Abstract
STUDY QUESTION
Do singleton uncomplicated term pregnancies conceived by assisted reproductive technology (ART) have adverse peripartum and postpartum outcomes?
SUMMARY ANSWER
Term pregnancies following ART, even if uncomplicated until birth, have a higher risk of retained placenta and postpartum hemorrhage (PPH).
WHAT IS KNOWN ALREADY
There is consistent evidence that pregnancies following ART have higher incidence of complications during pregnancy. However, few studies specifically investigated birth outcomes in ART term pregnancies.
STUDY DESIGN, SIZE, DURATION
A retrospective cohort study was conducted on 14 415 deliveries at two university tertiary care obstetric units. Clinical data were extracted by reviewing obstetric records of all deliveries from 1 January 2010 to 31 December 2014, in a standardized electronic database regarding the mother’s health before and during pregnancy, complications during pregnancy and at birth, and neonatal outcome.
PARTICIPANTS/MATERIALS, SETTING, METHODS
Following an accurate evaluation of exclusion criteria (multiparity, maternal pre-pregnancy diseases, prior uterine surgery, fetal malformations, intrauterine deaths, elective cesarean section and pregnancy complications), the group of uncomplicated singleton term pregnancies from autologous ART conception by in vitro fertilization (IVF) or intracytoplasmic sperm injection (ICSI) (n = 188) was compared with a maternal age and body mass index (BMI) matched group of spontaneous pregnancies (n = 1168). Cases of intrauterine insemination (IUI) (n = 14) and ovulation induction with timed intercourse (n = 18) were not included. Labor, delivery and postpartum outcomes were evaluated. Odds ratios (OR) were adjusted with multivariable logistic regression to maternal age, BMI, nationality and gestational age at birth.
MAIN RESULTS AND THE ROLE OF CHANCE
The age of women in the final analysis ranged from 25 to 45 years, while BMI ranged from 17 to 34 kg/m2. Uncomplicated term pregnancies with ART conception had a higher risk of operative delivery (adjusted OR 1.40, 95% confidence interval (CI) 1.01–1.95), retained placenta (adjusted OR 2.63, 95% CI 1.31–5.26) and PPH (adjusted OR 2.86 95% CI 1.37–5.99). Conversely, ART conception did not increase the risk of induced labor (adjusted OR 1.18, 95% CI 0.85–1.65). However, patients that conceived by ART and underwent labor induction had a higher risk of failed induction compared with the control group (adjusted OR 2.53, 95% CI 1.23–5.21). Infants born after ART had a similar birthweight, Apgar score and arterial blood pH compared with spontaneously-conceived ones.
LIMITATIONS, REASONS FOR CAUTION
The database lacked specific information about causes of infertility, smoking habit, family income and details on ART (fresh versus frozen cycle, IVF versus ICSI), limiting, in part, our analysis of the results. However, only autologous IVF/ICSI pregnancies were included in order to prevent bias related to conception by oocyte/embryo donation. In vivo conception ART cases were excluded because they were too few to allow comparison with IVF/ICSI. Nevertheless, the inclusion of only uncomplicated pregnancies provides a highly homogeneous and still representative population sample. Study sample is representative of a well-resourced obstetric facility in a high-income country, limiting to some extent the generalizability of study results.
WIDER IMPLICATIONS OF THE FINDINGS
Pregnancies conceived by autologous ART that proceed uncomplicated until term may require counseling about the risk of placental retention with PPH.
STUDY FUNDING/COMPETING INTERESTS
The authors have no conflict of interest and funding to declare.
Keywords: ART, delivery, induction of labor, infertility, IVF, operative delivery, neonatal outcome, postpartum hemorrhage, retained placenta, uncomplicated pregnancy
Introduction
In the last few decades, the number of women having in vitro fertilization/intracytoplasmic sperm injection (IVF/ICSI) has increased worldwide (Ishihara et al., 2015; Williams et al., 2015) and there is consistent evidence that pregnancies following assisted reproductive technology (ART) have a higher risk of adverse obstetric and perinatal outcomes (Helmerhorst et al., 2004; Romundstad et al., 2006, 2008). This is attributed to the higher proportion of multiple pregnancies, but data available from systematic reviews showed that singleton pregnancies conceived after ART are at increased risk of preterm birth, hypertensive disorders, antepartum and postpartum hemorrhage (PPH), placental disorders and low birthweight infants (Pandey et al., 2012; Pinborg et al., 2013; Malchau et al., 2014; Qin et al., 2015). These factors were also associated with an increased incidence of cesarean deliveries (Helmerhorst et al., 2004) and induction of labor in women with singleton pregnancies (Pandian et al., 2001).
WHAT DOES THIS MEAN FOR PATIENTS?
This study looked at births after fertility treatment to see whether there were any additional complications with IVF. There has been evidence in the past to suggest that there may be more complications in pregnancy after IVF, but it is not always clear whether this may in part be linked to factors other than the treatment.
The researchers looked at more than 8000 births at two hospitals in Italy, ruling out any births where there had been problems during the pregnancies or where the mothers had pre-existing medical conditions. They matched characteristics such as the age and BMI of the mothers to ensure they were comparing like with like. All the pregnancies had progressed without any complications until the mother went into labor.
They found that even when the IVF pregnancies had been problem-free, there was a higher chance of the placenta being retained and of hemorrhage after birth, and a greater risk of induction not working and of having a forceps or ventouse for the birth. The study did not specify whether the women had IVF or ICSI or whether they had a frozen or fresh treatment cycle. The researchers say further studies are needed to investigate the reasons behind these differences.
Although many studies have attempted to evaluate obstetric and perinatal outcomes in women conceiving with the aid of ART, it is unclear whether ART procedures or maternal factors associated with infertility, such as maternal age, BMI, past obstetric outcome and medical history, contribute to these adverse outcomes (Hayashi et al., 2012; Raatikainen et al., 2012; Farhi et al., 2013; Messerlian et al., 2013; Stern et al., 2015). Despite the specific limitations of each study, the association of ART with poor obstetric and perinatal outcome is relevant (Barnhart, 2013; Vannuccini et al., 2016).
Unfortunately, few studies specifically investigated birth outcomes in full-term ART pregnancies. Indeed, previous reports included both complicated and uncomplicated pregnancies, so labor and delivery were managed according to the potential presence of an obstetric complication or pre-pregnancy diseases (Hayashi et al., 2012; Sun et al., 2014). In addition, a significant number of women underwent elective cesarean section (CS) on maternal request, even if the pregnancies were uncomplicated until term (Gillet et al., 2011).
Thus, the aim of this study was to evaluate the perinatal outcomes of singleton uncomplicated term pregnancies from ART conception in comparison with maternal age and BMI-matched term pregnancies from spontaneous conception.
Materials and Methods
A retrospective cohort study was conducted on 14 415 deliveries at the Careggi University Hospital in Florence and at the University Hospital in Siena, Italy. Clinical data were extracted by reviewing obstetric records of all deliveries from 1 January 2010 to 31 December 2014, in a standardized electronic database regarding the mother’s health before and during pregnancy, complications during pregnancy and at birth, and neonatal outcome. The research protocol involved only existing records, based on information routinely collected and stored in a de-identified dataset and hence was considered exempt from ethical review board approval and a requirement for written informed consent.
Maternal characteristics included age, pre-pregnancy BMI, parity, pre-existing maternal diseases and history of treatment for infertility, such as ovulation stimulation, IUI or IVF with or without ICSI and embryo transfer. Complications that occurred during pregnancy and all data regarding birth, including neonatal outcome, were extracted. These data conform to uniform coding specifications, have passed a rigorous quality check, and have been edited and reviewed by two different data managers for each institution.
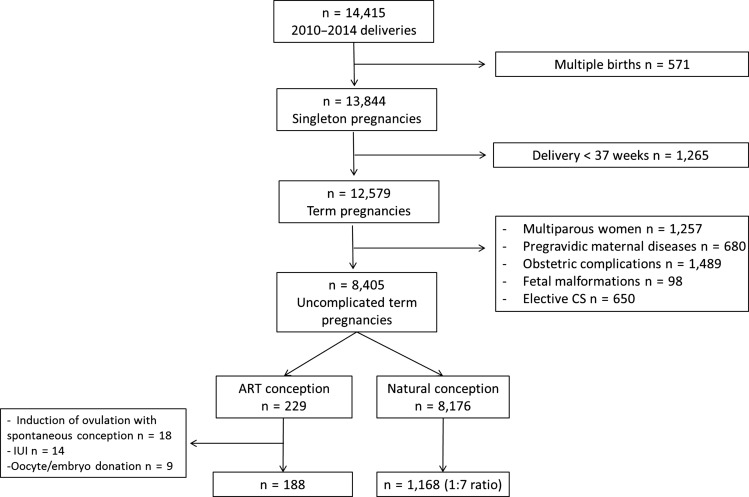
The flow diagram for study population selection is shown in Fig. 1. From the initial dataset of all deliveries (n = 14 415), the group was limited to singleton term pregnancies between 37 and 42 weeks gestational age (n = 12 579). To limit confounding, the following exclusion criteria were applied: multiparity, maternal pre-pregnancy diseases (diabetes, chronic hypertension, thyroid disease, renal disease, neurological diseases, inflammatory rheumatic diseases, respiratory diseases and gynecologic diseases, such as uterine fibroids, polycystic ovary syndrome (PCOS) and endometriosis), prior uterine surgery, obstetric complications diagnosed during pregnancy until labor onset (hypertensive disorders, gestational diabetes, obstetric cholestasis, intrauterine growth restriction, small-for-gestational age babies, oligo-polyhydramnios, placental diseases, placental abruption), fetal malformations, intrauterine deaths and elective CS (for breech or transverse fetal lie), including CS on maternal request.
Figure 1.
Flow chart of the population in a study of peripartum and postpartum outcomes in uncomplicated term pregnancy following ART.
The final cohort included 8405 uncomplicated term pregnancies, either following ART (n = 229) or spontaneous (n = 8176) conception. Singleton term pregnancies with autologous IVF/ICSI conception (excluding oocyte/embryo donation) were included in the study as the exposed group (n = 188). Cases of IUI (n = 14) and ovulation induction with timed intercourse (n = 18) were not included because they were too few to allow comparison with IVF/ICSI. Singleton pregnancies with spontaneous conception (non-exposed group) were matched to the exposed group for age and BMI (1:7 ratio) (n = 1168). The age ranged from 25 to 45 years, while BMI ranged from 17 to 34 kg/m2.
The following outcome measures related to birth and postpartum were evaluated: induction of labor, failed induction, length of active phase of labor, mode of delivery (spontaneous vaginal delivery, operative vaginal delivery or CS), ‘in labor’ CS, retained placenta, PPH, episiotomy and third/fourth degree perineal tears, neonatal birthweight, Apgar scores and umbilical cord blood gas analysis. The main indications for labor induction were prolonged rupture of membranes and late-term (41 completed weeks) pregnancy. Indications for ‘in labor’ CS were: non-reassuring fetal heart tracing, fetal distress, failure to progress (arrest of dilation or descent) or cephalopelvic disproportion.
Statistical analysis
Data were analyzed using GraphPad Prism version 5.00 for Windows (GraphPad Software, Inc, San Diego, CA, USA) and IBM SPSS version 22 (IBM, Armonk, NY, USA) statistical software packages. Data distribution was evaluated by the D’Agostino & Pearson omnibus normality test. Two-group comparisons were performed using Chi-square test with continuity correction or Fisher’s exact test for binomial variables, while Mann–Whitney U test was used for quantitative variables, which were expressed both as mean ± SD and median with interquartile range. P-values of <0.05 were considered to indicate statistical significance. Odds ratios (OR) and 95% confidence interval (CI) were calculated for each outcome and adjusted for maternal age, BMI, nationality and gestational age at birth using multivariable backward stepwise (conditional) logistic regression.
The study sample was calculated to detect a minimal effect size of two-fold increase (from an estimated 5% to 10%) in the risk of retained placenta, PPH, acute fetal distress or fetal hypoxemia, with a statistical power of 80% and confidence level of 95% (Chow et al., 2008).
Results
Maternal and perinatal characteristics of the study population are shown in Table I. The group of women with ART conception had similar gestational age at birth compared with the group of spontaneous conception. The two groups also had similar prevalence of previous miscarriage, non-European Union citizenship, CS, epidural analgesia, episiotomy and third or fourth degree perineal tears, whereas blood loss at birth was more abundant in the ART group (Table I). There was no case of maternal death. Concerning neonatal outcomes, no differences were observed between ART conception pregnancies and spontaneous ones (Table I).
Table I.
Maternal and perinatal characteristics of the study groups.
| ART conception (n = 188) | Spontaneous conception (n = 1168) | P | |
|---|---|---|---|
| Maternal baseline characteristics | |||
| Age (years) | 37.1 ± 3.8 | 36.4 ± 3.5 | 0.02 |
| 37 (35–40) | 37 (35–39) | ||
| BMI (kg/m2) | 22.0 ± 3.2 | 22.1 ± 3.3 | 0.67 |
| 21.3 (19.9–23.1) | 21.5 (19.8–23.4) | ||
| Previous miscarriage (1 or more) | 42/188 (22.3%) | 244/1168 (20.8%) | 0.60 |
| Non-European Union citizenship | 15/186 (8.1%) | 97/1137 (8.5%) | 0.94 |
| Perinatal outcome characteristics | |||
| Gestational age at birth (weeks) | 40.0 ± 1.2 | 40.1 ± 1.2 | 0.61 |
| 40.1 (39.1–41.0) | 40.1 (39.3–41.0) | ||
| Cesarean section | 42/188 (22.3%) | 195/1168 (16.7%) | 0.07 |
| Epidural analgesiaa | 37/81 (45.7%) | 168/438 (38.4%) | 0.22 |
| Episiotomya | 62/146 (42.5%) | 372/973 (38.2%) | |
| Perineal tears > II degreea | 15/91 (16.5%) | 66/591 (11.2%) | 0.20 |
| Blood loss at birth (ml) | 414 ± 279 | 292 ± 236 | 0.00 |
| 400 (200–600) | 200 (100–400) | ||
| Birthweight (g) | 3355 ± 415 | 3319 ± 416 | 0.19 |
| 3345 (3053–3650) | 3300 (3040–3600) | ||
| 5 min Apgar Score <7 | 0/188 (0.0%) | 4/1168 (0.3%) | 0.42 |
| Arterial blood pH | 7.27 ± 0.07 | 7.26 ± 0.08 | 0.29 |
| 7.27 (7.23–7.32) | 7.26 (7.21–7.32) | ||
Continuous variables are expressed as mean ± SD and median (interquartile range). Categorical variables are expressed as n (%).
aAmong cases of vaginal delivery.
The statistical tests applied were Mann–Whitney test (for continuous variables) and Chi-square test (for categorical variables).
Table II shows the crude and adjusted OR for pre-specified obstetric and perinatal outcomes according to the mode of conception. ART conception did not increase the risks of labor induction, ‘in labor’ CS, acute fetal distress or fetal hypoxemia. However, patients who conceived by ART and underwent labor induction had a higher risk of failed induction compared with the control group (adjusted OR 2.53, 95% CI 1.23–5.21). ART conception reduced the risk of prolonged labor, i.e. active labor phase longer than 4 h (adjusted OR 0.53, 95% CI 0.33–0.87). The ART group showed a higher risk of operative delivery (adjusted OR 1.40, 95% CI 1.01–1.95), retained placenta (adjusted OR 2.63, 95% CI 1.31–5.26) and PPH, i.e. blood loss more than 1000 ml (adjusted OR 2.86 95% CI 1.37–5.99) compared with the natural conception group (Table II). The difference related to postpartum bleeding remained significant even after repeating the analysis without cases of retained placenta.
Table II.
Crude and adjusted odds ratios of adverse perinatal outcomes associated with ART conception versus spontaneous conception.
| ART conception (n = 188) | Spontaneous conception (n = 1168) | Crude OR (95% CI) | Adjusted OR (95% CI) | |
|---|---|---|---|---|
| Induction of labor | ||||
| Yes | 73 | 382 | 1.29 (0.94–1.78) | 1.18 (0.85–1.65) |
| No | 114 | 772 | ||
| Failed inductiona | ||||
| Yes | 14 | 34 | 2.43 (1.23–4.80) | 2.53 (1.23–5.21) |
| No | 59 | 348 | ||
| Prolonged labor (>4 h)b | ||||
| Yes | 23 | 219 | 0.51 (0.31–0.84) | 0.53 (0.33–0.87) |
| No | 82 | 400 | ||
| Cesarean section in labor b | ||||
| Yes | 19 | 149 | 0.85 (0.51–1.41) | 0.88 (0.52–1.48) |
| No | 146 | 968 | ||
| Operative deliveryc | ||||
| Yes | 51 | 318 | 1.12 (0.79–1.60) | 1.40 (1.01–1.95) |
| No | 114 | 799 | ||
| Retained placentad | ||||
| Yes | 12 | 33 | 2.58 (1.30–5.12) | 2.63 (1.31–5.26) |
| No | 131 | 929 | ||
| Postpartum hemorrhage (blood loss >1000 ml) | ||||
| Yes | 11 | 28 | 2.67 (1.30–5.49) | 2.86 (1.37–5.99) |
| No | 136 | 924 | ||
| Acute fetal distress | ||||
| Yes | 12 | 59 | 1.28 (0.68–2.43) | 1.44 (0.75–2.76) |
| No | 176 | 1109 | ||
| Fetal hypoxemia (arterial blood pH <7.10) | ||||
| Yes | 3 | 22 | 0.82 (0.24–2.76) | 0.87 (0.25–2.95) |
| No | 130 | 777 |
aAmong cases of induced labor.
bAmong cases of spontaneous or induced labor.
cCesarean section or vacuum extractor.
dAmong cases of vaginal delivery.
Multivariable backward stepwise (conditional) logistic regression was used to calculate odds ratios (OR) and 95% CI for each outcome, adjusting for maternal age, BMI, nationality and gestational age at birth.
Discussion
The present study compared birth outcomes between women with healthy singleton pregnancies conceived through ART procedures and women who conceived naturally, matched by maternal characteristics. The results showed that singleton uncomplicated term pregnancies from ART conception have a higher risk of failed induction, retained placenta and PPH but no increased risk of acute fetal distress or fetal hypoxemia. To our knowledge, no previous study has evaluated a group of women exposed to ART excluding most of the confounding factors that affect perinatal outcomes. According to our results, birth and postpartum management in uncomplicated term ART pregnancies may require counseling women about the risk of placental retention with PPH, but patients may be reassured about the lack of additional risks to the neonate.
The prevalence of induced labor was similar between the two groups. An increased rate of labor induction in ART pregnancies has been reported, although mostly due to obstetric complications (Hayashi et al., 2012; Barnhart, 2013; Sun et al., 2014). In our cohort, the main indications for labor induction were prolonged rupture of membranes and late-term pregnancy; however, we found a higher risk of failed induction, may be due to a myometrial dysfunction (Vannuccini et al. 2016).
Concerning the mode of delivery, ART conception was a protection factor against prolonged labor while increasing the risk of operative (either vaginal or abdominal) birth. Altogether, these findings suggest that ART gestations might be more subject to medical interventions to accelerate delivery and avoid a prolonged labor. This fact cannot be ascribed to a greater probability of acute fetal distress in ART, at least in our study population, since we found the same risk of acute fetal distress, fetal hypoxemia and emergency (‘in labor’) CS in both study groups.
Our results show that ART pregnancies had higher risks of retained placenta, requiring manual removal and of PPH. Previous studies demonstrated a higher incidence of PPH and placental disorders in ART gestation, mostly related to placenta previa (Healy et al., 2010; Rombauts et al., 2014; Kaser et al., 2015). In our cohort, all known placental pathologies were excluded, but a higher risk of placental retention in ART pregnancies was still registered. A recent pathology study analyzed the morphological characteristics of the placental basal plate in ART pregnancies, suggesting a possible association with an increase in the amount of bleeding in deliveries (Nakamura et al., 2015). There was a significantly higher mean thickness of Rohr fibrinoid layer and a higher percentage of loss of decidua in ART placenta, correlating with the bleeding at birth. Probably, unidentified factors associated with determining the thickness of the Rohr fibrinoid layer may have indirectly-affected bleeding during placental separation. Moreover, hormonal treatments in early pregnancy may cause changes in the structure and/or function of the extracellular matrix in the decidual layer, as represented by the percentage of loss of decidua, and thereby contributing to an association with increased bleeding in deliveries (Nakamura et al., 2015). Thus, events around the time of implantation may induce suboptimal endometrial function as a critical mechanism (Vannuccini et al., 2016). High oestradiol and progesterone concentrations, as a result of multiple folliculogenesis, may produce suboptimal angiogenesis and placentation, predisposing to PPH. Therefore, a major role may be played by ART procedures themselves, but uterine and hormonal conditions associated with infertility may contribute to the increased failed induction and postpartum complications observed (Stern et al., 2015; Healy et al., 2010; Aziz et al., 2015).
Concerning neonatal outcome, we observed that term newborns from ART gestation had the same weight as naturally conceived counterparts and also the same risk of perinatal hypoxemia. A recent report on a large US IVF database showed that infants born from ART have a similar birthweight compared with spontaneously-conceived ones, suggesting that intrauterine growth is not reduced in singleton IVF babies (Dickey et al., 2016). Our present findings in full-term infants further suggest that ART conception does not increase the risk of perinatal hypoxemia, despite the possibly increased risk of abnormal placentation.
Gynecological conditions, such as PCOS, uterine fibroids and endometriosis, were excluded from our study population, but our database lacked specific information about causes of infertility, smoking habit and family income, limiting in part our results. In addition, a potential under-reporting of ART or incorrect information about the type of fertility treatment may have biased results, misclassifying the exposed and unexposed. The dataset lacks also specific information about the type of technique used (IVF or ICSI) and whether it was a fresh or a frozen cycle. Another limitation to acknowledge is a reduced generalizability of study findings to all nations and settings, as the data refer to well-resourced obstetric facilities in a high-income economy country. However, one of the strengths of the study is the strict inclusion criteria that allowed us to analyze a homogenous population and obtain more reliable results. In fact, only autologous IVF/ICSI pregnancies were included, in order to remove the bias related to conception by oocyte/embryo donation. In addition, the inclusion of only uncomplicated pregnancies until the onset of labor provides a well-defined and still largely representative population sample.
In conclusion, pregnancies conceived by autologous IVF or ICSI and managed in well-resourced obstetric facilities, even if uncomplicated until birth, have a higher risk of failed induction, retained placenta and PPH. Thus, patients should be counseled about the risk of peripartum and postpartum complications in the case of ART conception. Obstetricians often need to offer counsel about birth plans to this group of pregnant women, who are mostly nulliparous with advanced maternal age and become pregnant after years of infertility. The clinician’s role should be to provide the best evidence-based counseling to the pregnant woman for a better management of the birth, and postpartum. This observation has implications not only for counseling, but also in terms of health services and health policies. In fact, this group of women should be considered as an ‘at risk’ category, and thus preventative strategies should be applied for postpartum management. However, sufficient evidence to support specific medical interventions to prevent these complications is still lacking. This is mostly because of a paucity of studies investigating the underlying pathogenetic mechanisms that explain the increased risk of these complications in ART pregnancy.
Therefore, further studies are needed in order to investigate the potential endometrial or myometrial factors implicated in the pathogenesis of peripartum and postpartum complications in pregnancies conceived by ART.
Authors’ roles
SV, CF, MDT and FP developed the study design. CF, FP and SP contributed to data collection and management. SV, FMR and CF performed the statistical analysis. All authors contributed substantially interpretation of data. SV wrote the first draft of the manuscript. All authors contributed to redrafting of the manuscript. MDT, FP, FMR and FMS revised critically the manuscript for important intellectual content. All authors approved the final submitted version.
Funding
The authors declare no relationship with funding sources or sponsorships.
Conflict of interest
The authors report no conflict of interest.
References
- Aziz MM, Guirguis G, Maratto S, Benito C, Forman EJ. Is there an association between assisted reproductive technologies and time and complications of the third stage of labor? Arch Gynecol Obstet 2015;293:1193–1196. [DOI] [PubMed] [Google Scholar]
- Barnhart KT. Assisted reproductive technologies and perinatal morbidity: interrogating the association. Fertil Steril 2013;99:299–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chow S, Shao J, Wang H. 2008. Sample Size Calculations in Clinical Research. 2nd Ed. Chapman & Hall/CRC Biostatistics Series.
- Dickey RP, Xiong X, Pridjian G, Klempel MC. Singleton birthweight by gestational age following in vitro fertilization in the United States. Am J Obstet Gynecol 2016;214:101. [DOI] [PubMed] [Google Scholar]
- Farhi A, Reichman B, Boyko V, Hourvitz A, Ron-El R, Lerner-Geva L. Maternal and neonatal health outcomes following assisted reproduction. Reprod Biomed Online 2013;26:454–461. [DOI] [PubMed] [Google Scholar]
- Gillet E, Martens E, Martens G, Cammu H. Prelabour caesarean section following IVF/ICSI in older-term nulliparous women: too precious to push? J Pregnancy 2011;2011:362518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayashi M, Nakai A, Satoh S, Matsuda Y. Adverse obstetric and perinatal outcomes of singleton pregnancies may be related to maternal factors associated with infertility rather than the type of assisted reproductive technology procedure used. Fertil Steril 2012;98:922–928. [DOI] [PubMed] [Google Scholar]
- Healy DL, Breheny S, Halliday J, Jaques A, Rushford D, Garrett C, Talbot JM, Baker HW. Prevalence and risk factors for obstetric haemorrhage in 6730 singleton births after assisted reproductive technology in Victoria Australia. Hum Reprod 2010;25:265–274. [DOI] [PubMed] [Google Scholar]
- Helmerhorst FM, Perquin DA, Donker D, Keirse MJ. Perinatal outcome of singletons and twins after assisted conception: a systematic review of controlled studies. BMJ 2004;328:261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ishihara O, Adamson GD, Dyer S, de Mouzon J, Nygren KG, Sullivan EA, Zegers-Hochschild F, Mansour R. International committee for monitoring assisted reproductive technologies: world report on assisted reproductive technologies, 2007. Fertil Steril 2015;103:402–413. [DOI] [PubMed] [Google Scholar]
- Kaser DJ, Melamed A, Bormann CL, Myers DE, Missmer SA, Walsh BW, Racowsky C, Carusi DA. Cryopreserved embryo transfer is an independent risk factor for placenta accreta. Fertil Steril 2015;103:1176–1184. [DOI] [PubMed] [Google Scholar]
- Malchau SS, Loft A, Henningsen AK, Nyboe Andersen A, Pinborg A. Perinatal outcomes in 6,338 singletons born after intrauterine insemination in Denmark, 2007 to 2012: the influence of ovarian stimulation. Fertil Steril 2014;102:1110–1116. [DOI] [PubMed] [Google Scholar]
- Messerlian C, Maclagan L, Basso O. Infertility and the risk of adverse pregnancy outcomes: a systematic review and meta-analysis. Hum Reprod 2013;28:125–137. [DOI] [PubMed] [Google Scholar]
- Nakamura Y, Yaguchi C, Itoh H, Sakamoto R, Kimura T, Furuta N, Uchida T, Tamura N, Suzuki K, Sumimoto K et al. . Morphologic characteristics of the placental basal plate in in vitro fertilization pregnancies: a possible association with the amount of bleeding in delivery. Hum Pathol 2015;46:1171–1179. [DOI] [PubMed] [Google Scholar]
- Pandey S, Shetty A, Hamilton M, Bhattacharya S, Maheshwari A. Obstetric and perinatal outcomes in singleton pregnancies resulting from IVF/ICSI: a systematic review and meta-analysis. Hum Reprod Update 2012;18:485–503. [DOI] [PubMed] [Google Scholar]
- Pandian Z, Bhattacharya S, Templeton A. Review of unexplained infertility and obstetric outcome: a 10 year review. Hum Reprod 2001;16:2593–2597. [DOI] [PubMed] [Google Scholar]
- Pinborg A, Wennerholm UB, Romundstad LB, Loft A, Aittomaki K, Söderström-Anttila V, Nygren KG, Hazekamp J, Bergh C. Why do singletons conceived after assisted reproduction technology have adverse perinatal outcome? Systematic review and meta-analysis. Hum Reprod Update 2013;19:87–104. [DOI] [PubMed] [Google Scholar]
- Qin J, Liu X, Sheng X, Wang H, Gao S. Assisted reproductive technology and the risk of pregnancy-related complications and adverse pregnancy outcomes in singleton pregnancies: a meta-analysis of cohort studies. Fertil Steril 2015;105:73–85. [DOI] [PubMed] [Google Scholar]
- Raatikainen K, Kuivasaari-Pirinen P, Hippeläinen M, Heinonen S. Comparison of the pregnancy outcomes of subfertile women after infertility treatment and in naturally conceived pregnancies. Hum Reprod 2012;27:1162–1169. [DOI] [PubMed] [Google Scholar]
- Rombauts L, Motteram C, Berkowitz E, Fernando S. Risk of placenta praevia is linked to endometrial thickness in a retrospective cohort study of 4537 singleton assisted reproduction technology births. Hum Reprod 2014;29:2787–2793. [DOI] [PubMed] [Google Scholar]
- Romundstad LB, Romundstad PR, Sunde A, von Düring V, Skjaerven R, Gunnell D, Vatten LJ. Effects of technology or maternal factors on perinatal outcome after assisted fertilisation: a population-based cohort study. Lancet 2008;372:737–743. [DOI] [PubMed] [Google Scholar]
- Romundstad LB, Romundstad PR, Sunde A, von Düring V, Skjaerven R, Vatten LJ. Increased risk of placenta previa in pregnancies following IVF/ICSI; a comparison of ART and non-ART pregnancies in the same mother. Hum Reprod 2006;21:2353–2358. [DOI] [PubMed] [Google Scholar]
- Stern JE, Luke B, Tobias M, Gopal D, Hornstein MD, Diop H. Adverse pregnancy and birth outcomes associated with underlying diagnosis with and without assisted reproductive technology treatment. Fertil Steril 2015;103:1438–1445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun LM, Lanes A, Kingdom JC, Cao H, Kramer M, Wen SW, Wu J, Chen Y, Walker MC. Intrapartum interventions for singleton pregnancies arising from assisted reproductive technologies. J Obstet Gynaecol Can 2014;36:795–802. [DOI] [PubMed] [Google Scholar]
- Vannuccini S, Clifton VL, Fraser IS, Taylor HS, Critchley H, Giudice LC, Petraglia F. Infertility and reproductive disorders: impact of hormonal and inflammatory mechanisms on pregnancy outcome. Hum Reprod Update 2016;22:104–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams RS, Doody KJ, Schattman GL, Adashi EY. Public reporting of assisted reproductive technology outcomes: past, present, and future. Am J Obstet Gynecol 2015;212:157–162. [DOI] [PubMed] [Google Scholar]