Abstract
Aortic thrombosis is rare, especially in non-atherosclerotic aortae. A 51-year-old woman presented with intermittent claudication in the right lower extremity. She was diagnosed as having peripheral artery disease on ultrasound. A computed tomography scan showed a large, sessile, aortic mural thrombus from the infrarenal abdominal aorta to the right common iliac artery. An arteriogram showed an abrupt occlusion of the right superficial femoral artery with collateral arteries. She had no risk factors for atherosclerosis. Interestingly, this occurred before early esophageal cancer progressed. Heparin was administered intravenously and later changed to warfarin. In the follow-up period, the thrombus disappeared, and her symptoms improved. A careful investigation for malignant disease is needed when aortic thrombus occurs in patients with no atherosclerosis risk factors.
<Learning objective: Aortic thrombosis is rare, especially in non-atherosclerotic aortae. A patient who presented with descending aortic thrombosis and peripheral embolism complicating early esophageal carcinoma is presented. Interestingly, this occurred before the cancer progressed. A careful investigation for malignant disease is needed when aortic thrombus occurs in patients with no atherosclerosis risk factors.>
Keywords: Aorta, Thrombus, Embolism, Cancer, Peripheral artery disease
Introduction
Venous thromboembolism is a frequent complication in cancer patients. Aortic thromboembolism is, however, extremely rare even in cancer patients. A case of descending aortic thrombosis and distal embolism preceding the progression of early esophageal carcinoma is reported. To the best of our knowledge, this is the first report of aortic thrombosis complicating early-stage cancer.
Case report
A 51-year-old Japanese woman presented with intermittent claudication (Fontaine IIa) in the right lower extremity. This symptom appeared and gradually worsened over 2 months prior to admission. She initially consulted an orthopedist and was diagnosed as having peripheral artery disease on ultrasound. She was referred for cardiology consultation. She had no risk factors for atherosclerosis. Her medical history revealed that she had undergone a gastrectomy for gastric cancer at the age of 42 years, and she was diagnosed as having early esophageal cancer one and half years earlier. The esophageal cancer was localized in situ at the cervical portion; the pathological diagnosis was squamous cell carcinoma in situ. Lymph node and other organ metastases were ruled out on imaging studies, and the clinical stage was determined to be early esophageal cancer. Because she rejected surgery, combination therapy including radiotherapy and chemotherapy with fluorouracil (5-FU) was performed until she attended the cardiology consultation.
Physical examination revealed that her right popliteal artery was not palpable, and her right calf was cold and pale, although the other extremities looked normal. The ankle to brachial pressure index was 0.74 on the right and 1.04 on the left. Laboratory examinations revealed a normal hemogram except for mild iron deficiency anemia (hemoglobin: 8.1 g/dl, mean corpuscular volume: 74.7 fl, ferritin: 3.2 ng/ml). Serum tests for hepatitis B and C viruses and syphilis were negative, and the activities of protein C and S were within normal limits. Auto-antibodies against nuclear antigen, double-stranded DNA, cardiolipin, and neutrophil cytoplasmic antigens were all negative. Prothrombin time, activated partial thromboplastin time, and fibrinogen concentration were normal. Only her D-dimer was elevated to 5.25 μg/ml, which suggested the possibility of thrombosis. On ultrasound examination, there was no evidence of deep vein thrombosis or intracardiac thrombus.
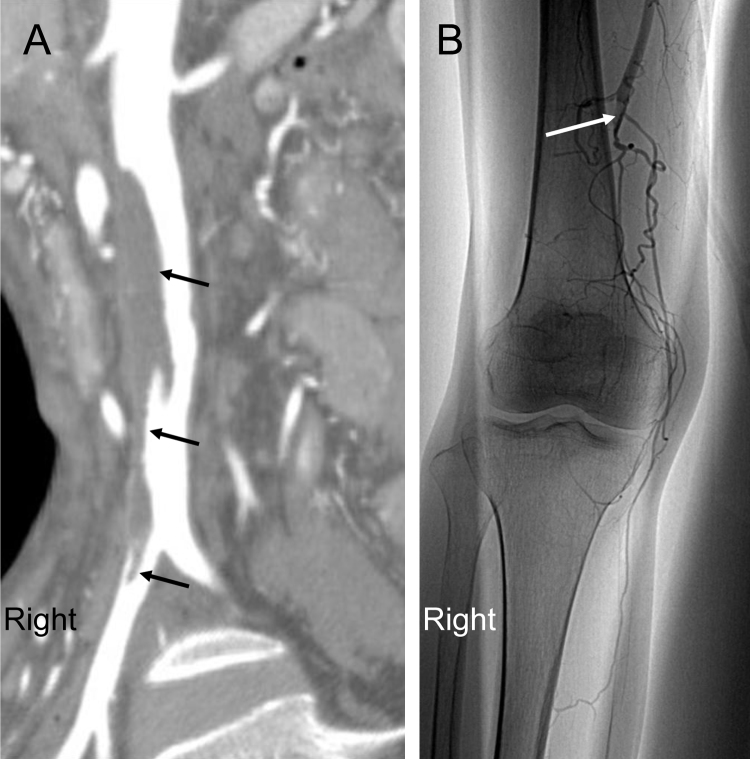
A computed tomography (CT) scan showed a large, sessile, aortic mural thrombus from the infrarenal abdominal aorta to the right common iliac artery (Fig. 1A), which was not recognized on the CT three months earlier. The previous radiation therapy was not considered to have reached near or to the nidus of the aortic thrombus. When hospitalized, she felt pain in her right great toe even at rest. Magnetic resonance imaging showed normal thickness and regular margin, suggesting no inflammatory changes in the vessel wall. There was no evidence of underlying atherosclerotic disease in the aorta on these imaging studies. An arteriogram showed an abrupt occlusion of the right superficial femoral artery with collateral arteries (Fig. 1B).
Fig. 1.
(A) Enhanced spiral computed tomography demonstrating a primary aortic mural thrombus (arrow). (B) Angiography demonstrating an abrupt occlusion of the right superficial femoral artery (arrow).
Heparin was administered intravenously and later changed to warfarin. A vascular surgery team was consulted, and it was decided to continue conservative therapy. One month later, the thrombus was dramatically decreased at CT imaging, and her symptoms improved.
On discharge, the endoscopy study showed that the esophageal mucosa was clear, and the pathological samples had no malignancy. Combination therapy was restarted for cancer, and she had no complaints for 6 months. However, endoscopy and biopsy examination revealed progression and recurrence of esophageal cancer at that time, with pathological evidence of high-grade neoplasia. Endoscopic submucosal dissection was performed safely, and she was discharged well. Interestingly, the latest systemic CT image, 3 months after starting anticoagulation therapy, confirmed that the aortic thrombus and distal artery obstruction had disappeared completely.
Discussion
A peripheral arterial emboligenic source can be identified in about 90% of patients on noninvasive imaging examinations. Around 85% of them originate in the heart. It has been estimated that 5% of embolisms originate in the aorta [1]. Aortic thrombosis is relatively common among patients with severe atherosclerosis, aneurysm, cardiovascular surgery, trauma, uncontrolled diabetes mellitus, active tuberculosis, and aortitis [1], [2], [3]. Aortic thrombosis is rare, however, in an apparently healthy vascular segment. In these cases, aortic thrombosis may be related to identifiable hypercoagulable states or to factors predisposing to the formation of clots, such as sepsis, polycythemia, disseminated intravascular coagulation, autoimmune disease, and myeloid leukemia [2], [3], [4]. A hypercoagulable state related to cancer is a well-known risk factor for venous thrombosis [5]. On the other hand, there are fewer data on arterial thrombosis than for venous thrombosis. Nevertheless, thrombosis in arteries has long been recognized [6], [7]. Although the correct mechanisms remain unclear, it is known that tumor cells are directly prothrombotic and normal host cells may be also as a second response against the cancer cells [7]. Additionally increased levels of coagulation factors, blood turbulence, coexisting inflammatory diseases, use of growth factors, chemotherapy, and irradiation therapy may all induce thrombosis. One possible mechanism is endothelial damage with the loss of its natural anticoagulant nature and acquisition of a procoagulant profile [7]. The current case is a rare case of aortic thrombosis complicating esophageal cancer in a patient 1 year and 4 months after radiation and chemotherapy without apparent recurrence and metastasis.
There is a general consensus that these patients should receive anticoagulation therapy [2]. Surgical thrombectomy should be performed for selected cases of recurrent embolism or persistent thrombus despite proper anticoagulation. Patients with a threatened extremity should undergo emergency surgical revascularization to resolve the symptoms of acute distal embolization, in addition to perioperative intravenous heparin therapy with conversion to oral anticoagulation, so that primary aortic fibrinolysis can occur. Indeed, anticoagulant therapy decreased the size of the aortic thrombus in the present case.
The risk of thrombosis due to cancer is compounded by the effects of chemotherapy and other treatments. Since the patient had received 5-FU treatment when complaining of intermittent claudication, a possible effect of chemotherapy on the occurrence of her arterial thrombosis cannot be completely excluded. However, no case of aortic thrombosis in a patient with even advanced esophageal cancer with or without chemotherapy has been reported. To the best of our knowledge, this is the first report of aortic thrombosis complicating esophageal carcinoma. The clinical stage was considered to be early cancer. Interestingly, progression of the cancer was not noted until 6 months after the aortic thrombus was found, suggesting that the hypercoagulable state may have been caused by the proliferative activity of the cancer.
In conclusion, a thorough evaluation for malignant disease should be performed in patients with an aortic thrombus and embolism in non-atherosclerotic aortae.
References
- 1.Cañadas V., Vilacosta I., Luaces M., Bustos A., Ferreirós J., Aragoncillo P., Pérez de Isla L., Rodríguez E. Thrombosis of an apparently normal thoracic aorta and arterial embolism. Rev Esp Cardiol. 2008;61:196–200. [PubMed] [Google Scholar]
- 2.Hahn T.L., Dalsing M.C., Sawchuk A.P., Cikrit D.F., Lalka S.G. Primary aortic mural thrombus: presentation and treatment. Ann Vasc Surg. 1999;13:52–59. doi: 10.1007/s100169900220. [DOI] [PubMed] [Google Scholar]
- 3.Vaideeswar P., Deshpande J.R. Non-atherosclerotic aorto-arterial thrombosis: a study of 30 cases at autopsy. J Postgrad Med. 2001;47:8–14. [PubMed] [Google Scholar]
- 4.Zhang L., Hollensead S., Parker J.C., Jr. Extensive aortic thromboembolism due to acquired hypercoagulable state: an autopsy case report. Arch Pathol Lab Med. 2005;129:247–250. doi: 10.5858/2005-129-247-EATDTA. [DOI] [PubMed] [Google Scholar]
- 5.Zwicker J.I., Furie B.C., Furie B. Cancer-associated thrombosis. Crit Rev Oncol Hematol. 2007;62:126–136. doi: 10.1016/j.critrevonc.2007.01.001. [DOI] [PubMed] [Google Scholar]
- 6.Poiree S., Monnier-Cholley L., Tubiana J.M., Arrive L. Acute abdominal aortic thrombosis in cancer patients. Abdom Imaging. 2004;29:511–513. doi: 10.1007/s00261-003-0144-5. [DOI] [PubMed] [Google Scholar]
- 7.Blann A.D., Dunmore S. Arterial and venous thrombosis in cancer patients. Cardiol Res Pract. 2011;2011:394740. doi: 10.4061/2011/394740. [DOI] [PMC free article] [PubMed] [Google Scholar]