Abstract
STUDY QUESTION
Are Australian fertility clinics adequately addressing unhealthy lifestyle in patients seeking fertility treatment?
SUMMARY ANSWER
This study has highlighted deficiencies in practices and education around managing patients with unhealthy lifestyle undergoing fertility treatment.
WHAT IS KNOWN ALREADY
The association between lifestyle and fertility is well documented, with obesity and smoking being of particular concern to fertility and pregnancy outcomes. Guidelines recommend that unhealthy lifestyle is addressed prior to conception, yet anecdotal experience suggests this is not being addressed. Lifestyle modification programmes can be effective in improving pregnancy rates and outcomes, however, recruitment to such programmes can be challenging.
STUDY DESIGN SIZE, DURATION
A cohort study of Australian fertility clinics’ attitudes and practices regarding lifestyle modification to augment reproductive treatment outcomes was conducted between August and October 2015.
PARTICIPANTS/MATERIALS, SETTING, METHOD
An online survey was administered to senior fertility nurses, from all registered fertility clinics in Australia. Data were collated and subjected to a univariate data analysis, where frequency tables were produced for each question. A separate qualitative analysis was undertaken of data from open ended questions.
MAIN RESULTS AND THE ROLE OF CHANCE
Fifty-three out of 85 potential respondents (62.4%), all from different clincis, completed the survey, with almost all acknowledging the importance of addressing unhealthy lifestyle before offering ART treatment. However, most clinics did not offer internal resources to assist with lifestyle modification. Whilst the promotion of healthy lifestyle was recognised as a key component of the role of a fertility nurse, participants did not feel that nurses were best equipped to provide lifestyle modification programmes, owing to a lack of resources and specific skills in this area. Suggested areas for improved practice included prioritising general health prior to offering treatment, and further utilising and upskilling nurses to assist with lifestyle modification programmes.
LIMITATIONS REASONS FOR CAUTION
The survey was completed by only one nurse from each clinic and as such may not be entirely representative of all clinic practices.
WIDER IMPLICATIONS OF THE FINDINGS
Fertility clinics are likely to see an increasing number of patients with unhealthy lifestyle, resulting in health concerns such as obesity. The results of this study provide an insight into how unhealthy lifestyle is currently being addressed in fertility clinics and suggested areas that could be targeted for improving practice and outcomes.
STUDY FUNDING/COMPETING INTERESTS
No conflict of interest to declare. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
TRIAL REGISTRATION NUMBER
NA
Keywords: lifestyle modification, BMI, pregnancy, assisted reproduction, reproductive outcomes, fertility nurses
Introduction
Fertility and reproductive outcomes can be adversely affected by unhealthy lifestyle factors such as obesity, poor diet, cigarette smoking and excessive stress (Homan et al., 2007; Anderson et al., 2010; Sharma et al., 2013). Obesity and smoking are associated with reduced chance of conception, increased risk of miscarriage, and other adverse pregnancy outcomes (Castro and Avina, 2002; Neal et al., 2005; Soares and Melo, 2008; Rittenberg et al., 2011; Chavarro et al., 2012; Firns et al., 2015; Mei-Dan et al., 2015; Valsamakis et al., 2015; Baugh et al., 2016; Lindam et al., 2016). Furthermore, smoking and obesity in pregnancy have been linked with possible adverse long-term health implications for the child, such as childhood cancer and metabolic disease in adulthood (Drake and Reynolds, 2010; Ortega-Garcia et al., 2010; Tan et al., 2015). The mechanisms for the association between pre-pregnancy obesity and impaired fertility and offspring health are not entirely clear (Jungheim et al., 2013; Klenov and Jungheim, 2014), but could include changes to oocyte quality (Minge et al., 2008), epigenetic changes in the embryo (Lane et al., 2015) and impaired uterine implantation potential (Tremellen et al., 2017a). Finally, there is also evidence of an association between certain factors, such as poor diet and psychological stress, and negative fertility outcomes (Group, 2006; Chavarro et al., 2007; Matthiesen et al., 2011; Coughlan et al., 2014), underpinning the importance of pre-conception health counselling for infertile couples to promote and maintain a healthy lifestyle prior to conceiving and throughout pregnancy. Best practice guidelines advise women preparing to conceive to have a health assessment and address unhealthy lifestyle prior to conception (ASRM, 2015; NICE, 2015; RANZCOG, 2015; RTAC, 2015).
In the up to 50% of pregnancies that are unplanned (Rowe et al., 2016), the opportunity to take steps to be in the best health possible before conception does not exist. However, when couples seek fertility care, pre-conception health promotion allows people to learn what they can do to optimise their chance of having a healthy baby. Couples seeking ART treatment to conceive are an ideal group to target for pre-conception care as they are highly motivated to conceive a healthy child. Despite this, little is known about how pre-conception health promotion is addressed within fertility clinics.
Fertility nurses are an essential part of the professional health care team in fertility clinics. They are well educated about reproductive health and fertility, and arguably have the most contact with patients as they undergo ART treatment. However, the role and scope of their practice, particularly with regard to primary health care (PHC) defined as ‘the promotion of a healthy lifestyle to optimise reproductive outcomes’ and in particular pre-conception health promotion, is not well defined (Barber, 2002; Applegarth et al., 2013; Wilson and Leese, 2013; Donati, 2016).
The objective of this study was to investigate current attitudes and practices to pre-conception counselling and the promotion of healthy lifestyle in Australian fertility clinics, and the role that fertility nurses play in this area.
WHAT DOES THIS MEAN FOR PATIENTS?
This study looked at whether fertility clinics in Australia were addressing the lifestyle issues which can make a difference to the outcomes of treatment for their patients.
It is known that obesity, smoking and poor diet can be linked to fertility problems and so guidelines suggest that these should be addressed before starting fertility treatment. This study questioned senior nurses in fertility clinics across Australia to ask what measures were in place at their clinic to address lifestyle issues that might impact on treatment outcomes.
The researchers found that although nurses often raised issues such as obesity, poor diet, lack of exercise and smoking with patients, most of the nurses did not feel they had the skills or resources to offer support to address these issues in their clinics. Only a quarter of clinics had a structured programme in place to support patients to make lifestyle changes and very few of those were recording whether it was making a difference.
The researchers suggest that clinics should educate patients about the importance of a healthy lifestyle and offer support to make changes where necessary. They also suggest that fertility nurses should be given training so that they can help to deliver healthy lifestyle programmes and that the outcomes of such schemes should be monitored.
Materials and Methods
Survey
The Lifestyle in Fertility Care (LIFE) study consisted of a 29-item online survey administered through Survey Monkey Gold software. The questionnaire was divided into four sections, seeking data concerning: information given to patients regarding lifestyle and fertility; resources and support available to facilitate lifestyle modification; the role of fertility nurses, in relation to the ‘promotion of a healthy lifestyle to maximise optimum reproductive outcomes’ and optimising patient health prior to ART treatment; and background information relating to the size of the fertility clinic and the years of ART clinical experience of the respondent. Most questions had fixed-choice response options, however, some provided the participant with an opportunity to include further information. The full questionnaire is available in the Supplementary Data.
Ethical approval
The Social & Behavioural Research Ethics Committee of Flinders University approved this study (Approval number 6749). Completion of the online survey was considered as implied consent.
Participant recruitment
All registered IVF service providers in Australia were identified from the Fertility Society of Australia (FSA) website and the Nurse Manager (or Nurse Co-ordinator) of every listed clinic was approached and informed of the study. Following this initial telephone call an email was sent inviting the nurse to participate, together with an information sheet and a link to the anonymous online survey. Of the 85 clinics approached by telephone, 82 agreed to receive an email invitation containing a link to the survey. After two follow up email contacts, a total of 53 out of 85 potential respondents completed the online survey, a 62% response rate.
Data analysis
Data from the survey were extracted from Survey Monkey (Survey Monkey Inc., Palo Alto, CA, USA) and entered into Excel software (Microsoft, WA, USA), before being subjected to a univariate data analysis in which frequency tables were produced for each question. In Question 12, participants were asked to rate nine lifestyle factors; weight, stress, alcohol, environment, exercise, diet, caffeine, smoking and drugs, using a 9-point Likert scale, where 1 was the most important and 9 the least important. Responses were collapsed into three categories – 1–3 major importance, 4–6 moderate importance and 7–9 minor importance. Free text responses were read and coded by two researchers (GH & SD) and grouped into common categories.
Results
The 53 participating clinics were located across all states and territories of Australia with four in South Australia, 16 in New South Wales, six in Victoria, three in the Australian Capital Territory, three in Western Australia, 19 in Queensland and one each in the Northern Territory and Tasmania. Approximately half of the participants (24) were employed in small clinics that completed less than 400 cycles per year, with the remainder employed in large clinics completing up to 4500 cycles per year. Most of the clinics were located in metropolitan areas (83%), with the remainder in smaller regional cities. Most participants (64%) had been employed as a fertility nurse for 10 years or more, while 19% had been a fertility nurse for 5–10 years and the remaining 17% for 1–5 years.
Informing patients about the impact of lifestyle on fertility
The clear majority of participants (N = 52, 98%) thought that clinics do have a responsibility to address unhealthy lifestyle before offering ART treatment, with most (N = 43, 83%) raising this for discussion at the first clinic visit. Most (N = 50, 94%) also indicated that the provision of information about the potential impact of lifestyle on fertility was very or extremely important, and that both doctors and nurses should provide this information. Ninety two percent (N = 48) of respondents reported that the nurses and 73% (N = 38) of doctors in their clinic did provide patients with this information and advice when appropriate. More than half (N = 31, 58%) reported that nurses in their clinic routinely educate and advise all patients about lifestyle modification, and a further 40% (N = 21) said that nurses did so intermittently depending on their perception of patient’s circumstances. Eighty one percent (N = 43) indicated that it was very important to provide patients with resources to assist with lifestyle modification. However, only 41% (N = 22) considered it very important for the clinic to provide specific support, such as regular phone calls and emails from the fertility nurses, to assist with lifestyle modification.
Addressing lifestyle factors in fertility clinics
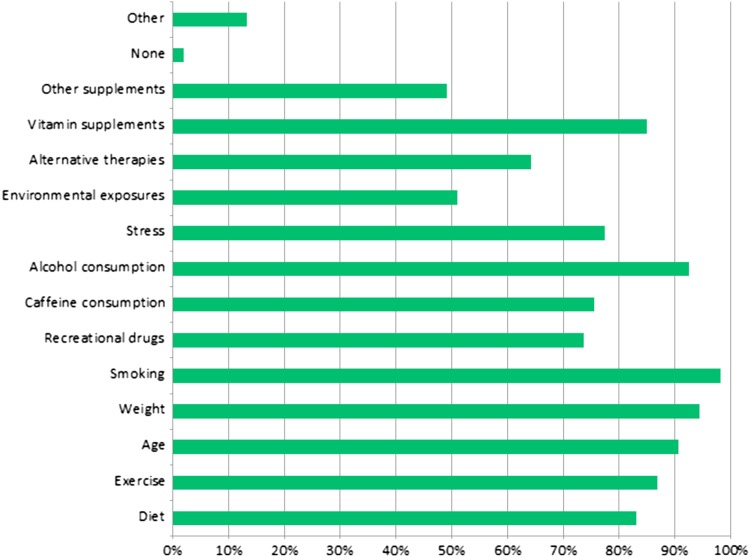
As outlined in Fig. 1, clinics throughout Australia routinely discuss with their patients a wide range of lifestyle factors that may impact on fertility and ART treatment outcomes.
Figure 1.
Lifestyle factors routinely discussed with patients in fertility clinics.
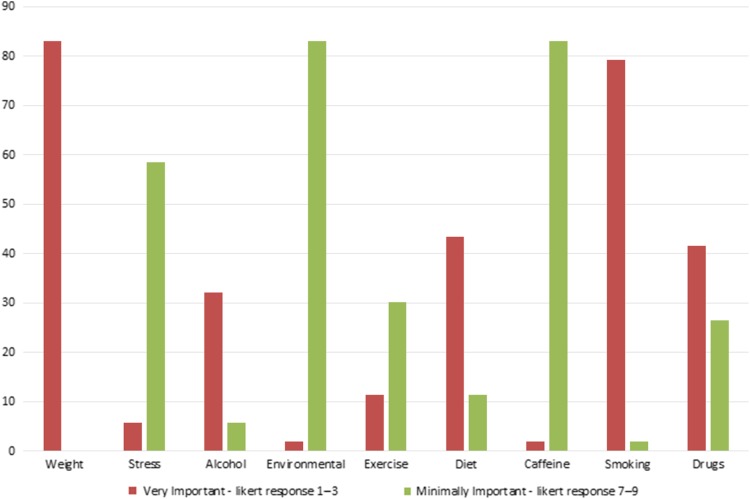
Participants were asked to rate the importance of a range of lifestyle factors, with weight being considered the most important lifestyle factor by respondents, followed by smoking (Fig. 2). The effects of stress, caffeine consumption and recreational drug use were considered of moderate importance, and environmental factors were considered the least important.
Figure 2.
Rating of lifestyle factors in perceived order of importance. Very important: Likert response 1–3, minimally important: Likert scale 7–9.
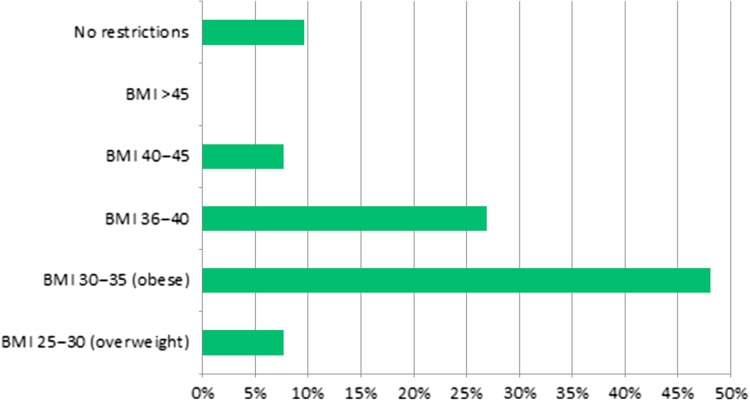
Considering the current recommendations around pre-conception weight (ASRM, 2015; NICE, 2015; RANZCOG, 2015; RTAC, 2015), we asked if there should be a BMI cut-off point for accessing ART treatment. Almost all participants (90%) thought that some BMI related restrictions should be in place. Forty-eight percent thought that the cut-off for treatment should be a BMI in the obese range of 30–35 kg/m2, while 27% thought that the cut-off should be higher at 36–40 kg/m2 (Fig. 3).
Figure 3.
Participants views on the BMI (kg/m2) that should be used as a cut-off point for exclusion from ART treatment.
When asked about policies in their clinic, approximately half (55%) indicated that the clinic did have a policy to guide practice around patient BMI, and 23% of respondents reported that their clinic strictly enforced a BMI restriction for offering ART treatment. A BMI of 35 kg/m2 was used as the cut-off for offering IVF in 15% of the clinics surveyed, and a further 8% used BMI restrictions directly related to the day surgery policy where patient oocyte collections were performed, however a specific BMI was not provided.
Primary health care and ART – supporting patients in making lifestyle modifications
Only 25% of the clinics surveyed offered a structured lifestyle modification programme for their patients. In this study, lifestyle modification programme refers to a programme designed to assist and support patients in addressing any unhealthy lifestyle behaviour, such as poor diet, lack of exercise and smoking, and may include referral to external allied health professionals and resources such as dieticians and physiotherapists.
Those participants whose clinics did offer a programme for patients were asked a series of questions about the programme. Most programmes were run or co-ordinated by a fertility nurse and a few were run by a combination of a nurse and another health professional such as a doctor or dietician. Further content analysis of the responses revealed that some programmes were specifically tailored for individual patients (N = 5), others were designed using a group approach (N = 2), and the remainder consisted of a combination of both approaches (N = 6). A variety of advertising methods were utilised, including the use of fliers, face-to-face contact, a clinic website and social media. One clinic advertised that IVF costs would be reduced (by the cost of the lifestyle modification programme) if a patient completed the programme and did not fall pregnant, however it was not specified whether any patients took advantage of this offer.
Of the programmes being offered, only two clinics said that they were auditing outcomes, with one programme asking patients to complete a questionnaire following completion and the second recording weight loss and pregnancy. While for most programmes data were not formally audited, when asked how the success of the programme was defined, weight loss, pregnancy and live birth were the most common definitions. One response referred to long-term outcomes, ‘the programme provided tools and knowledge to continue with healthy lifestyle’, and another considered patient attendance to be a measurement of success. Participants were also asked if they had any further comments about their programme and one respondent wrote ‘It has not been taken up by many patients, however, those who have, said the programme was of great benefit’.
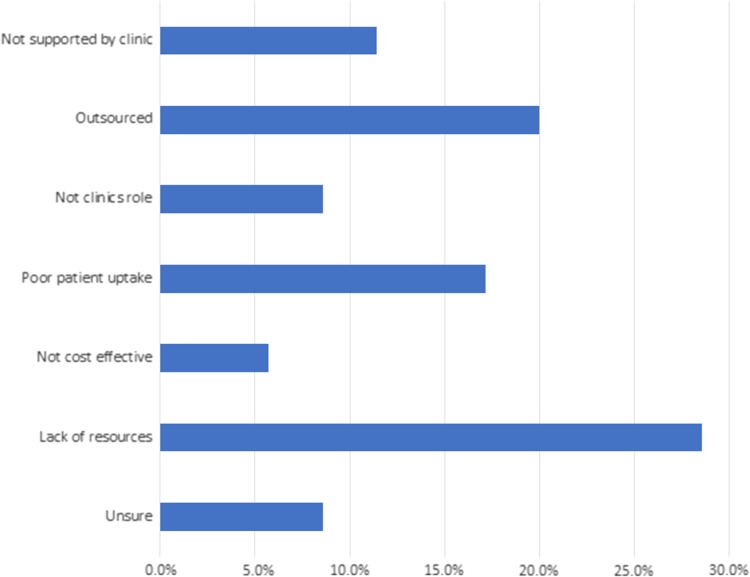
Participants who reported that their clinic did not offer a programme were asked why, and content analysis of their responses revealed some common reasons for not offering a programme. These included a lack of resources, including allocated nursing time and skills to run a programme, limited support from the clinic to run a programme, lack of uptake by patients in the past and the perception that an internal programme was not needed because this service should be outsourced to external allied health providers (Fig. 4).
Figure 4.
Reasons given for clinics not offering a lifestyle modification programme.
Engagement with a primary health care role
When asked their views about the role of fertility nurses in relation to the promotion of primary health care, most respondents (75%) reported that they viewed PHC as a component of their nursing role in a fertility clinic and that nurses in their clinic (58%) were routinely engaged in educating and advising patients about lifestyle modification.
Discussion
Conception is a critical period for the development of an embryo (Norman, 2015) and health professionals working in fertility clinics are in a unique position, where they can recommend and offer lifestyle modification advice and interventions prior to conception. Infertile patients generally attend a specialised fertility clinic after a period of time attempting to conceive naturally and as a result are highly motivated to become pregnant. This provides an opportunity for counselling and encouraging optimum pre-conception health, to improve health outcomes for mothers and babies. At present, the results of this survey suggest this opportunity is not being fully utilised.
The perceived importance placed on a range of modifiable lifestyle factors by the nurses surveyed largely reflected the strength of the evidence in the literature, with weight and smoking being ranked as the most important. Although stress was ranked highly by a few, overall it was not viewed as particularly important by most. Stress has been reported to negatively impact IVF success (Ying et al., 2016) and to be a major factor in ceasing ART treatment (Olivius et al., 2004; McDowell and Murray, 2011), however, it remains unclear whether stress directly impacts on outcomes and how best to address this important area (Pasch et al., 2012). The importance of managing psychological stress in infertility care is evident in the code of practice of the Reproductive Technology Accreditation Committee (RTAC), the body that issues permission to practice ART in Australia. It states that clinics must ensure that patients can access a counsellor should they need to (RTAC, 2015).
Challenges and concerns regarding how best to address poor lifestyle behaviours and suboptimal health in the pre-conception period may increase in the future, with increasing rates of obesity, poor diet and sedentary lifestyle.
Despite recommended national guidelines to address unhealthy lifestyle, such as obesity, prior to conceiving (RANZCOG, 2015; RTAC, 2015), our survey has identified that few clinics had a formal policy that included a specific cut-off BMI for offering ART or lifestyle modification programmes. This is similar in the USA, where a recent study found that only 35% of US clinics use a BMI cut-off for eligibility for treatment, and most do not provide any recommended programme to assist with weight loss (Turner-McGrievy and Grant, 2015).
Addressing obesity in fertility clinics is a complex area, fraught with ethical issues concerning a refusal of access to ART based on weight (Tremellen et al., 2017b), and a tension between the need for weight loss, the time it takes to achieve, and decreasing female fertility with advancing age. There is a need to view obesity in a broad sense and consider a range of associated factors including physical, psychological and social factors. Indeed the need for a thorough pre-conception assessment, including metabolic health and co-morbidities, patient age and history of weight loss attempts has been suggested, in order to determine the most appropriate pathway to follow (Tremellen et al., 2017b).
Given the reticence of clinics to provide structured lifestyle modification programmes despite the potential advantages of such an approach, we suggest that RTAC considers mandating the availability of lifestyle modification programmes in all Australian fertility clinics as a condition of accreditation.
We were surprised to identify that only 85% of clinics discussed the use of prenatal vitamins, despite the overwhelming evidence supporting their effectiveness at reducing foetal abnormalities (RANZCOG, 2015). Furthermore, only 49% of clinics discussed over-the-counter (OTC) supplements with patients. OTC supplements refers to any non-prescription supplements (including herbal), and it has been reported that women of reproductive age including those seeking fertility treatment, often take these despite very limited evidence of benefit and some evidence of potential harm (Stankiewicz et al., 2007; Smith et al., 2013; Byard et al., 2017).
This study has revealed some interesting possible barriers to fertility nurses providing effective pre-conception counselling and assistance with lifestyle modification where appropriate. These barriers include a lack of resources and clinic support, limited knowledge of the most effective strategies to facilitate change, poor patient participation rates in earlier attempts at lifestyle modification, as well as pressure from patients who want to access ART as soon as possible.
Recruitment to lifestyle modification programmes and ongoing maintenance is often challenging, and this has also been found in other health areas (Dalle Grave et al., 2013). A recent RCT highlighted the challenges of establishing and running an effective lifestyle modification programme. Here a 22% drop out rate was reported, mostly due to lack of motivation and minimal outcomes in terms of weight loss, with only 38% achieving their goal of 5–10% weight loss (Mutsaerts, 2016). This may in part be explained by the fact that behavioural change is complex and multifactorial, with some factors being beyond an individual’s control (Michie et al., 2011).
Disappointingly, most of the clinics in our study that offered a lifestyle programme did not audit their results. Resources and future planning are often allocated on performance and evidence of benefit, and auditing outcomes is a useful means of evaluating the success of programmes and of providing a rationale for allocating resources.
Nurses in this study thought that PHC, including assisting patients to modify unhealthy lifestyle, was an important component of their role. Fertility nurses have proven to be effective in managing lifestyle modification programmes (Homan et al., 2012) (Ockhuijsen et al., 2012) (Clark et al., 1998). In these programmes participants successfully modified their lifestyle and nurses were a key factor in the provision of education, guidance and support. In summary, lifestyle modification programmes in ART can work, but only if well planned and executed. Fertility nurses can play a critical role in the provision of these services.
Limitations to the study
A limitation of this study was the survey being completed by only one nurse from each clinic. In future studies, the views of a broader group of health professionals could be investigated. Another limitation was a lack of specific detail requested about pre-conception counselling and any assessment tools that were used in clinics. Finally, only 63% of Australian clinics participated in this survey. While this percentage is generally accepted as a reasonable response for a survey, it would be interesting to examine why a third of clinics did not participate. If their failure to participate indicates a lack of recognition of the importance of lifestyles impact on ART outcomes amongst nurse leaders in fertility care, that would be of concern.
Key recommendations
Recommendations from this study include a need to:
develop and use effective pre-conception screening tools;
prioritise healthy lifestyle before offering ART;
offer resources to facilitate lifestyle modification where appropriate, including programmes and support;
audit the results of lifestyle modification programmes;
utilise fertility nurses in this area by broadening their scope of practice, including further training and recognition of skills.
Supplementary Material
Acknowledgements
The authors thank all the fertility clinics and in particular the nurses who participated in the study.
Supplementary data
Supplementary data are available at Human Reproduction Open online.
Authors’ roles
All authors contributed to the study design, analysis and interpretation of the research, as well as drafting revision and approval of this article.
Funding
No funding was given for this study.
Conflict of interest
The authors declare no conflicts of interest regarding this study.
References
- Anderson K, Norman RJ, Middleton P. Preconception lifestyle advice for people with subfertility. Cochrane Database Syst Rev 2010;14:Cd008189. [DOI] [PubMed] [Google Scholar]
- Applegarth J, Dwyer T, Moxham L, Happell B. Identifying and acquiring the contextual skills and knowledge for nursing practice in assisted reproductive technology: a grounded theory study. J Clin Nurs 2013;22:1738–1747. [DOI] [PubMed] [Google Scholar]
- ASRM Obesity and reproduction: a committee opinion. Fertil Steril 2015;104:1116–1126. [DOI] [PubMed] [Google Scholar]
- Barber D. The extended role of the nurse: practical realities. Hum Fertil (Camb) 2002;5:13–16. [DOI] [PubMed] [Google Scholar]
- Baugh N, Harris DE, Aboueissa AM, Sarton C, Lichter E. The impact of maternal obesity and excessive gestational weight gain on maternal and infant outcomes in maine: analysis of pregnancy risk assessment monitoring system results from 2000 to 2010. J Pregnancy 2016;2016:5871313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byard RW, Musgrave I, Maker G, Bunce M. What risks do herbal products pose to the Australian community? Med J Aust 2017;206:86–90. [DOI] [PubMed] [Google Scholar]
- Castro LC, Avina RL. Maternal obesity and pregnancy outcomes. Curr Opin Obstet Gynecol 2002;14:601–606. [DOI] [PubMed] [Google Scholar]
- Chavarro JE, Ehrlich S, Colaci DS, Wright DL, Toth TL, Petrozza JC, Hauser R. Body mass index and short-term weight change in relation to treatment outcomes in women undergoing assisted reproduction. Fertil Steril 2012;98:109–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chavarro JE, Rich-Edwards JW, Rosner BA, Willett WC. Diet and lifestyle in the prevention of ovulatory disorder infertility. Obstet Gynecol 2007;110:1050–1058. [DOI] [PubMed] [Google Scholar]
- Clark AM, Thornley B, Tomlinson L, Galletley C, Norman RJ. Weight loss in obese infertile women results in improvement in reproductive outcome for all forms of fertility treatment. Hum Reprod 1998;13:1502–1505. [DOI] [PubMed] [Google Scholar]
- Coughlan C, Walters S, Ledger W, Li TC. A comparison of psychological stress among women with and without reproductive failure. Int J Gynaecol Obstet 2014;124:143–147. [DOI] [PubMed] [Google Scholar]
- Dalle Grave R, Calugi S, El Ghoch M. Lifestyle modification in the management of obesity: achievements and challenges. Eat Weight Disord 2013;18:339–349. [DOI] [PubMed] [Google Scholar]
- Donati D. Patient Management: A Nursing Perspective. Organization and management of IVF. New York: Springer Science, 2016, 103–113. [Google Scholar]
- Drake AJ, Reynolds RM. Impact of maternal obesity on offspring obesity and cardiometabolic disease risk. Reproduction 2010;140:387–398. [DOI] [PubMed] [Google Scholar]
- Firns S, Cruzat VF, Keane KN, Joesbury KA, Lee AH, Newsholme P, Yovich JL. The effect of cigarette smoking, alcohol consumption and fruit and vegetable consumption on IVF outcomes: a review and presentation of original data. Reprod Biol Endocrinol 2015;13:134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Group, E. C. W Nutrition and reproduction in women. Hum Reprod Update 2006;12:193–207. [DOI] [PubMed] [Google Scholar]
- Homan GF, Davies M, Norman R. The impact of lifestyle factors on reproductive performance in the general population and those undergoing infertility treatment: a review. Hum Reprod Update 2007;13:209–223. [DOI] [PubMed] [Google Scholar]
- Homan G, Litt J, Norman RJ. The FAST study: Fertility ASsessment and advice Targeting lifestyle choices and behaviours: a pilot study. Hum Reprod 2012;27:2396–2404. [DOI] [PubMed] [Google Scholar]
- Jungheim ES, Travieso JL, Hopeman MM. Weighing the impact of obesity on female reproductive function and fertility. Nutr Rev 2013;71:S3–S8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klenov VE, Jungheim ES. Obesity and reproductive function: a review of the evidence. Curr Opin Obstet Gynecol 2014;26:455–460. [DOI] [PubMed] [Google Scholar]
- Lane M, Zander-Fox DL, Robker RL, McPherson NO. Peri-conception parental obesity, reproductive health, and transgenerational impacts. Trends Endocrinol Metab 2015;26:84–90. [DOI] [PubMed] [Google Scholar]
- Lindam A, Johansson S, Stephansson O, Wikstrom AK, Cnattingius S. High maternal body mass index in early pregnancy and risks of stillbirth and infant mortality – a population-based sibling study in Sweden. Am J Epidemiol 2016;184:98–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthiesen SM, Frederiksen Y, Ingerslev HJ, Zachariae R. Stress, distress and outcome of assisted reproductive technology (ART): a meta-analysis. Hum Reprod 2011;26:2763–2776. [DOI] [PubMed] [Google Scholar]
- McDowell S, Murray A. Barriers to continuing in vitro fertilisation—why do patients exit fertility treatment? Aust N Z J Obstet Gynaecol 2011;51:84–90. [DOI] [PubMed] [Google Scholar]
- Mei-Dan E, Walfisch A, Weisz B, Hallak M, Brown R, Shrim A. The unborn smoker: association between smoking during pregnancy and adverse perinatal outcomes. J Perinat Med 2015;43:553–558. [DOI] [PubMed] [Google Scholar]
- Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci 2011;6:42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minge CE, Bennett BD, Norman RJ, Robker RL. Peroxisome proliferator-activated receptor-gamma agonist rosiglitazone reverses the adverse effects of diet-induced obesity on oocyte quality. Endocrinology 2008;149:2646–2656. [DOI] [PubMed] [Google Scholar]
- Mutsaerts MA. Randomized trial of a lifestyle program in obese infertile women. Ned Tijdschr Geneeskd 2016;160:D916. [PubMed] [Google Scholar]
- Neal MS, Hughes EG, Holloway AC, Foster WG. Sidestream smoking is equally as damaging as mainstream smoking on IVF outcomes. Hum Reprod 2005;20:2531–2535. [DOI] [PubMed] [Google Scholar]
- NICE The National Institute for Health and Care Excellence. 2015https://www.nice.org.uk/
- Norman RJ. From little things, big things grow: the importance of periconception medicine. RANZCOG Arthur Wilson Memorial Oration. Aust N Z J Obstet Gynaecol 2015;55:535–540. [DOI] [PubMed] [Google Scholar]
- Ockhuijsen HD, Gamel CJ, van den Hoogen A, Macklon NS. Integrating preconceptional care into an IVF programme. J Adv Nurs 2012;68:1156–1165. [DOI] [PubMed] [Google Scholar]
- Olivius C, Friden B, Borg G, Bergh C. Why do couples discontinue in vitro fertilization treatment? A cohort study. Fertil Steril 2004;81:258–261. [DOI] [PubMed] [Google Scholar]
- Ortega-Garcia JA, Martin M, Lopez-Fernandez MT, Fuster-Soler JL, Donat-Colomer J, Lopez-Ibor B, Claudio L et al. . Transgenerational tobacco smoke exposure and childhood cancer: an observational study. J Paediatr Child Health 2010;46:291–295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pasch LA, Gregorich SE, Katz PK, Millstein SG, Nachtigall RD, Bleil ME, Adler NE. Psychological distress and in vitro fertilization outcome. Fertil Steril 2012;98:459–464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- RANZCOG Royal Australian and New Zealand College of Obstetricians and Gynaecologists guidelines – Pre pregnancy counselling. 2015https://www.ranzcog.edu.au/Statements-Guidelines
- Rittenberg V, Sobaleva S, Ahmad A, Oteng-Ntim E, Bolton V, Khalaf Y, Braude P, El-Toukhy T. Influence of BMI on risk of miscarriage after single blastocyst transfer. Hum Reprod 2011;26:2642–2650. [DOI] [PubMed] [Google Scholar]
- Rowe H, Holton S, Kirkman M, Bayly C, Jordan L, McNamee K, McBain J et al. . Prevalence and distribution of unintended pregnancy: the Understanding Fertility Management in Australia National Survey. Aust N Z J Public Health 2016;40:104–109. [DOI] [PubMed] [Google Scholar]
- RTAC Code of Practice for Assisted Reproductive Technology Units Fertility Society of Australia. 2015https://www.fertilitysociety.com.au/rtac/
- Sharma R, Biedenharn KR, Fedor JM, Agarwal A. Lifestyle factors and reproductive health: taking control of your fertility. Reprod Biol Endocrinol 2013;11:66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith CA, Bateson DJ, Weisberg E. A survey describing the use of complementary therapies and medicines by women attending a family planning clinic. BMC Complement Altern Med 2013;13:224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soares SR, Melo MA. Cigarette smoking and reproductive function. Curr Opin Obstet Gynecol 2008;20:281–291. [DOI] [PubMed] [Google Scholar]
- Stankiewicz M, Smith C, Alvino H, Norman R. The use of complementary medicine and therapies by patients attending a reproductive medicine unit in South Australia: a prospective survey. Aust N Z J Obstet Gynaecol 2007;47:145–149. [DOI] [PubMed] [Google Scholar]
- Tan HC, Roberts J, Catov J, Krishnamurthy R, Shypailo R, Bacha F. Mother’s pre-pregnancy BMI is an important determinant of adverse cardiometabolic risk in childhood. Pediatr Diabetes 2015;16:419–426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tremelen K, Wilkinson D, Savulescu J. Should obese women’s access to assisted fertility treatment be limited? A scientific and ethical analysis. Aust N Z J Obstet Gynaecol 2017;57:569–574. [DOI] [PubMed] [Google Scholar]
- Tremellen K, Pearce K, Zander-Fox D. Increased miscarriage of euploid pregnancies in obese women undergoing cryopreserved embryo transfer. Reprod Biomed Online 2017;34:90–97. [DOI] [PubMed] [Google Scholar]
- Turner-McGrievy GM, Grant BL. Prevalence of body mass index and body weight cut-off points for in vitro fertilization treatment at U.S. clinics and current clinic weight loss strategy recommendations. Hum Fertil (Camb) 2015;18:215–219. [DOI] [PubMed] [Google Scholar]
- Valsamakis G, Kyriazi EL, Mouslech Z, Siristatidis C, Mastorakos G. Effect of maternal obesity on pregnancy outcomes and long-term metabolic consequences. Hormones (Athens) 2015;14:345–357. [DOI] [PubMed] [Google Scholar]
- Wilson C, Leese B. Do nurses and midwives have a role in promoting the well-being of patients during their fertility journey? A review of the literature. Hum Fertil (Camb) 2013;16:2–7. [DOI] [PubMed] [Google Scholar]
- Ying L, Wu LH, Loke AY. The effect of psychological interventions on the mental health, pregnancy rates, and maritial function of infertile couples undergoing in vitro fertilization: a systematic review. J Assist Reprod Genet 2016;33:689. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.