Highlights
-
•
Chikungunya in infants may lead to unusual neurological manifestations.
-
•
Chikungunya virus may cause Horner syndrome.
-
•
We believe that a vasculitis caused by the CHIKV infection led to Horner syndrome.
Keywords: Chikungunya virus, Horner syndrome
Abstract
We describe an infant with Chikungunya virus (CHIKV) infection who developed Horner syndrome. The infant had diagnostic confirmation of CHIKV infection by IgM-ELISA positive in serum and cerebrospinal fluid, and clinical signs of Horner syndrome. Magnetic resonance angiography showed alterations in the cervical and intra cavernous portions of the internal carotid artery. To the best of our knowledge this is the first report of the association of CHIKV infection with Horner syndrome.
Introduction
Chikungunya Virus (CHIKV) is an arthropod-borne virus that recently spread out of its usual endemic area with an outbreak in Latin America especially in Brazil [1,2]. The first cases of CHIKV infection in Brazil were reported in 2014 [3]. The main symptoms are fever, muscle aches, vomiting, cutaneous rash and polyarthralgia [4]. Neurological manifestations have been reported as encephalitis, myelitis, seizures, altered level of consciousness, acute flaccid paralysis, retrobulbar neuritis, cognitive deficits, neuro-psychiatric behavioral disturbances and Guillain-Barré syndrome [5,6]. However, Horner syndrome has not been reported associated with CHIKV. Horner syndrome is characterized by the triad of clinical signs consisting of: miosis, ptosis and facial anhidrosis. Horner syndrome is due to a disruption of any part of the ipsilateral sympathetic innervation of the eye. Here we report an infant with CHIKV infection who developed Horner syndrome.
Case report
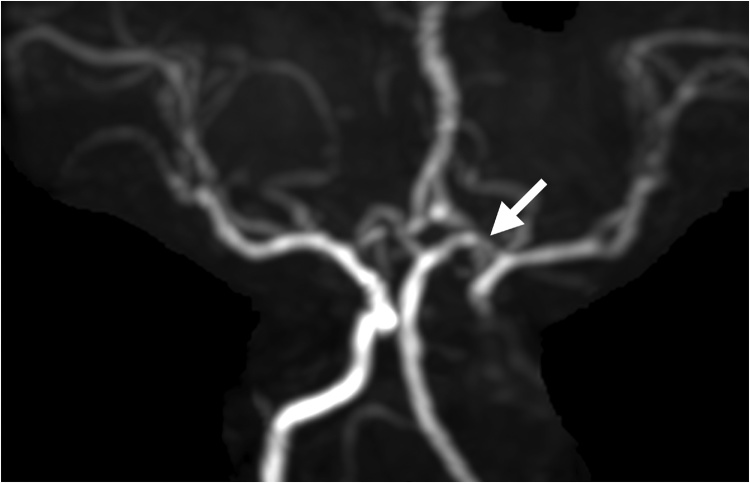
On January 13, 2018, a 2-month-old female resident from Recife, northeast Brazil, was admitted at Instituto de Medicina Integral Prof. Fernando Figueira (IMIP) with high-grade fever and rash for 5 days. The mother reported other similar cases with fever and muscular pain in her neighborhood. The infant presented with a compromised general condition, irritability and altered sensorium. She had a rash which was described as initially macular erythematous and progressed to hyperpigmentation and skin peeling, especially in abdomen and upper and lower limbs. Admission tests showed anemia (Hb = 7.2 g/dL), thrombocytopenia (50.000 u/L), hypokalemia (3.2 mmol/L) and some hepatic involvement (ALT = 80 u/L). The infant received hydration, parenteral antimicrobials (ceftriaxone and oxacillin), packed red blood cells and platelet concentrate in the pediatric intensive care unit. In the 4th day of hospitalization, she was found to have anisocoric pupils, myosis and ipsilateral ptosis; direct and consensual photomotor reflexes were present in both eyes. Fundoscopy was normal. Carotid doppler ultrasound was normal. Magnetic resonance angiography showed no flow in the cervical and intra-cavernous portions of the left internal carotid artery; recanalization of the supra-cavernous portion of the carotid artery and accentuation of the cerebrospinal fluid spaces surrounding the carotid arteries were observed (Fig. 1). IgM ELISA for CHIKV was positive in serum and cerebrospinal fluid cell counts and chemistries were normal. The infant was discharged at the tenth day of hospitalization and she still continued to have ptosis and myosis in the left eye.
Fig. 1.
Magnetic resonance angiography showing absence of flow in the cervical and intra cavernous portions of the internal carotid artery (left), with recanalization of the supra-cavernous portion.
Discussion
To the best of our knowledge this is the first report of the association of CHIKV infection with Horner syndrome. The infant had diagnostic confirmation of CHIKV infection (IgM-ELISA positive in serum and cerebrospinal fluid) and clinical signals of Horner syndrome. CHIKV is usually considered to cause a self-limiting benign illness in children. However, especially in infants and elderly, unusual neurological manifestations may be present and a high mortality may be observed [7]. Direct viral neuroinvasion with CHIKV seem to occur particularly in infants and elderly patients, while autoimmune forms were more common in middle-aged and previously healthy patients [8]. However as in our case Horner syndrome developed during the second week of CHIKV infection we think that it is most likely an autoimmune response.
Neuro-ophthalmic manifestations of Chikungunya are uncommon and include: optic neuritis, neuroretinitis, hemianopia and external ophthalmoplegia [9]. Bilateral external ophthalmoplegia has been also described as a part of the spectrum of neuro-ophthalmic manifestations of Chikungunya fever [10]. We believe that a vasculitis caused by the CHIKV infection lead to Horner syndrome. CNV vasculitis was described previously in a patient with concomitant infection with CHIKV, Zika virus and dengue virus [11].
A significant number of pediatric Horner syndromes are idiopathic. George et al found no etiology in 16 of 23 (70%) infants with Horner syndrome identified in the 1 st year of life [11]. Smith et al could not identify an etiology in 35% of children with a Horner syndrome who were followed for a mean period of 5 years [12].
In conclusion CHIKV infection may be associated with Horner syndrome in infants, possibly leading from a central nervous system vasculitis.
Declarations of interest
None.
Financial disclosure
None of the authors have financial involvement in any organization or direct financial involvement in the subject matter or materials.
Authorship
All authors contributed to conception of the study. All authors have participated signifincatly in writing of this manuscript and approve of its content. The final manuscript has been seen and approved by all authors.
Ethical approval
This work has been carried out in accordance with The Code of Ethics of the World Medical Association (Declaration of Helsinki). This study was previously approved by IMIP’s Ethics Committee. An informed consent was obtained from the parents.
Conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.Fernández-Salas I., Danis-Lozano R., Casas-Martínez M., Ulloa A., Bond J.G., Marina C.F. Historical inability to control Aedes aegypti as a main contributor of fast dispersal of chikungunyaoutbreaks in Latin America. Antiviral Res. 2015;124:30–42. doi: 10.1016/j.antiviral.2015.10.015. [DOI] [PubMed] [Google Scholar]
- 2.Magalhaes T., Braga C., Cordeiro M.T., Oliveira A.L.S., Castanha P.M.S., Maciel A.P.R. Zika virus displacement by a chikungunya outbreak in Recife, Brazil. PLoS Negl Trop Dis. 2017;11(11) doi: 10.1371/journal.pntd.0006055. e0006055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nunes M.R.T., Faria N.R., de Vasconcelos J.M., Golding N., Kraemer M.U.G., de Oliveira L.F. Emergence and potential for spread of Chikungunya virus in Brazil. BMC Med. 2015;13:102. doi: 10.1186/s12916-015-0348-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Peper S.M., Monson B.J., Van Schooneveld T., Smith C.J. That which bends up: a case report and literature review of Chikungunya virus. J Gen Intern Med. 2016;31:576–581. doi: 10.1007/s11606-015-3459-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Singh A., Jain R. Neurological manifestations of Chikungunya in children. Indian Pediatr. 2017;54:249. doi: 10.1007/s13312-017-1040-3. [DOI] [PubMed] [Google Scholar]
- 6.Brizzi K. Neurologic manifestation of Chikungunya virus. Curr Infect Dis Rep. 2017;9:6. doi: 10.1007/s11908-017-0561-1. [DOI] [PubMed] [Google Scholar]
- 7.Brito C.A.A. Alert: severe cases and deaths associated with Chikungunya in Brazil. Rev Soc Bras Med Trop. 2017;50:585–589. doi: 10.1590/0037-8682-0479-2016. [DOI] [PubMed] [Google Scholar]
- 8.Cerny T., Schwarz M., Schwarz U., Lemant J., Gerardin P., Keller E. The range of neurological complications in Chikungunya fever. Neurocrit Care. 2017;27:447–457. doi: 10.1007/s12028-017-0413-8. [DOI] [PubMed] [Google Scholar]
- 9.Rose N., Anoop T.M., John A.P. Acute optic neuritis following infection with Chikungunya virus in southern rural India. Int J Infect Dis. 2011;15:e147–e150. doi: 10.1016/j.ijid.2010.10.004. [DOI] [PubMed] [Google Scholar]
- 10.Dutta P., Sharma A. A case of atypical ophthalmoplegia after Chikungunya fever. Int Ophthalmol. 2017 doi: 10.1007/s10792-017-0529-z. [DOI] [PubMed] [Google Scholar]
- 11.Acevedo N., Waggoner J., Rodriguez M., Rivera L., Landivar J., Pinsky B. Zika Virus, Chikungunya virus, and dengue virus in cerebrospinal fluid from adults with neurological manifestations, Guayaquil. Ecuador. Front Microbiol. 2017;8:42. doi: 10.3389/fmicb.2017.00042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.George N.D., Gonzalez G., Hoyt C.S. Does Horner’s syndrome in infancy require investigation? Br J Ophthalmol. 1998;82:51–54. doi: 10.1136/bjo.82.1.51. [DOI] [PMC free article] [PubMed] [Google Scholar]