Abstract
In this study we investigate the molecular mechanisms of caspases and mitochondria in the extrinsic and intrinsic signal apoptosis pathways in human leukemia HL-60 cells after in vitro exposure to 18α-glycyrrhetinic acid (18α-GA). Cells were exposed to 18α-GA at various concentrations for various time periods and were harvested for flow cytometry total viable cell and apoptotic cell death measurements. Cells treated with 18α-GA significantly inhibited cell proliferation and induced cell apoptosis in a dose-dependent manner, with an IC50 value of 100 μM at 48 h. The cell growth inhibition resulted in induction of apoptosis and decreased the mitochondria membrane potential (ΔΨm) and increased caspase-8, -9 and -3 activities. Furthermore, cytochrome c and AIF were released from mitochondria, as shown by western blotting and confirmed by confocal laser microscopy. Western blotting showed that 18α-GA increased the levels of pro-apoptotic proteins such as Bax and Bid and decreased the anti-apoptotic proteins such as Bcl-2 and Bcl-xl, furthermore, results also showed that 18α-GA increased Fas and Fas-L which are associated with surface death receptor in HL-60 cells. Based on those observations, the present study supports the hypothesis that 18α-GA-induced apoptosis in HL-60 cells involves the activation of the both extrinsic and intrinsic apoptotic pathways.
Keywords: 18α-glycyrrhetinic acid, mitochondria, caspase-3, apoptosis, HL-60 cells
1. Introduction
Leukemia is a heterogeneous group of hematopoietic malignancies [1] and the sixth leading cause of cancer-associated death, causing 7.1 deaths per 100,000 persons per year in the USA [2]. In Taiwan, where 4.2 per 100,000 persons die annually from the disease based on the 2012 report from the Department of Health, Executive Yuan, Taiwan [3] leukemia is the 13th leading cause of cancer-associated death. Acute leukemia are clonal disorders of hematopoietic stem cells that can be divided into acute myeloid leukemia (AML) which can occur at all ages and acute lymphoid leukemia (ALL) which most often occurs in children and adolescents, with approximately 60% of patients being younger than 20 years [4,5,6]. It was reported that about 50% of the young adult patients and approximately 90% of older patients with AML or ALL die from those diseases [5,6]. Currently, the cure-rate for patients with AML remains at approximately 25% [7], mainly due to the side effects which still are the major limit to treatment success. Thus, finding new compounds derived from natural products for leukemia is needed.
Induction of cancer cell apoptosis has been recognized to be one of the best strategies for anticancer agent activity. Apoptosis, a programmed cell death, can be divided into extrinsically and intrinsically mediated pathways. Both pathways involve the activation of caspases (cysteine proteases) for inducing cell apoptosis [8,9]. The extrinsically-activated pathway involves the activation of cell surface ligand-gate death receptors such as Fas and Fas-L and triggering of the pro-caspase-8 to form active-caspase-8 followed by activation of caspase-3 to induce apoptosis [10,11]. The intrinsically-activated pathway, also called the mitochondria-mediated pathway, through mitochondrial dysfunction, leads to cytochrome c release into the cytoplasm and induction of apoptosome formation with Apaf-1 and the activation of caspases for inducing apoptosis [12,13,14]. Furthermore, pro-apoptotic protein Bax, the ratio of Bak and anti-apoptotic protein Bcl-2 and Bcl-xl also play an important role affecting the mitochondrial dysfunction involved in the mitochondria-dependent apoptosis pathway [15,16].
Currently, about 47.1% of approved anticancer drugs are unmodified natural products, their semisynthetic derivatives, or molecules synthesized based on natural products [17]. Glycyrrhetic acid (GA), a component of the plant Glycyrrhiza uralensis, exhibits in vivo biological activities such as hepatoprotective, anti-inflammatory and anticancer functions [18,19,20]. The mechanisms of GA’s anticancer activities have been known to involve reduced cell proliferation, induced cell cycle arrest and apoptosis and the inhibition of cellular metastasis [19,21,22]. 18α-Glycyrrhetinic acid (18α-GA), a hydrolyzed metabolite of glycyrrhizin, had been shown to display anti-inflammatory, antiviral and anticancer activities [18,23,24,25]. It was reported that 18α-GA inhibits the proliferation of activated hepatic stellate cells (HSCs) and induces apoptosis and increases peroxisome proliferator-activated receptor-γ (PPAR-γ) expression and decreases NF-κB DNA-binding activity [26]. Glycyrrhetinic acid (GE) (a hydrolysis product of glycyrrhizic acid) had been shown to prevent or to induce the mitochondrial permeability transition (a phenomenon related to oxidative stress) in rat heart mitochondria depending on its concentration [27]. Recently, it was reported that 18α-GA inhibited gingival fibroblast growth by suppressing the G1/S phase transition and inducing apoptosis [28]. However, there is no available information to show the effects of 18α-GA on human leukemia cells, thus, the aim of present study was to investigate the in vitro toxic effects of 18α-GA on human leukemia HL-60 cells. The results showed that 18α-GA treatment of HL-60 cells resulted in apoptotic cell death through mediation by extrinsically and intrinsically mediated pathways.
2. Results
2.1. 18α-GA-Induced Cytotoxic Effects on Human Leukemia HL-60 Cells
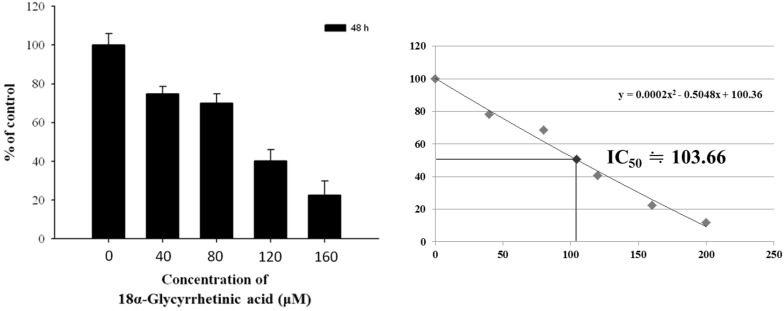
The cytotoxic effects of 18α-GA on HL-60 cells were evaluated by MTT colorimetric assay with the results shown in Figure 1. 18α-GA displayed the strongest HL-60 cell growth inhibition potency, accompanied by a reduction of viable cells and this inhibition is dose-dependent. The calculated IC50 for 18α-GA on HL-60 cells was 100 μM. Thus, we selected this concentration for further experiments.
Figure 1.
18α-GA induced cytotoxic effects on human leukemia HL-60 cells. HL-60 cells (1 × 104 cells/well) were placed onto 96-well plated in 100 μM of RPMI-1640 medium. The medium was containing 18α-GA (0, 40, 80, 120 and 160 μM) for 48 h. Percent of cell proliferation was measured by MTT assay as described in the Materials and Methods section.
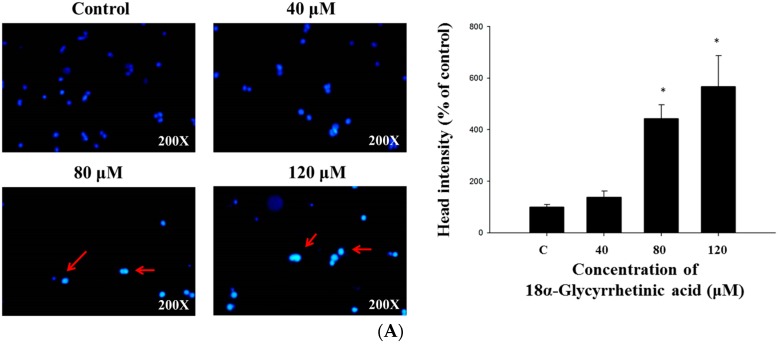
2.2. 18α-GA Induced Nuclear Condensation, DNA Damage and Fragmentation in HL-60 Cells
HL-60 cells were treated with 18α-GA (0, 40, 80 and 120 μM) for 48 h. Cells were stained with DAPI for measuring nuclear condensation (Figure 2A), or cells were subjected to a Comet assay for DNA damage evaluation (Figure 2B). The results indicated a brighter fluorescence of HL-60 cells after 48 h treatment of 18α-GA at 40–120 μM (Figure 2A) and this bright fluorescence represents nicked DNA and nuclear chromatin condensation. The results also indicated a comet tail for HL-60 cells after 48 h treatment of 18α-GA at 40–120 μM (Figure 2B) and the longer comet tail represents DNA damage. Both effects are dose-dependent manner. Cells were treated with 100 μM of 18α-GA for 48 h and DNA was isolated for gel electrophoresis with results shown in Figure 2C, where 18α-GA at 100 μM clearly induced a typical ladder pattern of internucleosomal fragmentation (DNA fragmentation). DNA fragmentation is a hallmark of cell apoptosis, thus this finding suggests that 18α-GA induces apoptosis of HL-60 cells.
Figure 2.
18α-GA induced nuclear condensation, DNA damage and fragmentation in HL-60 cells. HL-60 cells were treated with 18α-GA (0, 40, 80 and 120 μM) for 48 h. Cells were stained with DAPI for measuring nuclear condensation (A) or cells were performed by Comet assay for DNA damage evaluated (B); Cells were treated with 100 μM of 18α-GA for 48 h and DNA was isolated for gel electrophoresis for examining DNA fragmentation (C) as described in the Materials and Methods section. * p < 0.05, significant difference between 18α-GA-treated groups and control as analyzed by Student’s t test.
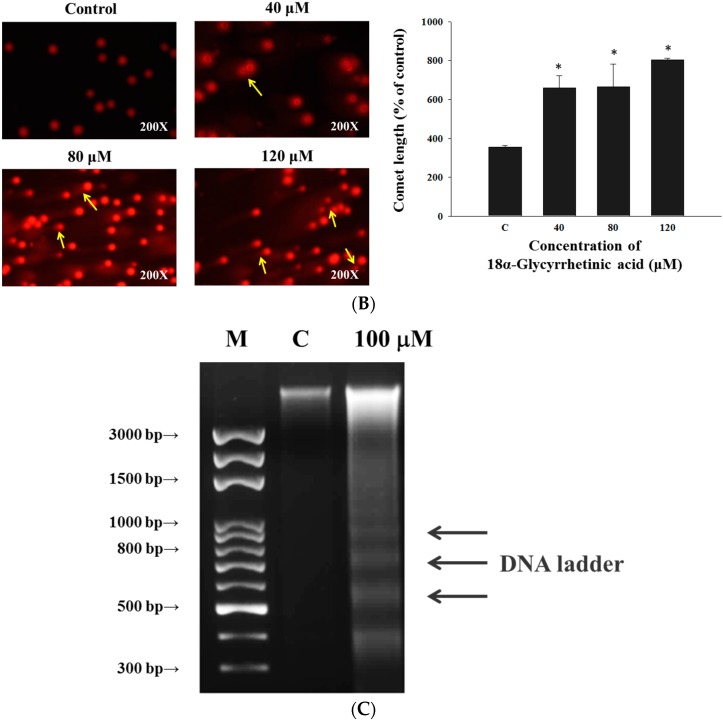
2.3. 18α-GA Decreased the Levels of Mitochondrial Membrane Potential (ΔΨm) and Increased the Activities of Caspase-8, -9 and -3 in HL-60 Cells
In order to confirm that 18α-GA induced cell apoptosis through the dysfunction of mitochondria and activations of caspase-8, -9 and -3 in HL-60 cells, cells were treated with 18α-GA (100 μM) for 6, 12, 24 and 48 h and were analyzed by flow cytometric assay and the results are shown in Figure 3. 18α-GA decreased the levels of mitochondrial membrane potential (ΔΨm) from 6 h to 48 h treatment (Figure 3A) when compared to untreated groups. These results indicated that ΔΨm are involved in 18α-GA induced cell apoptosis in HL-60 cells in vitro. The results showed that 18α-GA increased caspase-8 (Figure 3B), -9 (Figure 3C) and -3 (Figure 3D) activities compared to untreated groups, thus, caspase-8, -9 and -3 are involved in 18α-GA induced cell apoptosis of HL-60 cells in vitro. Cells were pretreated with caspase-3 inhibitor (z-DEVD-FMK) for 1 h and then treated with 18α-GA and the results shown in Figure 3E,F indicated that 18α-GA increased the total viability but decreased the activities of caspase-3 when compared to untreated groups. Based on these findings, it indicated that 18α-GA induced cell apoptosis through the activation of caspase-3.
Figure 3.
18α-GA decreased the levels of mitochondrial membrane potential (ΔΨm) and increased the activities of caspase-8, -9 and -3 in HL-60 cells. Cells were treated with 18α-GA (100 μM) for 6, 12, 24 and 48 h and were analyzed by flow cytometric assay for the levels of mitochondrial membrane potential (ΔΨm) (A); caspase-8 (B); caspase-9 (C) and caspase-3 (D) activities. Cells were pretreated with z-DEVD-FMK (caspase-3 inhibitor) and then treated with 18α-GA for measuring the activities of caspase-3 (E) and cell viability (F). * p < 0.05, significant difference between 18α-GA-treated groups and the control as analyzed by Student’s t test.
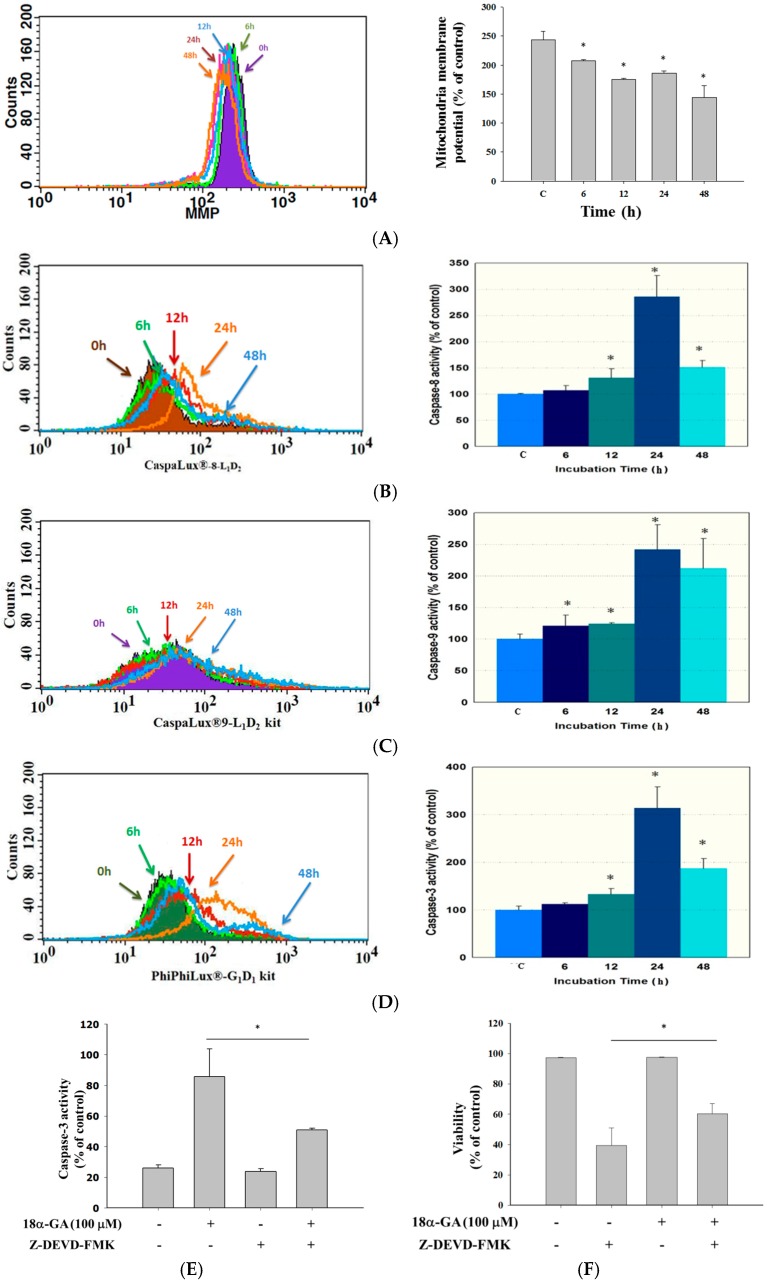
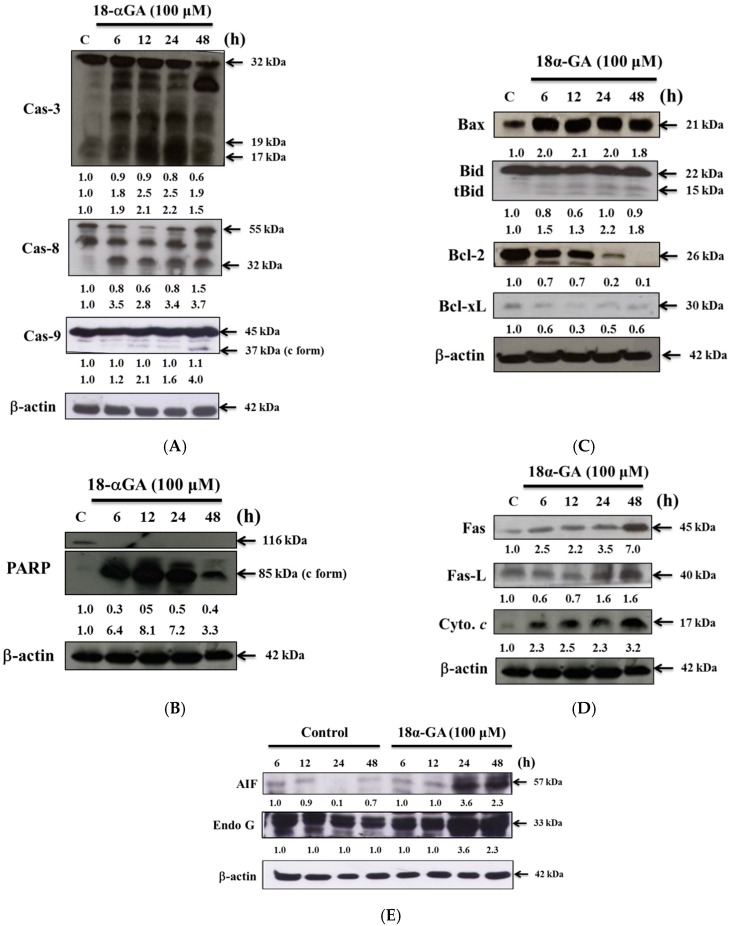
2.4. 18α-GA Altered Apoptosis Associated Protein Expression in HL-60 Cells
In order to examine 18α-GA-induced cell apoptosis via the alteration of apoptosis associated protein expression in HL-60 cells, cells were treated with 18α-GA (100 μM) for 6, 12, 24 and 48 h and then apoptosis-associated proteins were examined by western blotting (Figure 4). The results showed that 18α-GA significantly increased the expression of active-caspase-3, -8 and -9 (Figure 4A), cleaved-form-PARP (Figure 4B), Bax and t-Bid (Figure 4C), Fas, Fas-L and cytochrome c (Figure 4D), AIF and Endo G (Figure 4E) but decreased the anti-apoptotic proteins such as Bcl-2 and Bcl-xL (Figure 4C) in HL-60 cells that are associated with cell apoptosis. Those results indicate that 18α-GA induces apoptosis of HL-60 cells through surface death receptor and mitochondria-dependent pathways.
Figure 4.
18α-GA affects apoptosis associated protein expression in HL-60 cells. Cells were treated with 18α-GA (100 μM) for 6, 12, 24 and 48 h and then apoptosis associated proteins were examined by western blotting as described in the Materials and Methods section. (A) active-caspase-8,-9 and -3; (B) PARP; (C) Bax, Bid, Bcl-2 and Bcl-xL; (D) Fas, Fas-L and cytochrome c (Figure 4D); (E) AIF and Endo G.
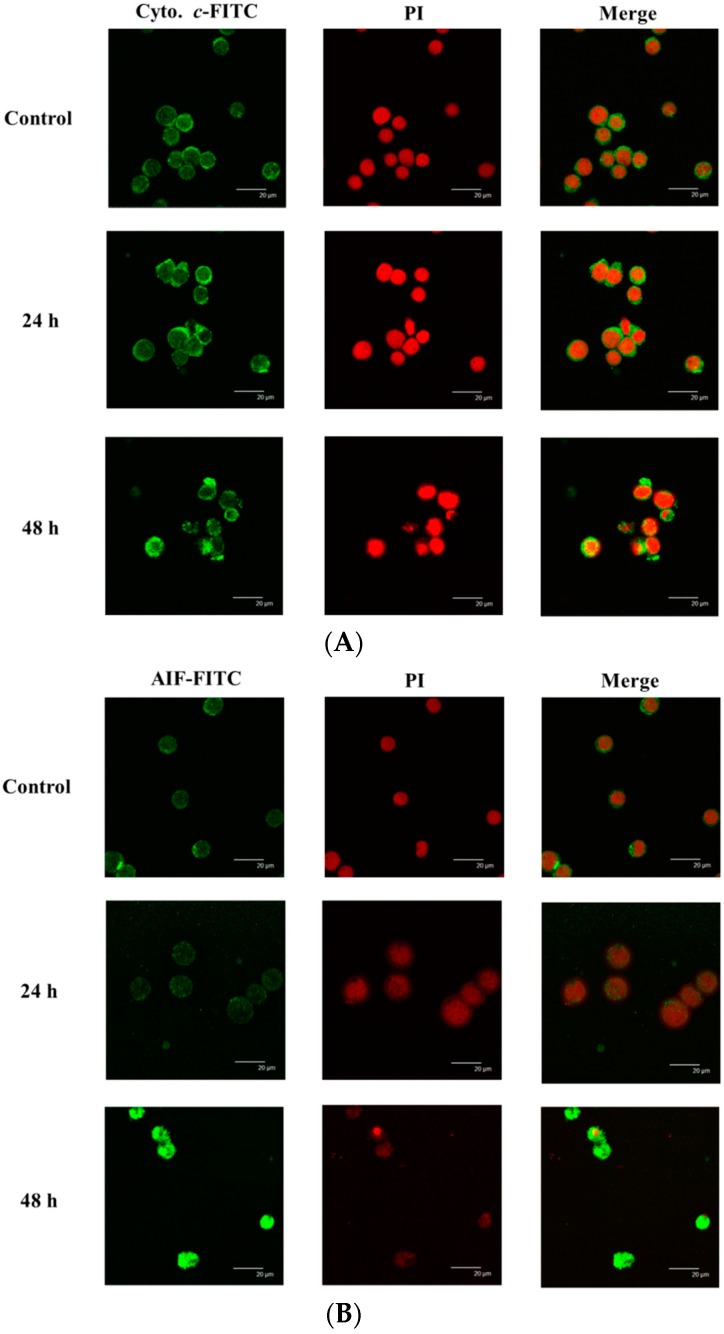
2.5. 18α-GA Altered the Translocation of Apoptotic Associated Proteins in HL-60 Cells
To further investigate how 18α-GA alters the translocation of apoptosis-associated proteins in HL-60 cells, we conducted confocal laser microscopy experiments (Figure 5). The results indicated that 18α-GA increased cytochrome c (Figure 5A) and AIF (Figure 5B) expression in HL-60 cells. These observations indicate that cytochrome c and AIF were released from the mitochondria into the cytoplasm compared to the control group.
Figure 5.
18α-GA affects the translocation of apoptotic associated proteins in HL-60 cells. Cells were treated with 100 μM of 18α-GA for 48 h and stained by anti- cytochrome c (A); and AIF (B) and then stained with secondary antibody and examined and photographed with a Leica TCS SP2 confocal laser microscopy system as described in the Materials and Methods section.
3. Discussion
Numerous reports have shown that some clinical anticancer drugs could be obtained from natural products, thus, finding novel anticancer agents from natural plants has been recognized as one of the best strategies for the development of chemotherapeutic agents. Glycyrrhetinic acid (GE) can occupy mineralocorticoid and glucocorticoid receptors [29] with a measurable affinity for mineralocorticoid receptors in mononuclear leukocytes [30]. Furthermore, GE can block 11-β-hydroxysteroid dehydrogenase type 1, thus reducing the availability of cortisol at the adipocyte level [31]. Although several reports have demonstrated that 18α-GA induced cytotoxic effects on human cancer cells, there is no available information to show if 18α-GA induces cytotoxic effects on human leukemia HL-60 cells. In the present study, we examined the in vitro cytotoxicity of 18α-GA on HL-60 cells. Firstly, the anti-proliferation effects of 18α-GA on HL-60 cells were investigated and MTT assay results indicated that 18α-GA inhibited cell proliferation with an IC50 of 100 μM (Figure 1). Next, we examined 18α-GA-induced nuclear condensation, DNA damage and fragmentation and we found that 18α-GA induced nuclear condensation (Figure 2A), DNA damage (Figure 2B) and fragmentation (Figure 2C) that are the hallmarks of cell apoptosis, which means that 18α-GA induces cell apoptosis in HL-60 cells in vitro. Thirdly, we investigated 18α-GA induced cell apoptosis and whether or not it occurred through mitochondrial dysfunction and involved caspase activities and the results indicated that 18α-GA decreased the levels of ΔΨm (Figure 3A), and increased the activities of caspas-8, -9 and -3 (Figure 3B–D). Fourth, we investigated possible protein expression associated with cell apoptosis, thus, western blotting was used to examine the protein expression and the results indicated that 18α-GA increased caspase-8, -9 and -3 (Figure 4A) and cleaved-form-PARP (Figure 4B), increased pro-apoptotic proteins such as Bax, t-Bid and decreased anti-apoptotic proteins like Bcl-2 and Bcl-xL (Figure 4C) and induced Fas, Fas-L and cytochrome c (Figure 4D), and increased AIF and Endo G (Figure 4E). Fifth, we further investigated whether 18α-GA induced cytochrome c and AIF from mitochondria, which was assayed by confocal laser microscopy and results indicated that 18α-GA increased the releases of cytochrome c and AIF from mitochondria into the cytoplasm (Figure 5A,B).
Herein, we found that 18α-GA inhibited cell proliferation and led to a decrease in the total viability when compared to untreated groups, which is in agreement with other reports which demonstrated that 18α-GA inhibits the proliferation of activated hepatic stellate cells (HSCs) [26]. In order to investigate how 18α-GA reduced total viability and whether this went through the induction of apoptosis in HL-60 cells, we used a DNA gel electrophoresis assay which indicated that 18α-GA induced cell apoptosis based on the development of DNA fragmentation (DNA ladder) that is a characteristic of cell apoptosis and this finding also is in agreement with other reports which indicated that 18α-GA induced cell apoptosis in hepatic stellate cells (HSCs) [26].
It is well documented that anticancer drugs induced cell death through the induction of cell apoptosis which can go through mitochondrial dysfunction or decreased levels of ΔΨm [32,33]. Furthermore, Ca2+ accumulation can impair mitochondrial function and lead to increased release of reactive oxygen species (ROS) [34]. We used a flow cytometry assay and found that 18α-GA decreased the levels of ΔΨm in HL-60 cells (Figure 3A) and these effects are time-dependent. This pathway is named the intrinsic signaling pathway. It was reported that the ratio of Bax/Bcl-2 is involved in the levels of ΔΨm, so if this agent caused decreased levels of ΔΨm in mitochondria which can cause cytochrome c and/or AIF release, it could lead to cell apoptosis [35,36]. Thus, we examined associated protein expression and we found that 18α-GA increased the pro-apoptotic proteins such as Bax and t-Bid (Figure 4B) and decreased the anti-apoptotic proteins Bcl-2 and Bcl-xl (Figure 4C) and also increased cytochrome c and AIF (Figure 4E) in HL-60 cells. This finding is in agreement with reports which indicated that 18α-GA decreased the anti-apoptotic proteins such as Bcl-2 and Bcl-xL in human gingival fibroblasts [28]. Based on those findings, we suggest that 18α-GA induces apoptosis of HL-60 cells through a mitochondria-dependent pathway. We also used confocal laser microscopy to examine the release of apoptotic proteins from the mitochondria and the results indicated that 18α-GA increased cytochrome c (Figure 5A) and AIF (Figure 5B) release from mitochondria to the cytoplasm.
It also is well known that some anticancer drugs inducing cancer cell apoptosis are involved in the activation of caspases such as caspase-8, -9 and -3, therefore, some apoptotic pathways are also named caspases-dependent pathways [37]. We used flow cytometry to assay the activities in HL-60 cells after exposure to 100 μM of 18α-GA and we found that 18α-GA increased the activities of caspase-8, -9 and -3 (Figure 3B–D), which was also confirmed by western blotting (Figure 4A) which indicated that 18α-GA increased the active forms of caspase-8, -9 and -3 in HL-60 cells. It is well documented that cell apoptosis may go through the extrinsic death receptor pathway and/or the intrinsic mitochondrial pathway [38,39]. In the extrinsic pathway, Fas and Fas-L activate pro-caspase-8 and then activate downstream executioner caspases, including caspase-3, causing apoptosis or they also cleave Bid into truncated Bid this leads to mitochondrial dysfunction leading to cytochrome c release and induced caspase-9 and -3 activation to induce apoptosis, which is called the intrinsic pathway [12]. Those pathways also can be called caspases-dependent pathways. Furthermore, it is also well documented that agent-induced cell apoptosis may go through the decrease of the levels of ΔΨm and subsequent release of AIF and Endo G from the mitochondria into nuclei to induce apoptosis. It was reported that mTOR inhibitors have been used to treat several advanced cancers [40], thus, further investigations are needed regarding whether or not 18α-GA induced cancer cell apoptosis involves AKT/mTOR pathways.
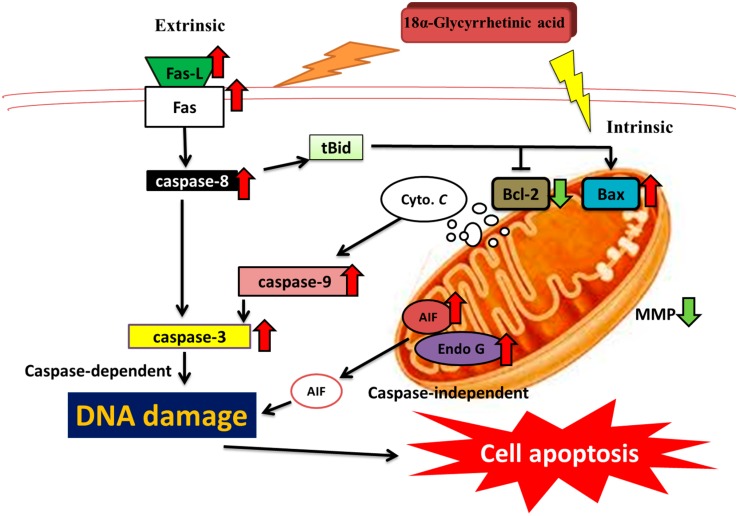
In summary, the present study demonstrated that 18α-GA inhibits the in vitro cell growth of HL-60 cells by inducing cellular apoptosis. Those findings also revealed that 18α-GA induced cell apoptosis was caspase-dependent and the mitochondria-dependent pathways were accompanied by the releases of cytochrome c, caspase-9 and -3 activation and/or AIF release. Overall the possible pathways for 18α-GA induced cell apoptosis are summarized in Figure 6. These findings indicate the therapeutic potential of 18α-GA in treating human leukemia.
Figure 6.
The possible signaling pathways for 18α-GA induced apoptosis in human leukemia HL-60 cells in vitro.
4. Materials and Methods
4.1. Chemicals and Reagents
18α-Glycyrrhetinic acid (18α-GA), 4,6-diamidino-2-phenylindole (DAPI), dimethyl sulfoxide (DMSO), N-acetyl-l-cysteine (NAC), propidium iodide (PI) and trypsin-EDTA were obtained from Sigma Chemical Co. (St. Louis, MO, USA). RPMI-1640 medium, fetal bovine serum (FBS), l-glutamine and antibiotics (penicillin-streptomycin) were purchased from GIBCO®/Invitrogen Life Technologies (Carlsbad, CA, USA). Primary antibody against PARP, caspase-3,-8, -9, AIF, Endo G, Bid, Bax, Bcl-2, Bcl-xL, cytochrome c, Fas, Fas-L and peroxidase conjugated secondary antibodies were purchased from Cell Signaling (St Louis, MO, USA). 18α-GA was dissolved in DMSO. Cell culture grade DMSO was used for vehicle at 0.1%.
4.2. Cell Culture
The human leukemia HL-60 cell line was purchased from the Food Industry Research and Development Institute (Hsinchu, Taiwan). HL-60 cells were routinely maintained in RPMI-1640 medium supplemented with 10% FBS and antibiotics (100 units/mL penicillin, 100 μg/mL streptomycin and 2 mM glutamine) in a humidified atmosphere containing 5% CO2 at 37 °C [41,42].
4.3. Cell Proliferation Examination
Cytotoxicity of 18α-GA was evaluated by the MTT assay. HL-60 cells (1 × 104 cells/well) were placed onto 96-well plates in 100 μM of RPMI-1640 medium. The medium contained 18α-GA (0, 40, 80, 120 and 160 μM) for 48 h. MTT (5 mg/mL, 20 μL) was added to each well for 4 h and then 100 μL/well of DMSO was added to dissolve the formazan. Optical density of each well was measured by a microplate reader (Bio-Rad 680, BioRad Inc., Hercules, CA, USA) at 570 nm as previously described [41,43,44].
4.4. Nuclear Staining with DAPI
Cells were placed in 6-well plate at a density of 2 × 105 cells/well and cells were incubated with 18α-GA at concentrations ranging from 40–120 μM for 48 h. Cells were fixed in 3% formaldehyde for 20 min, and then washed with PBS. After disrupting with 0.1% Triton X-100/PBS for 20 min and then washed with PBS. Finally, we add the DAPI solution (1 μg/mL) at 37 °C without light. Nuclear morphologies were photographed using a fluorescence microscope (Eclipse TE 300, Nikon, Tokyo, Japan) as described previously [45].
4.5. Comet Assay
Cells were placed in 6-well plate at a density of 2 × 105 cells/well and cells were incubated with 18α-GA ranging from 40–120 μM for 48 h. After treatment, cells from each treatment were harvested to examine the DNA damage with the Comet assay as described previously [45].
4.6. DNA Gel Electrophoresis
Cells (2 × 105 cells/well) were maintained in 6-well plates and incubated with 18α-GA concentrations ranging from 40–120 μM for 48 h. Cells were harvested and DNA extracted by using DNA isolation kit as described previously [46]. DNA from each treatment (2 μg) was separated in 0.5% agarose gel as described previously [46]. Ethidium bromide was added to stain DNA and the intensity of the DNA bands was examined and photographed under a fluorescence microscope.
4.7. Measurement of the Levels of Mitochondrial Membrane Potential (ΔΨm)
Cells (2 × 105 cells/well/6-well plate) were treated with 100 μM of 18α-GA for 0, 6, 12, 24 and 48 h. Cells from each treatment were harvested and washed twice with PBS, re-suspended in 500 μL of DiOC6 (4 mol/L) and were incubated at 37 °C for 30 min without light. After incubations, cells were measured for the levels of ΔΨm by flow cytometry (FACS Calibur, Becton Dickinson, San Joes, CA, USA) as described previously [41].
4.8. Measurements of Caspase-3, Caspase-8 and Caspase-9 Activities
Cells (2 × 105 cells/well/6-well plate) were treated with 100 μM of 18α-GA for 0, 6, 12, 24 and 48 h. Cells were collected, re-suspended in 25 μL of 10 μM substrate solution containing CaspaLux8-L1D2 for caspase-8 activity measurement, or containing PhiPhiLux-G1D1 for caspase-3 activity measurement, or containing CaspaLux9-M1D2 for caspase-9 activity measurement before being incubated at 37 °C for 60 min. After incubations, cells were washed and caspase-8, -3 and -9 activities were analyzed by flow cytometry as described previously [41], or cells were pretreated with caspase-3 inhibitor (Z-EDVD-FMK) for 1 h [41] and then were treated with 100 μM of 18α-GA for 48 h and cell viability and caspase-3 activity was measured by flow cytometry.
4.9. Western Blotting Analysis
Cells (1 × 106 cells/dish) were placed in 10 cm dish and treated with 100 μM of 18α-GA for 0, 6, 12, 24 and 48 h. Both adherent and floating cells were collected and lysed by lysis buffer and total protein was measured by Bio-Rad protein assay kit (Bio-Rad) as described previously [45]. The protein of total cells was separated by 12% (v/v) sodium dodecyl sulfate polyacrylamide gel electrophoresis (SDS-PAGE) and transferred onto polyvinylidene difluoride (PVDF) membranes (Millipore, Temecula, CA, USA) which were subsequently stained with the primary antibodies against caspase-8, -3 and -9, PARP, Bax, Bid, Bcl-2, Bcl-xL, Fas, Fas-L, cytochrome c, AIF, Endo G, and β-actin followed by a peroxidase conjugated secondary antibodies. Protein bands on the membrane were visualized and detected using an enhanced chemiluminescence using ECL detection system (Millipore) [45,46]. Protein expression was quantified by densitometry using Image J.
4.10. Confocal Laser Scanning Microscopy Assay
Cells (2 × 105 cells/well) were placed in 6-well plate and were treated with 100 μM of 18α-GA for 48 h and then were fixed with 4% formaldehyde in PBS for 15 min. After fixation, cells were treated with 0.1% Triton-X 100 in PBS for 20 min and using 2% BSA for blocking non-specific binding sites, were washed with PBS twice and stained with primary antibodies anti-cytochrome c and -AIF (all in green fluorescence) for overnight. Cells were washed and were stained with secondary antibody (FITC-conjugated goat anti-mouse IgG) and PI (red fluorescence) for nuclein examinations. Slides were mounted, examined and photo-micrographed under a Leica TCS SP2 Confocal Spectral Microscope (Leica Microsystems, Heidelberg, Germany) as described previously [45].
4.11. Statistical Analysis
Values were presented as mean ± standard deviation (SD) from triplicate experiments. Statistical analysis of all data was conducted by Student’s t test. The p < 0.05 was considered statistically significant.
Acknowledgments
This work was supported by grant CMU103-ASIA-01 from China Medical University, Taichung, Taiwan. Experiments and data analysis were performed in part through the use of the Medical Research Core Facilities Center, Office of Research & Development at China medical University, Taichung, Taiwan.
Author Contributions
Y.C.H., P.P.W. and J.G.C. contributed equally to the conception and design of the study; Y.C.H. contributed equally to acquisition of data and analysis and interpretation of data; C.L.K., K.W.L., J.J.L., J.L.Y. and R.S.C.W. drafting the article or revising it critically for important intellectual content; P.P.W. and J.G.C. final approval of the version to be submitted.
Conflicts of Interest
The authors declare that there are no conflicts of interest.
Footnotes
Sample Availability: Samples of the compounds are not available from the authors.
References
- 1.Song H., Fares M., Maguire K.R., Siden A., Potacova Z. Cytotoxic effects of tetracycline analogues (doxycycline, minocycline and COL-3) in acute myeloid leukemia HL-60 cells. PLoS ONE. 2014;9:e114457. doi: 10.1371/journal.pone.0114457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.National Cancer Institute Surveillance, Epidemiology, and End Results Program website. [(accessed on 19 May 2014)]; Available online: http://seer.cancer.gov/statfacts/html/leuks.html.
- 3.Ministry of Health and Welfare Caues of death in Taiwan, 2012. [(accessed on 27 July 2013)]; Available online: http://www.mohw.gov.tw/CHT/DOS/Statistic.aspx?f_list_no=474&fod_list_no=5007.
- 4.Bene M.C., Nebe T., Bettelheim P., Buldini B., Bumbea H., Kern W., Lacombe F., Lemez P., Marinov I., Matutes E., et al. Immunophenotyping of acute leukemia and lymphoproliferative disorders: A consensus proposal of the European LeukemiaNet Work Package 10. Leukemia. 2011;25:567–574. doi: 10.1038/leu.2010.312. [DOI] [PubMed] [Google Scholar]
- 5.Dohner H., Estey E.H., Amadori S., Appelbaum F.R., Buchner T., Burnett A.K., Dombret H., Fenaux P., Grimwade D., Larson R.A., et al. Diagnosis and management of acute myeloid leukemia in adults: Recommendations from an international expert panel, on behalf of the European LeukemiaNet. Blood. 2010;115:453–474. doi: 10.1182/blood-2009-07-235358. [DOI] [PubMed] [Google Scholar]
- 6.Pui C.H., Robison L.L. Look, A.T.Acute lymphoblastic leukaemia. Lancet. 2008;371:1030–1043. doi: 10.1016/S0140-6736(08)60457-2. [DOI] [PubMed] [Google Scholar]
- 7.Warkentin A.A., Lopez M.S., Lasater E.A., Lin K., He B.L., Leung A.Y., Smith C.C., Shah N.P., Shokat K.M. Overcoming myelosuppression due to synthetic lethal toxicity for FLT3-targeted acute myeloid leukemia therapy. eLife. 2014;3 doi: 10.7554/eLife.03445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim R. Recent advances in understanding the cell death pathways activated by anticancer therapy. Cancer. 2005;103:1551–1560. doi: 10.1002/cncr.20947. [DOI] [PubMed] [Google Scholar]
- 9.Philchenkov A., Zavelevich M., Kroczak T.J., Los M. Caspases and cancer: Mechanisms of inactivation and new treatment modalities. Exp. Oncol. 2004;26:82–97. [PubMed] [Google Scholar]
- 10.Jayaraj R., Gupta N., Rao P.V. Multiple signal transduction pathways in okadaic acid induced apoptosis in HeLa cells. Toxicology. 2009;256:118–127. doi: 10.1016/j.tox.2008.11.013. [DOI] [PubMed] [Google Scholar]
- 11.Pietraforte D., Matarrese P., Straface E., Gambardella L., Metere A., Scorza G., Leto T.L., Malorni W., Minetti M. Two different pathways are involved in peroxynitrite-induced senescence and apoptosis of human erythrocytes. Free Radic. Biol. Med. 2007;42:202–214. doi: 10.1016/j.freeradbiomed.2006.10.035. [DOI] [PubMed] [Google Scholar]
- 12.Fulda S. Targeting extrinsic apoptosis in cancer: Challenges and opportunities. Semin. Cell Dev. Biol. 2015;39:20–25. doi: 10.1016/j.semcdb.2015.01.006. [DOI] [PubMed] [Google Scholar]
- 13.Kroemer G., Galluzzi L., Brenner C. Mitochondrial membrane permeabilization in cell death. Physiol Rev. 2007;87:99–163. doi: 10.1152/physrev.00013.2006. [DOI] [PubMed] [Google Scholar]
- 14.Zhou Q., Li Y., Jin J., Lang L., Zhu Z., Fang W., Chen X. Lx2–32c, a novel taxane derivative, exerts anti-resistance activity by initiating intrinsic apoptosis pathway in vitro and inhibits the growth of resistant tumor in vivo. Biol. Pharm. Bull. 2012;35:2170–2179. doi: 10.1248/bpb.b12-00513. [DOI] [PubMed] [Google Scholar]
- 15.Brunelle J.K., Letai A. Control of mitochondrial apoptosis by the Bcl-2 family. J. Cell Sci. 2009;122:437–441. doi: 10.1242/jcs.031682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nascimento Pde S., Ornellas A.A., Campos M.M., Scheiner M.A., Fiedler W., Alves G. Bax and bcl-2 imbalance and HPB infection in penile tumors and adjacent tissues. Prog. Urol. 2004;14:353–359. [PubMed] [Google Scholar]
- 17.Newman D.J., Cragg G.M. Natural products as sources of new drugs over the last 25 years. J. Nat. Prod. 2007;70:461–477. doi: 10.1021/np068054v. [DOI] [PubMed] [Google Scholar]
- 18.Jeong H.G., You H.J., Park S.J., Moon A.R., Chung Y.C., Kang S.K., Chun H.K. Hepatoprotective effects of 18beta-glycyrrhetinic acid on carbon tetrachloride-induced liver injury: Inhibition of cytochrome P450 2E1 expression. Pharmacol. Res. 2002;46:221–227. doi: 10.1016/S1043-6618(02)00121-4. [DOI] [PubMed] [Google Scholar]
- 19.Sharma G., Kar S., Palit S., Das P.K. 18beta-glycyrrhetinic acid induces apoptosis through modulation of Akt/FOXO3a/Bim pathway in human breast cancer MCF-7 cells. J. Cell. Physiol. 2012;227:1923–1931. doi: 10.1002/jcp.22920. [DOI] [PubMed] [Google Scholar]
- 20.Xiao Y., Xu J., Mao C., Jin M., Wu Q., Zou J., Gu Q., Zhang Y., Zhang Y. 18Beta-glycyrrhetinic acid ameliorates acute Propionibacterium acnes-induced liver injury through inhibition of macrophage inflammatory protein-1alpha. J. Biol. Chem. 2010;285:1128–1137. doi: 10.1074/jbc.M109.037705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jayasooriya R.G., Dilshara M.G., Park S.R., Choi Y.H., Hyun J.W., Chang W.Y., Kim G.Y. 18beta-Glycyrrhetinic acid suppresses TNF-αinduced matrix metalloproteinase-9 and vascular endothelial growth factor by suppressing the AKT-dependent NF-κB pathway. Toxicol. In Vitro. 2014;28:751–758. doi: 10.1016/j.tiv.2014.02.015. [DOI] [PubMed] [Google Scholar]
- 22.Lin D., Zhong W., Li J., Zhang B., Song G., Hu T. Involvement of BID translocation in glycyrrhetinic acid and 11-deoxy glycyrrhetinic acid-induced attenuation of gastric cancer growth. Nutr. Cancer. 2014;66:463–473. doi: 10.1080/01635581.2013.877498. [DOI] [PubMed] [Google Scholar]
- 23.Agarwal M.K., Iqbal M., Athar M. Inhibitory effect of 18β-glycyrrhetinic acid on 12-O-tetradecanoyl phorbol-13-acetate-induced cutaneous oxidative stress and tumor promotion in mice. Redox Rep. 2005;10:151–157. doi: 10.1179/135100005X57346. [DOI] [PubMed] [Google Scholar]
- 24.Hoever G., Baltina L., Michaelis M., Kondratenko R., Baltina L., Tolstikov G.A., Doerr H.W., Cinatl J., Jr. Antiviral activity of glycyrrhizic acid derivatives against SARS-coronavirus. J. Med. Chem. 2005;48:1256–1259. doi: 10.1021/jm0493008. [DOI] [PubMed] [Google Scholar]
- 25.Matsui S., Matsumoto H., Sonoda Y., Ando K., Aizu-Yokota E., Sato T., Kasahara T. Glycyrrhizin and related compounds down-regulate production of inflammatory chemokines IL-8 and eotaxin 1 in a human lung fibroblast cell line. Int. Immunopharmacol. 2004;4:1633–1644. doi: 10.1016/j.intimp.2004.07.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zong L., Qu Y., Xu M.Y., Dong Y.W., Lu L.G. 18alpha-glycyrrhetinic acid extracted from Glycyrrhiza radix inhibits proliferation and promotes apoptosis of the hepatic stellate cell line. J. Dig. Dis. 2013;14:328–336. doi: 10.1111/1751-2980.12041. [DOI] [PubMed] [Google Scholar]
- 27.Battaglia V., Brunati A.M., Fiore C., Rossi C.A., Salvi M., Tibaldi E., Palermo M., Armanini D., Toninello A. Glycyrrhetinic acid as inhibitor or amplifier of permeability transition in rat heart mitochondria. Biochim. Biophys. Acta. 2008;1778:313–323. doi: 10.1016/j.bbamem.2007.10.008. [DOI] [PubMed] [Google Scholar]
- 28.Takeuchi R., Hiratsuka K., Arikawa K., Ono M., Komiya M., Akimoto Y., Fujii A., Matsumoto H. Possible pharmacotherapy for nifedipine-induced gingival overgrowth: 18alpha-glycyrrhetinic acid inhibits human gingival fibroblast growth. Br. J. Pharmacol. 2016;173:913–924. doi: 10.1111/bph.13410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Armanini D., Karbowiak I., Funder J.W. Affinity of liquorice derivatives for mineralocorticoid and glucocorticoid receptors. Clin. Endocrinol. 1983;19:609–612. doi: 10.1111/j.1365-2265.1983.tb00038.x. [DOI] [PubMed] [Google Scholar]
- 30.Armanini D., Wehling M., Weber P.C. Mineralocorticoid effector mechanism of liquorice derivatives in human mononuclear leukocytes. J. Endocrinol. Investig. 1989;12:303–306. doi: 10.1007/BF03349993. [DOI] [PubMed] [Google Scholar]
- 31.Armanini D., Nacamulli D., Francini-Pesenti F., Battagin G., Ragazzi E., Fiore C. Glycyrrhetinic acid, the active principle of licorice, can reduce the thickness of subcutaneous thigh fat through topical application. Steroids. 2005;70:538–542. doi: 10.1016/j.steroids.2005.01.007. [DOI] [PubMed] [Google Scholar]
- 32.Mohan S., Abdelwahab S.I., Kamalidehghan B., Syam S., May K.S., Harmal N.S., Shafifiyaz N., Hadi A.H., Hashim N.M., Rahmani M., et al. Involvement of NF-κB and Bcl2/Bax signaling pathways in the apoptosis of MCF7 cells induced by a xanthone compound Pyranocycloartobiloxanthone A. Phytomedicine. 2012;19:1007–1015. doi: 10.1016/j.phymed.2012.05.012. [DOI] [PubMed] [Google Scholar]
- 33.Simon H.U., Haj-Yehia A., Levi-Schaffer F. Role of reactive oxygen species (ROS) in apoptosis induction. Apoptosis. 2000;5:415–418. doi: 10.1023/A:1009616228304. [DOI] [PubMed] [Google Scholar]
- 34.Santulli G., Xie W., Reiken S.R., Marks A.R. Mitochondrial calcium overload is a key determinant in heart failure. Proc. Natl. Acad. Sci. USA. 2015;112:11389–11394. doi: 10.1073/pnas.1513047112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Abarikwu S.O., Farombi E.O. Atrazine induces apoptosis of SH-SY5Y human neuroblastoma cells via the regulation of Bax/Bcl-2 ratio and caspase-3-dependent pathway. Pestic Biochem. Physiol. 2015;118:90–98. doi: 10.1016/j.pestbp.2014.12.006. [DOI] [PubMed] [Google Scholar]
- 36.Tor Y.S., Yazan L.S., Foo J.B., Wibowo A., Ismail N., Cheah Y.K., Abdullah R., Ismail M., Ismail I.S., Yeap S.K. Induction of Apoptosis in MCF-7 Cells via Oxidative Stress Generation, Mitochondria-Dependent and Caspase-Independent Pathway by Ethyl Acetate Extract of Dillenia suffruticosa and Its Chemical Profile. PLoS ONE. 2015;10:e0127441. doi: 10.1371/journal.pone.0127441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Minko T., Kopeckova P., Kopecek J. Preliminary evaluation of caspases-dependent apoptosis signaling pathways of free and HPMA copolymer-bound doxorubicin in human ovarian carcinoma cells. J. Control. Release. 2001;71:227–237. doi: 10.1016/S0168-3659(01)00220-6. [DOI] [PubMed] [Google Scholar]
- 38.Desagher S., Martinou J.C. Mitochondria as the central control point of apoptosis. Trends Cell Biol. 2000;10:369–377. doi: 10.1016/S0962-8924(00)01803-1. [DOI] [PubMed] [Google Scholar]
- 39.Reed J.C. Apoptosis-regulating proteins as targets for drug discovery. Trends Mol. Med. 2001;7:314–319. doi: 10.1016/S1471-4914(01)02026-3. [DOI] [PubMed] [Google Scholar]
- 40.Santulli G., Totary-Jain H. Tailoring mTOR-based therapy: Molecular evidence and clinical challenges. Pharmacogenomics. 2013;14:1517–1526. doi: 10.2217/pgs.13.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Shang H.S., Shih Y.L., Lee C.H., Hsueh S.C., Liu J.Y., Liao N.C., Chen Y.L., Huang Y.P., Lu H.F., Chung J.G. Sulforaphane-induced apoptosis in human leukemia HL-60 cells through extrinsic and intrinsic signal pathways and altering associated genes expression assayed by cDNA microarray. Environ. Toxicol. 2016 doi: 10.1002/tox.22237. [DOI] [PubMed] [Google Scholar]
- 42.Chang Y.-M., Velmurugan B.K., Kuo W.-W., Chen Y.-S., Ho T.-J., Tsai C.-T., Ye C.-X., Tsai C.-H., Tsai F.-J., Huang C.-Y. Inhibitory effect of alpinate Oxyphyllae fructus extracts on Ang II-induced cardiac pathological remodeling-related pathways in H9c2 cardiomyoblast cells. Biomedicine. 2013;3:148–152. doi: 10.1016/j.biomed.2013.05.001. [DOI] [Google Scholar]
- 43.Patathananone S., Thammasirirak S., Daduang J., Chung J.G., Temsiripong Y., Daduang S. Bioactive compounds from crocodile (Crocodylus siamensis) white blood cells induced apoptotic cell death in hela cells. Environ. Toxicol. 2015 doi: 10.1002/tox.22108. [DOI] [PubMed] [Google Scholar]
- 44.Ho T.-Y., Lo H.-Y., Li C.-C., Chen J.-C., Hsiang C.-Y. In vitro and in vivo bioluminescent imaging to evaluate anti-Escherichia coli activity of Galla Chinensis. Biomedicine. 2013;3:160–166. doi: 10.1016/j.biomed.2013.04.003. [DOI] [Google Scholar]
- 45.Yu C.C., Yang S.T., Huang W.W., Peng S.F., Huang A.C., Tang N.Y., Liu H.C., Yang M.D., Lai K.C., Chung J.G. Bisdemethoxycurcumin induces DNA damage and inhibits DNA repair associated protein expressions in NCI-H460 human lung cancer cells. Environ. Toxicol. 2015 doi: 10.1002/tox.22187. [DOI] [PubMed] [Google Scholar]
- 46.Ho C.C., Huang A.C., Yu C.S., Lien J.C., Wu S.H., Huang Y.P., Huang H.Y., Kuo J.H., Liao W.Y., Yang J.S., et al. Ellagic acid induces apoptosis in TSGH8301 human bladder cancer cells through the endoplasmic reticulum stress- and mitochondria-dependent signaling pathways. Environ. Toxicol. 2014;29:1262–1274. doi: 10.1002/tox.21857. [DOI] [PubMed] [Google Scholar]