Abstract
In this case report we describe a case of the Kounis–Zavras syndrome (coincidental occurrence of chest pain and allergic reactions accompanied by clinical and laboratory findings of cardiac ischemia). A 34-year-old woman presented to the emergency unit with severe chest pain from 2 h. She reported a medical history of asthma. On arrival, her heart rate was 125 beats/min and her systolic blood pressure (SBP) was 70 mmHg. A repeated electrocardiogram displayed dynamic changes with ST-segment elevation in D1-aVL leads and ST-segment depression in infero-posterior leads. Two episodes of ventricular fibrillation were observed. The coronary artery angiography showed multivessel coronary vasospasms. Intracoronary nitroglycerin was used to alleviate the coronary vasospasms. Contemporaneously, the patient's husband came to the hospital reporting a history of ketorolac consumption some hours before the onset of the acute event for headache symptoms. This crucial information permitted us to suppose it was a case of allergic myocardial infarction during anaphylactic shock due to ketorolac. Betametasone, chlorphenamine, and ranitidine were administered and progressively a full recovery of SBP and of clinical status was observed.
<Learning objective: Allergic myocardial infarction (Kounis-Zavras syndrome) is a complex acute coronary syndrome which requires rapid treatment decisions. Most of the information on this syndrome comes from case reports or small case series. It should be considered in young, healthy patients when they develop acute coronary syndrome after administration of potentially allergic agent. The treatment should both dilate coronary vessels and suppress the allergic reaction (steroids, antihistamines, fluid resuscitation, oxygen, nitrates, calcium channel blockers).>
Keywords: Myocardial infarction, Kounis–Zavras syndrome, Shock, Allergic reaction, Coronary vasospasm
Introduction
The Kounis–Zavras syndrome, also called allergic angina pectoris, is defined as the coincidental occurrence of chest pain and allergic reactions accompanied by clinical and laboratory findings of classical angina pectoris caused by inflammatory mediators released during the allergic insult [1], [2]. This syndrome encompasses the whole clinical spectrum of acute myocardial ischemia, from angina pectoris to acute myocardial infarction (MI), which occurs in coincidence with an “allergic” (hypersensitivity, anaphylactic, or anaphylactoid) reaction [1], [2]. Cardiac symptoms are due to coronary vasospasm [1], [2]. Angina is the more frequent clinical presentation, whereas MI is relatively rare. We report a case of allergic MI that was complicated by malignant ventricular arrhythmias and cardiogenic shock at clinical presentation.
Case report
A 34-year-old woman presented to the emergency unit with severe chest pain from 2 h. She was accompanied by a friend. She reported a medical history of asthma (actually in medical treatment with inhaled corticosteroid, budesonide 800 μg die, and β-agonist, formoterol 24 μg die). Asthma was well controlled and in the previous months no acute exacerbations were reported. She had a 4 month old baby to whom she had given birth without any complications. Five days before the hospital admission, she had been taking cabergoline (1 mg) so as to interrupt breast-feeding. Her pain was squeezing, substernal, and worsening. On arrival, her heart rate (HR) was 125 beats/min, and her systolic blood pressure (SBP) was 70 mmHg. She was afebrile. She had bilateral lung crackles and her chest radiograph revealed a bilateral pulmonary edema. Radial and femoral pulses were present, but very weak. A repeated electrocardiogram displayed dynamic changes with ST-segment elevation in D1-aVL leads and ST-segment depression in infero-posterior leads (Fig. 1). These alterations were dynamic with significant changes related to pain status. An echocardiogram was immediately performed. The exam showed a left ventricle not dilated and hypokinesia of apex. The left ventricle ejection fraction showed a minimal reduction (LVEF = 50%). No pericardial effusion was present. The general clinical picture did not indicate pericarditis or myocarditis or peripartum cardiomyopathy. In addition, the observed LVEF was not in agreement with a cardiogenic shock condition. A computed tomography (CT) with contrast media was performed to exclude aortic dissection and pulmonary embolism. The exam was absolutely negative. 15 min after the CT, cardiac arrest due to ventricular fibrillation (VF) was observed. Sinus rhythm recovered with DC shock (150 J). The patient was still suffering from continued chest pains, her vital parameters were HR 130 beats/min and SBP 65 mmHg. Suspecting spontaneous coronary arteries dissection, an emergency cardiac catheterization was done.
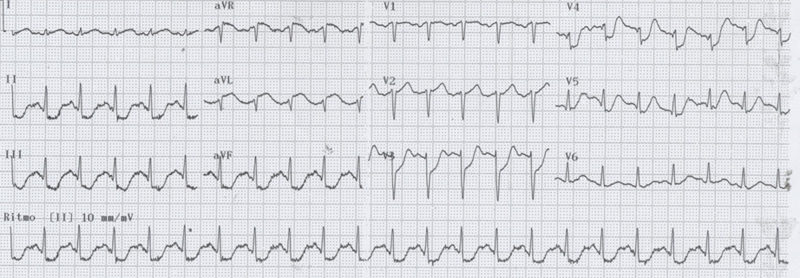
Fig. 1.
Electrocardiogram during chest pain.
Unexpectedly, the coronary artery angiography did not disclose any images suggesting a coronary dissection, but instead for multivessel coronary vasospasms (Fig. 2). During the diagnostic exam, a second episode of VF was observed. Interestingly, artery spasms were not only limited to coronary arteries. We observed also a spasm of femoral artery embracing 6 French arterial sheath (Fig. 3A). In spite of marked hypotension, intracoronary nitroglycerin was used to alleviate the coronary vasospasms. Contemporaneously, the patient's husband came to the hospital reporting important and crucial anamnestic information. First, the patient had a history of anaphylactic shock by aspirin (12 years previously). Second, some hours before the onset of symptoms and of the chest pain the patient consumed ketorolac for an important and prolonged episode of headache. Both these findings permitted us to suppose a case of allergic MI during anaphylactic shock due to ketorolac. Betametasone (4 mg), chlorphenamine (10 mg), and ranitidine (56 mg) were administered and progressively a recovery of SBP was observed. At coronary artery angiography, coronary vasospasm was resolved (Fig. 3B). Intravascular ultrasonography (IVUS) confirmed the absence of coronary dissection and of atherosclerotic plaques. During the following days, cardiac markers confirmed myocardial necrosis (creatine kinase-MB peak 18.1 ng/dl, normal value <5 ng/dl; troponin I peak 0.16, normal value <0.015). Electrocardiogram at discharge did not show q wave. Moreover, a history of nasal polyps emerged configuring the Samter–Beer triad (asthma, aspirin sensitivity, nasal polyps). The subsequent hospitalization was uneventful. She had been treated with verapamil (160 mg die), ranitidine (300 mg die), chlorphenamine (4 mg die), and inhaled corticosteroids (budesonide 1600 μg die). At discharge, apex hypokinesia persisted and LVEF = 50%.
Fig. 2.
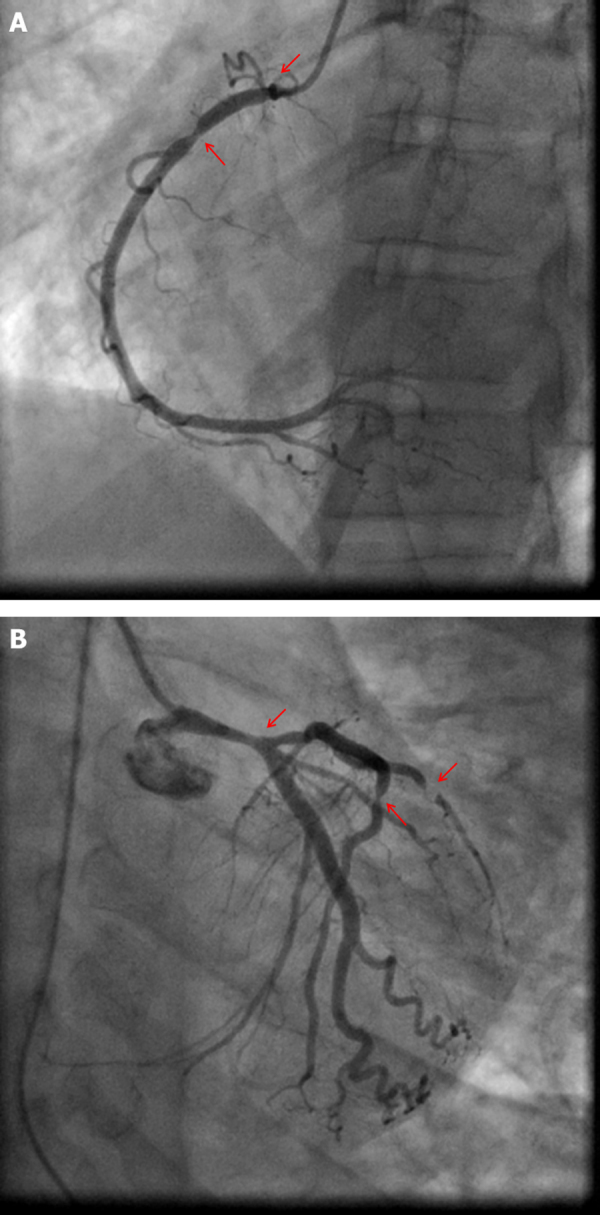
Coronary artery angiography showing multivessel vasospasms. (A) Right coronary artery with vasospasm in the ostium and in the proximal portion (red arrow). (B) Left coronary artery with vasospasm in the left main, in the proximal and distal part of left anterior descending, and in the first diagonal.
Fig. 3.
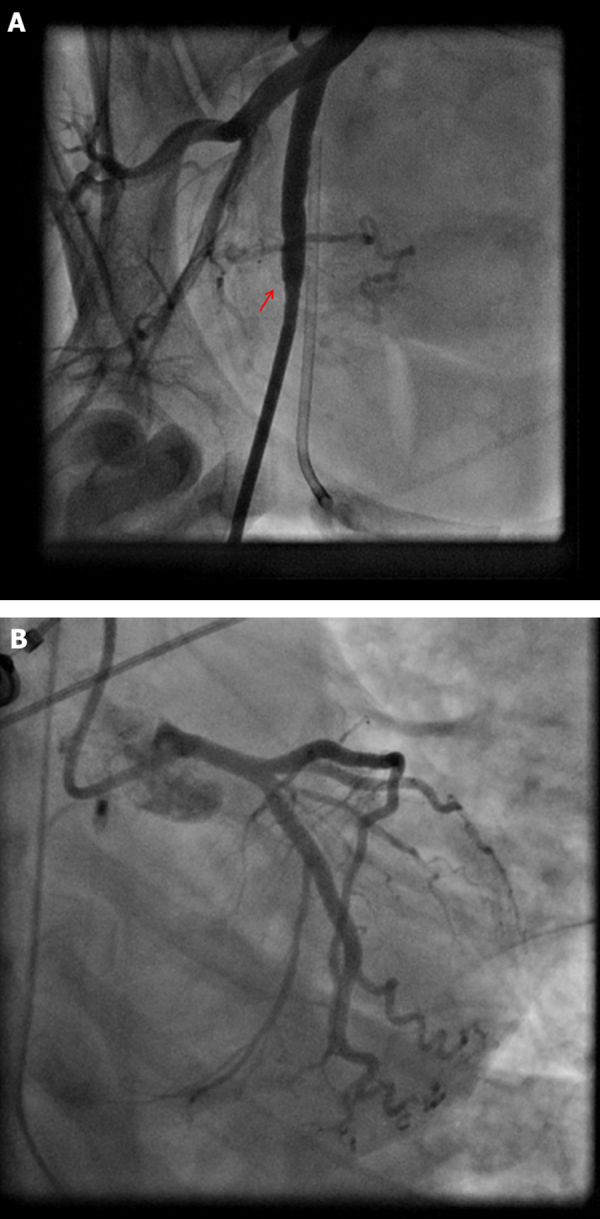
Angiography of femoral artery and coronary artery angiography after nitrate injection. (A) Femoral artery with vasospasm embracing arterial sheath. (B) Resolution of all vasospasms in the left coronary artery after intracoronary injection of nitrates.
Discussion
Kounis–Zavras syndrome is now the term used for allergic angina or MI [1]. Two variants have been described. Type I is an allergic insult resulting in coronary vasospasm in the setting of normal coronary arteries. The type II variant occurs in a patient with underlying quiescent coronary atherosclerotic disease. According the third universal definition of MI the type I variant of Kounis–Zavras syndrome may be included in the group of MI secondary to an ischemic imbalance (type 2) [3]. This subgroup included myocardial injury with necrosis, where a condition other than coronary artery disease contributes to an imbalance between myocardial oxygen supply and/or demand [3]. Also, coronary vasospasm and/or endothelial dysfunction have the potential to cause type 2 MI [3].
Our case report is a type I of Kounis–Zavras syndrome which is peculiar and interesting, principally for its seriousness of clinical presentation (cardiogenic shock, malignant ventricular arrhythmias) and for the initial lack of clinical information (aspirin sensitivity, ketorolac consumption). The trigger of the acute event (multiple coronary vasospasm with subsequent myocardial necrosis) was ketorolac, but also the ingestion of cabergoline (5 days before the acute event) may be involved in the severity of clinical presentation. Cabergoline, an ergot derivative, is a potent dopamine receptor agonist on D2 receptors. Previously, other authors described similar cases of coronary spasm associated with MI after the consumption of bromocriptine (an ergot derivative dopamine receptor agonist like cabergoline) for the suppression of lactation in the postpartum period [4], [5]. The mechanism whereby these agents could have precipitated coronary artery spasm is not clear. D2 receptors are associated with inhibition of adenylate cyclase, and they are located on postganglionic sympathetic nerve terminals, where they mediate inhibition of norepinephrine release. In normal conditions, these agents did not have serotoninergic or alpha-adrenergic agonist properties, but it is possible that in our patient the stimulation of D2-dopaminergic receptors could have resulted in a paradoxical constrictive response. We could speculate that cabergoline may be responsible for an unusual pathologic reactivity status of the arterial coronary wall where ketorolac acted as trigger of multiple coronary vasospasms.
While the exact pathophysiology is not known, inflammatory mediators released in the setting of anaphylactic reactions appear to be the primary mechanism leading to allergic MI. The mediators released include tryptase, chymase, histamine, platelet-activating factor, cytokines, and others, as well as prostaglandin and leukotriene synthesis. Many of these compounds in susceptible patients induce coronary vasospasm as well as platelet activation. In these cases, correct and prompt clinical information are crucial for the diagnosis and for the choice of adequate medical therapy. To overcome the acute phase, these patients require corticosteroids, anti-histamines (both H1- and H2-blockers), fluid resuscitation, and eventually epinephrine, and not the standard therapy for MI (e.g. aspirin, heparin, β-blockers, angiotensin-converting enzyme inhibitors, statins, percutaneous coronary intervention, stent implantation) [6]. Particularly, in these cases where coronary spasms are linked to allergic tendency, corticosteroids are essential (e.g. our patient had bronchial asthma and the trigger of events has been an allergic reaction to ketorolac) [7], [8]. Corticosteroids act principally through two mechanisms: (i) suppressing the hyper-reactivity of the vessel wall by alleviating the inflammation; (ii) direct action on the intracellular Ca2+ signals and protein kinase C of vascular smooth muscle cells [7], [8].
Our case report focused its attention on a very rare clinical entity, largely underdiagnosed, but potentially lethal. Finally, it is important to be reminded that, in these patients, an exhaustive allergologic–immunologic evaluation is recommended so as to identify the triggers and predisposing conditions and to educate the patient on how to avoid the risk factors for recurrence.
References
- 1.Kounis N.G. Kounis syndrome (allergic angina and allergic myocardial infarction): a natural paradigm. Int J Cardiol. 2006;110:7–14. doi: 10.1016/j.ijcard.2005.08.007. [DOI] [PubMed] [Google Scholar]
- 2.Fassio F., Almerigogna F. Kounis syndrome (allergic acute coronary syndrome): different views in allergologic and cardiologic literature. Intern Emerg Med. 2012 doi: 10.1007/s11739-012-0754-4. [DOI] [PubMed] [Google Scholar]
- 3.Thygesen K., Alpert J.S., Jaffe A.S., Simoons M.L., Chaitman B.R., White H.D. Third universal definition of myocardial infarction. J Am Coll Cardiol. 2012;60:1581–1598. doi: 10.1016/j.jacc.2012.08.001. [DOI] [PubMed] [Google Scholar]
- 4.Larrazet F., Spaulding C., Lobreau H.J., Weber S., Guerin F. Possible bromocriptine-induced myocardial infarction. Ann Intern Med. 1993;118:199–200. doi: 10.7326/0003-4819-118-3-199302010-00008. [DOI] [PubMed] [Google Scholar]
- 5.Ruch A., Duhring J.L. Postpartum myocardial infarction in a patient receiving bromocriptine. Obstet Gynecol. 1989;74:448–451. [PubMed] [Google Scholar]
- 6.Cevik C., Nugent K., Shome G.P., Kounis N.G. Treatment of Kounis syndrome. Int J Cardiol. 2010;143:223–226. doi: 10.1016/j.ijcard.2010.02.040. [DOI] [PubMed] [Google Scholar]
- 7.Habbab M.A., Szwed S.A., Haft J.I. Is coronary arterial spasm part of the aspirin-induced asthma syndrome. Chest. 1986;90:141–143. doi: 10.1378/chest.90.1.141. [DOI] [PubMed] [Google Scholar]
- 8.Takagi S., Goto Y., Hirose E., Terashima M., Sakuragi S., Suzuki S., Tsutsumi Y., Miyazaki S., Nonogi H. Successful treatment of refractory vasospastic angina with corticosteroids: coronary arterial hyperactivity caused by local inflammation. Circ J. 2004;68:17–22. doi: 10.1253/circj.68.17. [DOI] [PubMed] [Google Scholar]