Abstract
African trypanosomiasis is a vector-borne parasitic disease causing serious risks to the lives of about 60 million people and 48 million cattle globally. Nigerian medicinal plants are known to contain a large variety of chemical structures and some of the plant extracts have been screened for antitrypanosomal activity, in the search for potential new drugs against the illness. We surveyed the literatures on plants and plant-derived products with antitrypanosomal activity from Nigerian flora published from 1990 to 2014. About 90 plants were identified, with 54 compounds as potential active agents and presented by plant families in alphabetical order. This review indicates that the Nigerian flora may be suitable as a starting point in searching for new and more efficient trypanocidal molecules.
Keywords: Nigeria, trypanosomiasis, medicinal plants, plant products
1. Introduction
African trypanosomiasis is a parasitic disease caused by a protozoan of the genus Trypanosoma. Trypanosoma vivax (T. vivax), Trypanosoma congolense (T. congolense) and to a lesser extent Trypanosoma brucei brucei (T. b. brucei) are the main species responsible for African animal trypanosomosis (AAT) called nagana in West Africa while T. b. rhodesiense and T. b. gambiense cause sleeping sickness (human African trypanosomiasis, HAT). Surra and Dourine are caused by the other trypanosome species T. evansi and T. equiperdum respectively. The disease is transmitted by a bite of the vector—tsetse fly (Glossina species) [1].
In Nigeria, trypanosomiasis seems to be re-emerging as an important livestock disease, assuming major clinical importance in small ruminants and extending to previously designated tsetse-free zones [2,3]. Apart from the old Gboko endemic focus remaining active, there have been reports of the disease outbreak in many other communities in Nigeria [4,5].The prevalence rate in different breed of animals in Nigeria for the past few years have been studied and ranged from 8.4% to 15.53% [6,7].
In Africa, the annual loss in livestock production and mixed agriculture alone due to the disease is valued at 5 billion US dollars. In 1995, WHO Expert Committee estimated that 60 million people were at risk with an estimated 300,000 new cases per year in Africa, with fewer than 30,000 cases diagnosed and treated. In 2004, the number of new reported cases fell to 17,616 and WHO considered in that due to increased control, estimated cumulative rate to be between 50,000 and 70,000 cases. In 2009, the number of new cases reported dropped below 10,000 (9878) for the first time in 50 years and the estimated number of actual cases is currently 30,000. This trend has been maintained in 2012, with 7216 cases reported [8,9,10].
The current chemotherapy of HAT relies on only six drugs (suramin, pentamidine, melarsoprol, eflorinithine, arsobal and mel B), five of which were developed more than 30 years ago. Others such as homidium, isometamidium and diminazene aceturate are used in animal infections. Each of these drugs has one or more of these challenges: expensive, highly toxic, need parenteral administration and parasites increasing resistance. However, tireless effort being made by WHO, private partners and local governments to eliminate HAT is yielding significant success. The Drugs for Neglected Diseases initiative (DNDi) is developing fexinidazole to a new oral drug for HAT with a good chance of success. It has entered Phase II/III clinical study in patients with late-stage sleeping sickness. It is hoped that fexinidazole would solve the problems and limitations of current chemotherapeutic options [11,12,13].
Several reviews on medicinal plants used in treatment of trypanosomiasis have been published [14,15,16,17,18,19,20,21]. It is estimated that 66%–85% of the World’s population depends directly on plants as medicine and search for drugs derived from plants has accelerated in recent years [22,23,24,25,26,27,28,29,30]. Nigeria, located in West Africa on the Gulf of Guinea, has a rich biodiversity. There are many reports documenting the potentials of medicinal plants in Nigeria against several diseases except trypanosomiasis [31,32]. This paper documents works on Nigerian medicinal plants and derived products as source of trypanocidal agents which could be further investigated for the development of better drug molecules for the disease. We present the plants which are 84 by their plant families (40) in alphabetical order.
2. Acanthaceae, Amaryllidaceae, Anacardiaceae, Annonaceae, Apocynaceae, Araceae, Asclepiadaceae, Asteraceae and Burseraceae
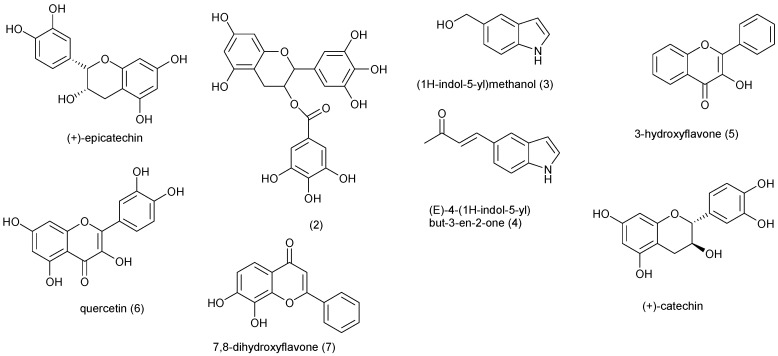
Plants produce a great diversity of substances that could be active in many fields of medicine. Natural products from plant are proven template for new drug development [33]. The plants in these families are summarized in Table 1 and the compounds isolated from them are shown in Figure 1. Peristrophe bicalyculata (Acanthaceae) is found almost throughout India, Afghanistan and Africa. The herb is used against tuberculosis, snake poison, in bone fracture, sprain, fever, cold, and cough treatments [34]. 50 mg/kg of Cold water whole plant extract of P. bicalyculata immobilized 90% of T. b. brucei in vitro after one hour of incubation, while the methanol extract of the plant showed a dose-dependent suppressive property in mice infected with T. evansi [35,36]. Nok and Williams described that the extract obtained from Allium sativum (Amaryllidaceae) completely eliminated trypanosomes in mice on administering 120 mg/kg live weight at 4 days post-treatment. A. sativum is thought to have caused cell death in trypanosomes by inhibiting the synthesis of membrane lipids of the cell [37,38]. The aqueous methanol root extracts of Lannea kerstingii and Mangifera indica from Anacardiaceae and petroleum ether root extract of Annona senegalensis (Annonaceae) at 4 mg/mL, stopped motility of T. brucei in vitro within an hour of incubation [39]. In another study, Adeiza et al. tested in vitro trypanocidal activity of A. senegalensis and found that the crude extract immobilized T. evansi at 10 mg/mL [40,41]. A fraction obtained from an aqueous leaf extract of Holarrhena africana (Apocynaceae) completely cleared T. b. rhodesiense at a dose of 40 mg/kg bw i.p. in infected mice for 5 days post treatment [42]. Hexane and methanol extracts of Spondias mombim (Anacardiaceae) root yielded Compounds 1 and 2 respectively and compounds 3 and 4 were obtained from the ethyl acetate seed extract of Monodora myristica (Annonaceae). Compounds 1, 3 and 4 were active in vitro against T. b. brucei with minimum inhibition concentration (MIC—μg/mL) of 25, 12.5 and 25 respectively [43]. The leaf extract of Lannea welwistchii showed trypanocidal activity (MIC = 6.3 mg/mL) against T. b. brucei [44]. Haematostaphis barteri is used by traditional medical practitioners in the north-eastern Nigeria to treat and manage trypanosomiasis [45]. Using short assay duration of 30 min, 0.5 mg/mL of H. barteri aqueous extract immobilize T. b. brucei and T. congolense [46].
Table 1.
Plants from Nigeria with activity against African trypanosomes.
| Family | Species | Traditional Uses | Plant Part | Ref. |
|---|---|---|---|---|
| Acanthaceae | Peristrophe bicalyculata | skin diseases, antidote for snake poison, diabetes | WP | [34] |
| Amaryllidaceae | Allium sativum | diabetes, tetanus, swellings | WP | [37] |
| Anacardiaceae | Lannea kerstingii | diarrhoea, cancer | R | [39] |
| Mangifera indica | clearing digestion and acidity due to pitta | R | [39] | |
| Spondias mombim | used as febrifuge and diuretic | R | [43] | |
| Lannea welwistchii | diarrhoea, dysentery, dropsy | L | [44] | |
| Haematostaphis barteri | trypanosomiasis | SB | [45] | |
| Annonaceae | Monodora myristica | stomachic, headaches, sores | SD | [43] |
| Anonna senegalensis | food and pneumonia | L, R, SB | [40] | |
| Apocynaceae | Carissa spinarum | analgesic | R | [47] |
| Adenium obesum | arrow poison for hunting | R | [39] | |
| Carrisa edulis | rheumatism, stomach disorder | R, B, L | [49] | |
| Holarrhena africana | dysentery, diarrhoea, snakebite, infertility, malarial, diabetics | L | [42] | |
| Saba florida | rheumatism, antidote against vomiting, diarrhoea and food poison | L | [50] | |
| Araceae | Anchomanes difformis | diabetes, diarrhoea | R | [48] |
| Asclepiadaceae | Gongronema latifolium | diabetes, high blood pressure | L, SB | [52] |
| Asteraceae | Tridax procumbens | inflammatory, microbial and protozoal diseases | WP | [53] |
| Artemisia maritima | worm, stomachic infusion | WP | [57] | |
| Burseraceae | Boswellia dalzielii | wound healing, diarrhea, syphilis, induce vomiting | L, SB, Re | [59] |
R = root, RB = root bark, SB = stem bark, L = leaves, WP = whole plant, Re = rhizome, B = bark.
Figure 1.
Chemical structures of compounds 1–8.
Carissa spinarum, also known as the conkerberry or bush plum, is a large shrub that belongs to the Apocynaceae. Its ethanol root extract has been shown to have in vivo activity against T. b. brucei at ≥100 mg/kg body weight in infected mice [47]. Using a one hour exposure time, methanol extracts of Adenium obesum stem bark (Apocynaceae) and Anchomanes difformis rhizome (Araceae) stopped 50% of the motility of T. b. brucei in vitro at 4 mg/mL [39,48]. In vivo trypanocidal activity of Carrisa edulis (Apocynaceae) against T. congolence infection in rats was investigated using a methanol root extract. Oral treatment at different doses did not significantly clear the parasitemia, however, animals treated with 100 mg/kg/day survived longer than those treated with 200 mg/kg/day and the infected control group [49]. Saba florida (Apocynaceae) is traditionally eaten as an antidote against vomiting, diarrhoea and food poisoning [50]. S. florida aqueous methanol leaf extract (400 mg/kg) exhibited in vivo activity by clearing T. b. brucei in infected rats after 7 days [51]. Gongronema latifolium (Asclepiadaceae) has been reported to stop motility of T. congolense after about 10 min of in vitro treatment using 400 mg/kg of the whole plant’s methanol extract [52]. The ethyl acetate and methanol extracts of Tridax procumbens (Asteraceae), in contrast to extracts obtained with other solvents, were trypanocidal towards T. b. brucei at 200 mg/kg [53]. Further investigation of the ethyl acetate extract of T. procumbens led to the isolation of four flavonoids; 3-hydroxyflavone (5), quercetin (6), 7,8-dihydroxyflavone (7) and catechin (8). Compounds 6 and 7 were described to exhibit trypanocidal activity in vitro and in vivo as pure compounds without affecting normal human cell [54,55,56]. In vitro studies showed T. b. brucei was immobilized by 0.4 mg/mL of Artemisia maritime (Asteraceae) chloroform and petroleum ether extracts using short assay duration of less than one hour [57]. Boswellia dalzielii (Burseraceae), a tree of the Savannah forest of Nigeria, is used for the treatment of wound, diarrhoea, syphilis and to induce vomiting [58,59]. Freiburghaus et al. found that the trypanocidal activity of B. dalzielii varies according to extraction medium and part of plant used. Based on this, Atawodi et al. tested activities of extracts of different parts of B. dalzielii against T. b. brucei. His results revealed that methanol leaf, stem and root bark extracts of the plant at 10 mg/mL significantly immobilized the trypanosome [60,61].
3. Capparaceae, Celastraceae, Clusiaceae, Combretaceae, Cucurbitaceae, Ebenaceae and Euphorbiaceae
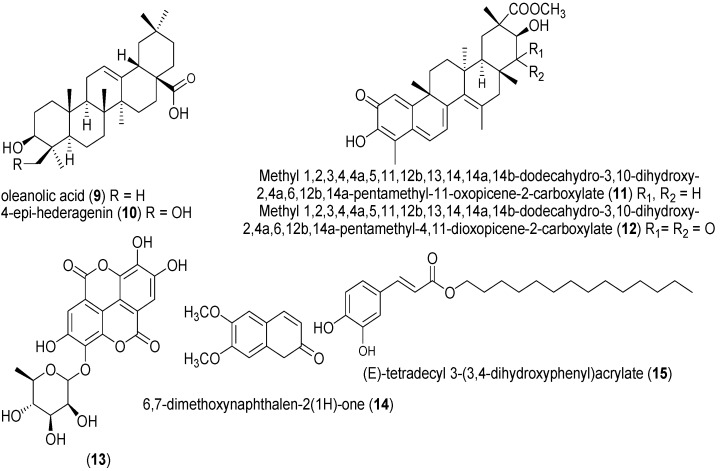
The plants in the families listed above are summarized in Table 2 and potential active isolates are represented in Figure 2. Leaves of Crateva adansonii (Capparaceae) are used to treat ear infections while its root is employed to treat syphilis, jaundice and yellow fevers [62]. The ethyl acetate and hexane crude extract of the plant demonstrated moderate in vitro activity (MIC 12.5 μg/mL) against T. b. brucei [63]. Two phytoconstituents (oleanolic acid (9) and 4-epi-hederagenin (10)), which were not tested for activity, had also been isolated from C. adansonii and could account for the activity of the plant. The seed extract of Bucholzia coriacea (Capparaceae) is locally used in treatment of feverish conditions in Eastern Nigeria [64]. T. b. brucei was cleared in infected mice after administering 1000 mg/kg of aqueous and methanol seed extracts of B. coriacea i.p. for five consecutive days [65,66]. MIC of 0.625 μg/mL has been reported for both compounds 11 and 12 isolated from the hexane-ethyl acetate fraction of Maytenus laevis (Celastraceae) root [44,67]. The highest in vivo trypanocidal activity of Garcinia kola (Clusiaceae) seeds was observed in the alkaloid fraction which brought about 92.25% reduction in parasitaemia at 100 mg/kg in T. b. brucei infected rats. The antitrypanosomal property of the alkaloids from G. kola has been suggested to be due to DNA intercalation in combination with protein biosynthesis inhibition [68].
Table 2.
Plants from Nigeria with activity against African trypanosomes.
| Family | Species | Traditional Uses | Plant Part | Ref. |
|---|---|---|---|---|
| Capparaceae | Crateva adansonii | stomach troubles, syphilis, jaundice and yellow fevers | L | [62] |
| Buchholzia coriacea | feverish, malaria | SD | [64] | |
| Celastraceae | Maytenus laevis | anti-inflammatory, analgesic | R | [67] |
| Clusiaceae | Garcinia kola | purgative, antiparasitic, antimicrobial | SD | [68] |
| Combretaceae | Anogeissus leiocarpus | trypanosomiasis, babesiosis | R, SB | [69] |
| Terminalia avicennioides | cancer, fungal, bacterial infections | B | [70] | |
| Terminalia superba | furniture making and musical instrument | B | [44] | |
| Cucurbitaceae | Mormordica balsamina | used to treat wound | WP | [48] |
| Ebenaceae | Diospyros mespiliformis | styptic to staunch bleeding, leprosy | L | [39] |
| Euphorbiaceae | Euphorbia poisonii | latex used as pesticides | B | [43] |
| Alchornea cordifolia | eye treatment, venereal diseases | S | [43] |
R = root, RB = root bark, SB = stem bark, L = leaves, S = stem, WP = whole plant, Re = rhizome, B = bark, SD = seed.
Figure 2.
Chemical structures of compounds 9 to 15.
Anogeissus leiocarpus (Combretaceae) is a tree widely distributed in northern Nigeria. The aqueous methanol bark extract of A. leiocarpus had the highest in vitro antitrypanosomal activity out of all the other parts of the plant. 200 mg/kg of the extract made T. b. brucei immotile after 10 min incubation. Furthermore, the extract (200 mg/kg) was analyzed in vivo using T. b. brucei infected rats. Although it did not clear parasitemia in experimental rats after seven days, the rats survived longer than the infected control group [69]. The hexane-ethyl acetate extract of Terminalia avicennioides (Combretaceae) bark inhibited T. b. brucei activity in vitro with MIC of 2.5 μg/mL [43,70,71]. Compound 13 was isolated from T. avicennioides but did not show activity. Methanol extracts of Terminalia superba (Combretaceae) root and stem were effective with MIC value of 3.1 mg/mL each against T. b. brucei in vitro [44]. Using a short assay duration of about an hour revealed that 10 mg/mL of both Momordica balsamina (Cucurbitaceae) and Diospyros Mespiliformis (Ebenaceae) methanol extract drastically reduced motility of T. b. brucei [39,48]. Two plants of Euphorbiaceae family whose crude extracts showed antitrypanosomal activity, yielded two active compounds; compound 14 (Euphorbia poisonii) and compounds 15 (Alchornea cordifolia). Compounds 14 and 15 had activity with (MIC of 1.56 μg/mL and < 0.2 μg/mL respectively) against T. b. brucei [43].
4. Fabaceae, Fagaceae, Hymenocardiaceae, Lamiaceae, Lauraceae, Loganiaceae, Lythraceae, Malvaceae and Melastomataceae
The compounds isolated from plants of the families listed above are shown in Figure 3 and summarized in Table 3. Northern and South-Western Nigerians use Acacia nilotica (Fabaceae) to treat dysentery, tuberculosis and diabetes. Methanol extract (400 mg/kg) of A. nilotica stem bark cleared T. b. brucei in infected mice within eight days [72,73]. In vitro activities of petroleum ether extract of Afzelia africana leaves, aqueous extract of Parkia clappertoniana root, aqueous extractof Piliostigma reticulatum leaves, chloroform extract of Prosopis africana stem bark, methanol extract of Afrormosia laxiflora leaves, chloroform extract of Erythrophleum suaveolus stem bark, methanol extract of Lonchocarpus laxiflorus stem bark and chloroform extract of Swartzia madagascariensis root (all from the Fabaceae family) against Trypanosoma species have been described using short assay durations of less than an hour [39,48,74,75,76]. Antia et al. further demonstrated that methanol extract of A. africana leaves and stems were active against T. b. brucei in vitro with MLC (mg/mL) values of 3.1 and 12.5, respectively [44]. Senna occidentalis (Fabaceae) is a weed distributed throughout the tropical and subtropical regions of the World. It has been reported as a remedy for bacterial and malaria infections [77,78,79,80,81]. The ethanol extract of S. occidentalis leaf at 6.66 mg/mL concentration, eliminated T. b. brucei in vivo in 10 min in infected rats. Acute anaemia recorded in the T. b. brucei infected rat is a consistent feature of Trypanosoma infection and the treatment with the extract was able to significantly (p < 0.05) ameliorate the disease-induced anaemia. Methanol extract of Quercus borealis (Fagaceae) leaves exhibited a significant trypanocidal activity in vitro towards T. evansi by reducing the average mean trypanosomes counts from initial concentration (40.00 ± 0.00) at 250 μg/mL and completely killing of trypanosomes at 9 h of incubation at the same concentration [82]. Denise and Barret proposed that constituents of Q. borealis exhibited trypanocidal action by intercalation with DNA of the parasite, blockage of glycolysis pathway and interference with flagella [83].
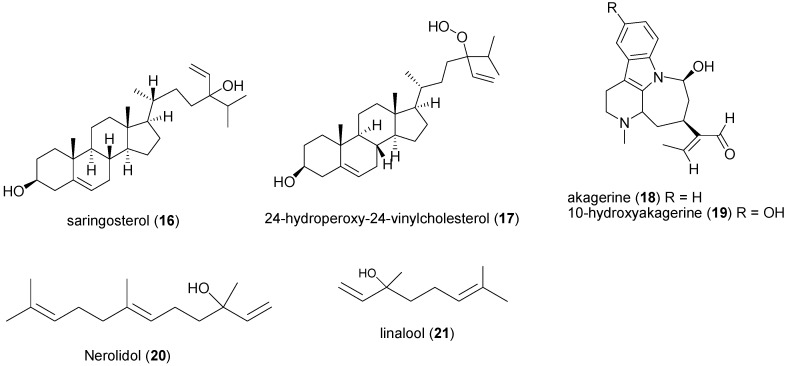
Figure 3.
Chemical structures of compounds 16 to 21.
Table 3.
Plants from Nigeria with activity against African trypanosomes.
| Family | Species | Traditional Uses | Plant Part | Ref. |
|---|---|---|---|---|
| Fabaceae | Acacia nilotica | used to treat cancers and/or tumours of ear, eye | SB | [72,73] |
| Afzelia Africana | trypanosomiasis, convulsion, hernia | WP | [74] | |
| Parkia clappertoniana | dental caries, conjunctivitis | R | [75] | |
| Piliostigma reticulatum | ulcer, boils, wounds, cancer, syphilis and diarrhoea | L | [76] | |
| Prosopis Africana | used to prepare food in Northern Nigeria | SB | [77] | |
| Afrormosia laxiflora | epilepsy and psychosis | L | [39] | |
| Erythrophleum suaveolus | arthritis, rheumatism, dropsy, swelling, eye treatment, laxative | SB | [39] | |
| Lonchocarpus laxiflorus | dermatitis, headache, intestinal worm, jaundice, ulcer, anthelmintic | SB | [48] | |
| Swartzia madagascariensis | poison arrow and fishing, insecticide | R | [48] | |
| Senna occidentalis | bacterial and malaria infections | L | [ 89] | |
| Fagaceae | Quercus borealis | dyspnea, nausea, emesis, diarrhoea and muscular pain | L | [78] |
| Hymenocardiaceae | Hymenocardia acida | Hypertension | R, SB | [80] |
| Lamiaceae | Ocimum gratissimum | the oil is medicine for respiratory tract infections, diarrhoea, eye problem, skin diseases | L | [88] |
| Hyptis spicigera | Cold, insecticides | L | [59] | |
| Lauraceae | Cassytha filiformis | food and infectious diseases | L, S | [48] |
| Loganiaceae | Anthocleista vogelii | purgative, diuretic, ulcer, stomach-ache | R, SB | [87] |
| Strychnos spinosa | taken by lactating women to stimulate breast milk production | L | [96] | |
| Loranthaceae | Tapinanthus globiferus | hypertension epilepsy, relief pain, tinnitus and trypanosomiasis | L, SB | [99] |
| Lythraceae | Lawsonia inermis | used to adorn women’s bodies as part of social and holiday celebration | L | [39] |
| Punica granatum | diarrhoea, dysentery | L | [100] | |
| Malvaceae | Bombax buonopozense | to treat edema | SB | [102] |
| Adansonia digitata | to treat cancer | SD | [101] | |
| Sterculia setigera | used as a thickener and emulsifier | R | [39] | |
| Melastomataceae | Heterotis rotundifolia | malaria, rheumatism, diarrhoea | WP | [102] |
| Dissotis rotundifolia | trypanosomiasis treatment | L | [104] |
R = root, RB = root bark, SB = stem bark, L = leaves, S = stem, WP = whole plant, Re = rhizome, B = bark, SD = seed.
In folkloric medicine of Idoma people of North Central Nigeria, Hymenocardia acida (Hymenocardiaceae) is used alone or in combination to treat trypanosomiasis and other fever related diseases [84]. Di-(2-ethylhexylphthalate (DEHP), friedelan-3-one, betulinic acid, lupeol, β-sitosterol, stigmasterol, oleic acid and homoorientin were isolated from the plant [85,86,87,88,89,90]. Aqueous ethanol extract of H. acida stem bark was active against T. b. brucei in vitro at MIC of 2.5 mg/mL in half an hour. At this concentration (2.5 mg/mL), morphology of red blood cells was unaffected [91]. None of the compounds from H. acida was tested for antitrypanosomal activity. The ethyl acetate extract of Ocimum gratissimum (Lamiaceae) leaves showed high antitrypanosomal in vitro activity (IC50 of 2.08 ± 0.01 μg/mL) and a high selective index of 29 [92]. In vitro analysis of chloroform extract of Sterculia setigera root revealed that 4 mg/mL of the extract only slightly reduced motility of T. b. brucei and T. congolense after 60 min exposure time [39]. Methanol extract of Cassytha filiformis (Lauraceae) stem (4 mg/mL) stopped T. b. brucei mobility after less than half an hour incubation time [48]. T. b. brucei (100%) was completely immobilized in vitro at MIC of 20 mg/mL of aqueous ethanol extract of Anthocleista vogelii (Loganiaceae) root bark [86,93,94,95].
In North-Eastern Nigeria, leaves and fruits of Strychnos spinosa (Loganiaceae) are consumed by lactating Fulani women to stimulate breast milk production [96]. Dichloromethane leaf extract of the plant yielded: saringosterol (16), 24-hydroperoxy-24-vinylcholesterol (17), akagerine (18) and 10-hydroxyakagerine (19). Out of the four compounds, only 16 and 17 exhibited significant antitrypanosomal in vitro activity with IC50 values of 7.8 ± 1.2 and 3.2 ± 1.2 µM respectively [97]. The essential oil from the plant’s leaves was active on T. b. brucei with IC50 13.5 µg/mL. Hoet et al., went further to show that nerolidol (20) and linalool (21), components of this oil, had a higher potency on the trypanosomes with IC50 values of 7.6 and 16.3 µM [98]. Ten and 4 mg/mL methanol extracts of Tamianthus globiferus (Loranthaceae) and Lawsonia inermis (Lythraceae) leaves respectively drastically ceased motility of T. congolense within 5 min [39,99]. A dose of 200 mg/kg of ethyl acetate extract of Punica granatum (Lythraceae) leaf reduced anaemia and promoted weight gain in mice infected with T. b. brucei [100]. The stem barks of Bombax buonopozense (Malvaceae) and Heterotis rotundifolia (Melastomataceae) methanol extracts (200 and 300 mg/kg body weight, respectively) cleared T. b. brucei within seven days of treatment duration, while 67% of T. b. brucei infected mice survived for over 43 days when treated with 400 mg/kg methanol seed extract of Adansonia digitata (Malvaceae) [70,101,102]. Dissotis rotundifolia (Melastomataceae) is a medicinal plant widely used in Nupe (Nigeria) ethno-medicine to treat trypanosomiasis [103,104]. Oral and i.p. administration of 800 mg/kg of ethanol leaf extract of the plant to rat infected with T. b. brucei significantly reduced parasitemia by 66.7% and 78.4%, respectively. The parasite was killed within 45 s of in vitro exposure to the same concentration of the extract. Hyptis spicigera (Lamiaceae) is locally known as “Bunsuru fadama” in Hausa language, Northern Nigeria. When the plant is crushed and applied to the head, it relieves headache [59]. Findings by Ladan et al., demonstrated that 0.5 µg/mL of the volatile oil from H. spicigera leaves, killed T. b. brucei in vitro within 6 min of administration. GC-MS was used to analyze the chemical composition of the essential oil and about 30 constituents were identified [105,106,107,108].
5. Meliaceae, Moraceae, Moringaceae, Myrtaceae, Ochnaceae, Phyllanthaceae, Poaceae, Polygalaceae, Rubiaceae, Rutaceae, Solanaceae, Ulmaceae, Verbenaceace, Vitaceae, Zingiberaceae
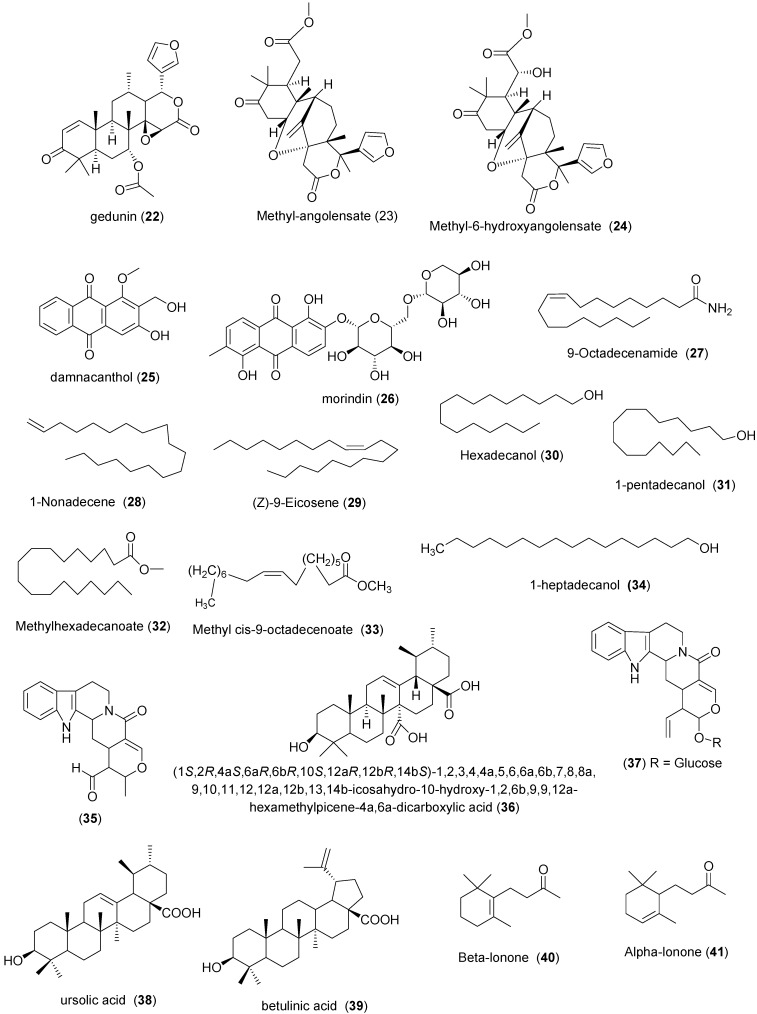
A summary of the plants and derived products of the above listed families are in Table 4 and Figure 4 respectively. Various extracts of leaf, bark, stem and seed of Khaya senegalensis (Meliaceae) were reported to treat several human diseases [109]. Rats infected with T. b. brucei showed a significant decrease in blood parasite burden within six days when treated with aqueous stem bark extract of K. senegalensis at 60–100 mg·kg−1 bw i.p. [110]. Umar et al. reported that the stem bark of K. sengalensis possessed the highest in vitro activity among the six extracts tested as it eliminated the parasites within 5 min of incubation time at 1 mg/mL [111]. The following triterpenoids: gedunin (22); methyl-angolensate (23); methyl-6-hydroxyangolensate (24), isolated from K. senegalensis stem bark, though not tested, could be responsible for its trypanocidal activity [112]. aqueous stem bark extract of Securidaca longepedunculata (Polygalaceae) and methanol stem bark extract of Pseudocedrella kotschi (Meliaceae), methanol stem bark extract of Ficus sycomorus (Moraceae), chloroform stem bark extract of Canarium schweinfurthii (Poaceae) and chloroform stem bark extract of Syzygium guineense (Myrtaceae) (4 mg/mL) ceased T. b. brucei motility in vitro within the incubation time of less than one hour [39,113].
Table 4.
Plants from Nigeria with activity against African trypanosomes.
| Family | Species | Traditional Uses | Plant Part | Ref. |
|---|---|---|---|---|
| Meliaceae | Khaya senegalensis | to treat malaria | L, AS | [109] |
| Pseudocedrella kotschi | to treat diarrhoea, dysentery, epilepsy | SB | [39] | |
| Moraceae | Ficus sycomorus | to treat snakebite, jaundice, dysentery | SB | [39] |
| Moringaceae | Moringa oleifera | to treat diabetes and intestinal worms | L, S, SB, R | [116] |
| Myrtaceae | Psidium guajava | to treat diarrhoea, hypertension | L | [118] |
| Syzygium guineense | used to bath ill person | SB | [113] | |
| Eucalyptus camaldulensis | used to treat malaria and typhoid fevers | L | [120] | |
| Ochnaceae | Lophira lanceolata | dermatosis, toothache, muscular tiredness | L, SB | [87] |
| Ximenia americana | treatment of fever, jaundice, impotence, sleeping sickness | SB | [123] | |
| Plantaginaceae | Picrorhiza kurroa | to treat asthma, bronchitis, chronic dysentery, malaria | WP | [124] |
| Poaceae | Canarium schweinfurthii | burnt for fumigation | SB | [39] |
| Polygalaceae | Securidaca longepedunculata | to treat cough, chest pain, toothache and diabetes | R | [113] |
| Rubiaceae | Gardenia erubescens | used as dye | L | [92] |
| Nauclea latifolia | to treat fever, dental caries, sceptic mouth, malaria | B | [125] | |
| Nauclea pobeguinii | to treat fever, dental caries, sceptic mouth, malaria | B | [43] | |
| Keetia leucantha | to treat malaria | L | [127] | |
| Mitracarpus scaber | to treat headache, toothache, venereal disease, amenorrhoea, dyspepsia, leprosy | L | [128] | |
| Morinda lucida | used to treat malaria | L | [115] | |
| Rutaceae | Zanthoxylum zanthoxyloides | stomach disorder, worm infection | SB | [70] |
| Solanaceae | Withania somnifera | to treat external tumors, tubercular glands and ulcer | WP | [43] |
| Ulmaceae | Trema orientalis | to treat cough, sore throats, asthma, bronchitis, gonorrhea, yellow fever, toothaches | L | [70] |
| Verbenaceace | Vitex doniana | anemia, gonorrhea, dysentery and to improve fertility | L | [70] |
| Vitex simplicifolia | to treat malaria | L | [131] | |
| Vitaceae | Cissus multistriata | for the management of protein deficiency | L | [130] |
| Zingiberaceae | Zingiber officinale | gastrointestinal diseases, dyspnea, nausea, emesis, diarrhoea and muscular pain | R | [83] |
R = root, RB = root bark, SB = stem bark, L = leaves, S = stem, WP = whole plant, Re = rhizome, B = bark, SD = seed, AS = axial stem.
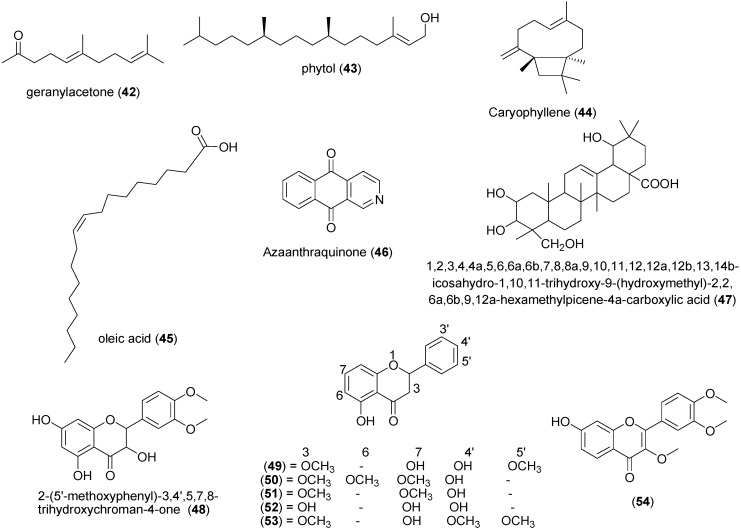
Figure 4.
Chemical structures of compounds 22–54.
Morinda lucida (Rubiaceae) root together with Mangifera indica, Carica papya and Cassia podocarba leaves are used in Nigeria to treat malaria [114]. Adewunmi and Adesogan isolated some anthraquinones such as damnacanthol (25) and morindin (26) from M. lucida. Intraperitoneal administration of methanol leaf extract of M. lucida caused a significant reduction in parasitemia in T. b. brucei infested rats and mice [115,116]. An in vitro assay revealed that the petroleum ether extract of the root bark, chloroform extract of the stem bark, methanol extract of the stem and the aqueous extract of all parts of Moringa oleifera (Moringaceae) were active at 4 and 2 mg/mL doses against T. b. brucei [117]. The anti-trypanosomal screening of Psidium guajava (Myrtaceae) leaves revealed that it inhibited growth of T. b. brucei (IC50 of 6.3 μg/mL and 48.9 μg/mL) for 80% and 20% ethanol preparations respectively [118,119,120]. Eucalyptus camaldulensis (Myrtaceae) methanol leaf extract at a dose of 150 mg/kg body weight/day extended the lifespan of T. b. brucei infected mice by six days [120]. GC-MS analysis of E. camaldulensis fraction yielded 9-octadecenamide (27), 1-nonadecene (28), (Z)-9-eicosene (29), hexadecanol (30), 1-pentadecanol (31) for fraction A; and methyl hexadecanoate (32), methyl cis-9-octadecenoate (33), and 1-heptadecanol (34) for fraction B [121,122]. Aqueous extract Lophira lanceolata (Ochnaceae) Leaf and ethanol extract of Gardenia erubescens (Rubiaceae) stem had 100% activity in vitro against T. b. brucei and T. congolense at 20 mg/mL [92,123]. Peter et al. showed that 1000 µg/mL methanol extract of Picrorhiza kurroa (Plantaginaceae) rhizome completely killed T. evansi in vitro after an incubation time of 8 h [124].
Among the three compounds 35, 36 and 37 isolated from the ethanol bark extracts of two plants from the Rubiaceae family (Nauclea pobeguinii and Nauclea latifolia), only 37 had activity in vitro (MIC = 12.5 μg/mL) against T. b. brucei [43,125,126]. Ten compounds with in vitro anti-trypanosomal properties; ursolic acid (38), oleanolic acid (9), betulinic acid (39), β-lonone (40), α-lonone (41), geranylacetone (42), phytol (43), caryophyllene (44) and oleic acid (45) have been isolated from Keetia leucantha (Rubiaceae). Compounds 38 and 9 demonstrated activities with IC50 of 2.5 and 7.3 μg/mL respectively towards T. b. brucei [127]. Mitracarpus scaber (Rubiaceae) is used in Nigeria to treat headache, toothache, venereal diseases, amenorrhoea, dyspepsia and leprosy [128]. Its methanol fraction yielded azaanthraquinone (46) which caused complete disappearance of T. congolense (in vivo) in mice at 50 mg/kg bw for 5 day without relapse. The authors suggested that the mechanism by which the compound performed its trypanocidal effect was by interfering with the mitochondrial electron transport system of the parasite [129]. Ximenia americana (Ochnaceae) is a plant used in traditional medicine for the treatment of malaria, ulcers, and infectious diseases. Aqueous extract of X. americana stem bark exhibited in vitro trypanocidal effect by immobilizing 90% of the T. congolenseafter 30 min incubation [123]. Zanthoxylum zanthoxyloides (Rutaceae) showed only trypanostatic effects and could not completely clear the T. b. brucei in vivo in infected mice [70].
Hexane whole plant extract of Withania somnifera (Solanaceae) had in vitro activity against T. b. brucei (MIC = 50 μg/mL) while 20 µg/mL of compound 47 isolated from the plant immobilized 78% of T. b. brucei [43]. Methanol leaves extracts of Trema orientalis (Ulmaceae) and Vitex doniana (Verbenaceace) exhibited in vitro activities with IC50 values of 3.50 and 6.58 μg/mL respectively against T. b. rhodesiense in less than one hour [70]. Aqueous methanol leaf extract of Cissus multistriata (Vitaceae) was very active against T. b. brucei. Parasitemia level in infected albino rats disappeared on sixth day of treatment with 400 mg/kg b.w of the plant extract intraperitoneally. Omale and Joseph suggested that the high trypanocidal activity of the plant could be due to its flavonoid content [51,130]. After 9 h of exposing T. evansi, in vitro, at 1000 μg/mL of methanol extract of Zingiber officinale (Zingiberaceae) rhizome, 95.86% of the parasites died [83]. Nwodo et al. reported that 2-(5'-methoxyphenyl)-3,4',5,7,8-trihydroxychroman-4-one (48), 2-(5'-methoxyphenyl)-4',5,7-trihydroxy-3-methoxychromen-4-one (49), penduletin (50), 2-(4'-hydroxy-phenyl)-5-hydroxy-3,7-dimethoxychromen-4-one (51), 2-(4-hydroxyphenyl)-3,5,7-trihydroxy-chromen-4-one (52), artemetin (53) and 2-(3',4'-dimethoxyphenyl)-7-hydroxychromen-4-one (54) from Vitex simplicifolia (Verbenaceace) leaf were active (IC50 values range 4.7–23.7 µM) against T. b. rhodesiense after less than one hour of incubation time. Compound 54 showed the most promising and selective trypanocidal activity (IC50 = 4.7 µM) with a selectivity index of 9.8. The authors observed that trypanocidal activity of the compounds increases with increase in methylation of hydroxyl groups. This is expected because methylation increases lipophilicity which increases permeability of molecule across membranes of the parasite [131,132,133].
6. Conclusions
This review, the first of its kind on antitrypanosomal medicinal plants from the Nigerian flora, represents an overview of the potentials of these plants in combating the disease. It is intended to serve as the scientific baseline information for the use of documented plants as well as a starting point for future studies for the discovery of better trypanocidal molecule(s). Most of the plants were evaluated as crude extracts. Only compounds 1, 3, 4, 9, 11–12, 14–17, 20–21, 37–38, 47–54 were actually tested for antitrypanosomal properties. Mode of action of the compounds has almost never been thoroughly studied; only possible mechanisms have been suggested. This calls for more detailed investigations in this direction. In general, even though not all plants reviewed here are native or unique to Nigeria or West Africa, this survey suggests that Nigerian flora is a potential suitable starting point to discovering new and better trypanocidal drug molecules.
Acknowledgments
The authors are grateful for the support from ResNet NPND and also to the Chemical and Bioactivity Information Centre (CBIC), Cameroon for access to the natural products database.
Author Contributions
NJN, AI, MUA and CJM conceived the ideas, FNK provided access to CBIC database and contributed in data analysis, NJN and AI wrote the first draft of the paper and all authors agreed on the final version before submission.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.D’Archivio S., Medina M., Cosson A., Chamond N., Rotureau B., Minoprio P. Genetic engineering of Trypanosoma (Dutonella) vivax and in vitro differentiation under axenic conditions. PLoS Negl. Trop. Dis. 2011;5:e1461. doi: 10.1371/journal.pntd.0001461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Joshua R.A., Magaji Y., Kayit Y.S. Isolation of human serum resistant Trypanozoon from cattle in Nigeria. Tropenmedizin Parasitol. 1983;13:201–202. [PubMed] [Google Scholar]
- 3.Ayodele O.M., Akinyemi F., Charles D., Kim P., Michael V.T., Susan C.W. A Longitudinal Survey of African Animal Trypanosomiasis in Domestic Cattle on the Jos Plateau, Nigeria: Prevalence, Distribution and Risk Factors. Parasites Vectors. 2013;6:239. doi: 10.1186/1756-3305-6-239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Airauhi L., Unuigbe E.I., Airauchi O.D. Human sleeping sickness (SS) in Nigeria: Knowledge, attitude and beliefs in a focus in the Abraka belt, Delta of Nigeria. Afr. J. Clin. Exp. Microbiol. 2001;2:6–9. [Google Scholar]
- 5.Edeghere H., Elhassan E., Ukah J.C.A., Sanda S., Ikenga M., Audu G. The scourge of human African trypanosomiasis in Abraka: possible control strategies. Nig. Soc. Parasitol. Abst. 1998;46:43. [Google Scholar]
- 6.Bauer B., Amsler-Delafosse S., Kabore I., Kamunga M. Improvement of cattle productivity through rapid alleviation of African management practice in the Agropastoral zone of Yale, Burkina Faso. Animal trypanosomosis by integrated disease. Trop. Anim. Health Prod. 1999;31:89–102. doi: 10.1023/A:1005115707181. [DOI] [PubMed] [Google Scholar]
- 7.Griffin L., Allonby W.E. The economic effect of trypanosomiasis in sheep and goats at a range research station in Kenya. Trop. Anim. Health Prod. 1979;11:127–132. doi: 10.1007/BF02237788. [DOI] [PubMed] [Google Scholar]
- 8.Mulumba K. Socio Economic and Agricultural Factors in the Research and Control of Trypanosomiasis. FAO/WHO/IAEA/OAU; Rome, Italy: Jan 03, 2003. PAAT Technical and Scientific Series 4. [Google Scholar]
- 9.Abenga J.N., Lawal I.A. Implicating roles of animal reservoir host in the resurgence of Gambian trypanosomiasis (Sleeping Sickiness) Afr. J. Biotechnol. 2005;4:134–137. [Google Scholar]
- 10.Fact Sheet N°259: Trypanosomiasis, Human African (Sleeping Sickness); WHO Media Centre: Geneva, Switzerland, 1 June. 2013. [(accessed on 27 February 2014)]. Available online: http:www.who.int/mediacentre/factsheets/fs259/en.
- 11.Maser P., Luscher A., Kaminsky R. Drug transport and drug resistance in African trypanosomes. Drug Resist. Updates. 2003;6:281–290. doi: 10.1016/j.drup.2003.09.001. [DOI] [PubMed] [Google Scholar]
- 12.Amaechi N. Toxicity of antiprotozoan drug diminazene aceturate in rats. J. Sustain. Agric. Environ. 2001;3:365–370. [Google Scholar]
- 13.Kaiser M., Bray M.A., Cal M., Trunz B.B., Torreele E., Brun R. Antitrypanosomal activity of Fexinidazole, a new oral Nitroimidazole drug candidate for treatment of sleeping sickness. Antimicrob. Agents Chemother. 2011;55:5602–5608. doi: 10.1128/AAC.00246-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ameenah G., Mohamad F.M. African flora as potential sources of medicinal plants: Towards the chemotherapy of major parasitic and other infectious diseases—A review. Jordan J. Biol. Sci. 2013;6:77–84. doi: 10.12816/0000263. [DOI] [Google Scholar]
- 15.Mbaya A.W., Ibrahim U.I. In vivo and in vitro activities of medicinal plants on haemic and humoral trypanosomes: A review. Int. J. Pharmacol. 2011;7:1–11. [Google Scholar]
- 16.Malebo H.M., Tanja W., Cal M., Swaleh S.A.M., Omolo M.O., Hassanali A., Séquin U., Hamburger M., Brun R., Ndiege I.O. Antiplasmodial, anti-trypanosomal, anti-leishmanial and cytotoxicity activity of selected Tanzanian medicinal plants. Tanzania J. Health Res. 2009;11:226–233. doi: 10.4314/thrb.v11i4.50194. [DOI] [PubMed] [Google Scholar]
- 17.Hoet S., Opperdoes F., Brun R., Quetin-Leclercq J. Natural products active against African trypanosomes: A step towards new drugs. Nat. Prod. Rep. 2004;21:353–364. doi: 10.1039/b311021b. [DOI] [PubMed] [Google Scholar]
- 18.Ibrahim M.A., Mohammed A., Isah M.B., Aliyu A.B. Anti-trypanosomal activity of African medicinal plants: A review update. J. Ethnopharmacol. 2014;154:26–54. doi: 10.1016/j.jep.2014.04.012. [DOI] [PubMed] [Google Scholar]
- 19.Schmidt T.J., Khalid S.A., Romanha A.J., Alves T.M.A., Biavatti M.W., Brun R., Da Costa F.B., de Castro S.L., Ferreira V.F., de Lacerda M.V.G., et al. The Potential of Secondary Metabolites from Plants as Drugs or Leads against Protozoan Neglected Diseases Part I. Curr. Med. Chem. 2012;19:2128–2175. doi: 10.2174/092986712800229023. [DOI] [PubMed] [Google Scholar]
- 20.Schmidt T.J., Khalid S.A., Romanha A.J., Alves T.M.A., Biavatti M.W., Brun R., Da Costa F.B., de Castro S.L., Ferreira V.F., de Lacerda M.V.G., et al. The Potential of Secondary Metabolites from Plants as Drugs or Leads against Protozoan Neglected Diseases Part II. Curr. Med. Chem. 2012;19:2176–2228. [PubMed] [Google Scholar]
- 21.Ogungbe I.V., Setzer W.N. Comparative Molecular Docking of Antitrypanosomal Natural Products into Multiple Trypanosoma brucei Drug Targets. Molecules. 2009;14:1513–1536. doi: 10.3390/molecules14041513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Newmann D.J., Cragg G.M. Natural products as sources of new drugs over the 30 years from 1981 to 2010. J. Nat. Prod. 2012;75:311–335. doi: 10.1021/np200906s. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Matthews H.B., Lucier G.W., Fisher K.D. Medicinal herbs in the United States: Research needs. Environ. Health Perspect. 1999;107:773–778. doi: 10.1289/ehp.99107773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yeh G.Y., Eisenberg D.M., Kaptchuk T.J., Phillips R.S. Systematic review of herbs and dietary supplements for glycemic control in diabetes. Diabetes Care. 2003;26:1277–1294. doi: 10.2337/diacare.26.4.1277. [DOI] [PubMed] [Google Scholar]
- 25.Hamdan I.I., Afifi F.U. Studies on the in vitro and in vivo hypoglycemic activities of some medicinal plants used in treatment of diabetes in Jordanian traditional medicine. J. Ethnopharmacol. 2004;93:117–121. doi: 10.1016/j.jep.2004.03.033. [DOI] [PubMed] [Google Scholar]
- 26.Rangasamy O., Raoelison G., Rakotoniriana F.E. Screening for anti-infective properties of several medicinal plants of the Mauritians flora. J. Ethnopharmacol. 2007;109:331–337. doi: 10.1016/j.jep.2006.08.002. [DOI] [PubMed] [Google Scholar]
- 27.Mahomoodally M.F., Gurib-Fakim A., Subratty A.H. Antimicrobial activities and phytochemical profiles of endemic medicinal plants of Mauritius. Pharm. Biol. 2005;43:237–242. doi: 10.1080/13880200590928825. [DOI] [Google Scholar]
- 28.Mahomoodally M.F., Gurib-Fakim A., Subratty A.H. Screening for alternative antibiotics: An investigation into the antimicrobial activities of medicinal food plants of Mauritius. J. Food Sci. 2010;75:173–177. doi: 10.1111/j.1750-3841.2010.01555.x. [DOI] [PubMed] [Google Scholar]
- 29.Ranilla L.G., Kwon Y.I., Apostolidis E., Shetty K. Phenolic compounds, antioxidant activity and in vitro inhibitory potential against key enzymes relevant for hyperglycemia and hypertension of commonly used medicinal plants, herbs and spices in Latin America. Bioresour. Technol. 2010;101:4676–4689. doi: 10.1016/j.biortech.2010.01.093. [DOI] [PubMed] [Google Scholar]
- 30.Ravi-Kumar A., Ponnusamy S., Ravindran R., Zinjarde S., Bhargava S. Evaluation of traditional Indian antidiabetic medicinal plants for human pancreatic amylase inhibitory effect in vitro. Evid. Based Complement. Altern. Med. 2011;2011 doi: 10.1155/2011/515647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Administrative Map of Nigeria—Nations Outline Project. [(accessed on 2 February 2015)]. Available online: http://www.nationsonline.org.
- 32.Lifongo L.L., Simoben V.C., Ntie-Kang F., Babiaka B.S., Judson N.P. A bioactivity versus ethnobotanical survey of medicinal plants from Nigeria, West Africa. Nat. Prod. Bioprospect. 2014;4:1–19. doi: 10.1007/s13659-014-0005-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cragg G.M., Newmann D.J., Snader K.M. Natural products in drug discovery and development. J. Nat. Prod. 1997;60:52–60. doi: 10.1021/np9604893. [DOI] [PubMed] [Google Scholar]
- 34.Guadani R., Patel J., Prajapati H., Mehta B., Agrawal S. Peristrophe bicalculata—A review. Pharmacogn. J. 2010;2:39–45. [Google Scholar]
- 35.Abdulazeez M.A., Ibrahim A.B., Edibo Z.Y., Sidali J.O., Idris H.O. Anti-trypanosomal effect of Peristrophe bicalyculata extract on Trypanosoma brucei brucei-infected rats. Asian Pac. J. Trop. Biomed. 2013;3:523–531. doi: 10.1016/S2221-1691(13)60107-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Awulu E.A., Oniye S.J., Adelanwa M.A. Phytochemical Screening and in vivo Antitrypanosomal Activity of Methanol Extracts of Peristrophe bicalyculata in Mice Infected with Trypanosoma evansi. Int. J. Sci. Technol. 2013;3:34–39. [Google Scholar]
- 37.Nok A.J., Williams S. Allium sativum—Induced death of African Trypanosomes. Parasitol. Res. 1996;82:634–637. doi: 10.1007/s004360050177. [DOI] [PubMed] [Google Scholar]
- 38.Alawa J.P., Jokthan G.E., Akut K. Ethnoveterinary medical practice for ruminants in the sub-humid zone of northern Nigeria. Prev. Vet. Med. 2002;54:79–90. doi: 10.1016/S0167-5877(01)00273-2. [DOI] [PubMed] [Google Scholar]
- 39.Atawodi S.E., Bulus T., Ibrahim S., Ameh D.A., Nok A.J., Mamman M., Galadima M. In vitro trypanocidal effect of methanolic extract of some Nigerian savannah plants. Afr. J. Biotechnol. 2003;2:317–321. [Google Scholar]
- 40.Adeiza A.A., Maikai V.A., Hassan F.B. Phytochemical screening and evaluation of some medicinal plants for their in vitro activities on Trypanosoma evansi. J. Med. Plants Res. 2009;3:315–318. [Google Scholar]
- 41.Ogbadoyi E.O., Abdulganiyu A.O., Adama T.Z., Okogun J.J. In vivo Trypanocidal activity of Annona senegalensis. Pers leaf extract against T. brucei brucei. J. Ethnopharmacol. 2007;112:85–89. doi: 10.1016/j.jep.2007.02.015. [DOI] [PubMed] [Google Scholar]
- 42.Nwodo N.J., Brun R., Osadebe P.O. In vitro and in vivo evaluation of the antitrypanosomal of fraction of Holarrhena africana. J. Ethnopharmacol. 2007;113:556–559. doi: 10.1016/j.jep.2007.07.018. [DOI] [PubMed] [Google Scholar]
- 43.Igoli J.O., Gray A.I., Clements C.J., Mouad H.A. Anti-Trypanosomal Activity and cytotoxicity of some compounds and extracts from Nigerian Medicinal Plants. In: Rasooli I., editor. Phytochemicals—Bioactivities and Impact on Health. In Tech; Shanghai, China: 2011. pp. 375–388. [Google Scholar]
- 44.Antia R.E., Olayemi J.O., Aina O.O., Ajaiyeoba E.O. In vitro and in vivo animal model antitrypanosomal evaluation of ten medicinal plant extracts from south west Nigeria. Afr. J. Biotechnol. 2009;8:1437–1440. [Google Scholar]
- 45.Sofowora A. Medicinal Plants and Traditional Medicines in Africa. Spectrum Books LTD; Ibadan, Nigeria: 1990. p. 289. [Google Scholar]
- 46.Sofowora A. Research on Medicinal Plants and Traditional Medicine in Africa. J. Altern. Complement. Med. 1996;2:365–372. doi: 10.1089/acm.1996.2.365. [DOI] [PubMed] [Google Scholar]
- 47.Onotu C.S., Musa U.B., Fajinmi A.O., Mazadu M.R., Shaida S.S. Physiochemical evaluation of ethanolic root extract of Carissa spinarum (Wild Karanda) on Trypanosoma brucei brucei (Federe Strain) infected mice. Int. J. Pharm. Sci. Invent. 2013;2:18–26. [Google Scholar]
- 48.Atawodi S.E. Comparative in vitro trypanocidal activities of petroleum ether, chloroform, methanol and aqueous extracts of some Nigerian savannah plants. Afr. J. Biotechnol. 2005;4:177–182. [Google Scholar]
- 49.Wurochekke A.U., Nuhu N., Anyanwu G.O. Trypanocidal potential of Carrisa edulis in male wistar rats infected with T. congolense. Am. J. Res. Commun. 2014;2:234–244. [Google Scholar]
- 50.Omale J., Omajali J.B. Studies on some nutritional characteristics of the fruit and leaf of Sabaflorida (Benth) from Ibaji forest. Int. J. Nutr. Metab. 2010;2:011–026. [Google Scholar]
- 51.Omale J., Joseph J.E. Comparative evaluation of trypanocidal activities of Cissus multistriata and Saba florida (benth) leaf extracts. J. Biosci. Technol. 2011;2:197–204. [Google Scholar]
- 52.Abedo J.A., Jonah O.A., Abdullahi R.S., Mazadu M.R., Idris H.Y., Muhammed H., Shettima F.T., Ombugadu S., Daudu M., Garba J., et al. Evaluation of trypanosomal activity of Tapinanthus globiferus and Gongronema latifolium on Trypanosoma congolense. Biosci. Res. 2013;10:20–28. [Google Scholar]
- 53.Abubakar A., Ogbadoyi E.O., Okogun J.I., Gbodi T.I., Ibikunle G.F. The identification of putative antitrypanosomal compounds in Tridax procumbens extracts. Int. J. Med. Aromat. Plants. 2012;2:185–194. [Google Scholar]
- 54.Cordell G.A., Quinn-Beattie M.L., Farnsworth N.R. The potential of alkaloids in drug discovery. Phytother. Res. 2001;15:183–205. doi: 10.1002/ptr.890. [DOI] [PubMed] [Google Scholar]
- 55.Tasdemir D., Kaiser M., Brun R., Yardley V., Schmidt T.J., Tosun F., Ruedi P. Antitrypanosomal and antileishmanial activities of flavonoids and their analogues: In vitro, in vivo, structure-activity relationship, and quantitative structure-activity relationship studies. Antimicrob. Agents Chemother. 2006;50:1352–1364. doi: 10.1128/AAC.50.4.1352-1364.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mamani-Matsuda M., Rambert J., Malvy D., Lejoly-Boisseau H., Daulouede S., Thiolat P., Coves S., Courtois P., Vincendeau P., Djavad M.M. Quercetin induces apoptosis of Trypanosoma brucei gambiense and diseases the proinflammatory response of human macrophages. Antimicrob. Agent Chemother. 2004;48:924–929. doi: 10.1128/AAC.48.3.924-929.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ene A.C., Atawodi S.E., Apeh Y.E.O. In vitro and in vivo antitrypanosomal effects of petroleum ether, chloroform and methanol extracts of Artemisia maritima Linn. Br. J. Pharm. Res. 2014;4:751–758. doi: 10.9734/BJPR/2014/7631. [DOI] [PubMed] [Google Scholar]
- 58.Nwude N., Ibrahim M.A. Plants used in traditional veterinary medical practice in Nigeria. J. Vet. Pharmacol. Ther. 1980;3:261–273. doi: 10.1111/j.1365-2885.1980.tb00491.x. [DOI] [Google Scholar]
- 59.Dalziel J.M. Useful Plants of West Tropical Africa. Crown Agent for Overseas Governments; London, UK: 1937. pp. 462–463. [Google Scholar]
- 60.Freiburghaus F., Kaminsky R., Nkuna M.H.N., Brun R. Evaluation of African medicinal plants for their in vitro trypanocidal activity. J. Ethnopharmacol. 1996;55:1–11. doi: 10.1016/S0378-8741(96)01463-8. [DOI] [PubMed] [Google Scholar]
- 61.Atawodi S.E., Joseph-Idrisu J., Uche S.N., Yusufu L.M.L. Phytochemical and Antitrypanosomal Studies of Different Solvents Extracts of Boswellia dalzielii. Int. J. Biol. 2011;3:179–184. [Google Scholar]
- 62.Burkill H.M. The Useful Plants of West Tropical Africa. Volume 1. Royal Botanic Garden, Kew Publishing; London, UK: 1985. Families A–D; p. 960. [Google Scholar]
- 63.Igoli N.P., Gray A.I., Clements C.J., Igoli J.O., Nzekwe U., Singla R.K. Scientific Investigation of Antitrypanosomal Activity of Crateva adansonii DC Leaves Extracts. Indo Glob. J. Pharm. Sci. 2012;2:226–229. [Google Scholar]
- 64.Nweze N.E., Fakae L.B., Asuzu I.U. Trypanocidal activity of the ethanolic extract of Buchholzia coriacea seed. Niger. Vet. J. 2009;29:1–6. [Google Scholar]
- 65.Okere O.S., Iliemene U.D. Proximate Analysis, Phytochemical Screening and Antitrypanocidal Potentials of Bucholzia coriacea in Trypanosoma brucei brucei-Infected Mice. J. Pharm. Biol. Sci. 2014;9:69–77. [Google Scholar]
- 66.Nweze N.E., Anene B.M., Asuzu I.U. Investigation of the antitrypanosomal activity of Buchholzia coriacea seed extract against a field strain of Trypanosoma congolense. Afr. J. Tradit. Complement. Altern. Med. 2011;8:175–180. doi: 10.4314/ajtcam.v8i5S.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Igoli J.O., Ogaji O.G., Tor-Anyiin T.A., Igoli N.P. Traditional Medicine Practices Amongst the Igede people of Nigeria. Part II. Afr. J. Tradit. CAM. 2005;2:134–152. [Google Scholar]
- 68.Johnson T.O., Omoniwa B.P. In Vivo Trypanocidal Activity of Ethanolic Crude Extract and Phytochemical Fractions of Garcinia kola Seeds. Ann. Res. Rev. Biol. 2014;4:212–222. doi: 10.9734/ARRB/2014/5716. [DOI] [Google Scholar]
- 69.Wurochekke A.U., Anyanwu G.O. Antitrypanosomal activity of Anogeissus leiocarpus in rats infected with Trypanosoma brucei brucei. Int. Res. J. Biotechnol. 2012;3:005–009. [Google Scholar]
- 70.Mann A., Ogbadoyi E.O. Evaluation of Medicinal Plants from Nupeland for Their in Vivo Antitrypanosomal Activity. Am. J. Biochem. 2012;2:1–6. doi: 10.5923/j.ajb.20120201.01. [DOI] [Google Scholar]
- 71.Mann A., Ibrahim K., Oyewale A.O., Amupitan J.O., Fatope M.O., Okogun J.I. Antimycobacterial Friedelane-terpenoid from the Root Bark of Terminalia Avicennioides. Am. J. Chem. 2011;1:52–55. doi: 10.5923/j.chemistry.20110102.11. [DOI] [Google Scholar]
- 72.Ahmad M., Zaman F., Sharif T., Zabta C.M. Antidiabetic and hypolipidemic effects of aqueous methanolic extract of Acasia nilotica pods in alloxan-induced diabetic rabbits. Scand. J. Lab. Anim. Sci. 2008;35:29–34. [Google Scholar]
- 73.Ogbadoyi E.O., Garba M.H., Kabiru A.Y., Mann A., Okogun J. Therapeutic evaluation of Acacia nilotica (Linn) stem bark extract in experimental African trypanosomiasis. Int. J. Appl. Res. Nat. Prod. 2011;4:11–18. [Google Scholar]
- 74.Akinpelu D.A., Aitegoro A.O., Okoh A.I. Studies on the biocidal and cell membrane disruption potential s of stem bark extracts of Afzelia africana. Biol. Res. 2009;42:339–349. doi: 10.4067/S0716-97602009000300008. [DOI] [PubMed] [Google Scholar]
- 75.Banwo G.O., Abdullahi I., Duguryil M. The antimicrobial activity of the stem-bark and leaf of Parkia clappertoniana Keay family Leguminosae against selected microorganism. Niger. J. Pharm. Res. 2004;3:16–22. [Google Scholar]
- 76.Dsso K., N’guessan B.B., Bidie A.P., Gnangoran B.N., Meite S., N’guessan D., Yapo A.P., Ehile E.E. Antidiarrhoeal activity of an ethanolic extract of the stem bark of Pilistigma reticulatum (Caesalpiniaceae) in rats. Afr. J. Tradit. Complement. Altern. Med. 2012;9:242–249. doi: 10.4314/ajtcam.v9i2.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Abiodun O.O., Gbotosho G.O., Ajaiyeoba E.O., Brun R., Oduola A.M. Antitrypanosomal activity of some medicinal plants from Nigerian ethnomedicine. Parasitol. Res. 2012;110:521–526. doi: 10.1007/s00436-011-2516-z. [DOI] [PubMed] [Google Scholar]
- 78.Tona L., Ngimbi N.P., Tsakala M., Mesia K., Cimanga K., Apers S. Antimalaria activity of 20 crude extracts from nine African medicinal plants used in Kinshasa, Congo. J. Ethnopharmacol. 1999;68:193–203. doi: 10.1016/S0378-8741(99)00090-2. [DOI] [PubMed] [Google Scholar]
- 79.Samy R.P., Ignacimuthu S. Antibacterial activity of some folklore medicinal plants used by tribals in Western Ghats of India. J. Ethnopharmacol. 2000;69:63–71. doi: 10.1016/S0378-8741(98)00156-1. [DOI] [PubMed] [Google Scholar]
- 80.Tona L., Mesia K., Ngimbi N.P., Chrimwami B., Cimanga K. In vivo antimalarial activity of Cassia occentalis, Morinda morindoides and Phyllanthus niruri. Ann. Trop. Med. Parasitol. 2001;95:47–57. doi: 10.1080/00034980020035915. [DOI] [PubMed] [Google Scholar]
- 81.Chukwujekwu J.C., Coombes P.H., Mulholland D.A., Vanstaden J. Emordin, an antibacterial anthraquinone from the roots of Cassia occidentalis. S. Afr. J. Bot. 2006;72:295–297. doi: 10.1016/j.sajb.2005.08.003. [DOI] [Google Scholar]
- 82.Barminas J.T., Maina H.M., Ali J. Nutrient content of Prosopis africana seeds. Plant Food Hum. Nutr. 1998;52:325–328. doi: 10.1023/A:1008045218320. [DOI] [PubMed] [Google Scholar]
- 83.Shaba P., Pandey N.N., Sharma O.P., Rao J.R., Singh R.K. In vitro trypanocidal activity of methanolic extracts of Quercus borealis leaves and Zingiber officinale roots against Trypanosoma evansi. Greener J. Agric. Sci. 2011;1:41–47. [Google Scholar]
- 84.Denise M., Barret M.P. Uptake and mode of activity of drugs used against sleeping sickness. J. Biochem. Pharmacol. 2001;61:1–5. doi: 10.1016/S0006-2952(00)00477-9. [DOI] [PubMed] [Google Scholar]
- 85.Ada G.A., Claffey H. Trees of Idoma Land. Dik Publishers; Otukpo, Nigeria: 2003. p. 177. [Google Scholar]
- 86.Igoli J.O., Gray L.A. Friedelanone and other triterpenoids from Hymenocardia acida. Int. J. Phys. Sci. 2008;3:156–158. [Google Scholar]
- 87.Sofidiya M., Lange C., Sattler L., Beukes D., Afolayan A., Odukoya O., Familoni O. Bioactivity profile of compounds isolated from Hymenocardia acida Tul. leaves. Planta Med. 2010;76:141. doi: 10.1055/s-0030-1264439. [DOI] [Google Scholar]
- 88.Mpiana P.T., Tshibanga D.S.T., Shetonde O.M., Ngobula K.N. In vitro antidrepanocytary activity (antisickle cell anaemia) of some Congolese plants. Phytomedicine. 2007;14:192–195. doi: 10.1016/j.phymed.2006.05.008. [DOI] [PubMed] [Google Scholar]
- 89.Mahmout Y., Mianpeurem T., Dolmazon R., Bouchu D., Fenet B. phiphile triterpenoids from Hymenorcardia acida Tul; Proceedings of 15 ème colloque sur la pharmacopée et la Médecine Traditionnelles Africaines; Libreville, Gabon. 1–4 December 2008. Phytoantimalarial and anti-inflammatory activities. [Google Scholar]
- 90.Abu A.H., Uchendu C.N. In vivo trypanocidal activity of hydroethanolic extract of Hymenocardia acida stem bark in rats. Vet. World. 2011;4:113–116. [Google Scholar]
- 91.Amom T.T., Yahwe S.R., Vershima A.J. Phytochemical and medicinal activities of Hymenocardia acida Tul (Euphorbiaceae): A Review. J. Nat. Prod. Plant Resour. 2013;3:11–16. [Google Scholar]
- 92.Abu A.H., Uchendu C.N., Ofukwu R.A. In vitro anti trypanosomal activity of crude extracts of some Nigerian medicinal plants. J. Appl. Biosci. 2009;21:1277–1282. [Google Scholar]
- 93.Umar I.A., Ene O., Okodaso D., Kimeng E., Stancheva G., Omage J.J. Amelioration of anaemia and organ damage by combined intraperitoneal administration of Vitamins A and C to Trypanosome brucei brucei infected rats. Afr. J. Biotechnol. 2007;6:2083–2086. [Google Scholar]
- 94.Umar I.A., Toh Z.A., Igbalajobi F.I., Igbokwe I.O., Gidado A. The effect of orally administered vitamins C and E on the severity of anaemia in T. brucei-infected rats. Trop. Vet. 1999;18:71–77. [Google Scholar]
- 95.Ibrahim M.A., Aliyu A.B., Sallau A.B., Bashir M., Yunusa I., Umar T.S. Senna occidentalis leaf extract possesses antitrypanosomal activity and ameliorates the trypanosome- induced anemia and organ damage. Pharmacog. Res. 2010;2:175–180. doi: 10.4103/0974-8490.65513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Lockett C.T., Grivetti L.E. Food related behaviour during drought: A study of rural Fulani, North Eastern Nigeria. Int. J. Food Sci. Nutr. 2000;51:91–107. doi: 10.1080/096374800100796. [DOI] [PubMed] [Google Scholar]
- 97.Hoet S., Pieters L., Muccioli G.G., Jean-Louis H., Opperdoes F.R., Quetin-Leclercq J. Antitrypanosomal activity of triterpenoids and sterols from the leaves of Strychnos spinosa and related compounds. J. Nat. Prod. 2007;70:1360–1363. doi: 10.1021/np070038q. [DOI] [PubMed] [Google Scholar]
- 98.Hoet S., Stevigny C., Herent M.F., Quetin-Leclerc J. Antitrypanosomal compounds from the leave essential oil of Strychnos spinosa. Planta Med. 2006;72:480–482. doi: 10.1055/s-2005-916255. [DOI] [PubMed] [Google Scholar]
- 99.Adesina S.K., Illoh H.C., Imoh I.J., Imoh E.J. African Mistletoes (Lornthacaee); Ethnopharmacology, Chemsitry and Medicinal values: An Update. Afr. J. Tradit. Complement. Altern. Med. 2013;10:161–170. doi: 10.4314/ajtcam.v10i4.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Inabo H.I., Fathuddin M.M. In vivo antitrypanosomal potentials of ethyl acetate leaf extracts of Punicagra natum against Trypanosoma brucei brucei. Adv. Agric. Biotechnol. 2011;1:82–88. [Google Scholar]
- 101.Ibrahim H.M., Ogbadoyib E.O., Bellob M.U., Yemisi I. Evaluation of antitrypanosomal activity of Adansonia digitata (methanol seed extract) in Albino mice. J. Sci. J. Vet. Adv. 2013;2:1–6. [Google Scholar]
- 102.Mann A., Gbate M., Nda-Umar A. Medicinal and Economic Plants of Nupeland. Jube-Evans Books and Publications; Bida, Nigeria: 2003. p. 276. [Google Scholar]
- 103.Gills L.S. Ethnomedical Uses of Plants in Nigeria. University of Nigerian Press; Benin City, Nigeria: 1992. p. 103. [Google Scholar]
- 104.Mann A., Egwim E.C., Banji B., Nda-Umar A., Mohammed G., Ekanem J.T. Efficacy of Dissotis rotundifolia on Trypanosoma brucei brucei infection in rats. Afr. J. Biochem. Res. 2009;3:005–008. [Google Scholar]
- 105.Tchoumbougnang F., Zollo P.H.A., Boyom F.F., Ngegae M.A., Bessiere J.M., Menut C. Aromatic plants of tropical Central Africa. XLVIII. Comparative study of the essential oils of four Hyptis species from Cameroun: H. lancedata Poit, H. pectinata (L) Poit, Hyptis spicigera Lam and Hyptis suaveoleus Poit. Flavour Fragr. J. 2005;20:340–343. doi: 10.1002/ffj.1441. [DOI] [Google Scholar]
- 106.Onayade O.A., Looma A., Scheffer J.J., Svendsen A.B. Composition of the leaf essential oil Hyptis Spicigera Lam. Flavour Fragr. J. 1990;5:101–105. doi: 10.1002/ffj.2730050209. [DOI] [Google Scholar]
- 107.Ladan Z., Amupitan J.O., Oyewale O.A., Okonkwo E.M., Ladan E.O., Odjobo B., Habila N. Chemical composition and biological activity of the volatile oils of Hyptisspicigera against Trypanosoma brucei brucei, (Tbb) found in Northern Nigeria. Afr. J. Pure Appl. Chem. 2011;5:53–58. [Google Scholar]
- 108.Arbonnier M. Trees, Shrubs and Lianas of West African Dry Zones. Cirad Margraf Publishers; Wageningen, The Netherlands: 2002. pp. 189–426. [Google Scholar]
- 109.Ibrahim M.A., Njoku G.C., Sallau A.B. In vivo activity of stem barks aqueous extract of Khaya senegalensis against Trypanosoma brucei. Afr. J. Biotechnol. 2008;7:661–663. [Google Scholar]
- 110.Umar I.A., Ibrahim M.A., Fari N.A., Isah S., Balogun D.A. J. In-vitro and -vivo anti-Trypanosoma evansi activities of extracts from different parts of Khaya senegalensis. Cell Anim. Biol. 2010;4:91–95. [Google Scholar]
- 111.Takin M.C., Attindehou S., Sezan A., Attakpa S.E., Baba-Moussa L. Bioactivity, therapeutic utility and toxicological risks of Khaya senegalensis. Ind. J. Pharm. Biol. Res. 2013;1:122–129. [Google Scholar]
- 112.Haruna Y., Kwanashie H.O., Anuka J.A., Atawodi S.E., Hussaini I.M. Bioassay- guided fractionation and Anti-trypanosocidal effect of fractions and crude methanol roots extracts of Securidaca longepedunculata in mice and rats. Int. J. Mod. Biochem. 2013;2:1–14. [Google Scholar]
- 113.Gbile Z.O., Adesina S.K. Nigerian Flora and its pharmaceutical potentials. J. Ethnopharmacol. 1987;19:1–17. doi: 10.1016/0378-8741(87)90135-8. [DOI] [PubMed] [Google Scholar]
- 114.Alli L.A., Okochi V.I., Adesokan A.A. Anti-trypanosomal activity and haematological effects of aqueous extract of leaves of Morinda lucida on Trypanosoma brucei brucei infected rats. Asian J. Pharm. Health Sci. 2011;1:111–115. [Google Scholar]
- 115.Asuzu I.U., Chineme C.N. Effects of Morinda lucida leaf extract on Trypanosoma brucei brucei infection in mice. J. Ethnopharmacol. 1990;30:307–313. doi: 10.1016/0378-8741(90)90109-7. [DOI] [PubMed] [Google Scholar]
- 116.Edoga C.O., Njoku O.O., Amadi E.N., Afomezie P.I. Effect of aqueous extract of Moringa oleifera on serum protein of Trypanosoma brucei-infected rats. Int. J. Sci. Technol. 2013;3:85–87. [Google Scholar]
- 117.Adeyemi O.S., Akanji M.A., Oguntoye S.A. Ethanolic leaf extract of Psidium guajava: Phytochemical and trypanocidal activity in rats infected with Trypanosoma brucei brucei. J. Med. Plant Res. 2009;3:420–423. [Google Scholar]
- 118.Oluyomi S.A., Melissa L.S., Musbau A.A., Vicky M.A. Anti-trypanosomal and cytotoxic activity of ethanolic extracts of Psidium guajava leaves in Alamar Blue based assays. Vet. Arh. 2011;81:623–633. [Google Scholar]
- 119.Adeyemi O.S., Akanji M.A., Ekanem J.T. Ethanolic extract of Psidium guajava influences protein and bilirubin levels in Trypanosome brucei brucei infested rats. J. Biol. Sci. 2012;12:111–116. doi: 10.3923/jbs.2012.111.116. [DOI] [Google Scholar]
- 120.Kabiru Y.A., Ogbadoyi E.O., Okogun J.I., Gbodi T.A., Makun H.A. Anti-trypanosomal Potential of Eucalyptus camaldulensis. Br. J. Pharmacol. Toxicol. 2013;4:25–32. [Google Scholar]
- 121.Shyam K., Hrubiec R.T., Furubayashi R., Cosby L.A., Sartorelli A.C. Methylating agents for use in the treatment of trypanosomiasis. J. Med. Chem. 1987;30:2157–2161. doi: 10.1021/jm00394a040. [DOI] [PubMed] [Google Scholar]
- 122.Philip G.P., Alan A.D., Krishnamurthy S., Curtis L.P., Alan C.S. The effects of the methylating agent 1,2-Bis (methylsulfonyl)-1-methylhydrazine on morphology, DNA content and mitochondrial function of Trypanosoma brucei subspecies. J. Eukaryot. Microbiol. 1991;38:172–177. doi: 10.1111/j.1550-7408.1991.tb04425.x. [DOI] [PubMed] [Google Scholar]
- 123.Maikai V.A., VivMaikai B., Kobo P.I. In vitro Effect of Aqueous Extract and Fraction IV Portion of Ximenia americana Stem Bark on Trypanosoma congolense DNA. J. Parasit. Res. 2014:2014. doi: 10.1155/2014/904318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Peter S., Nandal P.N., Prakash S.O., Rao J., Kumar S.P. In vitro antitrypanosomal evaluation of Picrorhiza kurroa rhibomes. J. Pharm. 2012;3:205–208. [Google Scholar]
- 125.Hotellier F., Delaveau P., Pousset J.L. Naucleidinal et epinaucleidinal, alcaloides du Nauclea latifolia. Phytochemistry. 1980;19:1884–1885. doi: 10.1016/S0031-9422(00)83847-9. [DOI] [Google Scholar]
- 126.Cerri R., Aquino R., de Simone F., Pizza C. New quinovic acid glycosides from Uncaria tomentosa. J. Nat. Prod. 1988;51:257–261. doi: 10.1021/np50056a010. [DOI] [PubMed] [Google Scholar]
- 127.Bero J., Beaufay C., Hannaert V., Hérent M.F., Michels P., Quetin-Leclercq J. Antitrypanosomal compounds from the essential oil and extracts of Keetia leucantha leaves with inhibitor activity on Trypanosoma brucei glyceraldehyde- 3-phosphate dehydrogenase. Phytomedicine. 2013;203:270–274. doi: 10.1016/j.phymed.2012.10.010. [DOI] [PubMed] [Google Scholar]
- 128.Benjamin T.V., Anucha T.C., Hugbo P.G. An approach to the study of medicinal plants with antimicrobial activity with reference to Mitracarpus scaber. In: Sofowora A., editor. The State of Medicinal Plants Research in Nigeria. Nigerian Society of Pharmacognosy, Ibadan University Press; Ibadan, Nigeria: 1986. pp. 243–245. [Google Scholar]
- 129.Nok A.J. Azaanthraquinone inhibits respiration and in vitro growth of long slender blood stream forms of Trypanosoma congolense. Cell Biochem. Funct. 2002;203:205–212. doi: 10.1002/cbf.948. [DOI] [PubMed] [Google Scholar]
- 130.Omale J., Okafor P.N. Comparative antioxidant capacity, membrane stabilization, polyphenol composition and cytotoxicity of the leaf and stem of Cissus multistriata. Afr. J. Biotechnol. 2008;7:3129–3133. [Google Scholar]
- 131.Nwodo N., Okoye F., Lai D., Debbab A., Kaiser M., Brun R., Proksch P. Evaluation of the in vitro trypanocidal activity of methylated flavonoid constituents of Vitex simplicifolia leaves. BMC Complem. Altern. Med. 2015;15:82. doi: 10.1186/s12906-015-0562-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Nwodo N.J., Agbo M.O., Brun R. In vitro and in vivo Antitrypanosomal studies of the leaf extract of Vitex simplicifolia. Afr. J. Pharm. Res. Dev. 2012;4:35–40. [Google Scholar]
- 133.Weniger B., Vonthron-Sénécheau C., Kaiser M., Brun R., Anton R. Comparative antiplasmodial, leishmanicidal and antitrypanosomal activities of several biflavonoids. Phytomedicine. 2006;13:176–180. doi: 10.1016/j.phymed.2004.10.008. [DOI] [PubMed] [Google Scholar]