Virally suppressed HIV-positive individuals on combination antiretroviral therapy who do not achieve a CD4 count >200 cells/µL have substantially increased long-term mortality. The increased mortality was seen across different patient groups and for all causes of death.
Keywords: HIV, CD4 cell recovery, sustained viral suppression, risk factors, mortality
Abstract
Background. Some human immunodeficiency virus (HIV)–infected individuals initiating combination antiretroviral therapy (cART) with low CD4 counts achieve viral suppression but not CD4 cell recovery. We aimed to identify (1) risk factors for failure to achieve CD4 count >200 cells/µL after 3 years of sustained viral suppression and (2) the association of the achieved CD4 count with subsequent mortality.
Methods. We included treated HIV-infected adults from 2 large international HIV cohorts, who had viral suppression (≤500 HIV type 1 RNA copies/mL) for >3 years with CD4 count ≤200 cells/µL at start of the suppressed period. Logistic regression was used to identify risk factors for incomplete CD4 recovery (≤200 cells/µL) and Cox regression to identify associations with mortality.
Results. Of 5550 eligible individuals, 835 (15%) did not reach a CD4 count >200 cells/µL after 3 years of suppression. Increasing age, lower initial CD4 count, male heterosexual and injection drug use transmission, cART initiation after 1998, and longer time from initiation of cART to start of the virally suppressed period were risk factors for not achieving a CD4 count >200 cells/µL. Individuals with CD4 ≤200 cells/µL after 3 years of viral suppression had substantially increased mortality (adjusted hazard ratio, 2.60; 95% confidence interval, 1.86–3.61) compared with those who achieved CD4 count >200 cells/µL. The increased mortality was seen across different patient groups and for all causes of death.
Conclusions. Virally suppressed HIV-positive individuals on cART who do not achieve a CD4 count >200 cells/µL have substantially increased long-term mortality.
The introduction of combination antiretroviral therapy (cART) has decreased morbidity and mortality in individuals infected with human immunodeficiency virus (HIV) due to viral suppression and CD4 cell recovery [1–3]. However, some individuals treated with cART achieve viral suppression but not CD4 cell recovery [4–6]. Several studies have shown that individuals with successful virological response to cART and incomplete CD4 recovery have increased mortality [4, 5, 7–9]. However, the only previous study exclusively examining long-term mortality in individuals started late on cART with sustained viral load (VL) suppression and low CD4 count is limited by small sample size [8].
By combining data from 2 large international collaborations of HIV cohorts, the Antiretroviral Therapy Cohort Collaboration (ART-CC) and the Collaboration of Observational HIV Epidemiological Research Europe (COHERE), we examined risk factors for failure to achieve CD4 recovery among treated individuals who were virally suppressed for >3 years, and compared mortality rates after 3 years of viral suppression according to the CD4 cell count reached at the end of the virally suppressed period.
METHODS
Setting and Participants
The ART-CC (http://www.art-cohort-collaboration.org) is an international collaboration of 18 cohort studies of HIV type 1 (HIV-1)–positive individuals from Europe and North America that was established in 2000 to examine the prognosis of HIV-1–positive, treatment-naive individuals initiating cART [10]. COHERE (http://www.cohere.org) was established in 2005 and is an international collaboration of 35 cohorts from 29 European countries. The COHERE data were pooled within the EuroCoord network (www.eurocoord.net). Each collaboration focuses on scientific questions requiring large sample sizes, which the contributing cohorts cannot answer individually [11].
Study Population and Design
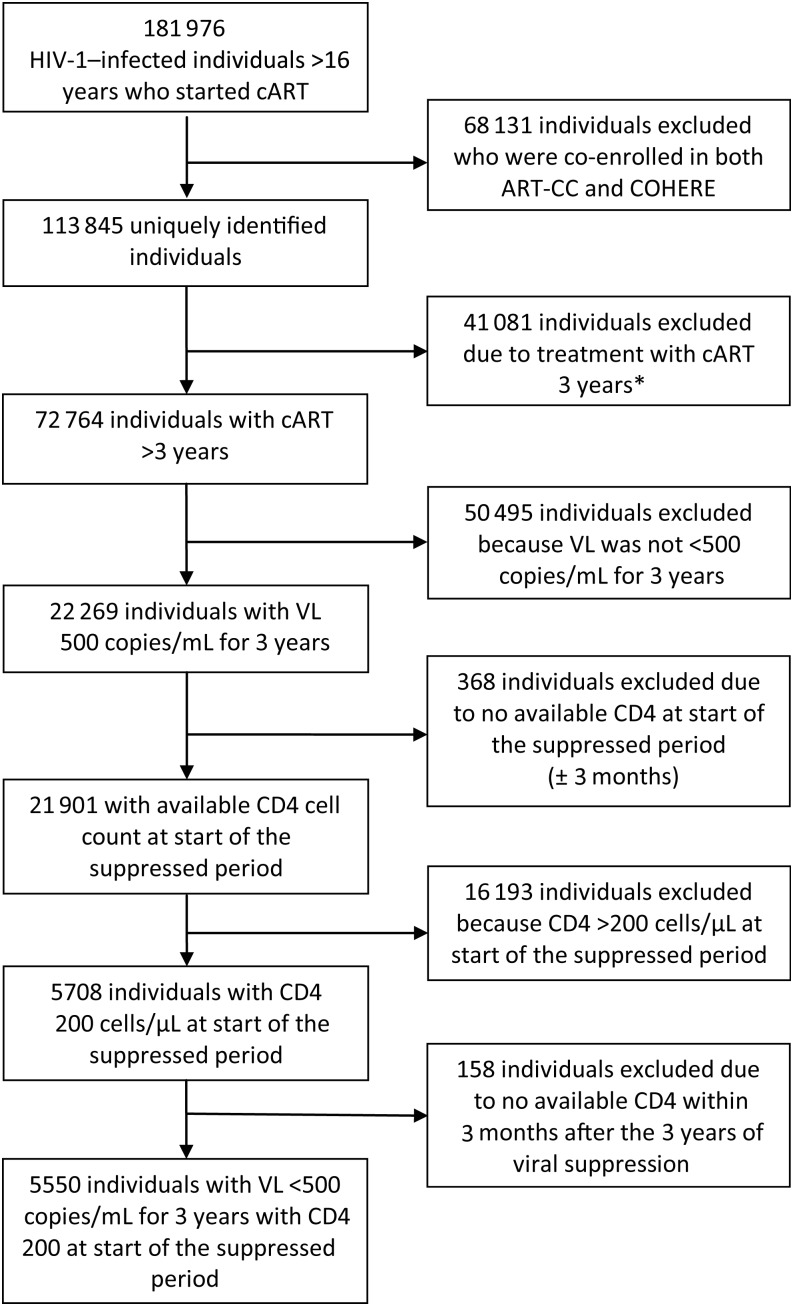
We identified all HIV-1–positive individuals who (1) were >16 years old at start of the suppressed period; (2) were on cART continuously (defined in ART-CC as treatment with at least 3 drugs from 2 different classes and in COHERE as the concomitant use of at least 3 antiretroviral drugs) for at least 3 years; (3) after start of cART had a period with suppressed VL of at least 3 years (all VL ≤500 HIV-1 RNA copies/mL and never a time span of >7 months between VL measurements); and (4) had a CD4 cell count ≤200 cells/µL at the start of the virally suppressed period (Figure 1). Individuals enrolled in >1 cohort were identified and only 1 record per individual was included. A VL cutoff of ≤500 copies/mL was chosen to overcome the heterogeneity of the assay detection limits used during the study period.
Figure 1.
Flowchart and study timeline. *Of the 41 081 patients who were not on combination antiretroviral therapy for >3 years, 4677 (11.3%) died. Among these individuals, 1020 (12.8%) had an available viral load measurement within 3 months from date of death, and 44 (4.3%) were virally suppressed at time of death. Abbreviations: ART-CC, Antiretroviral Therapy Cohort Collaboration; cART, combination antiretroviral therapy; COHERE, Collaboration of Observational HIV Epidemiological Research Europe; HIV-1, human immunodeficiency virus type 1; VL, viral load.
Statistical Analysis
Risk Factors for Failure to Achieve a CD4 Count >200 Cells/µL After 3 Years of Viral Suppression
We used logistic regression to identify risk factors for not achieving CD4 count >200 cells/µL after 3 years of sustained viral suppression. We assessed the effect of CD4 cell count at the start of the suppressed period as a categorical variable (0–25, 26–50, 51–100, 101–150, and 151–200 cells/µL). In a sensitivity analysis, we fit separate models for each of these CD4 strata. The following variables were included in all models: age at start of virally suppressed period (<30, 30–39, 40–49, ≥50 years), probable route of infection (men who have sex with men [MSM], male heterosexual sex, female heterosexual sex, injection drug use [IDU], other/unknown [the number of male and female injection drug user and other/unknowns did not allow for further classification according to sex]), pre-cART VL (last VL available within 3 months before start of cART or first VL within a month after start of cART if the former was not available; VL <100 000 copies/mL, ≥100 000 copies/mL, and missing), year of cART initiation (1996–1997, 1998–2000, 2001 onward), time from cART initiation to start of suppressed period (<12 months, ≥12 months), AIDS (no AIDS event, ≥1 AIDS event before start of the virally suppressed period). We tested for interactions between pairs of variables.
Risk Factors for Mortality After 3 Years of Viral Suppression
Person-years at risk were calculated from the date of the first CD4 count within 3 months after 3 years of viral suppression to the earlier of time of death, loss to follow-up, or end of observation. We estimated mortality rates and Kaplan-Meier plots according to CD4 count at the end of the 3-year virally suppressed period (≤200, 201–350, 351–500, or >500 cells/µL) and used Cox regression to estimate hazard ratios (HRs) for death according to these CD4 count groups. All analyses were adjusted for the covariates listed above (AIDS events in this analysis were up to the end of the virally suppressed period) and stratified by cohort. We used Cox regression to compare individuals with CD4 counts ≤200 cells/µL and >200 cells/µL at the end of the suppressed period within strata defined by age at start of virally suppressed period, route of infection, AIDS status, and CD4 at start of suppressed period. In sensitivity analyses, we used a cutoff value of 50 copies/mL to define viral suppression and included only study subjects reporting sexual route of transmission and no positive test for hepatitis C virus (HCV) coinfection (HCV was defined as a positive test for HCV RNA or a positive test for HCV immunoglobulin G antibody at any time during follow-up).
Analysis of Causes of Death
COHERE does not collect data on causes of death, so these analyses were restricted to individuals included in ART-CC. Supplementary Data 1 describes how the causes of death data in this study were assigned and categorized. Causes of death were further categorized as AIDS defining, non–AIDS defining, unnatural (accident/violent/suicide/drug abuse), and unknown [12]. Non-AIDS causes of death were further divided into hepatitis, cancers, and other. Because analyses of different causes of death can pose the problem of competing risks, we estimated both subdistribution HRs (using the Fine and Gray approach) and standard (Cox) HRs (adjusted only for age and sex due to the small number of events) [13]. Because these estimates did not differ appreciably, we report only the estimates from Cox models. SPSS statistical software, version 15.0 (Norusis; SPSS Inc, Chicago, Illinois) and R software, version 2.8.1, were used for data analysis.
RESULTS
We identified 113 845 unique HIV-1–positive individuals from the COHERE and ART-CC cohorts, of whom 41 081 were treated with cART for <3 years, 50 495 did not have sustained viral suppression, and 368 had no available CD4 measurement at the start of the suppressed period. Of 21 901 individuals who achieved sustained viral suppression for ≥3 years, 16 193 had a CD4 count >200 cells/µL at start of the virally suppressed period and 158 had no available CD4 measurement at the end of the suppressed period, leaving 5550 individuals (20 291 person-years of observation; median follow-up time; 3.4 years [interquartile range, 1.6–5.3 years]) eligible for analyses (Figure 1). A histogram of the distribution of CD4 count at the start of the virally suppressed period is shown in Supplementary Data 2. The majority of these (4715 [85.0%]) achieved a CD4 count >200 cells/µL after 3 years of viral suppression. Half (2904 [52.3%]) were aged >40 years at the start of the suppressed period (Table 1).
Table 1.
Clinical and Demographic Characteristics of 5550 Eligible HIV-Infected Individuals
| Characteristic | CD4 Count at End of Virally Suppressed
Period |
|
|---|---|---|
| ≤200 Cells/µL | >200 Cells/µL | |
| No. of patients (person-years of observation) | 835 (2936) | 4715 (17 355) |
| No. of deaths (mortality rate per 100 person-years at risk) | 66 (2.2) | 109 (0.6) |
| Median time from start of cART to start of the suppressed period, mo (IQR) | 2.8 (1.3–12.1) | 2.5 (1.2–5.5) |
| Age at start of the suppressed period, y | ||
| <30 | 45 (5.4) | 512 (10.9) |
| 30–39 | 233 (27.9) | 1956 (41.5) |
| 40–49 | 275 (32.9) | 1440 (30.5 |
| >50 | 282 (33.8) | 907 (17.1) |
| Route of transmission | ||
| MSM | 227 (27.2) | 1695 (35.9) |
| Male heterosexual sex | 216 (25.9) | 995 (21.1) |
| Female heterosexual sex | 101 (12.1) | 933 (19.8) |
| Injection drug use | 128 (15.3) | 489 (10.4) |
| Other/unknown | 163 (18.6) | 603 (12.8) |
| CD4 count at start of the suppressed period, cells/µL | ||
| ≤25 | 75 (9.0) | 223 (4.7) |
| 26–50 | 108 (12.9) | 370 (7.8) |
| 51–100 | 268 (32.1) | 970 (20.6) |
| 101–150 | 231 (27.7) | 1377 (29.2) |
| 151–200 | 153 (18.3) | 1775 (37.6) |
| Last viral load measurement before start of cART, copies/mL | ||
| <100 000 | 391 (46.8) | 2129 (38.4) |
| ≥100 000 | 424 (50.8) | 2470 (44.5) |
| Viral load measurement missing | 20 (2.4) | 116 (2.5) |
| Year of start of cART | ||
| 1996–1997 | 69 (8.3) | 442 (9.4) |
| 1998–2000 | 336 (40.2) | 1686 (35.8) |
| 2001 onward | 430 (51.5) | 2587 (54.9) |
| Time from cART initiation to start of suppressed period, mo | ||
| <12 | 626 (75.0) | 3952 (83.8) |
| ≥12 | 209 (25.0) | 763 (16.2) |
| 1 or more AIDS events before start of suppressed period | ||
| No AIDS event | 425 (51.9) | 2580 (54.7) |
| AIDS event | 410 (49.1) | 2135 (45.3) |
From the Antiretroviral Therapy Cohort Collaboration (ART-CC) and the Collaboration of Observational HIV Epidemiological Research Europe (COHERE), 2012. Data are presented as No. (%) unless otherwise specified.
Abbreviations: cART, combination antiretroviral therapy; HIV, human immunodeficiency virus; IQR, interquartile range; MSM, men who have sex with men.
Risk Factors for Failure to Achieve CD4 Count >200 Cells/µL
We found that risk of failure to achieve a CD4 count >200 cells/µL increased with increasing age and with decreasing CD4 count at start of the virally suppressed period (Table 2). Compared with MSM, men with heterosexual route of infection, injection drug users, and those with other or unknown transmission group had greater risk of incomplete CD4 recovery. Risk was also greater in those whose last viral load before start of cART was <100 000 copies/mL, those who initiated cART after 1998, and those who had 12 months or more from initiation of cART to start of the virally suppressed period. In models stratified on CD4 at start of the suppressed period, the impact of age and AIDS-defining illness on incomplete CD4 recovery appeared to be similar across CD4 strata (Supplementary Table 1). Patients infected via IDU had consistently higher risk of incomplete CD4 recovery than those infected via MSM transmission.
Table 2.
Factors Associated With Failure to Achieve CD4 Count >200 Cells/µL After 3 Years of Viral Suppression on Combination Antiretroviral Therapy
| Factor | Unadjusted OR (95% CI) | Adjusted ORa (95% CI) |
|---|---|---|
| Age at start of the suppressed period, y | ||
| <30 | 1 (reference) | 1 (reference) |
| 30–39 | 1.36 (.97–1.89) | 1.31 (.93–1.85) |
| 40–49 | 2.17 (1.56–3.03) | 2.04 (1.45–2.88) |
| ≥50 | 3.98 (2.85–5.55) | 4.01 (2.84–5.68) |
| Route of transmission | ||
| MSM | 1 (reference) | 1 (reference) |
| Male heterosexual sex | 1.62 (1.32–1.98) | 1.50 (1.21–1.85) |
| Female heterosexual sex | 0.81 (.63–1.04) | 0.89 (.68–1.15) |
| Injection drug use | 1.96 (1.54–2.48) | 2.03 (1.57–2.61) |
| Other/unknown | 2.02 (1.62–2.52) | 1.72 (1.37–2.17) |
| CD4 count at start of suppressed period, cells/µL | ||
| ≤25 | 3.90 (2.86–5.32) | 5.21 (3.75–7.23) |
| 26–50 | 3.39 (2.58–4.44) | 4.46 (3.35–5.95) |
| 51–100 | 3.21 (2.59–3.97) | 3.73 (2.99–4.68) |
| 101–150 | 1.95 (1.57–2.42) | 2.08 (1.67–2.60) |
| 151–200 | 1 (reference) | 1 (reference) |
| Last viral load measurement before start of cARTb, copies/mL | ||
| <100 000 | 1.07 (.92–1.24) | 1.13 (.97–1.33) |
| ≥100 000 | 1 (reference) | 1 (reference) |
| Year of start of cART | ||
| 1996–1997 | 1 (reference) | 1 (reference) |
| 1998–2000 | 1.28 (.97–1.69) | 1.44 (1.07–1.93) |
| 2001 onward | 1.07 (.81–1.40) | 1.37 (1.02–1.84) |
| Time from cART initiation to start of suppressed period, mo | ||
| <12 | 1 (reference) | 1 (reference) |
| ≥12 | 1.73 (1.45–2.06) | 2.05 (1.68–2.50) |
| 1 or more AIDS events before start of suppressed period | ||
| No AIDS event | 1.17 (1.01–1.35) | 0.89 (.76–1.04) |
| AIDS event | 1 (reference) | 1 (reference) |
From the Antiretroviral Therapy Cohort Collaboration (ART-CC) and the Collaboration of Observational HIV Epidemiological Research Europe (COHERE), 2012.
Abbreviations: cART, combination antiretroviral therapy; CI, confidence interval; HIV, human immunodeficiency virus; MSM, men who have sex with men; OR, odds ratio.
a All variables are included in the adjusted estimates.
b One hundred thirty-six individuals had no baseline viral load and were included in the analysis as missing viral load.
Time to Death From Any Cause
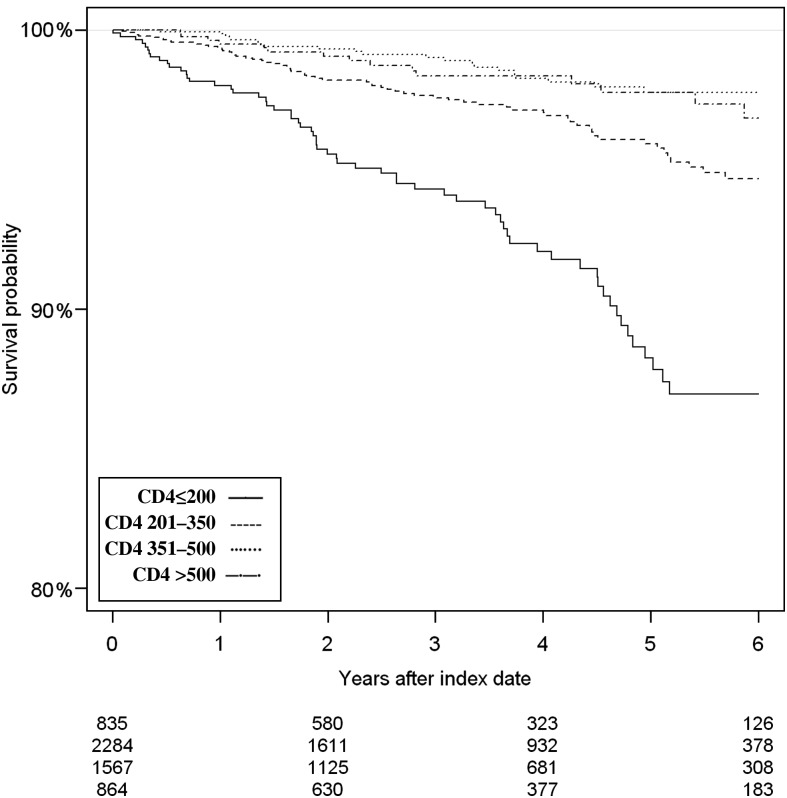
A total of 175 (3.2%) individuals died: 66 (7.9%) of those who did not attain a CD4 count >200 cells/µL and 109 (2.3%) of those who attained a CD4 count >200 cells/µL. Table 3 shows that individuals who did not attain a CD4 count >200 cells/µL after 3 years of sustained viral suppression had substantially increased mortality compared with those who achieved a CD4 count >200 cells/µL (adjusted HR, 2.60 [95% CI, 1.86–3.61]). The cumulative probability of survival stratified by CD4 count is presented in Figure 2. The estimated 5-year cumulative mortality (with 95% CIs) was 11.8% (8.9%–15.2%) in patients with a CD4 count <200 cells/µL at the end of the suppressed period, compared with 4.1% (3.1%–5.3%), 2.2% (1.4%–3.4%), and 2.2% (1.2%–3.7%) in patients with a CD4 count of 201–350, 351–500, and >500 cells/µL, respectively, at the end of the suppressed period. Compared with individuals with CD4 count >500 cells/µL at the end of the suppressed period, adjusted HRs in individuals with a CD4 count of 351–500, 201–350, and ≤200 CD4 cells/µL were 0.62 (95% CI, .32–1.19), 1.28 (95% CI, .74–2.23), and 2.62 (95% CI, 1.47–4.67), respectively.
Table 3.
Mortality Hazard Ratios Comparing Individuals With CD4 Count ≤200 and >200 Cells/µL at the End of the Suppressed Period
| Strata | Deaths, No. |
Person-Years of Observation |
Crude HR(95% CI) | Adjusteda HR (95% CI) | ||
|---|---|---|---|---|---|---|
| ≤200 Cells/µL | >200 Cells/µL | ≤200 Cells/µL | >200 Cells/µL | |||
| All individuals | 66 | 109 | 2937 | 17 346 | 3.35 (2.46–4.57) | 2.60 (1.86–3.61) |
| Age, y | ||||||
| <30 | 1 | 2 | 154 | 1826 | NA | NA |
| 30–39 | 8 | 25 | 863 | 7457 | 3.00 (1.33–6.76) | 3.01 (1.26–7.16) |
| 40–49 | 19 | 40 | 937 | 5174 | 2.50 (1.44–4.34) | 2.04 (1.12–3.70) |
| ≥50 | 38 | 42 | 983 | 2889 | 2.51 (1.61–3.93) | 3.18 (1.96–5.14) |
| Route of transmission | ||||||
| MSM | 13 | 30 | 84 | 6694 | 3.58 (1.85–6.93) | 2.62 (1.28–5.34) |
| Male heterosexual | 14 | 25 | 729 | 3516 | 2.86 (1.47–5.57) | 2.41 (1.19–4.86) |
| Female heterosexual | 7 | 7 | 298 | 2975 | 8.21 (2.80–24.05) | NA |
| Injection drug use | 12 | 27 | 461 | 1810 | 1.60 (.78–3.27) | 1.43 (.65–3.17) |
| Other/unknown | 20 | 20 | 605 | 2350 | 3.13 (1.68–5.83) | 2.53 (1.26–5.07) |
| CD4 count at start of suppressed period, cells/µL | ||||||
| ≤25 | 6 | 2 | 317 | 904 | NA | NA |
| 26–50 | 6 | 5 | 452 | 1386 | 2.92 (.86–9.93) | 2.76 (.66–11.46) |
| 51–100 | 17 | 26 | 973 | 3731 | 2.56 (1.35–4.85) | 1.43 (.71–2.88) |
| 101–150 | 22 | 40 | 735 | 5022 | 3.40 (2.00–5.75) | 2.62 (1.49–4.60) |
| 151–200 | 15 | 36 | 459 | 6303 | 5.57 (3.01–10.32) | 3.82 (1.95–7.45) |
| Last viral load before start of cART, copies/mL | ||||||
| Viral load <100 000 | 30 | 51 | 1365 | 7520 | 2.98 (1.88–4.72) | 2.23 (1.34–3.72) |
| Viral load ≥100 000 | 33 | 58 | 1517 | 9504 | 3.19 (2.06–4.94) | 2.61 (1.63–4.18) |
| Year of cART initiation | ||||||
| 1996–1997 | 8 | 22 | 394 | 2750 | 2.87 (1.24–6.64) | 2.25 (.87–5.84) |
| 1998–2000 | 40 | 56 | 1535 | 8453 | 3.65 (2.42–5.51) | 2.74 (1.74–4.30) |
| 2001 onward | 18 | 31 | 1008 | 6143 | 3.39 (1.87–6.14) | 3.03 (1.62–5.65) |
| Time from cART initiation to start of suppressed period, mo | ||||||
| <12 | 18 | 18 | 573 | 2336 | 3.04 (2.13–4.33) | 2.51 (1.23–5.14) |
| ≥12 | 48 | 91 | 2363 | 15 010 | 3.96 (2.03–7.70) | 2.53 (1.72–3.70) |
| 1 or more AIDS events by end of suppressed period | ||||||
| No AIDS event | 28 | 48 | 13 507 | 8584 | 3.51 (2.18–5.64) | 2.49 (1.47–4.20) |
| AIDS event | 38 | 61 | 1587 | 8762 | 3.05 (2.02–4.61) | 2.47 (1.59–3.83) |
From the Antiretroviral Therapy Cohort Collaboration (ART-CC) and the Collaboration of Observational HIV Epidemiological Research Europe (COHERE), 2012.
Abbreviations: cART, combination antiretroviral therapy; CI, confidence interval; HIV, human immunodeficiency virus; HR, hazard ratio; MSM, men who have sex with men; NA, numbers in these strata were too small for an analysis to be performed.
a Adjusted for all other covariates listed in the table. Stratification factor removed from list of adjustments.
Figure 2.
Cumulative probability of survival stratified by CD4 count at the end of the virally suppressed period: ≤200 cells/µL (full line); 201–350 cells/µL (broken line); 351–500 cells/µL (dotted line); and >500 cells/µL (broken and dotted line).
Mortality Hazard Ratios Stratified by Risk Factors
Table 3 shows that the impact on mortality of not achieving a CD4 count >200 cells/µL was most pronounced in individuals whose CD4 count at the start of the suppressed period was 151–200 cells/µL (those in whom the increase in CD4 since start of ART was lowest). However, estimated HRs within CD4 strata were estimated imprecisely, and their CIs overlapped. The impact of incomplete CD4 recovery appeared similar across strata defined by age, mode of transmission, viral load before start of cART, year of cART initiation, time from initiation of cART to start of the virally suppressed period, and AIDS-defining disease (Table 3).
Sensitivity Analyses
Of 2692 individuals who were eligible when a cutoff of 50 copies/mL for viral suppression was used, 2253 (83.7%) achieved a CD4 count >200 cells/µL. Estimated effects of risk factors for not achieving a CD4 count >200 cells/µL were broadly similar to those in the main analyses, although there was less evidence of elevated risk among heterosexual men (adjusted odds ratio, 1.17 [95% CI, .88–1.55]) and women (0.64 [95% CI, .45–.93]) (Supplementary Table 2). In this analysis, a total of 33 (7.5%) and 41 (1.8%) individuals with and without incomplete CD4 recovery, respectively, died during follow-up, and the adjusted HR for not attaining (compared with attaining) a CD4 count >200 cells/µL was 3.96 (95% CI, 2.36–6.66). Exclusion of 1625 (29.3%) individuals who did not report sexual route of transmission nor had HCV coinfection left 3925 individuals with 87 deaths. The adjusted HR for not attaining (compared with attaining) a CD4 count >200 cells/µL was 2.98 (95% CI, 1.85–4.79).
Time to Death From Specific Causes
Of 4135 individuals included in analyses of cause-specific mortality, 619 (15.0%) did not attain a CD4 count >200 cells/µL after the suppressed period and 121 (2.9%) died. Most deaths were from non-AIDS-defining causes, in both groups (Table 4). Mortality due to AIDS-defining, non-AIDS-defining, and unnatural causes of death was increased substantially in individuals who did not attain a CD4 count >200 cells/µL and was highest for hepatitis and non-AIDS-defining cancers (adjusted HRs, 6.76 [95% CI, 1.93–23.74] and 2.89 [95% CI, 1.44–5.28], respectively).
Table 4.
Cause-Specific Hazard Ratios Comparing HIV-Infected Individuals (ART-CC Only) With CD4 Count ≤200 Versus >200 Cells/µL at End of Suppressed Period
| Causes of Death | No. (%) of Deaths According to CD4 Count
at End of Suppressed Period |
HR (95% CI) |
||
|---|---|---|---|---|
| ≤200 Cells/µL | >200 Cells/µL | Unadjusted | Adjusteda | |
| All | 41 (100) | 80 (100) | 3.05 (2.10–4.44) | 2.52 (1.71–3.70) |
| AIDS-defining causes of death | 4 (9.8) | 7 (8.8) | 3.39 (0.99–11.57) | 2.75 (0.78–9.69) |
| Non-AIDS-defining causes of death | 26 (63.4) | 49 (61.3) | 3.14 (1.95–5.06) | 2.61 (1.61–4.23) |
| Hepatitis | 5 | 5 | 5.95 (1.72–20.56) | 6.76 (1.93–23.74) |
| Non-AIDS cancer | 14 | 23 | 3.50 (1.73–6.95) | 2.89 (1.44–5.28) |
| Other causes of deathb | 6 | 21 | 1.69 (0.68–4.18) | 1.24 (0.50–3.12) |
| Unnatural causes of death | 3 (7.3) | 8 (10.0) | 2.27 (0.60–8.57) | 2.07 (0.54–7.97) |
| Unknown causes of death | 8 (19.5) | 16 (19.5) | 3.00 (1.28–7.01) | 2.34 (0.98–5.59) |
From the Antiretroviral Therapy Cohort Collaboration (ART-CC) and the Collaboration of Observational HIV Epidemiological Research Europe (COHERE), 2012.
Abbreviations: ART-CC, Antiretroviral Therapy Cohort Collaboration; CI, confidence interval; HIV, human immunodeficiency virus; HR, hazard ratio.
aAdjusted for sex and age (≤50 years vs >50 years).
bOther causes of death for patients with CD4 count ≤200 cells/µL were related to infection (2), cardiovascular disease (2), and digestive system disease (2). Other causes of death for patients with CD4 count >200 cells/µL were related to infection (5), lung diseases (2), cardiovascular diseases (9), digestive system diseases (2), central nervous system diseases (2), and renal diseases (1).
DISCUSSION
Based on data combined from 2 large international HIV cohort collaborations, we found that among HIV-positive individuals with 3 years of viral suppression on cART, those with incomplete CD4 recovery (CD4 count ≤200 cells/µL) had markedly higher mortality rates than those who achieved a CD4 count >200 cells/µL. These higher rates were observed consistently across strata defined by age, sex, route of transmission, and prior AIDS-defining illness. Rates of both AIDS- and non-AIDS-defining causes of death were elevated. We identified older age, transmission via male heterosexual sex or IDU, lower CD4 count at start of the suppressed period, and longer time from initiation of cART to start of the virally suppressed period as risk factors for incomplete CD4 cell recovery.
Strengths and Weaknesses
Because 15% of treated HIV-positive individuals have a CD4 count <200 cells/µL after long-term viral suppression, prognosis of such patients is a major concern. By combining data from 2 collaborations of HIV cohort studies, we assembled a sufficiently large data set to permit us to examine both risk factors and prognosis for all-cause and cause-specific mortality among patients with incomplete CD4 recovery. The contributing cohort studies represent a wide variety of countries and settings, and our results are therefore likely to be generalizable to treated HIV-positive individuals in Western Europe and North America. Not all contributing cohorts link their data with national death registries, which may lead to an underestimation of mortality rates. However, estimates of relative mortality comparing different groups should not be biased, providing that nonascertained deaths are missing at random [14]. Serological tests for coinfection with HCV were not performed systematically in all cohorts; therefore, some coinfected individuals may have been misclassified. However, findings were similar in a sensitivity analysis excluding both injection drug users and HCV-coinfected individuals, and the impact of misclassification of HCV serostatus may have been limited because of its strong association with transmission via IDU, which was available from all cohorts. We did not have access to data on smoking, other comorbidity (eg, diagnosis of non-AIDS cancers) or non-cART medications (eg, cancer chemotherapy) and were therefore not able to adjust for such factors or assess whether they predict incomplete CD4 recovery.
Our definition of CD4 recovery (CD4 count >200 cells/µL after 3 years of viral suppression following cART initiation) differs from other definitions of recovery: for example, National Institutes of Health guidelines defined an adequate response as an increase in CD4 count in the range of 50–150 cells/µL per year [15]. Our definition of CD4 recovery was based on 2 considerations. First, the increase in CD4 count over time since start of cART in virologically suppressed patients depends on baseline CD4 count [6]. Second, the risk of mortality is strongly related to current CD4 count [16, 17].
Results in Context With Other Literature
Previous studies have identified age [8, 18, 19] and low baseline CD4 counts [4, 18, 20] as risk factors for incomplete CD4 cell recovery. However, 2 of these [16, 20] used designs that differed from ours in terms of inclusion criteria and length of the virally suppressed period. The effect of age observed in our study is consistent with its association with thymus size and activity and suggests that initiation of cART before immune incompetence occurs is especially important in older HIV-infected individuals [21–23].
Most studies that examined clinical endpoints according to achieved CD4 count in virally suppressed patients used short periods of viral suppression or did not have inclusion criteria relating to baseline CD4 count [9, 17, 24]. These studies mainly estimated short-term effects of changes in CD4 count, rather than elucidating the long-term impact of sustained low CD4 cell counts in patients who are virally suppressed long-term. Two previous studies examined implications of incomplete CD4 recovery among patients with sustained viral suppression, and our findings are in accordance with their estimates. Loutfy et al observed a 2.69-fold (95% CI, 1.26- to 5.78-fold) increase in mortality comparing 176 patients with a CD4 count <200 cells/µL with 1545 patients with a CD4 count >200 cells/µL after 2 years of viral suppression [24]. That study had both a shorter duration of and less strict criteria for viral suppression as well as a much smaller and less generalizable sample. We previously reported the relative risk of death to be 3.4 (95% CI, 1.4–8.0) in a small study comparing 55 immunological nonresponders with 236 responders in the Danish HIV Cohort Study, using a design almost identical to that of the present study [8]. Data on causes of death were not available in either of these 2 studies. Although we observed increased mortality in all subgroups of individuals with poor CD4 recovery, the relative risk of death was greatest among individuals with baseline CD4 count between 151 and 200 cells/µL. These individuals are characterized by the lowest increase (or even a decrease) in CD4 counts during the 3-year period of virological suppression, a phenomenon that may be related to non-HIV comorbidity such as cancer.
Consistent with our results, previous studies have found incomplete CD4 recovery to be associated with an increased risk of non-AIDS cancer [25–27]. It is still a matter of debate whether low CD4 counts lead to non-AIDS-defining cancers or whether common risk factors lead to low CD4 count and non-AIDS-defining cancers. Higher rates of non-AIDS mortality among individuals with incomplete CD4 recovery may be related to chronic immune activation in virally suppressed individuals [28, 29].
Implications and Conclusions
Our data underline the importance of early diagnosis of HIV and treatment with cART before patients have a low CD4 count. Although we have identified risk factors for poor CD4 recovery, no interventions to increase CD4 count in virally suppressed patients have been demonstrated to have beneficial effects on clinical endpoints and mortality. Previous studies have not consistently demonstrated differences between antiretroviral drug classes in effects on CD4 increases, and attempts to increase CD4 count with interleukin 2 were futile in terms of clinical benefit [30–32]. Virally suppressed patients with low CD4 counts should be monitored closely for diseases not conventionally considered to be HIV related, especially non-AIDS-defining cancers and liver diseases. Our study demonstrated an increased risk of non-AIDS causes of death in immunological nonresponders; further research is needed to elucidate the mechanisms that lead to persistently low CD4 counts despite viral suppression.
Supplementary Material
Notes
Members of ART-CC and COHERE:
Analysis and Writing Committee: Frederik N. Engsig (Danish HIV Cohort), Robert Zangerle (AHIVCOS), Olga Katsarou (AMACS), Francois Dabis (AQUITAINE), Peter Reiss (ATHENA), John Gill (Alberta HIV clinic), Kholoud Porter (CASCADE), Caroline Sabin (CHIC), Andrew Riordan (CHIPS), Gerd Fätkenheuer (Cologne Bonn), Félix Gutiérrez (CoRIS), Francois Raffi (COPILOTE), Ole Kirk (EuroSIDA), Murielle Mary-Krause (FHDH-ANRS CO4), Christoph Stephan (Frankfurt Cohort), Patricia Garcia de Olalla (GEMES), Jodie Guest (HAVACS), Hasina Samji (HOMER), Antonella Castagna (HSR), Antonella d'Arminio Monforte (ICONA), Adriane Skaletz-Rorowski (KompNet), Jose Ramos (Madrid HIV Cohort), Giuseppe Lapadula (MASTER Cohort), Cristina Mussini (MODENA), Lluís Force (PISCIS), Laurence Meyer (PRIMO), Fiona Lampe (Royal Free), Faroudy Boufassa (SEROCO), Heiner C. Bucher (SHCS), Stéphane De Wit (St. Pierre Cohort), Greer Burkholder (UAB), Ramon Teira (VACH), Amy Justice (VACS), Tim R Sterling (Vanderbilt), Heidi M. Crane (UW), Jan Gerstoft (Danish HIV Cohort), Jesper Grarup (COHERE), Margaret May (ART-CC), Geneviève Chêne (COHERE), Suzanne M. Ingle (ART-CC), Jonathan Sterne (ART-CC) and Niels Obel (Danish HIV Cohort).
The ART-CC Steering Committee: Andrew Boulle (IeDEA Southern Africa), Hans-Reinhard Brodt (Frankfurt), Jordi Casabona (PISCIS), Matthias Cavassini (SHCS), Geneviève Chêne (Aquitaine), Dominique Costagliola (FHDH), François Dabis (Aquitaine), Antonella D'Arminio Monforte (ICONA), Julia del Amo (CoRIS-MD), Ard Van Sighem (ATHENA), Gerd Fätkenheuer (Koln/Bonn), John Gill (Alberta HIV clinic), Jodie Guest (HAVACS), David Hans-Ulrich Haerry (EATG), Robert Hogg (HOMER), Amy Justice (VACS), Amanda Mocroft (EuroSIDA), Niels Obel (Danish HIV Cohort), Mari Kitahata (Washington), Fiona Lampe (Royal Free), Peter Reiss (ATHENA), Michael Saag (Alabama), Tim R. Sterling (Vanderbilt-Meherry), Ramon Teira (VACH), Matthew Williams (UK-CAB), Robert Zangerle (AHIVCOS); ART-CC Coordinating Centre, Bristol University: Suzanne Ingle, Margaret May, Jonathan Sterne.
COHERE Steering Committee: Contributing cohorts: Robert Zangerle (AHIVCOS), Giota Touloumi (AMACS), Josiane Warszawski (ANRS CO1 EPF/ANRS CO11 OBSERVATOIRE EPF), Laurence Meyer (ANRS CO2 SEROCO), François Dabis (ANRS CO3 AQUITAINE), Murielle Mary Krause (ANRS CO4 FHDH), Jade Ghosn (ANRS CO6 PRIMO), Catherine Leport (ANRS CO8 COPILOTE), Peter Reiss (ATHENA), Ferdinand Wit (ATHENA), Maria Prins (CASCADE), Heiner C. Bucher (CASCADE), Caroline Sabin (CHIC), Diana Gibb (CHIPS), Gerd Fätkenheuer (Cologne Bonn), Julia Del Amo (CoRIS), Niels Obel (Danish HIV Cohort), Claire Thorne (ECS), Amanda Mocroft (EuroSIDA), Ole Kirk (EuroSIDA), Christoph Stephan (Frankfurt), Santiago Pérez-Hoyos (GEMES-Haemo), Osamah Hamouda (German ClinSurv), Barbara Gussenheimer-Bartmeyer (German ClinSurv), Antoni Noguera-Julian (NENEXP and CORISPE-cat), Andrea Antinori (ICC), Antonella d'Arminio Monforte (ICONA), Norbert Brockmeyer (KOMPNET), José Ramos (Madrid Cohort), Manuel Battegay (MoCHIV and SHCS), Andri Rauch (SHCS), Cristina Mussini (Modena Cohort), Pat Tookey (NSHPC), Jordi Casabona (PISCIS), Jose M. Miró (PISCIS), Antonella Castagna (San Raffaele), Stephane de Wit (St Pierre Cohort), Tessa Goetghebuer (St Pierre Paediatric Cohort), Carlo Torti (Italian Master Cohort), Ramon Teira (VACH), Myriam Garrido (VACH). Paediatric cohort representatives: Ali Judd, Pablo Rojo Conejo. European AIDS Treatment Group: David Haerry.
COHERE Executive Committee: Ian Weller (Chair, COHERE), Jordi Casabona (PISCIS), Dominique Costagliola (FHDH), Antonella d'Arminio-Monforte (ICONA), Manuel Battegay (MoCHIV and SHCS), Stephane de Wit (St Pierre Cohort), Julia Del Amo (CoRIS), Jesper Grarup (Head, Copenhagen Regional Coordinating Centre), Geneviève Chêne (Head, Bordeaux Regional Coordinating Centre).
COHERE Regional Coordinating Centres: Bordeaux: Céline Colin, Christine Schwimmer, Monique Termote, Diana Barger; Copenhagen: Jesper Kjaer, Maria Campbell, Dorthe Raben.
Project Leaders and Statistical Analysis: Manuel Battegay, Julia Bohlius, Vincent Bouteloup, Heiner Bucher, Alessandro Cozzi-Lepri, François Dabis, Antonella d'Arminio Monforte, Julia del Amo, Maria Dorrucci, Matthias Egger, Frederik Engsig, Hansjakob Furrer, Ali Judd, Ole Kirk, Olivier Lambotte, Charlotte Lewden, Sara Lodi, Rebbeca Lodwick, Sophie Matheron, Laurence Meyer, Jose Miro, Amanda Mocroft, Susana Monge, Fumiyo Nakagawa, Niels Obel, Roger Paredes, Andrew Phillips, Massimo Puoti, Joanne Reekie, Caroline Sabin, Alexandra Scherrer, Colette Smit, Jonathan Sterne, Rodolphe Thiebaut, Claire Thorne, Carlo Torti, Giota Touloumi, Linda Wittkop.
Disclaimer. The funders had no role in the study design; in the collection, management, analysis, and interpretation of data; in the preparation, review, or approval of the manuscript; or in the decision to submit the article for publication.
Financial support. This work was supported by the European Union Seventh Framework Programme (FP7/2007–2013) under EuroCoord grant agreement number 260694. The COHERE study group has received unrestricted funding from Agence Nationale de Recherches sur le SIDA et les Hépatites Virales, France; HIV Monitoring Foundation, the Netherlands; and the Augustinus Foundation, Denmark. The EuroCoord acknowledgment appendix may be found at http://www.cphiv.dk/COHERE/StudyDocuments/tabid/298/Default.aspx. A list of the funders of the participating cohorts can be found on the COHERE website at http://www.cohere.org. The ART Cohort Collaboration was funded by the UK Medical Research Council (grant numbers G0700820 and MR/J002380/1).
Potential conflicts of interest. N. O. has received research funding from Roche, Bristol-Myers Squibb (BMS), Merck Sharp & Dohme (MSD), GlaxoSmithKline (GSK), Abbott, Boehringer Ingelheim, Janssen-Cilag, and Swedish Orphan. F. N. E. has received research funding from MSD. J. Ge. has received research funding from Abbott, Roche, BMS, MSD, Pharmasia, GSK, Swedish Orphan, and Boehringer Ingelheim. H. C. B. has received travel grants, honoraria, and unrestricted research grants from various pharmaceutical companies including GSK, BMS, Gilead, Janssen, Roche, Abbott, Tibotec, Boehringer-Ingelheim, and ViiV Healtcare, and is supported by grants from Santésuisse and the Gottfried and Julia-Bangerter-Rhyner-Foundation. F. G. has received research funding from Abbott, Boehringer-Ingelheim, BMS, Gilead Sciences, GSK, Janssen-Cilag, MSD, Pfizer, and ViiV Healthcare. G. C. has received consulting fees (Scientific Committee) from the French Agency for Research on AIDS and Viral Hepatitis, the European Commission (Framework Program 7), UK Medical Research Council, US National Institutes of Health, Fondation Plan Alzheimer, Gilead, Tibotec, Boehringer Ingelheim, GSK, Roche, Pfizer, Merck, Abbott, BMS, Janssen, and ViiV Healthcare. L. F. has received honoraria for advisory boards, a fee for speaking, and a fee for organizing education from various pharmaceutical companies including Abbott, BMS, Boehringer Ingelheim, Gilead Sciences, GSK, Merck, and Janssen-Cilag. T. R. S. has received research grants from Pfizer, BMS, and Virco to conduct HIV observational studies. C. Sa. has received funding for advisory board membership, speakers’ panels, and provision of educational materials from Gilead Sciences, Abbott Pharmaceuticals, MSD, Janssen-Cilag, and BMS. O. K. has had prior board membership with Viiv; has received payment for lectures and/or for development of educational presentations from Abbott, Gilead, and Tibotec/Janssen; and had expenses to travel/accommodations/meetings covered by Abbott, BMS, Gilead, Merck, and ViiV. J. S. has received payments for educational materials from Gilead Sciences. J. Gi. has received support for advisory board membership from ViiV, Gilead, Abbott, Merck, and Janssen. All other authors report no potential conflicts.
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1.Lohse N, Hansen AB, Pedersen G, et al. Survival of persons with and without HIV infection in Denmark, 1995–2005. Ann Intern Med. 2007;146:87–95. doi: 10.7326/0003-4819-146-2-200701160-00003. [DOI] [PubMed] [Google Scholar]
- 2.El-Sadr WM, Lundgren JD, Neaton JD, et al. CD4+ count-guided interruption of antiretroviral treatment. N Engl J Med. 2006;355:2283–96. doi: 10.1056/NEJMoa062360. [DOI] [PubMed] [Google Scholar]
- 3.The CASCADE Collaboration. Survival after introduction of HAART in people with known duration of HIV-1 infection. Concerted Action on SeroConversion to AIDS and Death in Europe. Lancet. 2000;355:1158–9. [PubMed] [Google Scholar]
- 4.Moore RD, Keruly JC. CD4+ cell count 6 years after commencement of highly active antiretroviral therapy in persons with sustained virologic suppression. Clin Infect Dis. 2007;44:441–6. doi: 10.1086/510746. [DOI] [PubMed] [Google Scholar]
- 5.Baker JV, Peng G, Rapkin J, et al. Poor initial CD4+ recovery with antiretroviral therapy prolongs immune depletion and increases risk for AIDS and non-AIDS diseases. J Acquir Immune Defic Syndr. 2008;48:541–6. doi: 10.1097/QAI.0b013e31817bebb3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hughes RA, Sterne JA, Walsh J, et al. Long-term trends in CD4 cell counts and impact of viral failure in individuals starting antiretroviral therapy: UK Collaborative HIV Cohort (CHIC) study. HIV Med. 2011;12:583–93. doi: 10.1111/j.1468-1293.2011.00929.x. [DOI] [PubMed] [Google Scholar]
- 7.Grabar S, Le MV, Goujard C, et al. Clinical outcome of patients with HIV-1 infection according to immunologic and virologic response after 6 months of highly active antiretroviral therapy. Ann Intern Med. 2000;133:401–10. doi: 10.7326/0003-4819-133-6-200009190-00007. [DOI] [PubMed] [Google Scholar]
- 8.Engsig FN, Gerstoft J, Kronborg G, et al. Long-term mortality in HIV patients virally suppressed for more than three years with incomplete CD4 recovery: a cohort study. BMC Infect Dis. 2010;10:318. doi: 10.1186/1471-2334-10-318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Young J, Psichogiou M, Meyer L, et al. CD4 cell count and the risk of AIDS or death in HIV-Infected adults on combination antiretroviral therapy with a suppressed viral load: a longitudinal cohort study from COHERE. PLoS Med. 2012;9:e1001194. doi: 10.1371/journal.pmed.1001194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Egger M, May M, Chene G, et al. Prognosis of HIV-1-infected patients starting highly active antiretroviral therapy: a collaborative analysis of prospective studies. Lancet. 2002;360:119–29. doi: 10.1016/s0140-6736(02)09411-4. [DOI] [PubMed] [Google Scholar]
- 11.de Wolf F, Sabin C, Kirk O, Thorne C, Chene G, Porter K. Developing a multidisciplinary network for clinical research on HIV infection: the EuroCoord experience. Clin Invest. 2012;2:255–64. [Google Scholar]
- 12.Gill J, May M, Lewden C, et al. Causes of death in HIV-1-infected patients treated with antiretroviral therapy, 1996–2006: collaborative analysis of 13 HIV cohort studies. Clin Infect Dis. 2010;50:1387–96. doi: 10.1086/652283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999;94:496–509. [Google Scholar]
- 14.Rubin D. Inference and missing data. Biometrika. 1976;63:581–92. [Google Scholar]
- 15.National Institutes of Health. Guidelines for the use of antiretroviral agents in HIV-1-infected adults and adolescents. 2013. Available at: http://aidsinfo.nih.gov/guidelines . Accessed 28 October 2013.
- 16.Chene G, Sterne JA, May M, et al. Prognostic importance of initial response in HIV-1 infected patients starting potent antiretroviral therapy: analysis of prospective studies. Lancet. 2003;362:679–86. doi: 10.1016/s0140-6736(03)14229-8. [DOI] [PubMed] [Google Scholar]
- 17.Lanoy E, May M, Mocroft A, et al. Prognosis of patients treated with cART from 36 months after initiation, according to current and previous CD4 cell count and plasma HIV-1 RNA measurements. AIDS. 2009;23:2199–208. doi: 10.1097/QAD.0b013e3283305a00. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kaufmann GR, Bloch M, Finlayson R, Zaunders J, Smith D, Cooper DA. The extent of HIV-1-related immunodeficiency and age predict the long-term CD4T lymphocyte response to potent antiretroviral therapy. AIDS. 2002;16:359–67. doi: 10.1097/00002030-200202150-00007. [DOI] [PubMed] [Google Scholar]
- 19.Hunt PW, Deeks SG, Rodriguez B, et al. Continued CD4 cell count increases in HIV-infected adults experiencing 4 years of viral suppression on antiretroviral therapy. AIDS. 2003;17:1907–15. doi: 10.1097/00002030-200309050-00009. [DOI] [PubMed] [Google Scholar]
- 20.Florence E, Lundgren J, Dreezen C, et al. Factors associated with a reduced CD4 lymphocyte count response to HAART despite full viral suppression in the EuroSIDA study. HIV Med. 2003;4:255–62. doi: 10.1046/j.1468-1293.2003.00156.x. [DOI] [PubMed] [Google Scholar]
- 21.Dion ML, Bordi R, Zeidan J, et al. Slow disease progression and robust therapy-mediated CD4+ T-cell recovery are associated with efficient thymopoiesis during HIV-1 infection. Blood. 2007;109:2912–20. doi: 10.1182/blood-2006-09-047308. [DOI] [PubMed] [Google Scholar]
- 22.Yamashita TE, Phair JP, Munoz A, et al. Immunologic and virologic response to highly active antiretroviral therapy in the Multicenter AIDS Cohort Study. AIDS. 2001;15:735–46. doi: 10.1097/00002030-200104130-00009. [DOI] [PubMed] [Google Scholar]
- 23.Khoury G, Rajasuriar R, Cameron PU, Lewin SR. The role of naive T-cells in HIV-1 pathogenesis: an emerging key player. Clin Immunol. 2011;141:253–67. doi: 10.1016/j.clim.2011.09.002. [DOI] [PubMed] [Google Scholar]
- 24.Loutfy MR, Genebat M, Moore D, et al. A CD4+ cell count <200 cells per cubic millimeter at 2 years after initiation of combination antiretroviral therapy is associated with increased mortality in HIV-infected individuals with viral suppression. J Acquir Immune Defic Syndr. 2010;55:451–9. doi: 10.1097/qai.0b013e3181ec28ff. [DOI] [PubMed] [Google Scholar]
- 25.Guiguet M, Boue F, Cadranel J, Lang JM, Rosenthal E, Costagliola D. Effect of immunodeficiency, HIV viral load, and antiretroviral therapy on the risk of individual malignancies (FHDH-ANRS CO4): a prospective cohort study. Lancet Oncol. 2009;10:1152–9. doi: 10.1016/S1470-2045(09)70282-7. [DOI] [PubMed] [Google Scholar]
- 26.Monforte A, Abrams D, Pradier C, et al. HIV-induced immunodeficiency and mortality from AIDS-defining and non-AIDS-defining malignancies. AIDS. 2008;22:2143–53. doi: 10.1097/QAD.0b013e3283112b77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Reekie J, Kosa C, Engsig F, et al. Relationship between current level of immunodeficiency and non-acquired immunodeficiency syndrome-defining malignancies. Cancer. 2010;116:5306–15. doi: 10.1002/cncr.25311. [DOI] [PubMed] [Google Scholar]
- 28.Gascon RL, Narvaez AB, Zhang R, et al. Increased HLA-DR expression on peripheral blood monocytes in subsets of subjects with primary HIV infection is associated with elevated CD4 T-cell apoptosis and CD4 T-cell depletion. J Acquir Immune Defic Syndr. 2002;30:146–53. doi: 10.1097/00042560-200206010-00002. [DOI] [PubMed] [Google Scholar]
- 29.Kuller LH, Tracy R, Belloso W, et al. Inflammatory and coagulation biomarkers and mortality in patients with HIV infection. PLoS Med. 2008;5:e203. doi: 10.1371/journal.pmed.0050203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Riddler SA, Haubrich R, DiRienzo AG, et al. Class-sparing regimens for initial treatment of HIV-1 infection. N Engl J Med. 2008;358:2095–106. doi: 10.1056/NEJMoa074609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Abrams D, Levy Y, Losso MH, et al. Interleukin-2 therapy in patients with HIV infection. N Engl J Med. 2009;361:1548–59. doi: 10.1056/NEJMoa0903175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Khanna N, Opravil M, Furrer H, et al. CD4+ T cell count recovery in HIV type 1-infected patients is independent of class of antiretroviral therapy. Clin Infect Dis. 2008;47:1093–101. doi: 10.1086/592113. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.