Abstract
Context:
Dengue fever (DF) altogether with its severe forms, dengue hemorrhagic fever (DHF) and dengue shock syndrome, has become public health concerns. Indonesia belongs to category A of endemicity for DF/DHF. One of the several efforts to control dengue virus infection in Indonesia is a passive surveillance called “Dengue Case Surveillance.” Timeliness report defined as a report sent within 24 h after the clinical diagnosis is needed to have a proper surveillance. The study on the evaluation of dengue case report in terms of accuracy, adequacy, and timeliness in Indonesia is still limited.
Aims:
The aim of this study was to identify the accuracy, adequacy, and timeliness from the reports of dengue viral infection (DVI) cases admitted from January 1 to December 31, 2015 to 7 major hospitals in Bandung, West Java, Indonesia.
Settings and Design:
This was a retrospective analysis study.
Materials and Methods:
To evaluate the accuracy, all medical records of DVI patients were reviewed epidemiologically, clinically, and laboratory using a standardized questionnaire. To evaluate the adequacy, hospital data were compared with reported data in Bandung Municipality Health Authority. To evaluate the timeliness of report, interview to the person in charge for dengue reporting cases in each hospital and in Bandung Municipality Health Authority were performed.
Statistical Analysis Used:
Univariate analysis was used for statistical analysis.
Results:
A total of 4096 (72%) of 5712 hospitalized DVI cases lived in Bandung Municipality. The accuracy of the clinical diagnosis was 3397 out of 4096 cases (82.9%). The adequacy of the accurate cases was 1553 out of 3397 cases (45.7%).
Conclusions:
The timeliness of report was varied, ranging from days to month. The accuracy of dengue cases was good, but the adequacy and timely reporting should be strengthened.
Keywords: Accuracy, adequacy, dengue, reporting, timely
INTRODUCTION
Dengue fever (DF) altogether with its severe forms, dengue hemorrhagic fever (DHF), and dengue shock syndrome (DSS), has become public health concerns. Over the past three decades, there has been a dramatic global increase in the frequency of DF, DHF, and DSS cases. Around 2.5 billion people, two-fifths of the world population, in tropical and subtropical countries, are at risk of being infected with dengue virus. It is estimated that 50 millions of dengue infections occur worldwide annually.[1]
Indonesia belongs to category A of endemicity for DF/DHF. It means that DF/DHF is a major public health problem and a leading cause of hospitalization or death among children. It also means that Indonesia has hyperendemicity of all four serotypes circulating in urban area, with the potential of spreading to rural area.[1] Data from 2016 report of Ministry of Health shows that dengue virus infection (DVI) is still a major health problem. It is found in all 34 provinces and 436 of 514 cities (85%) in the country. Cases reported in 2015 were 126,675 with 1229 fatalities, higher than 2014 of 100,347 cases with 907 deaths.[2]
One of several efforts to control DVI in Indonesia is a passive surveillance called “Dengue Case Surveillance.” In this surveillance, every DVI case should be reported to health authority, which is mandatory by law.[3] The aim of the surveillance is to monitor the dynamic of DVI in community which could predict epidemic so that a necessary action would be taken to prevent or to overcome the epidemic. This passive surveillance is less sensitive but is still a valuable tool in endemic countries with limited resources if it can fulfill a certain condition, such as an accurate, adequate, and timely report.[4]
Study on the evaluation of dengue case report in term of accuracy, adequacy, and timeliness in Indonesia is limited. Only one study had been performed in Bandung in 1994, which was more than 20 years ago. The study shows that the surveillance system for DHF/DSS in Bandung should be strengthened. DHF/DSS cases should be reported on the basis of a diagnosis made during hospitalization preferably after a serological confirmation is obtained.[5]
The aim of this study was to identify the accuracy, adequacy, and timeliness of the reports of hospitalized DVI cases in Bandung, West Java, Indonesia in 2015.
MATERIALS AND METHODS
Study design and subjects
This retrospective analysis study was conducted in the medical record department of 7 major hospitals in Bandung, West Java, Indonesia, that is, Dr. Hasan Sadikin Hospital, St. Borromeus Hospital, Adventist Hospital, St. Yusuf Hospital, Mother and Child Hospital Hermina Pasteur, Mother and Child Hospital Limijati, and Hermina Arcamanik Hospital. Patients included in this study are those having the ICD codes of A90–A91 for the final diagnosis in the medical resume and given informed consent to obtain the data needed. Those who had incomplete data were excluded from the study. The medical records of all DVI patients admitted from January 1 to December 31, 2015 were reviewed using a standardized questionnaire to evaluate epidemiological, clinical, and laboratory data. Only medical records of patients lived in Bandung Municipality were enrolled in this study. We also collected dengue case reporting data from Bandung Municipality Health Authority to be compared with reported case data from each hospital. To evaluate the timely report, we did an interview to the person in charge of dengue reporting cases in each hospital and to the person in charge of dengue control program in Bandung Municipality Health Authority.
Definitions
The accuracy of DVI case consists of confirmed, probable, and reportable cases.[1,6] Confirmed case was defined as clinical case with at least one of the following: virus culture, the detection of dengue virus antigen, viral genomic sequences detection by real-time polymerase chain reaction (RT-PCR), immunoglobulin M (IgM) seroconversion in paired sera, immunoglobulin G (IgG) seroconversion in paired sera, or fourfold IgG titer increase by haemagglutination inhibition (HI) test in paired sera. Probable case was defined as clinical case supported by serology test in single serum: IgM (+) or IgG (+) titer of 1280 or greater by HI test.[1] Reportable case was defined as patient with provisional diagnosis of DHF or DSS with a history of exposure in a dengue endemic or epidemic area.[6] Adequate was defined if the number of accurate diagnosis of DVI was similar to data from Bandung Municipality Health Authority. Timely was defined as reporting should be sent within 24 h after the clinical diagnosis has been made.
Statistical analysis
Statistical analysis was performed to evaluate the differences among age subgroups. For univariate analysis, a Chi-square analysis was performed for the categorical variables. P < 0.05 was considered to be statistically significant. SPSS (IBM Corp. Released 2013. IBM SPSS Statistics for Windows, Version 21.0. Armonk, NY: IBM Corp.) was used for all analyses.
Ethical clearance
The Health Research Ethics Committee Medical Faculty Universitas Padjadjaran approved the study proposal, and Bandung Health Authority gave the permission to conduct this study.
RESULTS
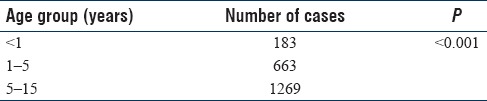
From January 1 to December 31, 2015, there were 5712 DVI cases hospitalized in 7 Bandung major hospitals. Out of those, 4096 (72%) cases lived in Bandung Municipality. Table 1 shows the number of patients living in Bandung Municipality from each hospital. Patients ≤15 years of age were found in 2115 (52%) cases, which is not so different from the number of patient in older age group which were 1981 (48%) cases. Among patients <15 years of age, we found that the most prevalent cases were found in the age group of 5–15 years old [Table 2].
Table 1.
Number of dengue viral infection cases by hospitals
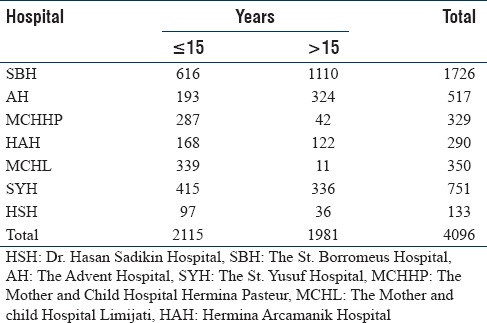
Table 2.
Age group distribution in cases <15 years old
In 3552 of 4096 (86.7%) cases, the duration of fever before admission was written on the medical records, while 1872 (52.1%) cases had three or less duration of fever on admission. Among these patients, 1040 (55.6%) were children under 15 years old.
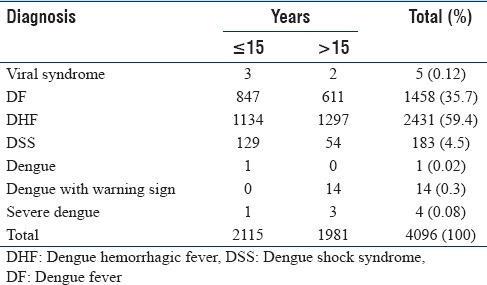
The terminology of clinical diagnosis of the patients was mostly following the criteria of World Health Organization (WHO) 1997/WHO 2011 guidelines. Only 0.4% used the criteria of WHO 2009 as dengue, dengue with warning signs, and severe dengue [Table 3].[7] Table 3 also reveals that even the most prevalent diagnosis was DHF, while the proportion of DF which actually in most cases could be managed as outpatient was also high (1458 or 35.7% cases). DSS was found in 183 cases and mostly found in children ≤15 years (129 or 70.5% cases vs. 54 or 29.5% cases, P < 0.001), fatal cases were found in 7 patient (0.17%) due to severe bleeding manifestation which were hematemesis, melena, and hematemesis melena that might be the sign of disseminated intravascular coagulopathy (DIC), encephalopathy that manifest as loss of consciousness with or without seizure, and prolonged shock.
Table 3.
Clinical diagnosis of dengue viral infection
Accuracy
Laboratory confirmation of the clinical diagnosis of DVI in this study used the rapid method of NS-1 dengue antigen and rapid method of serology test for the detection of IgM and IgG antidengue. Other sophisticated test like genomic virus sequences by RT-PCR was not a practice in daily management of DVI in Bandung. Patients who were admitted in early course of illness underwent NS-1 Dengue Antigen test, patients who had negative result underwent serology test on day 5 or 6. Patients who were admitted in the late course of illness underwent only serology test. No cases underwent serology test in paired sera. The results of detected NS-1 dengue antigen and IgM antidengue were summarized on Table 4.
Table 4.
Laboratory confirmation of the clinical diagnosis of dengue viral infection
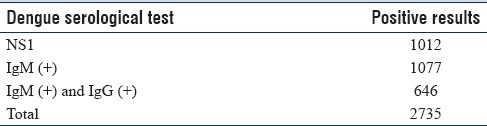
Confirmed cases based on NS-1 dengue antigen detection were found in 1012 (24.7%), probable case based on the detection of IgM antidengue alone or in combination with IgG antidengue was found in 1723 (42.1%).
The analysis of clinical diagnosis of 1361 (33.2%) patients with both negative detection of NS-1 dengue antigen and IgM antidengue, revealed DHF and DSS were found in 607 (44.6%) cases and 55 (4%) cases, respectively. The unique clinical features of DHF and DSS and its potential morbidity and fatality were considered as reportable cases. Hence, the accuracy of hospitalized patient in this study was the sum of confirmed, probable, and reportable cases, which were 3397 of 4096 cases (82.9%).
Adequacy
Data from Bandung Municipality Health Authority revealed that only 1553 hospitalized cases with suspected DF, DHF, and DSS were reported. If we compare that to the number of accurate diagnosis which was 3397, the adequacy of case reporting was 45.7%.
Timeliness
To evaluate the timely report, interviews were performed to the person in charge for dengue surveillance program in Bandung Municipality Health Authority and to persons in charge for case reporting in 7 major hospitals. Interview revealed varied responds, ranging from days to month sent by electronic mail whom often were not notified by the Municipality Health Authority.
DISCUSSION
From January 1 to December 31, 2015, there were 4096 cases out of 5712 hospitalized DVI lived in Bandung Municipality. Although cases in children <15 years old were more prevalent than cases in age group >15 years old, the difference was not significant [Table 1]. In children <15 years old group, DVI in 5–15 years group were significantly different with younger age group [Table 2]. Some previous studies showed the predominance of DF among children, nonetheless, certain studies have reported a changing epidemiological distribution in age group.[8,9,10,11,12] This study consistent with the data from the experience of 45-years incidence of DHF in Indonesia that revealed an increasing cases in over 15 years old, while in under 5 years old, it remained stable,[13] a pattern that has been observed in other high endemic Southeast Asia countries.[10,12,14] The demographic changes, that is, birth and death rate changes influence in the age distribution of cases.[10]
In 3552 cases (86.7%), the duration of fever before admission was known, 1872 (52.1%) cases were admitted on or before the 3rd days of fever. This data showed the increase awareness about DVI in the community.
The clinical diagnosis of cases, were mostly followed the WHO classification 1997/2011, only a very small proportion (0.46% of cases) followed the WHO classification 2009 [Table 3]. To achieve universal consensus regarding the clinical case classification of dengue virus-infected patients, the WHO released the guidelines. In the original guidelines WHO 1997,[6] patients are classified into three separate categories: DF, DHF, and DS. The utility and accuracy of this guideline had been a matter of debate. Therefore, reassessment of the classification criteria were proposed by several study groups, prompting the WHO to issue a revised classification, the 2009 WHO guideline,[7] which distinguish between severe and nonsevere dengue. To focus on new/additional topics of current in relevance to the member States of the Southeast Asia Region including Indonesia, the WHO-SEARO 2011, issued a classification which added expanded dengue syndrome/isolated organopathy (unusual manifestation) into the 1997 guideline.[1] For the purpose of surveillance, the classification of clinical diagnosis should be uniform. Systematic literature review[15] showed that the WHO classification 2009 has a high sensitivity but less specific, that can result in the increase of dengue cases admitted to the hospital.
Table 3 also shows the high proportion of DF which was 1458 (35.7%) cases, as DHF, a severe form of DVI, is not a continuum of DF,[1] most of DF could be treated as outpatient. However, in the early course of illness, signs, and symptoms of DF undistinguishable with DHF, after a few days with the appearance of plasma leakage the clinical diagnosis of DHF could be made.[6] Even though DHF occurs only in small proportion of DVI,[1] the severe complication such as shock or even death is unpredictable. This fact combined with the difficulty to distinguish DF from DHF in the early course of illness leads the parent and physician so worry about DHF, unnecessary hospitalization of children will take place. This phenomenon, especially occurs in regions with a high incidence of DHF cases, high rate of unnecessary hospitalizations results in burden disease for the nation. Shepard et al., 2013[16] estimated that economic and disease burden of dengue in Indonesia was the highest among Southeast Asia countries.
To minimize unnecessary hospitalization, The Working Group on Infectious and Tropical Diseases-The Indonesian Paediatric Society[17] recommends to treat DF as outpatient if there are no severe vomiting, no comorbids like thalassemia, etc., and warning sign(s) for DHF. Some notes of warning signs should be educated to the patient. The patient should come back immediately if the warning sign(s) appears, if it does not appear the patient should come every day for physical and laboratory evaluation. Social indications for admission are if the patient lives far from medical facility or if parent or caregiver is considered not capable to monitor the patient's condition at home. This retrospective study could not determine whether the high prevalence of DF hospitalization was due to correct indication or DHF phobia or in combination.
Accuracy
Accuracy is the important element in case surveillance to avoid overreporting which results in unnecessary action of health authority. This study showed that in 1872 (52.1%) cases were admitted on or before the 3rd day as of fever; these patients were the candidates to undergo NS-1 dengue antigen assay. This test could be detected until the 5th day of illness; however, the high sensitivity is on the first 2 days which around 83.3% to 92.9%.[18] The specificity of this test is 100%,[18,19] so patient which detected for NS-1 dengue Antigen is considered as confirmed case. The benefit of this test is early case detection and early report to Municipality Health Authority, but on the other hand, there were some studies that revealed unnecessary pressure of the parents for hospitalization of the children with detected NS1 dengue antigen.[20] Table 4 shows NS-1 dengue antigen detection was found in 1012 (24.7%), while probable case which was based on the detection of IgM antidengue alone or in combination with IgG antidengue was found in 1723 (42.1%).
In this study, no paired sera for serology tests was performed, therefore, the number of Ig M or IgG seroconversion was unknown. Further analysis of 1136 (33.2%) cases with both negative detection of NS-1 dengue antigen and IgM antidengue, revealed DHF and DSS was found in 607 (44,6%) and 55 (4%) cases, respectively. The unique clinical features of DHF and DSS and its potential morbidity and fatality were consider as reportable case.[6] Beside that, some studies estimated that for 1 case of DSS there usually 150 cases of DVI in the neighborhood.[6] Therefore, the accuracy of hospitalized patient in this study is the sum of confirmed, probable, and reportable cases, which was totally 3397 of 4096 cases (82.9%). This accuracy is higher than earlier study 20 years ago,[5] which was 76%.
Adequacy
Only 1153 (45.7%) cases out of 3397 accurately diagnosed of DVI found in the Municipality Health Authority data. Even though this adequacy is higher than earlier study conducted in the same area in 1994,[5] but still considered as underreporting. Since the short definition of surveillance is data collecting for action, underreporting would delay the action taken by health authority in case of if there is an outbreak. Passive surveillance itself is less sensitive in predicting an outbreak, underreporting would worsen the prediction. Interview to person in charges for dengue case reporting in both hospitals and Municipality Health Authority could not elicit the exact cause of this underreporting. Further prospective study is needed to find out this problem.
Timeliness
This study showed that the timely reporting was weak in fulfilling the regulation that every case should be reported within 24 h after the diagnosis had been made. Interview to person in charges for dengue case reporting in both hospitals and Municipality Health Authority revealed a variable response, ranging from days to month. Detection of NS-1 dengue antigen was found 1012 (24.7%) cases, the result of the test is rapid, <24 h. This test should be a benefit in reporting case to the Municipality Health Authority timely. The result of serology assay may take a little more time, 1–2 days using enzyme-linked immunosorbent assay method. Reportable case should be analyzed carefully and reported immediately, especially if the case is DSS.
Limitation
This study is a retrospective study, some important data such as the cause of poor adequacy and timely report could not elicit properly.
CONCLUSIONS
The hospital-based surveillance for dengue case report showed a good accuracy, but the adequacy and timeliness aspects should be strengthened.
Financial support and sponsorship
This study was financially supported by an Academic Leadership Grant (ALG) from Universitas Padjadjaran.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
This study was supported by an Academic Leadership Grant (ALG) from Universitas Padjadjaran. Professor Alex Chairulfatah, MD is the recipient of ALG from Universitas Padjadjaran.
REFERENCES
- 1.World Health Organization-SEARO. Comprehensive Guidelines for Prevention and Control of Dengue and Dengue Hemorrhagic Fever. New Delhi: World Health Organization; 2011. [Google Scholar]
- 2.InfoDATIN: Dengue Hemorrhagic Fever Situation in Indonesia. 2016. Apr 30, [Last download on 2017 Apr 21]. Ministry of Health Republic of Indonesia. Available from: http://www.depkes. go.id . [Google Scholar]
- 3.Ministry of Health Regulation No. 560/Menkes/Per/VIII/1989. Jakarta: Ministry of Health; 1989. Ministy of Health Republic Indonesia. [Google Scholar]
- 4.Ludovice ZO. Data needs and gaps in diseases surveillance to support primary health care. In: Azuri JC, editor. Diseases Surveillance in Primary Health Care. Tokyo: Southeast Asia Information Center; 1983. pp. 116–9. [Google Scholar]
- 5.Chairulfatah A, Setiabudi D, Agoes R, van Sprundel M, Colebunders R. Hospital based clinical surveillance for dengue Haemorrhagic fever in Bandung, Indonesia 1994-1995. Acta Trop. 2001;80:111–5. doi: 10.1016/s0001-706x(01)00180-2. [DOI] [PubMed] [Google Scholar]
- 6.World Health Organization. Dengue Hemorrhagic Fever: Diagnosis, Treatment and Control. Switzerland: World Health Organization; 1997. [Google Scholar]
- 7.World Health Organization. Dengue Guidelines for Diagnosis, Treatment, Prevention and Control. Geneve: World Health Organization; 2009. [PubMed] [Google Scholar]
- 8.Guha-Sapir D, Schimmer B. Dengue fever: New paradigms for a changing epidemiology. Emerg Themes Epidemiol. 2005;2:1. doi: 10.1186/1742-7622-2-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Beatty ME, Stone A, Fitzsimons DW, Hanna JN, Lam SK, Vong S, et al. Best practices in dengue surveillance: A report from the Asia-Pacific and Americas dengue prevention boards. PLoS Negl Trop Dis. 2010;4:e890. doi: 10.1371/journal.pntd.0000890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cummings DA, Iamsirithaworn S, Lessler JT, McDermott A, Prasanthong R, Nisalak A, et al. The impact of the demographic transition on dengue in Thailand: Insights from a statistical analysis and mathematical modeling. PLoS Med. 2009;6:e1000139. doi: 10.1371/journal.pmed.1000139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Thai KT, Nishiura H, Hoang PL, Tran NT, Phan GT, Le HQ, et al. Age-specificity of clinical dengue during primary and secondary infections. PLoS Negl Trop Dis. 2011;5:e1180. doi: 10.1371/journal.pntd.0001180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ooi EE, Gubler DJ. Dengue in Southeast Asia: Epidemiological characteristics and strategic challenges in disease prevention. Cad Saude Publica. 2009;25(Suppl 1):S115–24. doi: 10.1590/s0102-311x2009001300011. [DOI] [PubMed] [Google Scholar]
- 13.Karyanti MR, Uiterwaal CS, Kusriastuti R, Hadinegoro SR, Rovers MM, Heesterbeek H, et al. The changing incidence of dengue haemorrhagic fever in Indonesia: A 45-year registry-based analysis. BMC Infect Dis. 2014;14:412. doi: 10.1186/1471-2334-14-412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Muhammad Azami NA, Salleh SA, Neoh HM, Syed Zakaria SZ, Jamal R. Dengue epidemic in Malaysia: Not a predominantly urban disease anymore. BMC Res Notes. 2011;4:216. doi: 10.1186/1756-0500-4-216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Horstick O, Jaenisch T, Martinez E, Kroeger A, See LL, Farrar J, et al. Comparing the usefulness of the 1997 and 2009 WHO dengue case classification: A systematic literature review. Am J Trop Med Hyg. 2014;91:621–34. doi: 10.4269/ajtmh.13-0676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shepard DS, Undurraga EA, Halasa YA. Economic and disease burden of dengue in Southeast Asia. PLoS Negl Trop Dis. 2013;7:e2055. doi: 10.1371/journal.pntd.0002055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hadinegoro SR, Moedjito I, Chairulfatah A, editors. Guidelines of Diagnosis and Treatment of Dengue Virus Infection in Children. Jakarta: IDAI; 2016. Working Group on Infectious and Tropical Pediatric-Indonesian Pediatric Society. [Google Scholar]
- 18.Ahmed NH, Broor S. Comparison of NS1 antigen detection ELISA, real time RT-PCR and virus isolation for rapid diagnosis of dengue infection in acute phase. J Vector Borne Dis. 2014;51:194–9. [PubMed] [Google Scholar]
- 19.Aryati A, Trimarsanto H, Yohan B, Wardhani P, Fahri S, Sasmono RT, et al. Performance of commercial dengue NS1 ELISA and molecular analysis of NS1 gene of dengue viruses obtained during surveillance in Indonesia. BMC Infect Dis. 2013;13:611. doi: 10.1186/1471-2334-13-611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pothapregada S, Kamalakannan B, Thulasingam M, Sampath S. Is reactive dengue NS1Antigen test a warning call for hospital admissions? J Clin Diagn Res. 2016;10:SC04–7. doi: 10.7860/JCDR/2016/16178.7636. [DOI] [PMC free article] [PubMed] [Google Scholar]


