Abstract
Objectives: To date, the complex interrelationships between family function, doctor-patient communication, knowledge about tuberculosis (TB), stigma, and depressive symptoms among patients with TB are insufficiently understood. We explored the interrelationships between family function, doctor-patient communication, knowledge about TB, TB-related stigma, and depressive symptoms and examined whether TB-related stigma played a mediating role.
Methods: A cross-sectional survey was conducted between October 1, 2013 and March 31, 2014 in Hubei province, central China. Data were collected from 1,309 patients with TB using a structured questionnaire that measured family function, doctor-patient communication, knowledge about TB, stigma, and depressive symptoms. Structural equation modeling was used to examine the interrelationships among the study variables based on the hypothesized model.
Results: The proposed model provided a good fit to the obtained data. There were indirect effects between family function, doctor-patient communication, knowledge about TB, and depressive symptoms through stigma (β = −0.048, P = 0.002; β = −0.028, P = 0.001; β = −0.021, P = 0.009, respectively). Stigma partially mediated the effect of family function and knowledge about TB on depressive symptoms and fully mediated the effect of doctor-patient communication on depressive symptoms.
Conclusions: This study elucidated the pathways linking family function, doctor-patient communication, and knowledge about TB to depressive symptoms and confirmed that the effect of those variables on depressive symptoms can be mediated by stigma. Those findings provide direction and information for depression interventions among patients with TB.
Keywords: tuberculosis, stigma, depression, epidemiology, China
Introduction
Tuberculosis (TB) remains a major global health problem (1, 2). TB affects not only physical health, but also the mental well-being of patients. For patients with TB, depression is a common mental disorder (3). The presence of depressive disorder leads to poor treatment adherence (4), drug resistance, and high rates of community transmission, ultimately increasing morbidity, and mortality (5). Therefore, it is necessary to identify the related risk factors of depression among patients with TB and accordingly devise effective interventions.
At present, studies have begun to explore the influencing factors of depression in patients with TB to take measures to reduce the risk of depression. However, the prevalence of depressive symptoms in patients with TB is still high, as reported in India (39.5%) (6), Ethiopia (43.4%) (7), Pakistan (46.3%) (8), and Cameroon (61.1%) (9). Much of the existing TB programs were focused on outcomes of mortality and microbiological cure (10), while mental health-related outcomes were ignored, which may lead to the high prevalence of depression in patients with TB. In addition, inadequate research on the influencing factors of depression may be another key reason. Previous studies have reported that some personal and social factors were associated with depression in patients with TB, such as age, sex, lack of TB knowledge, insufficient social support, and TB-related stigma (7, 9). However, it is unclear whether these factors act independently or through complex mechanisms. Furthermore, previous studies exploring factors associated with depression mainly relied on analysis via logistic regression or linear regression analyses (9, 11). Although useful information was provided, these types of analyses considered the effects among the variables that may affect depression independently; However, it is possible that those variables interacted in a more complex way, which was not straightforwardly captured by the regression analysis. Therefore, the complexity of the interrelationships among them is less well-understood (12).The lack of research on those complex relationships makes it difficult to determine accurately what variables should be targeted in depression interventions (13).
An alternative method to tackle these issues is the use of structural equation modeling (SEM), a technique designed to decompose into direct and indirect effects of variables to understand mechanisms and pathways that may explain these relationships (14, 15). In addition, SEM analysis is generally more robust than regression analyses because measurement errors are considered (16). Consequently, we applied SEM to address the complex interrelationships between specific personal and social variables and depressive symptoms among patients with TB in China. Understanding complex pathways may increase the effectiveness of interventions to reduce depression risk among patients with TB, which may ultimately decrease the morbidity and mortality.
Theoretical background
Stigma and depressive symptoms
Goffman posited that stigma was a social process that reduced individuals “from a whole and usual person to a tainted, discounted one” (17). During this process, patients tend to conceal their symptoms and withdraw from interpersonal contact for fear of discrimination, thereby isolating themselves to avoid negative public attitudes. TB is usually associated with uncleanliness, and patients are often attached to a disease label and experience social stigma (18, 19). Previous studies on the impact of stigma among patients with TB suggested TB-related stigma may lead to diminished self-esteem and self-efficiency and has been found to be significantly associated with the development of mental health problems, especially suffering from depressive symptoms (20, 21). Moreover, a number of studies have confirmed that patients with TB are more likely to have depressive symptoms than the general population and a high level of stigma among patients with TB in different countries has been reported (7, 9, 20). However, few studies have investigated the status of stigma and their relationship with depression in patients with TB in China. Due to variation in socio-cultural elements, ethnicity, and region, factors associated with TB-related stigma may differ and it is necessary to focus on the stigma and depression of patients with TB in China.
Personal and social factors (e.g., family function, doctor-patient communication, knowledge about TB, etc.) and depressive symptoms
The evidence for the relationship between social support and depressive symptoms has been well-substantiated by previous studies (7, 11). Indeed, the family is the main source of social support when the disease occurs, whether through tangible instrumental support, such as administering medication and preparing meals, or through emotional support (22). A-well functioning family suggests that the family could adapt to the crisis including the patients illness and role change and may be effective in lowering the risk of depression, while family dysfunction would suggest that the home environment might be stressful to the patient with TB. In addition, good doctor-patient communication is also a source of social support for patients. Previous studies has demonstrated that the levels of perceived social support received from healthcare workers are negatively associated with depressive symptoms (23). Jittimanee et al. found that patients with low TB knowledge were more likely to have severe TB disease and to have depressive symptoms (24).
Personal and social factors (e.g., family function, doctor-patient communication, knowledge about Tb, etc.) and stigma
Various researchers have explored the relationship between personal and social factors (e.g., family function, doctor-patient communication, knowledge about TB, etc.) and stigma in patients with TB. The relationship between social support and TB-related stigma has been examined and low levels of social support was associated with high levels of TB-related stigma in patients with TB (25). Few studies, however, have been published to date on the relationship between family function and TB-related stigma. Only one study conducted in Pakistan showed that good family function can alleviate stigma in patients with TB (26). Stewart et al have reported doctor-patient communication may have negative correlation with stigma (27). Moreover, in our previous study, the relationship between patients' knowledge about TB and stigma in patients with TB has been confirmed. We found that knowledge about TB may have negative correlation with stigma using logistic regression (28).
Model assignment and hypotheses
In summary, previous studies provided some evidence that TB-related stigma are influenced by personal and social variables (e.g., family function, doctor-patient communication, knowledge about TB, etc.) (28, 29). Previous studies also provided evidence that patients with greater TB-related stigma were more likely to have higher levels of depression (7). However, the complex interrelationships between these variables have not been explored.
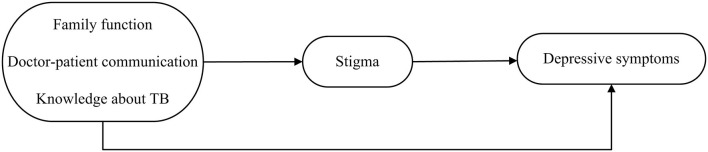
Based on the above review, a hypothetical model (Figure 1) was obtained. As illustrated in Figure 1, we proposed the following hypotheses: (Hypothesis 1) Family function, doctor-patient communication, and knowledge about TB will be negatively related to stigma. (Hypothesis 2) Stigma will be positively related to depressive symptoms. (Hypothesis 3) Stigma will mediate the relationship between family function, doctor-patient communication, knowledge about TB, and depressive symptoms.
Figure 1.
Hypothetical model of relationships between family function, doctor-patient communication, and knowledge about TB, stigma, and depression among patients with TB.
Methods
Participants and sampling
Ethical approval was provided by the Human Research Ethics Committee, Huazhong University of Science and Technology, Wuhan, China. Each participant was voluntary and provided written informed consent prior to participating in the study.
A cross-sectional study was carried out between October 1, 2013 and March 31, 2014 in Hubei province, central China. Multistage stratified sampling was performed. Counties across Hubei province were divided into three categories based on their economic development status (i.e., upper, middle, and lower), and a county was randomly selected from each category. Thereafter, patients with TB who attended TB clinics at the study sites in the selected counties were recruited as participants. The inclusion criterion was a diagnosis of active TB, based on national TB program guidelines, and the exclusion criterion was the presence of psychosis. Some elderly people with TB have more health problems, which makes it very difficult for them to complete the self-assessment questionnaire, resulting in a valid response rate of 84.7%. Thus, 1,430 patients with TB completed a structured, self-administered questionnaire anonymously. Of the collected 1,430 questionnaires, 88 were removed due to a large number of missing data, and eventually 1,342 TB patients were included in the analysis.
Measuring instruments
The questionnaire consisted of six sections: Demographic Characteristics, Family Function, Doctor-patient Communication, Knowledge about TB, TB-Related Stigma, Depressive Symptoms. The demographic characteristics included age, sex, educational level, and history of prior anti-TB treatment.
Patients' family function was measured using the Family APGAR Index developed by Smilkstein in 1978 (30). It was designed to evaluate the satisfaction with social support received from their family members based on five components: Adaptability, Partnership, Growth, Affection, and Resolve. Each item is scored using a 3-point Likert scale ranging from “scarcely” (= 0) to “often” (= 3). The item scores are summed to provide a total score (range: 0–10) and a higher score indicates better family function. The Family APGAR Index has been widely used in China, with good reliability and validity (31). In the present study, the Family APGAR Index showed high internal consistency (Cronbach's α = 0.86).
Doctor-patient communication was measured by the following four questions: (1) satisfaction with the doctors' service attitude; (2) extent to which the doctor introduces the illness; (3) extent to which the doctor explains the details of taking anti-TB agents; and (4) extent to which the doctor explains adverse drug reactions to anti-TB agents. Patients were asked to rate their answers in terms of satisfaction or detail scale ranging from 1 to 3 for the four questions listed above. The total score ranged from 4 to 12, and a higher score means better doctor-patient communication.
Patients' knowledge about TB was measured by six multiple-choice questions which were mainly from the questionnaire used in the National TB Epidemiological Survey of China (32): (1) the cause of TB, (2) the route of TB transmission, (3) whether TB can be cured, (4) duration of TB standard treatment regimens, (5) common clinical symptoms of TB, and (6) unhealthy behaviors that make TB susceptible to infection.
In the six questions, the first four questions have a single correct answer, and the patient scores 1 point for each correct answer; There were four correct answers to the remaining two questions, and the patient receives 0.5 point for each correct choice. If the answer is incorrect or “I do not know,” then the question score is 0 points. Thus, the total score of TB knowledge ranges from 0 to 8 points. The higher the TB knowledge score reflects that the patient has more knowledge of TB.
TB-related stigma was measured using the TB-Related Stigma Scale, which was developed by our research group according to the standard method for the development of new scales and has shown good validity and internal consistency (Cronbach's α = 0.88). Detailed information on the development and evaluation of this scale was available in our previous study (33). The scale consists of nine items divided between three subscales (Negative Experience, Emotional Reactions, and Coping Style). Responses for the items are provided using a 4-point Likert scale ranging from “strongly disagree” (= 0) to “strongly agree” (= 3). The item scores are summed to provide a total score (range: 0–27), and higher scores indicate greater stigma.
Depressive symptoms were measured using the Center for Epidemiologic Studies Depression (CES-D) Scale, developed to identify individuals who are at risk for depression (34). The scale consists of 20 items divided between four subscales: Depressive Mood, Somatic Symptoms, Interpersonal Relationships, and Positive Affect. Responses for the items are provided using a 4-point Likert scale ranging from “not at all” (= 0) to “almost daily” (= 3). The item scores are summed to provide a total score (range: 0–60). The CES-D has been widely used in china (35) and in the current study the scale demonstrated high internal consistency (Cronbach's α = 0.86).
Data analyses
Descriptive statistics comprised percentages, means, and standard deviations (SD). Student's t-test and analyses of variance were conducted to compare depressive symptoms scores between groups. Bivariate correlations were assessed using Pearson's correlation. The above analyses were conducted using SAS 9.4 software (SAS Institute Inc., Cary, NC). All differences were assessed using two-tailed tests, and the significance level was set at P < 0.05.
SEM was conducted using AMOS 17.0 software to assess the interrelationship between variables associated with depressive symptoms in patients with TB. In addition, the significance of direct and indirect effects was examined using a bias-corrected bootstrap 95% confidence interval (CI). The following fit indices were used to assess the overall model fit: root mean square error of approximation (RMSEA), comparative fit index (CFI), and Tucker-Lewis index (TLI). CFI and TLI values above 0.90 and RMSEA values below 0.08 indicated acceptable fit; CFI and TLI values above 0.95 and RMSEA values below 0.05 indicated good fit (36).
Results
Participants' characteristics
Participants' characteristics and their association with depressive symptoms are presented in Table 1. Participants mean age was 47.72 (SD = 17.06) years and most were aged 45 years or older. The mean score of depressive symptoms was 15.84 (SD = 8.26) and 48.00% of the participants had depressive symptoms. Being older, female, having low education, and a history of prior anti-TB treatment were associated with higher depressive symptoms scores.
Table 1.
Participants' characteristics and their associations with depressive symptom (n = 1342).
| Variables | All subject | Depressive symptoms | P-value | ||
|---|---|---|---|---|---|
| n | % | mean | SD | ||
| Age(Missing = 14) | 0.000 | ||||
| 11~29 | 283 | 21.31 | 13.79 | 7.85 | |
| 30~44 | 231 | 17.39 | 16.42 | 8.20 | |
| 45~59 | 440 | 33.13 | 16.04 | 8.00 | |
| 60+ | 374 | 28.16 | 16.84 | 8.52 | |
| Sex | 0.000 | ||||
| Male | 905 | 67.44 | 15.24 | 8.12 | |
| Female | 437 | 32.56 | 17.08 | 8.43 | |
| Education | 0.000 | ||||
| Primary or less | 574 | 42.77 | 17.50 | 8.50 | |
| Secondary | 540 | 40.24 | 15.30 | 7.98 | |
| High school or higher (above) | 228 | 16.99 | 13.00 | 7.36 | |
| History of prior anti-TB treatment | 0.025 | ||||
| No | 1174 | 87.48 | 15.65 | 8.16 | |
| Yes | 168 | 12.52 | 17.20 | 8.88 | |
SD, standard deviations; TB, tuberculosis.
Correlations of the variables, test of normality, and multicollinearity
Table 2 shows the means, SDs, and correlations among study variables. There were significant correlations between all study variables in the bivariate analysis. The correlation between family function and depressive symptoms was high compared to all the other combinations of correlations. Furthermore, skewness and kurtosis were used to examine the assumption of normality. The skewness of all study variables was within 1.90, and the absolute value of kurtosis was within 3.00; therefore, the results satisfy the assumption of a normal distribution (37). In addition, diagnostic checks for multicollinearity were conducted through variance inflation factors. In this study, the variance inflation factors ranged from 1.07 to 1.14, suggesting that there was no problem with multicollinearity (38).
Table 2.
Means, standard deviations, and correlations among study variables.
| Variables | Mean(SD) | Family function | Doctor-patient communication | Knowledge about TB | Stigma |
|---|---|---|---|---|---|
| Family function | 7.58 (2.39) | ||||
| Doctor-patient communication | 11.34 (1.24) | 0.22** | |||
| Knowledge about TB | 4.84 (2.02) | 0.25** | 0.16** | ||
| Stigma | 9.27 (4.25) | −0.23** | −0.15** | −0.16** | |
| Depressive symptoms | 15.84 (8.26) | −0.45** | −0.21** | −0.34** | 0.28** |
TB, tuberculosis; SD, standard deviations; All correlations were significant (p < 0.01);
p < 0.01.
Effect analysis of hypothesized model
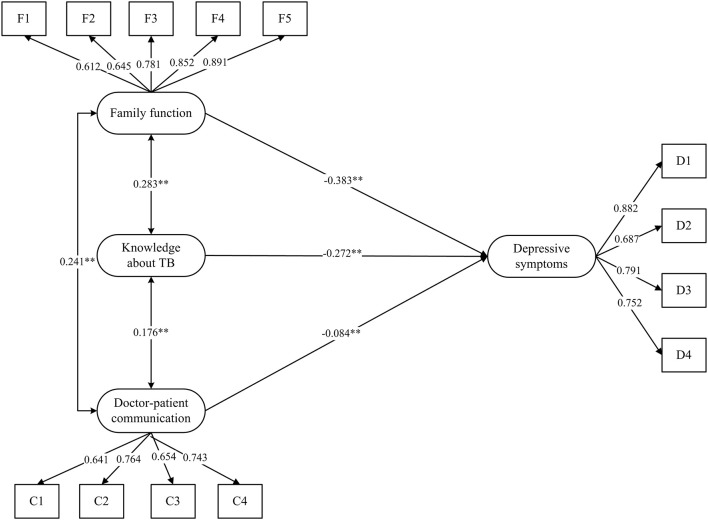
The first model without mediator
In the first model, the direct effects of the three variables (family function, doctor-patient communication, and knowledge about TB) on the dependent variable (depressive symptoms) were tested without a mediator using SEM. Figure 2 showed the first model with standardized path coefficients. We found that family function, doctor-patient communication, and knowledge about TB were negatively associated with depressive symptoms (standardized path coefficients were −0.38, −0.27, −0.08, respectively). The overall model fit indices of the first model were RMSEA = 0.039, CFI = 0.981, NFI = 0.972, TLI = 0.974, which all indicate that the model fit well.
Figure 2.
The first model without mediator. Estimates were obtained using full information maximum likelihood and all the coefficients in the figure were standardized. Five dimensions of the Family APGAR Index labeled F1,F2, F3, F4, and F5. Four questions of the doctor-patient communication Scale labeled C1, C2, C3, and C4. Four subscales of the Center for Epidemiologic Studies Depression (CES-D) Scale labeled D1, D2, D3, and D4. **p < 0.01.
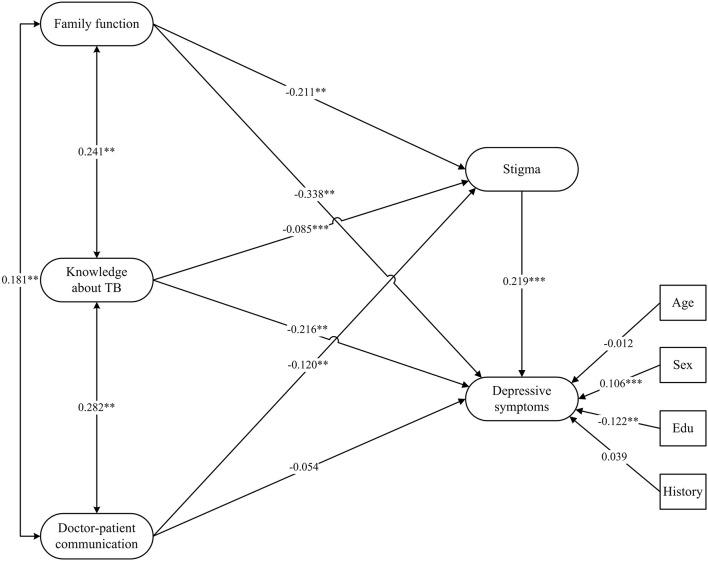
The final model
Figure 3 shows the final model with standardized path coefficients. The significance of all the effects were examined using a 95% bootstrapped confidence interval estimate. Age, sex, education, and history of prior anti-TB acted as covariates. The summary of the results are provided in Table 3. The overall model fit indices of the final model were RMSEA = 0.043, CFI = 0.956, NFI = 0.939, TLI = 0.946, which all indicate that the model fitted well.
Figure 3.
The final model. Estimates were obtained using full information maximum likelihood and all the coefficients in the figure were standardized; Age, Sex, Education, and History of prior anti-TB acted as covariates; Edu, Education; History, History of prior anti-TB (History); **p < 0.01; ***p < 0.001.
Table 3.
The results of hypothesized paths for the final model.
| Model paths | Standardized direct effects | 95% CI | Standardized indirect effects | 95% CI | ||
|---|---|---|---|---|---|---|
| Family function → Stigma | −0.211** | −0.276 | −0.135 | – | – | – |
| Doctor-patient communication → Stigma | −0.120** | −0.192 | −0.051 | – | – | – |
| Knowledge about TB → Stigma | −0.085** | −0.146 | −0.019 | – | – | – |
| Stigma → Depressive symptoms | 0.219** | 0.160 | 0.280 | – | – | – |
| Family function → Depressive symptoms | −0.338*** | −0.401 | −0.271 | −0.048** | −0.065 | −0.029 |
| Doctor-patient communication → Depressive symptoms | −0.054 | −0.118 | 0.007 | −0.028** | −0.045 | −0.011 |
| Knowledge about TB → Depressive symptoms | −0.216** | −0.273 | −0.162 | −0.021** | −0.034 | −0.005 |
TB, tuberculosis; CI, confidence interval; All of the effects were examined using a bias-corrected bootstrap 95% confidence interval; All of the indirect effects were significant (p < 0.01);
p < 0.01;
p < 0.001.
As can be seen in Table 3, the direct effect of family function, doctor-patient communication, and knowledge about TB on stigma were significant, which supported hypothesis 1. In addition, stigma exerted a direct effect on depressive symptoms, which supported hypothesis 2. The direct effect of family function and knowledge about TB on depressive symptoms were both significant; however, the direct effect of doctor-patient communication on depressive symptoms was non-significant. Further, the indirect effect of family function, doctor-patient communication, and knowledge about TB on depressive symptoms were significant; therefore, stigma partially mediated the effect of family function and knowledge about TB on depressive symptoms and fully mediated the effect of doctor-patient communication on depressive symptoms, which supported hypothesis 3.
Discussion
To the best of our knowledge, this was the first study to test the mediating effects of stigma on depressive symptoms in patients with TB. We examined the interrelationships between family function, doctor-patient communication, knowledge about TB, stigma, and depressive symptoms. More importantly, we elucidated the pathways linking family function, doctor-patient communication, and knowledge about TB to depressive symptoms and confirmed that the effect of those variables on depressive symptoms can be mediated by stigma, which supported our hypotheses.
Previous studies indicated that family function and doctor-patient communication were the most critical sources of social support for patients (39). Our results showed that family function and doctor-patient communication can also have an indirect negative effect on depression symptoms through stigma. Good family function and doctor-patient communication can increase patient life satisfaction and social confidence. Patients with family dysfunction and poor doctor-patient communication are more susceptible to being isolated and estranged. Because of these negative treatments, patients have developed negative feelings such as shame, guilt, discrimination, etc., which may result in a sense of stigma (40). Moreover, prominent levels of stigma was associated with psychological stress disorder, which can increase their risk of psychological problems, such as depression symptoms (20).
Knowledge about TB was another influencing factor that had both direct and indirect effects on depressive symptoms. This indirect negative effect was also achieved through stigma. Inadequate disease-related knowledge often represented the absence of a correct understanding of TB, leading to impaired confidence in treatment and diminished self-efficacy (41). Patients with low self-efficacy also experienced greater stigma (42), which contributed to their elevated levels of depression.
The present study is notable in that it disentangled the pathways between family function, doctor-patient communication, knowledge about TB, and depressive symptoms. Understanding these factors and their interrelationships offer an opportunity to effectively intervene in depression among patients with TB and interventions can be tailored to these specific pathways. Specifically, interventions aimed at reducing depression among patients with TB should focus on improving patients' family function, doctor-patient communication, and knowledge about TB. More importantly, the role of stigma should be understood and addressed. Given that stigma was not only a negative psychological reaction (18), but also mediated the effect of other factors on the mental health of patients with TB, interventions should be combined stigma-reduction measures, which is essential for promoting both physical and psychological well-being and, ultimately, better health outcomes. Specific stigma-reduction measures include routine screening for stigma of patients with TB, giving patients access to education on the concept of stigma, and offering techniques to deal with it.
This study had several limitations. First, analysis of cross-sectional data limits our ability to establish causal relationships among study variables. In addition, although this was one of the few studies to focus on the depressive symptoms of patients with TB in China, our sample only comprised patients with TB in a central province. Therefore, it is necessary to conduct more representative studies to determine the status of depressive symptoms among patients with TB across China.
Conclusion
In sum, we used SEM to explore the pathways linking family function, doctor-patient communication, and knowledge about TB to depressive symptoms and confirmed the mediating effect of stigma in the process. Awareness and management of depression in patients with TB may lead to better outcomes. There is an urgent need to develop effective interventions to prevent and decrease depression of patients. The current findings provide direction and information for depression interventions among patients with TB that improving family function and doctor-patient communication, increasing TB knowledge, and alleviating stigma may help to alleviate depressive symptoms among patients with TB. More research is needed to focus on psychological interventions for patients with TB and to assess the effectiveness of these interventions.
Author contributions
YG and XY designed the study. LQ, QY, and YT participated in the acquisition of data. LQ conducted the data analysis and drafted the manuscript. ZL, YG, and XY revised the manuscript. All authors reviewed the manuscript.
Conflict of interest statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors thank the Center for Disease Control and Prevention of Hubei Province for supporting. The authors also appreciate all study participants who have been involved and contributed to the procedure of data collection.
Footnotes
Funding. This project was funded by Young Scholars Fund of the Health and Family Planning Commission of Hubei Province (No.QJX2012-25) and Major Program of National Fund of Philosophy and Social Science (No.15ZDC037).
References
- 1.Naghavi M, Abajobir A, Abbafati C, Abbas K, Abd-Allah F, Abera S, et al. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet (2017) 390:1151–210. 10.1016/s0140-6736(17)32152-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization Global Tuberculosis Report 2017. Geneva: (2016). [Google Scholar]
- 3.Sweetland A, Oquendo M, Wickramaratne P, Weissman M, Wainberg M. Depression: a silent driver of the global tuberculosis epidemic. World psychiatry (2014) 13:325–6. 10.1002/wps.20134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Koyanagi A, Vancampfort D, Carvalho AF, DeVylder JE, Haro JM, Pizzol D, et al. Depression comorbid with tuberculosis and its impact on health status: cross-sectional analysis of community-based data from 48 low- and middle-income countries. BMC Med. (2017) 15:209. 10.1186/s12916-017-0975-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li Y, Ehiri J, Tang S, Li D, Bian Y, Lin H, et al. Factors associated with patient, and diagnostic delays in Chinese TB patients: a systematic review and meta-analysis. BMC Med. (2013) 11:156. 10.1186/1741-7015-11-156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Balaji AL, Abhishekh HA, Kumar NC, Mehta RM. Depression in patients with pulmonary tuberculosis in a tertiary care general hospital. Asian J Psychiatr. (2013) 6:251–2. 10.1016/j.ajp.2012.12.017 [DOI] [PubMed] [Google Scholar]
- 7.Duko B, Gebeyehu A, Ayano G. Prevalence and correlates of depression and anxiety among patients with tuberculosis at WolaitaSodo University Hospital and Sodo Health Center, WolaitaSodo, South Ethiopia, Cross sectional study. BMC psychiatry (2015) 15:214. 10.1186/s12888-015-0598-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Husain MO, Dearman SP, Chaudhry IB, Rizvi N, Waheed W. The relationship between anxiety, depression and illness perception in tberculosis patients in Pakistan. Clin Pract Epidemiol Ment Health (2008) 4:4. 10.1186/1745-0179-4-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kehbila J, Ekabe CJ, Aminde LN, Noubiap JJ, Fon PN, Monekosso GL. Prevalence and correlates of depressive symptoms in adult patients with pulmonary tuberculosis in the Southwest Region of Cameroon. Infect Dis Poverty (2016) 5:51. 10.1186/s40249-016-0145-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dos Santos AP, Lazzari TK, Silva DR. Health-related quality of life, depression and anxiety in hospitalized patients with tuberculosis. Tuberc Respir Dis (Seoul). (2017) 80:69–76. 10.4046/trd.2017.80.1.69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Masumoto S, Yamamoto T, Ohkado A, Yoshimatsu S, Querri AG, Kamiya Y. Prevalence and associated factors of depressive state among pulmonary tuberculosis patients in Manila, The Philippines. Int J Tuberc Lung Dis. (2014) 18:174–9. 10.5588/ijtld.13.0335 [DOI] [PubMed] [Google Scholar]
- 12.Shapiro-Mendoza CK. Commentary: Mediation and moderation analyses: a novel approach to exploring the complex pathways between maternal medical conditions, preterm birth and associated newborn morbidity risk. Int J Epidemiol. (2014) 43:815–7. 10.1093/ije/dyt285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Diiorio C, McCarty F, Depadilla L, Resnicow K, Holstad MM, Yeager K, et al. Adherence to antiretroviral medication regimens: a test of a psychosocial model. AIDS Behav. (2009) 13:10–22. 10.1007/s10461-007-9318-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nusair K, Hua N. Comparative assessment of structural equation modeling and multiple regression research methodologies: e-commerce context. Tourism Manage. (2010) 31:314–24. 10.1016/j.tourman.2009.03.010 [DOI] [Google Scholar]
- 15.Mota-Veloso I, Celeste RK, Fonseca CP, Soares MEC, Marques LS, Ramos-Jorge ML, et al. Effects of attention deficit hyperactivity disorder signs and socio-economic status on sleep bruxism and tooth wear among schoolchildren: structural equation modelling approach. Int J Paediatr Dent. (2017) 27:523–31. 10.1111/ipd.12291 [DOI] [PubMed] [Google Scholar]
- 16.Brunner J, Austin PC. Inflation of Type I error rate in multiple regression when independent variables are measured with error. Can J Stat. (2009) 37:33–46. 10.1002/cjs.10004 [DOI] [Google Scholar]
- 17.Goffman E. Stigma: Notes on the Management of Spoiled Identity. New York, NY: Simon & Schuster; (1963). [Google Scholar]
- 18.Juniarti N, Evans D. A qualitative review: the stigma of tuberculosis. J Clin Nurs. (2011) 20:1961–70. 10.1111/j.1365-2702.2010.03516.x [DOI] [PubMed] [Google Scholar]
- 19.Dhingra VK, Khan S. A sociological study on stigma among TB patients in Delhi. Indian J Tuberc. (2010) 57:12–8. [PubMed] [Google Scholar]
- 20.Lee LY, Tung HH, Chen SC, Fu CH. Perceived stigma and depression in initially diagnosed pulmonary tuberculosis patients. J Clin Nurs. (2017) 26:4813–21. 10.1111/jocn.13837 [DOI] [PubMed] [Google Scholar]
- 21.Cremers AL, de Laat MM, Kapata N, Gerrets R, Klipstein-Grobusch K, Grobusch MP. Assessing the consequences of stigma for tuberculosis patients in urban Zambia. PLoS ONE (2015) 10:e0119861. 10.1371/journal.pone.0119861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sun YH, Sun L, Wu HY, Zhang ZK, Wang B, Yu C, et al. Loneliness, social support and family function of people living with HIV/AIDS in Anhui rural area, China. Int J STD AIDS (2009) 20:255–8. 10.1258/ijsa.2008.008348 [DOI] [PubMed] [Google Scholar]
- 23.Anderson de Cuevas RM, Al-Sonboli N, Al-Aghbari N, Yassin MA, Cuevas LE, Theobald SJ. Barriers to completing TB diagnosis in Yemen: services should respond to patients' needs. PLoS ONE (2014) 9:e105194. 10.1371/journal.pone.0105194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jittimanee SX, Nateniyom S, Kittikraisak W, Burapat C, Akksilp S, Chumpathat N, et al. Social stigma and knowledge of tuberculosis and HIV among patients with both diseases in Thailand. PLoS ONE (2009) 4:e6360. 10.1371/journal.pone.0006360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Paz-Soldan VA, Alban RE, Jones CD, Oberhelman RA. The provision of and need for social support among adult and pediatric patients with tuberculosis in Lima, Peru: a qualitative study. BMC Health Serv Res. (2013) 13:290. 10.1186/1472-6963-13-290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Meulemans H, Mortelmans D, Liefooghe R, Mertens P, Zaidi SA, Solangi MF, et al. The limits to patient compliance with directly observed therapy for tuberculosis: a socio-medical study in Pakistan. Int J Health Plann Manage. (2002) 17:249–67. 10.1002/hpm.675 [DOI] [PubMed] [Google Scholar]
- 27.Stewart M, Brown JB, Donner A, McWhinney IR, Oates J, Weston WW, et al. The impact of patient-centered care on outcomes. J Fam Pract. (2000) 49:796–804. [PubMed] [Google Scholar]
- 28.Yin X, Yan S, Tong Y, Peng X, Yang T, Lu Z, et al. Status of tuberculosis-related stigma and associated factors: a cross-sectional study in central China. Trop Med Int Health (2018) 23:199–205. 10.1111/tmi.13017 [DOI] [PubMed] [Google Scholar]
- 29.Somma D, Thomas BE, Karim F, Kemp J, Arias N, Auer C, et al. Gender and socio-cultural determinants of TB-related stigma in Bangladesh, India, Malawi and Colombia. Int J Tuberc Lung Dis. (2008) 12:856–66. [PubMed] [Google Scholar]
- 30.Smilkstein G. The family APGAR: a proposal for a family function test and its use by physicians. J Fam Pract. (1978) 6:1231–9. [PubMed] [Google Scholar]
- 31.Nan H, Lee PH, Ni MY, Chan BH, Lam TH. Effects of depressive symptoms and family satisfaction on health related quality of life: the Hong Kong FAMILY study. PLoS ONE (2013) 8:e58436. 10.1371/journal.pone.0058436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wang Y. Report of the Fifth National Tuberculosis Epidemiological Survey. Beijing: Military Medical Science Press; (2011). [Google Scholar]
- 33.Yang TT. Development and evaluation of tuberculosis-related stigma scale. J Pubic Health Prev Med. (2016) 27:119–22. [Google Scholar]
- 34.Radloff LS. The CES-D Scale: a self-report depression scale for research in the general population. Appl Psychol Meas. (1977) 1:385–401. [Google Scholar]
- 35.Zhang J, Sun W, Kong Y, Wang C. Reliability and validity of the Center for Epidemiological Studies Depression Scale in 2 special adult samples from rural China. Compr Psychiatry (2012) 53:1243–51. 10.1016/j.comppsych.2012.03.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Modeling (1999) 6:1–55. 10.1080/10705519909540118 [DOI] [Google Scholar]
- 37.MacIntosh R. Program implementing Mardia's multivariate normality test for use in structural equation modeling with latent variables. Educ Psychol Meas. (1997) 57:357–9. [Google Scholar]
- 38.Grewal R, Cote JA, Baumgartner H. Multicollinearity and measurement error in structural equation models: implications for theory testing. Mark Sci. (2004) 23:519–29. 10.1287/mksc.1040.0070 [DOI] [Google Scholar]
- 39.Lee LT, Chen CJ, Suo J, Chen SC, Chen CY, Lin RS. Family factors affecting the outcome of tuberculosis treatment in Taiwan. J Formos Med Assoc. (1993) 92:1049–56. [PubMed] [Google Scholar]
- 40.Brown DC, Belue R, Airhihenbuwa CO. HIV and AIDS-related stigma in the context of family support and race in South Africa. Ethn Health (2010) 15:441–58. 10.1080/13557858.2010.486029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Buregyeya E, Kasasa S, Mitchell EM. Tuberculosis infection control knowledge and attitudes among health workers in Uganda: a cross-sectional study. BMC Infect Dis. (2016) 16:416. 10.1186/s12879-016-1740-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Li X, Huang L, Wang H, Fennie KP, He G, Williams AB. Stigma mediates the relationship between self-efficacy, medication adherence, and quality of life among people living with HIV/AIDS in China. AIDS Patient Care STDs (2011) 25:665–71. 10.1089/apc.2011.0174 [DOI] [PMC free article] [PubMed] [Google Scholar]