Abstract
Survival into adulthood is now routine for patients with congenital heart disease (CHD). Adult cardiology practices increasingly encounter these patients, however, are often challenged by the complexity of the cardiac lesions, prior surgical interventions, and associated conditions. We describe a case of a 64-year-old woman with history of CHD and multiple operations, including surgical aortic valve replacement, who presented for routine evaluation. During transthoracic echocardiogram she was believed to have idiopathic severe pulmonary hypertension (tricuspid regurgitation velocity of 4.6 m/s) and a ventricular septal defect (VSD). Consequently, she was referred to a pediatric CHD center. On noninvasive evaluation it became clear that a flow jet through a Gerbode defect, from left ventricle to right atrium, had led to the initial misdiagnosis of severe pulmonary hypertension. The patient was reassured that the VSD was small, restrictive, and that the pulmonary pressures were normal.
<Learning objective: Recognition of a left ventricle-to-right atrial shunt (Gerbode defect) is challenging in the adult congenital heart patient. However, this diagnosis can be made with a noninvasive imaging strategy in the context of a high clinical suspicion: A combination of transthoracic echocardiography and cardiac MRI findings of a high velocity “tricuspid regurgitation jet” but normal appearing right ventricular pressures in someone with prior subaortic membrane and aortic valve surgery led to the diagnosis of a Gerbode defect in our patient.>.
Keywords: Ventricular septal defect, Pulmonary hypertension, Echocardiography, Congenital heart disease, Shunt
Case report
A 64-year-old Hispanic woman with a remote history of congenital heart disease (CHD) presents to an adult cardiologist for evaluation and treatment. At age 9, she required open-heart surgery, presumably for sub-aortic membrane requiring surgical re-exploration during the same hospitalization in Puerto Rico. Subsequently, at 26 years of age, she underwent redo open heart surgery in New York. Finally, at age 48 she underwent surgical aortic valve replacement with a St. Jude metallic valve in New Jersey. She reported no major cardiovascular complaints during pregnancy and childbirth. Clinically, she now complains of longstanding atypical chest pain with mild exertion. Physical examination was remarkable for a grade 3/6 systolic murmur and normal point of maximal impulse. Echocardiographic report described the presence of a ventricular septal defect (VSD) and severe pulmonary hypertension, derived from a tricuspid regurgitation velocity jet of 4.6 m/s. Because of discrepancy between her symptoms and echocardiographic findings, she was referred to a CHD center for further evaluation.
Repeat echocardiogram demonstrated a small, pressure-restrictive membranous VSD associated with a left ventricle-to-right atrial shunt (Fig. 1, Fig. 2). The maximum instantaneous gradient through the defect was approximately 130 mmHg (Fig. 3). Systolic flattening of the septal wall was not noted, suggestive that the right ventricular pressure was less than half left ventricular pressure. Cardiac magnetic resonance imaging (MRI) confirmed normal biventricular size and function, normal septal position, and the absence of right ventricular hypertrophy with a mass index of 16.8 g/m2 and mass:volume ratio of 0.16. By flow analysis through both the aorta and main pulmonary artery, and also by comparison of ventricular stroke volumes there was negligible left-to-right shunting (estimated Qp:Qs ratio of <1.1). The left ventricle-to-right atrial shunt flow jet could not be well visualized because of susceptibility artifact from the adjacent metallic prosthetic aortic valve (Fig. 4).
Fig. 1.
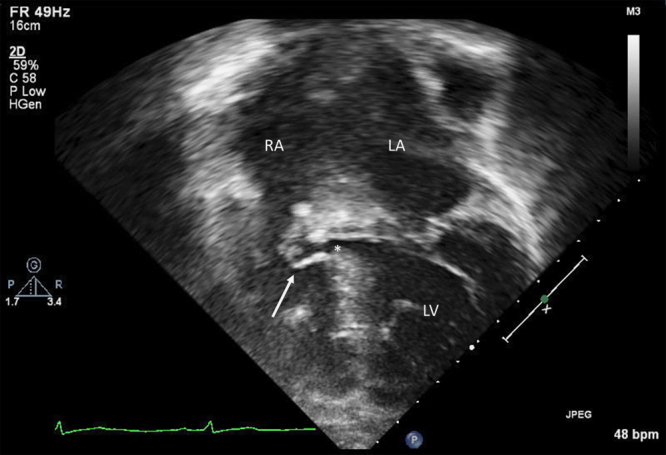
Apical four chamber view: note the complex pouch of accessory tricuspid valve tissue (white arrow) partially closing the ventricular septal defect (*). RA, right atrium; LA, left atrium; LV, left ventricle.
Fig. 2.
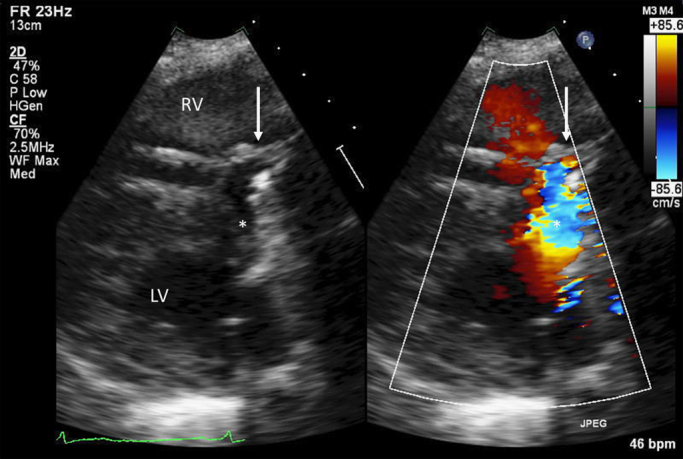
Parasternal long axis view with 2D and color Doppler interrogation showing the complex ventricular shunt beginning in the left ventricle (*), and directed by the aneurysmal pouch (white arrow) into the right atrium. RV, right ventricle; LV, left ventricle.
Fig. 3.
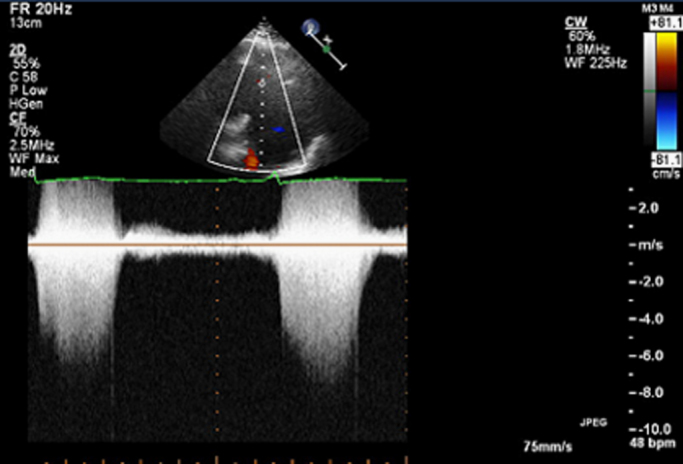
Continuous wave Doppler waveform of the high velocity jet (approximately 5.5 m/s) through the left-ventricle-to-right atrial defect that was initially misinterpreted as a high velocity tricuspid regurgitant jet. Note that it is directed toward the right atrium, in the same orientation as a typical tricuspid regurgitation jet.
Fig. 4.
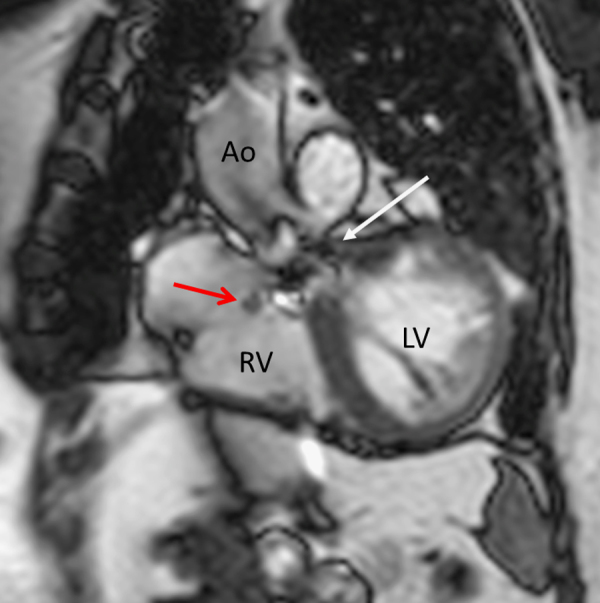
Cardiac magnetic resonance imaging cine steady-state free precession image in an oblique coronal view. The white arrow illustrates the artifact from the prosthetic aortic valve, which obscures assessment of the dark dephasing flow jet from the Gerbode defect (red arrow). RV, right ventricle; LV, left ventricle; Ao, ascending aorta.
The patient was diagnosed with a hemodynamically insignificant Gerbode-type VSD, which was initially mistaken as a high velocity tricuspid regurgitant jet and severe pulmonary hypertension. The patient was reassured that the defect would likely never require closure, nor any specific restrictions, and that the risk for developing pulmonary hypertension was low and similar to that of the general population.
Discussion
Dr Gerbode first described congenital left ventricle-to-right atrial shunt through a defect in the membranous septum in 1958 [1]. This congenital lesion has remained the least common form of VSD over the past 50 years; however, there have also been reports of acquired Gerbode defects occurring as a consequence of infective endocarditis [2], or as a complication of cardiothoracic surgery [3].
A high index of suspicion for a Gerbode defect should be present when a high velocity “tricuspid regurgitation” jet is seen, in the absence of any other clinical or echocardiographic features of pulmonary hypertension. A left ventricle-to-right atrial shunt is typically very difficult to image directly by 2-dimensional and color Doppler interrogation as it is located behind the frequently aneurysmal septal leaflet of the tricuspid valve (Fig. 1, Fig. 2), and the direction of the shunt exactly parallels that of tricuspid regurgitation. Cardiac MRI may be used as a complementary noninvasive diagnostic tool. In our case we confirmed that there was no significant residual intracardiac shunt. And perhaps more importantly, that this patient did not have significant pulmonary hypertension as was initially suspected; a right ventricular mass index of <20 g/m2 by MRI is more reliable than echocardiography for excluding pulmonary hypertension [4]. Had there still been questions regarding the diagnosis, the superior image quality of transesophageal echocardiography can often delineate the location of the shunt. Alternatively, had our patient undergone cardiac catheterization (as was initially suggested), she would have predictably shown normal pulmonary arterial pressures with a small oxygen saturation step-up at the level of the right ventricle. Left ventriculography in left anterior oblique/cranial angulation would have revealed her Gerbode defect with contrast opacification of the right atrium from the left ventricle. However, comprehensive noninvasive evaluation at a center with congenital heart expertise obviated the need for invasive catheterization by correctly identifying her lesion and clearing the patient of the initial diagnosis of pulmonary hypertension. Fortunately for her, small, pressure restrictive Gerbode defects have no consequence to cardiac function or physiology as there is minimal left-to-right shunting and thus rarely require intervention or cardiac restrictions.
Conclusion
Survival into adulthood after repair of congenital heart defects has become the rule, rather than the exception in 2012. This necessitates an understanding of congenital heart lesions and late post-surgical complications in the adult cardiology population, as well as a close relationship with a center experienced in the management of these patients. As in this case, noninvasive diagnostic evaluation, consisting of comprehensive transthoracic echocardiography, complemented by cardiac MRI may often be sufficient to provide an accurate assessment of post-surgical congenital cardiac anatomy and physiology, and obviate the need for invasive testing.
Conflict of interest
RG, RG, and RJ have no conflicts of interest or associations to disclose in regards to this case report.
References
- 1.Gerbode F., Hultgren H., Melrose D., Osborn J. Syndrome of left ventricular-right atrial shunt; successful surgical repair of defect in five cases, with observation of bradycardia on closure. Ann Surg. 1958;148:433–446. doi: 10.1097/00000658-195809000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Xhabija N., Prifti E., Allajbeu I., Sula F. Gerbode defect following endocarditis and misinterpreted as severe pulmonary arterial hypertension. Cardiovasc Ultrasound. 2010;8:44. doi: 10.1186/1476-7120-8-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moaref A.R., Aslani A., Zamirian M., Sharifkazemi M.B. Left ventricular to right atrial communication (Gerbode-type defect) after mitral valve replacement. J Am Soc Echocardiogr. 2008;21:408. doi: 10.1016/j.echo.2007.08.035. pp e1–e2. [DOI] [PubMed] [Google Scholar]
- 4.Swift A.J., Rajaram S., Condliffe R., Capener D., Hurdman J., Elliot C.A., Wild J.M., Kiely D.G. Diagnostic accuracy of cardiovascular magnetic resonance of right ventricular morphology and function in the assessment of suspected pulmonary hypertension. J Cardiovasc Magn Reson. 2012;14:40. doi: 10.1186/1532-429X-14-40. [DOI] [PMC free article] [PubMed] [Google Scholar]


