Abstract
Sporotrichosis is an infection caused by fungi of the Sporothrix complex. The clinical lymphocutaneous presentation corresponds to the great majority of cases. With the increased incidence of sporotrichosis in the State of Rio de Janeiro, Brazil, atypical clinical forms have been reported with increasing frequency, usually associated with immunosuppression. We report the case of a 47-year-old female, with HIV and disseminated sporotrichosis, presenting molluscum-like skin lesions, as well as lung, nasal, and oral mucosa involvement. We also report the first demonstration of culture of Sporothrix in scales of the skin lesion, a fact not identified in the consulted literature.
Keywords: Sporotrichosis, Immunosuppression, HIV, Immunodeficiency
Introduction
Sporotrichosis is an infection caused by fungi of the Sporothrix complex, comprising: S. schenkii, historically associated with the disease; S. brasiliensis, responsible for the majority of cases in the present epidemic in Rio de Janeiro; S. globosa, of global distribution, and the more rare S. mexicana and S. luriei [1]. Traditionally, the infection occurs after inoculation into the dermis and/or subcutaneous tissue after traumatism during contact with plants, wood, or earth [2]. Transmission from animals is considered rare in world literature; however, in Rio de Janeiro, since 1998, an epidemic of the disease transmitted by infected cats to humans is observed [3].
Clinical manifestations of sporotrichosis can be classified as follows: (a) localized cutaneous, when only focal involvement occurs, including fixed lymphocutaneous and cutaneous presentations and corresponding to 90% of the cases; (b) diffuse cutaneous, with extensive cutaneous involvement; and (c) disseminated form, in cases affecting extracutaneous regions [4, 5]. Extracutaneous involvement is not common; when it occurs, the most affected sites are the osteoarticular and pulmonary systems [2]. Reports of mucosal involvement are scarce in the literature; however, in Rio de Janeiro, an increased number of cases of involvement of those areas have been reported [6–8].
Case Report
A 47-year-old female patient, diagnosed with AIDS, who had abandoned treatment about 3 years before hospital admission, presented with a history of disseminated cryptococcosis treated in previous internments. She had psoriasis without follow-up for 7 years. The patient was admitted to our University Hospital with cough, fever, weight loss, and lowering of the consciousness level in the last 2 weeks.
One month earlier, she discovered an erythematous nodule on the side of her right calcaneus, with rapid evolution to ulceration (Fig. 1). She reported appearance of desquamative and itching lesions in plaque in her lower limbs with onset 15 days previously (Fig. 2). Normochromic papules were also observed, with smooth surface, some delineating a central umbilication (molluscum-like lesions) on the face and hands (Fig. 3, Fig. 4). A thorax tomography evidenced cavitation in the lower lobe of the left hemithorax (Fig. 5). Her CD4 count was 47 cells/mm3.
Fig. 1.
Ulceration on the lateral face of the calcaneus of the right foot with onset 1 month before hospitalization.
Fig. 2.
Residual hyperchromic plaques from previous psoriasis on the thigh and scaly plaques on the knee and legs with onset 15 days before hospital admission.
Fig. 3.
Molluscum-like lesions on the face.
Fig. 4.
Molluscum-like lesions on the hand.
Fig. 5.
Thorax CT at the time of admission revealing cavitation in the inferior lobe of the left lung.
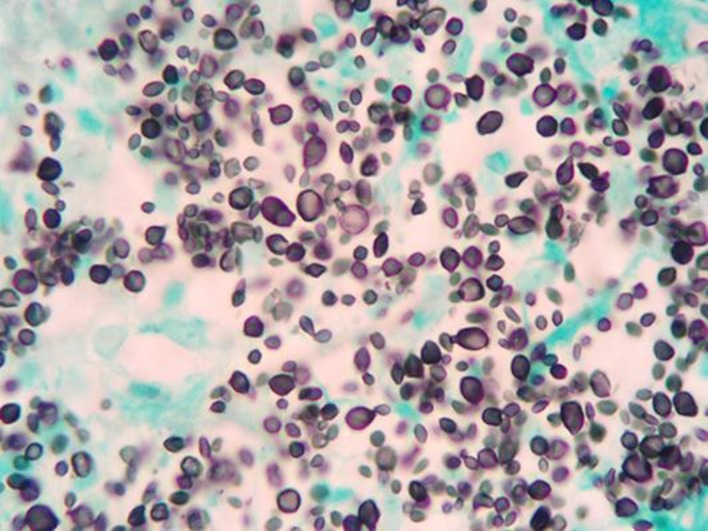
Cultures for common bacteria, microbacteria, and fungi were carried out on material collected from sputum, blood, liquor, and cutaneous scrapings from desquamative lesions of the lower limbs and from cutaneous lesions from two distinct sites: calcaneus ulceration and molluscum-like facial lesions. Cutaneous lesion fragments were also forwarded for histopathologic exam. Sporothrix spp. grew in the cultures of all materials, except for the liquor, which was negative. Grocott's technique revealed abundant cigar- and club-shaped structures (Fig. 6).
Fig. 6.
Histopathology of the calcaneus ulceration showing many rounded fungal forms, some in cigar shape and others in club shape (Grocott, 100×).
After demonstrating the presence of Sporothrix in skin and lungs, and also a positive hemoculture, the diagnosis of disseminated sporotrichosis was established. Administration of liposomal amphotericin B complex 100 mg/day (3 mg/kg daily) was started. Despite this treatment and reintroduction of antiretroviral therapy, the patient evolved with growth and spreading of lesions, and therefore, itraconazole 200 mg/day was associated, but she evolved with worsening of the picture and died 3 months after hospitalization.
Discussion
Cutaneous form is the most frequent clinical presentation of sporotrichosis. It begins with a nodule at the inoculation site, evolving later with ulceration and regional lymphangitis [2]. Disseminated cutaneous form typically presents as diffuse crusty ulcerated nodular lesions, more common in immunosuppressed patients [9–12]. After onset of the sporotrichosis epidemic in Rio de Janeiro, several atypical clinical forms of sporotrichosis have been observed [1]. The first reported case of sporotrichosis manifesting as a molluscum-like lesion was demonstrated by Schechtman et al. in 2011 [13].
Our patient is a new case of this atypical clinical form and, for the first time, a demonstration in culture of Sporothrix from scales of a cutaneous lesion. There was fever, cough, and weight loss, a typical picture of pulmonary tuberculosis, which initially also misled the medical team to suspect that diagnosis. Therefore, despite its rarity, pulmonary sporotrichosis should be considered as part of the differential diagnosis.
For treatment of disseminated sporotrichosis, amphotericin B in liposomal formulation in the dosage of 3–5 mg/kg daily is recommended. To improve evolution, itraconazole 200 mg/day can be associated, with gradual reduction of amphotericin dosage. Itraconazole should be maintained for 12 months and, in immunosuppressed cases, until CD4 exceeds 500 cells/mm3 [14]. Despite these recommendations, Paixão et al. [12], in a report from 2015, describe the difficulty of the therapeutic handling of disseminated sporotrichosis, especially in patients with acquired immunodeficiency syndrome. This fact had also been observed before by Schechtman et al. [13] in 2011, whose patient with disseminated cutaneous sporotrichosis did not show a good therapeutic response even with the use of amphotericin B associated to itraconazole. There are also reports of limited response with association of terbinafine 250 mg/day, itraconazole 200 mg/day, and amphotericin B in liposomal formulation 3–5 mg/kg daily [12, 14]. Paixão et al. [12] described a case where the use of posaconazole 800 mg/day associated to amphotericin B was necessary for sterilization of the liquor of their patient with disseminated sporotrichosis, highlighting the importance of mycological vigilance, especially in patients with neurological symptoms.
Conclusion
With the increasing number of sporotrichosis cases and sporotrichosis-HIV co-infection, the dermatologist must always be alert for less frequent clinical presentations. Treatment of disseminated sporotrichosis remains a challenge, mainly in immunosuppressed patients who often present an erratic therapeutic evolution and response.
Statement of Ethics
The authors have no ethical conflicts to disclose.
Disclosure Statement
The authors have no conflicts of interest to disclose.
References
- 1.Almeida-Paes R, de Oliveira MM, Freitas DF, do Valle AC, Zancopé-Oliveira RM, Gutierrez-Galhardo MC. Sporotrichosis in Rio de Janeiro, Brazil: sporothrix brasiliensis is associated with atypical clinical presentations. PLoS Negl Trop Dis. 2014 Sep;8((9)):e3094. doi: 10.1371/journal.pntd.0003094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Barros MB, de Almeida Paes R, Schubach AO. Sporothrix schenckii and Sporotrichosis. Clin Microbiol Rev. 2011 Oct;24((4)):633–54. doi: 10.1128/CMR.00007-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Silva MB, Costa MM, Torres CC, Galhardo MC, Valle AC, Magalhães MA, et al. [Urban sporotrichosis: a neglected epidemic in Rio de Janeiro, Brazil] Cad Saude Publica. 2012 Oct;28((10)):1867–80. doi: 10.1590/s0102-311x2012001000006. [DOI] [PubMed] [Google Scholar]
- 4.Freitas DF, de Siqueira Hoagland B, do Valle AC, Fraga BB, de Barros MB, de Oliveira Schubach A, et al. Sporotrichosis in HIV-infected patients: report of 21 cases of endemic sporotrichosis in Rio de Janeiro, Brazil. Med Mycol. 2012 Feb;50((2)):170–8. doi: 10.3109/13693786.2011.596288. [DOI] [PubMed] [Google Scholar]
- 5.Moreira JA, Freitas DF, Lamas CC. The impact of sporotrichosis in HIV-infected patients: a systematic review. Infection. 2015 Jun;43((3)):267–76. doi: 10.1007/s15010-015-0746-1. [DOI] [PubMed] [Google Scholar]
- 6.Yamagata JP, Nobre MC, Rudolph FS, de Paiva Barroso IF, Sampaio FM, Freitas DF, Ocular sporothrix Rio de Janeiro Section of the Brazilian Society of Dermatology. Monthly Meeting May 27 2015. http://sbdrj.org.br/eventos/agenda/action~agenda/page_offset~-2/cat_ids~74/request_format~html/ Last viewed Aug 26 2017.
- 7.Morais TS, Ferreira TA, Costa JM, Azambuja D, Setta CR, Sodré CT, Chemosis by Sporothrix Rio de Janeiro Section of the Brazilian Society of Dermatology. Monthly Meeting Sep 30 2015. http://sbdrj.org.br/eventos/agenda/action~agenda/page_offset~-2/cat_ids~74/request_format~html/ Last viewed Aug 26 2017.
- 8.Oliveros JF, Nery JA, Quintella LP, Schechtman RC, Petrosemolo A, Papaiordanou F, Spectral manifestation of ocular sporotrichosis and the role of the demratologist Rio de Janeiro Section of the Brazilian Society of Dermatology. Monthly Meeting Oct 28 2015. http://sbdrj.org.br/eventos/agenda/action~agenda/page_offset~-2/cat_ids~74/request_format~html/ Last viewed Aug 26 2017.
- 9.Romero-Cabello R, Bonifaz A, Romero-Feregrino R, Sanchez CJ, Linares Y, Zavala JT, Romero LC, Romero-Feregrino R, Vega JT. Disseminated sporotrichosis. BMJ Cas Rep. 2011 doi: 10.1136/bcr.10.2010.3404. pii: bcr1020103404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Carvalho MT, de Castro AP, Baby C, Werner B, Filus Neto J, Queiroz-Telles F. Disseminated cutaneous sporotrichosis in a patient with AIDS: report of a case. Rev Soc Bras Med Trop. 2002 Nov-Dec;35((6)):655–9. doi: 10.1590/s0037-86822002000600018. [DOI] [PubMed] [Google Scholar]
- 11.Hardman S, Stephenson I, Jenkins DR, Wiselka MJ, Johnson EM. Disseminated Sporothix schenckii in a patient with AIDS. J Infect. 2005 Oct;51((3)):e73–7. doi: 10.1016/j.jinf.2004.07.001. [DOI] [PubMed] [Google Scholar]
- 12.Paixão AG, Galhardo MC, Almeida-Paes R, Nunes EP, Gonçalves ML, Chequer GL, et al. The difficult management of disseminated Sporothrix brasiliensis in a patient with advanced AIDS. AIDS Res Ther. 2015 May;12((1)):16. doi: 10.1186/s12981-015-0051-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schechtman RC, Crignis GS, Pockstaller MP, Azulay-Abulafia L, Quintella LP, Belo M. Molluscum-like lesions in a patient with sporotrichosis. An Bras Dermatol. 2011 Nov-Dec;86((6)):1217–9. doi: 10.1590/s0365-05962011000600028. [DOI] [PubMed] [Google Scholar]
- 14.Kauffman CA, Bustamante B, Chapman SW, Pappas PG, Infectious Diseases Society of America Clinical practice guidelines for the management of sporotrichosis: 2007 update by the Infectious Diseases Society of America. Clin Infect Dis. 2007 Nov;45((10)):1255–65. doi: 10.1086/522765. [DOI] [PubMed] [Google Scholar]