Abstract
The search for more effective and lower cost therapeutic approaches for wound healing remains a challenge for modern medicine. In the search for new therapeutic options, plants and their metabolites are a great source of novel biomolecules. Among their constituents, the monoterpenes represent 90% of essential oils, and have a variety of structures with several activities such as antimicrobial, anti-inflammatory, antioxidant and wound healing. Based on that, and also due to the lack of reviews concerning the wound-healing activity of monoterpenes, we performed this systematic review—which provides an overview of their characteristics and mechanisms of action. In this search, the terms “terpenes”, “monoterpenes”, “wound healing” and “wound closure techniques” were used to retrieve articles published in LILACS, PUBMED and EMBASE until May 2013. Seven papers were found concerning the potential wound healing effect of five compouds (three monoterpenes and two iridoid derivatives) in preclinical studies. Among the products used for wound care, the films were the most studied pharmaceutical form. Monoterpenes are a class of compounds of great diversity of biological activities and therapeutic potential. The data reviewed here suggest that monoterpenes, although poorly studied in this context, are promising compounds for the treatment of chronic wound conditions.
Keywords: cicatrix, granulation tissue, terpene, monoterpene, wound-healing, wound closure technique
1. Introduction
Wounds are physical, chemical or thermal injuries that result in an opening or breaking in the integrity of the skin. The continuity of the skin should be restored, and appropriate methods for wound healing are essential for the restoration of disrupted anatomical continuity and disturbed function status of the skin [1].
The acute wound healing process is a complex series of interrelated events that are mediated in its different phases by a wide range of chemically coordinated cellular processes, as well as hormonal influences. It is characterized by a sequence of independent and/or overlapping events [2,3]. The process can be broadly categorized into three or four stages: coagulating phase, inflammatory phase, proliferative phase (formation of granulation tissue and collagen synthesis), and finally the remodeling phase, which ultimately determines the strength and appearance of the healed tissue [4,5,6,7,8].
For centuries, natural products such as medicinal plants have been used to treat a lot of illnesses worldwide, arousing scientific and commercial interests and still playing an important role in the health systems in many developed and developing countries, such as the United States and Brazil, respectively [9,10].
Monoterpenes belong to a large and diverse group of chemical compounds named terpenes. They represent a group of naturally-occurring organic compounds. They are the most representative molecules constituting 90% of the essential oils and have a great variety of structures [11], with relevant pharmacological properties such as antimicrobial, anti-inflammatory, antioxidant, antipruritic, hypotensive and analgesic activities [12,13,14,15,16]. Hence, medicinal plants and related compounds have traditionally played an important role in drug discovery and were the basis of most early medicines [17]. Additionally, the usage of techniques and products in wound care allied to substances with anti-inflammatory, antibacterial and antioxidant properties are powerful in the treatment of skin lesions [18].
Despite their importance, there are no reviews on the wound-healing potential of monoterpenes. Accordingly, we conducted for the first time a systematic review of the literature to examine and synthesize the literature on monoterpenes, to identify and to evaluate those that assess healing effects in wound-healing animal models.
2. Results and Discussion
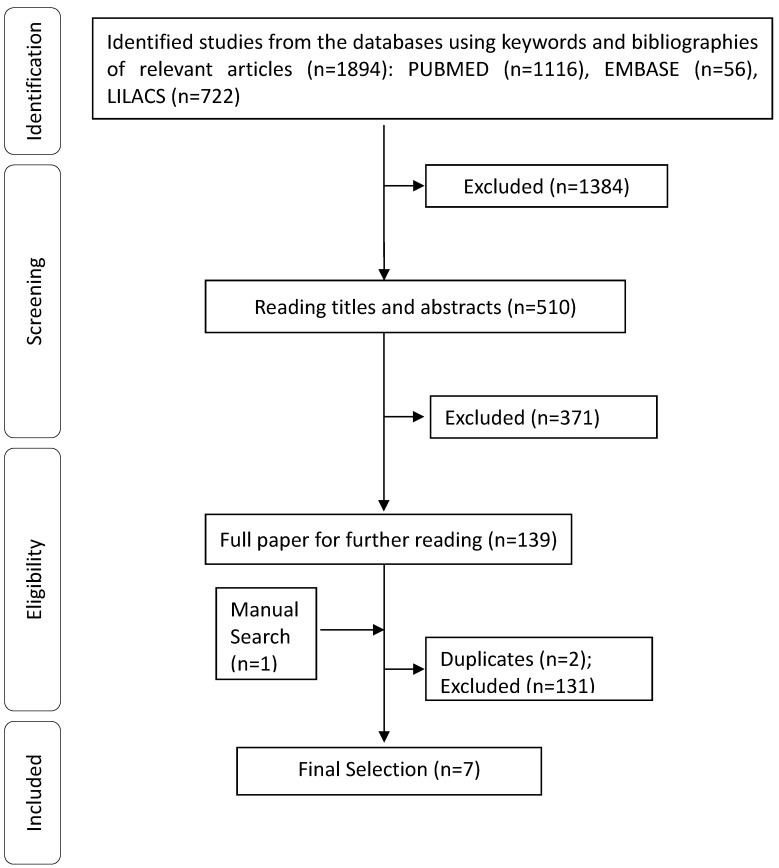
A total of 1,895 abstracts/citations were identified for preliminary review from electronic and manual searches. The primary search identified 1,894 articles, with 1,116 from PUBMED, 722 from LILACS, 56 from EMBASE and one from manual search. After removal of duplicates and screening for relevant titles and abstracts, a total of 140 articles were submitted for a full-text review. Seven articles met the inclusion and exclusion criteria established. A flow chart illustrating the progress of study selection and article number at each stage is shown (Figure 1).
Figure 1.
Flowchart of included studies. Studies were excluded according to the following exclusion criteria: studies in humans, studies of mixtures of substances or extracts from plants, review articles, meta-analyses, abstracts, conference proceedings, editorials/letters, case reports.
From seven final selected studies, most of that research was conducted in China (43%), Korea (29%), Brazil (14%) and Peru (14%). Regarding the pharmaceutical form of the products used for wound healing presented in the selected studies (Table 1), bioactive films (38%) were the most used, followed by ointments (25%) and solutions (25%) and finally suspensions (12%).
Table 1.
Characteristics of included studies.
| Authors, year, Country | Substance(s) | Animals | Doses, Concetration or Quantity | Pharmaceutical dosage forms | Model | Valued Parameter Settings | Results and Mechanisms | |
|---|---|---|---|---|---|---|---|---|
| Macroscopic | Microscopic | |||||||
| Mai L.M. et al., 2003, China | Borneol | Adult male Sprangue-Dawley rats | 4.5% and 0.7% | Vaselin-based ointment | Excision wound | Basic physiological conditions (body length, weight, food eaten, water intake); Wound areas measured by slide calipers and photographed |
Histological observation (HE) (skin appendages and collagen fibers quality); Measurement of the thinckness of the granulation tissue and newly formed epithelium |
This study found that the combination of Bismuth subgallate (BS) and Borneol (BO) and Vaseline had a synergistic effect in accelerating wound closure. All results were associated with the BS, while nothing about BO was reported. However, the precise mechanism of the drugs remains unclear and further work is necessary to study whether macrophages could secret growth factor to accelerate wound healing. |
| Riella K.R. et al., 2012, Brazil | Thymol | Adult male and female Wistar rats | 1.2 mg | Collagen-based films | Excision wound | Wound contraction rates by digital caliper | Inflammatory response and profile inflammatory (HE); Collagen deposition (Picrosirius) |
The modulation of the leukocyte influx by thymol was associated to increased levels of macrophage migration inhibitory factor (MIF) in central nervous system; The improved on granulation tissue by collagen-based containing thymol (COLTHY) films founded was associated to anti-inflammatory properties of thymol; Improvement in the replacement and arrangement by COLTHY was associated to modulatory effect on the flbroblast metabolism and collagen synthesis and the thymol able to enhance the flbroblasts growth in vitro. |
| Zhang K. et al., 2010, China | Genipin | Sprague–Dawley rats | 50 mg/mL | Silk fibroin/ hydroxybutyl chitosan | Excision wound | --------- | Histological examination of the inflammatory response; epithelization; proliferation of fibroblasts and collagen proliferation; blood vessels migration. | Greater proliferation of fibroblasts was observed in the nanofibers that was associated to a genipin crosslinked; Fibroblasts cells had greater proliferation and arranged in better order, densely in nanofibers that was too associated to a genipin crosslinked. |
| Villegas L.F. et al., 2001, Peru | α-Terpineol | Male mice | 0.05 mL | Suspension | Incision wound | Tensile strength | --------- | Epi-α-bisabolol, α-bisabolol and α-terpineol showed significant in vivo cicatrizant activity and did not have a significant effect on increasing cell migration. The mechanisms is not shown. |
| Chang W.H. et al., 2003, China | Genipin | Male Wistar rats | --------- | Wound dressing Membranes | Excision wound | Basic physiological conditions (infection) | Histological examination of the inflammatory response; epithelization and granulation tissue formation. | Genipin-crosslinked dressing membrane showed lower inflammatory reaction in the wound that may be due to the lower toxicity of its remaining residuesGenipin-crosslinked dressing membrane promotes early re-epithelialization, but mechanisms is not shown . |
| Lee S.W. et al., 1999, Republic of Korea | Aucubin | Male rats | 0.1% | Solution and based ointment | Incision wound | --------- | --------- | --------- |
In the selected articles, the wound models used to study the wound healing included excision and incision wound model. However, the main model used was the excision wound model (83%). In most of selected studies, both macroscopic and microscopic features were evaluated. A total of 56% selected searches evaluated tissue morphology aspects involved in the wound healing process.
Concerning the mechanisms of action involved in the wound healing proposed for different monoterpenes, the ones suggested were antimicrobial activity (inhibits RNA and protein biosynthesis of microorganisms), anti-inflammatory activity (decreases the amount of IL-6 and TNF-α production in mast cells, inhibits the release of LTC4 and has an effect on the release of TXB2); antioxidant activity (photoprotective effects and oxidative stress by inhibiting UVB-induced free radical production); low-toxicity characteristics, macrophage migration inhibitory factor (MIF) and fibroblast growth effects.
In this study, China was the country with the largest number of studies on the healing effects of monoterpenes. The use of plants for medicinal purposes to treat, cure and prevent diseases is one of the oldest forms of medical practice of Humanity [19]. In particular, Traditional Chinese Medicines (TCM) are composed by various combinations of medical plants and have been used as natural remedies for thousands of years [20].
Medicinal plants are the primary sources of many small molecule drugs and herbal products [21,22]. Several recent publications reiterate the importance of natural products as a source of drugs [23,24]. In this context, the advent of modern technologies has boosted medicinal plants as a highly valuable commodity in the patent market. Many developed and developing countries are actively engaged in the biomining of medicinal plants for therapeutically precious and biologically active phytochemicals [25].
According to the World Conservation Monitoring Centre (WCMC) of United Nations Environment Program (UNEP), China was identified as one of the largest mega-biodiversity countries [25]. According to Ravenhill, China is one of the largest countries in Asia, which have the richest arrays of registered and relatively well-known medicinal plants [26]. In addition, medicinal plants have been used in developing countries for thousands of years. The World Health Organization (WHO) estimated that 70%–80% of the population living in developing nations depends on traditional healthcare systems for primary healthcare [27]. Besides, in China about 40% of the total medicinal consumption is attributed to traditional medicines [27].
Brazil is one of the countries with the largest biodiversity in the planet and it is associated with an extensive ethical and cultural diversity (Indigenous, African and European) that traditionally uses natural products. It also presents social and economical characteristics that typify it as a developing country, where 80% of the population depends on the use of plants for the primary health care [28,29].
Despite the therapeutic potential of medicinal plants and their compounds, the great biodiversity and also the ethnic and cultural aspects of developing countries such as China and Brazil, few studies were found regarding the wound-healing effects of monoterpenes. For this study, only isolated monoterpenes were included, due to the fact that they provide structural molds for obtaining synthetic substances and also because they are considered as sources for drug development. Furthermore, they can be used as tools to identify mechanisms of action [30].
The healing process can be accelerated and enhanced by the use of wound care techniques and products [31,32]. In this review, it was observed that, among the products used for the wound care, the films were the most studied pharmaceutical form. The use of liquid dosage form provides the advantage of studying the action of the isolated compounds. However, the major problem is the short residence times on the wound site, especially where there is a measurable degree of wound fluid exuding [33].
It might also be noted that the bioactive films were studied in the most current research. Currently, it has been shown that wound healing becomes rapid and successful when a warm moist environment around the wound is provided. Unlike the solutions, recently the modern dressings have been developed with features to retain and create this great environment playing an active role in wound healing [33].
Moreover, the dressings-based biomaterials, for being part of the matrix of natural tissue, are biocompatible at the toxicological point, biodegradable and are able to permeate active ingredients such as antimicrobial agents or growth factors [34,35].
Wounds are heterogeneous, and the wound-healing process is multifactorial, and influenced by many extrinsic and intrinsic factors. In order to obtain new knowledge of the complexity of this process or substances effects, the use of animal models is required [36].
More specific human chronic wound treatments are absent, in a large part due to the lack of knowledge of the molecular abnormalities within the wound that prevent healing. Research is hindered by the absence of an easily reproducible animal model that mimics the human chronic wound state [37,38]. Currently, the chronic wound models described (and that represent the best available at present) are far from ideal [38].
In the present study, the excisional wound model was the most used. This is an acute wound model whose great advantage is the rapid introduction of injury and a relatively rapid course, besides being a wound model of easy and inexpensive execution when compared to chronic wound models [38,39].
Furthermore, the excisional wound model involves the removal of a significant volume of the target tissue, and the filling of the void created allows greater amount of material. The excision site can be harvested or biopsied to obtain cells, tissue, RNA, exudates, and histological specimens that have a wider cross-sectional area and volume when compared to incisional wound. This is suitable for in situ techniques or biomechanical strength (tensile strength) [39,40].
Concerning the evaluated parameters, the analysis of the kinetics of biological events in response to pharmacological substances is crucial for the development of effective therapeutic products able to stimulate wound healing [40]. This review shows that no study prioritized the molecular biology assays.
Monoterpenes or monoterpenoids are compounds with a core of 10 carbons. They are cyclized and oxidized in a variety of ways. Due to the low molecular weight, many of them exist in the form of essential oils [11]. A type of monoterpenes, the iridoids, is derived from geraniol. They are different from the similarly-named iridals (triterpenes). A subclass of iridoid, the iridoid glycosides and glucosides are compounds that include a glycoside or glucoside, respectively, moiety, usually found at the C-1 position.
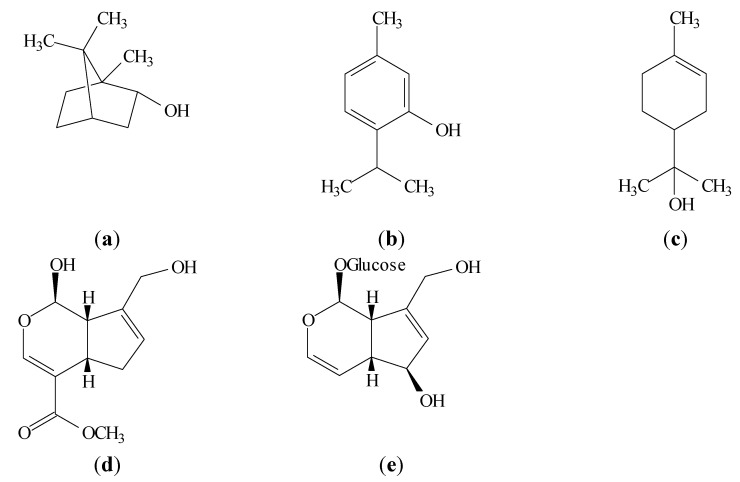
In the present study, articles with the following monoterpenes were selected, including types and their subclasses: borneol, thymol, α-terpineol, genipin and aucubin. According to the scientific literature, such compounds possess a range of biological activities that may be directly or indirectly related to wound-healing effects.
Borneol is a bicyclic monoterpenoid alcohol (Figure 2a). Borneol has shown effects such as antibiotic activity [41], wound-healing activity [42], anti-inflammatory activity by reducing leukocyte migration [43], anti-fibrosis activity by decreasing the fibroblasts growth, inhibiting collagen production, decreasing MMP-2 activity and inhibiting TIMP-1 production [44]. It showed no cytotoxicity [44], radical scavenging properties [12,45] and immunomodulatory effects [46]. This monoterpene was able to suppress the proinflammatory cytokine (IL-1β and IL-6) mRNA expression and act as bioactive material in the cellular signal transduction system [47]. It shows antibacterial activity and inhibitory effects on several Gram (−)ve and Gram (+)ve pathogenic microorganisms [48,49], antifungal activity [12,48,50,51,52], antioxidant activity by reducing intracellular reactive oxygen species (ROS) generation and attenuating the elevation of nitric oxide (NO), the increase of inducible nitric oxide synthase (iNOS) enzymatic activity and the upregulation of iNOS expression [53]. Borneol blocked NF-κB p65 nuclear translocation [53] and was shown to be a mast cell membrane stabilizer [54]. Finally, anti-inflammatory property was shown through fewer ICAM-1 positive vessels, IL-1β positive cells, TNF-α positive cells and number of neutrophils [55].
Figure 2.
Structural formulae of (a) (−)-borneol, (b) thymol, (c) α-terpineol, (d) genipin and (e) aucubin.
Thymol is a monoterpenoid phenol (Figure 2b) which exhibits multiple biological activities. Studies show that thymol modulates prostaglandin synthesis [56], it has anti-inflammatory effect in human neutrophils incubated [57] and beneficial effects on the antioxidant status by the influenced on docosahexaenoic acid (DHA) concentration [58]. Thymol prevented autoxidation of lipids [59] and the formation of toxic products through the action of reactive nitrogen species [60]. It exhibits antimicrobial activity [57,59,61,62,63] and wound-healing activity [64]. Thymol is able to increase the levels of macrophage migration inhibitory factor (MIF) in central nervous system [65], enhance the in vitro fibroblast growth [66] and interfere with elastase activity as evidenced by the reduced release of this proteinase by human neutrophils stimulated with the synthetic chemotactic peptide N-formyl-methionyl-leucyl-phenylalanine (fMLP) [57]. It effectively inhibited COX-1 [67], inhibited inducible lymphocyte proliferation [68] and showed anti-inflammatory effects through the reduction of the edema, inhibition of MPO activity and decreased leukocyte influx [64].
α-Terpineol is a monoterpenoid alcohol (Figure 2c) relatively non-toxic which is present in the essential oils of several species [69,70]. This monoterpene presented wound healing effect [69] and anti-inflammatory activity by inhibiting the COX enzyme and IL production [71,72]. α-Terpineol is also an NF-κB inhibitor and promotes down-regulation of IL-1β expression [73] and IL-6 formation [74]. Futhermore, the power in the reduction of TNF-α and NO production was demonstrated [75]. In addition, α-terpineol showed selective inhibition of ovine COX-2 activity [72], inhibited the neutrophil influx [75], exhibited strong antimicrobial activity [76] and antifungal effects [77].
Genipin is an iridoid compound (Figure 2d) and an alternative natural crosslinking agent [78,79,80,81,82]. It has shown ability to form biocompatible and stable crosslinked products and showed low cytotoxicity [83]. Moreover, it has been proved that genipin has anti-inflammatory [84], wound healing [81,82] and anti-oxidative effects [85] and abilities of inhibiting lipid peroxidation and production of nitrogen monoxide (NO) [86]. Additionally, genipin can increase the mitochondrial membrane potential [87], increase the ATP levels and close KATP channels [87] and stimulate insulin secretion [87]. Finally, studies showed that genipin suppress the alpha-TN4 lens epithelial cells and subconjunctival fibroblast migration induced by TGF-b [88,89].
Aucubin is an iridoid glycoside (Figure 2e) with a variety of pharmacological effects, such as antimicrobial [90,91,92], anti-inflammatory [93,94], dermal wound healing [95,96] and in vitro antioxidative capacity [97]. In addition, aucubin showed inhibition of RNA and protein biosyntheses [91,95,98,99,100]. Futher, aucubin inhibits TNF-α-induced secretion and mRNA synthesis including PAI-1, MCP-1, and IL-6 [101]. Furthermore, investigation revealed that aucubin suppressed extracellular signal-regulated kinase (ERK) activation [102], inhibitory kappa Bα (IκBα) degradation [102], and subsequent nuclear factor kappa B (NF-κB) activation [102]. Finally, aucubin was considered as a promising chemopreventive agent and was devoid of any cytotoxic activity [103,104,105].
3. Experimental
The present systematic review was conducted according to the guidelines for Transparent Reporting of Systematic Reviews and Meta-Analyses (PRISMA statement) [106].
3.1. Search Strategy
Three databases (Internet sources) were used to search for appropriate papers that fulfilled the study purpose. Those included the National Library of Medicine, Washington, DC, USA (MEDLINE-PubMed), Excerpta Medical Database by Elsevier (EMBASE), and Latin American and Caribbean Health Sciences (LILACS), using different combinations of the following keywords: wound healing, wound closure techniques, cicatrix, granulation tissue, monoterpenes and terpenes. The databases were searched for studies conducted in the period up to and including May 2013. The structured search strategy was designed to include any published paper that evaluated a wound healing to identify those that show potential therapeutic value. Citations were manually limited to animal studies. Additional papers were included in our study after analyses of all references from the selected articles. We did not contact investigators, nor did we attempt to identify unpublished data.
3.2. Study Selection
All electronic search titles, selected abstracts, and full-text articles were independently reviewed by a minimum of two reviewers (R.S.S.B., A.S.B. and L.J.Q.J.). Disagreements on study inclusion/exclusion were resolved with the reach of a consensus. The following inclusion criteria were applied: wound-healing studies, and the use of monoterpenes isolated or not isolated from medicinal plants (natural or synthetic product) for treatment. Studies were excluded according to the following exclusion criteria: studies in humans, studies of mixtures of substances or extracts from plants, review articles, meta-analyses, abstracts, conference proceedings, editorials/letters, case reports (Figure 1).
3.3. Data Extraction
Data were extracted by one reviewer using standardized forms and were checked by a second reviewer. Extracted information included data regarding the substance, animal models, dosages and concentrations, dosage form, evaluated parameters, results and proposed mechanisms of action.
4. Conclusions
For more than a decade, researchers have studied the wound-healing potential of monoterpenes through in vivo and in vitro assays. Therefore, as in Nature there are about 20,000 known different terpene metabolites [107], this superfamily, of which the monoterpenes are a part, still offers a great opportunity of new discoveries for this application. Nevertheless, this review described the study of only five monoterpenes or types of monoterpenes in models of wound healing in animals. In summary, it can be concluded that, although there are some studies about the wound-healing effects of monoterpenes, a class of compounds of great diversity of biological activities and therapeutic potential, they have been little studied for the treatment of wounds, which occurs especially in developing countries that have a wide biodiversity and tradition in the use of natural products such as Brazil.
Moreover, of those, every evaluated monoterpenes showed wound-healing effects. The anti-inflammatory action of monoterpenes is often related and correlated to wound-healing effect. However, further studies are required to better understand these mechanisms. All these findings make the monoterpenes a great potential source of compounds for the development of new drugs for the treatment of various pathological processes that afflict humanity, including chronic wound conditions.
Acknowledgments
This work was supported by grants from National Council of Technological and Scientific Development (CNPq/Brazil) and the Research Supporting Foundation of State of Sergipe (FAPITEC-SE/Brazil). We would like to thank also teacher Abilio Borghi, who helped us with the grammar review of the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Meenakshi S., Raghavan G., Nath V., Ajay Kumar S.R., Shanta M. Antimicrobial, wound healing and antioxidant activity of Plagiochasma. appendiculatum Lenm et Lind. J. Ethnopharmacol. 2006;107:67–72. doi: 10.1016/j.jep.2006.02.007. [DOI] [PubMed] [Google Scholar]
- 2.Diegelmann R.F., Evans M.C. Wound healing: An overview of acute, fibrotic and delayed healing. Front. Biosci. 2004;9:283–289. doi: 10.2741/1184. [DOI] [PubMed] [Google Scholar]
- 3.Chan E.W.C., Lim Y.Y., Wong L.F., Lianto F.S., Wong S.K., Lim K.K., Joe C.E., Lim T.Y. Antioxidant and tyrosinase inhibition properties of leaves and rhizomes of ginger species. Food Chem. 2008;109:477–483. doi: 10.1016/j.foodchem.2008.02.016. [DOI] [Google Scholar]
- 4.Sumitra M., Manikandana P., Suguna L. Efficacy of Buteamono sperma on dermal wound healing in rats. Int. J. Biochem. Cell Biol. 2005;37:566–573. doi: 10.1016/j.biocel.2004.08.003. [DOI] [PubMed] [Google Scholar]
- 5.Ayyanar M., Ignacimuthu S. Herbal medicines for wound healing among tribal people in Southern India: Ethnobotanical and Scientific evidences. Int. J. Appl. Res. Nat. Prod. 2009;2:29–42. [Google Scholar]
- 6.Dash G.K., Murthy P.N. Studies on wound healing activity of Heliotropium. indicum Linn. Leaves on Rats. ISRN Pharmacol. 2011;2011:847980. doi: 10.5402/2011/847980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Reinke J.M., Sorg H. Wound repair and regeneration. Eur. Surg. Res. 2012;49:35–43. doi: 10.1159/000339613. [DOI] [PubMed] [Google Scholar]
- 8.Rawat S., Singh R., Thakur P., Kaur S., Semwal A. Wound healing agents from medicinal plants: A review. Asian Pac. J. Trop. Biomed. 2012;2:S1910–S1917. doi: 10.1016/S2221-1691(12)60520-6. [DOI] [Google Scholar]
- 9.Süntar I., Akkol E.K., Nahar L., Sarker S.D. Wound healing and antioxidant properties: Do they coexist in plants? Free Rad. Antiox. 2012;2:1–7. [Google Scholar]
- 10.Li J.W., Vederas J.C. Drug discovery and natural products: End of an era or an endless frontier? Science. 2009;325:161–165. doi: 10.1126/science.1168243. [DOI] [PubMed] [Google Scholar]
- 11.Bakkali F., Averbeck S., Averbeck D., Idaomar M. Biological effects of essential oils–A Review. Food Chem. Toxicol. 2008;46:446–475. doi: 10.1016/j.fct.2007.09.106. [DOI] [PubMed] [Google Scholar]
- 12.Kordali S., Kotan R., Mavi A., Cakir A., Ala A., Yildirim A. Determination of the chemical composition and antioxidant activity of the essential oil of Artemisia dracunculus and of the antifungal and antibacterial activities of Turkish Artemisia absinthium, Artemisia dracunculus, Artemisia santonicum and Artemisia spicigera essential oils. J. Agric. Food. Chem. 2005;53:9452–9458. doi: 10.1021/jf0516538. [DOI] [PubMed] [Google Scholar]
- 13.Bastos J.F., Moreira I.J., Ribeiro T.P., Medeiros I.A., Antoniolli A.R., DeSouza D.P., Santos M.R. Hypotensive and vasorelaxant effects of citronellol, a monoterpene alcohol. Basic Clin. Pharmacol. Toxicol. 2010;106:331–337. doi: 10.1111/j.1742-7843.2009.00492.x. [DOI] [PubMed] [Google Scholar]
- 14.Menezes I.A., Barreto C.M., Antoniolli A.R., Santos M.R., DeSousa D.P. Hypotensive activity of terpenes found in essential oils. Z. Naturforsch. C. 2010;65:562–566. doi: 10.1515/znc-2010-9-1005. [DOI] [PubMed] [Google Scholar]
- 15.Guimarães A.G., Quintans J.S., Quintans-Júnior. L.J. Monoterpenes with analgesic activity–A systematic review. Phytother. Res. 2013;27:1–15. doi: 10.1002/ptr.4686. [DOI] [PubMed] [Google Scholar]
- 16.Carson C.F., Martelo K.A., Riley T.V. Melaleuca alternifolia (Tea Tree) de óleo: Uma revisão das propriedades medicinais antimicrobianos e outros. Clin. Microbiol. Rev. 2006;19:50–62. doi: 10.1128/CMR.19.1.50-62.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Butler M.S. Natural products to drugs: Natural product-derived compounds in clinical trials. Nat. Prod. Rep. 2008;25:475–516. doi: 10.1039/b514294f. [DOI] [PubMed] [Google Scholar]
- 18.Dias A.M.A., Braga M.E.M., Seabra I.J., Ferreira P., Gil M.H., de Sousa H.C. Development of natural-based wound dressings impregnated with bioactive compounds and using supercritical carbon dioxide. Int. J. Pharm. 2011;408:9–19. doi: 10.1016/j.ijpharm.2011.01.063. [DOI] [PubMed] [Google Scholar]
- 19.Viegas J.R., Bolzani C., Silva V., Barreto E.J. Os produtos naturais e a química medicinal moderna. Quim. Nova. 2006;29:326–337. doi: 10.1590/S0100-40422006000200025. [DOI] [Google Scholar]
- 20.Xiao P.G. Modern Chinese Materia Medica. Volume 1. Chemical Industry Press; Beijing, China: 2002. pp. 17–22. [Google Scholar]
- 21.Chen S., Yao H., Han J., Liu C., Song J., Shi L., Zhu Y., Ma X., Gao T., Pang X., et al. Validation of the ITS2 region as a novel DNA barcode for identifying medicinal plant species. PLoS One. 2010;5:e8613. doi: 10.1371/journal.pone.0008613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nalawade S.M., Sagare A.P., Lee C.Y., Kao C.L., Tsay H.S. Studies on tissue culture of Chinese medicinal plant resources in Taiwan and their sustainable utilization. Bot. Bull. Acad. Sin. 2003;44:79–98. [Google Scholar]
- 23.Oberlies N.H., Kroll D.J. Camptothecin and taxol: Historic achievements in natural products research. J. Nat. Prod. 2004;67:129–135. doi: 10.1021/np030498t. [DOI] [PubMed] [Google Scholar]
- 24.Srivastava V., Negi A.S., Kumar J.K., Gupta M.M., Khanuja S.P.S. Plant-based anticancer molecules: A chemical and biological profile of some important leads. Bioorg. Med. Chem. 2005;13:5892–5908. doi: 10.1016/j.bmc.2005.05.066. [DOI] [PubMed] [Google Scholar]
- 25.Rajeswara R.B.R., Syamasundar K.V., Rajput D.K., Nagaraju G., Adinarayana G. Biodiversity, conservation and cultivation of medicinal plants. J. Pharmacogn. 2012;3:59–62. [Google Scholar]
- 26.Ravenhill J. Is China an economic threat to southeast Asia? Asian Surv. 2006;46:653–674. doi: 10.1525/as.2006.46.5.653. [DOI] [Google Scholar]
- 27.Hoareau L., DaSilva E. Medicinal plants: A re-emerging health aid. Electronic J. Biotechnol. 1999;2:56–71. [Google Scholar]
- 28.Schuster B.G. Demonstrating the validity of natural products as anti-infective drugs. J. Altern. Compl. Med. 2001;7S:73–82. doi: 10.1089/107555301753393832. [DOI] [PubMed] [Google Scholar]
- 29.Guerra M.P., Nodari R.O. Biodiversidade: Aspectos Biológicos, Geográficos, Legais e éticos. In: Simões O.M.C., Schenkel R.P., Gosmann G., Mello P.C.J., Mentz A.L., Petrovick P.R., editors. Farmacognosia da Planta Medicamento. 3rd ed. Volume 1. Editora da UFSC; Porto Alegre/Florianópolis, Brazil: 2001. pp. 13–26. [Google Scholar]
- 30.McKernan R.M., Whiting P.J. Which GABAA-receptor subtypes really occurin the brain? Trends Neurosci. 1996;19:139–143. doi: 10.1016/S0166-2236(96)80023-3. [DOI] [PubMed] [Google Scholar]
- 31.Cooper D.M. Optimizing wound healing. A practice within nursing's domain. Nurs. Clin. North. Am. 1990;25:165–177. [PubMed] [Google Scholar]
- 32.Hanna J.R., Giacopelli J.A. A review of wound healing and wound dressing products. J. Foot Ankle Surg. 1997;36:2–14. doi: 10.1016/S1067-2516(97)80003-8. [DOI] [PubMed] [Google Scholar]
- 33.Boateng J.S., Matthews K.H., Stevens H.N., Eccleston G.M. Wound healing dressings and drugs delivery sytems: A review. J. Pharm. Sci. 2012;97:2892–2923. doi: 10.1002/jps.21210. [DOI] [PubMed] [Google Scholar]
- 34.Ovington L.G. Advances in wound dressings. Clin. Dermatol. 2007;25:33–38. doi: 10.1016/j.clindermatol.2006.09.003. [DOI] [PubMed] [Google Scholar]
- 35.Yudanova T.N., Reshetov I.V. Modern wound dressings: Manufacturing and properties. Pharm. Chem. J. 2006;40:85–92. doi: 10.1007/s11094-006-0065-z. [DOI] [Google Scholar]
- 36.Gottrup F., Agren M.S., Karlsmark T. Models for use in wound healing research: A survey focusing on in vitro and in vivo adult soft tissue. Wound Repair Regen. 2000;8:83–96. doi: 10.1046/j.1524-475x.2000.00083.x. [DOI] [PubMed] [Google Scholar]
- 37.Chen C., Schultz G.S., Bloch M., Edwards P.D., Tebes S., Mast B.A. Molecular and mechanistic validation of delayed healing rat wounds as a model for human chronic wounds. Wound Repair Regen. 1999;7:486–494. doi: 10.1046/j.1524-475X.1999.00486.x. [DOI] [PubMed] [Google Scholar]
- 38.Ansell D.M., Holden K.A., Hardman M.J. Animal models of wound repair: Are they cutting it? Exp. Dermatol. 2012;21:581–585. doi: 10.1111/j.1600-0625.2012.01540.x. [DOI] [PubMed] [Google Scholar]
- 39.Davidson J.M. Animal models for wound repair. Arch. Dermatol. Res. 1998;290:S1–S11. doi: 10.1007/PL00007448. [DOI] [PubMed] [Google Scholar]
- 40.Alborova A., Lademann J., Meye L., Kramer A., Patzelt A., Sterry W., Antoniou C. Application of laser scanning microscopy for the characterization of wound healing. GMS Krankenhaushyg. Interdiszip. 2007;2:1–6. [Google Scholar]
- 41.Unlu M., Daferera D., Donmez E., Polissiou M., Tepe B., Sokmen A. Compositions and the in vitro antimicrobial activities of the essential oils of Achillea. setacea and Achillea. teretifolia. J. Ethnopharmacol. 2002;83:117–121. doi: 10.1016/S0378-8741(02)00218-0. [DOI] [PubMed] [Google Scholar]
- 42.Mai L.M., Lin C.Y., Chen C.Y., Tsai Y.C. Synergistic effect of bismuth subgallate and borneol, the major components of Sulbogins, on the healing of skin wound. Biomaterials. 2003;24:3005–3012. doi: 10.1016/S0142-9612(03)00126-1. [DOI] [PubMed] [Google Scholar]
- 43.Almeida J.R.G.S., Souza G.R., Silva J.C., Lima-Saraiva S.R.G., Oliveira-Júnior R.G., Quintans J.S.S., Barreto R.S.S., Bonjardim L.R., Cavalcanti S.C.H., Quintans-Júnior L.J. Borneol, a bicyclic monoterpene alcohol, reduces nociceptive behavior and inflammatory response in mice. Sci. World J. 2013;2013:1–5. doi: 10.1155/2013/808460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Dai J.P., Chen J., Bei Y.F., Han B.X., Wang S. Influence of borneol on primary mice oral fibroblasts: A penetration enhancer maybe used in oral submucous fibrosis. J. Oral Pathol. Med. 2009;38:276–281. doi: 10.1111/j.1600-0714.2008.00738.x. [DOI] [PubMed] [Google Scholar]
- 45.Candan F., Unlü M., Tepe B., Daferera D., Polissiou M., Sökmen A., Akpulat H.A. Antioxidant and antimicrobial activity of the essential oil and methanol extracts of Achillea. millefolium subsp. Millefolium Afan. (Asteraceae) J. Ethnopharmacol. 2003;87:215–220. doi: 10.1016/S0378-8741(03)00149-1. [DOI] [PubMed] [Google Scholar]
- 46.Juhás S., Cikos S., Czikková S., Veselá J., Il’ková G., Hájek T., Domaracká K., Domaracky M., Bujnáková D., Rehák P., et al. Effects of borneol and thymoquinone on TNBS-induced colitis in mice. J. Folia Biol. 2008;54:1–7. doi: 10.14712/fb2008054010001. [DOI] [PubMed] [Google Scholar]
- 47.Park T.J., Park Y.S., Lee T.G., Ha H., Kim K.T. Inhibition of acetylcholine-mediated effects by borneol. Biochem. Pharmacol. 2003;65:83–90. doi: 10.1016/S0006-2952(02)01444-2. [DOI] [PubMed] [Google Scholar]
- 48.Knobloch K., Pauli A., Iberl B., Weigand H., Weis N. Antibacterial and antifungal properties of essential oil components. J. Essent. Oil Res. 1989;1:119–128. doi: 10.1080/10412905.1989.9697767. [DOI] [Google Scholar]
- 49.Tabanca N., Kirimer N., Demirci B., Demirci F., Baser K.H. Composition and antimicrobial activity of the essential oils of Micromeria. cristata subsp. Phrygia and the enantiomeric distribution of borneol. J. Agric. Food Chem. 2001;49:4300–4303. doi: 10.1021/jf0105034. [DOI] [PubMed] [Google Scholar]
- 50.Tuberoso C.I., Kowalczyk A., Coroneo V., Russo M.T., Dessi S., Cabras P. Chemical composition and antioxidant, antimicrobial and antifungal activities of the essential oil of Achillea. ligustica all. J. Agric. Food Chem. 2005;53:10148–10153. doi: 10.1021/jf0518913. [DOI] [PubMed] [Google Scholar]
- 51.Tabanca N., Demirci B., Baser K.H., Aytac Z., Ekici M., Khan S.I., Jacob M.R., Wedge D.E. Chemical composition and antifungal activity of Salvia macrochlamys and Salvia recognita essential oils. J. Agric. Food Chem. 2006;54:6593–6597. doi: 10.1021/jf0608773. [DOI] [PubMed] [Google Scholar]
- 52.Wenqiang G., Shufen L., Ruixiang Y., Yanfeng H. Comparison of composition and antifungal activity of Artemisia argyi Levl. et Vant inflorescence essential oil extracted by hydrodistillation and supercritical carbon dioxide. Nat. Prod. Res. 2006;20:992–998. doi: 10.1080/14786410600921599. [DOI] [PubMed] [Google Scholar]
- 53.Liu R., Zhang L., Lan X., Li L., Zhang T.T., Sun J.H., Du G.H. Protection by borneol on cortical neurons against oxygen-glucose deprivation/reperfusion: Involvement of anti-oxidation and anti-inflammation through nuclear transcription factor κappaB signaling pathway. Neuroscience. 2011;176:408–419. doi: 10.1016/j.neuroscience.2010.11.029. [DOI] [PubMed] [Google Scholar]
- 54.Watanabe K., Yano S., Horie T., Kachia R.S., Ikegami F., Yamamoto Y., Fujimori H., Kasai M. Borneol as Allergy Inhibitor. Aug 2, 1994. JP 06211713.
- 55.He X., Lu Q., Liu Y. Effects of borneol injection on inflammation in focal cerebral ischemia reperfusion rats. Hua Xi Yao Xue Za Zhi. 2006;21:523–526. [Google Scholar]
- 56.Anamura S., Dohi T., Shirakawa M., Okamoto H., Tsujimoto A. Effects of phenolic dental medicaments on prostaglandin synthesis by microsomes of bovine tooth pulp and rabbit kidney medulla. Arch. Oral Biol. 1988;33:555–560. doi: 10.1016/0003-9969(88)90129-X. [DOI] [PubMed] [Google Scholar]
- 57.Braga P.C., Dal Sasso M., Culici M., Bianchi T., Bordoni L., Marabini L. Anti-inflammatory activity of thymol inhibitory effect on the release of human neutrophil elastase. Pharmacology. 2006;77:130–136. doi: 10.1159/000093790. [DOI] [PubMed] [Google Scholar]
- 58.Youdim K.A., Deans S.G. Effect of thyme oil and thymol dietary supplementation on the antioxidant status and fatty acid composition of the ageing rat brain. Brit. J. Nutr. 2000;83:87–93. [PubMed] [Google Scholar]
- 59.Yanishlieva N.V., Marinova E.M., Gordon M.H., Raneva V.G. Antioxidant activity and mechanism of action of thymol and carvacrol in two lipid systems. Food Chem. 1999;64:59–66. doi: 10.1016/S0308-8146(98)00086-7. [DOI] [Google Scholar]
- 60.Prieto J.M., Iacopini P., Cioni P., Chericoni S. In vitro activity of the essential oils of Origanum vulgare, Satureja montana and their main constituents in peroxynitrite-induced oxidative processes. Food Chem. 2007;104:889–895. [Google Scholar]
- 61.Haeseler G., Maue D., Grosskreutz J., Bufler J., Nentwig B., Piepenbrock S., Dengler R., Leuwer M. Voltage-dependent block of neuronal and skeletal muscle sodium channels by thymo land menthol. Eur. J. Anaesthesiol. 2002;19:571–579. doi: 10.1017/s0265021502000923. [DOI] [PubMed] [Google Scholar]
- 62.Karpanen T.J., Worthington T., Hendry E.R., Conway B.R., Lambert P.A. Antimicrobial efficacy of chlorhexidine digluconate alone and in combination with eucalyptus oil, tea tree oil and thymol against planktonic and biofilm cultures of Staphylococcus epidermidis. J. Antimicrob. Chemother. 2008;62:1031–1036. doi: 10.1093/jac/dkn325. [DOI] [PubMed] [Google Scholar]
- 63.Mastelic J., Jerkovic I., Blazevic I., Poljak-Blazi M., Borovi S., Ivancic-Bace I., Smrecki V., Zarkovic N., Brci-Kostic K., Vikic-Topic D.Z., et al. Comparative study on the antioxidant and biological activities of carvacrol, thymol and eugenol derivatives. J. Agric. Food Chem. 2008;56:3989–3996. doi: 10.1021/jf073272v. [DOI] [PubMed] [Google Scholar]
- 64.Riella K.R., Marinho R.R., Santos J.S., Pereira-Filho R.N., Cardoso J.C., Albuquerque-Junior R.L.C., Thomazzi S.M. Anti-inflammatory and cicatrizing activities of thymol, a monoterpene of the essential oil from Lippia. gracilis, in rodents. J. Ethnopharmacol. 2012;143:656–663. doi: 10.1016/j.jep.2012.07.028. [DOI] [PubMed] [Google Scholar]
- 65.Denkinger M.D., Nikolaus T., Denkinger C., Lukas A. Physical activity for the prevention of cognitive decline. Current evidence from observational and controlled studies. Z. Gerontol. Geriatr. 2012;45:11–16. doi: 10.1007/s00391-011-0262-6. [DOI] [PubMed] [Google Scholar]
- 66.Khorshid F., Ali S.S., Alsofyani T., Albar H. Plectranthustenuiflorus (Shara) promoteswoundhealing: In vitro and in vivo studies. Int. J. Bot. 2010;6:69–80. doi: 10.3923/ijb.2010.69.80. [DOI] [Google Scholar]
- 67.Badr G., Alwasel S., Ebaid H., Mohany M., Alhazza I. Perinatal supplementation with thymoquinone improves diabetic complications and T cell immune responses in rat offspring. Cell. Immunol. 2011;267:133–140. doi: 10.1016/j.cellimm.2011.01.002. [DOI] [PubMed] [Google Scholar]
- 68.Amirghofran Z., Hashemzadeh R., Javidnia K., Golmoghaddam H., Esmaeilbeig A. In vitro immunomodulatory effects of extracts from three plants of the Labiatae family and isolation of the active compound(s) J. Immunotoxicol. 2011;8:265–273. doi: 10.3109/1547691X.2011.590828. [DOI] [PubMed] [Google Scholar]
- 69.Villegas L.F., Marçalo A., Martin J., Fernández I.D., Maldonado H., Vaisberg A.J., Hammond G.B. (+)-epi-α-Bisbolol is the wound-healing principle of Peperomia. galioides: Investigation of the in vivo wound-healing activity of related terpenoids. J. Nat. Prod. 2001;64:1357–1359. doi: 10.1021/np0102859. [DOI] [PubMed] [Google Scholar]
- 70.Dagne E., Bisrat D., Alemayehu M., Worku T. Essential oils of twelve eucalyptus species from Ethiopia. J. Essent. Oil Res. 2000;12:467–470. doi: 10.1080/10412905.2000.9699567. [DOI] [Google Scholar]
- 71.Khalil Z., Pearce A.L., Satkunanathan N., Storer E., Finlay-Jones J.J., Hart P.H. Regulation of wheal and flare by tea tree oil: Complementary human and rodent studies. J. Invest. Dermatol. 2004;123:683–690. doi: 10.1111/j.0022-202X.2004.23407.x. [DOI] [PubMed] [Google Scholar]
- 72.Kawata J., Kameda M., Miyazawa M. Cyclooxygenase-2 inhibitory effects of monoterpenoids with a p-methane skeleton. Int. J. Essent. Oil Ther. 2008;2:145–148. [Google Scholar]
- 73.Hassan S.B., Gali-Muhtasib H., Göransson H., Larsson R. Alpha terpineol: A potential anticancer agent which acts through suppressing NF-kappaB signalling. Anticancer Res. 2010;30:1911–1919. [PubMed] [Google Scholar]
- 74.Held S., Schieberle P., Somoza V. Identification of α-terpineol as an anti-inflammatory component of orange juice by in vitro and ex vivo studies; Recent Highlights in Flavor Chemistry & Biology; Proceedings of the Wartburg Symposium on Flavor Chemistry and Biology; Eisenach, Germany. 27 February–2 March 2007; Garching, Germany: Deutsche Forschungsanstalt für Lebensmittelchemie; 2007. pp. 239–244. [Google Scholar]
- 75.Oliveira M.G., Marques R.B., de Santana M.F., Santos A.B., Brito F.A., Barreto E.O., de Sousa D.P., Almeida F.R., Badauê-Passos D.J., Antoniolli A.R., et al. α-erpineol reduces mechanical hypernociception and inflammatory response. Basic. Clin. Pharmacol. Toxicol. 2012;111:120–125. doi: 10.1111/j.1742-7843.2012.00875.x. [DOI] [PubMed] [Google Scholar]
- 76.Park S.N., Lim Y.K., Freire M.O., Cho E., Jin D., Kook J.K. Antimicrobial effect of linalool and α-terpineol against periodontopathic and cariogenic bacteria. Anaerobe. 2012;18:369–372. doi: 10.1016/j.anaerobe.2012.04.001. [DOI] [PubMed] [Google Scholar]
- 77.Park M.J., Gwak K.S., Yang I., Kim K.W., Jeung E.B., Chang J.W., Choi I.G. Effect of citral, eugenol, nerolidol and α-terpineol on the ultrastructural changes of Trichophyton. mentagrophytes. Fitoterapia. 2009;80:290–296. doi: 10.1016/j.fitote.2009.03.007. [DOI] [PubMed] [Google Scholar]
- 78.Jin J., Song M., Hourston D.J. Novel chitosan based films cross-linked by genipin with improved physical properties. Biomacromolecules. 2004;5:162–168. doi: 10.1021/bm034286m. [DOI] [PubMed] [Google Scholar]
- 79.González A., Strumia M.C., Alvarez Igarzabal C.I. Cross-linked soy protein as material for biodegradable films: Synthesis, Characterization and biodegradation. J. Food Eng. 2011;106:331–338. [Google Scholar]
- 80.Pujana M.A., Pérez-Álvarez L., Iturbe L.C.C., Katime I. Biodegradable chitosan nanogels crosslinked with genipin. Carbohydr. Polym. 2013;94:836–842. doi: 10.1016/j.carbpol.2013.01.082. [DOI] [PubMed] [Google Scholar]
- 81.Zhang K., Qian Y., Wang H., Fan L., Huang C., Yin A., Mo X. Genipin-crosslinked silk fibroin/hydroxybutyl chitosan nanofibrous scaffolds for tissue-engineering application. J. Biomed. Mat. Res. A. 2010;95A:870–881. doi: 10.1002/jbm.a.32895. [DOI] [PubMed] [Google Scholar]
- 82.Chang W.H., Chang Y., Lai P.H., Sung H.W. A genipin-crosslinked gelatin membrane as wound-dressing material: In vitro and in vivo studies. J. Biomater. Sci. Polymer Edn. 2003;14:481–495. doi: 10.1163/156856203766652084. [DOI] [PubMed] [Google Scholar]
- 83.Sung H.W., Huang R.N., Huang L.L., Tsai L.L. In vitro evaluation of cytotoxicity of a naturally occurring cross-linking reagent for biological tissue fixation. J. Biomater. Sci. Polym. Ed. 1999;10:63–78. doi: 10.1163/156856299X00289. [DOI] [PubMed] [Google Scholar]
- 84.Nam K.N., Choi Y.S., Jung H.J., Park G.H., Park J.M., Moon S.K., Cho K.H., Kang C., Kang I., Myung S.O., et al. Genipin inhibits the inflammatory response of rat brain microglial cells. Int. Immunopharmacol. 2010;10:493–499. doi: 10.1016/j.intimp.2010.01.011. [DOI] [PubMed] [Google Scholar]
- 85.Wang G.F., Wu S.Y., Rao J.J., Lu L., Xu W., Pang J.X., Liu Z.Q., Wu S.G., Zhang J.J. Genipin inhibits endothelial exocytosis via nitric oxide in cultured human umbilical vein endothelial cells. Acta Pharmacol. Sin. 2009;30:589–596. doi: 10.1038/aps.2009.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Koo H.J., Song Y.S., Kim H.J., Park E.H. Antiinflammatory effects of genipin, an active principle of gardenia. Eur. J. Pharmacol. 2004;495:201–208. doi: 10.1016/j.ejphar.2004.05.031. [DOI] [PubMed] [Google Scholar]
- 87.Parton L.E., Ye C.P., Coppari R. Glucose sensing by POMC neurons regulates glucose homeostasis and is impaired in obesity. Nature. 2007;449:228–233. doi: 10.1038/nature06098. [DOI] [PubMed] [Google Scholar]
- 88.Kitano A., Saika S., Yamanaka O., Ikeda K., Reinach O.S., Nakajima Y., Okada Y., Shirai K., Ohnishi Y. Genipin suppresses subconjunctival fibroblast migration, proliferation and myofibroblast transdifferentiation. Ophthalmic. Res. 2006;38:355–360. doi: 10.1159/000096231. [DOI] [PubMed] [Google Scholar]
- 89.Kitano A., Saika S., Yamanaka O., Reinach P.S., Ikeda K., Okada Y., Shirai K., Ohnishi Y. Genipin suppression of fibrogenic behaviors of the alpha-TN4 lens epithelial cell line. J. Cataract. Refract. Surg. 2006;32:1727–1735. doi: 10.1016/j.jcrs.2006.05.015. [DOI] [PubMed] [Google Scholar]
- 90.Ishiguro K., Yamaki M., Takagi S. Studies on the iridoid related compound. I. On the antimicrobial activity of aucubigenin and certain iridoid aglycones. Yakugaku Zasshi. 1982;102:755–759. doi: 10.1248/yakushi1947.102.8_755. [DOI] [PubMed] [Google Scholar]
- 91.Davini E., Iavarone C., Trogolo C., Aureli P., Pasolini B. The quantitative isolation and antimicrobial activity of the aglycone of aucubin. Phytochemistry. 1986;25:2420–2422. doi: 10.1016/S0031-9422(00)81711-2. [DOI] [Google Scholar]
- 92.Yuan C.S., Zhang Q., Xie W.D., Yang X.P., Jia Z.J. Iridoids from Pedicularis kansuensis forma albiflora. Pharmazie. 2003;58:428–430. [PubMed] [Google Scholar]
- 93.Recio M.C., Giner R.M., Máñez S., Ríos J.L. Structural considerations on the iridoids as anti-inflammatory agents. Plant Med. 1994;60:232–234. doi: 10.1055/s-2006-959465. [DOI] [PubMed] [Google Scholar]
- 94.Park K.S., Chang I.M. Anti-inflammatory activity of aucubin by inhibition of tumor necrosis factor-alpha production in RAW264.7cells. Plant Med. 2004;70:778–779. doi: 10.1055/s-2004-827211. [DOI] [PubMed] [Google Scholar]
- 95.Shim K.M., Choi S.H., Jeong M.J., Kang S.S. Effects of aucubin on the healing of oral wounds. In Vivo. 2007;21:1037–1041. [PubMed] [Google Scholar]
- 96.Lee S.W., Kho H.S., Lee S.G. The effects of iridoid compounds on wound healing. J. Korean Acad. Oral Med. 1999;24:137–142. [Google Scholar]
- 97.Li F.R., Yang J.X., Shen X.T., Li S.J. Antioxidative activities of aucubin in vitro. J. Shaanxi Norm. Univ. 2004;32:98–101. [Google Scholar]
- 98.Chang I.M., Ryu J.C., Park Y.C., Yun H.S., Yang K.H. Protective activities of aucubin against carbon tetrachloride-induced liver damage in mice. Drug Chem. Toxicol. 1983;6:443–453. doi: 10.3109/01480548309014166. [DOI] [PubMed] [Google Scholar]
- 99.Chang I.M. Liver-protective activities of aucubin derived from traditional oriental medicine. Res. Commun. Mol. Pathol. Pharmacol. 1998;102:189–204. [PubMed] [Google Scholar]
- 100.Chang K.S., Yun H.S., Chang I.M. Effects of aucubin on DNA and RNA biosyntheses in sarcoma 180 cells. Korean Biochem. J. 1989;22:322–326. [Google Scholar]
- 101.Grundy S.M. Obesity, metabolic syndrome and cardiovascular diseases. J. Clin. Endocrinol. MeTable. 2004;89:2595–2600. doi: 10.1210/jc.2004-0372. [DOI] [PubMed] [Google Scholar]
- 102.Park K.S. Aucubin, a naturally occurring iridoid glycoside inhibits TNF-α-induced inflammatory responses through suppression of NF-κB activation in 3T3-L1 adipocytes. Cytokine. 2013;62:407–412. doi: 10.1016/j.cyto.2013.04.005. [DOI] [PubMed] [Google Scholar]
- 103.Hung J.Y., Yang C.J., Tsai Y.M., Huang H.W., Huang M.S. Antiproliferative activity of aucubin is through cell cycle arrest and apoptosis in human non-small cell lung cancer A549 cells. Clin. Exp. Pharmacol. Physiol. 2008;35:995–1001. doi: 10.1111/j.1440-1681.2008.04935.x. [DOI] [PubMed] [Google Scholar]
- 104.Cherng J.M., Shieh D.E., Chiang W., Chang M.Y., Chiang L.C. Aucubin has no effect on proliferation in cancer cells derived from nine human organs, including the lungs. Biosci. Biotechnol. Biochem. 2007;71:1500–1504. doi: 10.1271/bbb.70008. [DOI] [PubMed] [Google Scholar]
- 105.Gálvez M., Martín-Cordero C., Ayuso M.J. Iridoids as DNA topoisomerase I poisons. J. Enzyme Inhib. Med. Chem. 2005;20:389–392. doi: 10.1080/14756360500141879. [DOI] [PubMed] [Google Scholar]
- 106.Liberati A., Altman D.G., Tetzlaff J., Mulrow C., Gøtzsche P.C., Ioannidis J.P.A., Clarke M., Devereaux P.J., Kleijnen J., Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. BMJ. 2009;339:b2700. doi: 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Tholl D. Terpene synthases and the regulation, diversity and biological roles of terpene metabolism. Cur. Opin. Plant Biol. 2006;9:297–304. doi: 10.1016/j.pbi.2006.03.014. [DOI] [PubMed] [Google Scholar]