Abstract
STUDY QUESTION
Can the high rate and associated burden of unintended pregnancy (UP) and adolescent pregnancy in Latin America and the Caribbean (LAC) be reduced through wider access to and use of long-acting reversible contraceptive (LARC) methods?
SUMMARY ANSWER
Studies show that impoved access to and use of LARC methods is an effective tool for reducing the high rates of UP, unsafe abortion and abortion-related complications, and maternal deaths (as well as reducing their social and financial burden), and we have provided recommendations to help achieve this in LAC.
WHAT IS KNOWN ALREADY
LAC comprises 46 countries with 650 million inhabitants, and shows large disparities in socioeconomic development, access to health services and attention to sexual and reproductive health rights. The exercise of these rights and universal access to sexual and reproductive health (SRH) programmes is a key strategy for improving maternal health by reducing the number of UPs, the rate of women’s and child mortality and morbidity, and the number of unsafe abortions. The implementation of SRH programmes in the region has contributed to a decrease in pregnancy rates of more than 50% over 40 years. However, despite this progress, the numbers of UP and adolescent pregnancies are still among the highest worldwide, which can be attributed in large part to the low prevalence of use of LARC methods.
STUDY DESIGN, SIZE, DURATION
This is a position paper with the objective of reviewing the magnitude and burden of UP in LAC, as well as available LARC methods and barriers to their access, with the goal of increasing knowledge and awareness among healthcare professionals (HCP), policymakers and the general public about the potential to reduce UP rates through the increased use of LARC.
PARTICIPANTS/MATERIALS, SETTING, METHOD
We searched the electronic databases of PubMed and EMBASE to identify studies published up to May 2017. We also searched for websites regarding LAC, LARC methods, and UP including, for example, those from the United Nations, the World Health Organization, Pan American Health Organization, the Alan Guttmacher Institute and the United States Agency for International Development. Studies were included if they investigated mainly UP and their consequences as well as the use of LARC methods in the region. During 3 days of meetings, the importance of the studies identified and the appropriateness of inclusion were discussed.
MAIN RESULTS AND THE ROLE OF CHANCE
LAC is not one unit and shows great ethnic diversity as well as economic and cultural differences among the various countries. These differences must be taken into account when developing policies related to disseminating information and combatting misinformation regarding the use of LARC among different audiences, such as adolescents and young women, nulligravidas, indigenous populations and women with disabilities. Furthermore, only some governments have made efforts to increase accessibility to LARC methods, and there is a need to implement training programmes for HCPs, launch education campaigns for the general public, increase access and review the cost-benefit analyses specific to LARC, which have already demonstrated that the upfront cost of LARC is less than the cummulative expense of short-term contraceptives. Recommendations to achieve these goals are presented.
LIMITATIONS, REASONS FOR CAUTION
Knowledge and awareness of the contraceptive method itself and of the mix of individual countries in the region is essential to the development of specific strategies and actions, tailored to each particular country situation, aimed at increasing access to modern contraceptive methods, especially LARC.
WIDER IMPLICATIONS OF THE FINDINGS
Healthcare systems in LAC should consider LARC as a primary option for decreasing UP and adolescent pregnancy. Disseminating information, increasing awareness of their efficacy, removing barriers and improving access to LARC methods are the urgent actions recommended for government, academia, professional organizations, insurance companies and policymakers in order to address this major public health problem in LAC.
STUDY FUNDING/COMPETING INTERESTS
This manuscript was supported by a grant from the Americas Health Foundation (AHF), a 501(c)3 nonprofit organization dedicated to improving healthcare throughout the Latin American Region. LB and IM received additional support from the São Paulo Research Foundation (FAPESP) award # 2015/20504-9. The authors declare no conflict of interest.
Keywords: contraception, Latin America, Caribbean, long-acting reversible contraceptives, unplanned pregnancy, unsafe abortion, adolescents, fertility rate, burden of unplanned pregnancy, maternal mortality
Introduction
Latin America and the Caribbean (LAC or ‘the region’) comprises 46 countries with 650 million inhabitants and large disparities exisit in socioeconomic development, access to health services and attention to sexual and reproductive health rights (SRHR). An important component of SRHR is empowering women and men to control childbearing and plan fertility. The excercise of SRHR and universal access to sexual and reproductive health (SRH) programmes is a key strategy for improving maternal health by reducing the number of unintended pregnancies (UPs), the rate of women’s and child mortality and morbidity, and the number of unsafe abortions (Gipson et al., 2008; United Nations, 2015a).
The implementation of SRH programmes in LAC has contributed to a decrease in pregnancy rates of more than 50% over 40 years (Sedgh et al., 2014). Despite this progress, a high rate of UP still exists (about 60% of pregnancies in the region are UP), which can be attributed in large part to the low rates of use of long-acting reversible contraceptive (LARC) methods. Although UP rates in LAC are decreasing, they are still among the highest worldwide (with the exception of Mexico) (Sedgh et al., 2014). Consequently, the objective of this paper is to review the magnitude and burden of UP in LAC, as well as the availability of LARC methods and barriers to access, with the goal of increasing knowledge and awareness among healthcare professionals (HCPs), policymakers and the general public about the potential to reduce UP rates through the increased use of LARC methods.
WHAT DOES THIS MEAN FOR PATIENTS?
This paper looks at the use of long-acting reversible contraceptives, such as implants or intrauterine devices (coils), in Latin America and the Caribbean.
The researchers found that these regions have some of the highest rates of unplanned and adolescent pregnancies in the world, and suggest that one of the key reasons for this is the low use of long-acting reversible contraceptives. They suggest that long-acting reversible contraception is a good option because it is safe and effective with low failure rates and women do not have to do anything once they have had the contraceptive fitted.
The paper recommends that long-acting contraceptives should be the first option in this region for reducing unplanned pregnancies, and suggests that awareness campaigns and training for healthcare professionals could help improve the take-up.
Materials and Methods
We searched the electronic databases of PubMed and EMBASE to identify studies published up to May 2017. We also searched for websites regarding LAC, LARC methods, and UP including, for example, those from the United Nations, the World Health Organization, Pan American Health Organization, the Alan Guttmacher Institute and the United States Agency for International Development. Studies were included if they investigated mainly UP and their consequences as well as the use of LARC methods in the region. The authors of this study discussed, during 3 days of meeting, the importance of the studies identified and the appropriateness of inclusion.
The Burden of UP in LAC
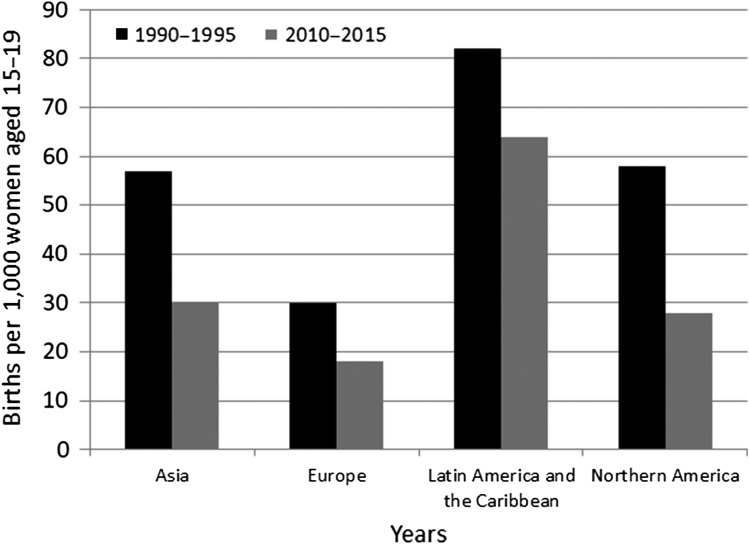
UP is defined as a pregnancy that is unwanted or that occurs before a desired point in time for the woman and encompasses emotional, cognitive and social factors (Tsui et al., 2010). UP is mainly a consequence of two factors: nonuse of contraceptive methods and contraceptive failure related to method failure or incorrect use (Cleland and Ali, 2004). In LAC, the implementation of SRH programmes has been associated with an increase in modern contraceptive use among women aged 15–49 years (Clifton and Kaneda, 2013). This translates into a decrease of 50% in total fertility rates (TFR) observed between 1980 and 2015 (decreasing from 4.2 to 2.1 births per woman aged 15–49 years) and a decrease of 29.1% in adolescent fertility rates (decreasing from 89.8 to 63.7 births per 1000 women aged 15–19 years) (World Bank, 2015). However, the adolescent fertility rate in LAC is still higher compared to Asia, USA or the European countries (Fig. 1).
Figure 1.
Adolescent birth rate by region, in 1990–1995 and 2010–2015 (adapted from World Fertility Patterns 2015—United Nations, 2015c).
Despite this significant reduction in TFR, UP rates only decreased by 4% between 1985 and 2015 (Sedgh et al., 2014). UP is associated with various factors that negatively affect maternal and child health, such as medical termination in unsafe conditions (Gipson et al., 2008), inadequate antenatal care, adolescent pregnancy and exacerbation of socioeconomic and health disparities.
Among sexually active women who are married or in union, 10.7% of women worldwide have an unmet need for contraception, although this number has been decreasing (United Nations, 2015b). The unmet need for SRH planning among women aged 15–49 years who are married or in union was 16% in the Caribbean (the highest in LAC), while Central and South America had rates of 11% and 10%, respectively (Alan Guttmacher Institute, 2017). However, it is important to note that these data exclude sexually active women who are not married or in union. Thus, the unmet need for contraception and SRH planning is likely higher.
Unsafe medical termination
Despite the fact that many countries in LAC restrict or prohibit abortion, between 40 and 42% of UP in LAC end in medical termination (Sedgh et al., 2014). Consequently, the World Health Organization (WHO) estimated that, in 2015, 6.5 million unsafe medical terminations occurred in LAC (Sedgh et al., 2016). Unsafe medical termination is performed outside medical facilities, in unsanitary conditions and/or with untrained HCP. Often women lack adequate post-abortion care, which can lead to complications such as post-abortion sepsis, haemorrhage, genital trauma and maternal death (WHO, 2011; Shah et al., 2014; ESHRE, 2017). A previous study reported an unsafe abortion rate of 31 per 1000 women aged 15–44 years in LAC (Sedgh et al., 2012). Moreover, in 2011, the WHO estimated that complications due to unsafe abortions in the region were responsible for 12% of maternal deaths (WHO, 2011), a rate that is 10 times higher than in Europe (Shah and Åhman, 2010; Åhman and Shah, 2011; WHO, 2011).
Inadequate antenatal care
Women carrying an UP are more prone to delaying or not seeking antenatal care (Dibaba et al., 2013; Guliani et al., 2014) and are thus at a higher risk of inadequate prenatal care when compared to women with planned pregnancies (Marston and Cleland, 2003; Dean et al., 2014; Dansereau et al., 2016), which is associated with twice the risk of severe maternal morbidity, including postpartum haemorrhage, eclampsia and placental abruption, when compared to women with adequate antenatal care. Also, an UP is associated with twice as high a risk of perinatal morbidity, including premature birth, severe intrauterine growth restriction and foetal death (Linard et al., 2017).
Adolescent pregnancy
Because of their high fertility, one of the groups most vulnerable to UP is adolescents. Despite a decrease in TFR in LAC, the rate of UP in adolescents has remained largely unchanged, or even increased (Prada et al., 2011), with 32–45% of the pregnancies in adolescents reported as unplanned (Cleland and Ali, 2004). Several reasons for this problem are that adolescents and young women fail to use contraceptive methods, choose to use less effective methods (Internal Displacement Monitoring Centre Norwegian Refugee Council, 2010), or lack access to contraceptives or SRH services. Moreover, misinformed HCPs sometimes impose nulliparity and age as a barrier to the use of LARCs, specifically intrauterine contraceptives (IUCs) (Bahamondes et al., 2015a). When compared with pregnant adult women, pregnant adolescents are at a higher risk of neonatal morbidity and mortality, and maternal morbidity and mortality (Conde-Agudelo et al., 2005; Ganchimeg et al., 2013).
Socioeconomic and health disparities
While many population studies about SRH planning in LAC treat the region as one unit, the use of LARC varies widely between LAC countries (Haiti, El Salvador, Honduras and Nicaragua are classified as low- and lower-middle-income countries, while Argentina, Brazil, Colombia, Chile and Mexico are classified as high- or upper-middle-income countries (http://databank.worldbank.org/data/download/site-content/OGHIST.xls, last accessed 29 July 2017)) and is highly impacted by government programmes and country income level (Tsui et al., 2010; United Nations, 2015b). This is especially true in high-risk groups such as adolescents (Souza et al., 2017; Svanemyr et al., 2017; Villalobos et al., 2017) and low-income women in rural settings with limited access to healthcare (Schuck-Paim et al., 2016). There are millions of low-income women in the region who are socially and economically disadvantaged and have an unmet need for contraception, often resulting in higher rates of UP (Marston and Cleland, 2003; Sedgh et al., 2014). This negatively affects maternal and child health, and is a factor in propagating the vicious circle of impoverishment (Marston and Cleland, 2003). In fact, although 62% of women aged 15–49 years in LAC seek to avoid a pregnancy, it is estimated that 22% of these women are not using an effective contraceptive method, accounting for 75% of all UP in the region (United Nations, 2015b).
LARC Prevalence in LAC
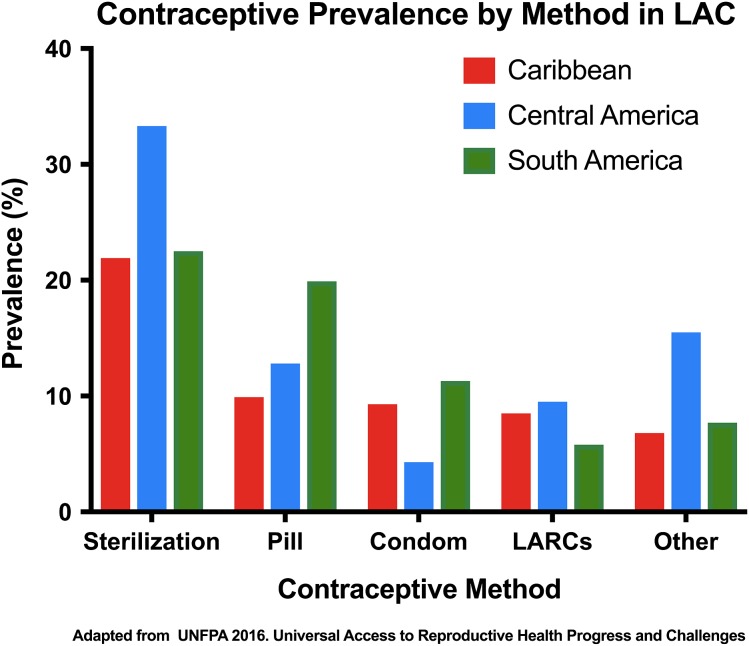
In LAC, 72.7% of sexually active women who are married or in union use some method of modern contraception. Within LAC, South America has the highest prevalence rate of modern contraceptive use (75%), followed by Central America (71%) and the Caribbean (62%) (UNFPA, 2016a). In the region, Guyana and Haiti had the lowest contraceptive prevalence rates (45% and 38%, respectively), while Nicaragua had the highest (80%). Brazil, Mexico, Peru and Colombia all had contraceptive prevalence rates between 70% and 78% (Alkema et al., 2013; UNFPA, 2016a, b). While the prevalence of the use of contraceptive methods has been increasing, the rate remains below the European and North American averages (UNFPA, 2016c).
Modern contraceptive methods can be split into three categories: permanent contraception, LARC, and short-acting reversible contraceptives (pills, injectables, patch, vaginal ring). In the region, short-acting reversible contraceptive methods account for 31.7% (mainly the contraceptive pill) of contraceptive use, while permanent female contraception accounts for 25.7%, and LARC methods account for only 6.7% (IUC 6.4%, implant 0.3%). The prevalence of the use of LARC methods varies widely both across regions and between countries in LAC (Alkema et al., 2013; United Nations, 2015a).
Contraceptive method mix (the percentage distribution of contraceptive users in a given country) is a tool for measuring the level of choice that women have regarding contraceptive methods (USAID, 2012). The prevalence of use of modern contraceptive methods varies widely between the three regions (Fig. 2).
Figure 2.
Contraceptive prevalence by method among sexually active women in Latin America and the Caribbean who are married or in union. LAC, Latin America and the Caribbean; LARCs, Long-Acting Reversible Contraceptive methods; Pill, oral contraceptive pill.
Contraception among adolescents
Among sexually active adolescent girls who are married or in union, the use of contraception has increased, but current levels are still lower than for other age groups. About 46% of these adolescents use some method of modern contraceptive but LARC account for only 5% of methods used. Among sexually active adolescents who are unmarried, the use of modern contraceptives is 65%, but LARC accounts for only 8% of use (UNFPA, 2016a, b). Knowledge and awareness of the contraceptive method mix of individual countries in the region is essential to the development of specific strategies and actions, tailored to each particular country situation, aimed at increasing access to modern contraceptive methods, especially LARC.
Safety and Effectiveness of LARC in LAC
All LARC methods are safe and highly effective. While short-acting reversible contraceptives require frequent attention from the user, which can decrease effectiveness, the effectiveness of LARC is independent of user behaviour. With perfect use, both short-acting contraceptives and LARC are highly effective, with failure rates between zero and 0.3/100 women years (W-Ys) (Trussell, 2011). However, with typical use, short-acting contraceptives presented failure rates higher than expected, while the failure rates for LARC remained unchanged, resulting in pregnancy rates of less than 1/100 W-Ys (Espey and Ogburn, 2011; Trussell, 2011; Bahamondes et al., 2014, 2015a; United Nations, 2015b).
When addressing the safety of LARC methods, one of the concerns regarding copper intrauterine device (IUD) use is the fear of developing pelvic inflammatory disease (PID), and future infertility mainly in young nulliparous women. However, several studies have found that after the first 20 days of insertion, the risk of PID is the same in both users and nonusers (Toivonen et al., 1991; Tsanadis et al., 2002; Lyus et al., 2010; Jatlaoui et al., 2016). Although another study showed that the rate of PID was slightly higher in the IUD group than the non-IUD group (0.46 and 0.09, respectively), the occurrence of PID was rare in both groups (<1.0%) (Birgisson et al., 2015), and the slightly higher rate could be explained by the reduced rate of condom usage in the IUD group. Moreover, when considering the safety of IUCs among young IUC users, a systematic review found that the risk of adverse outcomes related to pregnancy, perforation, infection, heavy menstrual bleeding or removals for bleeding was low. The risk of expulsion, especially for copper IUDs, however, is higher for younger women compared with older women (Jatlaoui et al., 2017).
Another common concern when using LARC methods is the risk of side effects. Side effects among all methods are low and generally similar, although IUD users reported a higher rate of lower abdominal pain and heavy menstrual bleeding than implant users (Bahamondes et al., 2015b). In a recent study comparing the use of the one-rod etonogestrel (ENG)—and the two-rod levonorgestrel (LNG)—implants with the copper IUD, the ENG- and LNG-implants both had very high and undistinguishable contraceptive efficacy (0.4/100 W-Y). Moreover, the continuation rates for the two implants were similar up to 2.5 years, and the continuation rate for the two implants combined was higher than that of the copper IUD. Bleeding disturbances were the most frequent reason for stopping the use of both implants and the IUD (Bahamondes et al., 2015b).
One option for increasing the use and cost-effectiveness of LARC is to extend their use beyond the lifespan labelled by health authorities (Hidalgo et al., 2009; McNicholas et al., 2015). In the case of the levonorgestrel releasing-intrauterine system (LNG-IUS), a study conducted by the WHO evaluating 1884 users (Rowe et al., 2016) presented a cumulative 7-year pregnancy rate of 0.5/100 W-Y. Although the data are insufficient to concretely recommend use beyond 5 years, it is reasonable to counsel women to maintain the same device for up to 7 years. Regarding the ENG-implant, in a WHO study with 390 women who used the implant for at least 5 years, no pregnancies occurred during the additional 2 years of follow-up. The overall 5-year cumulative pregnancy rate for the ENG-implant was 0.6 per 100/W-Y. The extended use of the ENG-implant showed 100% efficacy in Years 4 and 5 (Ali et al., 2016).
Success of LARC in Reducing Rates of Unwanted Pregnancy in Other Regions
The USA provides one example of a successful reduction in UP through the increased use of LARC. In this case, while the use of contraceptive methods increased only slightly between 2008 and 2012 (Jones et al., 2012; Branum and Jones, 2015; Daniels et al., 2015; Finer and Zoina, 2016), the use of LARC increased from 4% to 12% (Alan Guttmacher Institute, 2017; Kavanaugh et al., 2015), while the rate of abortions decreased by 13%. Morever, in the US-based CHOICE study, when given an option 67.1% of women chose LARC (Secura et al., 2010) and the UP rates were significantly lower among LARC users than among non-LARC users at 1, 2 and 3 years (Reeves et al., 2016). In addition, the US CHOICE study also showed a reduction of 50% in the overall abortion rate, and a reduction of 56% among adolescents (Peipert et al., 2012). When women had access to LARC at no cost, they presented a more evident reduction in UP (Winner et al., 2012). The continuation rates of LARC were higher than 80%, while those of the oral contraceptive pill were 55%. Satisfaction rates for LARC were higher than for the pill (over 80% versus 54%) (Peipert et al., 2011). Another study conducted in Brazil showed that the provision of no-cost LARC decreased not only the rates of UPs but also maternal-infant mortality and morbidity, and induced abortion rates (Bahamondes et al., 2014; Ferreira et al., 2017).
Barriers to Access to LARC in LAC
Barriers to the access and use of LARC methods result in a greater number of Ups, including among adolescents, and negatively affects both individual and collective health, particularly that of low-income and adolescent women. Factors hindering access to use can be of a subjective nature (misinformation, myths and beliefs) or of an objective nature (institutional, service-related, training-related, cost-related and others). Myths associated with the use of LARC, despite scientific evidence to the contrary, represent significant access barriers for LARC methods and contribute to the low rate of use of LARC methods in LAC (Luchetti and Romero, 2017).
The relatively high cost of LARC methods when compared with other contraceptives is a significant factor in obtaining access to these methods (Dehlendorf et al., 2010). Women of lower socioeconomic levels have more difficulty in accessing LARC due to insufficient availability at public services, high cost at private services, or the lack of reimbursement by private insurance. However, one study showed that when LARC were offered at no cost for potential users, they were well accepted and contributed to the reduction of UP rates (Peipert et al., 2012; Bahamondes et al., 2014; Ferreira et al., 2017). While this benefit applies to countries of all socioeconomic levels, it had a greater impact in low- and middle-income countries (Peipert et al., 2012).
Moreover, in an evaluation of the cost of post-abortion care (PAC) in Colombia (including labour cost of HCPs, drugs/supplies, overhead and capital), the expense of treating one PAC woman is equivalent to approximately 10% of their per capita income. The provision of LARC methods would cost just a fraction of the average cost of PAC (Vlassoff et al., 2016). One year of modern contraceptive services and supplies costs between 3% and 10% of that for treating one PAC patient. These estimates suggested that PAC costs are an important burden for the economy in developing countries and there are cost savings that support the use of LARC in order to prevent UP.
In addition to lower costs, increased access to adequate contraceptive counselling has been shown to increase the prevalence with which women choose LARC over other contraceptive methods (Peipert et al., 2011, 2012). However, when physicians are misinformed about the effectiveness of LARC, the result of contraceptive counselling can have the opposite effect. A study with obstetrician-gynaecologists (OBGYNs) from 19 Latin American countries showed that almost half of them believed that the effectiveness of LARC was lower than what the evidence showed. In addition, OBGYNs from this meeting responded that they did not routinely recommend the use of IUD for nulligravidas, and emphasized that the myth of association between the use of IUD and PID persists (Bahamondes et al., 2015a, c). This study illustrates the importance of increasing education and awareness of HCPs regarding the effectiveness and safety of LARC.
Some of the most common myths affecting the use of LARC methods (Weston et al., 2012; WHO, 2015) in LAC (Table I) are associated with the beliefs held by some policymakers, HCPs and the public at large (including users, partners, relatives and the general community). Myths and misconceptions must be addressed in the counselling process. Counselling must provide adequate, timely and updated information that is scientifically validated and is communicated in clear and understandable terms for the user (Lyus et al., 2010).
Table I.
Common myths affecting the use of long-acting reversible contraceptives methods in Latin America and the Caribbean.
| Stakeholders | Myth | Evidence |
|---|---|---|
| Policymakers | LARC methods are more costly than other modern methods of contraception | LARC methods are highly cost-effective in the long term as a result of their high efficacy (Trussell, 2011; Winner et al., 2012). |
| HCP | There are many requirements for IUC or implant placement | The commons requirements prior to placing an IUC is to have a gynaecologic exam and that the HCP be reasonably sure a woman is not currently pregnant (WHO, 2015). |
| LARC methods have low efficacy | LARC methods are top-tier contraceptives based on both efficacy and effectiveness, with pregnancy rates of less than 1 per 100 woman-years for both perfect and typical use (Trussell, 2011; Winner et al., 2012). | |
| Perforation risk is perceived to be greater in nulligravidas | No data show a difference in perforation risk between nulligravida and parous women (Lyus et al., 2010). | |
| Adolescents and young adults do not like to use LARC methods | Given the availability of no-cost contraception, ~75% of women (including adolescents) chose LARC, and continuation was significantly higher among LARC- than non-LARC users (McNicholas et al., 2015). | |
| Given their age, adolescents cannot decide for themselves an appropriate contraceptive method | The Convention on the Rights of the Child indicates the right to the highest level of health and access to medical services, with an emphasis on those related to primary healthcare (PAHO, 2017). | |
| Individuals with disabilities do not require contraceptive counselling | Prejudices associated with the sexuality and reproduction of the disabled have no bearing on their right to receive contraceptive counselling and methods (PAHO, 2017). | |
| Use of LARC causes osteoporosis | No significant decrease in bone mineral density has been shown following use of LARC (Bahamondes et al., 2014, 2015a). | |
| General Public (including users, partners, relatives and general community) | The pain associated with IUC placement is enough to serve as a deterrent | The available studies used a scale of 0 (no pain) to 10 (severe pain) and showed that the majority of women rated IUC placement as 2 or less, and only 4% rated it ≥7 (Elkhouly and Maher, 2017). |
| IUCs will not fit in the uterus of nulligravidas | WHO does not restrict use of IUCs on the basis of age or parity. Both parous and nulligravidas have an IUC expulsion rate of less than 5% (Secura et al., 2010; Bahamondes et al., 2015c; WHO, 2015). | |
| Implants and IUCs cause cancer | Neither implants nor IUCs have shown a causal relationship with gynaecologic or other cancers. Indeed, some IUCs have shown a potential protective effect against both endometrial and cervical cáncer (Castellsagué et al., 2011). | |
| The government encourages contraceptive use to limit minority populations | No evidence. However, HCPs must consider how women’s experiences may influence their responses to contraceptive counselling, particularly with regard to race and income (Peipert et al., 2012). | |
| Both HCPs and General Public | IUC use causes abortions | LARCs act prior to fertilization or by changing cervical mucus (Moraes et al., 2016). |
| IUC use carries a higher risk of developing PID and later infertility | After the first 20 days of placement, risk of PID is the same in both LARC users and nonusers. There is no change in fertility rates following removal of LARC (Toivonen et al., 1991; Tsanadis et al., 2002; Lyus et al., 2010; Jatlaoui et al., 2017). | |
| IUCs can only be placed during menstrual periods | An IUC can be safely placed at any time during the menstrual cycle (Whiteman et al., 2013). |
LARC, long-acting reversible contraceptive; HCP, healthcare professionals; IUC, intrauterine contraceptive; PID, pelvic inflammatory disease; WHO, the World Health Organization.
Economic and Social Factors Impacting the use of LARC
In accordance with WHO recommendations, the provision of adequate SRH services to all women would result in major health gains for the population. If governments, the private sector and civil society (foundations, non-governmental organizations (NGOs) and others) collaborate to close the gap for unmet modern contraceptive needs, UPs and unsafe medical termintions (as well as the consequences of unsafe medical termination, such as maternal and newborn deaths) would drop by 65%. Importantly, it has been shown that providing contraceptives and education to adolescents is the most important intervention for reducing UP in that age group (Oringanje et al., 2016).
High-quality female-centrered services, efficiently operated facilities, adequately and ethically trained HCPs, among others, are also essential for increasing access to LARC. For example, in addition to reviewing contraceptive efficacy, counselling should also involve reviewing other factors such as perceived or real negative side effects (Wigginton et al., 2016), especially because dissatisfied users are more likely to discontinue LARC use prematurely compared to satisfied users, an issue which could then lead users to adopt a different contraceptive method with a higher failure and UP rate (Gipson et al., 2008).
Reducing UP through the use of LARC and empowering women by giving them the ability to time and space their pregnancies results in other non-health benefits such as continuing their education, increased labour-force participation, higher productivity and earnings, and access to a higher quality of life. Ensuring that contraceptive needs are fully met in LAC would require a funding increase from the current annual level of $4.4 to $5.2 billion USD. Such an investment is cost-effective because each additional dollar spent on contraception reduces the cost of pregnancy-related care, and eliminates the social and economic burden created by UPs, unsafe abortions and other maternal and infant complications. Moreover, fewer UPs would result in fewer women and newborns requiring care (UNFPA, 2016c). As policymakers increasingly acknowledge the widespread benefits of LARC, these methods are becoming increasingly available, at no cost, for women in the public sector of some LAC countries, including Argentina, Brazil, Chile, Colombia, Costa Rica, Dominican Republic, Ecuador and Mexico, as the Ministries of Health and NGOs work to increase their availability, and laws requiring private insurance reimbursement for the device and placement procedure become increasingly widespread.
Conclusion
UP is a major public health problem for women worldwide, and the use of LARC methods is an effective tool for reducing the high rates of UP, abortion and abortion-related complications. Consequently, increasing access to and the use of LARC in the region will have a significant impact in decreasing the rate of UP, and reducing their social and financial burden.
Although many studies on LARC methods typically treat the region as one unit, there is great ethnic diversity as well as economic and cultural differences among the various countries, which must be taken into account when developing policies related to disemminating information and combatting misinformation regarding the use of LARC among different audiences, such as adolescents, indigenous populations and women with disabilities. Knowledge and awareness of the contraceptive method mix of individual countries in the region is essential to the development of specific strategies and actions, tailored to each particular country situation, aimed at increasing access to modern contraceptive methods and LARC in particular. Additionally, governments can increase accessibility to LARC methods by prioritizing the need to promote LARC methods, implementing training programmes for HCPs, launching education campaigns for the general public, increasing access, especially for vulnerable female populations, and reviewing the cost-benefit analyses specific to LARC, which have demonstrated that the upfront cost associated with LARC methods is less than the cummulative expense of short-term contraceptives.
Removing barriers and improving access to LARC methods is an urgent public policy action in LAC. Dissemination of information on LARC methods, awareness of their efficacy, and encouragement in LARC use is an urgent task for policymakers and stakeholders. Thus, a co-ordinated effort from different levels of government, academia, professional organizations, insurance companies, policymakers and stakeholders is necessary to ensure access to LARC methods for women. It may even be necessary to consider a new model of SRH planning management. Here we set forth a number of recommendations that should be urgently addressed to reduce the high number of UPs, and increase access to and use of LARC methods in the region.
Recommendations
The recommendations for urgent attention are that:
– Healthcare systems in LAC should consider LARC as a primary option for decreasing UP and its complications, and include LARC, at no charge or at affordable cost, in SRH services. LARC use and access should be promoted by covering the upfront costs in both public and private healthcare systems.
– Academic programmes about SRH for different cadres of HCPs should be reinforced at the undergraduate and postgraduate levels via the creation of competencies in SRH counselling, with an emphasis on the importance of female reproductive health empowerment. All programmes must be based on knowledge and respect of SRHR.
– Healthcare professional associations should implement continuous medical education programmes for their members to increase technical competencies in both counselling on LARC (including updated knowledge on LARC methods, scientific evidence of the benefits and risks, and ways to address cultural differences among potential users) and LARC placement.
– NGOs and Ministries of Health should collaborate to develop an awareness campaign promulgating the use of LARC and the consequences of UP.
– Professional societies in each country and within the region, with the support of HCPs, policymakers and stakeholders, should establish a multidisciplinary task force to promote the dissemination of RHS health knowledge to children and adolescents.
– These same national or regional multidisciplinary task forces should also advocate for increased awareness, education and access to LARC with local and regional key opinion leaders, public health officials and other key stakeholders.
– NGOs, community-based groups and the public sector should form strategic alliances to increase coverage and access of LARC methods for vulnerable populations and remote areas by establishing mobile health services where the placement of LARC methods can be offered and monitored. All HCPs providing such services should have training in cultural sensitivity to ensure inclusiveness.
– Government should support the development of community-based educational spaces for parents and adolescents designed to foster open and healthy discussions about SRHR.
– Government should facilitate SRH care for underage women via adolescent-friendly clinics and review the minimum age for autonomy of health decisions.
In conclusion, the application of these recommendations should facilitate improved access to and use of LARC methods in the region, and help to ensure a reduction in the high number of UPs.
Acknowledgements
To Mary Herdoiza, Mirona Dragnea, Elizabeth McElwee, Maria Fernanda Navarro and Richard Salvatierra from the Americas Health Foundation for the valuable help in the design and development of the manuscript. L.B. and I.M. received additional support from the São Paulo Research Foundation (FAPESP) award # 2015/20504-9.
Authors’ roles
All authors contributed equally to the study design, execution, analysis, manuscript drafting and critical discussion.
Funding
This manuscript was supported by a grant from the Americas Health Foundation (AHF), a 501(c)3 nonprofit organization dedicated to improving healthcare throughout the Latin American Region.
Conflict of interest
None declared.
References
- Åhman E, Shah IH. New estimates and trends regarding unsafe abortion mortality. Int J Gynecol Obstet 2011;115:121–126. [DOI] [PubMed] [Google Scholar]
- Alan Guttmacher Institute Adding It Up: Investing in Contraception and Maternal and Newborn Health, 2017. Available at: https://www.guttmacher.org/fact-sheet/adding-it-up-contraception-mnh-2017 (June 2017, date last accessed).
- Ali M, Akin A, Bahamondes L, Brache V, Habib N, Landoulsi S, Hubacher D, WHO study group on subdermal contraceptive implants for women . Extended use up to 5 years of the etonogestrel-releasing subdermal contraceptive implant: comparison to levonorgestrel-releasing subdermal implant. Hum Reprod 2016;31:2491–2498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alkema L, Kantorova V, Menozzi C, Biddlecom A. National, regional, and global rates and trends in contraceptive prevalence and unmet need for family planning between 1990 and 2015: a systematic and comprehensive analysis. Lancet 2013;381:1642–1652. [DOI] [PubMed] [Google Scholar]
- Bahamondes L, Bottura BF, Bahamondes MV, Gonçalves MP, Correia VM, Espejo-Arce X, Sousa MH, Monteiro I, Fernandes A. Estimated disability-adjusted life years averted by long-term provision of long acting contraceptive methods in a Brazilian clinic. Hum Reprod 2014;29:2163–2170. [DOI] [PubMed] [Google Scholar]
- Bahamondes L, Brache V, Meirik O, Ali M, Habib N, Landoulsi S for the WHO Study Group . A 3-year multicentre randomized controlled trial of etonogestrel- and levonorgestrel-releasing contraceptive implants, with non-randomized matched copper-intrauterine device controls. Hum Reprod 2015. b;30:2527–2538. [DOI] [PubMed] [Google Scholar]
- Bahamondes MV, Espejo-Arce X, Bahamondes L. Effect of vaginal administration of misoprostol before intrauterine contraceptive insertion following previous insertion failure: a double blind RCT. Hum Reprod 2015. c;30:1861–1866. [DOI] [PubMed] [Google Scholar]
- Bahamondes L, Makuch MY, Monteiro I, Marin V, Lynen R. Knowledge and attitudes of Latin American obstetricians and gynecologists regarding intrauterine contraceptives. Int J Womens Health 2015. a;7:717–722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birgisson NE, Zhao Q, Secura GM, Madden T, Peipert JF. Positive testing for Neisseria gonorrhoeae and Chlamydia trachomatis and the risk of pelvic inflammatory disease in IUD users. J Womens Health (Larchmt) 2015;24:354–359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Branum AM, Jones J Trends in long-acting reversible contraception use among U.S. women aged 15–44. NCHS data brief, no 188. Hyattsville, MD: National Center for Health Statistics, 2015. Available at: https://www.cdc.gov/nchs/products/databriefs/db188.htm (June 2017, date last accessed). [PubMed]
- Castellsagué X, Díaz M, Vaccarella S, de Sanjosé S, Muñoz N, Herrero R, Franceschi S, Meijer CJ, Bosch FX. Intrauterine device use, cervical infection with human papillomavirus, and risk of cervical cancer: a pooled analysis of 26 epidemiological studies. Lancet Oncol 2011;12:1023–1031. [DOI] [PubMed] [Google Scholar]
- Cleland J, Ali MM. Reproductive consequences of contraceptive failure in 19 developing countries. Obstet Gynecol 2004;104:314–320. [DOI] [PubMed] [Google Scholar]
- Clifton D, Kaneda T Family Planning Worldwide 2013 Data Sheet. Washington, DC: Population Reference Bureau, 2013. Available at http://www.prb.org/pdf13/family-planning-2013-datasheet_eng.pdf (12 July 2017, date last accessed).
- Conde-Agudelo A, Belizán JM, Lammers C. Maternal-perinatal morbidity and mortality associated with adolescent pregnancy in Latin America: cross-sectional study. Am J Obstet Gynecol 2005;192:342–349. [DOI] [PubMed] [Google Scholar]
- Daniels K, Daugherty J, Jones J, Mosher W Current contraceptive use and variation by selected characteristics among women aged 15–44: United States, 2011–2013. National health statistics reports; no 86. Hyattsville, MD: National Center for Health Statistics, 2015. Available at: https://www.cdc.gov/nchs/data/nhsr/nhsr086.pdf (May 2017, date last accessed). [PubMed]
- Dansereau E, McNellan CR, Gagnier MC, Desai SS, Haakenstad A, Johanns CK, Palmisano EB, Ríos-Zertuche D, Schaefer A, Zúñiga-Brenes P et al. . Coverage and timing of antenatal care among poor women in 6 Mesoamerican countries. BMC Pregnancy Childbirth 2016;16:234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dean SV, Lassi ZS, Imam AM, Bhutta ZA. Preconception care: closing the gap in the continuum of care to accelerate improvements in maternal, newborn and child health. Reprod Health 2014;11:S1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dehlendorf C, Rodriguez MI, Levy K, Borrero S, Steinauer J. Disparities in family planning. Am J Obstet Gynecol 2010;202:214–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dibaba Y, Fantahun M, Hindin MJ. The effects of pregnancy intention on the use of antenatal care services: systematic review and meta-analysis. Reprod Health 2013;10:50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elkhouly NI, Maher MA. Different analgesics prior to intrauterine device insertion: is there any evidence of efficacy? Eur J Contracept Reprod Health Care 2017;22:222–226. [DOI] [PubMed] [Google Scholar]
- ESHRE Capri Workshop Group Induced abortion. Hum Reprod 2017;32:1160–1169.28402552 [Google Scholar]
- Espey E, Ogburn T. Long-acting reversible contraceptives: intrauterine devices and the contraceptive implant. Obstet Gynecol 2011;117:705–719. [DOI] [PubMed] [Google Scholar]
- Ferreira JM, Monteiro I, Fernandes A, Bahamondes MV, Pitoli A, Bahamondes L. Estimated disability-adjusted life years averted by free-of-charge provision of the levonorgestrel-releasing intrauterine system over a 9-year period in Brazil. J Fam Plann Reprod Health Care 2017;43:181–185. [DOI] [PubMed] [Google Scholar]
- Finer LB, Zoina MR. Declines in unintended pregnancy in the United States, 2008–2011. N Engl J Med 2016;374:843–852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ganchimeg T, Mori R, Ota E, Koyanagi A, Gilmour S, Shibuya K, Torloni MR, Betran AP, Seuc A, Vogel J et al. . Maternal and perinatal outcomes among nulliparous adolescents in low- and middle-income countries: a multi-country study. BJOG 2013;120:1622–1630. [DOI] [PubMed] [Google Scholar]
- Gipson JD, Koenig MA, Hindin MJ. The effects of unintended pregnancy on infant, child, and parental health: a review of the literature. Stud Fam Plann 2008;39:18–38. [DOI] [PubMed] [Google Scholar]
- Guliani H, Sepehri A, Serieux J. Determinants of prenatal care use: evidence from 32 low-income countries across Asia, Sub-Saharan Africa and Latin America. Health Policy Plan 2014;29:589–602. [DOI] [PubMed] [Google Scholar]
- Hidalgo MM, Hidalgo-Regina C, Bahamondes MV, Monteiro I, Petta CA, Bahamondes L. Serum levonorgestrel levels and endometrial thickness during extended use of the levonorgestrel-releasing intrauterine system. Contraception 2009;80:84–89. [DOI] [PubMed] [Google Scholar]
- Internal Displacement Monitoring Centre Norwegian Refugee Council: Global Overview of Trends and Developments in 2009, Geneva, 2010. Available at: http://www.internal-displacement.org/assets/publications/2010/2010-global-overview2009-global-en.pdf (June 2017, date last accessed).
- Jatlaoui TC, Riley HE, Curtis KM. The safety of intrauterine devices among young women: a systematic review. Contraception 2017;95:17–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jatlaoui TC, Simmons KB, Curtis KM. The safety of intrauterine contraception initiation among women with current asymptomatic cervical infections or at increased risk of sexually transmitted infections. Contraception 2016;94:701–712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones J, Mosher WD, Daniels K. Current contraceptive use in the United States, 2006–2010, and changes in patterns of use since 1995. Natl Health Stat Report 2012;60:1–25. [PubMed] [Google Scholar]
- Kavanaugh ML, Jerman J, Finer LB. Changes in use of long-acting reversible contraceptive methods among United States women, 2009–2012. Obstet Gynecol 2015;126:917–927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linard M, Blondel B, Estellat C, Deneux-Tharaux C, Luton D, Oury JF, Schmitz T, Mandelbrot L, Azria E, PreCARE study group . Association between inadequate antenatal care utilisation and severe perinatal and maternal morbidity: an analysis in the PreCARE cohort. BJOG 2017; in press. 10.1111/1471-0528.14794. [DOI] [PubMed] [Google Scholar]
- Luchetti G, Romero M. Regional survey on determinants for offering and inserting intrauterine devices carried out among health care providers. Rev Argent Public Health Care 2017;8:8–12. [Google Scholar]
- Lyus R, Lohr P, Prager S, Board of the Society of Family Planning . Use of the Mirena LNG-IUS and Paragard CuT380A intrauterine devices in nulliparous women. Contraception 2010;81:367–371. [DOI] [PubMed] [Google Scholar]
- Marston C, Cleland J. Do unintended pregnancies carried to term lead to adverse outcomes for mother and child? An assessment in five developing countries. Popul Stud (Camb) 2003;57:77–93. [DOI] [PubMed] [Google Scholar]
- McNicholas C, Maddipati R, Zhao Q, Swor E, Peipert JF. Use of the etonogestrel implant and levonorgestrel intrauterine device beyond the US Food and Drug Administration approved duration. Obstet Gynecol 2015;125:599–604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moraes LG, Marchi NM, Pitoli AC, Hidalgo MM, Silveira C, Modesto W, Bahamondes L. Assessment of the quality of cervical mucus among users of the levonorgestrel-releasing intrauterine system at different times of use. Eur J Contracept Reprod Health Care 2016;21:318–322. [DOI] [PubMed] [Google Scholar]
- Oringanje C, Meremikwu MM, Eko H, Esu E, Meremikwu A, Ehiri JE. Interventions for preventing unintended pregnancies among adolescents. Cochrane Database Syst Rev 2016;2:CD005215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pam American Health Organization (PAHO) Salud de la población joven indígena en América Latina, 2017. Available at: http://www.paho.org/hq/dmdocuments/gdr-salud-de-la-poblacion-joven-indigena-en-america-latina-panorama-general.pdf (June 2017, date last accessed).
- Peipert JF, Madden T, Allsworth JE, Secura GM. Preventing unintended pregnancies by providing no-cost contraception. Obstet Gynecol 2012;120:1291–1297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peipert JF, Zhao Q, Allsworth JE, Petrosky E, Madden T, Eisenberg D, Secura G. Continuation and satisfaction of reversible contraception. Obstet Gynecol 2011;117:1105–1113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prada E, Biddlecom A, Singh S. Induced abortion in Colombia: new estimates and change between 1989 and 2008. Int Perspect Sex Reprod Health 2011;37:114–124. [DOI] [PubMed] [Google Scholar]
- Reeves MF, Zhao Q, Secura GM, Peipert JF. Risk of unintended pregnancy based on intended compared to actual contraceptive use. Am J Obstet Gynecol 2016;215:71.e1–6. [DOI] [PubMed] [Google Scholar]
- Rowe P, Farley T, Peregoudov A, Piaggio G, Boccard S, Landoulsi S, Meirik O, IUD Research Group of the UNDP/UNFPA/WHO/World Bank Special Programme of Research; Development and Research Training in Human Reproduction . Safety and efficacy in parous women of a 52-mg levonorgestrel-medicated intrauterine device: a 7-year randomized comparative study with the TCu380A. Contraception 2016;93:498–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuck-Paim C, López D, Simonsen L, Alonso W. Unintended pregnancies in Brazil—a challenge for the recommendation to delay pregnancy due to Zika. PLoS Curr 2016;8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Secura GM, Allsworth JE, Madden T, Mullersman JL, Peipert JF. The contraceptive CHOICE Project: reducing barriers to long-acting reversible contraception. Am J Obstet Gynecol 2010;203:115.e1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sedgh G, Bearak J, Singh S, Bankole A, Popinchalk A, Ganatra B, Rossier C, Gerdts C, Tunçalp Ö, Johnson BR Jr et al. . Abortion incidence between 1990 and 2014: global, regional, and subregional levels and trends. Lancet 2016;388:258–267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sedgh G, Singh S, Hussain R. Intended and unintended pregnancies worldwide in 2012 and recent trends. Stud Fam Plann 2014;45:301–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sedgh G, Singh S, Shah IH, Åhman E, Henshaw SK, Bankole A. Induced abortion: incidence and trends worldwide from 1995 to 2008. Lancet 2012;379:625–632. [DOI] [PubMed] [Google Scholar]
- Shah I, Åhman E. Unsafe abortion in 2008: global and regional levels and trends. Reprod Health Matters 2010;18:90–101. [DOI] [PubMed] [Google Scholar]
- Shah IH, Åhman E, Ortayli N. Access to safe abortion: progress and challenges since the 1994 International Conference on Population and Development (ICPD). Contraception 2014;90:S39–S48. [DOI] [PubMed] [Google Scholar]
- Souza ML, Lynn FA, Johnston L, Tavares ECT, Brüggemann OM, Botelho LJ. Fertility rates and perinatal outcomes of adolescent pregnancies: a retrospective population-based study. Rev Lat Am Enfermagem 2017;25:e2876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Svanemyr J, Guijarro S, Riveros BB, Chandra-Mouli V. The health status of adolescents in Ecuador and the country’s response to the need for differentiated healthcare for adolescents. Reprod Health 2017;14:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toivonen J, Luukkainen T, Allonen H. Protective effect of intrauterine release of levonorgestrel on pelvic infection: three years’ comparative experience of levonorgestrel- and copper-releasing intrauterine devices. Obstet Gynecol 1991;77:261–264. [DOI] [PubMed] [Google Scholar]
- Trussell J. Contraceptive efficacy In: Hatcher RA, Trussell J, Nelson AL, Cates W, Kowal D, Policar M (eds). Contraceptive Technology: Twentieth Revised Edition. New York, NY: Ardent Media, 2011. [Google Scholar]
- Tsanadis G, Kalantaridou SN, Kaponis A, Paraskevaidis E, Zikopoulos K, Gesouli E, Dalkalitsis N, Korkontzelos I, Mouzakioti E, Lolis DE. Bacteriological cultures of removed intrauterine devices and pelvic inflammatory disease. Contraception 2002;65:339–342. [DOI] [PubMed] [Google Scholar]
- Tsui AO, McDonald-Mosley R, Burke AE. Family planning and the burden of unintended pregnancies. Epidemiol Rev 2010;32:152–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNFPA Population Latin America and Caribbean. 2016. b. Available at: www.un.org/en/development/desa/population/publications/pdf/family/trendsContraceptiveUse2015Report.pdf (June 2017, date last accessed).
- UNFPA Universal Access to Reproductive Health Progress and Challenges. 2016. c. http://www.un.org/en/development/desa/population/publications/dataset/contraception/wcu2015.shtml (2 August 2017, date last accessed).
- UNFPA World Population Dashboard 2016. a. Available at: http://www.unfpa.org/world-population-dashboard (June 2017, date last accessed).
- United Nations The Millennium Development Goals Report 2015. 2015. a. Available at: http://wwwunorg/millenniumgoals/2015_MDG_Report/pdf (July 2015, date last accessed).
- United Nations World Fertility Patterns 2015. 2015. c. http://www.un.org/en/development/desa/population/publications/pdf/fertility/world-fertility-patterns-2015.pdf.
- United Nations, Department of Economic and Social Affairs, Population Division Trends in Contraceptive Use Worldwide 2015 (ST/ESA/SER.A/349). 2015. b. www.un.org/en/development/desa/population/publications/pdf/family/trendsContraceptiveUse2015Report.pdf (July 2017, date last accessed).
- USAID, DELIVER PROJECT Contraceptive Security Index 2012. Arlington, Va.: Task Order 4, 2012. Available at: http://jsi.com/JSIInternet/Inc/Common/_download_pub.cfm?id=16912&lid=3 (June 2017, date last accessed).
- Villalobos A, Allen-Leigh B, Salazar-Alberto J, De Castro F, Barrientos-Gutiérrez T, Leyva-López A, Rojas-Martínez R. Quality of reproductive healthcare for adolescents: a nationally representative survey of providers in Mexico. PLoS One 2017;12:e0173342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vlassoff M, Singh S, Onda T. The cost of post-abortion care in developing countries: a comparative analysis of four studies. Health Policy Plan 2016;31:1020–1030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weston ML, Martins S, Neustadt A, Gilliam M. Factors influencing uptake of intrauterine devices among postpartum adolescents: a qualitative study. Am J Obstet Gynecol 2012;206:40.e1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whiteman MK, Tyler CP, Folger SG, Gaffield ME, Curtis KM. When can a woman have an intrauterine device inserted? A systematic review. Contraception 2013;87:666–673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wigginton B, Harris ML, Loxton D, Lucke JC. A qualitative analysis of women’s explanations for changing contraception: the importance of non-contraceptive effects. J Fam Plann Reprod Health Care 2016; in press. 10.1136/jfprhc-2015-101184. [DOI] [PubMed] [Google Scholar]
- Winner B, Peipert JF, Zhao Q, Buckel C, Madden T, Allsworth JE, Secura GM. Effectiveness of long-acting reversible contraception. N Engl J Med 2012;366:1998–2007. [DOI] [PubMed] [Google Scholar]
- World Bank Indicators World Bank Open Data. 2015. Available from: http://data.worldbank.org (June 2015, date last accessed).
- World Health Organization Unsafe Abortion Incidence and Mortality: Global and Regional Estimates of the Incidence of Unsafe Abortion and Associated Mortality in 2008, 6th edn Geneva: World Health Organization, 2011. http://whqlibdoc.who.int/publications/2011/9789241501118_eng.pdf. (18 July 2017, date last accessed). [Google Scholar]
- World Health Organization Medical eligibility criteria for contraceptive use In: World Health Organization (ed) Reproductive Health and Research, 5th edn Geneva: World Health Organization, 2015. [Google Scholar]