Abstract
Background
Bispectral index (BIS) monitoring of depth of anesthesia has pioneered the field for more recent monitoring devices like the A-line ARX Index (AAI) or the state (SE) and response entropy (RE) monitoring devices. Following an observational design the present study aimed to simultaneously compare in the same patient recorded BIS, AAI and entropy values.
Methods
Data from patients (n = 32) undergoing minor gynecological operations were analyzed. For all patients, standardized anesthesia was used. Before induction of anesthesia AEP electrodes, BIS and entropy sensors were simultaneously placed on the forehead and recordings were started at 3 minutes before induction and continued until patient transfer to the postanesthesia care unit. Markers were set at defined landmarks.
Results
Anesthesia reduced mean BIS, AAI and entropy values. During uneventful, and even more pronounced, during eventful anesthesia BIS/ entropy and BIS/ AAI values showed better correlation than did AAI and entropy values. The prediction probability (Pk) of AAI (0.824 ± 0.036) and RE (0.786 ± 0.040) or SE (0.781 ± 0.040) for preanesthesia awake, postanesthesia awake or anesthesia was comparable and significantly greater than that of BIS (0.705 ± 0.047). However, only 20% of BIS, AAI and entropy values simultaneously categorized the state of the patient as awake, inadequate anesthesia, optimal anesthesia or deep anesthesia.
Conclusion
The prediction probability (Pk) of entropy and AAI was comparable and better than that of BIS. However, agreement between BIS, AAI and entropy measurements on patient state was poor.
Keywords: Bispectral index (BIS), A-line ARX Index (AAI) State (SE) response (RE) Entropy, Depth of anaesthesie prediction probability (Pk), Same patient
1. Introduction
The upsurge of interest in measuring depth of anesthesia is without doubt favored by the increased number of on-line depth-of-anesthesia monitoring devices available. Beyond this seemingly commercially fueled driving force, scientific evidence has substantiated that monitoring depth of anesthesia (e.g. bispectral index (BIS) monitoring) indeed reduced awareness in a defined patient population [1].
Apart from BIS, monitoring of auditory evoked potentials (e.g. A-line ARX Index (AAI)) and lately state (SE) and response entropy (RE) have become available to measure depth of anesthesia. Evaluation of these different concepts for monitoring depth of anesthesia is hampered by the absence of a “gold standard” depth-of-anesthesia monitoring device. Simultaneous use of these monitoring devices in the same patient does not circumvent this problem, but does allow for direct comparison at given endpoints. Following this approach Vanluchene-AL et al. already shows in the year 2004, comparable prediction probability for BIS, the A-line ARX Index (AAI), RE and SE for propofol effect site concentration [2]. Comparison of these three anesthetic depth monitors based on manually recorded readings taken every five minutes during mildly hypothermic (34°C) cardiopulmonary bypass showed “good agreement” for 62% of recorded paired indices [3]. The influence of temperature on EEG per se, however, has previously been shown [4].
Following an observational design the present study aimed to compare BIS, AAI, SE and RE values in the same patient at normothermia undergoing general anesthesia with propofol and remifentanil with regard to classification of depth of anesthesia.
2. Material and methods
Following approval by the local University Ethics Committee and written informed consent, patients (n = 32; ASA physical status I-III) scheduled for elective minor gynecological surgery were enrolled. All patients were premedicated with midazolam (0.1 mg/ kg, p.o., with a maximal dosage of 7.5mg p.o.). Boluses of fentanyl (2 mcg/ kg) and approx. three minutes later of propofol (2 – 3 mg/ kg) were given to induce anesthesia. To maintain anesthesia propofol (5 mg/ kg/ h) and remifentanil (0.2 – 0.4 mcg/ kg / min) were infused. At the anesthetist’s preference, either an endotracheal tube or a laryngeal mask was used for airway management. In the case of an endotracheal tube a remifentanil bolus (3 - 5 mcg/ kg) was given to facilitate intubation [5]. Normoventilation (EtCO2 = 40 ± 5 mmHg) was maintained throughout the procedure.
Entropy quantifies the probability density function of the distribution of values. Hypnotic drugs cause the probability density function to broaden and flatten, thereby changing from a skewed distribution to a more uniform distribution. The GE EntropyTM Module (it was developed by Datex-Ohmedam, now part of GE Healthcare) measures these changes by quantifying the irregularity of the EEG signals [6]. State entropy (SE) and response entropy (RE) values are generated. SE measures EEG activity up to a frequency of 32 Hz. RE includes frequencies up to 47 Hz for EEG and facial EMG activity.
The bispectral index (BIS) integrates several disparate descriptors of the EEG to form a single value [7]. For signal acquisition the Datex-Ohmeda BISTM module (S/5 BIS-Module, Datex-Ohmeda, Helsinki, Finland) was used.
Both BIS and entropy (e.g. RE and SE) values are given on a scale from 0 (isoelectric EEG) to 100 (awake). Values below 40 indicate deep anesthesia, values from 40 to 60 optimal and above 60 but below 90 inadequate anesthesia. In awake patients BIS and RE values are typically over 90, whereas SE values do not exceed 91 (Table 1) [6,7].
Table 1.
Defines patient state (awake, inadequate anesthesia, optimal anesthesia and deep anesthesia) in terms of bispectral index (BIS), A-line ARX Index (AAI), state entropy (SE) and response entropy (RE) values according to the manufacturer.
| awake | inadequate anesthesia | optimal anesthesia | deep anesthesia | |
|---|---|---|---|---|
| BIS | 90 – 100 | 61 – 89 | 40 – 60 | 0 – 39 |
| SE | 90 - 91 | 61 – 89 | 40 – 60 | 0 – 39 |
| RE | 90 – 100 | 61 – 89 | 40 – 60 | 0 – 39 |
| AAI | 60 – 100 | 26 – 59 | 15 – 25 | 0 – 14 |
Mid-latency auditory evoked potentials following bilateral click stimuli of 65 dB intensity and 2 ms duration applied through a pair of headphones with a repetition rate of 9 Hz were recorded with the ALARIS AEP® monitor (Danmeter, Odense, Denmark; software version 1.5). Artifact-cleared EEG sweeps were used for on-line calculation of the A-line ARX Index (AAI) [8]. AAI values below 15 indicate “deep anesthesia”, between 15 and 25 “optimal anesthesia”, and above 25 but below 60 “inadequate anesthesia”. In awake patients AAI values are typically over 60 (Table 1) [9].
Before induction of anesthesia commercially available AEP electrodes (silver-silver chloride electrodes, Alaris Medical System, UK), BIS (BISTM Quatro Sensor XP, Datex-Ohmeda, Helsinki, Finland) and entropy sensors (EntropyTM Sensor, Datex-Ohmeda, Helsinki, Finland) were simultaneously placed on the right (BIS) and left (entropy) side of the forehead of each patient as specified by the manufacturer. To ensure optimal signal quality the skin of the forehead was prepared with skin prep (Trace Prep, 3M Red Dot TM, Ontario, Canada).
Simultaneous BIS, AAI and entropy value recordings with a standard PC for subsequent off-line analysis were started at 3 minutes before induction of anesthesia and continued until patient transfer to the postanesthesia care unit (PACU). The anesthetist responsible for the patient was blinded to AAI, BIS and entropy values during the operation.
Markers were set at defined landmarks (e.g. “monitoring start”, “induction of anesthesia”, “skin incision”, “discontinuation of propofol infusion”, “extubation”, “patient transfer to postanesthesia care unit (PACU)”) along the routine course of the operation, but also for patient movement provoked by surgical stimulus. Three distinct clinical states (e.g. preanesthesia awake, postanesthesia awake, and anesthesia) were defined, whereby “preanesthesia awake” included all values from “monitoring start” to “induction of anesthesia”, “postanesthesia awake” all values from “extubation” to “patient transfer to PACU” and “anesthesia” all values from “skin incision” to “discontinuation of propofol infusion”.
3. Statistical analysis
Data are presented as mean ± SD (range). Normality of distribution was assessed when necessary using the Kolmogorov-Smirnov Test. Analysis of variance (ANOVA) for repeated measurements with Least-Square-Difference (LSD) correction for multiple testing was used to compare BIS, AAI and entropy (e.g. RE and SE) values during “preanesthesia awake” with values during “postanesthesia awake” but also with values during “anesthesia”. The ANOVA was applied to the mean values for each patient in each state [10]. Therefore, patients with missing values in one state were dropped. The correction factor for the degrees of freedom was calculated according to Box [11], Geisser and Greenhouse [12] and Huynh and Feldt [13]. In order to test whether the means of the non-movers during anesthesia differ significantly from those of the movers a T test was conducted.
The prediction probability (Pk) [14] of BIS, AAI and entropy for preanesthesia awake, postanesthesia awake and anesthesia was computed with a proprietary program (J.W.). Pk uses the rank ordering of the indicator value and the observed anesthetic depth (i.e. 1 = “preanesthesia awake”, 2 = “postanesthesia awake” and 3 = “during anesthesia”) for a pair of data points.
A Pk of 1 for the anesthetic depth indicators means that the indicator always decreases (increases) as the patient’s depth of anesthesia increases (decreases). Alternatively, a Pk of 0.5 means that the anesthetic depth indicator is useless for predicting the state of anesthesia. Subsequently, the Pk values of BIS, AAI, state (SE) and response entropy (RE) were paired-data-wise compared [14,15].
Moreover, Pearson’s correlation coefficient (r) was calculated between BIS, AAI and entropy values during preanesthesia awake, postanesthesia awake and anesthesia.
In a merely descriptive approach for each clinical state (e.g. preanesthesia awake, postanesthesia awake, anesthesia) the overall percentage of BIS, AAI and entropy values categorizing the state of the particular patient as awake, inadequate anesthesia, optimal anesthesia or deep anesthesia (Table 1) was determined. Additionally, agreement between the three monitors was defined as the percentage of BIS, AAI and entropy values simultaneously categorizing the state of the patient as awake, inadequate anesthesia, optimal anesthesia or deep anesthesia.
Furthermore, agreement between indices with the same scale (e.g. BIS, RE, and SE (except “awake”)) was evaluated using a Bland-Altman analysis [19]. The 95% confidence interval (CI) of the mean difference between BIS and RE (SE) served to test the null hypothesis that this difference did not significantly differ from 0. The limits of agreement were defined as the lower (upper) limit of the 95% CI of the mean difference minus (plus) 1.96*SD.
In the case of patient movement provoked by surgical stimulus heart rate (HR), BIS, AAI and entropy values at 120 seconds before movement were compared with those obtained 110 seconds before to 60 seconds following movement using ANOVA for repeated measurements.
A P ≤ 0.05 was considered statistically significant. The statistical computer package STATA/SE 9.1 for Windows was used for statistical analysis. Computation of the Pk was implemented in MATLAB ® 7.0.4 (R14 Service Pack 2).
4. Results
All patients enrolled (n = 32; female, age 43 ± 15 years, weight 67 ± 14 kg, height 163 ± 17 cm) completed the study without complication. Gynecological operations (n = 32) performed included curettage (10), mastectomy (6), knife or loop conization (5), laparoscopy (5), Human Papilloma virus (HPV) ablative therapy (3), abscess incision (2) hysterectomy (1). Laryngeal mask (n = 24 ) and endotracheal tube (n = 8) were used for airway management.
Technical quality of BIS, AAI, and entropy recordings was partly insufficient. In order to obtain a balanced design for ANOVA for repeated measurements patients with missing values in one state were dropped from the analysis (Table 2). Anesthesia reduced mean BIS, AAI and entropy values (Table 2). Postanesthesia awake BIS and SE values were lower than corresponding preanesthesia values (Table 2).
Table 2.
a) Descriptive analysis of all data collected
| awake (pre) | anesthesia | awake (post) | |
|---|---|---|---|
| (n = 29) | (n = 32) | (n = 27) | |
| (nT = 541) | (nT = 14,651) | (nT = 222) | |
| mean ± SD (range) | mean ± SD (range) | mean ± SD (range) | |
| BIS | 96 ± 3 (77 – 98) | 35 ± 11 (8 – 96) | 78 ± 9 (52 – 97) |
| SE | 87 ± 6 (24 – 92) | 40 ± 14 (3 – 92) | 81 ± 12 (45 – 91) |
| RE | 97 ± 5 (36 – 100) | 42 ± 16 (3 – 100) | 90 ± 13 (48 – 100) |
| AAI | 76 ± 15 (29 – 99) | 21 ± 12 (4 – 93) | 69 ± 23 (14 – 99) |
Table 2.
b) Descriptive analysis of data from patients with valid measurements in each state
| awake (pre) | anesthesia | awake (post) | |
|---|---|---|---|
| (n = 25) | (n = 25) | (n = 25) | |
| (nT = 467) | (nT = 9,991) | (nT = 179) | |
| mean ± SD (range) | mean ± SD (range) | mean ± SD (range) | |
| BIS | 96 ± 4 (77 – 98) | 36 ± 12 (8 – 96) 1 | 80 ± 8 (52 – 97) 1,2 |
| SE | 87 ± 7 (24 – 92) | 39 ± 13 (5 – 92) 1 | 84 ± 9 (45 – 91) 1,2 |
| RE | 97 ± 6 (36 – 100) | 42 ± 15 (5 – 100) 1 | 94 ± 8 (56 – 100) 2 |
| AAI | 75 ± 16 (29 – 99) | 22 ± 13 (4 – 93) 1 | 78 ± 15 (24 – 99) 2 |
Table 2 part a) gives descriptive statistics of all bispectral index (BIS), A-line ARX Index (AAI), response entropy (RE) and state entropy (SE) values collected during preanesthesia awake (awake pre), postanesthesia awake (awake post), and anesthesia (anesthesia).
Part b) summarizes only data from patients with valid measurements in each state, which were used for ANOVA with repeated measurements and post hoc analysis. Details of ANOVA are given in Appendix 1 (Appendix 1).
nT number of data pairs (number of patients × number of recorded time points)
1 significant to awake (pre), P ≤ 0.05
2 significant to anesthesia, P ≤ 0.05
During anesthesia BIS, AAI and RE mean values were significantly lower in patients without movement (non-movers) than in those with movement (movers) (Table 3).
Table 3.
Gives bispectral index (BIS), A-line ARX Index (AAI), response entropy (RE) and state entropy (SE) values during uneventful (non-movers) and eventful anesthesia (movers) (e.g. occurrence of patient movement provoked by surgical stimulus).
| anesthesia | anesthesia | |
|---|---|---|
| movers (n = 6) | non-movers (n = 26) | |
| (nT = 1,965) | (nT = 12,686) | |
| mean ± SD (range) | mean ± SD (range) | |
| BIS | 42 ± 15 (17 – 96) | 34 ± 10 (8 – 78) 1 |
| SE | 44 ± 18 (11 – 92) | 39 ± 13 (3 – 89) |
| RE | 49 ± 20 (12 – 100) | 41 ± 15 (3 – 100) 1 |
| AAI | 33 ± 20 (5 – 93) | 19 ± 9 (4 – 84) 1 |
nT number of data pairs (number of patients × number of recorded time points)
1 significant to movers, P ≤ 0.05
The sample Pk estimates obtained using equation (1) are for AAI 0.824, for RE 0.787, for SE 0.781, and for BIS 0.706. The jackknife Pk estimates and standard errors are given as (0.824 ± 0.036) for AAI, (0.786 ± 0.040) for RE, (0.781 ± 0.040) for SE and (0.705 ± 0.047) for BIS. All Pk values differ significantly from 0.5 (P ≤ 0.001). Paireddata jackknife comparison of the Pk values for alternative indicators showed the Pk values for BIS to be significantly lower than for SE (t = 3.12, P < 0.05), RE (t = 3.26, P < 0.05), or AAI (t = 3.72, P < 0.05). The Pk for AAI was comparable to that for SE (t = 1.48, P > 0.10) and RE (t = 1.29, P > 0.10).
Correlations between BIS, AAI and entropy values differed significantly from zero during anesthesia, postanesthesia awake and partly during preanesthesia awake (Table 4). Generally, all devices showed better correlation during postanesthesia awake than during preanesthesia awake (BIS vs SE: ZSteiger2 = 6.18, ZOlkinFinn2 = 6.77, P < 0.05; BIS vs RE: ZSteiger2 = 6.35, ZOlkinFinn2 = 6.98, P < 0.05). Correlation during uneventful anesthesia (non-movers) was less than during eventful anesthesia (movers) (Table 4) (Appendix 3). Overall, the devices BIS/ SE and BIS/ RE in patients with movement during anesthesia (movers) showed significantly greater correlation than during postanesthesia awake (BIS/ SE: ZSteiger2 = 6.67, ZOlkinFinn2 = 5.26, P < 0.05; BIS/ RE: ZSteiger2 = 6.37, ZOlkinFinn2 = 5.03, P < 0.05) (Table 4). Correlation between BIS/ SE, RE and BIS/ AAI during anesthesia was significantly greater than between AAI and entropy (Table 4) (Appendix 2). Finally, correlation between SE and RE, which is given for reasons of completeness, was greater during anesthesia than during postanesthesia (ZSteiger2 = 12.82; ZOlkinFinn2 = 27.90, P < 0.05) or preanesthesia awake (ZSteiger2 = 18.36; ZOlkinFinn2 = 9.54, P < 0.05) (Table 4).
Table 4.
presents Pearson’s correlation coefficient (r) between bispectral index (BIS), A-line ARX Index (AAI), and state entropy (SE) or response entropy (RE) values during preanesthesia awake (awake pre), postanesthesia awake (awake post), uneventful (anesthesia non-movers) and eventful anesthesia (anesthesia movers) (e.g. occurrence of patient movement provoked by surgical stimulus). Detailed results of correlation coefficient comparisons are given in the appendix (Appendix 3, Appendix 4). Correlation between SE and RE is given for the sake of completeness only.
| awake (pre) | anesthesia | awake (post) | ||
|---|---|---|---|---|
| non-movers | movers | |||
| (nT = 541) | (nT = 12,686) | (nT = 1,965) | (nT = 222) | |
| r | r | r | r | |
| BIS-vs-SE | 0.090* | 0.463* | 0.786* | 0.527* |
| BIS-vs-RE | 0.122* | 0.439* | 0.795* | 0.559* |
| BIS-vs-AAI | -0.004 | 0.443* | 0.593* | 0.541* |
| AAI-vs-SE | 0.016 | 0.269* | 0.446* | 0.635* |
| AAI-vs-RE | -0.010 | 0.235* | 0.443* | 0.714* |
| SE-vs-RE | 0.941* | 0.988* | 0.977* | 0.933* |
significantly different from zero, P < 0.05
During preanesthesia awake approximately 97% of RE and 91% of BIS but only 84% of AAI values indicated awake (Table 5). In contrast, during postanesthesia awake approximately 71% of RE and AAI but only 8% of BIS values indicated awake (Table 5).
Table 5.
Gives percentage of bispectral index (BIS), A-line ARX Index (AAI), response entropy (RE) and state entropy (SE) values for each clinical state of the patient (state clinic) (e.g. preanesthesia awake (awake pre), postanesthesia awake (awake post), eventful anesthesia (movers), uneventful anesthesia (non-movers)) and the state as defined by the monitor (state monitor) (e.g. awake (awake), inadequate anesthesia (inadequate), optimal anesthesia (optimal), deep anesthesia (deep)).
| state clinic | state monitor | BIS | SE | RE | AAI |
|---|---|---|---|---|---|
| (%) | (%) | (%) | (%) | ||
| awake pre | awake | 90.94 | 12.01 | 97.41 | 83.92 |
| (nT = 541) | inadequate | 9.06 | 86.51 | 2.03 | 16.08 |
| optimal | 0.00 | 1.11 | 0.37 | 0.00 | |
| deep | 0.00 | 0.37 | 0.18 | 0.00 | |
| anesthesia movers | awake | 0.97 | 1.58 | 6.62 | 13.99 |
| (nT = 1,965) | inadequate | 9.57 | 11.86 | 16.95 | 40.51 |
| optimal | 40.51 | 43.16 | 38.07 | 29.41 | |
| deep | 48.96 | 43.41 | 38.37 | 16.08 | |
| anesthesia non-movers | awake | 0.00 | 0.00 | 3.07 | 0.31 |
| (nT = 12,686) | inadequate | 1.70 | 4.97 | 4.29 | 20.05 |
| optimal | 21.13 | 38.55 | 45.29 | 43.00 | |
| deep | 77.17 | 56.48 | 47.36 | 36.65 | |
| awake post | awake | 8.11 | 7.66 | 70.72 | 71.17 |
| (nT = 222) | inadequate | 90.54 | 83.78 | 25.68 | 25.68 |
| optimal | 1.35 | 8.56 | 3.60 | 2.70 | |
| deep | 0.00 | 0.00 | 0.00 | 0.45 |
During uneventful anesthesia (non-movers) (n = 27) approximately 40% of AAI and entropy but only 20% of BIS values indicated optimal anesthesia (Table 5). Deep anesthesia was indicated more often by BIS than by entropy or AAI values (Table 5). Inadequate anesthesia, in contrast, was more often indicated by AAI than by entropy or BIS values (Table 5).
During eventful anesthesia (movers) (e.g. occurrence of patient movement provoked by surgical stimulus) (n = 6) BIS and entropy indicated optimal and deep (e.g. approx. 40%) but also inadequate (e.g. approx. 10% - 15%) anesthesia with comparable frequencies (Table 5). AAI values, in contrast, indicated more often awake and inadequate anesthesia (Table 5).
During preanesthesia awake, agreement between BIS, entropy (e.g. SE, RE) and AAI on patient state was about 12% (Table 6). During postanesthesia awake and anesthesia, agreement between BIS, entropy (e.g. SE, RE) and AAI was comparable and ranged from 5% to 18% (Table 6).
Table 6.
Gives percentage of agreement between bispectral index (BIS), A-line ARX Index (AAI), response entropy (RE) and state entropy (SE) values for each clinical state of the patient (state clinic) (e.g. preanesthesia awake (awake pre), postanesthesia awake (awake post), eventful anesthesia (movers), uneventful anesthesia (non-movers)) and the state as defined by the monitor (state monitor) (e.g. awake (awake), inadequate anesthesia (inadequate), optimal anesthesia (optimal), deep anesthesia (deep)).
| state clinic | state monitor | BIS + SE + RE + AAI | BIS + SE + AAI | BIS + RE + AAI | SE + RE |
|---|---|---|---|---|---|
| (%) | (%) | (%) | (%) | ||
| awake pre | awake | 11.65 | 11.65 | 73.20 | 12.01 |
| (nT = 541) | inadequate | 0.00 | 0.37 | 0.00 | 1.11 |
| optimal | 0.00 | 0.00 | 0.00 | 0.18 | |
| deep | 0.00 | 0.00 | 0.00 | 0.18 | |
| anesthesia movers | awake | 0.20 | 0.20 | 0.97 | 1.58 |
| (nT = 1,965) | inadequate | 1.53 | 2.29 | 1.98 | 6.82 |
| optimal | 3.77 | 5.60 | 3.97 | 33.03 | |
| deep | 6.51 | 8.24 | 6.51 | 38.37 | |
| anesthesia non-movers (nT = 12,686) | awake inadequate | 0.00 0.50 | 0.00 0.59 | 0.00 0.67 | 0.00 1.92 |
| optimal | 4.52 | 4.69 | 5.28 | 36.17 | |
| deep | 19.23 | 22.64 | 19.23 | 47.36 | |
| awake post | awake | 4.50 | 4.50 | 7.66 | 7.66 |
| (nT = 222) | inadequate | 17.12 | 21.17 | 18.92 | 21.17 |
| optimal | 0.00 | 0.00 | 0.00 | 3.60 | |
| deep | 0.00 | 0.00 | 0.00 | 0.00 |
Bland-Altman analysis showed the mean difference between BIS and entropy (RE, SE) to differ significantly from 0 for the overall recordings but also during anesthesia (BIS, RE, SE), pre- (BIS, RE) and post-anesthesia awake (BIS, RE) (Table 7). The observed difference ranged from approx. 25 (preanesthesia awake) to 54 (anesthesia) units (Table 7).
Table 7.
Summarizes the results of the Bland-Altman analysis of overall (overall) agreement between bispectral index (BIS), response entropy (RE), and state entropy (SE) values and agreement during preanesthesia awake (awake pre), postanesthesia awake (awake post), and anesthesia (anesthesia). The mean difference and its 95% CI, as well as the mean difference plus/minus 1.96*SD with its 95% CI are reported.
| BIS-RE | ||||
|---|---|---|---|---|
| mean difference | mean difference -1.96*SD | mean difference +1.96*SD | ||
| (95% CI) | (95% CI) | (95% CI) | nT | |
| overall | -6.9 (-7.1 to -6.6) | -33.3 (-33.7 to -32.9) | 19.6 (19.2 to 20.0) | 15414 |
| awake pre | -0.8 (-1.3 to -0.3) | -12.5 (-13.4 to -11.6) | 10.9 (10.0 to 11.8) | 541 |
| anesthesia | -7.0 (-7.2 to -6.8) | -33.8 (-34.2 to -33.4) | 19.8 (19.4 to 20.2) | 14651 |
| awake post | -11.8 (-13.3 to -10.4) | -32.8 (-35.3 to -30.4) | 9.2 (6.7 to 11.6) | 222 |
| BIS-SE | ||||
|---|---|---|---|---|
| mean difference | mean difference -1.96 SD | mean difference +1.96 SD | ||
| (95% CI) | (95% CI) | (95% CI) | nT | |
| overall | -3.9 (-4.1 to -3.7) | -28.0 (-28.3 to -27.6) | 20.2 (19.9 to 20.6) | 15414 |
| awake pre | 9.0 (8.4 to 9.6) | -4.7 (-5.8 to -3.7) | 22.7 (21.7 to 23.8) | 541 |
| anesthesia | -4.4 (-4.5 to -4.2) | -28.3 (-28.6 to -28.0) | 19.6 (19.3 to 19.9) | 14651 |
| awake post | -2.9 (-4.3 to -1.6) | -23.1 (-25.5 to -20.8) | 17.3 (14.9 to 19.7) | 222 |
Nota bene: The reliability of the agreement of BIS and SE values during pre- and postanesthesia awake is impaired since the range of BIS values (90 – 100) indicating “awake” differs from the range of SE values (90 - 91).
nT number of data pairs (number of patients × number of recorded time points)
BIS and entropy values increased significantly only within 60 seconds following movement (Figure 1, Appendix 4). AAI values and heart rate, in contrast, remained stable before and after movement (Figure 1, Appendix 4). None of the enrolled patients postoperatively reported awareness.
Figure 1.
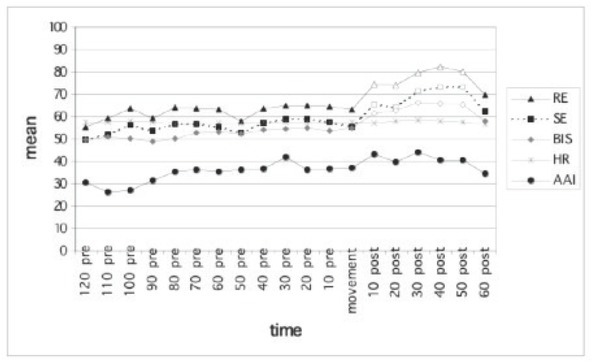
Depicts bispectral index (BIS), A-line ARX Index (AAI), state entropy (SE), response entropy (RE) and heart rate (HR) mean values during 120 s before (pre) and 60 s after (post) patient movement (n = 6) provoked by surgical stimulus. (for details see Appendix 4). not-filled markers significant to the corresponding value at 120 s before movement, (P < 0.05)
5. Discussion
The prediction probability (Pk) of entropy and AAI was comparable and greater than that of BIS. During uneventful and, even more pronounced, during eventful anesthesia BIS/ entropy and to a lesser degree BIS/ AAI values showed greater correlation than did AAI and entropy values. Agreement, however, between BIS, AAI and entropy during preanesthesia awake, postanesthesia awake and anesthesia did not exceed 20%.
Before discussing the results in detail it is important to outline that it was the present study’s clear intention to compare in an observational study design BIS, AAI and entropy values that were simultaneously recorded in each patient. The attending anesthesiologist was always deliberately blinded to the BIS, AAI and entropy readings. Any movement by the patient provoked by surgical stimulation was merely accidental and occurred in some patients (n = 6) as a clinical sign of inadequate anesthesia. In these cases the attending anesthesiologist deepened the state of anesthesia according to routine clinical practice while still being unaware of any depth-of-anesthesia monitor readings.
The hypothesis to be tested was that devices having a comparable capacity to objectively assess the patient’s depth of anesthesia should produce comparable readings, at least with regard to the state of consciousness, e.g. awake and anesthesia, but also with regard to three major states of anesthesia, e.g. deep, optimal and inadequate.
Each device’s ability to detect change in a patient’s state of consciousness was shown by the decrease in mean BIS, AAI and entropy values accompanying an increase in depth of anesthesia. The basic ability of the three devices to detect change in depth of anesthesia was also seen in the significantly greater mean BIS, AAI and RE values in patients with movement (movers). Furthermore, BIS and SE values were significantly lower in the postanesthesia period than in the period before onset of anesthesia. These latter findings indicate a certain degree of sedation, which was in all cases consistent with the clinical evaluation by the attending anesthesiologist.
However, a more appropriate measure for evaluating and comparing the performance of anesthetic depth indicator is the prediction probability (Pk) [14]. The present study’s Pk of AAI (0.824 ± 0.036), RE (0.786 ± 0.040) and SE (0.781 ± 0.040) was comparable for preanesthesia awake, postanesthesia awake or anesthesia and significantly greater than that of BIS (0.705 ± 0.047). These findings stand in contrast to those of others, who reported the Pk of BIS, AAI and entropy to be comparable [2].
According to the hypothesis, tested devices having a comparable capacity to objectively assess a patient’s depth of anesthesia should produce comparable depth-of-anesthesia readings. BIS and entropy devices use a scale from 0 (isoelectric EEG) to 100 (awake) that allow direct comparison of BIS and entropy readings. Since, however, AAI readings are given on a different scale, the present study’s BIS, entropy and AAI readings were categorized according to the manufacturer as awake, inadequate anesthesia, optimal anesthesia or deep anesthesia (Table 1). Thereafter, percentages of BIS, AAI and entropy values in each category were calculated.
During uneventful anesthesia BIS indicated more often deep and AAI more often inadequate anesthesia. During eventful anesthesia (movers), however, AAI values
indicated more often awake and inadequate anesthesia. Furthermore, during postanesthesia awake AAI and RE values predominantly indicated awake (approx. 70%) and somewhat less often inadequate (approx. 26%) anesthesia, whereas BIS and SE values above all indicated inadequate anesthesia. However, categorizing BIS, AAI and entropy values and analyzing the percentages as shown above neglects the time axis on which the BIS, AAI and entropy values were recorded. Therefore, correlation analysis was used as another approach to compare the present study’s simultaneously recorded BIS, AAI and entropy values. The present study’s correlation between BIS and entropy values during uneventful anesthesia was well comparable to that reported previously [20]. Furthermore, during uneventful and, even more pronounced, during eventful anesthesia (e.g. in patients with movement provoked by surgical stimulation) BIS/ entropy and to a lesser degree BIS/ AAI values showed greater correlation than did AAI/ entropy values.
Keeping in mind the above-mentioned time axis, it is of clinical relevance how often BIS, AAI and entropy values agreed on patient state (e.g. awake, inadequate anesthesia, optimal anesthesia or deep anesthesia). The present study’s agreement of BIS, AAI and entropy in normothermic patients was better during anesthesia and postanesthesia awake than during preanesthesia awake, but never exceeded 20%. These findings stand somewhat in contrast to those of Tiren et al. who, when using manually recorded readings taken every five minutes during mildly hypothermic (34°C) cardiopulmonary bypass, reported BIS, AAI and entropy values to agree in about 62% of recorded paired indices [3]. A possible explanation for this is given by the fact that the influence of temperature on EEG per se [4] and on EEG-derived indices (e.g. BIS, AAI and entropy) is well documented [21,22]. It was therefore to be expected that temperature (e.g. normothermia) would have an effect on the present study’s agreement between BIS- and entropy-derived classification of depth of anesthesia.
Another approach to test for agreement between BIS, AAI and entropy values is a Bland-Altman analysis [19], which, however, assumes comparable scales for the indices. This precondition is fulfilled only for BIS (0 – 100), RE (0-100) and SE (0 – 91) values, whereby the latter can range only from 90 –91 for “awake”. During anesthesia the present study’s agreement between BIS and entropy values was poor as differences of more than 50 units were observed. This finding is in accordance with that of others, who previously also reported poor agreement between BIS and entropy values [20].
As previously stated, patient movement during anesthesia was merely accidental and occurred only in a small fraction (6/ 32) of patients. Nevertheless, BIS, AAI and entropy values from 120 seconds before to 60 seconds following movement were analyzed. Only BIS and entropy values increased significantly and only within 60 seconds following movement.
This finding is of interest since, in contrast to the present study, AAI monitoring has previously been shown to predict movement in response to painful stimulus [23]. Prediction of patient movement, however, is an as yet largely unmet demand made of exclusively EEG-based depth-of-anesthesia monitoring devices (e.g. BIS) 14-[24]. Thus, it is not at all unexpected that BIS values in the present study did not increase before but only after patient movement.
Since the RE includes EEG and facial EMG activity, insufficient anesthesia of a patient causes an increase in RE value in response to a pain-induced increase in facial muscular activity [25]. Despite this contribution of facial EMG to RE, a significant increase in RE values prior to movement was not found in patients with movement provoked by surgical stimulation. Only within 60 seconds after movement did entropy values (SE, RE) increase significantly.
Possible points of criticism of our study are as follows. First, we tested only female patients and excluded patients at extreme ages and physiological limits. However it can be assumed that similar findings will be obtained in male patients with comparable preoperative condition. Second of all, we only used propofol/ remifentanil based anaesthesia. Our sample size was too small to address balanced anaesthesia and TIVA. For this purpose further work must be done. Thirdly, all patients were excluded with preexisting brain pathologies or using any centrally acting medications.
In conclusion, in an observational study based on simultaneously recorded BIS, AAI and entropy values we show the prediction probability of entropy and AAI to be comparable and better than that of BIS. Furthermore, during uneventful and, even more pronounced, during eventful anesthesia BIS/ entropy and to a lesser degree BIS/ AAI values showed greater correlation than did AAI or entropy values. In no instance, however, did agreement between BIS, AAI and entropy on patient state (e.g. awake, inadequate anesthesia, optimal or deep anesthesia) exceed 20%.
Appendix
Appendix 1 to Table 2
| Source, BIS | Partial SS | df* | MS | F | P |
|---|---|---|---|---|---|
| Model | 50185.45 | 26 | 1930.21 | 45.46 | 0.0000 |
| Patients | 774.40 | 24 | 32.27 | 0.76 | 0.7639 |
| States | 49411.05 | 2 | 24705.52 | 581.84 | 0.0000 |
| Residual | 2038.13 | 48 | 42.46 | ||
| Total | 52223.58 | 74 | 705.72 |
R2= 0.9610, adjusted R2= 0.9398
* Huynh-Feldt ε = 0.9044, Greenhouse-Geisser ε = 0.8470, Box’s conservative ε = 0.5000
| Source, SE | Partial SS | df* | MS | F | P |
|---|---|---|---|---|---|
| Model | 37474.18 | 26 | 1441.31 | 28.07 | 0.0000 |
| Patients | 2014.40 | 24 | 83.93 | 1.63 | 0.0734 |
| States | 35459.78 | 2 | 17729.89 | 345.24 | 0.0000 |
| Residual | 2465.08 | 48 | 51.36 |
R2= 0.9383, adjusted R2= 0.9048
* Huynh-Feldt ε = 0.9284, Greenhouse-Geisser ε = 0.8669, Box’s conservative ε = 0.5000
| Source, RE | Partial SS | df* | MS | F | P |
|---|---|---|---|---|---|
| Model | 49108.10 | 26 | 1888.77 | 29.99 | 0.0000 |
| Patients | 1914.16 | 24 | 79.76 | 1.27 | 0.2386 |
| States | 47193.94 | 2 | 23596.97 | 374.69 | 0.0000 |
| Residual | 3022.91 | 48 | 62.98 | ||
| Total | 52131.01 | 74 | 704.47 |
R2= 0.9420, adjusted R2= 0.9106
* Huynh-Feldt ε = 0.8401, Greenhouse-Geisser ε = 0.7932, Box’s conservative ε = 0.5000
| Source, AEP | Partial SS | df* | MS | F | P |
|---|---|---|---|---|---|
| Model | 58618.11 | 26 | 2254.54 | 17.37 | 0.0000 |
| Patients | 9059.28 | 24 | 377.47 | 2.91 | 0.0008 |
| States | 49558.83 | 2 | 24779.42 | 190.93 | 0.0000 |
| Residual | 6229.49 | 48 | 129.78 | ||
| Total | 64847.60 | 74 | 876.32 |
R2= 0.9039, adjusted R2= 0.8519
* Huynh-Feldt ε = 0.9914, Greenhouse-Geisser ε = 0.9188, Box’s conservative ε = 0.5000
Appendix 1 summarizes the details of ANOVA for repeated measurements used to test the overall hypothesis that the bispectral index (BIS), A-line ARX Index (AAI), response entropy (RE) and state entropy (SE) values differ significantly during preanesthesia awake (awake pre), postanesthesia awake (awake post), and anesthesia (anesthesia).
SS sum of squares
df degrees of freedom
MS mean sum of squares
Appendix 2 to Table 4
| anesthesia | |||||
|---|---|---|---|---|---|
| non-movers | movers | ||||
| (nT = 12,686) | (nT = 1,965) | ||||
| correlations | ZSteiger1 | ZOlkinFinn1 | ZSteiger1 | ZOlkinFinn1 | P |
| BIS/SE vs AAI/SE | 17.96 | 20.02 | 18.15 | 18.66 | 0.0000 |
| BIS/SE vs AAI/RE | 20.83 | 23.25 | 18.28 | 18.68 | 0.0000 |
| BIS/RE vs AAI/SE | 15.57 | 17.34 | 18.92 | 19.20 | 0.0000 |
| BIS/RE vs AAI/RE | 18.44 | 20.63 | 19.05 | 19.37 | 0.0000 |
| BIS/AAI vs AAI/SE | 15.95 | 17.91 | 6.35 | 7.87 | 0.0000 |
| BIS/AAI vs AAI/RE | 18.81 | 21.02 | 6.48 | 8.06 | 0.0000 |
Appendix 2 details comparison of Pearson’s correlation coefficients (correlations) considering overlapping variables using Steiger’s (ZSteiger 1) [16] and Olkin/ Finn’s (ZOlkinFinn 1) [18] approach for testing dependent correlation coefficients in single group.
nT number of data pairs (number of patients × number of recorded time points)
BIS bispectral index
AAI A-line ARX Index
RE response entropy
SE state entropy
non-movers uneventful anesthesia
movers eventful anesthesia (e.g. occurrence of patient movement provoked by surgical stimulus)
Appendix 3 to Table 4
| anesthesia | |||
|---|---|---|---|
| non-movers (nT = 12,686) vs. movers (nT = 1,965) | |||
| correlations | ZSteiger 2 | ZOlkinFinn2 | P |
| BIS-vs-SE | -23.07 | -29.12 | 0.0000 |
| BIS-vs-RE | -25.30 | -32.46 | 0.0000 |
| BIS-vs-AAI | -8.50 | -9.22 | 0.0000 |
| AAI-vs-SE | -8.41 | -8.91 | 0.0000 |
| AAI-vs-RE | -9.75 | -10.41 | 0.0000 |
| SE-vs-RE | 13.52 | 10.50 | 0.0000 |
Appendix 3 details comparison of independent Pearson’s correlation coefficients (correlations) using Steiger’s (ZSteiger2) [16] and Olkin/ Finn’s approach (ZOlkinFinn2) [18]. Results for SE and RE are given for the sake of completeness only.
nT number of data pairs (number of patients × number of recorded time points)
BIS bispectral index
AAI A-line ARX Index
RE response entropy
SE state entropy
non-movers uneventful anesthesia
movers eventful anesthesia (e.g. occurrence of patient movement provoked by surgical stimulus)
Appendix 4 to Figure 1
| Source, BIS | partial SS | df* | MS | F | Prob. > F |
|---|---|---|---|---|---|
| Model | 16962.75 | 23 | 737.51 | 14.23 | 0.0000 |
| Patients | 13363.76 | 5 | 2672.75 | 51.55 | 0.0000 |
| Time | 3598.99 | 18 | 199.94 | 3.86 | 0.0000 |
| Residual | 4665.88 | 90 | 51.84 | ||
| Total | 21628.63 | 113 | 191.40 |
R2= 0.7843, adj. R2= 0.7291
* Huynh-Feldt ε = 0.1465 (Prob.>F: 0.0390), Greenhouse-Geisser ε = 0.0977 (Prob.>F: 0.0665), Box’s conservative ε = 0.0556 (Prob.>F: 0.1068)
| Source, SE | partial SS | df* | MS | F | Prob. > F |
|---|---|---|---|---|---|
| Model | 15648.04 | 23 | 680.35 | 6.40 | 0.0000 |
| Patients | 10286.62 | 5 | 2057.32 | 19.36 | 0.0000 |
| Time | 5361.42 | 18 | 297.86 | 2.80 | 0.0007 |
| Residual | 9563.58 | 90 | 106.26 | ||
| Total | 25211.61 | 113 | 223.11 |
R2= 0.6207, adj. R2= 0.5237
* Huynh-Feldt ε = 0.2290 (Prob.>F: 0.0514), Greenhouse-Geisser ε = 0.1241 (Prob.>F: 0.0993), Box’s conservative ε = 0.0556 (Prob.>F: 0.1549)
| Source, RE | partial SS | df* | MS | F | Prob. > F |
|---|---|---|---|---|---|
| Model | 21486.75 | 23 | 934.21 | 9.81 | 0.0000 |
| Patients | 14876.33 | 5 | 2975.27 | 31.23 | 0.0000 |
| Time | 6610.42 | 18 | 367.25 | 3.86 | 0.0000 |
| Residual | 8573.25 | 90 | 95.26 | ||
| Total | 30060.00 | 113 | 266.02 |
R2= 0.7148, adj. R2= 0.6419
* Huynh-Feldt ε = 0.2288 (Prob.>F: 0.0165), Greenhouse-Geisser ε = 0.1240 (Prob.>F: 0.0498), Box’s conservative ε = 0.0556 (Prob.>F: 0.1068)
| Source, AEP | partial SS | df* | MS | F | Prob. > F |
|---|---|---|---|---|---|
| Model | 28923.06 | 23 | 1257.52 | 8.48 | 0.0000 |
| Patients | 26333.91 | 5 | 5266.78 | 35.51 | 0.0000 |
| Time | 2589.15 | 18 | 143.84 | 0.97 | 0.5006 |
| Residual | 13348.22 | 90 | 148.31 | ||
| Total | 42271.29 | 113 | 374.08 |
R2= 0.6842, adj. R2= 0.6035
* Huynh-Feldt ε = 0.2064 (Prob.>F: 0.4426), Greenhouse-Geisser ε = 0.4152 (Prob.>F: 0.0665), Box’s conservative ε = 0.0556 (Prob.>F: 0.3699)
Appendix 4 details comparison of bispectral index (BIS), A-line ARX Index (AAI), response entropy (RE) and state entropy (SE) values at 120 seconds before movement with those obtained 110 seconds before to 60 seconds following movement using ANOVA for repeated measurements.
partial SS partial sum of squares
df degrees of freedom
MS mean sum of squares
Footnotes
Conflict of interest: Authors state no conflict of interest.
References
- [1].Myles P., Leslie K., McNeil J., Forbes A., Chan M.. Bispectral index monitoring to prevent awareness during anaesthesia: the B-Aware randomised controlled trial. Lancet. 2004;363:1757–1763. doi: 10.1016/S0140-6736(04)16300-9. [DOI] [PubMed] [Google Scholar]
- [2].Vanluchene A., Struys M., Heyes B., Mortier E.. Spectral entropy measurement of patient responsiveness during propofol and remifentanil. A comparison with the bispectral index. Br J Anaesth. 2004;93:645–654. doi: 10.1093/bja/aeh251. [DOI] [PubMed] [Google Scholar]
- [3].Tiren C., Anderson R., Barr G., Owall A., Jakobsson J.. Clinical comparison of three different anaesthetic depth monitors during cardiopulmonary bypass. Anaesthesia. 2005;60:189–193. doi: 10.1111/j.1365-2044.2004.04063.x. [DOI] [PubMed] [Google Scholar]
- [4].Stecker M., Cheung A., Pochettino A., Kent G., Patterson T., Weiss S.. Deep hypothermic circulatory arrest: I. Effects of cooling on electroencephalogram and evoked potentials. Ann Thorac Surg. 2001;71:14–21. doi: 10.1016/s0003-4975(00)01592-7. [DOI] [PubMed] [Google Scholar]
- [5].Klemola U., Mennander S., Saarnivaara L.. Tracheal intubation without the use of muscle relaxants: remifentanil or alfentanil in combination with propofol. Acta Anaesthesiol Scand. 2000;44:465–469. doi: 10.1034/j.1399-6576.2000.440419.x. [DOI] [PubMed] [Google Scholar]
- [6].Viertiö-Oja H., Maja V., Särkelä M., Talja P., Tenkanan N., Tolvanan-Laakso H.. Description of the Entropy algorithm as applied in the Datex-Ohmeda S/5 Entropy Module. Acta Anaesthesiol Scand. 2004;48:154–161. doi: 10.1111/j.0001-5172.2004.00322.x. et al. [DOI] [PubMed] [Google Scholar]
- [7].Rampil A.. A primer for EEG signal processing in anesthesia. Anesthesiology. 1998;89:980–1002. doi: 10.1097/00000542-199810000-00023. [DOI] [PubMed] [Google Scholar]
- [8].Jensen E., Lindholm P., Henneberg S.. Autoregressive modeling with exogenous input of middle-latency auditory-evoked potentials to measure rapid changes in depth of anesthesia. Methods Inf Med. 1996;35:256–260. [PubMed] [Google Scholar]
- [9].Kurita T., Doi M., Katoh T., Sano S., Sato S., Mantzaridis H.. Auditory evoked potential index predicts the depth of sedation and movement in response to skin incision during sevoflurane anesthesia. Anesthesiology. 2001;95:364–370. doi: 10.1097/00000542-200108000-00017. [DOI] [PubMed] [Google Scholar]
- [10].Winer J., Rosenwasser R., Jimenez F.. Electroencephalographic activity and serum and cerebrospinal fluid pentobarbital levels in determining the therapeutic end point during barbiturate coma. Neurosurgery. 1991;29:739–741. doi: 10.1097/00006123-199111000-00016. [DOI] [PubMed] [Google Scholar]
- [11].Gep B. Some theorems on quadratic forms applied in the study of analysis of variance problems, I. Effect of inequality of variance in the one-way classification. Journal. 1954.
- [12].Sasg G.. An extension of Box’s results on the use of the F distribution in multivariate analysis. Annals of Mathematical Statistics. 1958;29:885–891. [Google Scholar]
- [13].Halsf H.. Estimation of the Box correction for the degrees of freedom from sample data in randomized block and split-plot designs. Journal of Educational Statistics. 1976:69–82. [Google Scholar]
- [14].Smith W., Dutton R., Smith N.. Measuring the performance of anesthetic depth indicators. Anesthesiology. 1996;84:38–51. doi: 10.1097/00000542-199601000-00005. [DOI] [PubMed] [Google Scholar]
- [15].Leslie K., Sessler D., Smith W., Larson M., Ozaki M., Blanchard D.. Prediction of movement during propofol/nitrous oxide anesthesia. Performance of concentration, electroencephalographic, pupillary, and hemodynamic indicators. Anesthesiology. 1996;84:52–63. doi: 10.1097/00000542-199601000-00006. [DOI] [PubMed] [Google Scholar]
- [16].Steiger J.. Tests for comparing elements of a correlation matrix. Psychological Bulletin. 1980;87:245–251. [Google Scholar]
- [17].Fisher R. On the probable error of a coefficient of correlation deduced from a small sample. Journal. 1921.
- [18].Konishi S.. Asymptotic distribution of functions of a correlation matrix. J. Multivariate Analysis. 1979;2:9, 259–266. doi: 10.1016/0047-259X(79)90083-6. [DOI] [Google Scholar]
- [19].Bland J., Altman D.. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–310. [PubMed] [Google Scholar]
- [20].Bonhomme V., Deflandre E., Hans P.. Correlation and agreement between bispectral index and state entropy of the electroencephalogram during propofol anaesthesia. Br J Anaesth. 2006;97:340–346. doi: 10.1093/bja/ael171. [DOI] [PubMed] [Google Scholar]
- [21].Mathew J., Weatherwax K., East C., White W., Reves J.. Bispectral analysis during cardiopulmonary bypass: the effect of hypothermia on the hypnotic state. J Clin Anesth. 2001;13:301–305. doi: 10.1016/s0952-8180(01)00275-6. [DOI] [PubMed] [Google Scholar]
- [22].Levy W., Pantin E., Mehta S., McGarvey M.. Hypothermia and the approximate entropy of the electroencephalogram. Anesthesiology. 2003;98:53–57. doi: 10.1097/00000542-200301000-00012. [DOI] [PubMed] [Google Scholar]
- [23].Alpiger S., Helbo-Hansen H., Vach W., Ording H.. Efficacy of the A-line AEP monitor as a tool for predicting successful insertion of a laryngeal mask during sevoflurane anesthesia. Acta Anaesthesiol Scand. 2004;48:888–893. doi: 10.1111/j.0001-5172.2004.00425.x. [DOI] [PubMed] [Google Scholar]
- [24].Katoh T., Ikeda K.. The effects of fentanyl on sevoflurane requirements for loss of consciousness and skin incision. Anesthesiology. 1998;88:18–24. doi: 10.1097/00000542-199801000-00006. [DOI] [PubMed] [Google Scholar]
- [25].Vakkuri A., Yli-Hankala A., Talja P., Mustola S., Tolvanan-Laakso H., Sampson T.. Time-frequency balanced spectral entropy as a measure of anesthetic drug effect in central nervous system during sevoflurane, propofol, and thiopental anesthesia. Acta Anaesthesiol Scand. 2004;48:145–153. doi: 10.1111/j.0001-5172.2004.00323.x. [DOI] [PubMed] [Google Scholar]


