Abstract
Background
Mortality statistics derived from cause of death data are an important source of information for population health monitoring, priority setting and planning. In Perú, almost all death certificates are issued by doctors because it is a legal requirement. However, the quality of cause of death data is poor. In August 2016, the Ministry of Health of Perú decided to make two specific interventions to improve cause of death data: to introduce an online death certification system and to train doctors in standard death certification practices.
Methods
The study comprised a random sample of 300 pre-intervention death certificates, 900 death certificates that were part of the online intervention, and 900 death certificates that were part of both the online and training interventions. All the deaths had occurred between January and September 2017. We used the Assessing the quality of death certification tool from the University of Melbourne for the assessment. We examined the frequency of common errors in death certificates, the frequency of any error and the average error score for each category of: age group, sex, doctor’s seniority, doctor’s speciality, level of health facility and broad cause of death.
Results
The average error score declined by 38% due to the online intervention and by a further 26% due to the training intervention. Improved certification practices remained after controlling for potentially confounding factors. Main improvements were reductions in the absence of a time interval (66% of certificates), incorrect sequence of causes (22%), and ill-defined conditions (13%).
Conclusions
This study demonstrates how the two interventions introduced by the Ministry of Health in Perú improved the correctness of death certificates. The study also provides evidence on necessary changes to the training program to address the poor certification practices that have remained after implementation of the online system.
Electronic supplementary material
The online version of this article (10.1186/s12889-018-6264-1) contains supplementary material, which is available to authorized users.
Keywords: Cause of death, Certification, Intervention, Mortality, Online, Perú, Quality, Training
Background
Routine cause of death data from civil registration and vital statistics (CRVS) systems are an important source of information and evidence for monitoring population health, identifying health priorities, and planning public health interventions [1–4]. However, many countries have registration systems that cover only part of the population, with no cause of death data for those dying outside of health facilities, and no routine compilation of data for analysis, dissemination, and policy purposes. Furthermore, many hospitals’ cause of death data, derived from medical certification, are of such poor quality to be not useful for policy making [5–10]. There are many reasons for the poor quality of death certification, including: i) absent, insufficient, or inadequate training on death certification and the concept of underlying cause of death, ii) limited understanding of the importance of death certification within the health sector, iii) an absence of doctors in some rural areas to certify deaths, iv) challenges in obtaining cause of death for external causes, v) doctors’ experience in the certification of deaths, and vi) limited availability of diagnostic equipment [11–13].
In 2016, approximately 145,500 deaths were registered in Perú, with registration completeness estimated at 75% [14]. Coverage is a major challenge for the country, with 89% of deaths registered in offices of the Civil Registry located in urban areas, and only 11% registered in municipalities, despite approximately one-quarter of the population living in rural areas [15]. While 95% of medical certificates of cause of death (‘death certificates’) are certified by doctors [16], international studies have shown that cause of death data from certificates are of limited use for country policy due to their poor quality [6, 17, 18]. Such findings are also supported by Perú’s low Vital Statistics Performance Index (VSPI) score (50%). The VSPI scores the quality of data on mortality and cause of death by assessing several components within a CRVS system, including the extent to which age and/or sex are missing in the data, and the number of biologically implausible underlying causes of death recorded on death certificates [19].
One reason for the poor quality of cause of death data in Perú is the poor quality of medical certification. Medical certification of cause of death is not a primary focus of the undergraduate medical curriculum in Peruvian universities, with the current curricula mostly focusing on prevention, and the recuperation and rehabilitation of patients. Many doctors do not understand the link between the causes they record on death certificates and national mortality statistics. Further, many doctors are not aware of standard death certification guidelines and practices. These factors all affect the quality of cause of death data reported in Perú [20–22].
To address these issues the Ministry of Health (MOH) of Perú, with the help of the Bloomberg Philanthropies Data for Health Initiative, introduced two specific interventions to improve the completeness of death registration, and the quality of cause of death data. The first intervention, in August 2016, was to introduce an online death notification and certification system (SINADEF1) to all health facilities and morgues. SINADEF is modelled on the system of online birth certification introduced by the MOH in 2012, which saw birth registration increase from 67% in 2011 to 84% in 2017 [23–25]. The introduction of online death certification was also supported by evidence from other countries that had shown improvements in the completeness of death notification and registration following their implementation [26, 27].
SINADEF was introduced to improve the processes of death notification and certification through providing a secure data entry and storage system. The system also improved the quality of cause of death data entered through: i) eliminating the effect of illegible handwriting; ii) reducing the use of ill-defined conditions by having a warning pop up dialog (for ‘cardiac arrest’ only); iii) not allowing for blank spaces to be left between the lines of events; and iv) decreasing the use of abbreviations, due to the high number of characters (300) allowed on each line. Given its online nature, SINADEF also improved the timeliness of data, as online certificates are available immediately to the MOH.
To ensure maximum benefit from SINADEF, the MOH also introduced a training program to doctors on medical certification, including how to complete the International Form of Medical Certificate of Cause of Death [28] correctly. A selected team of trained doctors and other professionals trained a group of doctors and statisticians from the main hospitals and morgues in how to use SINADEF, as well as a group of regional staff to replicate the training in other health facilities.
The training lasted two hours: one hour on the online system and one hour for certification of cause of death. The training was limited to two hours because all health facilities considered it was the maximum time that doctors could be released from clinical duties. The following topics were covered during the training: the importance of correct medical death certification of cause of death; understanding the International Form of Medical Certificate of Cause of Death; the concept of underlying cause of death (UCOD); case scenarios to demonstrate correct certification practices; and SINADEF.
Previous studies have shown the effectiveness of knowledge gained in medical certification training based on pre-and post-training tests using clinical scenarios. However, most of these studies have been conducted as one-off trainings with little or no follow up, and literature on the effectiveness of medical certification training producing sustainable changes to death certification practices is rare [29, 30]. The literature has shown the importance of periodically monitoring death certification accuracy to identify quality issues to provide feedback to certifiers and their administrators to improve them [31, 32].
To assess the effectiveness of the two interventions introduced by the MOH to increase the quality of cause of death data, in this study we compare the quality of medical certification correctness between three groups:
Paper death certificates completed prior to the two interventions (‘pre-intervention’)
Death certificates entered in SINADEF by doctors (‘online intervention’)
Death certificates entered in SINADEF by doctors who had also received medical certification training (‘online and training intervention’).
This study was carried out to evaluate the quality of cause of death data in Perú, as generated from medical certificates of cause of death completed by doctors. The results will provide feedback to doctors and their administrators about current routine medical certification correctness to identify areas that need further training, and provide recommendations to the MOH’s medical certification training program.
Methods
A random sample of 300 pre-intervention, 900 online intervention, and 900 online and training intervention death certificates, completed between January 2017 and September 2017 were selected for the study. Doctors were unaware they were being evaluated before and after the intervention. All online death certificates were obtained from SINADEF.
For the assessment, the tool Assessing the quality of death certificates from the University of Melbourne was used [33]. This tool is designed to assess the quality of death certification practices by checking for the presence of common errors in death certificates. The tool can also be used to assess the quality of death certification as part of routine assessment, or to assess the training needs of doctors in designing cause of death certification training and to evaluate the effect of death certification training. Errors were classified as major or minor errors, as shown in Table 1; and a summary error score was developed with two points applied to major errors and one point for minor errors.
Table 1.
Classification matrix of major and minor errors assessed in death certificates
| Error type | Description and implications |
|---|---|
| Major errors | |
| Multiple causes per line | The WHO ICD guidelines state that only one cause should be recorded per line in a death certificate. When more than one cause is reported on a single line, it makes it difficult for coders to establish the sequence of events leading to death, thus selecting the correct underlying cause of death would be more difficult |
| Absence of disease time interval | The time interval should be entered for all conditions reported on the death certificate, especially for the conditions reported in Part 1. Time intervals are very important for correctly coding certain diseases and provide a check on the accuracy of the reported sequence of conditions. |
| Incorrect sequence of events leading to death | Mortality statistics are based on the underlying cause of death, which is the condition or injury that initiated the sequence of events that led directly to death. When a clinically improbable sequence of events is recorded, it is impossible to select the correct underlying cause of death. |
| Ill-defined or poorly specified condition entered as the UCOD | Ill-defined or poorly specified conditions are of no value for public health officials, and do not provide any information for decision-makers to help them design preventive health programs. These include, for example, organ failure (hepatic or cardiac failure, etc.); symptoms or signs (hematemesis, dyspnoea, fever, etc.); mode of dying (cardiac arrest, respiratory arrest); pathophysiological findings (shock); other (trivial diseases such as colds, rhinitis, etc.). |
| Minor errors | |
| Presence of blank spaces within the sequence of events | In completing a death certificate the certifier should use consecutive lines in Part 1 of the death certificate starting at Line 1a. The UCOD should be recorded in the lowest used line of Part 1. There should not be any blank lines within the sequence/chain of events leading to death. |
| Abbreviations used in certifying the death | Doctors are encouraged not to use abbreviations when certifying deaths as abbreviations can mean different things to different people. There is a chance that coders may misinterpret the abbreviation and code the death to a non-relevant code. |
| Additional errors on the certificate | There may be other additional errors on death certificates including: incomplete information of the external cause of death (no site of the injury, intent or nature of it, etc.); insufficient information on neoplasms (no site, whether benign or malignant, etc.); failing to identify pregnancy and maternal deaths. |
The errors were categorized as major or minor based on the impact that the error can have on the final selection of underlying cause of death (UCOD) by the mortality coder. If the risk of mis-identification by coders is high, the error was classified as a major error. For example, recording multiple causes per line makes it difficult for coders to apply selection and modification rules for selecting the UCOD. On the other hand, presence of blank lines has a minor impact on the process of UCOD selection, and so was classified as a minor error.
Inclusion and exclusion criteria
The study was conducted in almost all departments (24 out of 25, one department was excluded because of an unreliable internet connection and doctors’ resistance to use the online system) that certify deaths using SINADEF in Perú. The study death certificates entered in SINADEF directly by certifying doctors, and certificates entered by trained statisticians. To minimize other factors that may influence the quality of certification, the selection excluded death certificates from doctors who were not the attending doctor for the deceased, and death certificates that were registered outside a health facility, as the doctors there may not have sufficient technology or information to correctly complete the death certificate.
Study procedures
Data from selected death certificates (online certificates completed by doctors and paper death certificates manually entered in SINADEF by statisticians) were downloaded. The data included general information on the deceased including age, sex, place and name of health facility where the person died; and certifier data such as doctor’s name and Medical Council registration number. The name and Medical Council registration number of doctors were matched with those from attendance lists at SINADEF training, to identify certificates for the ‘online and training intervention’ group. The name of health facility was matched with information from the National Health Superintendence (SUSALUD) to select the level of the facility (I-III). To complete the data about the doctor’s seniority and speciality, information from the Medical Council was used.
The evaluation of death certificates was carried out by one doctor with experience in death certification who received a training in using the death certification assessment tool that was conducted as part of the implementation of SINADEF.
Data analysis
Bivariate and multivariate analyses were conducted to assess the effectiveness of the three intervention groups. Bivariate relationships were analysed using chi-square and t-tests. The multivariate analysis conducted was an ordinal logit regression of the error score, to identify if the interventions had a statistically significant impact on the quality of death certification (measured by the error score), controlling for potentially confounding factors. The covariates in the model were study group status (pre-intervention, online intervention, online and training intervention), age group of the deceased, sex, doctor’s experience, doctor’s specialisation, level of health facility, and cause of death (as classified into Global Burden of Disease [GBD] group). Doctor’s experience and specialisation and the level of health facility may differ between the three stages of the study, and their inclusion in the regression removes any bias they may introduce into the results for the interventions. An ordinal logit is suitable when the dependent variable is ordered, such as the error score, which ranged from 0 to 9 [34]. The ordinal logit regression produces odds ratios; these show the odds of a variable category having a higher error score compared with the reference category for that variable, controlling for all other variables in the regression. The data were analysed using Stata 15 [35].
Results
Study population
From January to September 2017, 22,727 deaths were certified in SINADEF and 3298 deaths were originally certified using a paper certificate and then transcribed into the system. Of these records, 15,656 (69%) deaths occurred in a health facility and the other 7071 deaths occurred away from health facilities, including at home, at work, etc. A total of 2517 doctors certified the 15,656 deaths that occurred in a health facility, with 1257 doctors certifying the 2100 deaths from our random sample (approximately 50% of all doctors using SINADEF). The most common level of doctor’s experience was 11–15 years across all study groups. More information on attributes of the death certificates assessed are provided in Additional file 1.
Correctness of death certificates
Table 2 shows that the correctness of death certification was much higher following the interventions, increasing from 0 to 30% due to the introduction of the online system, and then further to 43% with the online system and training. The correctness at pre-intervention was 0% as the clear majority (96%) of certificates did not have the time interval recorded. When this error type is removed, the correctness of pre-intervention certificates increases to 15%.
Table 2.
Correctness of death certificates assessed
| Correctness of death certificates according to study group (%) | Percentage point improvement (%) | ||||
|---|---|---|---|---|---|
| Pre-intervention (n = 300) | Online intervention (n = 900) | Online and training intervention (n = 900) | Online intervention | Online and training intervention | |
| Correctly certified certificates | 0.0 | 30.1 | 43.3 | 30.1** | 43.3** |
| Certificates with one error | 16.3 | 18.2 | 18.6 | ||
| Certificates with two errors | 40.0 | 28.0 | 22.9 | ||
| Certificates with three errors | 27.3 | 17.9 | 12.8 | ||
| Certificates with four or more errors | 16.3 | 5.8 | 2.4 | ||
| Total (%) | 100.0 | 100.0 | 100.0 | ||
**p < 0.01
The composite error score declined by 38% due to the online intervention, and a further 26% due to the online and training intervention (Fig. 1).
Fig. 1.
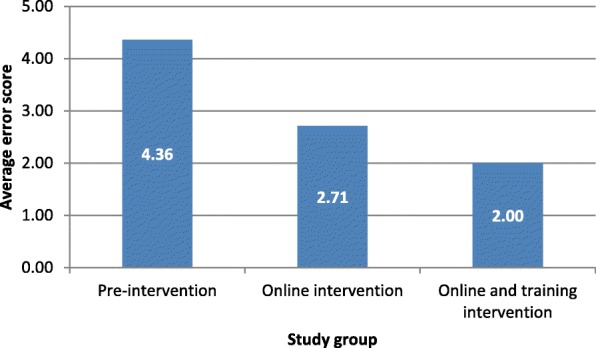
Average error scores of death certificates by study group
The most important improvement in the type of error was in the time interval of the disease, with 66% of the online and training intervention group certificates having this correctly completed. There was also an important improvement (22%) in the correctness of the sequence of events leading to death, and in no longer reporting ill-defined conditions as the underlying cause of death (13%) (Table 3).
Table 3.
Major and minor errors in death certificates assessed
| Error type | Correctness of death certificates according to study group (%) | Percentage point improvement (%) | |||
|---|---|---|---|---|---|
| Pre-intervention (n = 300) | Online intervention (n = 900) | Online and training intervention (n = 900) | Online intervention | Online and training intervention | |
| Major errors | |||||
| Multiples causes per line | 2.0 | 1.3 | 0.6 | 0.7 | 1.4 |
| Absence of disease time interval | 96.0 | 47.1 | 30.0 | 48.9** | 66.0** |
| Incorrect sequence of events leading to death | 40.3 | 25.9 | 17.9 | 14.4** | 22.4** |
| Ill-defined condition entered as an underlying cause of death | 52.0 | 45.4 | 38.9 | 6.6* | 13.1** |
| Minor errors | |||||
| Presence of blank lines within the sequence of events | 11.3 | 0.2 | 0.3 | 11.1** | 11.0** |
| Abbreviations used in certifying the death | 11.7 | 4.6 | 4.1 | 7.1** | 7.6** |
| Additional errors on the certificate | 32.3 | 26.6 | 21.0 | 5.7 | 11.3** |
| - External causes, missing details | 4.7 | 4.6 | 2.1 | ||
| - Neoplasms, missing details | 15.0 | 8.1 | 6.3 | ||
| - No units in age of deceased | 0.0 | 0.2 | 0.6 | ||
| - Other | 12.7 | 13.7 | 12.0 | ||
* p < 0.05 ** p < 0.01
The occurrence of additional errors in death certificates decreased from 32% in the pre-intervention group, to 21% in the online and training intervention group (Table 4). Within this error type, ‘other’ included non-specification of hypertension as essential or secondary, non-specification of diabetes as type I or II, and recording the UCOD in Part 2 of the death certificate. There was no change in the number of certificates with these ‘other’ errors when comparing pre-intervention with online and online and training interventions.
Table 4.
Certificates with any error and their average error score, according to attributes of the deceased and certifier
| Attributes of the deceased | Any error (%) | Average error score | Number of death certificates |
|---|---|---|---|
| Age group (years) | |||
| 0–4 | 50.2 | 1.59 | 194 |
| 5–44 | 65.7 | 2.65 | 248 |
| 45–64 | 64.9 | 2.47 | 373 |
| 65–74 | 71.5 | 2.76 | 368 |
| 75–84 | 72.9 | 2.85 | 516 |
| ≥ 85 | 74.6 | 2.92 | 394 |
| Sex | |||
| Male | 69.9 | 2.68 | 1087 |
| Female | 66.8 | 2.60 | 1007 |
| Cause of death (GBD categories) | |||
| Communicable diseases | 68.9 | 2.69 | 730 |
| Non-communicable diseases | 64.7 | 2.35 | 1175 |
| External causes | 87.7 | 3.93 | 71 |
| Ill-defined (unusable and insufficiently specified) causes of death | 100.0 | 5.00 | 124 |
| Attributes of the certifier | Any error (%) | Average error score | Number of death certificates |
| Doctor’s seniority (years) | |||
| 0–5 | 80.9 | 3.17 | 141 |
| 6–10 | 71.4 | 2.78 | 405 |
| 11–15 | 62.6 | 2.38 | 412 |
| 16–20 | 73.2 | 2.93 | 370 |
| 21–25 | 65.3 | 2.41 | 245 |
| 26–30 | 62.8 | 2.41 | 239 |
| > 30 | 68.4 | 2.57 | 288 |
| Doctor’s speciality | |||
| General medicine | 69.0 | 2.71 | 468 |
| Internal medicine | 67.4 | 2.58 | 746 |
| Pediatrics & neonatology | 52.1 | 1.62 | 165 |
| Intensive care medicine | 73.6 | 3.08 | 178 |
| Pneumology | 63.2 | 1.93 | 57 |
| Oncology | 55.6 | 2.33 | 36 |
| Emergency | 85.9 | 3.52 | 170 |
| General surgery | 74.6 | 2.75 | 63 |
| Others | 67.7 | 2.62 | 217 |
| Level of health facility | |||
| I (health centre) | 91.4 | 3.86 | 35 |
| II (hospital) | 68.8 | 2.66 | 982 |
| III (specialised hospital) | 67.5 | 2.58 | 1083 |
| Time from training to death certification+ | |||
| < 3 months | 54.7 | 1.87 | 234 |
| 3–6 months | 60.4 | 2.17 | 455 |
| > 6 months | 50.7 | 1.76 | 211 |
+Does not include certificates from the pre-intervention study group
Table 4 shows that the percentage of death certificates with any error and the average error score increased with age of the deceased. While there was no linear decrease in the number of errors and average error score as doctor’s seniority increased, overall, junior doctors (with 0–5 years’ experience) had the highest number of certificates with any error reported (81%) and the highest average error score (3.2). Level II and III hospitals are generally located in urban areas, while level I health centres are located in rural areas; certificates with the highest error score included those from Level I health facilities, those with unusable or external causes, and those certified by doctors specialising in emergency or intensive care medicine. For the period between receiving training and completing the death certificate, the highest error scores were from doctors that certified between 3 and 6 months following the training.
Table 5 shows the results from an ordinal regression of the error score of the pre-intervention, online intervention, and online and training intervention groups. Introduction of the online system resulted in a death certificate having smaller odds of having a higher error score compared with pre-intervention (0.283). For certificates in the online and training intervention, there was only 0.151 the odds of having a higher error score compared with pre-intervention. This means that certificates in the online and training intervention had 6.6 times greater odds (1/0.151) of having a lower error score compared with pre-intervention certificates.
Table 5.
Results of ordinal regression of the error score
| Variables | Odds Ratio | Std. Error | P > │z│ |
|---|---|---|---|
| Study group | |||
| Pre-intervention | Ref. | – | – |
| Online intervention | 0.283** | 0.034 | 0.000 |
| Online and training intervention | 0.151** | 0.019 | 0.000 |
| Online and training versus online intervention+ | 0.535** | 0.048 | 0.000 |
| Attributes of the deceased | |||
| Age group (years) | 1.009** | 0.002 | 0.000 |
| Sex | |||
| Male | Ref. | – | – |
| Female | 0.969 | 0.077 | 0.673 |
| Cause of death (GBD categories) | |||
| Ill-defined (unusable and insufficiently specified) causes of death | Ref. | – | – |
| Communicable diseases | 0.181** | 0.036 | 0.000 |
| Non-communicable diseases | 0.120** | 0.024 | 0.000 |
| External causes | 0.486* | 0.138 | 0.011 |
| Attributes of the certifier | Odds Ratio | Std. Error | P > │z│ |
| Doctor’s seniority (years) | |||
| 0–5 | Ref. | – | – |
| 6–10 | 0.825 | 0.151 | 0.295 |
| 11–15 | 0.591** | 0.109 | 0.004 |
| 16–20 | 0.967 | 0.187 | 0.864 |
| 21–25 | 0.713 | 0.143 | 0.091 |
| 26–30 | 0.783 | 0.160 | 0.231 |
| > 30 | 0.782 | 0.154 | 0.210 |
| Doctor’s speciality | |||
| General medicine | Ref. | – | – |
| Internal medicine | 1.134 | 0.133 | 0.285 |
| Pediatrics & neonatology | 0.877 | 0.190 | 0.544 |
| Intensive care medicine | 1.495* | 0.250 | 0.016 |
| Pneumology | 0.725 | 0.189 | 0.217 |
| Oncology | 0.753 | 0.263 | 0.417 |
| Emergency | 2.023** | 0.340 | 0.000 |
| General surgery | 1.057 | 0.260 | 0.822 |
| Others | 1.154 | 0.185 | 0.370 |
| Level of health facility | |||
| I (health centre) | Ref. | – | – |
| II (hospital) | 0.670 | 0.216 | 0.214 |
| III (specialised hospital) | 0.757 | 0.246 | 0.391 |
* p < 0.05 ** p < 0.01
+This result used “online intervention” as the reference category; all regression results for other variables were the same as when reference category is “pre-intervention”
Ref. Reference category
Additional analysis shows that the introduction of the training intervention resulted in significantly smaller odds (0.535) of having a higher error score compared with the online intervention only. Regarding attributes of the deceased, the odds of having a higher error score increased with age, and this was statistically significant.
Discussion
This study has clearly demonstrated the effect of the two interventions introduced by the Ministry of Health in Perú to improve the correctness of cause of death data. All pre-intervention death certificates had at least one error and with introduction of the online system SINADEF, one-third of them were improved. After introducing the training program to complement SINADEF, almost half of the death certificates were improved. The random sample of death certificates used in this study included about half of all doctors that are using the online system; making the results of the data assessment more generalisable.
Effect of the online system
Overall, introduction of the online system for death certification had the greatest impact on improving the quality of death certification; with the training program producing modest further improvements. There have been previous studies in France [27, 28], where researchers compared the quality of paper and electronic death certificates and found that doctors complete the electronic death certificates better than the paper ones. This study reinforces these findings. Having an electronic certificate with built-in requirements reduces the number of errors as, for example, doctors can’t leave blank spaces between the sequences of events as the system does not allow it. The use of abbreviations also decreased when using SINADEF, likely due to the high numbers of characters allowed (300) in each cause of death line, unlike the short space in paper death certificates. Also, entering an ill-defined condition as the UCOD decreased with SINADEF, likely as the system opens a warning window when the doctor records an ill-defined condition (such as cardiac arrest) indicating that it isn’t an UCOD.
While establishing an online system for death certification or any other part of the certification and registration process is a major undertaking, many countries are already implementing various electronic technologies as part of their CRVS systems. For developing countries especially, the innovative use of technology is allowing them to ‘leap-frog’ the traditional development pathway and achieve substantial gains [36]. This study further demonstrates the usefulness and feasibility of introducing an electronic system as part of routine CRVS processes.
Effect of the online system and training
Training in medical certification of cause of death has showed improvements in the correctness of certification at a routine level. Several studies have shown different levels of improvements with training [28, 29, 37–39]. While the addition of training did lower the average error score when compared with the online intervention alone, the impact was not substantial. This may be because subsequent improvements in certification are harder to achieve, after initial gains when implementing an online system. The limited improvement in the correctness of death certificates may also be due to:
Inadequacy of the training program (time or content) [28].
The change in knowledge (gained through training) does not produce significant change in certification behaviour at the practice level.
Inadequate assessment of death certification correctness and feedback to the certifiers.
The disjointed nature of training, highlighting the need to ensure continuous training to medical students, junior doctors, and experienced specialists [37, 40, 41].
After implementation of the online system, one-third of the remaining ill-defined conditions entered as an underlying cause of death were in the category of an intermediate cause [42]. This could mean that doctors don’t have further information to identify the UCOD; perhaps due to limited diagnostic capacities of the hospital, or that they were not aware of the importance of identifying and reporting the correct UCOD for public health. Additional research comparing death certificates with the medical reports would be necessary to identify the reason for the high proportion of intermediate cause of death. Additional errors in the death certificates included insufficiently specified causes, and listing an incorrect sequence of events leading to death. Future training programs should focus on these errors.
There are some limitations to our study. First, the study compares trained doctors versus non-trained ones as per the recent training by the MOH. We do not have information regarding any previous training exposures among the pre-intervention and the online intervention groups. However, we are assuming that most of the doctors did not have access to good quality training. We also did not have information on the frequency that trained doctors certify deaths, though the literature shows mixed results when comparing level of experience with correctly certified deaths [40, 43, 44]. A quality assessment with the same group of doctors pre- and post-training would provide better information. Second, it was observed that, despite being mandatory, older doctors were more likely to resist using the electronic system, which may have affected the results. However, doctor’s seniority was controlled for in the regression analysis and it was not found to be significant (apart from 11 to 15 years experience) so any impact of this effect is likely to be minimal. Third, many level I facilities are in remote rural areas lacking reliable access to the Internet, and so they were excluded from the study. However, the number of deaths in such facilities is minimal compared with those from levels II and III. A final limitation is the potential for introduction of random and systematic errors by only having one doctor review the certificates. However, the use of a single reviewer eliminated any inter-interviewer variability; the sample of certificates were reassessed by an experienced reviewer at the end of the study; and research has demonstrated that single, rather than duplicate, review processes do not lead to significant diagnostic inaccuracy, as previously assumed [45].
Conclusions
The study has demonstrated the significant impact that an online system can have on the quality of death certification, which in Perú will result in improved mortality statistics as the system is rolled out through the country. Online certification should be developed in other countries to improve not only completeness of registration, but also data quality. The lessons learned in Perú around the design and implementation of SINADEF hold important insights for other countries looking to implement similar systems: making key variables mandatory (for example, the time interval between disease onset and death, and not allowing blank lines when entering the sequence of events leading to death) would automatically improve the quality of death certificates. Similarly, having warning windows appear on-screen when a doctor attempts to enter an ill-defined condition as an underlying cause of death would likely lead to a decrease in such behaviour, and an increase in correctly coded mortality statistics.
The addition of medical certification training did not produce as large a change in death certification correctness as the introduction of SINADEF, possibly because the improvements due to SINADEF were relatively easier to achieve (i.e. inclusion of time interval on certificate). Again, countries wishing to improve the quality of their cause of death statistics can learn from the experiences of Perú and may look to: adapt their training programs to focus on certification errors that remain after the introduction of certification interventions (such as online systems or periodic reviews); introduce a master training program at the health facility level, where local trainers can provide training sessions on a regular basis; introduce certification training in medical curriculum, to ensure doctors receive adequate time on the subject as part of their education; and implement periodic death certificate assessments for further improvement of certification correctness. For the sustainability of periodic assessments, we recommend including training in assessing the quality of death certificates to a small team of health professionals in each department/health facility, so that they can do the follow up, bring feedback periodically, and retrain doctors. This team could analyse the main errors in the different health facilities of the department and change the content of the training for each place according to the results of the analysis.
In looking to the future for Peru, the next major step is to continue to roll-out implementation of Iris, the automated coding software. A team has been established within the Ministry of Health to develop a Peruvian version of the dictionary, and has re-coded 2016 data using Iris. Initial results have been very positive, with Iris able to code over 70% of medical certificates. The remaining certificates were analysed by a team of statistical personnel from the Ministry of Health and Directorates of Integrated Health Networks in Lima and Callao. In the coming months, 2017 data will also be analysed, as the country continues to move to electronic solutions for improving the quality of its mortality data.
Additional file
Attributes of death certificates assessed. (DOCX 13 kb)
Acknowledgements
William Valdez for revising the manuscript; Karim Pardo and the General Office of Information Technology (Ministry of Health) for implementing SINADEF in Perú.
Funding
This study was funded under an award from Bloomberg Philanthropies to the University of Melbourne to support the Data for Health Initiative. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Availability of data and materials
The data that support the findings of this study are available from the General Office of Information Technology (Ministry of Health, Perú) but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of the General Office of Information Technology (Ministry of Health, Perú).
Abbreviations
- CRVS
civil registration and vital statistics
- MOH
Ministry of Health, Perú
- SINADEF
Sistema Informático Nacional de Defunciones (National Death Information System)
- UCOD
underlying cause of death
- VSPI
Vital Statistics Performance Index
Authors’ contributions
JM contributed to the analytical framework, conducted the data analysis and validation, drafted earlier versions of the manuscript, and contributed to the final version of the manuscript. RR and TA conceptualised the research theme, contributed to the analytical framework, edited earlier versions of the manuscript, and contributed to the final version of the manuscript. NR contributed to the analytical framework, edited earlier versions of the manuscript, and contributed to the final version of the manuscript. JV and JC were responsible for implementing activities under the Bloomberg Philanthropies Data for Health Initiative, including those on improving medical certification as described. They edited earlier versions of the manuscript. All authors have read and approve the final manuscript.
Ethics approval and consent to participate
Ethics approval was not required for this study, as it was conducted as part of routine activities of the Ministry of Health as part of implementation of SINADEF. As per the Regulation of the Organisation and Functions of the Ministry of Health (ftp://ftp2.minsa.gob.pe/normaslegales/2017/rof_2017.pdf), page 38, Art.55, the Ministry is permitted to “Perform the analysis, validation and evaluation of the quality of the data in health by monitoring the veracity, timeliness, coverage and accuracy of them”. Further, no identifiable information from the death certificates or the certifiers was collected.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Footnotes
SINADEF is the abbreviation in Spanish of Sistema Informático Nacional de Defunciones (National Death Information System).
Contributor Information
Janet Miki, Email: chiaki.miki@gmail.com.
Rasika Rampatige, Email: rasika.rampatige@unimelb.edu.au.
Nicola Richards, Email: nicola.richards@unimelb.edu.au.
Tim Adair, Email: timothy.adair@unimelb.edu.au.
Juan Cortez-Escalante, Email: jcorteze@gmail.com.
Javier Vargas-Herrera, Email: javargashe@gmail.com.
References
- 1.Hernandez B, Ramirez-Villalobos D, Romero M, Gomez S, Atkinson C, Lozano R. Assessing quality of medical death certification: concordance between gold standard diagnosis and underlying cause of death in selected Mexican hospitals. Popul Health Metr. 2011;9. [DOI] [PMC free article] [PubMed]
- 2.Macintyre S, Chalmers I, Horton R, Smith R. Using evidence to inform health policy: case studs. Br Med J. 2001;322(7280):222–225. doi: 10.1136/bmj.322.7280.222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Petticrew M, Whitehead M, Macintyre SJ, Graham H, Egan M. Evidence for public health policy on inequalities: 1: the reality according to policymakers. J Epidemiol Community Health. 2004;58(10):811–816. doi: 10.1136/jech.2003.015289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Victora CG, Habicht JP, Bryce J. Evidence-based public health: moving beyond randomized trials. Am J Public Health. 2004;94(3):400–405. doi: 10.2105/AJPH.94.3.400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.AbouZahr C, De Savigny D, Mikkelsen L, Setel PW, Lozano R, Nichols E, et al. Civil registration and vital statistics: progress in the data revolution for counting and accountability. Lancet. 2015;386(10001):1373–1385. doi: 10.1016/S0140-6736(15)60173-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mikkelsen L, Phillips DE, AbouZahr C, Setel PW, de Savigny D, Lozano R, et al. A global assessment of civil registration and vital statistics systems: monitoring data quality and progress. Lancet. 2015;386(10001):1395–1406. doi: 10.1016/S0140-6736(15)60171-4. [DOI] [PubMed] [Google Scholar]
- 7.WHO. Improving the quality and use of birth, death and cause-of-death information, guidance for a standardsbased review of country practices. Geneva, Switzerland: World Health Organization 2010.
- 8.Benavides FG, Bolumar F, Peris R. Quality of death certificates in Valencia. Spain Am J Public Health. 1989;79(10):1352–1354. doi: 10.2105/AJPH.79.10.1352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hazard RH, Chowdhury HR, Adair T, Ansar A, Rahman AMQ, Alam S, et al. The quality of medical death certification of cause of death in hospitals in rural Bangladesh: impact of introducing the international form of medical certificate of cause of death. BMC Health Serv Res. 2017;17. [DOI] [PMC free article] [PubMed]
- 10.Mathers CD, Fat DM, Inoue M, Rao C, Lopez AD. Counting the dead and what they died from: an assessment of the global status of cause of death data. Bull World Health Organ. 2005;83(3):171–177. [PMC free article] [PubMed] [Google Scholar]
- 11.Filippatos G, Andriopoulos P, Panoutsopoulos G, Zyga S, Souliotis K, Gennimata V, et al. The quality of death certification practice in Greece. Hippokratia. 2016;20(1):19–25. [PMC free article] [PubMed] [Google Scholar]
- 12.Nojilana B, Groenewald P, Bradshaw D, Reagon G. Quality of cause of death certification at an academic hospital in Cape Town, South Africa. Samj S Afr Med J. 2009;99(9):648–652. [PubMed] [Google Scholar]
- 13.Pillay-van Wyk V, Bradshaw D, Groenewald P, Laubscher R. Improving the quality of medical certification of cause of death: The time is now! Samj S Afr Med J. 2011;101(9):626. [PubMed] [Google Scholar]
- 14.GBD 2016 Mortality Collaborators. Global, regional, and national under-five mortality, adult mortality, age-specific mortality, and life expectancy, 1970–2016: a systematic analysis for the Global Burden of Disease Study 2016 Lancet. 2017;390:1084–1150. doi: 10.1016/S0140-6736(17)31833-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Instituto Nacional De Estadisticia e Informatica. Peru: Estimaciones y proyecciones de población, 1950–2050. Boletin de Analisis Demografico No. 35. Lima; 2001.
- 16.Ministerio de Salud DGE. Indicadores Básicos de Salud 2015. Lima; 2017.
- 17.Rampatige R, Mikkelsen L, Hernandez B, Riley I, Lopez AD. Systematic review of statistics on causes of deaths in hospitals: strengthening the evidence for policy-makers. Bull World Health Organ. 2014;92(11):807–816. doi: 10.2471/BLT.14.137935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Garg A, Singh SV, Gupta VK. Accuracy of medical certification of the cause of death in a rural non-teaching hospital in Delhi. Natl Med J India. 2012;25(3):185–186. [PubMed] [Google Scholar]
- 19.Phillips DE, Lozano R, Naghavi M, Atkinson C, Gonzalez-Medina D, Mikkelsen L, et al. A composite metric for assessing data on mortality and causes of death: the vital statistics performance index. Popul Health Metr. 2014;12. [DOI] [PMC free article] [PubMed]
- 20.Soto-Caceres V. Calidad del llenado de los certificados de defunción en un Hospital Público de Chiclayo, Perú 2006 [Quality of the filing of death certificates in a Public Hospital of Chiclayo, Perú 2006] Rev Perú Med Exp Salud Publica. 2008;25(3):330–332. [Google Scholar]
- 21.Loreto Núñez MGIM. Calidad de las estadísticas de mortalidad en Chile, 1997-2003 [quality of mortality statistics in Chile, 1997-2003] Rev Med Chil. 2006;134:1191–1196. doi: 10.4067/s0034-98872006000900016. [DOI] [PubMed] [Google Scholar]
- 22.Valdez WG, Gutiérrez C, Siura G. Análisis de la calidad de la certificación de defunciones en la región Ica, 2007 [Analysis of the quality of the certification of deaths in the Ica región, 2007]. Revista Perúana de Epidemiologia. 2013;17(1).
- 23.Dirección Técnica de Demografía e Indicadores Sociales del Instituto Nacional de Estadística e Informática (INEI). Perú: Estimaciones y Proyecciones de Población Total, por Años Calendario y Edades Simples, 1950–2050. Lima, Perú; 2009.
- 24.Perú Ministerio de Salud. Compendio de Estadísticas de Hechos Vitales: Perú 2011. Lima, Perú; 2013.
- 25.Perú Ministerio de Salud. Repositorio Único Nacional de Información en Salud (REUNIS). Available at http://www.minsa.gob.pe/reunis/index.asp?op=51&box=501&item=5013 [Accessed 2 May 2018].
- 26.Lefeuvre D, Pavillon G, Aouba A, Lamarche-Vadel A, Fouillet A, Jougla E, et al. Quality comparison of electronic versus paper death certificates in France, 2010. Popul Health Metr. 2014;12(1):3. doi: 10.1186/1478-7954-12-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pavillon GC, Coilland P, Jougla E. Mise en place de la certification électronique des causes médicales de décès en France : premier bilan et perspectives. BEH thématique. 2007;35–36:306–308. [Google Scholar]
- 28.WHO. International Statisticsal Classiciation of Diseases and Related Health Problems. 10th revision, vol. 2, 10th ed. Geneva: World Health Organization; 2016.
- 29.Aung E, Rao C, Walker S. Teaching cause-of-death certification: lessons from international experience. Postgrad Med J. 2010;86(1013):143–152. doi: 10.1136/pgmj.2009.089821. [DOI] [PubMed] [Google Scholar]
- 30.Walker S, Rampatige R, Wainiqolo I, Aumua A. An accessible method for teaching doctors about death certification. Health Inf Manag J. 2012;41(1):4–10. doi: 10.1177/183335831204100101. [DOI] [PubMed] [Google Scholar]
- 31.Lakkireddy DR, Basarakodu KR, Vacek JL, Kondur AK, Ramachandruni SK, Esterbrooks DJ, et al. Improving death certificate completion: a trial of two training interventions. J Gen Intern Med. 2007;22(4):544–548. doi: 10.1007/s11606-006-0071-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.University of Melbourne. Strategies for improving the quality of cause of death data in hospitals. CRVS development series. Melbourne, Australia: Civil Registration and Vital Statistics Improvement, Bloomberg Philanthropies Data for Health Initiative, University of Melbourne; 2017.
- 33.University of Melbourne. Assessing the quality of death certificates: Guidance for the rapid tool. CRVS resources and tools. Melbourne, Australia: Civil Registration and Vital Statistics Improvement, Bloomberg Philanthropies Data for Health Initiative, University of Melbourne; 2018.
- 34.Long JS. Regression models for categorical and limited dependent variables. Thousand Oaks. Sage Publications. 1997:297.
- 35.StataCorp. Stata 15.0. 2015; College Station: StataCorp LP.
- 36.United Nations. United Nations e-Government Survey . Gearing e-government to support transformation towards sustainable and resilient societies. New York: United Nations; 2018. p. 2018. [Google Scholar]
- 37.Abos R, Perez G, Rovira E, Canela J, Domenech J, Bardina JR. A pilot program to improve causes of death certification in primary care of Catalonia, Spain. Gac Sanit. 2006;20(6):450–456. doi: 10.1157/13096527. [DOI] [PubMed] [Google Scholar]
- 38.Myers KA, Farquhar DR. Improving the accuracy of death certification. CMAJ. 1998;158(10):1317–1323. [PMC free article] [PubMed] [Google Scholar]
- 39.Villar J, Perez-Mendez L. Evaluating an educational intervention to improve the accuracy of death certification among trainees from various specialties. BMC Health Serv Res. 2007;7. [DOI] [PMC free article] [PubMed]
- 40.Myers KA, Eden D. Death duties: workshop on what family physicians are expected to do when patients die. Can Fam Physician. 2007;53(6):1035–1038. [PMC free article] [PubMed] [Google Scholar]
- 41.Weeramanthri T, Beresford B. Death certification in Western Australia--classification of major errors in certificate completion. Aust J Public Health. 1992;16(4):431–434. doi: 10.1111/j.1753-6405.1992.tb00092.x. [DOI] [PubMed] [Google Scholar]
- 42.Naghavi M, Abajobir AA, Abbafati C, Abbas KM, Abd-Allah F, Abera SF, et al. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980-2016: a systematic analysis for the global burden of disease study 2016. Lancet. 2017;390(10100):1151–1210. doi: 10.1016/S0140-6736(17)32152-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Maudsley G, Williams EM. Death certification by house officers and general practitioners--practice and performance. J Public Health Med. 1993;15(2):192–201. [PubMed] [Google Scholar]
- 44.Messite J, Stellman SD. Accuracy of death certificate completion: the need for formalized physician training. JAMA. 1996;275(10):794–796. doi: 10.1001/jama.1996.03530340058030. [DOI] [PubMed] [Google Scholar]
- 45.Joshi R, Lopez AD, MacMahon S, Reddy S, Dandona R, Dandona L, et al. Verbal autopsy coding: are multiple coders better? Bull World Health Organ. 2009;87:51–57. doi: 10.2471/BLT.08.051250. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Attributes of death certificates assessed. (DOCX 13 kb)
Data Availability Statement
The data that support the findings of this study are available from the General Office of Information Technology (Ministry of Health, Perú) but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of the General Office of Information Technology (Ministry of Health, Perú).


