the brain in affected cats and dogs with neurologic signs.106 Hypertension appears to be a risk factor for ischemic myelopathy of the cranial cervical spinal cord, resulting in ambulatory tetraparesis or tetraplegia with intact nociception in old cats.107
Cardiac abnormalities are common in hypertensive cats63, 64, 82 and dogs.108 When affected, the heart is a target organ and increased cardiac output is rarely the cause of hypertension in animals.63 In both dogs59, 108 and cats,63, 64, 82 physical examination abnormalities may include systolic murmurs and/or gallop sounds. The most common cardiac change associated with hypertensive cardiomyopathy in dogs and cats is cardiomegaly associated with left ventricular concentric hypertrophy (LVH),109, 110 although echocardiographic findings are variable and may be indistinguishable from those associated with feline idiopathic hypertrophic cardiomyopathy.63, 93, 94, 110, 111, 112, 113 Although LVH may not be a risk factor for decreased survival time,82 effective antihypertensive treatment may decrease the prevalence of LVH in affected cats.114 Cardiac failure and other serious complications are infrequent, but may occur.63, 94, 115
Cats with previously undiagnosed hypertension may unexpectedly develop signs of congestive heart failure after fluid therapy. Furthermore, cats with secondary hypertension because of other causes (eg, CKD) may die of cardiovascular complications,64 as frequently is the case in hypertensive people.116 Epistaxis, because of hypertension‐induced vascular abnormalities, has been associated with systemic hypertension but hypertension rarely is the primary cause of epistaxis in either species.117, 118, 119 Aortic aneurysm and aortic dissection are rare and serious complications of hypertension reported in both dogs and cats, and typically require a high index of suspicion and advanced imaging to diagnose.115, 120, 121
6. PREVALENCE AND SELECTION OF PATIENTS FOR HYPERTENSION SCREENING
There are 2 clear indications for evaluating BP in a patient for which systemic hypertension may be a concern. First, BP should be measured in patients with clinical abnormalities consistent with hypertensive TOD (Table 5), specifically, the presence of otherwise unexplained clinical findings associated with systemic hypertension should prompt BP measurement at the time of diagnosis. These include signs of hypertensive choroidopathy or retinopathy, hyphema, intracranial neurologic signs (eg, seizures, altered mentation, and focal neurological deficits), renal abnormalities (eg, proteinuria, microalbuminuria, and azotemia), and cardiovascular abnormalities (eg, LVH, gallop sound, arrhythmia, systolic murmur, and epistaxis). In the absence of these clinical findings, a high index of suspicion must be maintained to diagnose systemic hypertension and to avoid misclassification as situational hypertension. Clinical signs relating to systemic hypertension, evident to the owner or the veterinarian, may be subtle and attributable to aging or underlying clinical conditions that may as yet be undiagnosed. In people, early signs of hypertension are subjective and include morning headaches, facial flushing and feelings of anxiety. Such clinical signs would be difficult to recognize in dogs and cats. In cats, some nonspecific clinical signs have been associated with hypertension in the laboratory setting, including inactivity, lethargy, photophobia, and altered (increased or decreased) appetite (S.A. Brown, unpublished observations, 2004).
The presence of diseases or conditions causally associated with secondary hypertension (Table 3), treatment with pharmacological agents with a known effect on BP, or known or suspected exposure to intoxicants that may increase BP (Table 4) comprise the second group of indication for BP measurement. A thorough physical examination, including funduscopic evaluation, cardiac auscultation, assessment of renal function including proteinuria, and neurologic examination, should also be performed in at‐risk populations to assess for TOD. The correlation between advancing age and prevalence of systemic hypertension is not as clear in cats and dogs as in people, although recent data in healthy normotensive geriatric cats suggest an expected increase in BP of 0.4 ± 0.1 mm Hg per 100 days.122 Conditions resulting in secondary hypertension more frequently are observed in mature to geriatric cats (eg, those with CKD or hyperthyroidism) and dogs (eg, those with hyperadrenocorticism) and, therefore, it may be prudent to screen older animals for these conditions.
The prevalence of hypertension in dogs and cats is not known. Surveys of apparently healthy dogs have identified hypertension in 0.5% of 400 dogs,123 0.9% of 1000 young dogs,124 2% of 215 dogs,125 10% of 102 dogs,22 and 13% of healthy Shetland Sheepdogs.126 Others have provided evidence that suggests dogs are resistant to the development of hypertension.20, 80, 127 The prevalence of hypertension may be comparable in cats. In a study of 104 apparently healthy cats, 2% had SBP > 170 mm Hg.24 However, as noted elsewhere in these guidelines, the lack of uniform measurement techniques, variable inclusion criteria, and inconsistent thresholds for establishing a diagnosis of hypertension in veterinary medicine make prevalence data difficult to interpret. Nonetheless, hypertension seems to be rare in young otherwise healthy dogs and cats. Based on available data, it is still unclear whether or not routine screening of apparently healthy dogs and cats is a reliable method for detecting true hypertension in the population, because the risk of false diagnosis is likely to be high with widespread screening. Therefore, the panel does not recommend routine screening of all dogs and cats for the presence of systemic hypertension. Some conditions (eg, hyperthyroidism, hyperadrenocorticism, and CKD) that result in secondary hypertension are more prevalent in older animals, yet may be occult. Thus, it is reasonable to institute annual screening of cats and dogs ≥9 years of age. Still, high BP in otherwise healthy, particularly young, animals should be assumed to represent situational hypertension until proven otherwise with confirmatory measurements on multiple occasions.
7. DIAGNOSIS OF HYPERTENSION
The diagnosis of hypertension always should be based on reliable BP measurements, and therapeutic decisions in cats and dogs typically are based on SBP results (Figure 1). The presence of TOD (eg, retinopathy and CKD) justifies initiating treatment after a single measurement session, but in most cases, results should be confirmed by measurements repeated on multiple (>2) occasions. In cases of prehypertension (140‐159 mm Hg) or hypertension at moderate risk of TOD (160‐179 mm Hg), these measurement sessions can occur over 4‐8 weeks. With more severe hypertension (≥180 mm Hg), however, the risk of TOD dictates that the measurement sessions be completed in 1‐2 weeks. Once increases in BP are determined to be persistent, and not associated with measurement error or situational hypertension, the search for conditions associated with secondary hypertension (Table 3) should begin.
Figure 1.
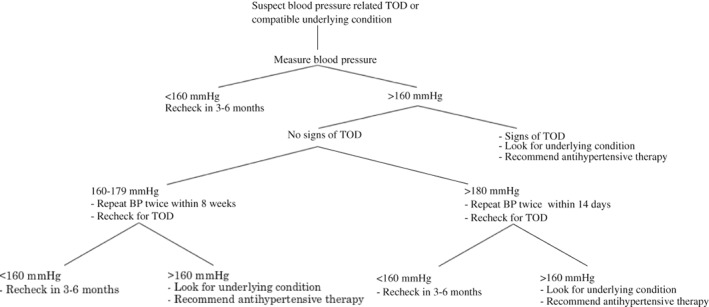
The recommended approach to the evaluation of a possibly hypertensive patient involves reliable measurements of blood pressure as well as the identification of possible target organ damage. Once a diagnosis of hypertension is established, a search for a compatible underlying condition and appropriate treatment should commence
Hypertension in both dogs and cats is classified based on the risk of TOD:
Normotensive (minimal TOD risk) SBP <140 mm Hg
Prehypertensive (low TOD risk) SBP 140‐159 mm Hg
Hypertensive (moderate TOD risk) SBP 160‐179 mm Hg
Severely hypertensive (high TOD risk)SBP ≥180 mm Hg
At this time, information regarding breed‐specific reference ranges is limited, but sight hounds are known to have higher in‐hospital BP than other breeds.32, 128 This difference appears to be because of situational hypertension and not a true difference in SBP.17 Nevertheless, a risk of TOD has been proposed for these dogs when in‐hospital SBP is >180 mm Hg.129 These guidelines likely will be refined as additional breed‐specific information becomes available.
In people, decreasing BP in hypertensive people lowers the risk of TOD. The precise BP at which TOD occurs in dogs and cats is not known. Nevertheless, treatment should be instituted in any patient that has a BP persistently in the hypertensive or severely hypertensive category. The goal should be to decrease BP into the prehypertensive or normotensive range.
8. THE HYPERTENSIVE PATIENT: EVALUATION AND DECISION TO TREAT
Patients with BP in the prehypertensive category typically are not treated with antihypertensive medications, but may benefit from increased frequency of monitoring of overall condition as well as BP. Patients in known renal risk categories (International Renal Interest Society CKD stage 2 or higher) or patients with systemic diseases associated with development of systemic hypertension (eg, hyperthyroidism and hyperadrenocorticism) may benefit from systemic wellness and BP evaluations every 6 months in order to manage systemic disease optimally and detect systemic hypertension when and if it develops.
Once a diagnosis of hypertension has been made and the possibility of situational hypertension has been eliminated, the search for a possible underlying disease or pharmacologic agent associated with secondary hypertension should be commenced. For cases in which secondary hypertension is identified, treatment of the underlying condition should be implemented immediately. Although doing so may decrease systemic BP and make the patient's hypertension more amenable to treatment, most pets fail to become normotensive and will continue to be at risk for TOD. For this reason, treatment of a patient's hypertension should not be postponed until the underlying condition is controlled.
Client education is paramount. In most cases, hypertension is silent and damage to target organs occurs over long periods of time, and it is easy for owners to underestimate the importance of appropriate treatment and follow‐up. Owners must realize that control of hypertension is likely to improve the quality of their pet's life over the long term, but potentially with little immediate observable benefit. The client should be provided with BP results, a working knowledge of the complications of both hypertension and the drugs used to manage it, and a clear understanding for the goals of treatment. The owner should never leave the office without a clear plan for reevaluation, including a future appointment.
For most patients, the onset of hypertension has been gradual and it can be treated and controlled as outlined below, but a few patients may experience acute increases in BP resulting in hypertensive choroidopathy, encephalopathy, or rapidly progressive acute kidney injury. In these patients, the increase in BP should be considered a hypertensive emergency. For recommendations regarding the management of these patients, the reader is referred to the section on hypertensive emergencies.
8.1. General treatment guidelines
Because hypertension in dogs and cats often is secondary (≥80% of cases), antihypertensive drug treatment should be initiated along with treatment for any underlying or associated condition. Initial considerations (Figure 2) always should include identification and management of conditions likely to be causing secondary hypertension and identification and treatment of TOD. If possible, these considerations should be addressed with specific targeted diagnostic and therapeutic regimens. Effective management of a condition causing secondary hypertension may lead to complete or partial resolution of the high BP in some, but not all, cases.4, 14, 55 Decisions to use antihypertensive drugs should be based on the integration of all clinically available information, and a decision to treat (which may effectively mandate lifelong drug treatment) warrants periodic re‐evaluation.
Figure 2.
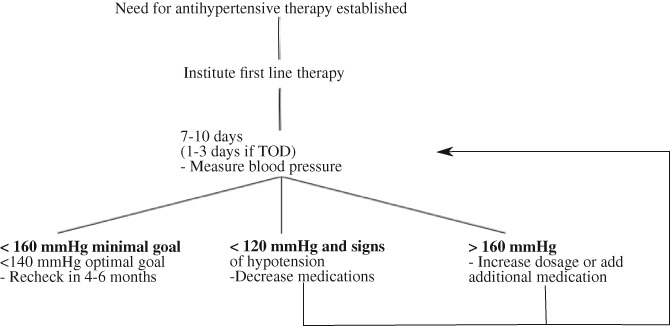
Management of hypertension involves a stepwise approach, including repeat blood pressure measurement and medication adjustments
Treatment for hypertension must be individualized to the patient and take into account concurrent conditions. Once daily treatment is ideal; fewer treatments always are preferred. A gradual persistent decrease in BP is the therapeutic goal. Acute marked decrease in BP should be avoided. If the chosen antihypertensive agent is only partially effective, the usual approach is to consider increasing the dosage or adding an additional drug. Management of highly resistant hypertension in people often requires multiagent (≥2) protocols; a similar situation often occurs in dogs, although this appears to be relatively rare in cats. It is often helpful to discuss with the owner the interindividual variability of response to antihypertensive medications when the first medication is prescribed, and the need for frequent monitoring until a therapeutic goal is reached.
The goal of antihypertensive treatment is to decrease the likelihood and severity of TOD. Hypertension generally is not an emergency, and rapid decreases in BP usually should not be sought aggressively. Studies in people indicate that reduction of risk for TOD by antihypertensive treatment is a continuum and that the lower the BP, the lower the risk for TOD. Results of a recent laboratory study in dogs78 suggest that BP is a continuous risk marker for progression of kidney disease and may justify a similar treatment approach in veterinary patients. The panel feels that regardless of the initial magnitude of BP, the goal of treatment should be to maximally decrease the risk of TOD (SBP < 140 mm Hg) and that antihypertensive treatment should be adjusted on re‐evaluation if SBP is ≥160 mm Hg, with a minimal goal of treatment being to achieve a decrease in SBP to ≤160 mm Hg (Table 6). Blood pressure <120 mm Hg, combined with clinical findings of weakness, syncope, or tachycardia, indicates systemic hypotension and treatment should be adjusted accordingly (Figure 2).
Table 6.
Hypertension in both dogs and cats classified based on the risk of target‐organ damage (TOD)
| Normotensive (minimal TOD risk) | SBP <140 mm Hg |
| Prehypertensive (low TOD risk) | SBP 140‐159 mm Hg |
| Hypertensive (moderate TOD risk) | SBP 160‐179 mm Hg |
| Severely hypertensive (high TOD risk) | SBP ≥180 mm Hg |
Although frequently recommended as an initial step in the pharmacological management of high BP (Figure 2), dietary salt restriction is controversial,84, 130, 131 and available evidence suggests that substantial sodium restriction alone generally does not decrease BP.130, 131, 132 Although sodium restriction activates the renin‐angiotensin‐aldosterone system (RAAS) axis59, 131 and has variable effects on BP,130, 132 it may enhance the efficacy of antihypertensive agents that interfere with this hormonal system (eg, angiotensin‐converting enzyme inhibitors [ACEi], angiotensin receptor blockers [ARB], and aldosterone receptor blockers). Although normal cats133, 134 and dogs135 generally are not salt‐sensitive, high salt intake may produce adverse consequences in some settings,136, 137 including animals with CKD.84 The panel therefore recommends avoiding high dietary sodium chloride intake. However, the selection of appropriate diet should include other patient‐specific factors, such as underlying or concurrent diseases and palatability.
8.2. Management of hypertension in dogs
Once a decision is made to treat a dog with hypertension, antihypertensive treatment should be individualized to the patient, based in large part on the animal's concurrent conditions, with a therapeutic goal of decreasing the likelihood of future TOD (ie, decreasing SBP by at least 1 SBP substage). In most dogs, hypertension is not an emergency and SBP should be decreased gradually over several weeks. Certain disease conditions may be best addressed using specific classes of agents, such as alpha‐ and beta‐adrenergic blockers for hypertension associated with pheochromocytoma or aldosterone receptor blockers for hypertension because of adrenal tumors associated with hyperaldosteronism.75, 138, 139, 140, 141 Otherwise, RAAS inhibitors and calcium channel blockers (CCB) are the most widely recommended antihypertensive agents for use in dogs.142 Because of their antiproteinuric effect and the high prevalence of CKD in hypertensive dogs, RAAS inhibitors are often chosen as first‐line antihypertensive agents in dogs. In dogs with concurrent CKD, a clinically relevant decrease in proteinuria (ie, urinary protein‐to‐creatinine [UPC] ratio decreased by ≥50%, preferably to <0.5) is a secondary goal of antihypertensive treatment. Available RAAS inhibitors include ACEi, ARB, and aldosterone antagonists, but most clinical experience in veterinary medicine has been with ACEi. An ACEi (eg, 0.5‐2.0 mg enalapril or benazepril/kg PO q12h) usually is recommended as the initial drug of choice in a hypertensive dog. An ARB (eg, 1.0 mg telmisartan/kg PO q24h) is an alternative method for RAAS inhibition. The exception to the use of a RAAS inhibitor as initial, sole agent, treatment is severely hypertensive dogs (SBP > 200 mm Hg) for which the initial coadministration of a RAAS inhibitor and a CCB (eg, 0.1‐0.5 mg/kg amlodipine PO q24h) is appropriate. The use of CCB as monotherapy in dogs should be avoided because CCB preferentially dilate the renal afferent arteriole potentially exposing the glomerulus to damaging increases in glomerular capillary hydrostatic pressure. Because ACEi and ARBs preferentially dilate the renal efferent arteriole, the coadministration of a RAAS inhibitor and a CCB may have a limited effect on glomerular capillary hydrostatic pressures.
If an antihypertensive regimen is ineffective, the usual decision is to increase the dosage of currently used agents or to add an alternative agent. A variety of other agents have BP‐lowering efficacy (Table 7) and these may be used as appropriate in patients for which risk reduction is not adequate with ACEi or CCB or a combination of these drugs (Figure 2). Although diuretics are frequently administered to hypertensive people, these agents are not first‐choice drugs for veterinary patients, particularly given the prevalence of CKD in hypertensive dogs and the adverse consequences of diuretic‐induced dehydration and volume depletion in this setting. However, diuretics can be considered in the small subset of hypertensive animals in which volume expansion is clinically apparent (eg, those with edema).
Table 7.
Oral antihypertensive agents
| Class | Drug | Usual oral dosage |
|---|---|---|
| Angiotensin converting enzyme inhibitor | Benazepril | D: 0.5 mg/kg q12‐24h |
| C: 0.5 mg/kg q12h | ||
| Enalapril | D: 0.5 mg/kg q12‐24h | |
| C: 0.5 mg/kg q24h | ||
| Angiotensin receptor blocker | Telmisartan | C: 1 mg/kg q24h |
| D: 1 mg/kg q24h | ||
| Calcium channel blocker | Amlodipine | D/C: 0.1‐0.25 mg/kg q24h |
| (up to 0.5 mg/kg in cats and dogs) | ||
| C: 0.625‐1.25 mg per cat q24h | ||
| α1 blocker | Prazosin | D: 0.5‐2 mg/kg q8‐12h C: 0.25‐0.5 mg/cat q24h |
| Phenoxybenzamine | D: 0.25 mg/kg q8‐12h or 0.5 mg/kg q24h | |
| C: 2.5 mg per cat q8‐12h or 0.5 mg/cat q24h | ||
| Acepromazine | D/C: 0.5‐2 mg/kg q8h | |
| Direct vasodilator | Hydralazine | D: 0.5‐2 mg/kg q12h |
| (start at low end of range) | ||
| C: 2.5 mg/cat q12‐24h | ||
| Aldosterone antagonist | Spironolactone | D/C: 1.0‐2.0 mg/kg q12h |
| β blocker | Propranolol | D: 0.2‐1.0 mg/kg q8h |
| (titrate to effect) | ||
| C: 2.5‐5 mg/cat q8h | ||
| Atenolol | D: 0.25‐1.0 mg/kg q12h | |
| C: 6.25‐12.5 mg/cat q12h | ||
| Thiazide diuretic | Hydrochlorothiazide | D/C: 2‐4 mg/kg q12‐24h |
| Loop diuretic | Furosemide | D/C: 1‐4 mg/kg q8‐24h |
C, cat; D, dog.
Antihypertensive agents in general, and RAAS inhibitors in particular, should be used with caution in dehydrated dogs in which GFR may decrease precipitously with their use. Unless severe hypertension with rapidly progressive TOD is present, these patients should be carefully rehydrated and then re‐evaluated before instituting antihypertensive treatment.
8.3. Management of hypertension in cats
Despite the potential role of either the systemic or intrarenal RAAS axis in the pathogenesis or maintenance of hypertension,26, 143, 144, 145, 146, 147, 148 CCB, specifically amlodipine besylate, have been the first choice for antihypertensive treatment because of established efficacy64, 75, 114, 149, 150, 151, 152 in cats with idiopathic hypertension or in those with CKD. A mean decrease in SBP of 28‐55 mm Hg typically is observed in cats in hypertensive to severely hypertensive cats.64, 149, 150, 152 Recent data indicate that an initial starting dose of 0.625 mg per cat per day amlodipine besylate is effective in cats in which initial SBP is <200 mm Hg, but that those cats with SBP >200 mm Hg may benefit from a higher starting dosage of 1.25 mg per cat per day.151 Rarely, dosages of up to 2.5 mg per cat per day however may be required. Given the efficacy of amlodipine as an antihypertensive agent, careful investigation of owner compliance should occur before increasing to the dose of amlodipine. Research evaluating plasma amlodipine concentration indicates that the need for dose escalation to adequately control BP appears to relate to severity of the hypertension rather than to body weight or amlodipine pharmacokinetics.151 Although transdermal application has been explored, efficacy of this route of administration has not been established and PO administration is therefore the preferred route of administration.153, 154 Adverse effects of amlodipine, including peripheral edema and gingival hyperplasia, are rarely reported in the dog and are also uncommon in cats. Although gingival hyperplasia has been reported in licensing studies during administration to young healthy cats, this seems to be relatively rare in clinical practice.155, 156
Despite dramatic antihypertensive efficacy, longitudinal control of SBP with amlodipine besylate has not been shown to increase survival time in hypertensive cats,64, 157 and its use may activate the systemic or intrarenal RAAS.148
A key predictive factor in the survival of hypertensive cats is proteinuria. A significant decrease in proteinuria has been identified in cats that are initially either borderline proteinuric or proteinuric when treated with CCB.157 However, although the combined use of amlodipine and an ACEi or amlodipine and an ARB is reportedly well tolerated,158, 159 studies exploring any additional survival benefit of add‐on antiproteinuric agents in hypertensive cats that remain proteinuric after BP control with amlodipine besylate are lacking. Nevertheless, based on the potential for proteinuria to contribute to the development and progression of renal disease in cats and its association with survival of cats with CKD,65, 160, 161 antiproteinuric treatment should be considered in this situation.162, 163
Telmisartan is an ARB currently licensed in Europe for the treatment of feline proteinuria due to CKD.158 Initial studies in healthy anesthetized cats undergoing radiotelemetric BP monitoring, telmisartan, but not losartan, significantly attenuated the pressor response to angiotensin I.164 Attenuation of the SBP rise was significantly higher than for benazepril when telmisartan was administered at a higher than currently licensed dosage (3 mg/kg PO q24h).164 More recently, a double‐blinded, randomized, placebo‐controlled clinical trial has explored the use of telmisartan administered at a dosage of 2 mg/kg/day for the treatment of naturally occurring hypertension in cats.165 In this study, after 14 days of treatment, a significantly larger decrease in mean SBP from baseline was identified for the telmisartan‐treated (−19 ± 22 mm Hg) compared to the placebo‐treated (−9 ± 17 mm Hg; P < 0.0001) group. After 28 days of treatment, 54.6% of cats receiving telmisartan had reached a target end point of a decrease in SBP > 20 mm Hg, compared to 27.6% in the placebo group. However, excluded from this study were cats with SBP >200 mm Hg, cats with evidence of ocular or central nervous system (CNS) TOD and those already being treated with vasoactive agents. Efficacy of telmisartan in severely hypertensive cats and in those with overt ocular and CNS hypertensive TOD has not been demonstrated. In addition, predefined inclusion removal criteria included cats that developed TOD or SBP >200 mm Hg, thus narrowing the population in the longitudinal study. The combination of amlodipine besylate and telmisartan was shown to be well tolerated in a small number (n = 8) of cats in which the antiproteinuric efficacy of telmisartan was evaluated, but the antihypertensive effect of telmisartan was not a primary outcome in this study.158
Use of ACEi in cats as a first‐line antihypertensive agent is not recommended. Although statistically significant decreases in SBP have been identified when direct arterial BP monitoring is possible, the decrease in SBP is small (±10 mm Hg) and unlikely to be sufficient in most cats.166 However, benazepril has been used in cats that require a second antihypertensive agent and, clinically, the combination of ACEi and amlodipine besylate is well tolerated.159
Angiotensin converting enzyme inhibitors and ARB preferentially dilate the renal efferent arteriole thereby decreasing intraglomerular pressure and the magnitude of proteinuria.158, 167, 168 However, a secondary consequence of efferent arteriolar dilatation is a theoretical tendency for GFR to decrease. Single nephron studies indicate that such is not necessarily the case in cats,169 and indeed administration of ACEi commonly produces only very modest increases in serum creatinine concentration (<0.5 mg/dL; <50 μmol/L), which is generally well tolerated. However, in a recent study, approximately 30% of cats with confirmed or suspected CKD experienced an increase in serum creatinine concentration within 30 days of starting benazepril with a >30% increase in serum creatinine concentration seen in 23.8% of cats with confirmed CKD.170 Deterioration in renal function tests and uremic crisis also was reported as an adverse event in 2/112 cats and 1/112 cats receiving telmisartan, respectively, although the initial stage of CKD in these cats is uncertain from data provided.73 In contrast, no alteration in serum creatinine concentration would be anticipated with introduction of a CCB such as amlodipine besylate.171 Clinicians should be aware of the potential for acute exacerbation of azotemia with concurrent ACEi and ARB, and careful monitoring is recommended.167, 169, 172, 173 Angiotensin converting enzyme inhibitors and ARB should not be started in dehydrated cats in which GFR may decrease precipitously. These patients should be carefully rehydrated and then re‐evaluated before instituting ACEi or ARB treatment.
Although several other antihypertensive agents (Table 7) were explored in early studies, their use rarely is required for treatment of hypertension in cats. Diuretics are not routinely used as antihypertensive agents in cats.63, 94 Beta‐blockers (eg, atenolol) may be useful to control heart rate in some tachycardic hypertensive cats (eg, those with hyperthyroidism), but have negligible antihypertensive effect in such patients and therefore should not be used as a sole agent for the management of hypertension.63, 94, 174 For cats diagnosed with concurrent systemic hypertension and hyperthyroidism, amlodipine besylate remains the first‐line antihypertensive agent, combined with management of hyperthyroidism. Vasodilator drugs such as hydralazine rarely are required for management of hypertension in cats, but they have historically been useful in emergency situations (see emergency management).175
In cats with primary hyperaldosteronism, management with aldosterone antagonists (eg, spironolactone), potassium supplementation, and adrenalectomy (if feasible) is necessary.176 However, antihypertensive treatment with amlodipine besylate often is required for adequate BP control and should be started concurrently, particularly in those patients presented with ocular TOD.177 Medical combination treatment can be utilized in long term for management of patients with primary hyperaldosteronism and hypertension when surgery is not an option.177 Facial dermatitis and excoriation have been reported as a rare adverse effect associated with the use of spironolactone in cats.178 Limited information is available about the effect of adrenalectomy on the ongoing requirements for antihypertensive treatment in cats with primary hyperaldosteronism. Some individual affected cats have not required treatment with amlodipine besylate postoperatively, but the frequency of BP monitoring in these patients is not clear.177 If another, nonadrenal, concurrent disease (such as CKD) was present and contributing to the pathogenesis of hypertension in an individual cat, adrenalectomy alone would not be expected to resolve systemic hypertension. In such case, ongoing antihypertensive management with amlodipine besylate would be required. Careful monitoring of BP therefore is recommended in the peri‐ and postoperative period in cats with primary aldosteronism treated with adrenalectomy.
Pheochromocytoma has been reported rarely in the cat.179, 180, 181, 182 Combination treatment with phenoxybenzamine, an α1‐ and α2‐adrenergic blocker, and amlodipine besylate, may be required to adequately control BP in affected cats.181 For cats in which tachyarrhythmias are of concern, beta‐adrenergic blocker (eg, atenolol) treatment may be considered, but it should only be added after α‐adrenergic blockade. For cats undergoing adrenalectomy, careful BP monitoring is required in the postoperative period, as persistent hypertension or hypotension may occur.
8.4. Hypertensive emergencies
When marked increases in BP are accompanied by signs of ongoing acute TOD, immediate and aggressive treatment is warranted. Clinical trials of therapies and therapeutic strategies for acute hypertensive crises in dogs and cats have not been published, and recommendations are anecdotal and extrapolated from recommendations made for human patients. In dogs and cats, overt evidence of acute TOD is most likely to be ocular (eg, retinal hemorrhage or detachment, hyphema) or neurologic (eg, coma, decreased mentation, generalized, or focal facial seizures). Regardless of knowledge of predisposing disease conditions, diagnosis of SBP ≥ 180 mm Hg (high TOD risk category) in a patient with signs of intracranial TOD (eg, focal facial seizures) necessitates immediate emergency treatment. The need for aggressive treatment in such cases typically requires 24‐hour care capability, and referral to such a facility is warranted when 24‐hour care is not available.
The therapeutic target in patients with acute hypertensive emergencies is an incremental decrease in SBP rather than acute normalization of BP. In cases of chronic hypertension, autoregulatory vascular beds in the brain and kidneys may have adapted to higher perfusion pressure, and acute marked BP reduction may result in hypoperfusion. Initial SBP should be decreased by approximately 10% over the first hour and another approximately 15% over the next few hours,183 followed by gradual return to normal BP.
Because of the requirement for incremental SBP decreases, optimal acute management of hypertensive emergencies requires parenteral treatment that can be titrated to effect, with rapid onset and conclusion of action. Several medications have been discussed in this setting in hypertensive human patients, and although several of these medications have been used anecdotally in dogs and cats, no comparative studies of these drugs in severely hypertensive dogs or cats are available. Current recommendations are based on mechanism of action, recommendations in human medicine and reports and anecdotal experience in veterinary patients.
One of the most feasible parenteral medications in veterinary clinical use (where available) may be fenoldopam,184 a selective dopamine‐1‐receptor agonist currently approved for use in hypertensive human emergency patients.185, 186 Although no veterinary studies of this medication are available in acute hypertension in dogs or cats, fenoldopam appears to be safe for treatment of acute kidney injury in veterinary patients.184 Through its dopamine‐1 agonist action, fenoldopam causes renal arterial vasodilation, natriuresis, and increased GFR in normal dogs,187 and it is associated with diuresis in healthy cats,188 all of which may be beneficial in veterinary patients with hypertensive emergencies. Fenoldopam is delivered as a constant rate infusion (CRI), initially at a dosage of 0.1 μg/kg/min with careful (ie, at intervals of at least 10 minutes) monitoring of BP. The dosage can be titrated up by 0.1 μg/kg/min increments every 15 minutes to the desired SBP, to a maximal dosage of 1.6 μg/kg/min. The plasma half‐life of fenoldopam in dogs and cats is short,106, 189 and effects can be expected to subside within several minutes of discontinuing the infusion. Other parenteral medications that may be effective in hypertensive dogs include labetolol (0.25 mg/kg IV over 2 minutes, repeated to a total dosage of 3.75 mg/kg, followed by a CRI of 25 μg/kg/min), hydralazine (loading dosage of 0.1 mg/kg IV over 2 minutes, followed by a CRI of 1.5‐5.0 μg/kg/min) or nitroprusside (0.5‐3.5 μg/kg/min IV CRI), although none of these medications has the advantage of renal vasodilatation. Phentolamine, a short‐acting competitive α‐adrenergic blocking drug anecdotally has been used successfully to manage intraoperative hypertension that may occur during removal of pheochromocytomas (loading dose, 0.1 mg/kg IV; CRI, 1 to 2 μg/kg/min).190 In cats, even anecdotal information regarding the use of parenterally administered vasodilators is sparse. Subcutaneous administration of hydralazine (1.0‐2.5 mg per cat SC) has been used to treat acute hypertension in postoperative feline renal transplant patients.98 In all cases of parenteral vasodilator administration, continuous or frequent monitoring of BP is required to ensure that adequate BP reductions are achieved, and to avoid hypotension. Orally administered medications can be started when BP has been controlled for 12‐24 hours, and parenteral medication can be titrated down as PO medication takes effect. In cases in which recommended parenteral medications are not available, and the patient can take PO medication, PO amlodipine or hydralazine may be administered as outlined below.
Patients with markedly increased SBP (≥180 mm Hg) but without evidence of acute TOD may be treated with PO medication. Preferred medications have a rapid onset of action when administered PO and decrease BP regardless of primary disease. Hydralazine (0.5‐2 mg/kg PO q12h) has a rapid onset of action and can be used for rapid reduction of BP in both cats and dogs. Amlodipine besylate can be administered at a dosage of 0.2‐0.4 mg/kg PO q24h; dosages up to 0.6 mg/kg PO q24h may be employed cautiously. Many clinicians prefer PO CCB such as amodipine, particularly in cats, because these agents have limited risk of causing hypotension.
9. CONCLUSION
Despite more than a decade since the original ACVIM consensus statement on the management of hypertension, our understanding of the pathophysiology, measurement, and treatment of systemic hypertension in companion animals continues to evolve. Substantial gaps in our knowledge remain.
To bridge these gaps, we recommend large multicenter clinical studies aimed at refining our understanding of normal BP and how it is best assessed. In addition, long‐term studies are necessary to determine the best approach to hypertension treatment, and how these treatments will affect patient quality of life and life expectancy of our patients. We hope this document will be updated periodically to reflect advances in the field of veterinary medicine.
CONFLICT OF INTEREST DECLARATION
Mark Acierno: Consultant for Boehringer Ingelheim. Research support from SunTech.
Scott Brown: Consultant for and grant support from Boehringer Ingelheim and Elanco.
Amanda Coleman: Consultant for and grant support from Boehringer Ingelheim.
Rosanne E. Jepson: Consultant and grant support from with Boehringer Ingelheim, Merial and Ceva.
Mark Papich: Support and consulting from Zoetis. Consulting activity for Elanco, Merck, and Dechra.
Rebecca Stepien: Consultant for Boehringer Ingelheim and Ceva.
Harriet Syme: Consultant and grant support from Boehringer Ingelheim, Elanco, MSD, Ceva, Merial.
ACKNOWLEDGMENTS
The authors acknowledge the authors of the 2007 ACVIM consensus statement on hypertension who provided the foundation for this document. Portions of this article were presented at the 2017 ACVIM Forum, National Harbor, MD.
OFF‐LABEL ANTIMICROBIAL DECLARATION
Authors declare no off‐label use of antimicrobials.
INSTITUTIONAL ANIMAL CARE AND USE COMMITTEE (IACUC) OR OTHER APPROVAL DECLARATION
Authors declare no IACUC or other approval was needed.
Acierno MJ, Brown S, Coleman AE, et al. ACVIM consensus statement: Guidelines for the identification, evaluation, and management of systemic hypertension in dogs and cats. J Vet Intern Med. 2018;32:1803–1822. 10.1111/jvim.15331
Consensus Statements of the American College of Veterinary Internal Medicine (ACVIM) provide the veterinary community with up‐to‐date information on the pathophysiology, diagnosis, and treatment of clinically important animal diseases. The ACVIM Board of Regents oversees selection of relevant topics, identification of panel members with the expertise to draft the statements, and other aspects of assuring the integrity of the process. The statements are derived from evidence‐based medicine whenever possible and the panel offers interpretive comments when such evidence is inadequate or contradictory. A draft is prepared by the panel, followed by solicitation of input by the ACVIM membership which may be incorporated into the statement. It is then submitted to the Journal of Veterinary Internal Medicine, where it is edited before publication. The authors are solely responsible for the content of the statements.
REFERENCES
- 1. Binns SH, Sisson DD, Buoscio DA, Schaeffer DJ. Doppler ultrasonographic, oscillometric sphygmomanometric, and photoplethysmographic techniques for noninvasive blood pressure measurement in anesthetized cats. J Vet Intern Med. 1995;32:1803‐1822. [DOI] [PubMed] [Google Scholar]
- 2. Garner D, Laks MM. New implanted chronic catheter device for determining blood pressure and cardiac output in conscious dog. Am J Physiol. 1985;249:H681‐H684. [DOI] [PubMed] [Google Scholar]
- 3. Scully P, Chan PS, Cervoni P. A method of measuring direct arterial blood pressure. Canine Pract. 1983;10:24‐33. [Google Scholar]
- 4. Kobayashi DL, Peterson ME, Graves TK, Nichols CE, Lesser M. Hypertension in cats with chronic renal failure or hyperthyroidism. J Vet Intern Med. 1990;4:58‐62. [DOI] [PubMed] [Google Scholar]
- 5. Stepien RL, Rapoport GS, Henik RA, Wenholz L, Thomas CB. Comparative diagnostic test characteristics of oscillometric and Doppler ultrasonographic methods in the detection of systolic hypertension in dogs. J Vet Intern Med. 2003;17:65‐72. [DOI] [PubMed] [Google Scholar]
- 6.Coulter DB, Keith JC Jr. Blood pressures obtained by indirect measurement in conscious dogs. J Am Vet Med Assoc 1984;184:1375–1378. [PubMed] [Google Scholar]
- 7. Prisant LM, Alpert BS, Robbins CB, et al. American National Standard for nonautomated sphygmomanometers. Summary report. Am J Hypertens. 1995;8:210‐213. [DOI] [PubMed] [Google Scholar]
- 8. Brown S, Atkins C, Bagley R, et al. Guidelines for the identification, evaluation, and management of systemic hypertension in dogs and cats. J Vet Intern Med. 2007;21:542‐558. [DOI] [PubMed] [Google Scholar]
- 9. Vachon C, Belanger MC, Burns PM. Evaluation of oscillometric and Doppler ultrasonic devices for blood pressure measurements in anesthetized and conscious dogs. Res Vet Sci. 2014;97:111‐117. [DOI] [PubMed] [Google Scholar]
- 10. Martel E, Egner B, Brown SA, et al. Comparison of high‐definition oscillometry—a non‐invasive technology for arterial blood pressure measurement—with a direct invasive method using radio‐telemetry in awake healthy cats. J Feline Med Surg. 2013;15:1104‐1113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bosiack AP, Mann FA, Dodam JR, Wagner‐Mann CC, Branson KR. Comparison of ultrasonic Doppler flow monitor, oscillometric, and direct arterial blood pressure measurements in ill dogs. J Vet Emerg Crit Care (San Antonio). 2010;20:207‐215. [DOI] [PubMed] [Google Scholar]
- 12. Haberman CE, Kang CW, Morgan JD, Brown SA. Evaluation of oscillometric and Doppler ultrasonic methods of indirect blood pressure estimation in conscious dogs. Can J Vet Res. 2006;70:211‐217. [PMC free article] [PubMed] [Google Scholar]
- 13. Jepson RE, Elliott J, Brodbelt D, Syme HM. Effect of control of systolic blood pressure on survival in cats with systemic hypertension. J Vet Intern Med. 2007;21:402‐409. [DOI] [PubMed] [Google Scholar]
- 14. Jacob F, Polzin DJ, Osborne CA, et al. Association between initial systolic blood pressure and risk of developing a uremic crisis or of dying in dogs with chronic renal failure. J Am Vet Med Assoc. 2003;222:322‐329. [DOI] [PubMed] [Google Scholar]
- 15. Gouni V, Tissier R, Misbach C, et al. Influence of the observer's level of experience on systolic and diastolic arterial blood pressure measurements using Doppler ultrasonography in healthy conscious cats. J Feline Med Surg. 2015;17:94‐100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Belew AM, Barlett T, Brown SA. Evaluation of the white‐coat effect in cats. J Vet Intern Med. 1999;13:134‐142. [DOI] [PubMed] [Google Scholar]
- 17. Marino CL, Cober RE, Iazbik MC, Couto CG. White‐coat effect on systemic blood pressure in retired racing greyhounds. J Vet Intern Med. 2011;25:861‐865. [DOI] [PubMed] [Google Scholar]
- 18. Williams TL, Elliott J, Syme HM. Measurement of systolic blood pressure (SBP) in cats by the indirect Doppler technique is not altered by the use of headphones. ECVIM Congress 2010.
- 19. Safar M. Ageing and its effects on the cardiovascular system. Drugs. 1990;39(Suppl 1):1‐8. [DOI] [PubMed] [Google Scholar]
- 20. Bodey AR, Michell AR. Epidemiological study of blood pressure in domestic dogs. J Small Anim Pract. 1996;37:116‐125. [DOI] [PubMed] [Google Scholar]
- 21. Bright JM, Dentino M. Indirect arterial blood pressure measurement in nonsedated Irish wolfhounds: reference values for the breed. J Am Anim Hosp Assoc. 2002;38:521‐526. [DOI] [PubMed] [Google Scholar]
- 22. Remillard RL, Ross JN, Eddy JB. Variance of indirect blood pressure measurements and prevalence of hypertension in clinically normal dogs. Am J Vet Res. 1991;52:561‐565. [PubMed] [Google Scholar]
- 23. Meurs KM, Miller MW, Slater MR, Glaze K. Arterial blood pressure measurement in a population of healthy geriatric dogs. J Am Anim Hosp Assoc. 2000;36:497‐500. [DOI] [PubMed] [Google Scholar]
- 24. Bodey AR, Sansom J. Epidemiological study of blood pressure in domestic cats. J Small Anim Pract. 1998;39:567‐573. [DOI] [PubMed] [Google Scholar]
- 25. Sparkes AH, Caney SM, King MC, Gruffydd‐Jones TJ. Inter‐ and intraindividual variation in Doppler ultrasonic indirect blood pressure measurements in healthy cats. J Vet Intern Med. 1999;13:314‐318. [DOI] [PubMed] [Google Scholar]
- 26. Mishina M, Watanabe T, Fujii K, et al. Non‐invasive blood pressure measurements in cats: clinical significance of hypertension associated with chronic renal failure. J Vet Med Sci. 1998;60:805‐808. [DOI] [PubMed] [Google Scholar]
- 27. Bijsmans ES, Jepson RE, Chang YM, Syme HM, Elliott J. Changes in systolic blood pressure over time in healthy cats and cats with chronic kidney disease. J Vet Intern Med. 2015;29:855‐861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Payne JR, Brodbelt DC, Luis FV. Blood pressure measurements in 780 apparently healthy cats. J Vet Intern Med. 2017;31:15‐21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Surman S, Couto CG, Dibartola SP, et al. Arterial blood pressure, proteinuria, and renal histopathology in clinically healthy retired racing greyhounds. J Vet Intern Med. 2012;26:1320‐1329. [DOI] [PubMed] [Google Scholar]
- 30. Perez‐Sanchez AP, Del‐Angel‐Caraza J, Quijano‐Hernandez IA, et al. Obesity‐hypertension and its relation to other diseases in dogs. Vet Res Commun. 2015;39:45‐51. [DOI] [PubMed] [Google Scholar]
- 31. Schneider HP, Truex RC, Knowles JO. Comparative observations of the hearts of mongrel and greyhound dogs. Anat Rec. 1964;149:173‐179. [DOI] [PubMed] [Google Scholar]
- 32. Cox RH, Peterson LH, Detweiler DK. Comparison of arterial hemodynamics in the mongrel dog and the racing greyhound. Am J Physiol. 1976;230:211‐218. [DOI] [PubMed] [Google Scholar]
- 33. Rattez EP, Reynolds BS, Concordet D, et al. Within‐day and between‐day variability of blood pressure measurement in healthy conscious beagle dogs using a new oscillometric device. J Vet Cardiol. 2010;12:35‐40. [DOI] [PubMed] [Google Scholar]
- 34. Schellenberg S, Glaus TM, Reusch CE. Effect of long‐term adaptation on indirect measurements of systolic blood pressure in conscious untrained beagles. Vet Rec. 2007;161:418‐421. [DOI] [PubMed] [Google Scholar]
- 35. Chetboul V, Tissier R, Gouni V, et al. Comparison of Doppler ultrasonography and high‐definition oscillometry for blood pressure measurements in healthy awake dogs. Am J Vet Res. 2010;71:766‐772. [DOI] [PubMed] [Google Scholar]
- 36. Hoglund K, Hanas S, Carnabuci C, et al. Blood pressure, heart rate, and urinary catecholamines in healthy dogs subjected to different clinical settings. J Vet Intern Med. 2012;26:1300‐1308. [DOI] [PubMed] [Google Scholar]
- 37. Joles JA. Obesity in dogs: effects on renal function, blood pressure, and renal disease. Vet Q. 1998;20:117‐120. [DOI] [PubMed] [Google Scholar]
- 38. Rocchini AP, Yang JQ, Gokee A. Hypertension and insulin resistance are not directly related in obese dogs. Hypertension. 2004;43:1011‐1016. [DOI] [PubMed] [Google Scholar]
- 39. Davy KP, Hall JE. Obesity and hypertension: two epidemics or one? Am J Physiol Regul Integr Comp Physiol. 2004;286:R803‐R813. [DOI] [PubMed] [Google Scholar]
- 40. Dwyer TM, Banks SA, Alonso‐Galicia M, et al. Distribution of renal medullary hyaluronan in lean and obese rabbits. Kidney Int. 2000;58:721‐729. [DOI] [PubMed] [Google Scholar]
- 41. Alonso‐Galicia M, Brands MW, Zappe DH, Hall JE. Hypertension in obese Zucker rats. Role of angiotensin II and adrenergic activity. Hypertension. 1996;28:1047‐1054. [DOI] [PubMed] [Google Scholar]
- 42. Montoya JA, Morrios PJ, Bautista I, et al. Hypertension: a risk factor associated with weight status in dogs. J Nutr. 2006;136:2011S‐2013S. [DOI] [PubMed] [Google Scholar]
- 43. Brown SA, Brown CA, Hendi R. Does systemic hypertension damage the canine kidney? J Vet Intern Med. 2000;14:351A. [Google Scholar]
- 44. Whittemore JC, Nystrom MR, Mawby DI. Effects of various factors on Doppler ultrasonographic measurements of radial and coccygeal arterial blood pressure in privately owned, conscious cats. J Am Vet Med Assoc. 2017;250:763‐769. [DOI] [PubMed] [Google Scholar]
- 45. Mooney AP, Mawby DI, Price JM, Whittemore JC. Effects of various factors on Doppler flow ultrasonic radial and coccygeal artery systolic blood pressure measurements in privately‐owned, conscious dogs. PeerJ. 2017;5:e3101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Rondeau DA, Mackalonis ME, Hess RS. Effect of body position on indirect measurement of systolic arterial blood pressure in dogs. J Am Vet Med Assoc. 2013;242:1523‐1527. [DOI] [PubMed] [Google Scholar]
- 47. Scansen BA, Vitt J, Chew DJ, Schober KE, Bonagura JD. Comparison of forelimb and hindlimb systolic blood pressures and proteinuria in healthy Shetland sheepdogs. J Vet Intern Med. 2014;28:277‐283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Syme HM, Barber PJ, Markwell PJ, Elliott J. Prevalence of systolic hypertension in cats with chronic renal failure at initial evaluation. J Am Vet Med Assoc. 2002;220:1799‐1804. [DOI] [PubMed] [Google Scholar]
- 49. Martin CA, McGrath BP. White‐coat hypertension. Clin Exp Pharmacol Physiol. 2014;41:22‐29. [DOI] [PubMed] [Google Scholar]
- 50. Cuspidi C, Sala C, Grassi G, Mancia G. White coat hypertension: to treat or not to treat? Curr Hypertens Rep. 2016;18:80. [DOI] [PubMed] [Google Scholar]
- 51. Kallet AJ, Cowgill LD, Kass PH. Comparison of blood pressure measurements obtained in dogs by use of indirect oscillometry in a veterinary clinic versus at home. J Am Vet Med Assoc. 1997;210:651‐654. [PubMed] [Google Scholar]
- 52. Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2013;31:1281‐1357. [DOI] [PubMed] [Google Scholar]
- 53. Franklin SS, O'Brien E, Staessen JA. Masked hypertension: understanding its complexity. Eur Heart J. 2016;38(15):1112‐1118. [DOI] [PubMed] [Google Scholar]
- 54. Goy‐Thollot I, Pechereau D, Keroack S, Dezempte JC, Bonnet JM. Investigation of the role of aldosterone in hypertension associated with spontaneous pituitary‐dependent hyperadrenocorticism in dogs. J Small Anim Pract. 2002;43:489‐492. [DOI] [PubMed] [Google Scholar]
- 55. Ortega TM, Feldman EC, Nelson RW, Willits N, Cowgill LD. Systemic arterial blood pressure and urine protein/creatinine ratio in dogs with hyperadrenocorticism. J Am Vet Med Assoc. 1996;209:1724‐1729. [PubMed] [Google Scholar]
- 56. Syme HM, Elliott J. Prevalence of hypertension in hyperthyroid cats at diagnosis and following treatment. J Vet Intern Med. 2003;17:754A. [Google Scholar]
- 57. Syme HM, Elliott J. ECVIM . Prevalence of hypertension in hyper‐ thyroid cats at diagnosis and following treatment [abstract]. Proceedings of the 13th ECVIM‐CA Congress 2003: 754. ECVIM 2003.
- 58. Bovee KC, Littman MP, Saleh F, et al. Essential hereditary hypertension in dogs: a new animal model. J Hypertens Suppl. 1986;4:S172‐S171. [PubMed] [Google Scholar]
- 59. Bovee KC, Littman MP, Crabtree BJ, Aguirre G. Essential hypertension in a dog. J Am Vet Med Assoc. 1989;195:81‐86. [PubMed] [Google Scholar]
- 60. Littman MP, Robertson JL, Bovee KC. Spontaneous systemic hypertension in dogs: five cases (1981‐1983). J Am Vet Med Assoc. 1988;193:486‐494. [PubMed] [Google Scholar]
- 61. Slaughter JB 2nd, Padgett GA, Blanchard G, et al. Canine essential hypertension: probable mode of inheritance. J Hypertens Suppl. 1986;4:S170‐S171. [PubMed] [Google Scholar]
- 62. Tippett FE, Padgett GA, Eyster G, Blanchard G, Bell T. Primary hypertension in a colony of dogs. Hypertension. 1987;9:49‐58. [DOI] [PubMed] [Google Scholar]
- 63. Maggio F, DeFrancesco TC, Atkins CE, et al. Ocular lesions associated with systemic hypertension in cats: 69 cases (1985‐1998). J Am Vet Med Assoc. 2000;217:695‐702. [DOI] [PubMed] [Google Scholar]
- 64. Elliott J, Barber PJ, Syme HM, Rawlings JM, Markwell PJ. Feline hypertension: clinical findings and response to antihypertensive treatment in 30 cases. J Small Anim Pract. 2001;42:122‐129. [DOI] [PubMed] [Google Scholar]
- 65. Jepson RE, Brodbelt D, Vallance C, Syme HM, Elliott J. Evaluation of predictors of the development of azotemia in cats. J Vet Intern Med. 2009;23:806‐813. [DOI] [PubMed] [Google Scholar]
- 66. Bakris GL. Microalbuminuria: what is it? Why is it important? What should be done about it? J Clin Hypertens (Greenwich). 2001;3:99‐102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Palatini P. Microalbuminuria in hypertension. Curr Hypertens Rep. 2003;5:208‐214. [DOI] [PubMed] [Google Scholar]
- 68. Cortadellas O, del Palacio MJ, Bayon A, et al. Systemic hypertension in dogs with leishmaniasis: prevalence and clinical consequences. J Vet Intern Med. 2006;20:941‐947. [DOI] [PubMed] [Google Scholar]
- 69. Bacic A, Kogika MM, Barbaro KC, Iuamoto CS, Simões DMN, Santoro ML. Evaluation of albuminuria and its relationship with blood pressure in dogs with chronic kidney disease. Vet Clin Pathol. 2010;39:203‐209. [DOI] [PubMed] [Google Scholar]
- 70. Syme HM, Markwell PJ, Pfeiffer D, Elliott J. Survival of cats with naturally occurring chronic renal failure is related to severity of proteinuria. J Vet Intern Med. 2006;20:528‐535. [DOI] [PubMed] [Google Scholar]
- 71. Chakrabarti S, Syme HM, Brown CA, Elliott J. Histomorphometry of feline chronic kidney disease and correlation with markers of renal dysfunction. Vet Pathol. 2013;50:147‐155. [DOI] [PubMed] [Google Scholar]
- 72. King JN, Gunn‐Moore DA, Tasker S, Gleadhill A, Strehlau G, Benazepril in Renal Insufficiency in Cats Study Group . Tolerability and efficacy of benazepril in cats with chronic kidney disease. J Vet Intern Med. 2006;20:1054‐1064. [DOI] [PubMed] [Google Scholar]
- 73. Sent U, Gossl R, Elliott J, et al. Comparison of efficacy of long‐term oral treatment with telmisartan and benazepril in cats with chronic kidney disease. J Vet Intern Med. 2015;29:1479‐1487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Chakrabarti S, Syme HM, Elliott J. Clinicopathological variables predicting progression of azotemia in cats with chronic kidney disease. J Vet Intern Med. 2012;26:275‐281. [DOI] [PubMed] [Google Scholar]
- 75. Mathur S, Syme H, Brown CA, et al. Effects of the calcium channel antagonist amlodipine in cats with surgically induced hypertensive renal insufficiency. Am J Vet Res. 2002;63:833‐839. [DOI] [PubMed] [Google Scholar]
- 76. McLeland SM, Cianciolo RE, Duncan CG, et al. A comparison of biochemical and histopathologic staging in cats with chronic kidney disease. Vet Pathol. 2015;52:524‐534. [DOI] [PubMed] [Google Scholar]
- 77. Wehner A, Hartmann K, Hirschberger J. Associations between proteinuria, systemic hypertension and glomerular filtration rate in dogs with renal and non‐renal diseases. Vet Rec. 2008;162:141‐147. [DOI] [PubMed] [Google Scholar]
- 78. Finco DR. Association of systemic hypertension with renal injury in dogs with induced renal failure. J Vet Intern Med. 2004;18:289‐294. [DOI] [PubMed] [Google Scholar]
- 79. Braga ET, Leite JH, Rosa FA, et al. Hypertension and its correlation with renal lesions in dogs with leishmaniosis. Rev Bras Parasitol Vet. 2015;24:45‐51. [DOI] [PubMed] [Google Scholar]
- 80. Michell AR, Bodey AR, Gleadhill A. Absence of hypertension in dogs with renal insufficiency. Ren Fail. 1997;19:61‐68. [DOI] [PubMed] [Google Scholar]
- 81. Cortadellas O, del Palacio MJ, Bayon A, et al. Systemic hypertension in dogs with leishmaniasis: prevalence and clinical consequences. J Vet Intern Med. 2006;20:941‐947. [DOI] [PubMed] [Google Scholar]
- 82. Chetboul V, Lefebvre HP, Pinhas C, Clerc B, Boussouf M, Pouchelon JL. Spontaneous feline hypertension: clinical and echocardiographic abnormalities, and survival rate. J Vet Intern Med. 2003;17:89‐95. [DOI] [PubMed] [Google Scholar]
- 83. Van Boxtel SA. Hypertensive retinopathy in a cat. Can Vet J. 2003;44:147‐149. [PMC free article] [PubMed] [Google Scholar]
- 84. Turner JL, Brogdon JD, Lees GE, et al. Idiopathic hypertension in a cat with secondary hypertensive retinopathy associated with a high‐salt diet. J Am Anim Hosp Assoc. 1990;26:647‐651. [Google Scholar]
- 85. Stiles J, Polzin DJ, Bistner SI. The prevalence of retinopathy in cats with systemic hypertension and chronic renal failure or hyperthyroidism. J Am Anim Hosp Assoc. 1994;30:564‐572. [Google Scholar]
- 86. Sansom J, Rogers K, Wood JL. Blood pressure assessment in healthy cats and cats with hypertensive retinopathy. Am J Vet Res. 2004;65:245‐252. [DOI] [PubMed] [Google Scholar]
- 87. Komaromy AM, Andrew SE, Denis HM, Brooks DE, Gelatt KN. Hypertensive retinopathy and choroidopathy in a cat. Vet Ophthalmol. 2004;7:3‐9. [DOI] [PubMed] [Google Scholar]
- 88. van de Sandt RR, Stades FC, Boeve MH, et al. Arterial hypertension in the cat. A pathobiologic and clinical review with emphasis on the ophthalmologic aspects. Tijdschr Diergeneeskd. 2003;128:2‐10. [PubMed] [Google Scholar]
- 89. Carter JM, Irving AC, Bridges JP, Jones BR. The prevalence of ocular lesions associated with hypertension in a population of geriatric cats in Auckland, New Zealand. N Z Vet J. 2014;62:21‐29. [DOI] [PubMed] [Google Scholar]
- 90. Sansom J, Bodey A. Ocular signs in four dogs with hypertension. Vet Rec. 1997;140:593‐598. [DOI] [PubMed] [Google Scholar]
- 91. Crispin SM, Mould JR. Systemic hypertensive disease and the feline fundus. Vet Ophthalmol. 2001;4:131‐140. [DOI] [PubMed] [Google Scholar]
- 92. Leblanc NL, Stepien RL, Bentley E. Ocular lesions associated with systemic hypertension in dogs: 65 cases (2005‐2007). J Am Vet Med Assoc. 2011;238:915‐921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Morgan RV. Systemic hypertension in four cats: ocular and medical findings. J Am Anim Hosp Assoc. 1986;22:615‐621. [Google Scholar]
- 94. Littman MP. Spontaneous systemic hypertension in 24 cats. J Vet Intern Med. 1994;8:79‐86. [DOI] [PubMed] [Google Scholar]
- 95. Sansom J, Barnett K, Dunn K, et al. Ocular disease associated with hypertension in 16 cats. J Small Anim Pract. 1994;35:604‐611. [Google Scholar]
- 96. Henik RA. Diagnosis and treatment of feline systemic hypertension. Compendium. 1997;19:163‐178. [Google Scholar]
- 97. Bagley RS. The brain as a target organ In: Egner B, Carr A, Brown S, eds. Essential Facts of Blood Pressure in Dogs and Cats. Babenhausen, Germany: Vet Verlag; 2003:129‐139. [Google Scholar]
- 98. Kyles AE, Gregory CR, Wooldridge JD, et al. Management of hypertension controls postoperative neurologic disorders after renal transplantation in cats. Vet Surg. 1999;28:436‐441. [DOI] [PubMed] [Google Scholar]
- 99. Kletzmayr J, Uffmann M, Schmaldienst S. Severe but reversible hypertensive encephalopathy. Wien Klin Wochenschr. 2003;115:416. [DOI] [PubMed] [Google Scholar]
- 100. Schwartz RB. Hyperperfusion encephalopathies: hypertensive encephalopathy and related conditions. Neurologist. 2002;8:22‐34. [DOI] [PubMed] [Google Scholar]
- 101. Tejani A. Post‐transplant hypertension and hypertensive encephalopathy in renal allograft recipients. Nephron. 1983;34:73‐78. [DOI] [PubMed] [Google Scholar]
- 102. Mathews KG, Gregory CR. Renal transplants in cats: 66 cases (1987‐1996). J Am Vet Med Assoc. 1997;211:1432‐1436. [PubMed] [Google Scholar]
- 103. Gregory CR, Mathews KG, Aronson LR, et al. Central nervous system disorders after renal transplantation in cats. Vet Surg. 1997;26:386‐392. [DOI] [PubMed] [Google Scholar]
- 104. Manolio TA, Olson J, Longstreth WT. Hypertension and cognitive function: pathophysiologic effects of hypertension on the brain. Curr Hypertens Rep. 2003;5:255‐261. [DOI] [PubMed] [Google Scholar]
- 105. Lowrie M, De Risio L, Dennis R, et al. Concurrent medical conditions and long‐term outcome in dogs with nontraumatic intracranial hemorrhage. Vet Radiol Ultrasound. 2012;53:381‐388. [DOI] [PubMed] [Google Scholar]
- 106. O'Neill J, Kent M, Glass EN, Platt SR. Clinicopathologic and MRI characteristics of presumptive hypertensive encephalopathy in two cats and two dogs. J Am Anim Hosp Assoc. 2013;49:412‐420. [DOI] [PubMed] [Google Scholar]
- 107. Simpson KM, De Risio L, Theobald A, et al. Feline ischaemic myelopathy with a predilection for the cranial cervical spinal cord in older cats. J Feline Med Surg. 2014;16:1001‐1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Misbach C, Gouni V, Tissier R, et al. Echocardiographic and tissue Doppler imaging alterations associated with spontaneous canine systemic hypertension. J Vet Intern Med. 2011;25:1025‐1035. [DOI] [PubMed] [Google Scholar]
- 109. Littman MP, Drobatz KJ. Hypertensive and hypotensive disorders In: Ettinger SJ, ed. Textbook of Veterinary Internal Medicine. Philadelphia, PA: W.B. Saunders; 1995:93‐100. [Google Scholar]
- 110. Lesser M, Fox PR, Bond BR. Assessment of hypertension in 40 cats with left ventricular hypertrophy by Doppler‐shift sphygmomanometry. J Small Anim Pract. 1992;33:55‐58. [Google Scholar]
- 111. Sennello KA, Schulman RL, Prosek R, Siegel AM. Systolic blood pressure in cats with diabetes mellitus. J Am Vet Med Assoc. 2003;223:198‐201. [DOI] [PubMed] [Google Scholar]
- 112. Henik RA, Stepien RL, Bortnowski HB. Spectrum of m‐mode echocardiographic abnormalities in 75 cats with systemic hypertension. J Am Anim Hosp Assoc. 2004;40:359‐363. [DOI] [PubMed] [Google Scholar]
- 113. Carlos Sampedrano C, Chetboul V, Gouni V, et al. Systolic and diastolic myocardial dysfunction in cats with hypertrophic cardiomyopathy or systemic hypertension. J Vet Intern Med. 2006;20:1106‐1115. [DOI] [PubMed] [Google Scholar]
- 114. Snyder PS, Sadek D, Jones GL. Effect of amlodipine on echocardiographic variables in cats with systemic hypertension. J Vet Intern Med. 2001;15:52‐56. [DOI] [PubMed] [Google Scholar]
- 115. Wey AC, Atkins CE. Aortic dissection and congestive heart failure associated with systemic hypertension in a cat. J Vet Intern Med. 2000;14:208‐213. [PubMed] [Google Scholar]
- 116. Collins AJ, Li S, Gilbertson DT, Liu J, Chen SC, Herzog CA. Chronic kidney disease and cardiovascular disease in the Medicare population. Kidney Int Suppl. 2003;64:S24‐S31. [DOI] [PubMed] [Google Scholar]
- 117. Bissett SA, Drobatz KJ, McKnight A, Degernes LA. Prevalence, clinical features, and causes of epistaxis in dogs: 176 cases (1996–2001). J Am Vet Med Assoc. 2007;231:1843‐1850. [DOI] [PubMed] [Google Scholar]
- 118. Mylonakis ME, Saridomichelakis MN, Lazaridis V, Leontides LS, Kostoulas P, Koutinas AF. A retrospective study of 61 cases of spontaneous canine epistaxis (1998 to 2001). J Small Anim Pract. 2008;49:191‐196. [DOI] [PubMed] [Google Scholar]
- 119. Strasser JL, Hawkins EC. Clinical features of epistaxis in dogs: a retrospective study of 35 cases (1999‐2002). J Am Anim Hosp Assoc. 2005;41:179‐184. [DOI] [PubMed] [Google Scholar]
- 120. Scollan K, Sisson D. Multi‐detector computed tomography of an aortic dissection in a cat. J Vet Cardiol. 2014;16:67‐72. [DOI] [PubMed] [Google Scholar]
- 121. Waldrop JE, Stoneham AE, Tidwell AS, Jakowski RM, Rozanski EA, Rush JE. Aortic dissection associated with aortic aneurysms and posterior paresis in a dog. J Vet Intern Med. 2003;17:223‐229. [PubMed] [Google Scholar]
- 122. Bijsmans ES, Jepson RE, Chang YM, Syme HM, Elliott J. Changes in systolic blood pressure over time in healthy cats and cats with chronic kidney disease. J Vet Intern Med. 2015;29:855‐861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. McCubbin JW, Corcoran AC. Arterial pressures in street dogs: incidence and significance of hypertension. Proc Soc Exp Biol Med. 1953;84:130‐131. [DOI] [PubMed] [Google Scholar]
- 124. Katz JI, Skom JH, Walkerlin GE. Pathogenesis of spontaneous and pyelonephritic hypertension in the dog. Circ Res. 1954;5:137‐143. [DOI] [PubMed] [Google Scholar]
- 125. Hamilton WF, Pund ER, Slaughter RF, et al. Blood pressure values in street dogs. Am J Physiol. 1940;128:233‐237. [Google Scholar]
- 126. Scansen BA, Vitt J, Chew D, et al. Comparison of forelimb and hindlimb systolic blood pressures and proteinuria in healthy Shetland sheepdogs. J Vet Intern Med. 2014;28:277‐283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127. Michell AR. Salt, hypertension and renal disease: comparative medicine, models and real diseases. Postgrad Med J. 1994;70:686‐694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Bodey AR, Rampling MW. Comparison of haemorrheological parameters and blood pressure in various breeds of dog. J Small Anim Pract. 1999;40:3‐6. [DOI] [PubMed] [Google Scholar]
- 129.IRIS. 4. Treatment Recommendations for CKD in Dogs 2015.
- 130. Greco DS, Lees GE, Dzendzel G, Carter AB. Effects of dietary sodium intake on blood pressure measurements in partially nephrectomized dogs. Am J Vet Res. 1994;55:160‐165. [PubMed] [Google Scholar]
- 131. Buranakarl C, Mathur S, Brown SA. Effects of dietary sodium chloride intake on renal function and blood pressure in cats with normal and reduced renal function. Am J Vet Res. 2004;65:620‐627. [DOI] [PubMed] [Google Scholar]
- 132. Hansen B, DiBartola SP, Chew DJ, Brownie C, Nagode L. Clinical and metabolic findings in dogs with chronic renal failure fed two diets. Am J Vet Res. 1992;53:326‐334. [PubMed] [Google Scholar]
- 133. Chetboul V, Reynolds BS, Trehiou‐Sechi E, et al. Cardiovascular effects of dietary salt intake in aged healthy cats: a 2‐year prospective randomized, blinded, and controlled study. PLoS One. 2014;9:e97862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134. Reynolds BS, Chetboul V, Nguyen P, et al. Effects of dietary salt intake on renal function: a 2‐year study in healthy aged cats. J Vet Intern Med. 2013;27:507‐515. [DOI] [PubMed] [Google Scholar]
- 135. Hall JE, Guyton AC, Smith MJ Jr, Coleman TG. Long‐term regulation of arterial pressure, glomerular filtration and renal sodium reabsorption by angiotensin II in dogs. Clin Sci (Lond). 1980;59(Suppl 6):87s‐90s. [DOI] [PubMed] [Google Scholar]
- 136. Allen TJ, Waldron MJ, Casley D, Jerums G, Cooper ME. Salt restriction reduces hyperfiltration, renal enlargement, and albminuria in experimental diabetes. Diabetes. 1997;46:119‐124. [DOI] [PubMed] [Google Scholar]
- 137. Coleman TG, Guyton AC. Hypertension caused by salt loading in the dog. 3. Onset transients of cardiac output and other circulatory variables. Circ Res. 1969;25:153‐160. [DOI] [PubMed] [Google Scholar]
- 138. Grauer G, Greco D, Gretzy D, et al. Effects of enalapril treatment versus placebo as a treatment for canine idiopathic glomerulonephritis. J Vet Intern Med. 2000;14:526‐533. [DOI] [PubMed] [Google Scholar]
- 139. Brown SA, Finco DR, Brown CA, et al. Evaluation of the effects of inhibition of angiotensin converting enzyme with enalapril in dogs with induced chronic renal insufficiency. Am J Vet Res. 2003;64:321‐327. [DOI] [PubMed] [Google Scholar]
- 140. Brown SA, Walton CL, Crawford P, Bakris GL. Long‐term effects of antihypertensive regimens on renal hemodynamics and proteinuria. Kidney Int. 1993;43:1210‐1218. [DOI] [PubMed] [Google Scholar]
- 141. Gaber L, Walton C, Brown S, Bakris G. Effects of different antihypertensive treatments on morphologic progression of diabetic nephropathy in uninephrectomized dogs. Kidney Int. 1994;46:161‐169. [DOI] [PubMed] [Google Scholar]
- 142. Brown S. Introduction from the international renal interest society. J Vet Intern Med. 2013;27(Suppl 1):S1. [DOI] [PubMed] [Google Scholar]
- 143. Taugner F, Baatz G, Nobiling R. The renin‐angiotensin system in cats with chronic renal failure. J Comp Pathol. 1996;115:239‐252. [DOI] [PubMed] [Google Scholar]
- 144. Steele JL, Henik RA, Stepien RL. Effects of angiotensin‐converting enzyme inhibition on plasma aldosterone concentration, plasma renin activity, and blood pressure in spontaneously hypertensive cats with chronic renal disease. Vet Ther. 2002;3:157‐166. [PubMed] [Google Scholar]
- 145. Jensen J, Henik RA, Brownfield M, Armstrong J. Plasma renin activity and angiotensin I and aldosterone concentrations in cats with hypertension associated with chronic renal disease. Am J Vet Res. 1997;58:535‐540. [PubMed] [Google Scholar]
- 146. Miller RH, Lehmkuhl LB, Smeak DD, DiBartola S, Radin J. Effect of enalapril on blood pressure, renal function, and the renin‐angiotensin‐aldosterone system in cats with autosomal dominant polycystic kidney disease. Am J Vet Res. 1999;60:1516‐1525. [PubMed] [Google Scholar]
- 147. Pedersen KM, Pedersen HD, Haggstrom J, Koch J, Ersbøll AK. Increased mean arterial pressure and aldosterone‐to‐renin ratio in Persian cats with polycystic kidney disease. J Vet Intern Med. 2003;17:21‐27. [PubMed] [Google Scholar]
- 148. Jepson RE, Syme HM, Elliott J. Plasma renin activity and aldosterone concentrations in hypertensive cats with and without azotemia and in response to treatment with amlodipine besylate. J Vet Intern Med. 2014;28:144‐153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149. Henik RA, Snyder PS, Volk LM. Treatment of systemic hypertension in cats with amlodipine besylate. J Am Anim Hosp Assoc. 1997;33:226‐234. [DOI] [PubMed] [Google Scholar]
- 150. Snyder PS. Amlodipine: a randomized, blinded clinical trial in 9 cats with systemic hypertension. J Vet Intern Med. 1998;12:157‐162. [DOI] [PubMed] [Google Scholar]
- 151. Bijsmans ES, Doig M, Jepson RE, et al. Factors influencing the relationship between the dose of amlodipine required for blood pressure control and change in blood pressure in hypertensive cats. J Vet Intern Med. 2016;30:1939‐1676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152. Huhtinen M, Derré G, Renoldi HJ, et al. Randomized placebo‐controlled clinical trial of a chewable formulation of amlodipine for the treatment of hypertension in client‐owned cats. J Vet Intern Med. 2015;29:786‐793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153. Helms SR. Treatment of feline hypertension with transdermal amlodipine: a pilot study. J Am Anim Hosp Assoc. 2007;43:149‐156. [DOI] [PubMed] [Google Scholar]
- 154. Mixon W, Helms SR. Transdermal amlodipine besylate in lipoderm for the treatment of feline hypertension: a report of two cases. Int J Pharm Compd. 2008;12:392‐397. [PubMed] [Google Scholar]
- 155. Creevy KE, Scuderi MA, Ellis AE. Generalised peripheral oedema associated with amlodipine therapy in two dogs. J Small Anim Pract. 2013;54:601‐604. [DOI] [PubMed] [Google Scholar]
- 156. Pariser MS, Berdoulay P. Amlodipine induced gingival hyperplasia in a Great Dane. J Am Anim Hosp Assoc. 2011;47:375‐376. [DOI] [PubMed] [Google Scholar]
- 157. Jepson RE, Elliott J, Brodbelt D, Syme HM. Effect of control of systolic blood pressure on survival in cats with systemic hypertension. J Vet Intern Med. 2007;21:402‐409. [DOI] [PubMed] [Google Scholar]
- 158. Sent U, Gössl R, Elliott J, Syme HM, Zimmering T. Comparison of efficacy of long‐term oral treatment with telmisartan and benazepril in cats with chronic kidney disease. J Vet Intern Med. 2015;29:1479‐1487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159. Elliott J, Fletcher M, Souttar K, et al. Effect of concomitant amlodipine and benazepril therapy in the management of feline hypertension (abstract). J Vet Intern Med. 2004;18:788. [Google Scholar]
- 160. Syme HM, Markwell PJ, Pfeiffer D, Elliott J. Survival of cats with naturally occurring chronic renal failure is related to severity of proteinuria. J Vet Intern Med. 2006;20:528‐535. [DOI] [PubMed] [Google Scholar]
- 161. Chakrabarti S, Syme HM, Elliott J. Clinicopathological variables predicting progression of azotemia in cats with chronic kidney disease. J Vet Intern Med. 2012;26:275‐281. [DOI] [PubMed] [Google Scholar]
- 162. Syme HM. Proteinuria in cats. J Feline Med Surg. 2009;11:211‐218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163. Vaden S, Elliott J. Management of proteinuria in dogs and cats with chronic kidney disease. Vet Clin North Am Small Anim Pract. 2016;46:1115‐1130. [DOI] [PubMed] [Google Scholar]
- 164. Jenkins TL, Coleman AE, Schmiedt CW, Brown SA. Attenuation of the pressor response to exogenous angiotensin by angiotensin receptor blockers and benazepril hydrochloride in clinically normal cats. Am J Vet Res. 2015;76:807‐813. [DOI] [PubMed] [Google Scholar]
- 165. Glaus A, Elliott J, Albrecht B. Efficacy of telmisartan in hypertensive cats: results of a large European Clinical Trial 27th ECVIM‐CA Congress. Malta: John Wiley & Sons, Ltd.; 2017. [Google Scholar]
- 166. Brown SA, Brown CA, Jacobs G, Stiles J, Hendi RS, Wilson S. Effects of the angiotensin converting enzyme inhibitor benazepril in cats with induced renal insufficiency. Am J Vet Res. 2001;62:375‐383. [DOI] [PubMed] [Google Scholar]
- 167. King JN, Gunn‐Moore DA, Tasker S, Gleadhill A, Strehlau G, Benazepril in Renal Insufficiency in Cats Study Group . Tolerability and efficacy of benazepril in cats with chronic kidney disease. J Vet Intern Med. 2006;20:1054‐1064. [DOI] [PubMed] [Google Scholar]
- 168. Mizutani H, Koyama H, Watanabe T, et al. Evaluation of the clinical efficacy of benazepril in the treatment of chronic renal insufficiency in cats. J Vet Intern Med. 2006;20:1074‐1079. [DOI] [PubMed] [Google Scholar]
- 169. Brown SA, Brown CA, Jacobs G, Stiles J, Hendi RS, Wilson S. Effects of the angiotensin converting enzyme inhibitor benazepril in cats with induced renal insufficiency. Am J Vet Res. 2001;62:375‐383. [DOI] [PubMed] [Google Scholar]
- 170. Lavallee JO, Norsworthy GD, Huston CL, Chew DJ. Safety of benazepril in 400 azotemic and 110 non‐azotemic client‐owned cats (2001‐2012). J Am Anim Hosp Assoc. 2017;53:119‐127. [DOI] [PubMed] [Google Scholar]
- 171. Elliott J, Barber PJ, Syme HM, Rawlings JM, Markwell PJ. Feline hypertension: clinical findings and response to antihypertensive treatment in 30 cases. J Small Anim Pract. 2001;42:122‐129. [DOI] [PubMed] [Google Scholar]
- 172. Group CS . Controlled clinical evaluation of enalapril in dogs with heart failure: results of the Cooperative Veterinary Enalapril Study Group. J Vet Intern Med. 1995;9:243‐252. [DOI] [PubMed] [Google Scholar]
- 173. Ettinger SJ, Benitz AM, Ericsson GF, et al. Effects of enalapril maleate on survival of dogs with naturally acquired heart failure. The Long‐Term Investigation of Veterinary Enalapril (LIVE) study group. J Am Vet Med Assoc. 1998;213:1573‐1577. [PubMed] [Google Scholar]
- 174. Henik RA, Stepien RL, Wenholz LJ, Dolson MK. Efficacy of atenolol as a single antihypertensive agent in hyperthyroid cats. J Feline Med Surg. 2008;10:577‐582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175. Kyles AE, Gregory CR, Wooldridge JD, et al. Management of hypertension controls postoperative neurologic disorders after renal transplantation in cats. Vet Surg. 1999;28:436‐441. [DOI] [PubMed] [Google Scholar]
- 176. Schulman RL. Feline primary hyperaldosteronism. Vet Clin North Am Small Anim Pract. 2010;40:353‐359. [DOI] [PubMed] [Google Scholar]
- 177. Ash AR, Harvey AM, Tasker S. Primary hyperaldosteronism in the cat: a series of 13 cases. J Feline Med Surg. 2005;7:173‐182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178. MacDonald KA, Kittleson MD, Kass PH, White SD. Effect of spironolactone on diastolic function and left ventricular mass in Maine Coon cats with familial hypertrophic cardiomyopathy. J Vet Intern Med. 2008;22:335‐341. [DOI] [PubMed] [Google Scholar]
- 179. Calsyn JDR, Green RA, Davis GJ, Reilly CM. Adrenal pheochromocytoma with contralateral adrenocortical adenoma in a cat. J Am Anim Hosp Assoc. 2010;46:36‐42. [DOI] [PubMed] [Google Scholar]
- 180. Henry CJ, Brewer WG, Montgomery RD. Adrenal pheochromocytoma in a cat. J Vet Intern Med. 1993;7:199‐201. [DOI] [PubMed] [Google Scholar]
- 181. Wimpole JA, Adagra CFM, Billson MF, Pillai DN, Foster DJ. Plasma free metanephrines in healthy cats, cats with non‐adrenal disease and a cat with suspected phaeochromocytoma. J Feline Med Surg. 2010;12:435‐440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182. Chun R, Jakovljevic S, Morrison WB. Apocrine gland adenocarcinoma and pheochromocytoma in a cat. J Am Anim Hosp Assoc. 1997;33:33‐36. [DOI] [PubMed] [Google Scholar]
- 183. Elliott WJ. Management of hypertension emergencies. Curr Hypertens Rep. 2003;5:486‐492. [DOI] [PubMed] [Google Scholar]
- 184. Nielsen LK, Bracker K, Price LL. Administration of fenoldopam in critically ill small animal patients with acute kidney injury: 28 dogs and 34 cats (2008‐2012). J Vet Emerg Crit Care (San Antonio). 2015;25:396‐404. [DOI] [PubMed] [Google Scholar]
- 185. Rodriguez MA, Kumar SK, De Caro M. Hypertensive crisis. Cardiol Rev. 2010;18:102‐107. [DOI] [PubMed] [Google Scholar]
- 186. Murphy MB, Murray C, Shorten GD. Fenoldopam: a selective peripheral dopamine‐receptor agonist for the treatment of severe hypertension. N Engl J Med. 2001;345:1548‐1557. [DOI] [PubMed] [Google Scholar]
- 187. Kelly KL, Drobatz KJ, Foster JD. Effect of fenoldopam continuous infusion on glomerular filtration rate and fractional excretion of sodium in healthy dogs. J Vet Intern Med. 2016;30:1655‐1660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188. Simmons JP, Wohl JS, Schwartz DD, Edwards HG, Wright JC. Diuretic effects of fenoldopam in healthy cats. J Vet Emerg Crit Care. 2006;16:96‐103. [Google Scholar]
- 189. Bloom CA, Labato MA, Hazarika S, et al. Preliminary pharmacokinetics and cardiovascular effects of fenoldopam continuous rate infusion in six healthy dogs. J Vet Pharmacol Ther. 2012;35:224‐230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190. Kyles AE, Feldman EC, De Cock HE, et al. Surgical management of adrenal gland tumors with and without associated tumor thrombi in dogs: 40 cases (1994‐2001). J Am Vet Med Assoc. 2003;223:654‐662. [DOI] [PubMed] [Google Scholar]
- 191. Anderson LJ, Fisher EW. The blood pressure in canine interstitial nephritis. Res Vet Sci. 1968;9:304‐313. [PubMed] [Google Scholar]
- 192. Cowgill LD, Kallet AJ. Recognition and management of hypertension in the dog In: Kirk RW, ed. Curent Veterinary Therapy VIII. Philadelphia, PA: W.B. Saunders; 1983:1025‐1028. [Google Scholar]
- 193. Chalifoux A, Dallaire A, Blais D, Larivière N, Pelletier N. Evaluation of the arterial blood pressure of dogs by two noninvasive methods. Can J Comp Med. 1985;49:419‐423. [PMC free article] [PubMed] [Google Scholar]
- 194. Stepien RL, Rapoport GS. Clinical comparison of three methods to measure blood pressure in nonsedated dogs. J Am Vet Med Assoc. 1999;215:1623‐1628. [PubMed] [Google Scholar]
- 195. Brown S, Langford K, Tarver S. Effects of pharmacological agents on diurnal pattern of blood pressure, heart rate, and motor activity in cats. Am J Vet Res. 1997;58:647‐652. [PubMed] [Google Scholar]
- 196. Slingerland LI, Robben JH, Schaafsma I, Kooistra HS. Response of cats to familiar and unfamiliar human contact using continuous direct arterial blood pressure measurement. Res Vet Sci. 2008;85:575‐582. [DOI] [PubMed] [Google Scholar]
- 197. Zwijnenberg RJ, del Rio CL, Cobb RM, Ueyama Y, Muir WW. Evaluation of oscillometric and vascular access port arterial blood pressure measurement techniques versus implanted telemetry in anesthetized cats. Am J Vet Res. 2011;72:1015‐1021. [DOI] [PubMed] [Google Scholar]
- 198. Jenkins TL, Coleman AE, Schmiedt CW, Brown SA. Attenuation of the pressor response to exogenous angiotensin by angiotensin receptor blockers and benazepril hydrochloride in clinically normal cats. Am J Vet Res. 2015;76:807‐813. [DOI] [PubMed] [Google Scholar]
- 199. Lin CH, Yan CJ, Lien YH, et al. Systolic blood pressure of clinically normal and conscious cats determined by an indirect Doppler method in a clinical setting. J Vet Med Sci. 2006;68:827‐832. [DOI] [PubMed] [Google Scholar]
- 200. dos Reis GF, Nogueira RB, Silva AC, et al. Spectral analysis of femoral artery blood flow waveforms of conscious domestic cats. J Feline Med Surg. 2014;16:972‐978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201. Taffin ER, Paepe D, Ghys LF, et al. Systolic blood pressure, routine kidney variables and renal ultrasonographic findings in cats naturally infected with feline immunodeficiency virus. J Feline Med Surg. 2017;19:672‐679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202. Quimby JM, Smith ML, Lunn KF. Evaluation of the effects of hospital visit stress on physiologic parameters in the cat. J Feline Med Surg. 2011;13:733‐737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203. Paige CF, Abbott JA, Elvinger F, Pyle RL. Prevalence of cardiomyopathy in apparently healthy cats. J Am Vet Med Assoc. 2009;234:1398‐1403. [DOI] [PubMed] [Google Scholar]
- 204. Rapoport GS, Stepien RL. Direct arterial blood pressure measurement in 54 dogs presented for systemic hypertension screening 1998‐2001. In: Proc 11th European College of Veterinary Internal Medicine Annual Congress 2001:62.
- 205. Buranakarl C, Ankanaporn K, Thammacharoen S, et al. Relationships between degree of azotaemia and blood pressure, urinary protein:creatinine ratio and fractional excretion of electrolytes in dogs with renal azotaemia. Vet Res Commun 2007;31(3):245–257. [DOI] [PubMed] [Google Scholar]
- 206. O'Neill DG, Elliott J, Church DB, McGreevy PD, Thomson PC, Brodbelt DC. Chronic kidney disease in dogs in UKveterinary practices: prevalence, risk factors, and survival. J Vet Intern Med. 2013;27:814‐821. [DOI] [PubMed] [Google Scholar]
- 207. Francey T, Cowgill LD. Hypertension in dogs with severe acute renal failure. J Vet Intern Med. 2004;18:418(A). [Google Scholar]
- 208. Geigy CA, Schweighauser A, Doherr M, Francey T. Occurrence of systemic hypertension in dogs with acute kidney injury and treatment with amlodipine besylate. J Small Anim Pract. 2011;52:340‐346. [DOI] [PubMed] [Google Scholar]
- 209. Chen HY, Lien YH, Huang HP. Association of renal resistive index, renal pulsatility index, systemic hypertension, and albuminuria with survival in dogs with pituitary‐dependent hyperadrenocorticism. Int J Endocrinol. 2016;2016:3814034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210. Smets PM, Lefebvre HP, Meij BP, et al. Long‐term follow‐up of renal function in dogs after treatment for ACTH‐dependent hyperadrenocorticism. J Vet Intern Med. 2012;26:565‐574. [DOI] [PubMed] [Google Scholar]
- 211. Lien YH, Hsiang TY, Huang HP. Associations among systemic blood pressure, microalbuminuria and albuminuria in dogs affected with pituitary‐ and adrenal‐dependent hyperadrenocorticism. Acta Vet Scand. 2010;52:61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212. Struble AL, Feldman EC, Nelson RW, Kass PH. Systemic hypertension and proteinuria in dogs with diabetes mellitus. J Am Vet Med Assoc. 1998;213:822‐825. [PubMed] [Google Scholar]
- 213. Marynissen SJ, Smets PM, Ghys LF, et al. Long‐term follow‐up of renal function assessing serum cystatin C in dogs with diabetes mellitus or hyperadrenocorticism. Vet Clin Pathol. 2016;45:320‐329. [DOI] [PubMed] [Google Scholar]
- 214. Herring IP, Panciera DL, Werre SR. Longitudinal prevalence of hypertension, proteinuria, and retinopathy in dogs with spontaneous diabetes mellitus. J Vet Intern Med. 2014;28:488‐495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215. Piantedosi D, Di Loria A, Guccione J, et al. Serum biochemistry profile, inflammatory cytokines, adipokines and cardiovascular findings in obese dogs. Vet J. 2016;216:72‐78. [DOI] [PubMed] [Google Scholar]
- 216. Tvarijonaviciute A, Ceron JJ, Holden SL, et al. Obesity‐related metabolic dysfunction in dogs: a comparison with human metabolic syndrome. BMC Vet Res. 2012;8:147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217. Breitschwerdt EB, Meuten DJ, Greenfield CL. Idiopathic hyperaldosteronism in a dog. J Am Vet Med Assoc. 1985;187:841‐845. [PubMed] [Google Scholar]
- 218. Gojska‐Zygner O, Lechowski R, Zygner W. Functioning unilateral adrenocortical carcinoma in a dog. Can Vet J. 2012;53:623‐625. [PMC free article] [PubMed] [Google Scholar]
- 219. Barthez PY, Marks SL, Woo J, Feldman EC, Matteucci M. Pheochromocytoma in dogs: 61 cases (1984‐1995). J Vet Intern Med. 1997;11:272‐278. [DOI] [PubMed] [Google Scholar]
- 220. Gilson SD, Withrow SJ, Wheeler SL, Twedt DC. Pheochromocytoma in 50 dogs. J Vet Intern Med. 1994;8:228‐232. [DOI] [PubMed] [Google Scholar]
- 221. Herrera MA, Mehl ML, Kass PH, Pascoe PJ, Feldman EC, Nelson RW. Predictive factors and the effect of phenoxybenzamine on outcome in dogs undergoing adrenalectomy for pheochromocytoma. J Vet Intern Med. 2008;22:1333‐1339. [DOI] [PubMed] [Google Scholar]
- 222. Gwin RM, Gelatt KN, Terrell TG, et al. Hypertensive retinopathy associated with hypothyroidism, hypercholesterolemia, and renal failure in a dog. J Am Anim Hosp Assoc. 1978;14:200‐209. [Google Scholar]
- 223. Hoareau GL, Jourdan G, Mellema M, Verwaerde P. Evaluation of arterial blood gases and arterial blood pressures in brachycephalic dogs. J Vet Intern Med. 2012;26:897‐904. [DOI] [PubMed] [Google Scholar]
- 224. Sander C, Horauf A, Reusch C. Indirect blood pressure measurement in cats with diabetes mellitus, chronic nephropathy and hypertrophic cardiomyopathy. Tierarztl Prax Ausg K Kleintiere Heimtiere. 1998;26:110‐118. [PubMed] [Google Scholar]
- 225. Al‐Ghazlat SA, Langston CE, Greco DS, et al. The prevalence of microalbuminuria and proteinuria in cats with diabetes mellitus. Top Companion Anim Med. 2011;26:154‐157. [DOI] [PubMed] [Google Scholar]
- 226. Williams TL, Peak KJ, Brodbelt D, Elliott J, Syme HM. Survival and the development of azotemia after treatment of hyperthyroid cats. J Vet Intern Med. 2010;24:863‐869. [DOI] [PubMed] [Google Scholar]
- 227. Morrow LD, Adams VJ, Elliott J et al. Hypertension in hyperthyroid cats: prevalence, incidence and predictors of its development. In: Proceedings of ACVIM forum 2009;699.
- 228. Williams TL, Elliott J, Syme HM. Renin‐angiotensin‐aldosterone system activity in hyperthyroid cats with and without concurrent hypertension. J Vet Intern Med. 2013;27:522‐529. [DOI] [PubMed] [Google Scholar]
- 229. Flood SM, Randolph JF, Gelzer AR, Refsal K. Primary hyperaldosteronism in two cats. J Am Anim Hosp Assoc. 1999;35:411‐416. [DOI] [PubMed] [Google Scholar]
- 230. MacKay AD, Holt PE, Sparkes AH. Successful surgical treatment of a cat with primary aldosteronism. J Feline Med Surg. 1999;1:117‐122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231. Ahn A. Hyperaldosteronism in cats. Semin Vet Med Surg (Small Anim). 1994;9:153‐157. [PubMed] [Google Scholar]
- 232. Rijnberk A, Voorhout G, Kooistra HS, et al. Hyperaldosteronism in a cat with metastasised adrenocortical tumour. Vet Q. 2001;23:38‐43. [DOI] [PubMed] [Google Scholar]
- 233. Eger CE, Robinson WF, Hustable CRR. Primary aldosteronism (Conn's syndrome) in a cat. J Small Anim Pract. 1983;24:293‐307. [Google Scholar]
- 234. Javadi S, Djajadiningrat‐Laanen SC, Kooistra HS, et al. Primary hyperaldosteronism, a mediator of progressive renal disease in cats. Domest Anim Endocrinol. 2005;28:85‐104. [DOI] [PubMed] [Google Scholar]
- 235. Ash RA, Harvey AM, Tasker S. Primary hyperaldosteronism in the cat: a series of 13 cases. J Feline Med Surg. 2005;7:173‐182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236. Henry CJ, Brewer WG, Montgomery RD. Adrenal pheochromocytoma in a cat. J Vet Intern Med. 1993;7:199‐203. [DOI] [PubMed] [Google Scholar]
- 237. Maher ER Jr, McNiel EA. Pheochromocytoma in dogs and cats. Vet Clin North Am Small Anim Pract. 1997;27:359‐380. [DOI] [PubMed] [Google Scholar]
- 238. Valentin SY, Cortright CC, Nelson RW, et al. Clinical findings, diagnostic test results, and treatment outcome in cats with spontaneous hyperadrenocorticism: 30 cases. J Vet Intern Med. 2014;28:481‐487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239. Brown AL, Beatty JA, Lindsay SA, Barrs VR. Severe systemic hypertension in a cat with pituitary‐dependent hyperadrenocorticism. J Small Anim Pract. 2012;53:132‐135. [DOI] [PubMed] [Google Scholar]
- 240. Schellenberg S, Mettler M, Gentilini F, Portmann R, Glaus TM, Reusch CE. The effects of hydrocortisone on systemic arterial blood pressure and urinary protein excretion in dogs. J Vet Intern Med. 2008;22:273‐281. [DOI] [PubMed] [Google Scholar]
- 241. Nakamoto H, Suzuki H, Kageyama Y, et al. Characterization of alterations of hemodynamics and neuroendocrine hormones in dexamethasone induced hypertension in dogs. Clin Exp Hypertens A. 1991;13:587‐606. [DOI] [PubMed] [Google Scholar]
- 242. Nakamoto H, Suzuki H, Kageyama Y, et al. Depressor systems contribute to hypertension induced by glucocorticoid excess in dogs. J Hypertens. 1992;10:561‐569. [DOI] [PubMed] [Google Scholar]
- 243. Martinez NI, Panciera DL, Abbott JA, et al. Evaluation of pressor sensitivity to norepinephrine infusion in dogs with iatrogenic hyperadrenocorticism. Pressor sensitivity in dogs with hyperadrenocorticism. Res Vet Sci. 2005;78:25‐31. [DOI] [PubMed] [Google Scholar]
- 244. Hall JE, Morse CL, Smith MJ Jr, et al. Control of arterial pressure and renal function during glucocorticoid excess in dogs. Hypertension. 1980;2:139‐148. [DOI] [PubMed] [Google Scholar]
- 245. Ueno Y, Mohara O, Brosnihan KB, Ferrario CM. Characteristics of hormonal and neurogenic mechanisms of deoxycorticosterone‐induced hypertension. Hypertension. 1988;11:I172‐I177. [DOI] [PubMed] [Google Scholar]
- 246. Metzler CH, Gardner DG, Keil LC, Baxter JD, Ramsay DJ. Increased synthesis and release of atrial peptide during DOCA escape in conscious dogs. Am J Physiol. 1987;252:R188‐R192. [DOI] [PubMed] [Google Scholar]
- 247. Rodbard S, Freed SC. The effect of desoxycorticosterone acetate on the blood pressure of the dog. Endocrinology. 1942;30:365‐368. [Google Scholar]
- 248. Goering JL, Raich PC, Zimmerman BG. Renal hemodynamics and vascular reactivity in canine DOCA‐salt hypertension. Am J Physiol. 1988;255:R563‐R568. [DOI] [PubMed] [Google Scholar]
- 249. Kaplan AJ, Peterson ME. Effects of desoxycorticosterone pivalate administration on blood pressure in dogs with primary hypoadrenocorticism. J Am Vet Med Assoc. 1995;206:327‐331. [PubMed] [Google Scholar]
- 250. Cowgill LD, James KM, Levy JK, et al. Use of recombinant human erythropoietin for management of anemia in dogs and cats with renal failure. J Am Vet Med Assoc. 1998;212:521‐528. [PubMed] [Google Scholar]
- 251. Randolph JE, Scarlett JM, Stokol T, et al. Expression, bioactivity, and clinical assessment of recombinant feline erythropoietin. Am J Vet Res. 2004;65:1355‐1366. [DOI] [PubMed] [Google Scholar]
- 252. Randolph JE, Scarlett J, Stokol T, et al. Clinical efficacy and safety of recombinant canine erythropoietin in dogs with anemia of chronic renal failure and dogs with recombinant human erythropoietin‐induced red cell aplasia. J Vet Intern Med. 2004;18:81‐91. [DOI] [PubMed] [Google Scholar]
- 253. Fiocchi EH, Cowgill LD, Brown DC, et al. The use of Darbepoetin to stimulate erythropoiesis in the treatment of Anemia of chronic kidney disease in dogs. J Vet Intern Med. 2017;31:476‐485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254. Chalhoub S, Langston CE, Farrelly J. The use of darbepoetin to stimulate erythropoiesis in anemia of chronic kidney disease in cats: 25 cases. J Vet Intern Med. 2012;26:363‐369. [DOI] [PubMed] [Google Scholar]
- 255. Noel S, Massart L, Hamaide A. Urodynamic and haemodynamic effects of a single oral administration of ephedrine or phenylpropanolamine in continent female dogs. Vet J. 2012;192:89‐95. [DOI] [PubMed] [Google Scholar]
- 256. Richter KP, Ling GV. Clinical response and urethral pressure profile changes after phenylpropanolamine in dogs with primary sphincter incompetence. J Am Vet Med Assoc. 1985;187:605‐611. [PubMed] [Google Scholar]
- 257. Byron JK, March PA, Chew DJ, DiBartola SP. Effect of phenylpropanolamine and pseudoephedrine on the urethral pressure profile and continence scores of incontinent female dogs. J Vet Intern Med. 2007;21:47‐53. [DOI] [PubMed] [Google Scholar]
- 258. Ginn JA, Bentley E, Stepien RL. Systemic hypertension and hypertensive retinopathy following PPA overdose in a dog. J Am Anim Hosp Assoc. 2013;49:46‐53. [DOI] [PubMed] [Google Scholar]
- 259. Peterson KL, Lee JA, Hovda LR. Phenylpropanolamine toxicosis in dogs: 170 cases (2004–2009). J Am Vet Med Assoc. 2011;239:1463‐1469. [DOI] [PubMed] [Google Scholar]
- 260. Herring IP, Jacobson JD, Pickett JP. Cardiovascular effects of topical ophthalmic 10% phenylephrine in dogs. Vet Ophthalmol. 2004;7:41‐46. [DOI] [PubMed] [Google Scholar]
- 261. Pascoe PJ, Ilkiw JE, Stiles J, Smith EM. Arterial hypertension associated with topical ocular use of phenylephrine in dogs. J Am Vet Med Assoc. 1994;205:1562‐1564. [PubMed] [Google Scholar]
- 262. Carofiglio F, Hamaide AJ, Farnir F, Balligand MH, Verstegen JP. Evaluation of the urodynamic and hemodynamic effects of orally administered phenylpropanolamine and ephedrine in female dogs. Am J Vet Res. 2006;67:723‐730. [DOI] [PubMed] [Google Scholar]
- 263. Kang MH, Park HM. Application of carvedilol in a dog with pseudoephedrine toxicosis‐induced tachycardia. Can Vet J. 2012;53:783‐786. [PMC free article] [PubMed] [Google Scholar]
- 264. Tjostheim SS, Stepien RL, Markovic LE, Stein TJ. Effects of toceranib phosphate on systolic blood pressure and proteinuria in dogs. J Vet Intern Med. 2016;30:951‐957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265. Luckschander N, Iben C, Hosgood G, Gabler C, Biourge V. Dietary NaCl does not affect blood pressure in healthy cats. J Vet Intern Med. 2004;18:463‐467. [DOI] [PubMed] [Google Scholar]
- 266. Kirk CA, Jewell DE, Lowry SR. Effects of sodium chloride on selected parameters in cats. Vet Ther. 2006;7:333‐346. [PubMed] [Google Scholar]
- 267. Xu L, Mei M, Haskins ME, et al. Immune response after neonatal transfer of a human factor IX‐expressing retroviral vector in dogs, cats, and mice. Thromb Res. 2007;120:269‐280. [DOI] [PubMed] [Google Scholar]
- 268. Langston JB, Guyton AC, Douglas BH, et al. Effect of changes in salt intake on Aterial pressure and renal function in partially Nephrectomized dogs. Circ Res. 1963;12:508‐513. [Google Scholar]
- 269. Coleman TG, Guyton AC. Hypertension caused by salt loading in dog. 3. Onset transients of cardiac output and other circulatory variables. Circ Res. 1969;25:153‐160. [DOI] [PubMed] [Google Scholar]
- 270. Thomas EK, Drobatz KJ, Mandell DC. Presumptive cocaine toxicosis in 19 dogs: 2004–2012. J Vet Emerg Crit Care (San Antonio). 2014;24:201‐207. [DOI] [PubMed] [Google Scholar]
- 271. Appel NM, Li SH, Holmes TH, Acri JB. Dopamine D3 receptor antagonist (GSK598809) potentiates the hypertensive effects of cocaine in conscious, freely‐moving dogs. J Pharmacol Exp Ther. 2015;354:484‐492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272. Pei Z, Zhang X. Methamphetamine intoxication in a dog: case report. BMC Vet Res. 2014;10:139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273. Bischoff K, Beier E 3rd, Edwards WC. Methamphetamine poisoning in three Oklahoma dogs. Vet Hum Toxicol. 1998;40:19‐20. [PubMed] [Google Scholar]
- 274. Tontodonati M, Fasdelli N, Moscardo E, Giarola A, Dorigatti R. A canine model used to simultaneously assess potential neurobehavioural and cardiovascular effects of candidate drugs. J Pharmacol Toxicol Methods. 2007;56:265‐275. [DOI] [PubMed] [Google Scholar]
- 275. Jennifer H, Mariana P, Karyn B. Serotonin syndrome from 5‐Hydroxytryptophan supplement ingestion in a 9‐month‐old Labrador retriever. J Med Toxicol. 2017;13:183‐186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276. Chobanian AV, Bakris GL, Black HR, et al. The seventh report of the joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. 2003;289:2560‐2572. [DOI] [PubMed] [Google Scholar]
- 277. Rasmussen CB, Glisson JK, Minor DS. Dietary supplements and hypertension: potential benefits and precautions. J Clin Hypertens (Greenwich). 2012;14:467‐471. [DOI] [PMC free article] [PubMed] [Google Scholar]


