Abstract
Acute coronary syndrome due to antithrombin III deficiency has been rarely reported. We describe a case of a 30-year-old woman, with no conventional risk factors, presenting with an extensive myocardial infarction. Coronary angiography revealed a simultaneous thrombosis of the left anterior descending artery and the circumflex artery, thrombus aspiration was performed, and the result of percutaneous coronary intervention was satisfactory. The biological examinations identified an antithrombin III deficiency, and long-term anticoagulation was indicated.
<Learning objective: Acute coronary syndrome in young adults is rare. The coronary event should evoke the diagnosis of hypercoagulable states. Early recognition and appropriate treatment may prevent recurrences.>
Keywords: Acute coronary syndrome, Young adult, Antithrombin III deficiency
Introduction
Acute coronary syndrome in young adults is rare, the pathophysiology is different, traditional risk factors are usually missing, conditions leading to premature atherosclerosis or hypercoagulable states must be investigated. We report the case of a young woman, who presented with an extensive myocardial infarction due to simultaneous thrombosis of two coronary arteries; the biological examinations identified an antithrombin III deficiency.
Case report
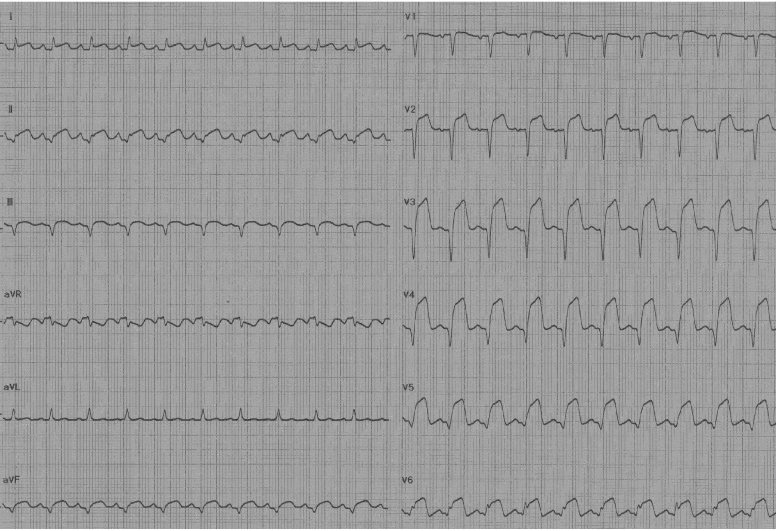
We report the case of a 30-year-old woman, with no cardiovascular risk factors, with a history of oral contraception, who presented to the emergency department with sudden onset of a severe chest pain radiating to both arms. Physical examination showed a pale patient with profuse sweating, the blood pressure was 130/70 mmHg, the pulse was 110 beats per minute, cardiac examination was normal, the lungs were clear. The electrocardiogram showed ST segment elevation in anterior and inferior leads with Q waves (Fig. 1). The echocardiography showed anterior, inferior, septal, and apicalakinesis with an ejection fraction of 40%. Urgent coronary angiography performed 5 h after symptoms onset revealed ostial occlusion of the left anterior descending artery (LAD), intracoronary thrombus was present in both LAD artery and proximal left circumflex artery with no evidence of atherosclerosis (Fig. 2). The right coronary artery was normal. We performed a thrombus aspiration without balloon angioplasty; an important improvement was observed with thrombolysis in myocardial infarction 3 flow in both arteries (Fig. 3). After the percutaneous coronary intervention, the patient became stable without chest pain.
Fig. 1.
ST segment elevation in anterior and inferior leads with Q waves.
Fig. 2.
Coronary angiography revealed a total thrombotic occlusion of the left anterior descending coronary artery with thrombus in left circumflex artery.
Fig. 3.
Successful thrombus aspiration of the left anterior descending coronary artery.
Laboratory data showed an elevated level of C-reactive protein (72 mg/L), fibrinogen level was normal, cardiac enzyme peaks were 50 ng/ml for troponin and 1867 UI/L for creatine kinase. The transaminases were elevated (280 UI/L for alanine transaminase and 345 UI/L for aspartate transaminase); the other parameters of the liver function were within the normal limits. The lipid profile was normal. The coagulation tests revealed a decrease in antithrombin III activity to 19% (normal range from 80% to 120%), the activity of protein C was 81% (normal range from 70% to 130%), the activity of protein S was 72% (normal range from 70% to 140%), and the antiphospholipid level was normal. The genetic tests found a normal variant of factor V Leiden and prothrombin gene.
Further radiological investigations including abdominal ultrasound, a lower-limb Doppler ultrasound and a transesophageal echocardiography were normal.
The patient was discharged after five days, her therapy included carvedilol, captopril, simvastatin, clopidogrel, aspirin, and warfarin with an international normalized ratio of 2.
Six months later, the patient remains asymptomatic, the ejection fraction rose to 50% and the antithrombin III activity became normal after oral contraception discontinuation.
Discussion
Acute coronary syndrome in young adults is an uncommon condition; only 2–8% of acute myocardial infarction subjects are under 40 years’ old [1], [2]. Males are typically more affected, females account for only 6% in this age group [3].
The mean cause of acute coronary syndrome in the young is atherosclerosis; numerous factors can lead to premature and accelerating process (insulin resistance, familial lipid disorder, human immunodeficiency virus infection) [4]. Our patient had no risk factors.
Acute coronary syndromes may have non-atherosclerotic etiologies: congenital coronary artery anomalies, spontaneous coronary artery dissection, vasospasm, illicit drug use, and hypercoagulable states (nephrotic syndrome, antiphospholipid syndrome, protein S, and antithrombin III deficiency). In the case of our patient, laboratory data revealed a decrease in antithrombin III activity [4], [5].
Antithrombin III is a physiological inhibitor of coagulation cascade; its decrease is a well known risk factor for thrombosis. Antithrombin III deficiency can be congenital or acquired, many pathological conditions can be associated with a decrease in antithrombin III activity (liver cirrhosis, gastrointestinal disease, disseminated intravascular coagulation, oral contraception) [6]. Our patient reported a two-week history of oral contraception.
In 1970, Von Kaulla et al. described the first case of antithrombin III deficiency induced by oral contraceptives [7], an average reduction of 9% was observed in another study [8]. The contraception induced antithrombin III deficiency due to estrogen administration. Fortin et al. described a case of a myocardial infarction in an estrogen-dependent genetic male transsexual with an antithrombin III deficiency [9]. To the authors’ knowledge, this is the second case of myocardial infarction due to estrogen-induced antithrombin III deficiency.
Antithrombin III deficiency is usually associated with venous thrombosis, arterial thrombosis is rare. In the present case, the patient had no history of venous thromboembolism; the coronary thrombosis was the first manifestation of the deficiency. To our knowledge, only few cases of coronary thrombosis associated with antithrombin III deficiency have been reported [10], [11], [12], [13].
Limited studies have focused on the management of acute coronary syndrome in the young, but percutaneous coronary intervention gives good results. In hypercoagulable states, long-term anticoagulation should be considered [14].
Acute coronary syndrome in young adults is unusual and the coronary event may be the manifestation of underlying disease. Biological investigations must be performed, and depending on etiology, an appropriate treatment must be prescribed to prevent recurrence.
Acknowledgment
The authors do not report any conflict of interest regarding this work.
References
- 1.Fullhaas J.U., Rickenbacher P., Pifisterer M., Ritz R. Longterm prognosis of young patients after myocardial infarction in the thrombolytic era. Clin Cardiol. 1997;20:993–998. doi: 10.1002/clc.4960201204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Imazio M., Bobbio M., Bergerone S., Barlera S., Maggioni A.P. Clinical and epidemiological characteristics of juvenilemyocardial infarction in Italy: the GISSI experience. G Ital Cardiol. 1998;28:505–512. [PubMed] [Google Scholar]
- 3.Teixeira M., Santos Mendes I., Martins L. Acute coronary syndrome in young adults. Rev Port Cardiol. 2010;29:947–955. [PubMed] [Google Scholar]
- 4.Aguiar C. Acute coronary syndrome in younger patients: an avoidable atherothrombotic complication. Rev Port Cardiol. 2010;29:957–960. [PubMed] [Google Scholar]
- 5.Cengel A., Tanindi A. Myocardial infarction in young. Postgrad Med J. 2009;55:305–313. doi: 10.4103/0022-3859.58944. [DOI] [PubMed] [Google Scholar]
- 6.Büller H.R., ten Cate J.W. Acquired antithrombin III deficiency: laboratory diagnosis, incidence, clinical implications, and treatment with antithrombin III concentrate. Am J Med. 1989;87:44S–48S. doi: 10.1016/0002-9343(89)80531-5. [DOI] [PubMed] [Google Scholar]
- 7.Von Kaulla E., Von Kaulla K.N. Oral contraceptives and low antithrombin-III activity. Lancet. 1970;295:36. doi: 10.1016/s0140-6736(70)90543-x. [DOI] [PubMed] [Google Scholar]
- 8.Weerknk G.H., Kahle L.H., Lampring R.I., ten Cate J.W., Treffers P.E. Antithrombin III inoral contraceptive users and during normotensive pregnancy. Acta Obstet Gynecol Stand. 1984;63:57–61. doi: 10.3109/00016348409156274. [DOI] [PubMed] [Google Scholar]
- 9.Fortin C.J., Klein T., Messmore H.L., O’Connell J.B. Myocardial infarction and severe thromboembolic complications. As seen in an estrogen-dependent transsexual. Arch Intern Med. 1984;144:1082–1083. [PubMed] [Google Scholar]
- 10.Peeters S., Vandenplas Y., Jochmans K., Bougatef A., De Waele M., De Wolf D. Myocardial infarction in a neonate with hereditary antithrombin III deficiency. Acta Paediatr. 1993;82:610–613. doi: 10.1111/j.1651-2227.1993.tb12770.x. [DOI] [PubMed] [Google Scholar]
- 11.Loubser P.G., MacCarthy J.J., Attar M. Coronary thrombosis associated with antithrombin III deficiency. J Cardiothorac Vasc Anesth. 1997;11:756–759. doi: 10.1016/s1053-0770(97)90171-3. [DOI] [PubMed] [Google Scholar]
- 12.Peovska I., Maksimovic J., Kalpak O., Pejkov H., Bosevski M. Recurrent myocardial infarction in a young football player with antithrombin III deficiency. Cardiol J. 2008;15:463–466. [PubMed] [Google Scholar]
- 13.Tu C.M., Hsueg C.H., Chu K.M., Cheng S.M., Tsao T.P. Simultaneous thromboses of double coronary arteries in a young male with antithrombin III deficiency. Am J Emerg Med. 2009;27(1169):e3–e6. doi: 10.1016/j.ajem.2008.12.006. [DOI] [PubMed] [Google Scholar]
- 14.Osula S., Bell G.M., Hornung R.S. Acute myocardial infarction in young adults: causes and management. Postgrad Med. 2002;78:27–30. doi: 10.1136/pmj.78.915.27. [DOI] [PMC free article] [PubMed] [Google Scholar]