Abstract
This review paper summarizes the antibacterial effects of phytochemicals of various medicinal plants against pathogenic and cariogenic streptococcal species. The information suggests that these phytochemicals have potential as alternatives to the classical antibiotics currently used for the treatment of streptococcal infections. The phytochemicals demonstrate direct bactericidal or bacteriostatic effects, such as: (i) prevention of bacterial adherence to mucosal surfaces of the pharynx, skin, and teeth surface; (ii) inhibition of glycolytic enzymes and pH drop; (iii) reduction of biofilm and plaque formation; and (iv) cell surface hydrophobicity. Collectively, findings from numerous studies suggest that phytochemicals could be used as drugs for elimination of infections with minimal side effects.
Keywords: streptococci, biofilm, adherence, phytochemical, quorum sensing, S. mutans, S. pyogenes, S. agalactiae, S. pneumoniae
1. Introduction
The aim of this review is to summarize the current knowledge of the antimicrobial activity of naturally occurring molecules isolated from plants against Streptococcus species, focusing on their mechanisms of action. This review will highlight the phytochemicals that could be used as alternatives or enhancements to current antibiotic treatments for Streptococcus species. The scope of the review is limited to inhibitory effects of phytochemicals, mainly polyphenols, against Streptococcus species and where possible, their mechanisms of action against the major virulence factors will be discussed. Due to their major implications on human health, this review has largely focused on four Streptococcus species: (i) S. mutans (ii) S. pyogenes (iii) S. agalactiae and (iv) S. pneumoniae. To explain the potential mechanisms of inhibition of the phytochemicals, S. mutans has been used as the major example.
1.1. Streptococci
Streptococcus species are bacteria belonging to the Firmicutes phylum under the order of Lactobacillales and the family of Streptococcaceae [1]. Three genera exist within the family of Streptococcaceae including Streptococcus, Lactococcus and Lactovum of which Streptococcus is most diverse, containing 79 species [1]. A number of Streptococcus species are pathogenic to humans and animals, with S. pyogenes and S. pneumoniae as the most important pathogens [1]. These Gram positive bacteria generally appear as pairs or chains, are spherical to ovoid in shape, nutritionally fastidious, with fermentative metabolism and many of them form capsules [2].
Streptococcus species are found mostly in the oral cavity and nasopharynx and form a significant portion of the normal microbiota of humans and animals [2,3]. In healthy individuals, normal microbiota are harmless, however, they can cause infection under certain conditions, such as immune compromised stage [2,4]. Streptococcus species (e.g., S. pyogenes, S. agalactiae, and S. pneumoniae) can be classified serologically based on the cell wall carbohydrates into groups A to V [2,5,6]. Streptococci can also be grouped based on morphological differences, type of hemolysis on blood agar, biochemical reactions, cell wall pili-associated protein, and polysaccharide capsule (specific for group B streptococci) [7]. To date more than 85 capsule antigenic types of S. pneumoniae, 124 serotypes of S. pyogenes and nine CPS (capsular polysaccharide) serotypes of S. agalactiae have been proposed [7,8,9]. The cell wall of streptococci is among the most studied bacterial cell walls [7,10].
1.2. Streptococcal Infections and Major Virulence Factors
The diseases caused by streptococci range from non-life-threatening conditions like dental caries, pharyngitis (strep throat) to life-threatening conditions such as necrotizing fasciitis and meningitis (Table 1) [5]. Of all the oral streptococci, S. mutans is considered to be the etiological agent of dental caries. According to Petersen et al., industrialized countries spend 5%–10% of their public health expenditures on periodontal disease, dental caries and related dental care [11]. Unquestionably, one of the most common global diseases is dental caries [12].
Table 1.
Demonstrated virulence factors of streptococci species, disease caused and the associated social and financial cost with the disease.
| Organism | Diseases | Adherence Site | Estimated Cases/Costs |
|---|---|---|---|
| S. mutans | Dental caries | Tooth surface, other bacteria present in the biofilm on the surface of the tooth [5] | 500 million visits to dentists and an estimated $108 billion spent on dental services in united states in 2010 [27] |
| Dental plaque | |||
| Endocarditis | |||
| S. pyogenes | Pharyngitis | Mucosal surfaces of pharynx, skin [25] | 1–2.6 million cases of strep throat, erythromycin-resistant, invasive S. pyogenes causes 1300 illnesses and 160 deaths in united states each year. The total cost (medical and non-medical ) of group A streptococcal pharyngitis among school aged children in united states ranges from $224 to $539 million per year [27] |
| Cellulitis | |||
| Streptococcal toxic-shock syndrome | |||
| Necrotizing fasciitis | |||
| Rheumatic fever | |||
| Sequela | |||
| Erysipelas glomerulonephritis | |||
| S. agalactiae | Neonatal sepsis | Mucosal surfaces of vaginas and recta of pregnant women, skin [32] | Clindamycin-resistant S. agalactiae causes an estimated 7600 illnesses and 440 deaths yearly in U.S. 27,000 cases of severe S. agalactiae disease, such as blood infections or meningitis, occurred in 2011, causing 1575 deaths in U.S. [27] |
| Meningitis | |||
| Systemic infection in immuno-compromised individuals | |||
| S. pneumoniae | Otitis media | Mucous membranes of the nasopharynx [33] | Cases of resistant pneumococcal pneumonia result in about 32,000 additional doctor visits and about 19,000 additional hospitalizations and costs associated are approximately $96 million in U.S. [27] |
| Bacteraemia | |||
| Pneumonia | |||
| Meningitis | |||
| Bronchitis | |||
| Sinusitis | |||
| Laryngitis | |||
| Epiglottitis |
A more pathogenic Streptococcus specie, S. pyogenes can be carried asymptomatically by humans but can cause mild to severe diseases, such as pharyngitis, tonsillitis, scarlet fever, cellulitis, erysipelas, rheumatic fever, post-streptococcal glomerulonephritis, necrotizing fasciitis, etc. (Table 1) [13]. It has been estimated that severe S. pyogenes infections lead to 517,000 deaths per year globally in addition to 233,000 deaths caused by rheumatic fever disease [14]. In United States alone 1800 invasive S. pyogenes disease-related deaths (necrotizing fasciitis and streptococcal toxic shock syndrome) are reported annually [15,16].
Another specie that most frequently has been linked to neonatal infections (early-onset and late-onset) such as sepsis, pneumonia and meningitis is S. agalactiae [17,18]. Late-onset neonatal infections (occurring at the age of 1–3 months) put infants at higher risk (as high as 20% even with proper antibiotic treatment) than early-onset neonatal infections of neonates (occurring within the first 24–48 h up to 7 days) [17]. In adults, S. agalactiae could cause peripartum choriomamniotitis, bacteremia, pneumonia, endocarditis, osteomyelitis, urinary tract infections, skin and soft tissue infections with immunocompromised individuals at highest risk (Table 1) [18,19].
Other important human pathogenic streptococci, S. pneumoniae, claimed the lives of 826,000 children under the age of five in year 2000 [20,21]. Globally, about 14.5 million episodes of invasive pneumococcal disease occur every year however mortality varies at 5%–35% depending on other factors (e.g., comorbidity, age, site of infection) [22]. In USA, annually 4 million episodes of pneumococcal diseases account for 445,000 hospitalizations and 22,000 deaths and S. pneumoniae is still the leading cause of bacteremia, meningitis, and pneumonia among all age groups (Table 1) [23].
Streptococci have a variety of potent virulence factors enabling them to cause such diverse infections [5]. Adhesins are one such factor because they play an important role in colonization [5]. Adhesins and virulence factors of streptococci have been reviewed extensively [5,6,24,25]. Carcinogenicity capacity of S. mutans is largely dependent on the ability of the bacteria to adhere and produce acid [12]. S. mutans glucosyltransferases assist in the adhesion process by synthesizing insoluble glucan from sucrose [12]. On the other hand, S. pyogenes produces extracellular proteins that have been shown to give rise to the remarkable virulence of the organism, triggering a nonspecific host immunological response [26]. Specific virulence factors assist S. pyogenes to attach to the host tissue, escape phagocytosis, and spread by infiltrating the host epithelial layers followed by colonizing [5,17,27,28,29]. In the case of S. agalactiae, major virulence and pathogenic factors enable the bacterium to stimulate sepsis syndrome, adhere to epithelial surface succeeding invasion, and avoidance of phagocytosis [30]. S. agalactiae attaches to host cells via fibronectin, fibrinogen and laminin [30]. For S. pneumoniae, a number of proteins, including hyaluronate lyase, pneumolysin, neuraminidases, the major autolysin, choline binding protein A, pneumococcal surface antigen A have been suggested to be virulence associated factors of this bacterium [31]. In addition, polysaccharide capsule is considered to be a key virulence factor [31].
1.3. Mechanism of Pathogenicity of Streptococcal Diseases
1.3.1. Adhesion, Plaque, and Biofilm Formation of Streptococcal Species
To cause disease, a bacterial pathogen needs to meet several basic requirements. First, it must be able to adhere to the tissue surface and compete with the normal microbiota present on that surface [5,34,35]. Subsequently, for sustainable attachment, biofilms are developed and this may lead to invasion of the host tissue [6]. To establish biofilm, planktonic bacteria attaches to either inert or coated surfaces and this can be mediated by electrostatic contacts or bacterial surface adhesins [36]. Attachment is followed by proliferation of the primary colonizers and their co-aggregation with other planktonic bacteria, production of exopolysaccharide which stabilizes the architecture, leading to the maturation of the biofilm [36]. Sessile bacteria then could detach and form biofilms at different site [36,37,38]. Biofilm formation is not an attribute only specific to a few species, but a general ability of all microorganisms. Biofilm formation pathways are species specific, diverse, and dependent on environmental factors [39]. Although diverse, there are common features among all biofilms: (i) cells in the biofilm are glued together by an extracellular matrix made of exopolysaccharides, proteins, and occasionally nucleic acids; (ii) biofilm formation is initiated by environmental and bacterial signals; and (iii) biofilm offers bacteria protection from antibiotics and environmental stresses including immunological responses of the host [39]. Bacterial biofilms can build up on abiotic (plastic, glass, metal, etc.) or biotic (plants, animals, and humans) surfaces [34,38,40]. Mammalian-tissue colonizing species of Streptococcus live within biofilm in the natural environment [6,41,42].
Bacteria increase the expression of their outer cell surface adhesins when environmental conditions allow promoting cell-cell and cell-surface interaction [6,43]. Streptococci owe their success in colonization to their wide range of proteins expressed on their surfaces [5,6]. Surface adhesins facilitate interrelation with salivary, serum, extracellular matrix elements, host cells and other microbes [5,6]. Many of these adhesins are anchored to the cell wall peptidoglycan via their C-terminus or to the cell membrane via their N-terminal lipid (lipoproteins), and other adhesins remain surface localized through non-covalent interactions with other proteins or polysaccharides on the cell surface [6,44].
Most bacterial pathogens, including streptococci, have long filamentous structures known as pilli or fimbriae that are also involved in adhesion and biofilm formation [34]. In Gram-positive bacteria, hydrophobic components can be found: (i) covalently bound to cell wall, such as streptococcal M and F proteins, (ii) in the cytoplasmic membrane (e.g., lipoteichoic acid (LTA) of S. pyogenes or sialic acid of S. agalactiae) or (iii) located on the surface, like pilli or fimbriae [6,44,45]. Aside from adherence, biofilms are of significant importance as approximately 65% of human bacterial infections involve biofilms [45] including Streptococcus species (e.g., S. mutans, S. pyogenes, S. agalactiae, and S. pneumoniae) [34,40,41,46]. Clinically, biofilms are important because they reduce susceptibility of the bacteria to antimicrobials, prospering resistant bacteria leading to persistent infections [47,48].
The primary cause of dental caries is dental plaque which is a complex biofilm [41]. Broad spectrum of saliva proteins contribute to and initiate adhesion and dental biofilm formation [41,49,50]. Adhesion of S. pyogenes to various host cells is facilitated by the capsule and several factors embedded in the cell wall including M protein, LTA, and F protein [6,25,51]. M protein not only helps bacteria to attach to the host tissue but also inhibits opsonization by binding to host complement regulators and to fibrinogen [52]. A recent study has demonstrated that S. pyogenes pilus promotes pharyngeal cell adhesion and biofilm formation [53]. Altering surface hydrophobicity by sub-minimum inhibitory concentration of penicillin and rifampin reduces the adhesion of S. pyogenes to epithelial cells suggesting that surface-associated LTA will determine the surface hydrophobicity content of S. pyogenes, which consequently affects the bacteria’s interaction with mammalian host cells [54,55,56].
S. agalactiae produces several virulence factors such as adhesins [6]. These surface proteins and LTA of S. agalactiae bacterial cell wall contribute to the adhesion process mediating the invasion of eukaryotic cells [30]. Non-encapsulated S. agalactiae strains show increased adherence to eukaryotic cells [30]. In vitro studies have shown that S. agalactiae adheres to vaginal, buccal, endothelial and pulmonary epithelial cells [30]. Many clinical isolates of S. mutans, S. pyogenes, and S. agalactiae have been reported to be hydrophobic while their avirulent counterpart strains lacked this feature [57,58,59,60]. Studies have shown that S. pneumoniae adheres to abiotic surfaces, e.g., polystyrene or glass, and forms three-dimensional biofilm structures that are about 25 micrometers deep [34]. This three-dimensional structure enables the bacteria to survive for long periods within the bacterial community [34].
1.3.2. Proton-Extrusion and Glycolysis of Streptococcal Species
Vital to the survival of bacteria is the regulation of the cytoplasmic pH as cellular activity requires a specific pH range [61]. Cytoplasmic pH is modulated by environmental pH, production, or consumption of internal protons, and transferring acids and bases across the plasma membrane [62]. The function of F-adenosine triphosphatase (F-ATPase) in streptococci is to regulate internal pH by pumping protons out of the cell [62,63]. The physiological role of streptococcal F0F1-ATPase is to alkalinize the cytoplasmic pH in the acidic pH range and to establish a proton reserve for a variety of secondary transport systems [64,65,66]. Streptococci are deficient in respiratory chains and are unable to produce a large proton gradient across the membrane, however, they make up for this lack by utilizing a range of basic transport systems [66]. For example, synthesizing a cytochrome-like respiratory chain, formation of adenosine triphosphate (ATP) from adenosine diphosphate (ADP) and inorganic phosphate by coupling the nicotinamide adenine dinucleotide hydrogen (NADH) oxidation with phosphorylation reaction [66,67,68]. Generally, ATPase in streptococci does not function as ATP synthase because of lack of a functional electron transport system; thus, it functions as hydrolase for proton movements coupled to ATP hydrolysis that are used for the generation of the proton gradient [66]. Streptococci utilize the glycolytic pathway to metabolize glucose to lactic acid [4,66]. Glucose is taken up, phosphorylated to glucose-6-phosphate through the phosphoenolpyruvate-dependent phosphotransferase system, and then converted to pyruvate, and eventually to lactic acid [66,69].
S. pneumoniae and oral streptococci could adapt to different environments and this capability is facilitated by ATPase regulating the intracellular concentration of solutes, including protons, and maintaining the pH homeostasis by proton extrusion [66,70]. Adherence is dependent: (i) on the synthesis of extracellular polysaccharides (mostly glucans) from the disaccharide sucrose through glucosyltransferases (GTFs) for S. mutans, and (ii) bacteria’s ability to produce acid by glycolysis and its tolerance to the produced acid [71]. S. mutans has the properties of acid production from sugar metabolism causing a drop in pH in dental plaque [72]. Low pH values in the plaque matrix leads to demineralization of tooth enamel, selection of acid-tolerant streptococci and eventually dental caries [72]. The glucans synthesized by GTFs promote the binding and accumulation of S. mutans and other bacteria on the tooth surface and contribute to the formation of biofilms [72,73,74,75]. S. mutans increases the proton-translocation, and F-ATPase activity when the environment’s pH drops, thereby this bacterium could withstand acidification influences [66,76,77]. F-ATPase transfers protons out of cells with the assistance of ATP hydrolysis to maintain its intracellular pH (e.g., more alkaline than the extracellular environment) [76]. F-ATPase enzyme is composed of two domains; (i) F1, the cytoplasmic catalytic domain; and (ii) F0, the proton-conducting membrane domain [67,78]. S. mutans does not produce catalase or cytochromes (thus a heme-based electron transport system) and so does not have oxidative phosphorylation linked to trans-membrane electron transport [66,79].
1.3.3. Glucan Synthesis, Aggregation and Quorum Sensing of Streptococcal Species
Glucans interact with surface-associated glucan binding proteins of S. mutans to initiate colonization, cell-cell aggregation and the firm adherence of its cells to tooth surfaces [72,80]. S. mutans produces three types of GTFs: GTFB, GTFC, GTFD, and each of these enzymes are composed of two functional domains: (i) an amino-terminal catalytic domain (CAT); and (ii) a carboxyl-terminal glucan-binding domain (GBD) [81]. GTFB and GTFC, located on the cell surface, are encoded by gtfB and gtfC genes and GTFD is encoded by the gtfD gene [82]. Therefore, one of the strategies to control biofilm formation and dental caries is to inhibit the activity of GTFs: (i) GTFB (which synthesizes a polymer of mostly insoluble α1, 3-linked glucan); (ii) GTFC (which synthesizes a mixture of insoluble α-1,3-linked glucan and soluble α-1,6-linked glucan); and/or (iii) GTFD (which synthesizes water-soluble glucans rich in α-1,6-glucosidic linkages) [83,84].
Many streptococci use quorum-sensing systems to regulate several physiological properties, including the ability to incorporate foreign deoxyribonucleic acid (DNA), tolerate acid, form biofilm, and become virulent [85,86,87,88]. Quorum sensing, a strategy of cell-to-cell communication in a biofilm community, regulates unnecessary over-population and nutrient competition [89,90]. Bacterial activities including virulence gene expression within biofilms is regulated by the occurrence of quorum sensing [91]. This topic as well has comprehensively been discussed in review articles [87,92,93].
1.4. Treatment of Streptococcal Infection
Penicillin or one of its derivatives (e.g., amoxicillin and ampicillin) are the recommended antibiotic treatment for non-allergic patients diagnosed with S. pyogenes and S. agalactiae infections [27]. For allergic individuals, azithromycin and clarithromycin are recommended and in fact, azithromycin is prescribed more commonly than penicillin [94]. For severe S. pyogenes infections like necrotizing fasciitis and toxic shock syndrome, a combination of penicillin and clindamycin are prescribed [95]. S. pyogenes and S. agalactiae are not resistant to penicillin, but over time they have become resistant to clindamycin, tetracycline, vancomycin and macrolides (e.g., erythromycin, azithromycin and clarithromycin) [27]. Clarithromycin, clindamycin and vancomycin resistance among S. pyogenes and S. agalactiae strains are most concerning [27].
1.5. Antibiotic Resistance and Emerging Threats
Antimicrobial resistance is compromising the treatment of invasive infections including severe streptococcal infections [27]. This threat becomes significant in vulnerable patients (e.g., individuals undergoing chemotherapy, dialysis and organ transplants) due to infection-related complications [27]. This puts healthcare providers in the position to use antibiotics that may be more toxic to the patient, and frequently more expensive, leading to an increased risk of long-term disability and lower survival rates [27].
According to Frieden, director of the U.S. Center for Disease Control and Prevention (CDC), antimicrobial resistance is a serious health threat in the 21st century [27]. Infections caused by resistant bacteria are now on the rise and their resistance to multiple types and classes of antibiotics is worrisome [96]. The decrease in the rate of pathogen susceptibility to antibiotics has made it much more difficult to combat the infectious diseases [27]. The CDC’s 2013 report has prioritized drug-resistant S. pneumoniae as a serious threat, and erythromycin-resistant S. pyogenes and clindamycin-resistant S. agalactiae as concerning threats [27].
1.6. Possible Alternatives for Classical Antibiotics
Plants produce diverse secondary metabolites or phytochemicals, most of which are isoprenoids and polyphenols and their oxygen-substituted derivatives such as tannins that could be raw materials for future drugs [97]. Herbs and spices contain useful medicinal compounds including antibacterial chemicals, and researchers have found that many of these compounds inhibit the growth of pathogenic bacteria [97]. Accordingly, experimental observations have shown that herbal preparations are active against many of the pathogens (Table 2).
Table 2.
Folklore medicine used for Streptococcal diseases or diseases with similar clinical Presentations.
| Folklore Medicinal Plant | Targeted Disease Condition |
|---|---|
| Agrimonia eupatoria L. | Acute sore throat and chronic nasopharyngeal catarrh [118,119] |
| Arnica montana L. | Inflammation of oral, throat region [99,120,121] |
| Lonicera japonica Thunb. | Erysipelas, pharyngitis, upper respiratory infection [100] |
| Morella cerifera (L.) Small | Cold and sore throat [101,122] |
| Parmentiera aculeate (Kunth) Seem | Otitis media [123] |
| Adansonia digitata L. | Otitis media [102,124] |
| Anacardium occidentale L. | Sore throat [103,125] |
| Uvaria chamae P. Beauv. | Sore throat [64,126,127] |
| Adansonia digitata L. | Inflamed gums and infected teeth [128] |
| Carica papaya L. | Toothache [129] |
| Hyoscyamus niger L. | Toothache [130,131] |
| Eucalypthus camaldulensis Dehn. | |
| Anacardium occidentale L. | Toothache, sore gums [132] |
| Annona reticulata | Toothache [133,134] |
| Annona squamosa Linn | |
| Uvaria chamae P. Beauv | Inflamed gums [135] |
| Abutilon indicum (L.) Sweet, Baliospermum axillare Blume, Blumea lacera (Burm. f.) DC., Canna indica L., Ocimum tenuiflorum L., Oroxylum indicum (L.) Vent., Polygonum aviculare L., Solanum indicum Linn., Vernonia patula (Aiton) Merrill [136] | For the relief of symptoms of bronchitis, pneumonia, influenza [136] |
| Vigna radiata (L.) R. Wilczek Andrographis paniculata (Burm. f.) Wall. ex Nees [137,138] | Treatment of sepsis [137,138] |
From the period of 1981 to 2006, 109 new antibacterial drugs were approved for treatment of infectious diseases of which 69% originated from natural products, and 21% of antifungal drugs were natural derivatives or compounds mimicking natural products [98]. Various medicinal plants have recently been tested for their antimicrobial activity and all have proven that phytochemicals, particularly polyphenols, exhibit significant antibacterial activity against Streptococcus species (Table 3).
Table 3.
Inhibitory effects of phytochemicals against selected Streptococcus species.
| Species | Strain | Plant | EM | MIC, IZD | Ref. |
|---|---|---|---|---|---|
| S. pyogenes | Passiflora foetida L. | EE, ACE | 100–400 µg/mL, 10–20 mm | [139] | |
| ATCC 19615 | Ageratum conyzoides L. | AE, EE, ME | 1–2 mg/mL | [140] | |
| Laggera tomentosa Sch-Bip | |||||
| Syzygeum guineense DC. | |||||
| Cordia africana Lam. | |||||
| Ferula communis L. | |||||
| Discopodium peninervum Hochst | |||||
| Olea europea subsp. cuspidate | |||||
| Crescentia cujete L. | CEE | 5 mg/mL | [141] | ||
| Cl | Uvaria chamae P. Beauv | CAE, HAE | 9–12 mm, 100 µg/mL | [127] | |
| Vernonia amygdalina Del. | |||||
| Garcinia kola Heckel | |||||
| CI | Uvaria chamae P. Beauv | CDEE, HEE | 6–21 mm, 100 µg/mL | [127] | |
| Vernonia amygdalina Del. | |||||
| Garcinia kola Heckel | |||||
| Aframomum melegueta Schum. | |||||
| CI | Zingiber officinale Roscoe | EE | 2–6 mm, 0.0005–0.389 µg/mL | [142] | |
| CI | Garcinia kola Heckel | EE | 0.0005–0.44 µg/mL | [142] | |
| CI | Coccinia grandis (L.) Voigt | HE | 5.5–7 mm | [143] | |
| CI | Eucalyptus globulus Labill. | ME | 32–64 mg/L | [144] | |
| HITM 100 | Quercus ilex L. | BE, EAE | 10 mm, 512 μg/mL | [106] | |
| CI | Prunus armeniaca L. | CEE, BE | 250 μg/mL | [145] | |
| ATCC 19615 | Capsicum chinense Jacq. | AE | 15–34 mm | [146] | |
| ATCC 19615 | Allium sativum L. | AE | 29 mm | [146] | |
| CI | Spilanthes acmella Murr. | CHE | 256 μg/mL | [147] | |
| CI | Cinnamomum zeylanicum Garcin ex Blume | EO | 6.25 µL/mL | [107] | |
| CI | Thymus vulgaris L. Syzygium aromaticum (L.) Merr. & L.M. Perr | EO | 12.5 µL/mL | [107] | |
| CI | Sechium edule (Jacq.) Sw. | EE | 10–15 mm | [108] | |
| S. mutans | ATCC 25175 | Coffea canephora Pierre ex Froehner | AE | 5 mg/mL | [148,149] |
| ATCC 25175 | Baeckea frutescens L. | 75% ME | 14–22 mm, 20, 50 mg/mL | [150,151] | |
| Glycyrrhiza glabra L. | |||||
| Kaempferia pandurata Roxb. | |||||
| Physalis angulata L. | |||||
| Quercus infectoria Oliv. | |||||
| MTCC-890 | Nut gall (Quercus infectoria) | Petro, ether Water, metahnol |
12–23 mm | [150] | |
| UA159 | Rheedia brasiliensis Planch. & Triana | HE | 1.25–2.5 μg/mL | [152] | |
| UA159 | Camellia sinensis (L.) Kuntze | Epigallocatechin gallate by HPLC | 31.25 μg/mL | [153] | |
| ATCC 700610 | Prosopis spicigera Linn. | ACE, CHE DEE, EAE, EE, ME, PEE | 9.76–1250 μg/mL | [154] | |
| ATCC 700610 | Zingiber officinale Roscoe | ACE, CHE DEE, EAE, EE, ME, PEE | 625–2500 μg/mL | [154] | |
| Trachyspermum ammi (L.) Sprague ex Turrill | CE, PEE | 40–320 μg/mL | [155] | ||
| ATCC 25175 | Siraitia grosvenorii (Swingle) A. M. Lu & Zhi Y. Zhang | commercial extract | 6 μg/mL | [156,157] | |
| S. puenomonia | CI | Zingiber officinale Roscoe | EE | 0.001–0.7 µg/mL | [142] |
| serotype 6B | Agaricus blazei Murill | AE | [158] | ||
| serotype 6B | Plantago major L. | AE | 0.48 mg/kg | [159] | |
| ATCC 49619, penicillin resistant and sensitive clinical strains | Garcinia afzelii Engl. | 90% EE | 6– >1500 µg/mL | [160] | |
| Andira inermis (W. Wright) Kunth ex DC. | |||||
| Keetia hispida (Benth.) Bridson | |||||
| Uapaca togoensis Pax Combretum molle (R. Br. x. G. Don) | |||||
| Erythrina senegalensis DC. | |||||
| Piliostigma thonningii (Schum.) | |||||
| CI | Garcinia kola Heckel | EE | 0.00008–1.7 µg/mL | [142] | |
| CI | Eucalyptus globulus Labill. | ME | 16–32 mg/L | [144] | |
| ATCC 49619 | Salvia tom entosa Mill. | EO | 2.25 mg/mL | [161] | |
| CI | Thymus vulgaris L. Cinnamomum zeylanicum Garcin ex Blume | EO | 6.25 µL/mL | [107] | |
| Antibiotic resistant strains | Eucalyptus globulus Labill. | CAE | 0.7 mg/mL | [162] | |
| CI | Syzygium aromaticum (L.) Merr. & L.M. Perr | EO | 12.5 µL/mL | [107] | |
| ATCC 49619 | Euphorbia hirta L. | AE, EE, ME | 6–11 mm, 60–80 mg/mL | [163] | |
| Laggera tomentosa Sch-Bip | ME, AE | 1–2 mg/mL | [140] | ||
| Syzygeum guineense (Wild.) DC. | |||||
| Cordia africana Lam. | |||||
| Ferula communis L. | |||||
| Olea europea subsp. cuspidate | |||||
| S. agalactiae | NCIM 2401 | Ficus tsiela Roxb. | EE | 9.5 mm | [109] |
| NCIM 2401 | Hibiscus sabdariffa L. | AE | 9 mm | [109] | |
| HITM 80 | Quercus ilex L. | BE, EAE | 8–11 mm, 512 μg/mL | [106] | |
| CI |
Syzygium aromaticum (L.) Merr. & L.M. Perr Cinnamomum zeylanicum Garcin ex Blume |
EO | 12.5 µL/mL | [107] | |
| CI | Thymus vulgaris L. | EO | 6.25 µL/mL | [107] | |
| CI | Spathodea campanulata P. Beauv. | CAE, CME | 2–7 mm | [110] | |
| Tridax Procumbens L. | |||||
| Sechium edule (Jacq.) Sw. | EE | 15 mm | [108] |
Abbreviations: ACE; Acetone Extract, AE; Aqueous Extract, BE; Butanolic Extract, CAE; Crude Aqueous Extract, CDEE; Cold Ethanolic Extract, CE; Crude Extract, CHE; Chloroform Extract, CEE; Crude Ethanolic Extract, CI; Clinical Isolate, CME; Crude Methanolic Extract, DEE; diethyl ether extract, EAE; Ethyl Acetate Extract, EE; Ethanolic Extract, EM; Extraction Method, EO; Essential Oil, HAE; Hot Aqueous Extract, HE; Hexane Extract, HPLC; High Performance Liquid Chromatography, IZD; Inhibition Zone Diameter, ME; Methanolic Extract, MIC; Minimum Inhibitory Concentration, PE; Petroleum Extract, PEE; Petroleum Ether Extract, Ref.; References.
2. Anti-Streptococcal Attributes of Phytochemicals
Many fruits and plants have shown to possess anti-streptococcal effects (Table 3). Folklore medicinal plants have long been used for the treatment of S. pyogenes infections (Table 2) including pharyngitis. For example cashew plant (Anacardium occidentale), stickwort (Agrimonia eupatoria), mountain daisy (Arnica montana), bayberry (Myrica cerifera), soft leafed honeysuckle (Lonicera japonica), cuajilote (Parmentiera aculeate) or baobab (Adansonia digitata) [99,100,101,102,103,104], (Table 2). Particularly more attention has been given to anti-streptococcal effects of phytochemicals against S. mutans due to its cariogenic properties. A wide range of commercial and freshly prepared polyphenolic rich extracts (70% propanone) of various teas including green and black tea, lemon, cinnamon, hibiscus, peppermint, grape seed, sloe berry skin, cocoa, blackberry, pomegranate skin, blackcurrant, hawthorn berry skin, red and white wine was tested for their anti-streptococcal activity against oral streptococci (various strains of S. mutans, S. oralis, S. gordonii, S. salivarius, S. sanguis) [105]. All the tested products exhibited their minimum inhibitory effect at concentrations ranging 0.25–32 mg/mL against Streptococcus species [105]. Red grape seed propanone extract was most potent against S. mutans and Agro tea extract least effective with minimum inhibitory concentration of 0.5 mg/mL and 32 mg/mL respectively [105]. Phytochemicals, although very limited, also have been shown to hinder the growth of S. agalactiae [106,107,108,109,110,111,112]. Aqueous, ethanolic and chloroform extracts of bael, Indian gooseberry, moringa, neem, Chinese mahogany exert their minimum inhibitory effects at concentrations ranging from 0.15 mg/mL to 10 mg/mL against S. agalactiae, chloroform extract of Chinese mahogany being the most active one [111]. In a study by Nguelefack et al. ethyl acetate bark extract of Distemonanthus benthamianus at Minimum Bactericidal Concentration (MBC) of 4096 µg/mL was effective against S. agalactiae and its phytochemical profile was indicative of presence of flavonoids and phenolics and absence of sterols, triterpenes and alkaloids [113]. Moderate inhibitory effect of wild Asparagus racemosus ethanol extract at concentration of 500 μg/disc was also reported for S. agalactiae [114].
2.1. Phytochemicals with Inhibitory Activities against Adhesion, Plaque, and Biofilm Formation
Phytochemical-rich extracts and their associated pure compounds have repeatedly shown inhibitory effects against adhesion, plaque, and biofilm formation of streptococcal species (Table 4 and Table 5). High molecular weight non-dialysable materials extracted from cranberry juice (NDM) exhibit adhesion reduction activity in a dose-dependent manner at concentrations of 66–1330 µg/mL against S. sobrinus [115]. In another study, the ethanolic extract of Helichrysum italicum at concentrations of 15–31 µg/mL inhibited the sucrose-dependent adherence of S. mutans cells to a glass surface by 90% to 93% [116]. Cranberry juice powder (25%) at 500 μg/mL concentration inhibited the biofilm formations of S. sobrinus and S. sanguinis significantly [117]. In the same study, cranberry juice powder decreased the cell surface hydrophobicity of S. mutans and S. sobrinus 6715 by more than 40% [117].
Table 4.
Inhibitory effects of phytochemicals against adhesion, biofilm formation and hydrophobicity.
| Plant/Fruit Name | Bioactive Compounds and EM | Bacterial Strain | Concentration and Assay Type | Results | Ref. |
|---|---|---|---|---|---|
| Maidenhair tree (Ginkgo biloba L.) South African geranium (Pelargonium sidoides DC.) Cranberry (Vaccinium macrocarpon Aiton) |
Purified PAC, AE, AEE, ME | S. pyogenes DSM 2071 |
P. sidoides 40% G. biloba 100% Adhesion reduction at 3 h incubation time |
P. sidoides 40% G. biloba 25% |
[164] |
| Cranberry (Vaccinium macrocarpon Aiton) |
High MW non-dialyzable materials Juice powder 25% concentration, dissolved in water |
S. mutans MT 8148R, JC2, Ingbritt, ATCC 10449 S. criceti E49 S. oralis ATCC 10557 S. mitis ATCC 9811 S. gordonii Challis |
100–500 μg/mL Inhibition of biofilm formation |
Significant inhibition | [117] |
|
S. mutans MT 8148R, JC2, Ingbritt S. sobrinus 6715 |
Effect on hydrophobicity | 40%–60% reduction | |||
| Cocoa (Theobroma cacao L.) |
PP fractions Oligomers: Monomer MW 290 Dimer MW 578 Tetramer MW 1154 Pentamer MW 1442 HE |
S. mutans NCTC 10449 CI of S. sanguinis LDI1 |
35 μM Biofilm biomass reduction after 4 h |
In absence of sucrose S. sanguinis 48% S. mutans 68% |
[165] |
| In presence of sucrose S. sanguinis 79% S. mutans 44% |
|||||
| Cranberry (Vaccinium macrocarpon Aiton) |
High MW non-dialysable material, CJ |
S. sobrinus 6715 | 1.33 mg/mL Adhesion to glucan or fructan coated hydroxyapatite reduction |
95% | [115] |
| Red grape (Vitis vinifera L.) Pine bark | Red grape marc extract (GME): 20% PP, 3% A, Red wine extract (RWE): 95% PP Pine bark extract (PBE) Commercial preparation |
S. mutans ATCC 25175 | 2 mg/mL Adhesion to glass surface Inhibition |
GME significant inhibition, RWE, PBE effective at >4 mg/mL |
[166] |
| Blueberry (Vaccinium myrtillus L.) Small cranberry (Vaccinium oxycoccos L.) Lingonberry (Vaccinium vitis-idaea L.) Cloudberry (Rubus chamaemorus L.) Crowberry (Empetrum nigrum L.) Blackcurrant (Ribes nigrum L.) Sour cherry (Prunus cerasus L.) |
Molecular size of fractions; F1 <10 kDa, F2 10–100 kDa, F3 >100 kDa F2 and F3: polyphenol macromolecular complexes: PACs, polyhydroxy flavonoids AE, CJ |
CI of S. pneumoniae SB 53845 S. agalactiae B133 III R |
Binding activity of bacterial cells |
S. pneumonia bound to fraction FI of cranberry and bilberry juices S. agalactiae bound to bilberry juice and cranberry fractions FII and FIII and to all fractions of cranberry juice and lingonberry |
[112] |
| Clove (Syzygium aromaticum (L.) Merr. & L.M. Perr) |
CAE | S. mutans ATCC 25175 | 20 mg/mL Precent cell-surface hydrophobicity |
0.3% ± 0.1% | [167] |
| CAE | S. mutans ATCC 25175 | 20 mg/mL Adherence inhibition |
100% | ||
| CME | S. mutans ATCC 25175 | 20 mg/mL Percent cell-surface hydrophobicity reduction |
25.2% ± 4.7% | ||
| CME | S. mutans ATCC 25175 | 15 mg/mL Adherence inhibition |
100% | ||
| Cocoa (Theobroma cacao L.) |
Bean husk extract 12.6% PP compounds 30% EE |
S. mutans MT8148 | 1 mg/mL Adherence to saliva-coated hydroxyapatite inhibition |
31% | [168] |
| S. mutans MT8148 | 1 mg/mL Plaque formation inhibition |
Significantly inhibited | |||
| Guava (Psidium guajava L.) |
Quercetin-3-O-alpha-l-arabinopyranoside (guaijaverin) ME |
S. mutans MTCC1943 | 2 mg/mL Percent cell hydrophobicity |
20% | [169] |
| Cranberry (Vaccinium macrocarpon Aiton) |
PP fraction |
S. sobrinus 6715 S. sobrinus B13 S. mutans MT8148R S. mutans JC2 |
500 μg/mL Hydrophobicity reduction |
S. sobrinus 6715 90% S. sobrinus B13 85% S. mutans MT 8148R 90% S. mutans JC2 65% |
[170] |
| Devil’s horsewhip (Achyranthes aspera L.) |
AE, BE, ME, PEE | CI of S. mutans | 125 µg/mL Biofilm inhibition |
Complete to partial biofilm inhibition | [171] |
| Meswak (Salvadora persica L.) |
ACE, AE, CHE, EE, ME | CI of S. mutans | 2.6 mg/mL Biofilm inhibition |
significant inhibition | [172] |
| Indian gooseberry (Emblica Officinalis L.) |
CE, EF | S. mutans MTCC 497 | 39.04 µg/mL CE, 78.08 µg/mL ethanolic fraction Biofilm inhibition |
50% inhibition | [173] |
| 156 µg/mL CE and 312.5 µg/mL ethanolic fraction Adherence inhibition |
50% inhibition | ||||
| Hydrophobicity reduction | Partial reduction | ||||
| Papaya (Carica papaya L.) |
Fermented papaya preparation (FPP) Alkaloids Flavonoids Glucosides Anthraquinones |
S. mutans 25175 S. mitis 6249 |
50 mg/mL Percent hydrophobicity |
S. mutans: 1.01% S. mitis: 7.66% |
[174] |
| Curry (Helichrysum Italicum G. Don) |
Apigenin Luteolin Gnaphaliin Naringenin Pinocembrin Tiliroside EE |
S. mutans ATCC 35668 S. salivarius ATCC 13419 S. sanguis ATCC 10556 |
16–31 μg/mL Adherence to glass surface inhibition |
90%–93% | [116] |
| sub-MIC 8–31 μg/mL Cell-surface hydrophobicity reduction |
90% |
Abbreviations: A; Anthocyanin, ACE; Acetone Extract, AE; Aqueous Extract, AEE; Aqueous Ethanolic Extract, BE; Butanolic Extract, CAE; Crude Aqueous Extract, CE; Crude Extract, CHE; Chloroform Extract, CI; Clinical Isolate, CJ; Concentrated Juice, CME; Crude Methanolic Extract, EE; Ethanolic Extract, EF; Ethanolic Fractions, EM; Extraction Method, FPP; Fermented Papaya Preparation, GME; Red Grape Marc Extract, HE; Hexane Extract, kDA; Kilodalton, ME; Methanolic Extract, MW; Molecular Weight, PAC; Proanthocyanidin, PBE; Pine Bark Extract, PEE; Petroleum Ether Extract, PP; Polyphenol, Ref.; References, RWE; Red Wine Extract.
Table 5.
Inhibitory effects of pure phytochemicals against adhesion, biofilm formation, quorum sensing and hydrophobicity.
| Bioactive Compounds | Bacterial Strain | Concentration and Assay Type | Results | Ref. |
|---|---|---|---|---|
| (−)-Epicatechin (−)-epicatechin-3-O-gallate (−)-epigallocatechin (−)-epigallocatechin-3-O-gallate |
S. pyogenes DSM 2071 | 30 μg/mL Adhesion reduction to HEp-2 cells |
(−)-epigallocatechin 15% (−)-epigallocatechin-3-O-gallate 40% |
[164] |
| Morin | S. pyogenes MGAS 6180 | 225 μM Biofilm biomass reduction |
50%–60% | [175] |
| Ursolic acid (UA) Oleanolic acid (OA) |
S. mutans UA159 Actinomyces viscosus ATCC 15987 |
1024 μg/mL Adherence inhibition to tooth surface |
Complete inhibition | [176] |
| EGCG | ComC-deficient S. mutans | 0.25 mg/mL Biofilm inhibition |
81% Biofilm inhibition | [177] |
| QS inhibition | Partial inhibition |
Abbreviations: ComC; competence factor, EGCG; Epigallocatechingallate, HEp-2; Human Epithelial Type 2 (Hep-2) Cells, OA; Oleanolic Acid, QS; Quorum Sensing, Ref.; References, UA; Ursolic Acid.
In a different study, anti-adhesion, biofilm inhibition and eradication activity of the two-terpenoids, ursolic acid (UA) and oleanolic acid (OA), were examined. UA and OA showed a Minimum Inhibitory Concentration (MIC) of 256 µg/mL and 1024 µg/mL against S. mutans UA159, respectively [176]. The Minimum Bactericidal Concentration (MBC) for UA and OA against the same bacterium were 256 µg/mL and >1024 µg/mL correspondingly [176]. Microtiter plate biofilm assay showed that sub-MIC dose of the compounds inhibited the biofilm formation [176]. Gallic acid at 1–4 mg/mL concentration inhibited up to 70% of S. mutans biofilm establishment [178]. Gallic acid, quercetin, and tannic acid all produced significant biofilm inhibition attributes against S. mutans however gallic acid was most potent [179]. Methyl gallate at concentrations of 1–4 mg/mL rendered biofilm formation of S. mutans to up to 80% [178]. Green and oolong tea contain substantial quantities of gallic acid and epigallocatechin gallate and have exhibited slight inhibition effect on the attachment of S. mutans and other oral bacterial to collagen, tooth surfaces and gingival cell line [180]. In the same study, fermented tea with high tannin content opposed to green tea and oolong tea had shown more activity towards attachment of S. mutans and other oral bacterial to collagen, tooth surfaces and gingival cell line [180].
Adhesion of S. mutans to the tooth surface was hindered after treatment with UA at 256 µg/mL [176]. Sub-MIC dose of UA also affected the adhesion consequently hindering the biofilm formation [176]. UA moreover eradicated the biofilm cells at concentrations of 500–2000 µg/mL [176]. Polyphenolics-rich tea extract at concentrations as low as 1–4 mg/mL prevented the attachment of S. mutans to collagen coated hydroxyapatite beads [181].
In another study, the effect of cocoa polyphenol fractions on S. mutans biofilm reduction in the absence and presence of sucrose were measured. At 35 μM concentration and after 4 h, biofilm mass was reduced to 68% in the absence of sucrose and to 44% in the presence of sucrose [165]. Biofilm of S. mutans on saliva coated hydroxyapatite surface was preformed and then treated (60 s) with purified proanthocyanidin (PAC)-containing fraction of cranberry (various degree of polymerization) [182]. At concentrations of 100 µM (single or combined fractions in 1:1 ratio), confocal 3D images show distorted architecture and deficient biofilm accumulation suggestive of reduced biomass and thickness of adherent bacteria and EPS [182]. Expressions of 119 genes of S. mutans within biofilm were altered post exposure to PAC-rich fractions of cranberry [182]. The expression of genes particularly related to adhesion, acid stress tolerance, glycolysis and other cellular activities during biofilm development were downregulated [182]. Structure activity relationship analysis revealed that PAC oligomers with more than eight epicatechin units exhibit higher anti-adhesion effects up to 85% against S. mutans however the increase in potency is not proportional [182]. This not only is associated with degree of polymerization but may also be associated with number and location of A-type linkages in the oligomers, and type of interflavan bonds [182].
The anti-adhesive properties of root extract of Pelargonium sidoides have been studied against S. pyogenes attachment to human epithelial type 2 (HEp-2) cells [164]. Results have shown that after pre-treatment of S. pyogenes with methanol insoluble and methanol soluble fractions of the extracts of Pelargonium sidoides at concentrations of 30 µg/mL, adhesion of the pathogen to HEp-2 cells was inhibited up to 30% to 35% [183]. To characterize the anti-adhesive constituents of these fractions, comparative chemical studies were performed. The study revealed that the proanthocyanidins content of the fraction was of prodelphinidin nature, and inhibition of the adhesion was in a specific rather than non-specific manner [164,183]. Successful inhibition of adhesion and hydrophobic interactions could reduce and or prevent sore throat caused by S. pyogenes [164]. It has been suggested that polymeric flavonoids or other large molecule polyphenols may exhibit higher anti-adhesion effects against streptococci [180]. Coffee high molecular weight fraction nearly completely (91%) hindered the adhesion of S. mutans [184].
Similarly, a study on the binding activity of S. pneumoniae and S. agalactiae to different molecular size fractions (F1, F2, F3) of Vaccinium family polyphenols found that binding was highest to wild cranberry (Vaccinium oxycoccos) [112]. S. pneumoniae cells bound mostly to cranberry juice low-molecular size fraction (F1) and S. agalactiae cells to high-molecular size fraction (F3) [112]. S. pneumoniae bound to F1 of bilberry and cranberry juices and S. agalactiae attached most actively to F2 and F3 of berry and juice preparations belonging to Vaccinium species [112]. Phytochemical analysis has shown that F2 and F3 fractions contain polyphenol macromolecular complexes, including proanthocyanidins and polyhydroxy flavonoids [112]. At sub-MIC level of 2 mg/mL red grape marc extract, composed of 20% polyphenols and 3% anthocyanin, inhibited the adherence of S. mutans and Fusobacterium nucleatum cells to glass surface [166]. Morin, a flavonol, reduced biofilm biomass of S. pyogenes at concentrations exceeding 225 μM up to 65% [175]. Epigallocatechin gallate (EGCG) of Camellia sinensis has various physiological effects on S. mutans UA159 (Figure 1) and has been proven to inhibit the enzymatic activity of glucosyltransferases, F1F0-ATPase, lactate dehydrogenase, biofilm formation and growth [153].
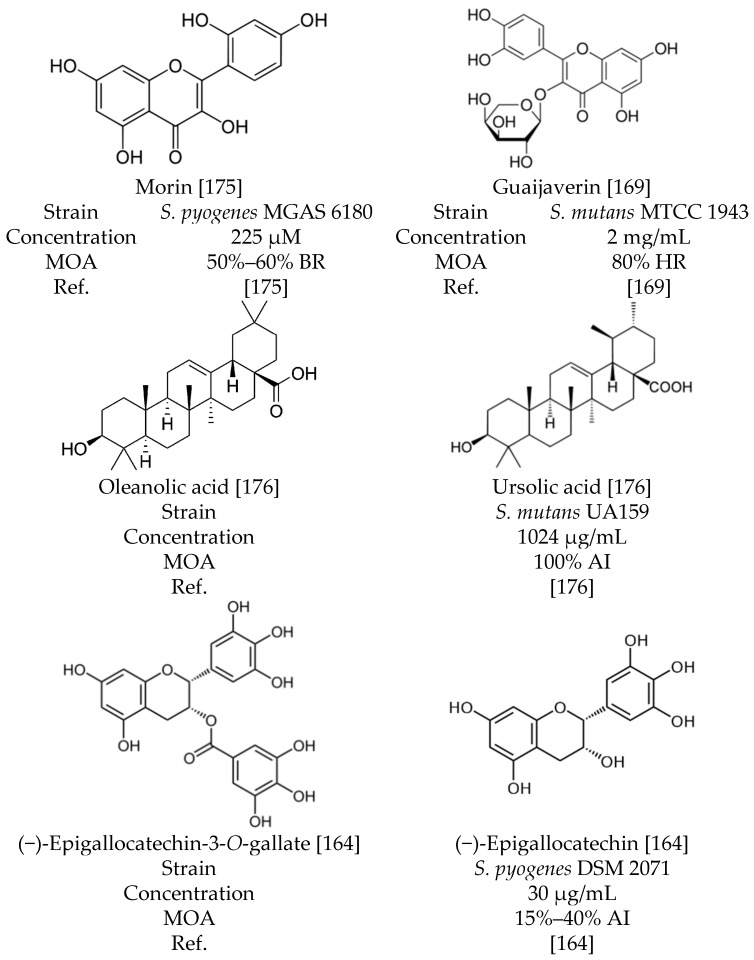
Figure 1.
Chemical structure of polyphenols with inhibition activity against adherence, biofilm biomass and hydrophobicity. Abbreviations: AI; Adherence Inhibition, BR; Biofilm Biomass Reduction, HR; Hydrophobicity Reduction, MOA; Mode of Action, Ref.; References.
2.2. Phytochemicals with Inhibitory Activities against F-ATPase and Glycolytic pH-drop
Phytochemical-rich extracts not only possess anti-adhesion, anti-plaque and anti-biofilm attributes, but also have demonstrated inhibitory effects on streptococcal species F-ATPase and glycolytic pH-drop activities (Table 6, Figure 2). Plants and fruits have been studied for their anti-streptococcal effects and fruits such as cranberry (V. macrocarpon), cocoa (Theobroma cacao), babchi (Psoralea corylifolia), mangosteen (Garcinia mangostana) and grape (Vitis vinifera) have shown inhibitory effects on F0-ATPase and F1-ATPase, glucosyltransferases (GTFB and GTFC) and acid production activities of S. mutans [80,84,165,185]. The lack of inhibitory activity of monophenolic compounds suggest that the inhibition of F1–F0-ATPase by phenolics require two or more phenolic structures [186]. The flavones have also been shown to interact with other ATPases, such as Ca2+-ATPase [187] and Na+/K+-ATPase [188], in addition to their inhibitory effects on F1–F0-ATPase [189]. Glycolysis of S. mutans is inhibited by α-mangostin leading to indirect inhibition of respiration by α-mangostin [190]. Glucan production by GTFs and F-ATPase is inhibited by α-mangostin suggesting that S. mutants can be eliminated selectively [190].
Table 6.
Inhibitory effects of phytochemicals on F-ATPase activity and glycolytic pH-drop.
| Plant | Bioactive Compounds and EM | Bacterial Strain | Concentration and Assay Type | Results | Ref. |
|---|---|---|---|---|---|
| Cranberry (Vaccinium macrocarpon Aiton) |
FLAV A PAC |
S. mutans UA159 | PAC 500 µg/mL FLAV 125 µg/mL A 200 µg/mL F-ATPase activity inhibition |
PAC alone or in combinations >85% FLAV 20% |
[84] |
| 500 µg/mL Glycolytic pH-drop |
PAC alone or in combinations pH 4.7–4.9 |
||||
| Cranberry (Vaccinium macrocarpon Aiton) | Low MW PP | S. mutans UA159 | 500 µg/mL F-ATPase activity inhibition |
Myricetin 32% procyanidin A2 29% Myricetin + procyanidin A2 43% |
[191] |
| Glycolytic pH-drop | Significant disruption | ||||
| Cocoa (Theobroma cacao L.) | Oligomers: Monomer MW 290 Dimer MW 578 Tetramer MW 1154 Pentamer MW 1442 HE of PP fractions |
S. mutans NCTC 10449 S. sanguinis LDI 1, CI |
500 µM pentamer Glycolytic pH-drop |
30% | [165] |
| Red wine grape (Vitis vinifera L.) |
Gallic acid Catechin Epicatechin Procyanidin B1 Procyanidin B2 Resveratrol Fermented |
S. mutans UA159 | 125 µg/mL F-ATPase activity inhibition |
30%–65% | [195] |
| 500 μg/mL Glycolytic pH-drop | Significant inhibition | ||||
| Green tea Camellia sinensis (L.) Kuntze | EGCG EE |
S. mutans UA159 | 15.6 μg/mL Glycolytic pH-drop |
Significant inhibition | [153] |
| Methuselah’s beard (Usnea longissima Ach.) |
Herbo-metallic preparations | S. mutans | 5%–15% Glycolytic enzymes inhibition (GEI) |
Decreased ATPase, enolase, lactate dehydrogenase, protease, glucosidase, EPS and acid production activity |
[196] |
| Purple mangosteen (Garcinia mangostana L.) |
α-mangostin EE |
S. mutans UA159 S. rattus FA-1 S. salivarius ATCC 13419 |
GEI | IC50
31 µM Lactic dehydrogenase, 45 µM Aldolase, 95 µM Glyceraldehyde-3-phosphate dehydrogenase inhibition |
[190] |
Abbreviations: A; Anthocyanin, EE; Ethanolic Extract, EGCG; Epigallocatechingallate, EM; Extraction Method, EPS; Exopolysaccharide, FLAV; Flavonol, F-ATPase; F-Adenosine triphosphatase, GEI; Glycolytic Enzymes Inhibition, HE; Hexane Extract, IC50; Inhibition Concentration 50%, MW; Molecular Weight, PAC; Proanthocyanidin, PP; Polyphenol, Ref.; References.
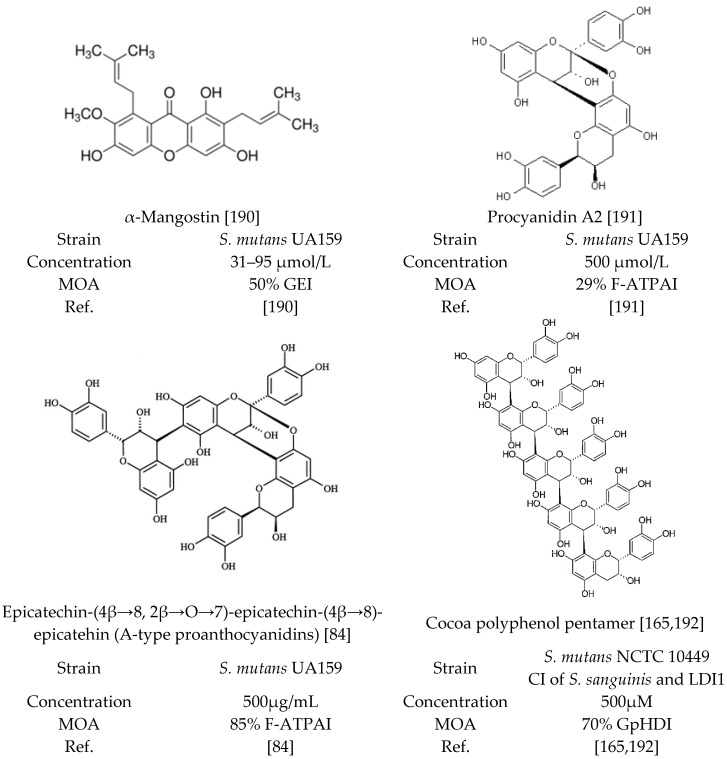
Figure 2.
Chemical structure of polyphenols with inhibition activity against F-ATPase, glycolytic enzymes and glycolytic pH-drop. Abbreviations: CI; Clinical Isolate, F-ATPAI; F-ATPase Activity Inhibition, GEI; Glycolytic Enzymes Inhibition, GpHDI; Glycolytic pH-Drop Inhibition, MOA; Mode of Action, Ref.; References.
Analysis of low molecular weight cranberry polyphenols against glucosyltransferases, acid production and F-ATPase activity of S. mutans UA159 has suggested that compounds like phenolic acids have no inhibitory effect on these virulence factors [84]. Quercetin, quercetin-3-O-glucoside, quercetin-3-O-galactoside, quercetin-3-O-arabinofuranoside, quercetin-3-O-rhamnoside, myricetin, PAC-monomer, PAC-dimer, and procyanidin A2, at the concentrations of 500 µM inhibited the enzymatic activity of the proton-translocating F-ATPase to some degree [191]. Myricetin, procyanidin A2 and the combination of the two were most effective inhibitors with 32%, 29% and 43% inhibition against F-ATPase activity, respectively [192]. The flavonoids, particularly myricetin, procyanidin A2 and the combination of the two significantly interrupted the glycolytic pH-drop by S. mutans cells; however, epicatechin, myricetin-3-O-rhamnoside, caffeic acid, chlorogenic acid had no effect [191]. In presence of cocoa polyphenol pentamer, the terminal pH is increased to 4.67 ± 0.09 within 20 min while in untreated pH was as low as 4.50 ± 0.08 (S. mutans converts sucrose to acid and lowers the pH) [165]. These results suggest that 500 µM cocoa polyphenol pentamer reduced the rate of acid production, at pH 7.0, by 30% [165].
2.3. Phytochemicals with Inhibitory Activities against Glucosyltransferases, Aggregation, and Quorum Sensing
Moreover, phytochemicals-rich extracts have been reported for their inhibitory properties against glucosyltransferases, aggregation, and quorum sensing attributes of streptococcal species (Table 7). Low molecular weight polyphenols of cranberry reduced the glucan synthesis of S. mutans cells by GTFB and GTFC [191]. At 500 µM, the inhibition activities of the tested polyphenols varied from 15%–45% (epicatechin 15%, myricetin-3-O-rhamnoside 20%, procyanidin A2 30%, quercetin-3-O-arabinofuranoside 35% and quercetin-3-O-arabinofuranoside in combination with procyanidin A2 45%) [191]. It is notable that theaflavin of green tea at 10 mM inhibited the GTF activities of S. mutans significantly [193].
Table 7.
Inhibitory effects of phytochemicals on glucosyltransferases, aggregation and quorum sensing.
| Plant/Fruit Name | Bioactive Compounds and EM | Bacterial Strain | Concentration and Assay Type | Results | Ref. |
|---|---|---|---|---|---|
| Whortleberry or Bilberry (Vaccinium myrtillus L.) |
Molecular size of fractions; F1 <10 kDa, F2 10–100 kDa, F3 >100 kDa CJ |
CI of S. mutans IH 113728 A. naeslundii AHP 28639, AHP 28651 F. nucleatum AHN 23952, AHN 23937 |
48 mg/g of SS Inhibition of aggregation and reversal activity | F2 of bilberry juice 100% | [194] |
| Neem (Azadirachta indica A. Juss.) |
AE |
S. sobrinus ATCC 27607 S. mutans ATCC 25175 S. cricetus ATCC 19642 S. sanguis H7PR3 |
250 µg/mL Bacterial aggregation |
Microscopically observable bacterial aggregation |
[197] |
| Red Wine Grape (Vitis Vinifera L.), and its pomace |
Gallic acid Catechin Epicatechin Procyanidin B1 Procyanidin B2 Resveratrol |
S. mutans UA159 | 62.5 µg/mL Inhibition of GTF B and C activities |
70%–85% | [195] |
| Green tea and black tea (Camellia sinensis (L.) Kuntze), and polyphenol mixtures |
Theaflavin: its mono- and digallates (+)-catechin (−)-epicatechin and their enantiomers Epigallocatechin (−)-gallocatechin HAE |
S. mutans OMZ 176 | Theaflavin 1–10 mM Inhibition of GTF activities |
significant inhibition | [193] |
| Leaves of Oolong tea (Camellia sinensis (L.) Kuntze) |
Oolong tea polyphenol OTF6 (polymeric polyphenol) EE |
S. mutans MT8148R | 60–850 µg/mL rGTFs (rGTFB, rGTFD, rGTFC) synthesis inhibition |
50% | [197] |
| Rock cinquefoil (Drymocallis rupestris (L.) Sojak) |
PRU2 PRU TAC 155 mg/g TPC 4.6 mg/g TFC 10.2 mg/g |
S. mutans CAPM 6067 S. sobrinus CAPM 6070, DSM 20381, downei CCUG 21020 S. sanguis ATCC 10556 |
0.75–1.5 mg/mL PRU and PRU2 Inhibition of GTF activities |
60% | [198] |
| Apple (Malus domestica Borkh.) |
Apple condensed tannins (ACT) Apple PP and apple juice |
S. mutans MT 8148 (serotype C) S. sobrinus 6715 (serotype G) |
1.5–5 μg/mL ACT Inhibition of GTF activities |
50% | [80] |
| Hop (Humulus lupulus L.) | High MW PP 36,000–40,000 AEE |
S. mutans MT 8148 (serotype C) S. sobrinus ATCC 33478 (serotype G) |
0.1% Inhibition of GTF activities | significant effect | [199] |
| Cranberry (Vaccinium macrocarpon Aiton) |
FLAV A PAC |
S. mutans UA159 | PAC; 500 µg/mL FLAV; 125 µg/mL A; 200 µg/mL Inhibition of GTF B and C activities |
FLAV, PAC or in combination 30%–60% |
[84] |
| Cranberry (Vaccinium macrocarpon Aiton) |
High MW non-dialysable material (NDM) CJ |
S. sobrinus 6715 | 2 mg/mL Inhibition of GTF, FTF activities, 1 h incubation |
GTF 20% FTF 40% |
[115] |
| Cranberry (Vaccinium macrocarpon Aiton) |
Low MW PP | S. mutans UA 159 | 500 µM/L Reduction of glucan synthesis by GTFB, GTFC |
Quercetin-3-arabinofuranoside + procyanidin A2 45% | [191] |
| Beard lichen (Usnea longissima Ach.) |
Herbo-metallic preparations | S. mutans | 5%–15% Inhibition of violacein production |
Partial QS inhibition | [196] |
| Indian gooseberry (Emblica Officinalis L.) |
Crude and EF | S. mutans MTCC 497 | QS inhibition (suppression of comDE), glucan synthesis reduction | [173] | |
| Marupá (Eleutherine americana Merr.) Rose myrtle (Rhodomyrtus tomentosa (Aiton) Hassk. |
CE of different extractive solvents | CI of S. pyogenes and NPRC109 | 250 mg/mL QS inhibition | Partial to strong inhibition; R. tomentosa |
[90] |
Abbreviations: A; Anthocyanin, ACT; Apple condensed tannins, AE; Aqueous Extract, AEE; Aqueous Ethanolic Extract, CE; Crude Extract, CEE; Crude Ethanolic Extract, CI; Clinical Isolate, CJ; Concentrated Juice, comDE; two-component signal transduction system, EE; Ethanolic Extract, EF; Ethanolic Fractions, EM; Extraction Method, FLAV; Flavonol, FTF; Fructosyltransferase, GTF; Glucosyltransferases, HAE; Hot Aqueous Extract, KDa; Kilodalton, MW; Molecular Weight, NDM; High Molecular Weight Non-Dialysable Materials Extracted From Cranberry Juice, PAC; Proanthocyanidin, PP; Polyphenol, PRU; Aqueous Extract Sub-Fraction, PRU2; Diethyl Ether Sub-Fraction, QS; Quorum Sensing, Ref.; References, SS; Solid Soluble, TFC; Total Flavonoid Content, TPC; Total Proanthocyanidins Content, TTC; Total Tannin Content.
The effects of fractions (F1, F2, and F3) of juice concentrates of bilberry (Vaccinium myrtillus), lingonberry (Vaccinium vitis-idaea), cloudberry (Rubus chamaemorus), crowberry (Empetrum nigrum and hermaphroditum), apple (Malus domestica), and blackcurrant (Ribes nigrum) on anti-coaggregation and anti-aggregation activities of dental plaque bacteria have been tested [194]. Test has been done on the pairs of S. mutans IH 113728 with the two strains of Actinomyces naeslundii (AHP 28639 and AHP 28651) and S. mutans IH 113728 with the two strains of Fusobacterium nucleatum (AHN 23952 and AHN 23937) [194]. The anti-aggregation and anti-coaggregation activity was found in F2 and F3 of bilberry, blackcurrant, and crowberry and lingonberry juices [194]. Also, F2 and F3 of crowberry at 48 mg/g of Solid Solubles (SS) showed anti-co-aggregation against some of the pairs at 91% and 86%, respectively [194]. The anti-aggregation activity was detected in all bacterial pairs with fraction F2 of bilberry, crowberry and lingonberry juices [194]. The anti-aggregation was mainly achieved with a berry concentration of 48 mg/g of SS [194]. Analysis of composition of the juice fractions showed that F2 and F3 were composed of macromolecular polyphenol complexes, PAC, polyhydroxy flavonoids [194]. Absolute co-aggregation inhibition and anti-aggregation activity were achieved with the F2 of bilberry juice at the concentration of 48 mg/g of SS [194].
Crude extract of Eleutherine americana at 250 mg/mL inhibited the quorum-sensing of a clinical isolate of S. pyogenes, partially, while at the same concentration Rhodomyrtus tomentosa had a stronger inhibition activity [90]. Betulin, oleanane-3,12-dione, benzyl (6Z,9Z,12Z)-6,9,12-octadecatrienoate, and 3-benzyloxy-1-nitrobutan-2-ol possess great anti-quorum sensing inhibition activities (Figure 3A,B). Few bioactives compounds of A. aspera have shown to effectively interact with quorum sensing response regulators of S. mutans thus preventing expression of virulence elements [171]. Molecular docking revealed that A. aspera bioactive compounds, 3,12-oleandione and betulin, could inhibit quorum sensing by interacting with S. mutans OmpR subfamily QS regulatory DNA-binding response regulator and S. mutans glycosyltransferase (EPS synthesizing enzyme), respectively [171]. Al-Sohaibani et al. performed similar analysis on the bioactive compounds of Salvadora persica methanolic extract [172]. Results suggest that benzyl (6Z,9Z,12Z)-6,9,12-octadecatrienoate and 3-benzyloxy-1-nitrobutan-2-ol (Figure 3C,D) are capable of interacting with S. mutans OmpR subfamily QS regulatory DNA-binding response regulator thus hindering biofilm formation by this or similar quorum sensing pathway [172].
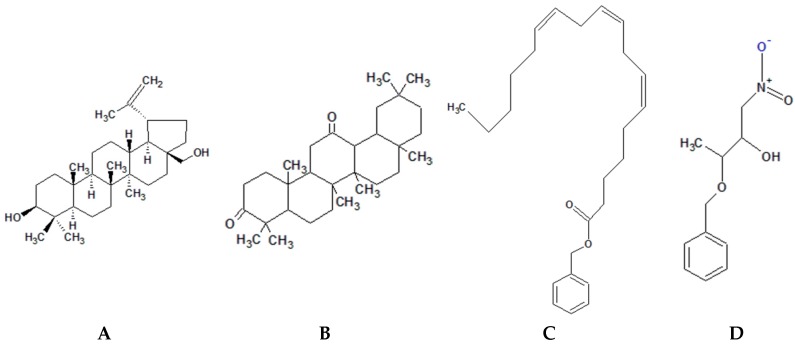
Figure 3.
Chemical structure of phytochemicals with S. mutans quorum sensing inhibition activity. (A): Betulin; (B): Oleanane-3,12-dione; (C): Benzyl (6Z,9Z,12Z)-6,9,12-octadecatrienoate; (D): 3-Benzyloxy-1-nitrobutan-2-ol.
3. Conclusions and Prospects
Each class of classical antibacterial agents (antibiotics) usually targets different sites and processes of pathogenic bacteria. Major antimicrobial actions include disruption of membrane structure, inhibition of protein synthesis, and inhibition of production of folate coenzymes, nucleic acids, and peptidoglycans. Natural antimicrobials like their synthetic counterparts (antibiotics) target different molecules and processes to inhibit the colonization and viability of the bacteria or to inactivate bacterial toxins and or modulate the molecules and processes pre-requisite for bacteria’s metabolic pathways or reduce the rate of protein synthesis. It is worth noting that natural antimicrobial products not necessarily have to be bactericidal to suppress such processes and activities. It is plausible that a compound is likely to be efficient bacterial growth inhibitor if it can deteriorate the cytoplasmic pH, increase the permeability of plasma membrane, prevent extracellular and intracellular microbial enzyme production, interrupt bacterial metabolic pathways, or disrupt plaque and biofilm formation. As observed, there is considerable amount of scientific evidence that phytochemicals exert significant multiple anti-streptococcal effects and apart from their bactericidal effects, their main bacteriostatic strategy is the anti-adhesiveness attribute.
The efficacy of natural products as antimicrobials with fewer or no side effects is likely to depend on the structure of the compound that interacts with the toxin or pathogen and not with molecules of the host meaning that their effect is specific. This approach has become the rationale for natural drug design studies as a new field of research. Attempts have been made to understand certain features relating to phytochemical structure and the associated antibacterial activity. High molecular weight and complex phytochemicals exert greater inhibitory effects such as pentamer polyphenolic fraction of cocoa, high molecular weight non-dialyzable material of cranberry and F2 or F3 fractions of crowberry and bilberry. The side effects of the current antimicrobials and the spread of drug-resistant microorganisms have become a significant concern and a threat to successful therapy of microbial diseases. Therefore, there is an urgent demand for the discovery of safe natural compounds with diverse chemical structures and mechanisms of action satisfying both the consumer and the healthcare providers as potential useful therapeutic tools of the post-antibiotic era. Intensive research on such plants could lead to the incorporation of the most potent chemically defined extracts into nutraceuticals or natural health products and becoming a solution to this global concern of evolution of drug-resistant microorganisms.
Acknowledgments
We would like to acknowledge the funds received through Nova Scotia Graduate Scholarship (SA) and Canada Research Chair Program (HPVR).
Author Contributions
All the authors contributed to the designing, writing, and editing of this review article.
Conflicts of Interest
The authors declare no conflict of interest
References
- 1.Toit M.D., Huch M., Cho G.S., Franz C.M. The family streptococcaceae. In: Holzapfel W.H., Wood B.J.B., editors. Lactic Acid Bacteria: Biodiversity and Taxonomy. 1st ed. John Wiley & Sons, Ltd.; New York, NY, USA: 2014. pp. 445–446. [Google Scholar]
- 2.Shi E. Personal communication. University of California; Davis, CA, USA: 2009. Flesh-Eating Bacteria: Various Strains and Virulence; pp. 1–8. [Google Scholar]
- 3.Hayes C.S., Williamson H., Jr. Management of group a beta-hemolytic streptococcal pharyngitis. Am. Fam. Phys. 2001;63:1557–1565. [PubMed] [Google Scholar]
- 4.Baron S., Davis C.P. Normal flora. In: Baron S., editor. Medical Microbiology. 4th ed. University of Texas Medical Branch; Galveston, TX, USA: 1996. [PubMed] [Google Scholar]
- 5.Mitchell T.J. The pathogenesis of streptococcal infections: From tooth decay to meningitis. Nat. Rev. Microbiol. 2003;1:219–230. doi: 10.1038/nrmicro771. [DOI] [PubMed] [Google Scholar]
- 6.Nobbs A.H., Lamont R.J., Jenkinson H.F. Streptococcus adherence and colonization. Microbiol. Mol. Biol. Rev. 2009;73:407–450. doi: 10.1128/MMBR.00014-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Patterson M.J. Streptococcus. In: Baron S., editor. Medical Microbiology. 4th ed. University of Texas Medical Branch; Galveston, TX, USA: 1996. [PubMed] [Google Scholar]
- 8.Facklam R.F., Martin D.R., Marguerite L., Dwight R.J., Efstratiou A., Thompson T.A., Gowan S., Kriz P., Tyrrell G.J., Kaplan E. Extension of the lancefield classification for group a streptococci by addition of 22 new m protein gene sequence types from clinical isolates: Emm103 to emm124. Clin. Infect. Dis. 2002;34:28–38. doi: 10.1086/324621. [DOI] [PubMed] [Google Scholar]
- 9.Public Health Agency of Canada. [(accessed on 29 January 2015)]. Available online: http://www.Phac-aspc.Gc.Ca/lab-bio/res/psds-ftss/streptococcus-agalactiae-eng.Php#footnote2.
- 10.Zapun A., Vernet T., Pinho M.G. The different shapes of cocci. FEMS Microbiol. Rev. 2008;32:345–360. doi: 10.1111/j.1574-6976.2007.00098.x. [DOI] [PubMed] [Google Scholar]
- 11.Petersen P.E., Bourgeois D., Ogawa H., Estupinan-Day S., Ndiaye C. The global burden of oral diseases and risks to oral health. Bull. World Health Organ. 2005;83:661–669. [PMC free article] [PubMed] [Google Scholar]
- 12.Matsui R., Cvitkovitch D. Acid tolerance mechanisms utilized by Streptococcus mutans. Future Microbiol. 2010;5:403–417. doi: 10.2217/fmb.09.129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stevens D.L. Streptococcal toxic-shock syndrome: Spectrum of disease, pathogenesis, and new concepts in treatment. Emerg. Infect. Dis. 1995;1:69–78. doi: 10.3201/eid0103.950301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Carapetis J.R., Steer A.C., Mulholland E.K., Weber M. The global burden of group a streptococcal diseases. Lancet Infect. Dis. 2005;5:685–694. doi: 10.1016/S1473-3099(05)70267-X. [DOI] [PubMed] [Google Scholar]
- 15.Torralba K.D., Quismorio F.P. Soft tissue infections. Rheum. Dis. Clin. N. Am. 2009;35:45–62. doi: 10.1016/j.rdc.2009.03.002. [DOI] [PubMed] [Google Scholar]
- 16.Guarner J., Sumner J., Paddock C.D., Shieh W.-J., Greer P.W., Reagan S., Fischer M., van Beneden C.A., Zaki S.R. Diagnosis of invasive group a streptococcal infections by using immunohistochemical and molecular assays. Am. J. Clin. Pathol. 2006;126:148–155. doi: 10.1309/KHGVR72CBRM4FQ58. [DOI] [PubMed] [Google Scholar]
- 17.Sherris J.C., Ray C.G. An Introduction to Infectious Diseases. In: Sherris J.C., editor. Medical Microbiology. 2nd ed. Elsevier Science Publishing Co.; New York, NY, USA: 1990. pp. 149–169. [Google Scholar]
- 18.Public Health Agency of Canada. [(accessed on 29 January 2015)]. Available online: http://www.Phac-aspc.Gc.Ca/lab-bio/res/psds-ftss/streptococcus-agalactiae-eng.Php.
- 19.Kothari N.J., Morin C.A., Glennen A., Jackson D., Harper J., Schrag S.J., Lynfield R. Invasive group b streptococcal disease in the elderly, Minnesota, USA, 2003–2007. Emerg. Infect. Dis. 2009;15:1279–1281. doi: 10.3201/eid1508.081381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.WHO Pneumococcal conjugate vaccine for childhood immunization. Wkly. Epidemiol. Rec. 2007;82:93–104. [PubMed] [Google Scholar]
- 21.O’Brien K.L., Wolfson L.J., Watt J.P., Henkle E., Deloria-Knoll M., McCall N., Lee E., Mulholland K., Levine O.S., Cherian T. Burden of disease caused by Streptococcus pneumoniae in children younger than 5 years: Global estimates. Lancet. 2009;374:893–902. doi: 10.1016/S0140-6736(09)61204-6. [DOI] [PubMed] [Google Scholar]
- 22.Martens P., Worm S.W., Lundgren B., Konradsen H.B., Benfield T. Serotype-specific mortality from invasive Streptococcus pneumoniae disease revisited. BMC Infect. Dis. 2004;4:21. doi: 10.1186/1471-2334-4-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Huang S.S., Johnson K.M., Ray G.T., Wroe P., Lieu T.A., Moore M.R., Zell E.R., Linder J.A., Grijalva C.G., Metlay J.P. Healthcare utilization and cost of pneumococcal disease in the united states. Vaccine. 2011;29:3398–3412. doi: 10.1016/j.vaccine.2011.02.088. [DOI] [PubMed] [Google Scholar]
- 24.Bisno A., Brito M., Collins C. Molecular basis of group a streptococcal virulence. Lancet Infect. Dis. 2003;3:191–200. doi: 10.1016/S1473-3099(03)00576-0. [DOI] [PubMed] [Google Scholar]
- 25.Cunningham M.W. Pathogenesis of group a streptococcal infections. Clin. Microbiol. Rev. 2000;13:470–511. doi: 10.1128/CMR.13.3.470-511.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ferretti J.J., McShan W.M., Ajdic D., Savic D.J., Savic G., Lyon K., Primeaux C., Sezate S., Suvorov A.N., Kenton S. Complete genome sequence of an M1 strain of Streptococcus pyogenes. Proc. Natl. Acad. Sci. USA. 2001;98:4658–4663. doi: 10.1073/pnas.071559398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Frieden T. Antibiotic Resistance Threats in the United States. Centers for Disease Control and Prevention; Atlanta, GA, USA: 2013. pp. 11–93. [Google Scholar]
- 28.Dajani A., Taubert K., Ferrieri P., Peter G., Shulman S. Treatment of acute streptococcal pharyngitis and prevention of rheumatic fever: A statement for health professionals. Pediatrics. 1995;96:758–764. [PubMed] [Google Scholar]
- 29.Kreikemeyer B., McIver K.S., Podbielski A. Virulence factor regulation and regulatory networks in Streptococcus pyogenes and their impact on pathogen–host interactions. Trends Microbiol. 2003;11:224–232. doi: 10.1016/S0966-842X(03)00098-2. [DOI] [PubMed] [Google Scholar]
- 30.Nizet V., Rubens C.E. Gram-Positive Pathogens. ASM Press; Washington, DC, USA: 2000. Pathogenic mechanisms and virulence factors of group b streptococci; pp. 125–136. [Google Scholar]
- 31.Jedrzejas M.J. Pneumococcal virulence factors: Structure and function. Microbiol. Mol. Biol. Rev. 2001;65:187–207. doi: 10.1128/MMBR.65.2.187-207.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schrag S.J., Zywicki S., Farley M.M., Reingold A.L., Harrison L.H., Lefkowitz L.B., Hadler J.L., Danila R., Cieslak P.R., Schuchat A. Group b streptococcal disease in the era of intrapartum antibiotic prophylaxis. N. Engl. J. Med. 2000;342:15–20. doi: 10.1056/NEJM200001063420103. [DOI] [PubMed] [Google Scholar]
- 33.Aljicevic M., Karcic E., Bektas S., Karcic B. Representation of Streptococcus pneumoniae in outpatient population of sarajevo canton. Med. Arch. 2015;69:177–180. doi: 10.5455/medarh.2015.69.177-180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Moscoso M., García E., López R. Biofilm formation by Streptococcus pneumoniae: Role of choline, extracellular DNA, and capsular polysaccharide in microbial accretion. J. Bacteriol. 2006;188:7785–7795. doi: 10.1128/JB.00673-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hasty D., Ofek I., Courtney H., Doyle R. Multiple adhesins of streptococci. Infect. Immun. 1992;60:2147–2152. doi: 10.1128/iai.60.6.2147-2152.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hall-Stoodley L., Costerton J.W., Stoodley P. Bacterial biofilms: From the natural environment to infectious diseases. Nat. Rev. Microbiol. 2004;2:95–108. doi: 10.1038/nrmicro821. [DOI] [PubMed] [Google Scholar]
- 37.Akiyama H., Morizane S., Yamasaki O., Oono T., Iwatsuki K. Assessment of Streptococcus pyogenes microcolony formation in infected skin by confocal laser scanning microscopy. J. Dermatol. Sci. 2003;32:193–199. doi: 10.1016/S0923-1811(03)00096-3. [DOI] [PubMed] [Google Scholar]
- 38.Davey M.E., O’toole G.A. Microbial biofilms: From ecology to molecular genetics. Microbiol. Mol. Biol. Rev. 2000;64:847–867. doi: 10.1128/MMBR.64.4.847-867.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lemon K., Earl A., Vlamakis H., Aguilar C., Kolter R. Bacterial Biofilms. Springer; New York, NY, USA: 2008. Biofilm development with an emphasis on bacillus subtilis; pp. 1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.O’Toole G.A., Kolter R. Initiation of biofilm formation in pseudomonas fluorescens wcs365 proceeds via multiple, convergent signalling pathways: A genetic analysis. Mol. Microbiol. 1998;28:449–461. doi: 10.1046/j.1365-2958.1998.00797.x. [DOI] [PubMed] [Google Scholar]
- 41.Cvitkovitch D.G., Li Y.H., Ellen R.P. Quorum sensing and biofilm formation in streptococcal infections. J. Clin. Investig. 2003;112:1626–1632. doi: 10.1172/JCI200320430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fux C., Costerton J., Stewart P., Stoodley P. Survival strategies of infectious biofilms. Trends Microbiol. 2005;13:34–40. doi: 10.1016/j.tim.2004.11.010. [DOI] [PubMed] [Google Scholar]
- 43.Götz F. Staphylococcus and biofilms. Mol. Microbiol. 2002;43:1367–1378. doi: 10.1046/j.1365-2958.2002.02827.x. [DOI] [PubMed] [Google Scholar]
- 44.Navarre W.W., Schneewind O. Surface proteins of gram-positive bacteria and mechanisms of their targeting to the cell wall envelope. Microbiol. Mol. Biol. Rev. 1999;63:174–229. doi: 10.1128/mmbr.63.1.174-229.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lewis K. Persister cells, dormancy and infectious disease. Nat. Rev. Microbiol. 2007;5:48–56. doi: 10.1038/nrmicro1557. [DOI] [PubMed] [Google Scholar]
- 46.Domenech M., García E., Moscoso M. Biofilm formation in Streptococcus pneumoniae. Microb. Biotechnol. 2012;5:455–465. doi: 10.1111/j.1751-7915.2011.00294.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lewis K. Multidrug tolerance of biofilms and persister cells. In: Romeo T., editor. Bacterial Biofilms. 1st ed. Springer Berlin Heidelberg; Heidelberg, Germany: 2008. pp. 107–131. [DOI] [PubMed] [Google Scholar]
- 48.Chen L., Wen Y.-M. The role of bacterial biofilm in persistent infections and control strategies. Int. J. Oral Sci. 2011;3:66–73. doi: 10.4248/IJOS11022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gibbons R.J. Bacterial adhesion to oral tissues: A model for infectious diseases. J. Dent. Res. 1989;68:750–760. doi: 10.1177/00220345890680050101. [DOI] [PubMed] [Google Scholar]
- 50.Whittaker C.J., Klier C.M., Kolenbrander P.E. Mechanisms of adhesion by oral bacteria. Ann. Rev. Microbiol. 1996;50:513–552. doi: 10.1146/annurev.micro.50.1.513. [DOI] [PubMed] [Google Scholar]
- 51.Starr C.R., Engleberg N.C. Role of hyaluronidase in subcutaneous spread and growth of group a streptococcus. Infect. Immun. 2006;74:40–48. doi: 10.1128/IAI.74.1.40-48.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Fischetti V.A. Streptococcal M protein: Molecular design and biological behavior. Clin. Microbiol. Rev. 1989;2:285–314. doi: 10.1038/scientificamerican0691-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Manetti A.G., Zingaretti C., Falugi F., Capo S., Bombaci M., Bagnoli F., Gambellini G., Bensi G., Mora M., Edwards A.M. Streptococcus pyogenes pili promote pharyngeal cell adhesion and biofilm formation. Mol. Microbiol. 2007;64:968–983. doi: 10.1111/j.1365-2958.2007.05704.x. [DOI] [PubMed] [Google Scholar]
- 54.Lachica R., Zink D. Plasmid-associated cell surface charge and hydrophobicity of yersinia enterocolitica. Infect. Immun. 1984;44:540–543. doi: 10.1128/iai.44.2.540-543.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Tylewska S., Hjerten S., Wadström T. Effect of subinhibitory concentrations of antibiotics on the adhesion of Streptococcus pyogenes to pharyngeal epithelial cells. Antimicrob. Agents Chemother. 1981;20:563–566. doi: 10.1128/AAC.20.5.563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Miörner H., Johansson G., Kronvall G. Lipoteichoic acid is the major cell wall component responsible for surface hydrophobicity of group a streptococci. Infect. Immun. 1983;39:336–343. doi: 10.1128/iai.39.1.336-343.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Westergren G., Olsson J. Hydrophobicity and adherence of oral streptococci after repeated subculture in vitro. Infect. Immun. 1983;40:432–435. doi: 10.1128/iai.40.1.432-435.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wibawan I.W.T., Lämmler C., Pasaribu F.H. Role of hydrophobic surface proteins in mediating adherence of group b streptococci to epithelial cells. J. Gen. Microbiol. 1992;138:1237–1242. doi: 10.1099/00221287-138-6-1237. [DOI] [PubMed] [Google Scholar]
- 59.Wadström T., Schmidt K.H., Kühnemund O., Havlícek J., Köhler W. Comparative studies on surface hydrophobicity of streptococcal strains of groups a, b, c, d and g. J. Gen. Microbiol. 1984;130:657–664. doi: 10.1099/00221287-130-3-657. [DOI] [PubMed] [Google Scholar]
- 60.Doyle R.J. Contribution of the hydrophobic effect to microbial infection. Microbes Infect. 2000;2:391–400. doi: 10.1016/S1286-4579(00)00328-2. [DOI] [PubMed] [Google Scholar]
- 61.Cotter P.D., Hill C. Surviving the acid test: Responses of gram-positive bacteria to low ph. Microbiol. Mol. Biol. Rev. 2003;67:429–453. doi: 10.1128/MMBR.67.3.429-453.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kuhnert W.L., Quivey R.G., Jr. Genetic and biochemical characterization of the F-ATPase operon from Streptococcus sanguis 10904. J. Bacteriol. 2003;185:1525–1533. doi: 10.1128/JB.185.5.1525-1533.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Martinez A.R., Abranches J., Kajfasz J.K., Lemos J.A. Characterization of the Streptococcus sobrinus acid-stress response by interspecies microarrays and proteomics. Mol. Oral Microbiol. 2010;25:331–342. doi: 10.1111/j.2041-1014.2010.00580.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ofek I., Doyle R.J. Bacterial Adhesion to Cells and Tissues. 1st ed. Volume 735. Chapman and Hall Inc.; New York, NY, USA: 1994. pp. 136–170. [Google Scholar]
- 65.Manson M.D., Tedesco P., Berg H.C., Harold F.M., van der Drift C. A protonmotive force drives bacterial flagella. Proc. Natl. Acad. Sci. USA. 1977;74:3060–3064. doi: 10.1073/pnas.74.7.3060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kakinuma Y. Inorganic cation transport and energy transduction in enterococcus hirae and other streptococci. Microbiol. Mol. Biol. Rev. 1998;62:1021–1045. doi: 10.1128/mmbr.62.4.1021-1045.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Futai M., Noumi T., Maeda M. Atp synthase (H+-ATPase): Results by combined biochemical and molecular biological approaches. Ann. Rev. Biochem. 1989;58:111–136. doi: 10.1146/annurev.bi.58.070189.000551. [DOI] [PubMed] [Google Scholar]
- 68.Bender G.R., Sutton S.V., Marquis R.E. Acid tolerance, proton permeabilities, and membrane atpases of oral streptococci. Infect. Immun. 1986;53:331–338. doi: 10.1128/iai.53.2.331-338.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Vadeboncoeur C., Pelletier M. The phosphoenolpyruvate: Sugar phosphotransferase system of oral streptococci and its role in the control of sugar metabolism. FEMS Microbiol. Rev. 1997;19:187–207. doi: 10.1111/j.1574-6976.1997.tb00297.x. [DOI] [PubMed] [Google Scholar]
- 70.Denda K., Konishi J., Hajiro K., Oshima T., Date T., Yoshida M. Structure of an atpase operon of an acidothermophilic archaebacterium, sulfolobus acidocaldarius. J. Biol. Chem. 1990;265:21509–21513. [PubMed] [Google Scholar]
- 71.Quivey R.G., Kuhnert W.L., Hahn K. Genetics of acid adaptation in oral streptococci. Crit. Rev. Oral Biol. Med. 2001;12:301–314. doi: 10.1177/10454411010120040201. [DOI] [PubMed] [Google Scholar]
- 72.Kuramitsu H.K. Virulence factors of mutans streptococci: Role of molecular genetics. Crit. Rev. Oral Biol. Med. 1993;4:159–176. doi: 10.1177/10454411930040020201. [DOI] [PubMed] [Google Scholar]
- 73.Yamashita Y., Bowen W.H., Burne R.A., Kuramitsu H.K. Role of the Streptococcus mutans gtf genes in caries induction in the specific-pathogen-free rat model. Infect. Immun. 1993;61:3811–3817. doi: 10.1128/iai.61.9.3811-3817.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Bowen W.H. Do we need to be concerned about dental caries in the coming millennium? Crit. Rev. Oral Biol. Med. 2002;13:126–131. doi: 10.1177/154411130201300203. [DOI] [PubMed] [Google Scholar]
- 75.Schilling K.M., Bowen W.H. Glucans synthesized in situ in experimental salivary pellicle function as specific binding sites for Streptococcus mutans. Infect. Immun. 1992;60:284–295. doi: 10.1128/iai.60.1.284-295.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Sturr M.G., Marquis R.E. Comparative acid tolerances and inhibitor sensitivities of isolated f-atpases of oral lactic acid bacteria. Appl. Environ. Microbiol. 1992;58:2287–2291. doi: 10.1128/aem.58.7.2287-2291.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Quivey R.G., Faustoferri R., Monahan K., Marquis R. Shifts in membrane fatty acid profiles associated with acid adaptation of Streptococcus mutans. FEMS Microbiol. Lett. 2000;189:89–92. doi: 10.1111/j.1574-6968.2000.tb09211.x. [DOI] [PubMed] [Google Scholar]
- 78.Pedersen P.L., Amzel L.M. Atp synthases. Structure, reaction center, mechanism, and regulation of one of nature’s most unique machines. J. Biol. Chem. 1993;268:9937–9940. [PubMed] [Google Scholar]
- 79.Higuchi M., Yamamoto Y., Poole L.B., Shimada M., Sato Y., Takahashi N., Kamio Y. Functions of two types of nadh oxidases in energy metabolism and oxidative stress of Streptococcus mutans. J. Bacteriol. 1999;181:5940–5947. doi: 10.1128/jb.181.19.5940-5947.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Yanagida A., Kanda T., Tanabe M., Matsudaira F., Oliveira Cordeiro J.G. Inhibitory effects of apple polyphenols and related compounds on cariogenic factors of mutans streptococci. J. Agric. Food Chem. 2000;48:5666–5671. doi: 10.1021/jf000363i. [DOI] [PubMed] [Google Scholar]
- 81.Matsumoto M., Hamada S., Ooshima T. Molecular analysis of the inhibitory effects of oolong tea polyphenols on glucan-binding domain of recombinant glucosyltransferases from Streptococcus mutans mt8148. FEMS Microbiol. Lett. 2003;228:73–80. doi: 10.1016/S0378-1097(03)00723-7. [DOI] [PubMed] [Google Scholar]
- 82.Hanada N., Kuramitsu H.K. Isolation and characterization of the Streptococcus mutans gtfd gene, coding for primer-dependent soluble glucan synthesis. Infect. Immun. 1989;57:2079–2085. doi: 10.1128/iai.57.7.2079-2085.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Bowen W., Koo H. Biology of Streptococcus mutans-derived glucosyltransferases: Role in extracellular matrix formation of cariogenic biofilms. Caries Res. 2011;45:69–86. doi: 10.1159/000324598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Duarte S., Gregoire S., Singh A.P., Vorsa N., Schaich K., Bowen W.H., Koo H. Inhibitory effects of cranberry polyphenols on formation and acidogenicity of Streptococcus mutans biofilms. FEMS Microbiol. Lett. 2006;257:50–56. doi: 10.1111/j.1574-6968.2006.00147.x. [DOI] [PubMed] [Google Scholar]
- 85.Suntharalingam P., Cvitkovitchemail D.G. Quorum sensing in streptococcal biofilm formation. Trends Microbiol. 2005;13:3–6. doi: 10.1016/j.tim.2004.11.009. [DOI] [PubMed] [Google Scholar]
- 86.Jiang S.M., Cieslewicz M.J., Kasper D.L., Wessels M.R. Regulation of virulence by a two-component system in group b streptococcus. J. Bacteriol. 2005;187:1105–1113. doi: 10.1128/JB.187.3.1105-1113.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Jimenez J.C., Federle M.J. Quorum sensing in group a streptococcus. Front. Cell. Infect. Microbiol. 2014;4 doi: 10.3389/fcimb.2014.00127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Cook L.C., LaSarre B., Federle M.J. Interspecies communication among commensal and pathogenic streptococci. MBio. 2013;4:e00382–e00313. doi: 10.1128/mBio.00382-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Donlan R.M. Biofilms: Microbial life on surfaces. Emerg. Infect. Dis. 2002;8:881–890. doi: 10.3201/eid0809.020063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Limsuwan S., Voravuthikunchai S.P. Boesenbergia pandurata (ROXB.) schltr., eleutherine americana merr. And rhodomyrtus tomentosa (aiton) hassk. As antibiofilm producing and antiquorum sensing in Streptococcus pyogenes. FEMS Immunol. Med. Microbiol. 2008;53:429–436. doi: 10.1111/j.1574-695X.2008.00445.x. [DOI] [PubMed] [Google Scholar]
- 91.Nazzaro F., Fratianni F., Coppola R. Quorum sensing and phytochemicals. Int. J. Mol. Sci. 2013;14:12607–12619. doi: 10.3390/ijms140612607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Kaur G., Rajesh S., Princy S.A. Plausible drug targets in the Streptococcus mutans quorum sensing pathways to combat dental biofilms and associated risks. Indian J. Microbiol. 2015;55:349–356. doi: 10.1007/s12088-015-0534-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Li Y.H., Tian X. Quorum sensing and bacterial social interactions in biofilms. Sensors. 2012;12:2519–2538. doi: 10.3390/s120302519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Marcy S.M. Treatment options for streptococcal pharyngitis. Clin. Pediatr. 2007;46:36S–45S. doi: 10.1177/0009922807299720. [DOI] [Google Scholar]
- 95.Stevens D.L., Bisno A.L., Chambers H.F., Dellinger E.P., Goldstein E.J., Gorbach S.L., Hirschmann J.V., Kaplan S.L., Montoya J.G., Wade J.C. Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 update by the infectious diseases society of america. Clin. Infect. Dis. 2014;59:e10–e52. doi: 10.1093/cid/ciu296. [DOI] [PubMed] [Google Scholar]
- 96.Ciofu O., Giwercman B., HØIBY N., Pedersen S.S. Development of antibiotic resistance in pseudomonas aeruginosa during two decades of antipseudomonal treatment at the danish cf center. Apmis. 1994;102:674–680. doi: 10.1111/j.1699-0463.1994.tb05219.x. [DOI] [PubMed] [Google Scholar]
- 97.Benzie I.F.F., Wachtel-Galor S. Herbal Medicine: Biomolecular and Clinical Aspects. 2nd ed. CRC Press; Boca Raton, FL, USA: 2011. pp. 1–500. [PubMed] [Google Scholar]
- 98.Savoia D. Plant-derived antimicrobial compounds: Alternatives to antibiotics. Future Microbiol. 2012;7:979–990. doi: 10.2217/fmb.12.68. [DOI] [PubMed] [Google Scholar]
- 99.Clair S. Arnica: A proven first aid remedy for injuries and accidents. J. N. Zeal. Assoc. Med. Herbal. 2010:12–13. [Google Scholar]
- 100.Shang X., Pan H., Li M., Miao X., Ding H. Lonicera japonica thunb.: Ethnopharmacology, phytochemistry and pharmacology of an important traditional chinese medicine. J. Ethnopharmacol. 2011;138:1–21. doi: 10.1016/j.jep.2011.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Yarnell E., Abascal K., Hooper C.G. Chronic sinusitis. Altern. Complement. Ther. 2003;9:39–41. doi: 10.1089/10762800360520785. [DOI] [Google Scholar]
- 102.Mathieu G., Meissa D. Traditional leafy vegetables in senegal: Diversity and medicinal uses. Afr. J. Tradit. Complement. Altern. Med. 2008;4:469–475. doi: 10.4314/ajtcam.v4i4.31239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Konan N.A., Bacchi E.M., Lincopan N., Varela S.D., Varanda E.A. Acute, subacute toxicity and genotoxic effect of a hydroethanolic extract of the cashew (Anacardium occidentale L.) J. Ethnopharmacol. 2007;110:30–38. doi: 10.1016/j.jep.2006.08.033. [DOI] [PubMed] [Google Scholar]
- 104.Li Y., Ooi L.S., Wang H., But P.P., Ooi V.E. Antiviral activities of medicinal herbs traditionally used in southern mainland china. Phytother. Res. 2004;18:718–722. doi: 10.1002/ptr.1518. [DOI] [PubMed] [Google Scholar]
- 105.Smullen J., Koutsou G., Foster H., Zumbé A., Storey D. The antibacterial activity of plant extracts containing polyphenols against Streptococcus mutans. Caries Res. 2007;41:342–349. doi: 10.1159/000104791. [DOI] [PubMed] [Google Scholar]
- 106.Berahou A., Auhmani A., Fdil N., Benharref A., Jana M., Gadhi C. Antibacterial activity of quercus ilex bark’s extracts. J. Ethnopharmacol. 2007;112:426–429. doi: 10.1016/j.jep.2007.03.032. [DOI] [PubMed] [Google Scholar]
- 107.Fabio A., Cermelli C., Fabio G., Nicoletti P., Quaglio P. Screening of the antibacterial effects of a variety of essential oils on microorganisms responsible for respiratory infections. PTR Phytother. Res. 2007;21:374–377. doi: 10.1002/ptr.1968. [DOI] [PubMed] [Google Scholar]
- 108.Ordoñez A., Gomez J., Cudmani N., Vattuone M., Isla M. Antimicrobial activity of nine extracts of sechium edule (jacq.) swartz. Microb. Ecol. Health Dis. 2003;15:33–39. doi: 10.1080/0891060010015583. [DOI] [Google Scholar]
- 109.Nair R., Chanda S. Activity of some medicinal plants against certain pathogenic bacterial strains. Indian J. Pharmacol. 2006;38:142–144. [Google Scholar]
- 110.Das M., Dhanabalan R., Doss A. In vitro antibacterial activity of two medicinal plants against bovine udder isolated bacterial pathogens from dairy herds. Ethnobot. Leafl. 2009;2009:152–158. [Google Scholar]
- 111.Kamble M.T., Gallardo W., Yakuitiyage A., Chavan B.R., Rusydi R., Rahma A. Antimicrobial activity of bioactive herbal extracts against Streptococcus agalactiae biotype 2. Int. J. Basis Appl. Biol. 2014;2:152–155. [Google Scholar]
- 112.Toivanen M., Huttunen S., Duricová J., Soininen P., Laatikainen R., Loimaranta V., Haataja S., Finne J., Lapinjoki S., Tikkanen-Kaukanen C. Screening of binding activity of Streptococcus pneumoniae, Streptococcus agalactiae and Streptococcus suis to berries and juices. PTR Phytother. Res. 2010;24:S95–S101. doi: 10.1002/ptr.2939. [DOI] [PubMed] [Google Scholar]
- 113.Nguelefack E.M., Ngu K.B., Atchade A., Dimo T., Tsabang N., Mbafor J.T. Phytochemical composition and in vitro effects of the ethyl acetate bark extract of distemonanthus benthamianus baillon (caesalpiniaceae) on Staphylococcus aureus and Streptococcus agalactiae. Cameroon J. Exp. Biol. 2006;1:50–53. doi: 10.4314/cajeb.v1i1.37927. [DOI] [Google Scholar]
- 114.Karmakar U.K., Biswas S.K., Chowdhury A., Raihan S.Z., Akbar M.A., Muhit M.A., Mowla R. Phytochemical investigation and evaluation of antibacterial and antioxidant potentials of asparagus racemosus. Int. J. Pharmacol. 2012;8:53–57. [Google Scholar]
- 115.Steinberg D., Feldman M., Ofek I., Weiss E.I. Effect of a high-molecular-weight component of cranberry on constituents of dental biofilm. J. Antimicrob. Chemother. 2004;54:86–89. doi: 10.1093/jac/dkh254. [DOI] [PubMed] [Google Scholar]
- 116.Nostro A., Cannatelli M.A., Crisafi G., Musolino A.D., Procopio F., Alonzo V. Modifications of hydrophobicity, in vitro adherence and cellular aggregation of Streptococcus mutans by Helichrysum italicum extract. LAM Lett. Appl. Microbiol. 2004;38:423–427. doi: 10.1111/j.1472-765X.2004.01509.x. [DOI] [PubMed] [Google Scholar]
- 117.Yamanaka A., Kimizuka R., Kato T., Okuda K. Inhibitory effects of cranberry juice on attachment of oral streptococci and biofilm formation. Oral Microbiol. Immunol. 2004;19:150–154. doi: 10.1111/j.0902-0055.2004.00130.x. [DOI] [PubMed] [Google Scholar]
- 118.Khare C.P. In: Indian Medicinal Plants: An Illustrated Dictionary. 1st ed. Khare C.P., editor. Springer Science & Business Media; New York, NY, USA: 2008. pp. 25–27. [Google Scholar]
- 119.Cavero R., Calvo M. Medicinal plants used for respiratory affections in navarra and their pharmacological validation. J. Ethnopharmacol. 2014;158:216–220. doi: 10.1016/j.jep.2014.10.003. [DOI] [PubMed] [Google Scholar]
- 120.Cornu C., Joseph P., Gaillard S., Bauer C., Vedrinne C., Bissery A., Melot G., Bossard N., Belon P., Lehot J.J. No effect of a homoeopathic combination of Arnica montana and Bryonia alba on bleeding, inflammation, and ischaemia after aortic valve surgery. Br. J. Clin. Pharmacol. 2010;69:136–142. doi: 10.1111/j.1365-2125.2009.03574.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Ashu Agbor M., Naidoo S. Ethnomedicinal plants used by traditional healers to treat oral health problems in cameroon. Evid. Based Complement. Altern. Med. 2015;2015:649832. doi: 10.1155/2015/649832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Monte A., Kabir M., Cook J., Rott M., Schwan W., Defoe L. Anti-Infective Agents and Methods of Use. US20060089415 A1. U.S. Patents. 2006 Apr 27;
- 123.Lim T.K. Edible Medicinal and Non-Medicinal Plants. 1st ed. Fruits. Springer; Dordrecht, The Netherlands: 2012. Parmentiera cereifera; pp. 510–514. [Google Scholar]
- 124.Locher C., Burch M., Mower H., Berestecky J., Davis H., van Poel B., Lasure A., Berghe D.V., Vlietinck A. Anti-microbial activity and anti-complement activity of extracts obtained from selected hawaiian medicinal plants. J. Ethnopharmacol. 1995;49:23–32. doi: 10.1016/0378-8741(95)01299-0. [DOI] [PubMed] [Google Scholar]
- 125.Omojasola P., Awe S. The antibacterial activity of the leaf extracts of anacardium occidentale and gossypium hirsutum against some selected microorganisms. Biosci. Res. Commun. 2004;60:25–58. [Google Scholar]
- 126.James O., Godwin E.U., Otini I.G. In vivo neutralization of naja nigricollis venom by uvaria chamae. Am. J. Biochem. Biotechnol. 2013;9:224–234. doi: 10.3844/ajbbsp.2013.224.234. [DOI] [Google Scholar]
- 127.Ogbulie J., Ogueke C., Nwanebu F. Antibacterial properties of uvaria chamae, congronema latifolium, garcinia kola, vemonia amygdalina and aframomium melegueta. Afr. J. Biotechnol. 2007;6:1549–1553. [Google Scholar]
- 128.Wickens G.E. The uses of the baobab (Adansonia digitata L.) in Africa. In: Kunkel G., editor. Taxonomic Aspects of African Economic Botany. 1st ed. AETFAT; Las Palmas de Gran Canaria, Spain: 1979. pp. 27–34. [Google Scholar]
- 129.Hebbar S., Harsha V., Shripathi V., Hegde G. Ethnomedicine of dharwad district in karnataka, india—plants used in oral health care. J. Ethnopharmacol. 2004;94:261–266. doi: 10.1016/j.jep.2004.04.021. [DOI] [PubMed] [Google Scholar]
- 130.Sezik E., Yeşilada E., Honda G., Takaishi Y., Takeda Y., Tanaka T. Traditional medicine in turkey x. Folk medicine in central anatolia. J. Ethnopharmacol. 2001;75:95–115. doi: 10.1016/S0378-8741(00)00399-8. [DOI] [PubMed] [Google Scholar]
- 131.Sezik E., Yeşİlada E., Tabata M., Honda G., Takaishi Y., Fujita T., Tanaka T., Takeda Y. Traditional medicine in turkey viii. Folk medicine in east anatolia; erzurum, erzíncan, ağri, kars, iğdir provinces. Econ. Bot. 1997;51:195–211. doi: 10.1007/BF02862090. [DOI] [Google Scholar]
- 132.Akinpelu D.A. Antimicrobial activity of anacardium occidentale bark. Fitoterapia. 2001;72:286–287. doi: 10.1016/S0367-326X(00)00310-5. [DOI] [PubMed] [Google Scholar]
- 133.Morton J.F., Dowling C.F. In: In Fruits of Warm Climates. 1st ed. Morton J., editor. Creative Resource Systems Inc.; Winterville, FL, USA: 1987. [Google Scholar]
- 134.Ganesan S. Traditional oral care medicinal plants survey of tamil nadu. Nat. Prod. Rad. 2008;7:166–172. [Google Scholar]
- 135.Okwu D.E., Iroabuchi F. Phytochemical composition and biological activities of uvaria chamae and clerodendoron splendens. J. Chem. 2009;6:553–560. doi: 10.1155/2009/190346. [DOI] [Google Scholar]
- 136.Mollik M.A.H., Hossan M.S., Paul A.K., Taufiq-Ur-Rahman M., Jahan R., Rahmatullah M. A comparative analysis of medicinal plants used by folk medicinal healers in three districts of bangladesh and inquiry as to mode of selection of medicinal plants. Ethnobot. Res. Appl. 2010;8:195–218. [Google Scholar]
- 137.Zhu S., Li W., Li J., Jundoria A., Sama A.E., Wang H. It is not just folklore: The aqueous extract of mung bean coat is protective against sepsis. Evid. Based Complement. Altern. Med. 2012;2012:498467. doi: 10.1155/2012/498467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Chao W.W., Kuo Y.H., Hsieh S.L., Lin B.F. Inhibitory effects of ethyl acetate extract of andrographis paniculata on nf-κb trans-activation activity and lps-induced acute inflammation in mice. Evid. Based Complement. Altern. Med. 2011;2011:254531. doi: 10.1093/ecam/nep120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Mohanasundari C., Natarajan D., Srinivasan K., Umamaheswari S., Ramachandran A. Antibacterial properties of Passiflora foetida L.—A common exotic medicinal plant. Afr. J. Biotechnol. 2007;6:2650–2653. [Google Scholar]
- 140.Geyid A., Abebe D., Debella A., Makonnen Z., Aberra F., Teka F., Kebede T., Urga K., Yersaw K., Biza T. Screening of some medicinal plants of ethiopia for their anti-microbial properties and chemical profiles. J. Ethnopharmacol. 2005;97:421–427. doi: 10.1016/j.jep.2004.08.021. [DOI] [PubMed] [Google Scholar]
- 141.Lim T.K. Edible Medicinal and Non-Medicinal Plants. 1st ed. Fruits. Springer; Dordrecht, The Netherlands: 2012. Crescentia cujete; pp. 480–485. [Google Scholar]
- 142.Akoachere J.T., Ndip R., Chenwi E., Ndip L., Njock T., Anong D. Antibacterial effects of zingiber officinale and garcinia kola on respiratory tract pathogens. East Afr. Med. J. 2002;79:588–592. doi: 10.4314/eamj.v79i11.8804. [DOI] [PubMed] [Google Scholar]
- 143.Farrukh U., Shareef H., Mahmud S., Ali S.A., Rizwani G.H. Antibacterial activities of coccinia grandis l. Pak. J. Bot. 2008;40:1259–1262. [Google Scholar]
- 144.Salari M., Amine G., Shirazi M., Hafezi R., Mohammadypour M. Antibacterial effects of eucalyptus globulus leaf extract on pathogenic bacteria isolated from specimens of patients with respiratory tract disorders. Clin. Microbiol. Infect. 2006;12:194–196. doi: 10.1111/j.1469-0691.2005.01284.x. [DOI] [PubMed] [Google Scholar]
- 145.Rashid F., Ahmed R., Mahmood A., Ahmad Z., Bibi N., Kazmi S.U. Flavonoid glycosides fromprunus armeniaca and the antibacterial activity of a crude extract. Arch. Pharmacal Res. 2007;30:932–937. doi: 10.1007/BF02993959. [DOI] [PubMed] [Google Scholar]
- 146.Cichewicz R.H., Thorpe P.A. The antimicrobial properties of chile peppers (capsicum species) and their uses in mayan medicine. J. Ethnopharmacol. 1996;52:61–70. doi: 10.1016/0378-8741(96)01384-0. [DOI] [PubMed] [Google Scholar]
- 147.Prachayasittikul S., Suphapong S., Worachartcheewan A., Lawung R., Ruchirawat S., Prachayasittikul V. Bioactive metabolites from spilanthes acmella murr. Molecules. 2009;14:850–867. doi: 10.3390/molecules14020850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Antonio A.G., Moraes R.S., Perrone D., Maia L.C., Santos K.R.N., Iório N.L., Farah A. Species, roasting degree and decaffeination influence the antibacterial activity of coffee against Streptococcus mutans. Food Chem. 2010;118:782–788. doi: 10.1016/j.foodchem.2009.05.063. [DOI] [Google Scholar]
- 149.Antonio A., Iorio N., Pierro V., Candreva M., Farah A., Dos-Santos K., Maia L. Inhibitory properties of coffea canephora extract against oral bacteria and its effect on demineralisation of deciduous teeth. Arch. Oral Biol. 2011;56:556–564. doi: 10.1016/j.archoralbio.2010.12.001. [DOI] [PubMed] [Google Scholar]
- 150.Vermani A. Screening of quercus infectoria gall extracts as anti-bacterial agents against dental pathogens. Indian J. Dent. Res. 2009;20:337–339. doi: 10.4103/0970-9290.57380. [DOI] [PubMed] [Google Scholar]
- 151.Hwang J.K., Shim J.S., Chung J.Y. Anticariogenic activity of some tropical medicinal plants against Streptococcus mutans. Fitoterapia. 2004;75:596–598. doi: 10.1016/j.fitote.2004.05.006. [DOI] [PubMed] [Google Scholar]
- 152.Almeida L.S.B.D., Murata R.M., Yatsuda R., Dos Santos M.H., Nagem T.J., Alencar S.M.D., Koo H., Rosalen P.L. Antimicrobial activity of rheedia brasiliensis and 7-epiclusianone against Streptococcus mutans. Phytomedicine. 2008;15:886–891. doi: 10.1016/j.phymed.2007.12.003. [DOI] [PubMed] [Google Scholar]
- 153.Xu X., Zhou X.D., Wu C.D. The tea catechin epigallocatechin gallate suppresses cariogenic virulence factors of Streptococcus mutans. Antimicrob. Agents Chemother. 2011;55:1229–1236. doi: 10.1128/AAC.01016-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Khan R., Zakir M., Afaq S.H., Latif A., Khan A.U. Activity of solvent extracts of prosopis spicigera, zingiber officinale and trachyspermum ammi against multidrug resistant bacterial and fungal strains. J. Infect. Dev. Ctries. 2010;4:292–300. doi: 10.3855/jidc.621. [DOI] [PubMed] [Google Scholar]
- 155.Khan R., Adil M., Danishuddin M., Verma P.K., Khan A.U. In vitro and in vivo inhibition of Streptococcus mutans biofilm by trachyspermum ammi seeds: An approach of alternative medicine. Phytomedicine. 2012;19:747–755. doi: 10.1016/j.phymed.2012.04.004. [DOI] [PubMed] [Google Scholar]
- 156.Zheng Y., Liu Z., Ebersole J., Huang C.B. A new antibacterial compound from luo han kuo fruit extract (siraitia grosvenori) J. Asian Natl. Prod. Res. 2009;11:761–765. doi: 10.1080/10286020903048983. [DOI] [PubMed] [Google Scholar]
- 157.Mu J. Anti-cariogenicity of maceration extract of momordica grosvenori: Laboratory study. Chin. J. Stomatol. 1998;33:183–185. [PubMed] [Google Scholar]
- 158.Bernardshaw S., Johnson E., Hetland G. An extract of the mushroom agaricus blazei murill administered orally protects against systemic Streptococcus pneumoniae infection in mice. Scand. J. Immunol. 2005;62:393–398. doi: 10.1111/j.1365-3083.2005.01667.x. [DOI] [PubMed] [Google Scholar]
- 159.Hetland G., Samuelsen A., Loslash V., Paulsen B., Aaberge I., Groeng E.C., Michaelsen T. Protective effect of plantago major l. Pectin polysaccharide against systemic Streptococcus pneumoniae infection in mice. Scand. J. Immunol. 2000;52:348–355. doi: 10.1046/j.1365-3083.2000.00793.x. [DOI] [PubMed] [Google Scholar]
- 160.Koné W.M., Atindehou K.K., Kacou-N A., Dosso M. Evaluation of 17 medicinal plants from northern cote d’ivoire for their in vitro activity against Streptococcus pneumoniae. Afr. J. Tradit. Complement. Altern. Med. 2007;4:17–22. [PMC free article] [PubMed] [Google Scholar]
- 161.Tepe B., Daferera D., Sokmen A., Sokmen M., Polissiou M. Antimicrobial and antioxidant activities of the essential oil and various extracts of salvia tomentosa miller (lamiaceae) Food Chem. 2005;90:333–340. doi: 10.1016/j.foodchem.2003.09.013. [DOI] [Google Scholar]
- 162.Kuta F.A., Ndamitso M.M., Ibrahim H. Antibacterial effect of eucalyptus globulus leaves extract on antibiotic resistant strains of Streptococcus pneumoniae. Appl. Med. Inform. 2008;22:52–54. [Google Scholar]
- 163.Kuta F., Damisa D., Adamu A., Nwoha E., Bello I. Antibacterial activity of euphorbia hirta against Streptococcus pneumoniae, klebsiella pneumoniae and proteus vulgaris. Bayero J. Pure Appl. Sci. 2014;6:65–68. doi: 10.4314/bajopas.v6i2.14. [DOI] [Google Scholar]
- 164.Janecki A., Kolodziej H. Anti-adhesive activities of flavan-3-ols and proanthocyanidins in the interaction of group a-streptococci and human epithelial cells. Molecules. 2010;15:7139–7152. doi: 10.3390/molecules15107139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Percival R.S., Devine D.A., Duggal M.S., Chartron S., Marsh P.D. The effect of cocoa polyphenols on the growth, metabolism, and biofilm formation by Streptococcus mutans and Streptococcus sanguinis. EOS Eur. J. Oral Sci. 2006;114:343–348. doi: 10.1111/j.1600-0722.2006.00386.x. [DOI] [PubMed] [Google Scholar]
- 166.Furiga A., Lonvaud Funel A., Dorignac G., Badet C. In vitro anti-bacterial and anti-adherence effects of natural polyphenolic compounds on oral bacteria. JAM J. Appl. Microbiol. 2008;105:1470–1476. doi: 10.1111/j.1365-2672.2008.03882.x. [DOI] [PubMed] [Google Scholar]
- 167.Rahim Z.H.A., Khan H.B.S.G. Comparative studies on the effect of crude aqueous (ca) and solvent (cm) extracts of clove on the cariogenic properties of Streptococcus mutans. J. Oral Sci. 2006;48:117–123. doi: 10.2334/josnusd.48.117. [DOI] [PubMed] [Google Scholar]
- 168.Matsumoto M., Tsuji M., Okuda J., Sasaki H., Nakano K., Osawa K., Shimura S., Ooshima T. Inhibitory effects of cacao bean husk extract on plaque formation in vitro and in vivo. Eur. J. Oral Sci. 2004;112:249–252. doi: 10.1111/j.1600-0722.2004.00134.x. [DOI] [PubMed] [Google Scholar]
- 169.Prabu G.R., Gnanamani A., Sadulla S. Guaijaverin—A plant flavonoid as potential antiplaque agent against Streptococcus mutans. J. Appl. Microbiol. 2006;101:487–495. doi: 10.1111/j.1365-2672.2006.02912.x. [DOI] [PubMed] [Google Scholar]
- 170.Yamanaka-Okada A., Sato E., Kouchi T., Kimizuka R., Kato T., Okuda K. Inhibitory effect of cranberry polyphenol on cariogenic bacteria. Bull. Tokyo Dent. Coll. 2008;49:107–112. doi: 10.2209/tdcpublication.49.107. [DOI] [PubMed] [Google Scholar]
- 171.Murugan K., Sekar K., Sangeetha S., Ranjitha S., Sohaibani S. Antibiofilm and quorum sensing inhibitory activity of achyranthes aspera on cariogenic Streptococcus mutans: An in vitro and in silico study. Pharm. Biol. 2013;51:728–736. doi: 10.3109/13880209.2013.764330. [DOI] [PubMed] [Google Scholar]
- 172.Al-Sohaibani S., Murugan K. Anti-biofilm activity of salvadora persica on cariogenic isolates of Streptococcus mutans: In vitro and molecular docking studies. Biofouling. 2012;28:29–38. doi: 10.1080/08927014.2011.647308. [DOI] [PubMed] [Google Scholar]
- 173.Hasan S., Danishuddin M., Adil M., Singh K., Verma P.K., Khan A.U. Efficacy of e. Officinalis on the cariogenic properties of Streptococcus mutans: A novel and alternative approach to suppress quorum-sensing mechanism. PLoS ONE. 2012;7:e40319. doi: 10.1371/journal.pone.0040319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Somanah J., Bourdon E., Bahorun T., Aruoma O.I. The inhibitory effect of a fermented papaya preparation on growth, hydrophobicity, and acid production of Streptococcus mutans, Streptococcus mitis, and Lactobacillus acidophilus: Its implications in oral health improvement of diabetics. FSN3 Food Sci. Nutr. 2013;1:416–421. doi: 10.1002/fsn3.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Green A.E., Rowlands R.S., Cooper R.A., Maddocks S.E. The effect of the flavonol morin on adhesion and aggregation of Streptococcus pyogenes. FEMS Microbiol. Lett. 2012;333:54–58. doi: 10.1111/j.1574-6968.2012.02598.x. [DOI] [PubMed] [Google Scholar]
- 176.Zhou L., Ding Y., Chen W., Zhang P., Chen Y., Lv X. The in vitro study of ursolic acid and oleanolic acid inhibiting cariogenic microorganisms as well as biofilm. ODI Oral Dis. 2013;19:494–500. doi: 10.1111/odi.12031. [DOI] [PubMed] [Google Scholar]
- 177.Evans J., Gregory R.L., Huang R. Polyphenol effect on Streptococcus mutans comc-biofilm. Indiana Univ. Sch. Dent. 2015 doi: 10.1111/j.1600-0765.2012.01506.x. [DOI] [Google Scholar]
- 178.Kang M.S., Oh J.S., Kang I.C., Hong S.J., Choi C.H. Inhibitory effect of methyl gallate and gallic acid on oral bacteria. J. Microbiol. 2008;46:744–750. doi: 10.1007/s12275-008-0235-7. [DOI] [PubMed] [Google Scholar]
- 179.Sendamangalam V., Choi O.K., Kim D., Seo Y. The anti-biofouling effect of polyphenols against Streptococcus mutans. Biofouling. 2011;27:13–19. doi: 10.1080/08927014.2010.535897. [DOI] [PubMed] [Google Scholar]
- 180.Wang Y., Chung F.F., Lee S.M., Dykes G.A. Inhibition of attachment of oral bacteria to immortalized human gingival fibroblasts (HGF-1) by tea extracts and tea components. BMC Res. Notes. 2013;6:143. doi: 10.1186/1756-0500-6-143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Xiao Y., Liu T., Zhan L., Zhou X. The effects of tea polyphenols on the adherence of cariogenic bacterium to the collagen in vitro. West China J. Stomatol. 2000;18:340–342. [PubMed] [Google Scholar]
- 182.Feng G., Klein M.I., Gregoire S., Singh A.P., Vorsa N., Koo H. The specific degree-of-polymerization of a-type proanthocyanidin oligomers impacts Streptococcus mutans glucan-mediated adhesion and transcriptome responses within biofilms. Biofouling. 2013;29:629–640. doi: 10.1080/08927014.2013.794456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Janecki A., Conrad A., Engels I., Frank U., Kolodziej H. Evaluation of an aqueous-ethanolic extract from pelargonium sidoides (EPs® 7630) for its activity against group A-streptococci adhesion to human HEp-2 epithelial cells. J. Ethnopharmacol. 2011;133:147–152. doi: 10.1016/j.jep.2010.09.018. [DOI] [PubMed] [Google Scholar]
- 184.Stauder M., Papetti A., Mascherpa D., Schito A.M., Gazzani G., Pruzzo C., Daglia M. Antiadhesion and antibiofilm activities of high molecular weight coffee components against Streptococcus mutans. J. Agric. Food Chem. 2010;58:11662–11666. doi: 10.1021/jf1031839. [DOI] [PubMed] [Google Scholar]
- 185.Koo H., Nino de Guzman P., Schobel B.D., Vacca Smith A.V., Bowen W.H. Influence of cranberry juice on glucan-mediated processes involved in Streptococcus mutans biofilm development. Caries Res. 2006;40:20–27. doi: 10.1159/000088901. [DOI] [PubMed] [Google Scholar]
- 186.Zheng J., Ramirez V.D. Inhibition of mitochondrial proton F0F1-ATPase/ATP synthase by polyphenolic phytochemicals. Br. J. Pharmacol. 2000;130:1115–1123. doi: 10.1038/sj.bjp.0703397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.McKenna E., Smith J.S., Coll K.E., Mazack E.K., Mayer E.J., Antanavage J., Wiedmann R.T., Johnson R.G., Jr. Dissociation of phospholamban regulation of cardiac sarcoplasmic reticulum Ca2+ ATPase by quercetin. J. Biol. Chem. 1996;271:24517–24525. doi: 10.1074/jbc.271.40.24517. [DOI] [PubMed] [Google Scholar]
- 188.Hirano T., Oka K., Akiba M. Effects of synthetic and naturally occurring flavonoids on Na+, K+-atpase: Aspects of the structure-activity relationship and action mechanism. Life Sci. 1989;45:1111–1117. doi: 10.1016/0024-3205(89)90168-9. [DOI] [PubMed] [Google Scholar]
- 189.Lang D.R., Racker E. Effects of quercetin and F1 inhibitor on mitochondrial atpase and energy-linked reactions in submitochondrial particles. Biochim. Biophys. Acta. 1974;333:180–186. doi: 10.1016/0005-2728(74)90002-4. [DOI] [PubMed] [Google Scholar]
- 190.Nguyen P.T.M., Marquis R.E. Antimicrobial actions of α-mangostin against oral streptococci. Can. J. Microbiol. 2011;57:217–225. doi: 10.1139/W10-122. [DOI] [PubMed] [Google Scholar]
- 191.Gregoire S., Singh A., Vorsa N., Koo H. Influence of cranberry phenolics on glucan synthesis by glucosyltransferases and Streptococcus mutans acidogenicity. J. Appl. Microbiol. 2007;103:1960–1968. doi: 10.1111/j.1365-2672.2007.03441.x. [DOI] [PubMed] [Google Scholar]
- 192.Adamson G.E., Lazarus S.A., Mitchell A.E., Prior R.L., Cao G., Jacobs P.H., Kremers B.G., Hammerstone J.F., Rucker R.B., Ritter K.A., et al. HPLC method for the quantification of procyanidins in cocoa and chocolate samples and correlation to total antioxidant capacity. J. Agric. Food Chem. 1999;47:4184–4188. doi: 10.1021/jf990317m. [DOI] [PubMed] [Google Scholar]
- 193.Hattori M., Kusumoto I.T., Namba T., Ishigami T., Hara Y. Effect of tea polyphenols on glucan synthesis by glucosyltransferase from Streptococcus mutans. Chem. Pharm. Bull. 1990;38:717–720. doi: 10.1248/cpb.38.717. [DOI] [PubMed] [Google Scholar]
- 194.Riihinen K., Ryynanen A., Toivanen M., Kononen E., Torronen R., Tikkanen-Kaukanen C. Antiaggregation potential of berry fractions against pairs of Streptococcus mutans with fusobacterium nucleatum or actinomyces naeslundii. Phytother. Res. PTR. 2011;25:81–87. doi: 10.1002/ptr.3228. [DOI] [PubMed] [Google Scholar]
- 195.Thimothe J., Bonsi I.A., Padilla-Zakour O.I., Koo H. Chemical characterization of red wine grape (vitis vinifera and vitis interspecific hybrids) and pomace phenolic extracts and their biological activity against Streptococcus mutans. J. Agric. Food Chem. 2007;55:10200–10207. doi: 10.1021/jf0722405. [DOI] [PubMed] [Google Scholar]
- 196.Singh B.N., Pandey G., Jadaun V., Singh S., Bajpai R., Nayaka S., Naqvi A.H., Rawat A.K.S., Upreti D.K., Singh B.R. Development and characterization of a novel swarna-based herbo-metallic colloidal nano-formulation–inhibitor of Streptococcus mutans quorum sensing. RSC Adv. 2015;5:5809–5822. doi: 10.1039/C4RA11939H. [DOI] [Google Scholar]
- 197.Wolinsky L.E., Mania S., Nachnani S., Ling S. The inhibiting effect of aqueous azadirachta indica (neem) extract upon bacterial properties influencing in vitro plaque formation. J. Dent. Res. 1996;75:816–822. doi: 10.1177/00220345960750021301. [DOI] [PubMed] [Google Scholar]
- 198.Tomczyk M., Pleszczyńska M., Wiater A. In vitro anticariogenic effects of aerial parts of drymocallis rupestris and its phytochemical profile. Planta Med. 2012;78:PI343. doi: 10.1055/s-0032-1321030. [DOI] [PubMed] [Google Scholar]
- 199.Tagashira M., Uchiyama K., Yoshimura T., Shirota M., Uemitsu N. Inhibition by hop bract polyphenols of cellular adherence and water-insoluble glucan synthesis of mutans streptococci. Biosci. Biotechnol. Biochem. 1997;61:332–335. doi: 10.1271/bbb.61.332. [DOI] [PubMed] [Google Scholar]