Abstract
Background
Little is known about the distribution of activity over the full 24-hour spectrum in late old age and its association with demographic and health factors. Therefore, we aimed to evaluate the distribution of physical activity (PA), sedentary behavior and sleep and associated factors in the elderly population.
Methods
Our study included 1210 participants (51.9% women) aged 70-94 years (mean age 77.5 years, standard deviation (SD): 5.0) from the population-based Rotterdam Study. Participants wore a triaxial accelerometer (GeneActiv) around the wrist for seven days, between July 2014 and June 2016. We examined if PA, sedentary behavior and sleep differed by age, sex, body mass index (BMI), smoking status, alcohol consumption, education, season, functional capacity, marital status, presence of chronic disease and use of sleep medication.
Results
Mean total PA, expressed in milli-gravity (mg) units, was slightly higher for women (20.3, SD:5.6) than for men (19.3, SD: 5.2, p<.01). Mean (SD) daily duration spent in sedentary behavior and light and moderate-to-vigorous PA was 13.3 (1.5) hours/d, 147.5 (31.5) minutes/d and 75.0 (25.5) minutes/d, respectively, among women; and 13.8 (1.6) hours/d, 140.5 (31.1) minutes/d and 71.5 (24.5) minutes/d, respectively, among men. Women spent on average 6.7 (SD: 1.1) hours/d sleeping and men 6.6 (1.4) hours/d. Across increasing categories of age and BMI and in participants with chronic disease and disability, time spent in light and moderate-to-vigorous PA was decreased. Sedentary time increased across higher strata of BMI and age. Additionally, obese men spent slightly more time sleeping than their normal weight counterparts and women spent slightly less time sleeping in the summer than in spring.
Conclusions
PA and sedentary behavior in the elderly differed by sex, age, BMI, prevalence of chronic disease and disability, whereas there were no clear patterns for sleep. On average, our participants spent up to 79.5% of their time awake being sedentary and 7-8% in moderate-to-vigorous PA. Replacing sedentary behavior with light PA would be a good starting point for those with the lowest level of PA. Older adults, those with high BMI and worse health could benefit from targeted interventions to increase PA.
Keywords: physical activity, accelerometer, elderly, Rotterdam Study
Introduction
Physical activity (PA) plays a major role in healthy aging, by preventing disease, reducing disability and improving well-being.1–3 Given the importance of PA in older adulthood, understanding the levels of PA in elderly adults might provide information for public health institutions to create targeted recommendations. In epidemiological studies, PA is usually assessed by questionnaires.4 However, these data are known to be prone to reporting errors and recall bias, especially for low intensity behaviors.5,6 These limitations may be exacerbated in older populations, in whom cognitive impairment is more likely.7 Therefore, accelerometers are increasingly used to measure PA and sedentary behavior objectively.8
To date, several studies objectively assessed PA and sedentary behavior using accelerometers in adults aged 60 years and over9–19 and examined the associations with demographic and health factors. It has been shown that PA levels decrease with increasing age9–13,16,19 and across increasing levels of BMI.9–12,14 Whereas these studies provided useful information, the associations were often obtained from unadjusted analyses. Moreover, there is limited information on the 24-hour activity spectrum in the elderly, including PA, sedentary behavior and sleep. It remains unknown how these factors are interrelated and how they are distributed across age-groups and other demographic and health factors. In previous studies, accelerometers have most often been worn on the hip and had to be removed for sleeping. Wrist-worn devices can be worn day and night, thereby allowing for collection of 24-hour of activity data, recently shown to be valid indicators of activity energy expenditure.20,21 Additionally, wrist-worn devices have been argued to promote better compliance of device wear.22
The Rotterdam Study is one of the first large population studies to objectively assess PA in an elderly population of adults aged 70-94 years using a triaxial accelerometer. The main aim of this study was to provide a description of objectively measured activity in elderly adults from the Rotterdam Study, over the complete 24-hour period. Additionally, we examined the demographic and health factors associated with activity measures in this cohort.
Methods
Study population
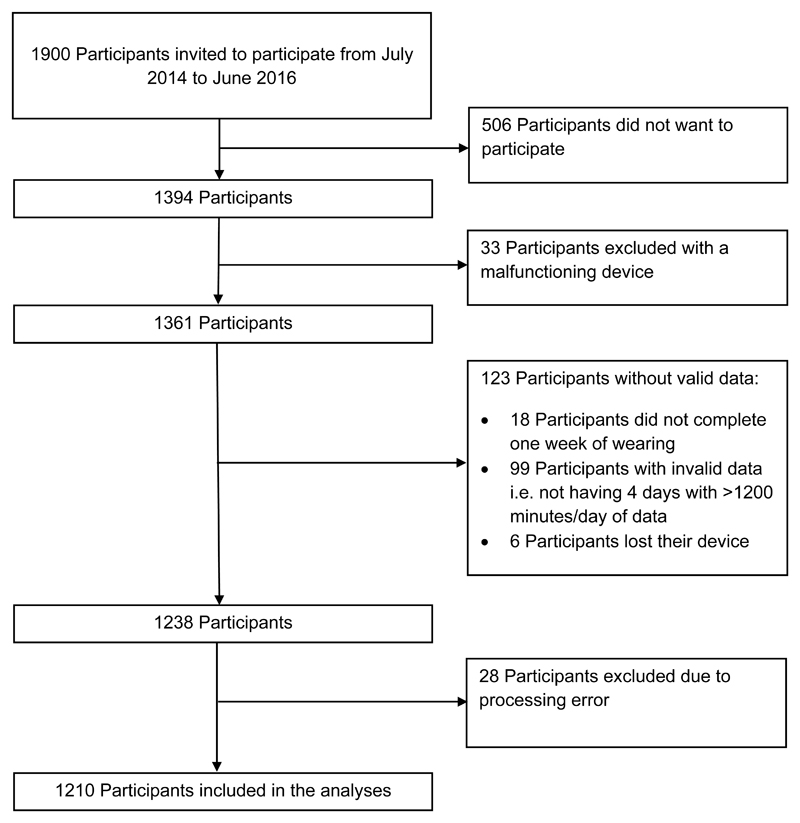
This study was embedded in the Rotterdam Study, a prospective population-based cohort in the Netherlands. The main aim of this study was to examine the incidence of risk factors for neurological, cardiovascular, psychiatric, and other chronic diseases. Details of the study have been published previously.23 For the current study, 1900 successive participants of the Rotterdam Study were invited to participate, from July 2014 to May 2016, of which 506 did not consent. For 1210 participants valid data (>1200 min/day) on at least 4 days was available (See Figure 1).
Figure 1.
Flow chart of participant inclusion for the Rotterdam Study.
All subjects gave written informed consent, and the study protocol was approved by the medical ethics committee of Erasmus University, Rotterdam. Detailed information on the design of the Rotterdam Study can be found elsewhere.23
Accelerometer-assessed physical activity
All participants were asked to wear a triaxial accelerometer (GeneActiv; Activinsights Ltd, Kimbolton, Cambridgeshire, UK, http://www.geneactiv.org/) on the non-dominant wrist for 7 consecutive days and nights and to complete a 7-day sleep diary to report overnight sleep periods. The accelerometer sampled at 50 Hz and as in previous studies18,24,25 acceleration was expressed relative to gravity (g units; 1 g =9.81 m/s2 at this location in the Netherlands26), since the sensors are calibrated relative to gravity. Calibration error was estimated based on static periods in the data and corrected if necessary.27
We used two vector magnitude-based measures to quantify the acceleration related to the movement registered. The first was the Euclidean norm minus 1 g with negative numbers rounded to zero (ENMO).21 In addition, we calculated the high-pass filtered vector magnitude (HPFVM), which applies a high-pass filter to the acceleration signal with a cut-off frequency of 0.2 Hertz, treating gravity as a low-frequency component to be filtered out.20
Accelerometer data were processed in Python (2.6.6) using the open access PAMPRO software. Pampro is a software program for the systematic analysis of physical activity data collected in epidemiological studies.28 Data was extracted from the first wearing day up to seven days later.
Non-wear time was estimated as time periods where the standard deviation of acceleration in all three axes fell below 13mg for longer than 1 hour,20 and any non-wear period was excluded from analyses. The pattern of non-wear time was accounted for by balancing the weighting of the data according to the diurnal profile.29
Assessment of factors
Information on health behaviors was collected through home interviews or measured at the study center, as described previously.30,31 Alcohol use was defined as the number of times drinking alcohol per time unit (i.e. never drinking alcohol; drinking 1-4 per month; drinking 2-4 per week). Education was assessed in line with the International Standard Classification of Education and categorized as primary, lower, intermediate and higher education.32 Smoking was divided in three categories: current, former and never. Height and weight were measured to calculate body mass index (BMI) (kg/m2) and categorised as normal weight (<25 kg/m2), overweight (25–30 kg/m2) and obese (>30 kg/m2). Marital status was defined as living with a partner or not. Functional capacity was assessed by the Activities of Daily Living from the Stanford Health Assessment Questionnaire Disability Index (HAQ-DI).33 In accordance with literature we used a HAQ-DI 0.5 ≥1.0 to define a participant as disabled and a HAQ-DI ≥ 1.0 to define a participant as severely disabled.34 Use of sleep medication was obtained from the sleep diary, and used as a binary variable (not in the past 7 days/at least one day in the past 7 days). The presence of cardiovascular disease (CVD), diabetes mellitus (DM) and cancer were determined using medical records, to define presence of chronic disease. The LASA Physical Activity Questionnaire (LAPAQ) was used to determine total self-reported PA and was expressed in MET·hours·week-1. The questionnaire included questions on walking, cycling, housekeeping, sports and gardening. Finally, using the first wearing date of the GeneActiv, we classified the season according to the light definition, centered at equinoxes (winter: November 6 to February 4, spring: February 5 to May 6, summer: May 7 to August 5 and autumn: August 6 to November 5.35
Data analysis
Descriptive statistics for continuous PA variables are presented as mean and standard deviation (SD) or median and interquartile range (IQR) if data were not normally distributed. We created 9 intervals, to visually evaluate the distribution of time spent in overall PA, and how it varied by gender and age-group. Additionally, we categorized activity based on HPFVM in sedentary (<48 mg), light (48 < 154 mg), moderate (154 <389 mg) and vigorous activity (>389 mg), based on a recent study.20 For the current study, we combined moderate and vigorous activity in our main analyses. Sleep duration was assessed with a validated algorithm,36 using information on bed time and awake time from the sleep diary, and was subtracted from total sedentary behavior.
To describe our data and test differences in average time per day spent in sedentary behavior, light PA, moderate-to-vigorous PA and sleep across two categories or across three or more categories of the health-related and socio-demographic variables, we used t-tests and Analyses of variance (ANOVA), respectively. We further examined the robustness of the individual associations by mutually adjusting for all demographic and health factors in linear regression analyses. All determinants were entered as categorical variables and the activity variables were the outcome variables in these analyses. To evaluate the explained variance by the determinants, we obtained the adjusted R-squared. We decided a priori to present the results stratified by sex for comparability with previous and future studies. The average time/d in each activity level was plotted as a portion of the 1440 minutes of the day to graphically inspect the distribution of activity levels across age-groups and BMI-groups. The average time across BMI-groups was adjusted for age.
In sensitivity analyses, we tested whether the health-related and socio-demographic characteristics differed between men and women, to be able to explain any gender differences. We also tested whether those participating differed from those not agreeing to participate, in regard to baseline characteristics. Furthermore, we repeated the linear regression analyses stratified by age (older or younger than 80 years), to examine if the associations in the oldest old (i.e. 80 years or older) were different than in those younger than 80 years. We also repeated the linear regression analyses stratified by a BMI of 27 kg/m2, the median level in the population.
Analyses were conducted using SPSS software version 20 (IBM SPSS Statistics for Windows, Armonk, NY: IBM Corp), R version 3.2.1 (R Foundation for Statistical Computing, Vienna, Austria) and Stata version 14.1 SE (StataCorp LP, College Station, Texas).37 A double-sided p < 0.05 was considered statistically significant.
Results
Participants who agreed to participate in the study were more often men and less often disabled than those who did not agree to wear an accelerometer (Supplementary Table 1). In the total sample of 1200 participants, a total of 71,232 valid days were recorded, in accordance with an average of 5.9 (SD: 0.4) days per participant. The proportion of males in the sample was 48.1% and the mean age was 77.5 (SD: 5.0). The median (IQR) accelerometer wear-time was slightly higher in men registering 154.2 hours (152.6, 156.4) than in women registering 153.6 hours (151.6, 156.0), p <0.001. Furthermore, participating women were more often obese or disabled than men, whereas men more often had prevalent chronic disease (Supplementary Table 2). The proportion of participants who reported engaging in walking, cycling, housework, gardening and sports in the LAPAQ is shown in Supplementary Figure 1. Men participated significantly more in cycling and gardening than women (p<0.05).
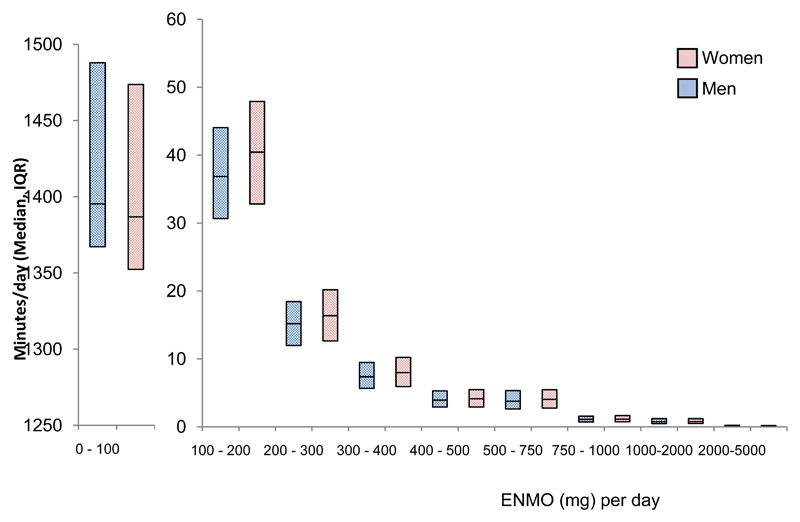
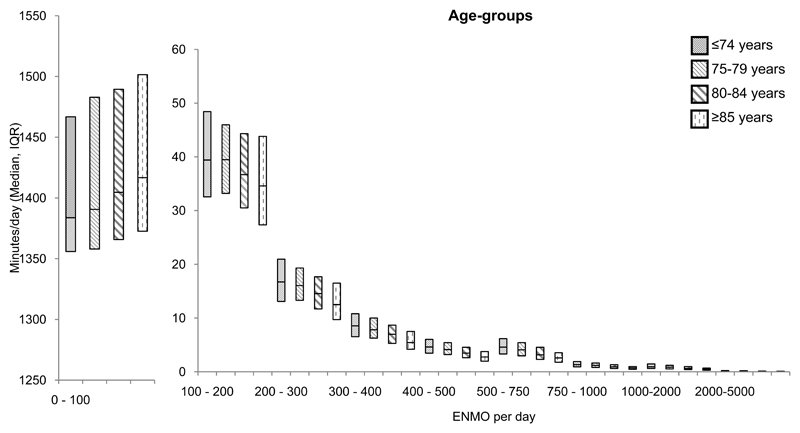
Total PA, expressed in mg, was slightly higher for women (20.3, SD:5.5) than for men (19.3, SD: 5.2, p=0.002). Figure 2 and Figure 3 show the acceleration distribution of time spent in 9 systematic intervals (including time spent sleeping), stratified by sex and age category, respectively. Women spent less time in the interval with the lowest acceleration (0-100 mg), and spent more time in each other interval than men. For the age-categories, the oldest age-group (≥ 85 years) spent the most time in the lowest interval (0-100 mg) and spent less time in each other interval.
Figure 2.
Activity distribution of time spent in acceleration (mg) categories (intensity) stratified by sex.
Abbreviations: ENMO, The Euclidean norm minus 1 g with negative numbers rounded to zero; IQR, interquartile range.
Figure 3.
Activity distribution of time spent in acceleration (mg) categories (intensity) stratified by age-group.
Abbreviations: ENMO, The Euclidean norm minus 1 g with negative numbers rounded to zero; IQR, interquartile range.
Mean (SD) time per day spent in sedentary behavior and light and moderate-to-vigorous intensity PA was 13.3 (1.5) hours/d, 147.5 (31.5) minutes/d and 75.0 (25.5) minutes/d, respectively, among women (Table 1); and 13.8 (1.6) hours/d, 140.5 (31.1) minutes/d and 71.5 (24.5) minutes/d, respectively, among men (Table 2). Time spent in moderate and vigorous PA separately and in total sedentary behavior (including sleep) is presented in Supplementary Table 3 (women) and Supplementary Table 4 (men). Women spent 6.7 hours/d (SD: 1.4) sleeping and men (6.6 hours/d, SD: 1.4), p = 0.12. Men spent significant more minutes in sedentary behavior (p<0.001) and less time in light (p<0.001) and moderate PA (p<0.004). The time spent in vigorous PA did not differ significantly between men and women. The percentage of awake time spent sedentary was 79.5% for men and 78.2% for women (Supplementary Table 5-6) and 6.9% and 7.4% of the waking time was spent in moderate-to-vigorous PA in men and women, respectively.
Table 1. Objectively assessed physical activity subcomponents and sedentary time in women (n=628), according to characteristics of the study population.
| n | Acceleration (mg/day) | Sedentary time (h/day) | Light PA (min/day) | Moderate-vigorous PA (min/day) | Sleep time (accelerometer) (h/day) | |
|---|---|---|---|---|---|---|
| Total | 628 | 20.3 (5.6) | 13.3 (1.5) | 147.5 (31.5) | 75 (25.5) | 6.7 (1.4) |
| Age-group | ||||||
| 70-74 | 200 | 22.3 (6.2) | 13.3 (1.4) | 153.5 (30.7) | 85.2 (27.0) | 6.6 (1.2) |
| 75-79 | 226 | 20.2 (5.1) | 13.2 (1.6) | 147.7 (31.2) | 75.0 (23.3) | 6.8 (1.4) |
| 80-84 | 130 | 18.9 (4.5) | 13.4 (1.4) | 144.5 (30.4) | 67.7 (21.0) | 6.8 (1.4) |
| ≥85 | 72 | 17.5 (4.9) | 13.6 (1.6) | 135.7 (33.1) | 59.7 (23.6) | 6.9 (1.5) |
| p | <0.001 | 0.33 | <0.001 | <0.001 | 0.19 | |
| Education | ||||||
| Primary education | 41 | 18.1 (5.3) | 13.7 (1.8) | 135.2 (31.9) | 64.8 (25.9) | 6.7 (1.6) |
| Lower education | 337 | 20.1 (5.1) | 13.3 (1.4) | 147.0 (30.7) | 74.5 (23.9) | 6.8 (1.3) |
| Intermediate education | 163 | 20.3 (5.9) | 13.4 (1.5) | 146.0 (30.5) | 74.3 (26.1) | 6.7 (1.3) |
| Higher education | 75 | 21.5 (6.0) | 13.3 (1.5) | 157.1 (33.8) | 82.2 (27.2) | 6.5 (1.4) |
| p | 0.02 | 0.31 | 0.003 | 0.004 | 0.47 | |
| Season | ||||||
| Spring | 163 | 20.2 (5.2) | 13.2 (1.6) | 146.7 (31.3) | 75.0 (24.7) | 6.9 (1.4) |
| Summer | 74 | 21.3 (6.5) | 13.4 (1.6) | 148.1 (30.9) | 78.0 (27.5) | 6.6 (1.5) |
| Autumn | 206 | 19.9 (5.9) | 13.3 (1.4) | 145.5 (32.6) | 73.0 (27.1) | 6.7 (1.3) |
| Winter | 182 | 20.3 (5.0) | 13.4 (1.4) | 149.4 (30.5) | 75.4 (23.3) | 6.6 (1.3) |
| p | 0.38 | 0.56 | 0.67 | 0.52 | 0.44 | |
| BMI | ||||||
| Normal weight | 183 | 22.4 (5.9) | 12.8 (1.3) | 157.9 (29.9) | 84.0 (25.7) | 6.9 (1.3) |
| Overweight | 265 | 20.3 (5.4) | 13.3 (1.5) | 148.2 (30.7) | 75.2 (25.4) | 6.7 (1.4) |
| Obese | 179 | 18.2 (4.6) | 13.9 (1.5) | 136.1 (30.3) | 65.7 (21.7) | 6.6 (1.4) |
| p | <0.001 | <0.001 | <0.001 | <0.001 | 0.10 | |
| Smoking | ||||||
| Non smoker | 282 | 20.7 (5.6) | 13.1 (1.4) | 150.8 (31.3) | 76.7 (25.5) | 6.8 (1.4) |
| Former smoker | 310 | 20.1 (5.5) | 13.5 (1.4) | 145.4 (31.4) | 74.0 (25.4) | 6.6 (1.3) |
| Current smoker | 36 | 19.0 (5.5) | 13.6 (2.0) | 139.3 (32.1) | 70.1 (25.9) | 6.7 (1.7) |
| p | 0.14 | 0.01 | 0.03 | 0.22 | 0.15 | |
| Alcohol consumption | ||||||
| Never drinks alcohol | 123 | 19.7 (4.7) | 13.3 (1.5) | 145.2 (30.3) | 72.1 (22.9) | 6.8 (1.4) |
| Drinks 1-4 times per month | 217 | 19.5 (5.2) | 13.4 (1.4) | 142.5 (31.7) | 71.5 (24.5) | 6.8 (1.4) |
| Drinks 2-4 times per week | 288 | 21.2 (6.0) | 13.3 (1.6) | 152.2 (31.4) | 78.8 (26.8) | 6.6 (1.3) |
| p | 0.001 | 0.83 | 0.002 | 0.002 | 0.27 | |
| Functional capacity | ||||||
| Not disabled | 243 | 21.5 (5.4) | 13.2 (1.3) | 152.0 (30.3) | 81.1 (25.5) | 6.7 (1.3) |
| Disabled | 139 | 20.8 (5.7) | 13.1 (1.6) | 150.6 (29.2) | 77.0 (24.5) | 6.9 (1.5) |
| Severely disabled | 245 | 18.9 (5.4) | 13.6 (1.5) | 141.2 (33.1) | 67.8 (24.4) | 6.7 (1.3) |
| p | <0.001 | 0.003 | <0.001 | <0.001 | 0.40 | |
| Prevalent CVD, DM or cancer | ||||||
| Not present | 336 | 21.3 (5.7) | 13.1 (1.4) | 151.4 (30.7) | 79.3 (25.7) | 6.8 (1.3) |
| Present | 292 | 19.1 (5.1) | 13.5 (1.5) | 143.0 (31.9) | 70.0 (24.3) | 6.7 (1.4) |
| p | <0.001 | 0.001 | 0.001 | <0.001 | 0.42 | |
| Marital status | ||||||
| Living alone | 309 | 19.2 (5.4) | 13.5 (1.6) | 141.1 (31.9) | 69.7 (25.0) | 6.8 (1.4) |
| Living with partner | 319 | 21.3 (5.6) | 13.2 (1.4) | 153.7 (29.9) | 80.1 (25.0) | 6.7 (1.3) |
| p | <0.001 | 0.02 | <0.001 | <0.001 | 0.41 | |
| Sleep medication | ||||||
| Not using any medication | 459 | 20.5 (5.3) | 13.5 (1.2) | 148.9 (31.6) | 76.2 (24.8) | 6.6 (1.1) |
| Using on 1 or more days/week | 135 | 19.7 (6.2) | 13.7 (1.4) | 142.7 (30.1) | 71.6 (27.3) | 6.5 (1.2) |
| p | 0.16 | 0.13 | 0.04 | 0.06 | 0.36 | |
Abbreviations: BMI, body mass index; ENMO, The Euclidean norm minus 1 g with negative numbers rounded to zero; n, number; PA, physical activity. Body mass index was calculated as weight in kilograms divided by height in meters squared. Categories were defined as normal weight: 18.5 < 25 kg/m2, overweight: 25 < 30 kg/m2 and obese: ≥ 30 kg/m2.
Results are obtained from t-tests for determinants with two categories and analysis of variance (ANOVA) for determinants with 3 or more categories. Data are mean (SD).
Total N varies due to variation in the amount of missing data for different covariates.
Table 2. Objectively assessed physical activity subcomponents and sedentary time in men (n=582), according to characteristics of the study population.
| n | Acceleration (mg/day) | Sedentary time (h/day) | Light PA (min/day) | Moderate-vigorous PA (min/day) | Sleep time (accelerometer) (h/day) | |
|---|---|---|---|---|---|---|
| Total | 582 | 19.3 (5.2) | 13.8 (1.6) | 140.5 (31.1) | 71.5 (24.5) | 6.6 (1.4) |
| Age-group | ||||||
| 70-74 | 201 | 20.2 (5.3) | 13.8 (1.5) | 140.2 (30.2) | 76.0 (25.1) | 6.5 (1.3) |
| 75-79 | 203 | 20.0 (4.9) | 13.5 (1.7) | 144.2 (30.3) | 74.8 (23.3) | 6.8 (1.6) |
| 80-84 | 130 | 18.2 (5.0) | 13.9 (1.4) | 137.2 (32.0) | 65.6 (22.8) | 6.6 (1.3) |
| ≥85 | 48 | 16.0 (4.6) | 14.2 (1.6) | 134.6 (34.5) | 54.5 (21.6) | 6.5 (1.4) |
| p | <0.001 | 0.01 | 0.11 | <0.001 | 0.10 | |
| Education | ||||||
| Primary education | 22 | 17.2 (4.3) | 13.7 (1.4) | 133.3 (32.7) | 61.8 (19.5) | 6.9 (1.6) |
| Lower education | 146 | 19.3 (5.0) | 13.8 (1.5) | 140.6 (28.7) | 71.0 (24.3) | 6.6 (1.4) |
| Intermediate education | 224 | 19.1 (5.2) | 13.7 (1.7) | 139.9 (32.3) | 71.0 (24.7) | 6.6 (1.5) |
| Higher education | 180 | 19.8 (5.4) | 13.9 (1.6) | 141.7 (31.7) | 73.2 (25.1) | 6.5 (1.3) |
| p | 0.16 | 0.81 | 0.68 | 0.22 | 0.38 | |
| Season | ||||||
| Spring | 140 | 18.4 (5.0) | 13.9 (1.6) | 136.3 (28.0) | 67.7 (23.7) | 6.6 (1.5) |
| Summer | 64 | 20.7 (5.6) | 13.1 (1.9) | 143.9 (32.8) | 77.1 (26.9) | 7.0 (1.8) |
| Autumn | 163 | 19.7 (5.3) | 13.8 (1.6) | 142.4 (31.8) | 72.8 (24.9) | 6.5 (1.5) |
| Winter | 213 | 19.4 (5.0) | 13.9 (1.3) | 140.7 (31.9) | 71.4 (23.9) | 6.5 (1.2) |
| p | 0.02 | 0.01 | 0.27 | 0.07 | 0.06 | |
| BMI | ||||||
| Normal weight | 167 | 20.6 (5.7) | 13.5 (1.6) | 146.8 (31.3) | 77.3 (26.9) | 6.6 (1.3) |
| Overweight | 298 | 19.4 (4.8) | 13.7 (1.5) | 140.7 (29.7) | 71.8 (22.4) | 6.7 (1.4) |
| Obese | 117 | 17.5 (4.9) | 14.3 (1.8) | 130.6 (32.0) | 62.4 (23.8) | 6.4 (1.7) |
| p | <0.001 | <0.001 | <0.001 | <0.001 | 0.16 | |
| Smoking | ||||||
| Non smoker | 127 | 19.4 (5.2) | 13.8 (1.5) | 139.6 (27.4) | 72.0 (24.2) | 6.6 (1.4) |
| Former smoker | 425 | 19.4 (5.2) | 13.7 (1.6) | 141.4 (31.7) | 71.8 (24.5) | 6.6 (1.4) |
| Current smoker | 28 | 17.4 (5.5) | 13.8 (1.6) | 129.5 (36.9) | 62.0 (25.4) | 6.8 (1.4) |
| p | 0.13 | 0.82 | 0.14 | 0.12 | 0.75 | |
| Alcohol consumption | ||||||
| Never drinks alcohol | 66 | 19.7 (6.2) | 13.7 (1.8) | 145.2 (31.2) | 72.4 (30.1) | 6.6 (1.5) |
| Drinks 1-4 times per month | 128 | 18.7 (4.9) | 13.9 (1.7) | 134.6 (30.8) | 68.9 (23.1) | 6.6 (1.5) |
| Drinks 2-4 times per week | 387 | 19.5 (5.1) | 13.7 (1.5) | 141.7 (31.0) | 72.1 (24.0) | 6.6 (1.4) |
| p | 0.27 | 0.64 | 0.04 | 0.41 | 0.94 | |
| Functional capacity | ||||||
| Not disabled | 302 | 20.6 (5.0) | 13.6 (1.5) | 145.3 (29.7) | 77.5 (23.7) | 6.6 (1.3) |
| Disabled | 87 | 18.0 (5.2) | 13.8 (1.6) | 137.2 (32.5) | 65.4 (23.5) | 6.8 (1.4) |
| Severely disabled | 192 | 18.0 (5.1) | 14.0 (1.7) | 134.5 (31.6) | 64.6 (23.9) | 6.6 (1.6) |
| p | <0.001 | 0.07 | <0.001 | <0.001 | 0.49 | |
| Prevalent CVD, DM or cancer | ||||||
| Not present | 232 | 20.5 (5.1) | 13.7 (1.6) | 145.3 (29.0) | 76.8 (22.9) | 6.6 (1.4) |
| Present | 350 | 18.5 (5.1) | 13.8 (1.6) | 137.2 (32.0) | 67.9 (25.0) | 6.6 (1.4) |
| p | <0.001 | 0.16 | 0.002 | <0.001 | 0.53 | |
| Marital status | ||||||
| Living alone | 100 | 18.5 (5.5) | 13.8 (1.7) | 138.6 (32.1) | 66.7 (26.0) | 6.6 (1.5) |
| Living with partner | 481 | 19.5 (5.1) | 13.8 (1.6) | 140.9 (30.9) | 72.4 (24.1) | 6.6 (1.4) |
| p | 0.08 | 0.70 | 0.51 | 0.03 | 0.28 | |
| Sleep medication | ||||||
| Not using | 504 | 19.3 (5.2) | 13.9 (1.4) | 140.3 (31.2) | 71.4 (24.5) | 6.4 (1.1) |
| Using | 53 | 19.7 (4.8) | 13.9 (1.6) | 144.9 (28.2) | 74 (22.4) | 6.4 (1.3) |
| p | 0.62 | 0.70 | 0.30 | 0.45 | 0.75 | |
Abbreviations: BMI, body mass index; ENMO, The Euclidean norm minus 1 g with negative numbers rounded to zero; n, number; PA, physical activity. Body mass index was calculated as weight in kilograms divided by height in meters squared. Categories were defined as normal weight: 18.5 < 25 kg/m2, overweight: 25 < 30 kg/m2 and obese: ≥ 30 kg/m2.
Results are obtained from t-tests for determinants with two categories and analysis of variance (ANOVA) for determinants with 3 or more categories. Data are mean (SD).
Total N varies due to variation in the amount of missing data for different covariates.
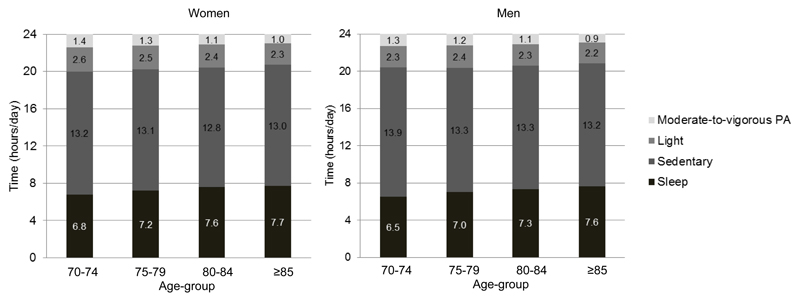
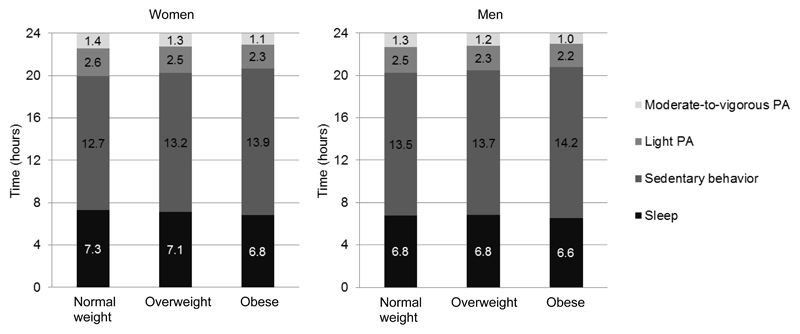
Table 1 (women) and Table 2 (men) show the results from the univariate analyses (ANOVA and t-test), and show that PA levels decreased across higher strata of age and BMI and with worsening health in both men and women. None of the variables was associated with sleep duration in these analyses. The distribution of the respective activity levels across age-groups and BMI categories is visually presented in Figure 4 and 5.
Figure 4.
Distribution of activity across the 24-hour period in men and women, according to age-group
Abbreviations: PA, physical activity
Figure 5.
Distribution of activity across the 24-hour period in men and women, according to normal weight, overweight and obesity
Abbreviations: PA, physical activity.
Body mass index was calculated as weight in kilograms divided by height in meters squared. Categories were defined as normal weight: 18.5 < 25 kg/m2, overweight: 25 < 30 kg/m2 and obese: ≥ 30 kg/m2.
The average time spent in each activity level was adjusted for age.
Table 3 (women) and Table 4 (men) show the results from the linear regression analyses with mutual adjustment for all demographic and health factors. The explained variance by the determinants was highest for moderate-to-vigorous PA in men (16.6%) and women (22.2%). Factors significantly associated with total PA (expressed in mg) and light and moderate-to-vigorous PA were age, BMI, functional capacity and prevalent chronic disease. Older participants, those with higher BMI and those with chronic disease or disability were less physically active. Moreover, in women, living with a partner was associated with significant higher levels of total PA and light and moderate-to-vigorous PA and lower time spent sedentary. Sedentary time increased across higher strata of age and BMI and was higher in those with chronic disease (women). Regarding sleep duration, obese men spent more hours sleeping than normal weight men (Table 4) and women spent slightly less time sleeping in the summer, compared to spring (Table 3).
Table 3. The association between activity measures and demographic and health factors in women (n=577); results from linear regression analyses.
| Acceleration (mg/day) | Sedentary time (h/day) | Light PA (min/day) | Moderate-vigorous PA (min/day) | Sleep time (accelerometer) (h/day) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | n | β ± SE | p | β ± SE | p | β ± SE | p | β ± SE | p | β ± SE | p |
| Age-group | |||||||||||
| 70-74 | 187 | Referent | Referent | Referent | Referent | Referent | |||||
| 75-79 | 201 | -1.51 ± 0.52 | 0.003 | 0.06 ± 0.13 | 0.61 | -1.78 ± 3.07 | 0.56 | -7.28 ± 2.35 | 0.002 | 0.04 ± 0.12 | 0.71 |
| 80-84 | 124 | -2.61 ± 0.61 | <0.001 | 0.13 ± 0.15 | 0.39 | -3.94 ± 3.63 | 0.28 | -13.14 ± 2.78 | <0.001 | 0.08 ± 0.14 | 0.57 |
| ≥85 | 65 | -3.81 ± 0.80 | <0.001 | 0.51 ± 0.20 | 0.01 | -10.13 ± 4.76 | 0.03 | -19.88 ± 3.65 | <0.001 | -0.04 ± 0.18 | 0.81 |
| Education | |||||||||||
| Primary education | 39 | Referent | Referent | Referent | Referent | Referent | |||||
| Lower education | 313 | -0.49 ± 0.87 | 0.58 | -0.14 ± 0.22 | 0.52 | 1.31 ± 5.18 | 0.80 | -2.36 ± 3.97 | 0.55 | 0.11 ± 0.19 | 0.58 |
| Intermediate education | 154 | -0.25 ± 0.91 | 0.79 | -0.06 ± 0.23 | 0.80 | -0.18 ± 5.41 | 0.97 | -2.52 ± 4.15 | 0.54 | 0.07 ± 0.20 | 0.74 |
| Higher education | 71 | 0.25 ± 1.03 | 0.81 | -0.10 ± 0.26 | 0.69 | 8.75 ± 6.15 | 0.16 | 2.22 ± 4.71 | 0.64 | -0.08 ± 0.23 | 0.71 |
| Season | |||||||||||
| Spring | 142 | Referent | Referent | Referent | Referent | Referent | |||||
| Summer | 63 | 1.48 ± 0.75 | 0.05 | 0.30 ± 0.19 | 0.11 | 2.89 ± 4.47 | 0.52 | 4.66 ± 3.43 | 0.17 | -0.40 ± 0.17 | 0.02 |
| Autumn | 203 | 0.58 ± 0.54 | 0.28 | -0.02 ± 0.13 | 0.85 | 3.17 ± 3.20 | 0.32 | 1.84 ± 2.46 | 0.45 | -0.04 ± 0.12 | 0.75 |
| Winter | 169 | 0.38 ± 0.56 | 0.50 | 0.05 ± 0.14 | 0.74 | 3.13 ± 3.35 | 0.35 | 1.53 ± 2.57 | 0.55 | -0.10 ± 0.13 | 0.44 |
| BMI | |||||||||||
| Normal weight | 164 | Referent | Referent | Referent | Referent | Referent | |||||
| Overweight | 246 | -2.06 ± 0.50 | <0.001 | 0.45 ± 0.12 | <0.001 | -9.29 ± 2.97 | 0.002 | -8.70 ± 2.28 | <0.001 | -0.10 ± 0.11 | 0.38 |
| Obese | 167 | -3.87 ± 0.57 | <0.001 | 0.90 ± 0.14 | <0.001 | -19.05 ± 3.36 | <0.001 | -16.79 ± 2.58 | <0.001 | -0.24 ± 0.13 | 0.06 |
| Smoking | |||||||||||
| Non smoker | 261 | Referent | Referent | Referent | Referent | Referent | |||||
| Former smoker | 283 | -0.35 ± 0.43 | 0.42 | 0.19 ± 0.11 | 0.08 | -2.76 ± 2.57 | 0.28 | -1.35 ± 1.97 | 0.49 | -0.12 ± 0.10 | 0.22 |
| Current smoker | 33 | -1.97 ± 0.94 | 0.04 | 0.41 ± 0.23 | 0.08 | -9.04 ± 5.58 | 0.11 | -8.51 ± 4.28 | 0.05 | -0.08 ± 0.21 | 0.70 |
| Alcohol consumption | |||||||||||
| Never drinks alcohol | 117 | Referent | Referent | Referent | Referent | Referent | |||||
| Drinks 1-4 times per month | 204 | 0.50 ± 0.58 | 0.39 | -0.05 ± 0.14 | 0.71 | 0.15 ± 3.42 | 0.96 | 2.43 ± 2.62 | 0.35 | 0.04 ± 0.13 | 0.74 |
| Drinks 2-4 times per week | 256 | 0.78 ± 0.56 | 0.16 | 0.11 ± 0.14 | 0.43 | 3.22 ± 3.33 | 0.33 | 3.26 ± 2.55 | 0.20 | -0.17 ± 0.13 | 0.17 |
| Functional capacity | |||||||||||
| Not disabled | 223 | Referent | Referent | Referent | Referent | Referent | |||||
| Disabled | 123 | 0.04 ± 0.56 | 0.94 | -0.06 ± 0.14 | 0.69 | 1.54 ± 3.36 | 0.65 | -0.33 ± 2.57 | 0.90 | 0.00 ± 0.13 | 1.00 |
| Severely disabled | 231 | -0.93 ± 0.50 | 0.06 | 0.06 ± 0.12 | 0.64 | -3.43 ± 2.97 | 0.25 | -5.42 ± 2.28 | 0.02 | 0.04 ± 0.11 | 0.75 |
| Prevalent CVD, DM or cancer | |||||||||||
| Not present | 308 | Referent | Referent | Referent | Referent | Referent | |||||
| Present | 269 | -1.65 ± 0.41 | <0.001 | 0.35 ± 0.10 | <0.001 | -6.77 ± 2.47 | 0.01 | -6.82 ± 1.89 | <0.001 | -0.13 ± 0.09 | 0.18 |
| Marital status | |||||||||||
| Living alone | 288 | Referent | Referent | Referent | Referent | Referent | |||||
| Living with partner | 289 | 1.47 ± 0.44 | <0.001 | -0.18 ± 0.11 | 0.10 | 9.66 ± 2.61 | <0.001 | 6.62 ± 2.00 | <0.001 | -0.10 ± 0.10 | 0.32 |
| Sleep medication | |||||||||||
| Not using any medication | 444 | Referent | Referent | Referent | Referent | Referent | |||||
| Using on 1 or more days/week | 133 | -0.50 ± 0.49 | 0.30 | 0.15 ± 0.12 | 0.21 | -5.15 ± 2.90 | 0.08 | -3.43 ± 2.23 | 0.12 | -0.10 ± 0.11 | 0.37 |
Abbreviations: BMI, body mass index; CVD, cardiovascular disease; DM, diabetes mellitus; n, number; PA, physical activity; SE, standard error. Body mass index was calculated as weight in kilograms divided by height in meters squared. Categories were defined as normal weight: 18.5 < 25 kg/m2, overweight: 25 < 30 kg/m2 and obese: ≥ 30 kg/m2
The explained variance in the models, according the adjusted R-squared, was 21.0%, 11.4%, 13.2%, 22.2% and 0.8% for acceleration, sedentary behavior, light physical activity, moderate-to-vigorous physical activity and sleep, respectively.
Total N is reduced due to variation in the amount of missing data for different covariates.
The multivariate linear regression analysis was adjusted for all variables included in the table.
Table 4. The association between physical activity measures and demographic and health factors in men (n=543); results from linear regression analyses.
| Acceleration (mg/day) | Sedentary time (h/day) | Light PA (min/day) | Moderate-vigorous PA (min/day) | Sleep time (accelerometer) (h/day) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | n | β ± SE | p | β ± SE | p | β ± SE | p | β ± SE | p | β ± SE | p |
| Age-group | |||||||||||
| 70-74 | 191 | Referent | Referent | Referent | Referent | Referent | |||||
| 75-79 | 181 | -0.16 ± 0.51 | 0.76 | -0.13 ± 0.14 | 0.37 | 4.70 ± 3.22 | 0.14 | -0.85 ± 2.39 | 0.72 | 0.09 ± 0.12 | 0.49 |
| 80-84 | 127 | -1.49 ± 0.58 | 0.01 | 0.10 ± 0.16 | 0.55 | -1.1 ± 3.69 | 0.77 | -7.99 ± 2.74 | 0.004 | 0.02 ± 0.14 | 0.90 |
| ≥85 | 44 | -3.77 ± 0.88 | <0.001 | 0.64 ± 0.25 | 0.01 | -5.23 ± 5.57 | 0.35 | -19.77 ± 4.14 | <0.001 | -0.18 ± 0.21 | 0.40 |
| Education | |||||||||||
| Primary education | 21 | Referent | Referent | Referent | Referent | Referent | |||||
| Lower education | 138 | 1.46 ± 1.13 | 0.20 | 0.04 ± 0.32 | 0.91 | 4.70 ± 7.12 | 0.51 | 6.59 ± 5.29 | 0.21 | -0.18 ± 0.27 | 0.51 |
| Intermediate education | 212 | 0.96 ± 1.10 | 0.38 | 0.22 ± 0.31 | 0.48 | 1.87 ± 6.95 | 0.79 | 4.73 ± 5.16 | 0.36 | -0.28 ± 0.27 | 0.30 |
| Higher education | 172 | 0.90 ± 1.12 | 0.42 | 0.41 ± 0.31 | 0.19 | 1.21 ± 7.09 | 0.86 | 3.80 ± 5.26 | 0.47 | -0.42 ± 0.27 | 0.12 |
| Season | |||||||||||
| Spring | 129 | Referent | Referent | Referent | Referent | Referent | |||||
| Summer | 63 | 1.30 ± 0.79 | 0.10 | -0.13 ± 0.22 | 0.55 | 3.74 ± 5.00 | 0.45 | 4.07 ± 3.72 | 0.27 | -0.06 ± 0.19 | 0.77 |
| Autumn | 203 | 1.23 ± 0.57 | 0.03 | -0.05 ± 0.16 | 0.73 | 7.20 ± 3.58 | 0.04 | 4.47 ± 2.66 | 0.09 | -0.17 ± 0.14 | 0.22 |
| Winter | 169 | 0.58 ± 0.55 | 0.29 | -0.04 ± 0.15 | 0.82 | 3.11 ± 3.48 | 0.37 | 1.49 ± 2.58 | 0.56 | -0.06 ± 0.13 | 0.68 |
| BMI | |||||||||||
| Normal weight | 156 | Referent | Referent | Referent | Referent | Referent | |||||
| Overweight | 279 | -1.26 ± 0.49 | 0.01 | 0.26 ± 0.14 | 0.06 | -5.10 ± 3.11 | 0.10 | -5.52 ± 2.31 | 0.02 | -0.11 ± 0.12 | 0.38 |
| Obese | 108 | -2.76 ± 0.63 | <0.001 | 0.96 ± 0.18 | <0.001 | -13.51 ± 4.01 | <0.001 | -13.12 ± 2.98 | <0.001 | -0.54 ± 0.15 | 0.001 |
| Smoking | |||||||||||
| Non smoker | 119 | Referent | Referent | Referent | Referent | Referent | |||||
| Former smoker | 397 | 0.67 ± 0.51 | 0.19 | -0.10 ± 0.14 | 0.51 | 4.05 ± 3.24 | 0.21 | 3.00 ± 2.41 | 0.21 | -0.03 ± 0.12 | 0.79 |
| Current smoker | 27 | -2.71 ± 1.05 | 0.01 | 0.13 ± 0.30 | 0.67 | -13.34 ± 6.67 | 0.05 | -13.13 ± 4.95 | 0.01 | 0.20 ± 0.26 | 0.44 |
| Alcohol consumption | |||||||||||
| Never drinks alcohol | 60 | Referent | Referent | Referent | Referent | Referent | |||||
| Drinks 1-4 times per month | 121 | -1.04 ± 0.77 | 0.18 | 0.08 ± 0.22 | 0.70 | -11.33 ± 4.87 | 0.02 | -4.19 ± 3.62 | 0.25 | 0.23 ± 0.19 | 0.23 |
| Drinks 2-4 times per week | 362 | -0.47 ± 0.68 | 0.49 | -0.07 ± 0.19 | 0.71 | -4.66 ± 4.29 | 0.28 | -1.84 ± 3.18 | 0.56 | 0.25 ± 0.16 | 0.13 |
| Functional capacity | |||||||||||
| Not disabled | 286 | Referent | Referent | Referent | Referent | Referent | |||||
| Disabled | 83 | -1.95 ± 0.61 | <0.001 | 0.13 ± 0.17 | 0.44 | -5.82 ± 3.87 | 0.13 | -9.61 ± 2.88 | <0.001 | 0.14 ± 0.15 | 0.34 |
| Severely disabled | 174 | -2.11 ± 0.47 | <0.001 | 0.37 ± 0.13 | 0.01 | -9.54 ± 3.00 | <0.001 | -10.81 ± 2.23 | <0.001 | -0.04 ± 0.12 | 0.76 |
| Prevalent CVD, DM or cancer | |||||||||||
| Not present | 215 | Referent | Referent | Referent | Referent | Referent | |||||
| Present | 328 | -1.28 ± 0.44 | 0.004 | -0.03 ± 0.12 | 0.81 | -6.69 ± 2.77 | 0.02 | -4.91 ± 2.06 | 0.02 | 0.20 ± 0.11 | 0.06 |
| Marital status | |||||||||||
| Living alone | 91 | Referent | Referent | Referent | Referent | Referent | |||||
| Living with partner | 452 | 0.08 ± 0.58 | 0.89 | 0.06 ± 0.16 | 0.72 | 0.02 ± 3.68 | 1.00 | 1.25 ± 2.73 | 0.65 | -0.05 ± 0.14 | 0.70 |
| Sleep medication | |||||||||||
| Not using any medication | 490 | Referent | Referent | Referent | Referent | Referent | |||||
| Using on 1 or more days/week | 53 | 0.34 ± 0.70 | 0.62 | -0.04 ± 0.20 | 0.86 | 4.55 ± 4.41 | 0.30 | 2.57 ± 3.27 | 0.43 | -0.09 ± 0.17 | 0.61 |
Abbreviations: BMI, body mass index; CVD, cardiovascular disease; DM, diabetes mellitus; n, number; PA, physical activity; SE, standard error. Body mass index was calculated as weight in kilograms divided by height in meters squared. Categories were defined as normal weight: 18.5 < 25 kg/m2, overweight: 25 < 30 kg/m2 and obese: ≥ 30 kg/m2.
The multivariate linear regression analysis was adjusted for all variables included in the table. Total N is reduced due to variation in the amount of missing data for different covariates.
The explained variance in the models, according the adjusted R-squared, was 15.7%, 6.9%, 6.9%, 16.6% and 1.5% for acceleration, sedentary behavior, light physical activity, moderate-to-vigorous physical activity and sleep, respectively.
In sensitivity analyses split by age, we observed that in the oldest old (i.e. 80 years and older), there were less gender differences and there was no effect of season, compared to those younger than 80 years (Supplementary Table 7-8). Moreover, in the oldest old, functional capacity and marital status were not associated with sedentary behavior or PA, whereas these were associated with activity in participants younger than 80 years. In the analyses split by BMI, we observed that marital status was not associated with activity in participants with a BMI < 27 kg/m2, whereas it was associated with activity in those with higher BMI (Supplementary Table 9-10). In contrast, smoking status was a determinant of activity in those with BMI< 27 kg/m2 and not in participants with ≥ 27 kg/m2.
Discussion
The aim of this study was to provide a comprehensive description of objectively measured activity in old participants from the Rotterdam Study, by socio-demographic characteristics and other health-related variables. We show that sedentary behavior and light and moderate-to-vigorous PA vary by age-group, sex, BMI, prevalence of disease and functional capacity, whereas we observed no clear differences between categories for sleep duration. Overall, men and women spent 13.8 (79.5%) hours and 13.3 (78.2%) hours of their waking time in sedentary behavior, respectively, and around 70 minutes of their waking time (7-8%) in moderate-to-vigorous PA.
When examining differences by age-groups, we found the lowest PA volume in the oldest age-group (aged ≥ 85 years), which is in accordance with literature indicating that PA declines with increasing age.9,10,12,16,19 In men and women, the time spent in light, moderate and vigorous intensity PA declined with age, whereas the absolute time spent sedentary increased with age. Considering that sleep time was constant across age groups, the increase in sedentary behavior was at the extent of both light and moderate-to-vigorous PA. Since literature indicates that total sleep time decreases with age,38 it is possible that the algorithm used to detect sleep overestimated sleep time, if participants lay motionless, but awake, in bed at night.36 If this is the case, older adults were actually sleeping inefficiently during their time in bed. A better understanding of the distribution of activity across the 24-hour time span might benefit public health interventions. Since daily PA might enhance sleep quality,39,40 replacing sedentary behavior with light or moderate activity might improve PA levels and sleep quality simultaneously. Future studies are required to identify activities in which elderly adults can engage in to improve PA levels.
In our study, men and women spent around 70 minutes per day in moderate-to vigorous PA. In similar study populations in Iceland,9 Norway16 and the United Kingdom12 these numbers were up to 15, 36 and 23 minutes per day, respectively. Comparisons are hampered by the different study population characteristics (e.g. age), use of different devices and anatomical placements, the use of counts per minute and the stratification into sedentary time and light, moderate and vigorous activity by different cut-offs. Consequently, we cannot be sure whether participants in our study were really more active, or that the different estimates are the result of the different cut-points. Because the Ommoord district in which most participants live is a safe neighborhood with opportunity to walk and cycle in a safe manner, it could be expected that the participants from our study were indeed more active in comparison to other studies.
In our study, we found higher levels of acceleration in women compared to men, in all age-groups. This is in contrast with most studies in older adults,9,12,14,41 but in agreement with two others.11,19 In addition, in the total population, we found that women spent more time in moderate PA than men. An explanation for the higher activity in women compared to men might be traditional gender roles, in which women are more involved in household activities than men. Chen et al. indicated that the discrepancies between the studies might be related to cultural lifestyle differences.11 Nevertheless, they performed their study among Japanese elderly and our participants come from a Western population, in which men often are reported to be more active than women.9,12,14,41 The results from the current study might be explained by the fact that men more often had chronic disease than women (60.1% vs. 46.5%). However, women were more often disabled and obese than men, both variables associated with lower PA levels. Another explanation for the difference might be related to the fact that men reported significantly more cycling than women (47.3% in men versus 33.6% in women) in the current study. A wrist-worn accelerometer is known to underestimate activities performed with the lower extremities.42 Future studies are needed to examine whether the observed results reflect a true difference between sexes. Moreover, more research is needed to be able to identify lower body activities with wrist-worn accelerometers.
Important correlates of sedentary behavior and PA were BMI, age, functional capacity and the prevalence of chronic disease in both sexes. Obese individuals had a lower acceleration and lower levels of light and moderate-to-vigorous PA, compared to their normal weight counterparts. These results are in agreement with existing data.9–12,14 Moreover, in women, living with a partner was associated with more time spent in light and moderate-to-vigorous PA. In sensitivity analyses split by age and BMI, we showed that living with a partner was also associated with activity in participants younger than 80 years and in those with BMI ≥ 27 kg/m2. These results suggest opportunities for focused intervention, targeting specifically those with higher BMI and age, as well as those suffering from a chronic condition or disability. The fact that women living with a partner were more active than those living alone, might indicate that women are more likely to engage in PA socially. Public health programs might provide opportunities for specific sub-groups with the lowest levels of PA, including organized PA programs. Furthermore, in sensitivity analyses in the oldest old, we observed no gender differences for PA levels. However, in these participants, being obese was associated with larger decreases in light and moderate-to-vigorous PA than in participants younger than 80 years. Possibly, the additional weight is more of a burden in the oldest old. This stresses the importance of a healthy weight, even in old age.
This study has several strengths. It is one of the first studies providing a detailed description of the full intensity distribution of PA in this age-range of participants over the 24-hour period. Additionally, since the accelerometer device was waterproof and was worn day and night, we could collect comprehensive information of all activity performed. However, some limitations also have to be acknowledged. Using raw accelerometer derived data to describe activity is relatively new and therefore the cut-off points to define intensity of behavior have not been firmly established. Moreover, as in other studies using objectively measured PA, not all PA can be accurately captured. For example, cycling or other activities mostly performed with the legs will be underestimated.42 Additionally, since no method exists for differentiating between the postural allocations of sitting, standing and lying down from triaxial wrist acceleration signals in this population, we were unable to distinguish socializing from driving. Furthermore, we used an algorithm to define sleep, in which we defined sleep as an absence of change in arm angle greater than 5 degrees for 5 minutes or more.36 Using another sleep definition may influence estimated sleep time and hence the sedentary time observed in our participants. Although van Hees et al36 made extensive effort to validate their algorithm in the Whitehall II Study using polysomnography, future studies are needed to optimize the used algorithm. Another limitation is that we did not have up-to-date information on cancer, cardiovascular disease and diabetes. Therefore, some residual confounding might be present and might have resulted in bias towards the null for those comparisons. Additionally, participants that agreed to participate were less often disabled and more often men. This might affect the generalizability towards the total population of older adults. Finally, participants attending these visits of the Rotterdam Study might have a better health-status than the general population, an issue often occurring in cohort studies.
In conclusion, in this population based cohort study of elderly individuals, men spent significantly more time in sedentary behavior and less time in light and moderate-to-vigorous PA compared to women. However, whereas this difference was significant, it was of small numeric value, indicating that both men and women spent a high proportion of their day sedentary. Furthermore, our findings suggest that sedentary behavior and light and moderate-to-vigorous PA patterns differ according to age, BMI, functional capacity and presence of disease, whereas sleep duration did not differ according demographic factors and health behaviors. Replacing sedentary behavior with light PA would be a good starting point for those with the lowest level of PA. Older adults, those with high BMI and worse health could benefit from targeted interventions to increase PA.
Supplementary Material
Acknowledgments
All authors declare that there are no competing interests. This work was supported by a Netherlands Organization for Scientific Research grant (017.106.370) awarded to HT. The Rotterdam Study is funded by Erasmus Medical Center and Erasmus University Rotterdam; Netherlands Organization for the Health Research and Development; the Research Institute for Diseases in the Elderly; the Ministry of Education, Culture and Science; the Ministry for Health, Welfare and Sports; and the European Commission. O.H.F. works in ErasmusAGE, a center for aging research across the life course funded by Nestlé Nutrition (Nestec Ltd.), Metagenics Inc., and AXA. The work of SB was supported by UK Medical Research Council [MC_UU_12015/3].
We thank the staff of the Rotterdam Study and the participating general practitioners and pharmacists. We also thank Tom White (University of Cambridge, UK), primary author of the open-access PAMPRO software.
Footnotes
Author contributions
CMK, OHF and FJAvR had the original idea for the study. CMK and FJAvR participated in the analyses and interpretation of the data and drafted the article. OHF, JS, MC, HT and SB revised the manuscript critically for important intellectual content. All authors gave final approval of the version to be published.
Conflict of interests
There are no conflict of interests to declare.
References
- 1.Gulsvik AK, Thelle DS, Samuelsen SO, Myrstad M, Mowe M, Wyller TB. Ageing, physical activity and mortality--a 42-year follow-up study. Int J Epidemiol. 2012;41(2):521–30. doi: 10.1093/ije/dyr205. [DOI] [PubMed] [Google Scholar]
- 2.Chief Medical Officer. At least five a week: evidence on the impact of physical activity and its relationship to health. London: Department of Health; 2004. [Google Scholar]
- 3.Keysor JJ. Does late-life physical activity or exercise prevent or minimize disablement? A critical review of the scientific evidence. Am J Prev Med. 2003;25(3 Suppl 2):129–36. doi: 10.1016/s0749-3797(03)00176-4. [DOI] [PubMed] [Google Scholar]
- 4.Ainsworth BE. How do I measure physical activity in my patients? Questionnaires and objective methods. Br J Sports Med. 2009;43(1):6–9. doi: 10.1136/bjsm.2008.052449. [DOI] [PubMed] [Google Scholar]
- 5.Schmid D, Ricci C, Leitzmann MF. Associations of Objectively Assessed Physical Activity and Sedentary Time with All-Cause Mortality in US Adults: The NHANES Study. PLoS One. 2015;10(3):e0119591. doi: 10.1371/journal.pone.0119591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ensrud KE, Blackwell TL, Cauley JA, Dam TT, Cawthon PM, Schousboe JT, Barrett-Connor E, Stone KL, Bauer DC, Shikany JM, Mackey DC, et al. Objective measures of activity level and mortality in older men. J Am Geriatr Soc. 2014;62(11):2079–87. doi: 10.1111/jgs.13101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rait G, Fletcher A, Smeeth L, Brayne C, Stirling S, Nunes M, Breeze E, Ng ES, Bulpitt CJ, Jones D, Tulloch AJ. Prevalence of cognitive impairment: results from the MRC trial of assessment and management of older people in the community. Age Ageing. 2005;34(3):242–8. doi: 10.1093/ageing/afi039. [DOI] [PubMed] [Google Scholar]
- 8.Lee IM, Shiroma EJ. Using Accelerometers to Measure Physical Activity in Large-Scale Epidemiologic Studies: Issues and Challenges. British journal of sports medicine. 2014;48(3):197–201. doi: 10.1136/bjsports-2013-093154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Arnardottir NY, Koster A, Van Domelen DR, Brychta RJ, Caserotti P, Eiriksdottir G, Sverrisdottir JE, Launer LJ, Gudnason V, Johannsson E, Harris TB, et al. Objective measurements of daily physical activity patterns and sedentary behaviour in older adults: Age, Gene/Environment Susceptibility-Reykjavik Study. Age Ageing. 2013;42(2):222–9. doi: 10.1093/ageing/afs160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Berkemeyer K, Wijndaele K, White T, Cooper AJ, Luben R, Westgate K, Griffin SJ, Khaw KT, Wareham NJ, Brage S. The descriptive epidemiology of accelerometer-measured physical activity in older adults. Int J Behav Nutr Phys Act. 2016;13(1):2. doi: 10.1186/s12966-015-0316-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chen T, Narazaki K, Honda T, Chen S, Haeuchi Y, Nofuji YY, Matsuo E, Kumagai S. Tri-Axial Accelerometer-Determined Daily Physical Activity and Sedentary Behavior of Suburban Community-Dwelling Older Japanese Adults. J Sports Sci Med. 2015;14(3):507–14. [PMC free article] [PubMed] [Google Scholar]
- 12.Davis MG, Fox KR, Hillsdon M, Sharp DJ, Coulson JC, Thompson JL. Objectively measured physical activity in a diverse sample of older urban UK adults. Med Sci Sports Exerc. 2011;43(4):647–54. doi: 10.1249/MSS.0b013e3181f36196. [DOI] [PubMed] [Google Scholar]
- 13.Evenson KR, Buchner DM, Morland KB. Objective measurement of physical activity and sedentary behavior among US adults aged 60 years or older. Prev Chronic Dis. 2012;9:E26. [PMC free article] [PubMed] [Google Scholar]
- 14.Golubic R, Martin KR, Ekelund U, Hardy R, Kuh D, Wareham N, Cooper R, Brage S, scientific N, data collection t Levels of physical activity among a nationally representative sample of people in early old age: results of objective and self-reported assessments. Int J Behav Nutr Phys Act. 2014;11:58. doi: 10.1186/1479-5868-11-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Innerd P, Catt M, Collerton J, Davies K, Trenell M, Kirkwood TB, Jagger C. A comparison of subjective and objective measures of physical activity from the Newcastle 85+ study. Age Ageing. 2015;44(4):691–4. doi: 10.1093/ageing/afv062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lohne-Seiler H, Hansen BH, Kolle E, Anderssen SA. Accelerometer-determined physical activity and self-reported health in a population of older adults (65-85 years): a cross-sectional study. BMC Public Health. 2014;14:284. doi: 10.1186/1471-2458-14-284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ortlieb S, Dias A, Gorzelniak L, Nowak D, Karrasch S, Peters A, Kuhn KA, Horsch A, Schulz H, Group KS. Exploring patterns of accelerometry-assessed physical activity in elderly people. Int J Behav Nutr Phys Act. 2014;11(1):28. doi: 10.1186/1479-5868-11-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sabia S, van Hees VT, Shipley MJ, Trenell MI, Hagger-Johnson G, Elbaz A, Kivimaki M, Singh-Manoux A. Association between questionnaire- and accelerometer-assessed physical activity: the role of sociodemographic factors. Am J Epidemiol. 2014;179(6):781–90. doi: 10.1093/aje/kwt330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Doherty A, Jackson D, Hammerla N, Plotz T, Olivier P, Granat MH, White T, van Hees VT, Trenell MI, Owen CG, Preece SJ, et al. Large Scale Population Assessment of Physical Activity Using Wrist Worn Accelerometers: The UK Biobank Study. PLoS One. 2017;12(2):e0169649. doi: 10.1371/journal.pone.0169649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.White T, Westgate K, Wareham NJ, Brage S. Estimation of Physical Activity Energy Expenditure during Free-Living from Wrist Accelerometry in UK Adults. PLoS One. 2016;11(12):e0167472. doi: 10.1371/journal.pone.0167472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.van Hees VT, Gorzelniak L, Dean Leon EC, Eder M, Pias M, Taherian S, Ekelund U, Renstrom F, Franks PW, Horsch A, Brage S. Separating movement and gravity components in an acceleration signal and implications for the assessment of human daily physical activity. PLoS One. 2013;8(4):e61691. doi: 10.1371/journal.pone.0061691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.van Hees VT, Renstrom F, Wright A, Gradmark A, Catt M, Chen KY, Lof M, Bluck L, Pomeroy J, Wareham NJ, Ekelund U, et al. Estimation of daily energy expenditure in pregnant and non-pregnant women using a wrist-worn tri-axial accelerometer. PLoS One. 2011;6(7):e22922. doi: 10.1371/journal.pone.0022922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hofman A, Brusselle GG, Darwish Murad S, van Duijn CM, Franco OH, Goedegebure A, Ikram MA, Klaver CC, Nijsten TE, Peeters RP, Stricker BH, et al. The Rotterdam Study: 2016 objectives and design update. Eur J Epidemiol. 2015;30(8):661–708. doi: 10.1007/s10654-015-0082-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hildebrand M, VANH VT, Hansen BH, Ekelund U. Age group comparability of raw accelerometer output from wrist- and hip-worn monitors. Med Sci Sports Exerc. 2014;46(9):1816–24. doi: 10.1249/MSS.0000000000000289. [DOI] [PubMed] [Google Scholar]
- 25.da Silva IC, van Hees VT, Ramires VV, Knuth AG, Bielemann RM, Ekelund U, Brage S, Hallal PC. Physical activity levels in three Brazilian birth cohorts as assessed with raw triaxial wrist accelerometry. Int J Epidemiol. 2014;43(6):1959–68. doi: 10.1093/ije/dyu203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Crombaghs M, de Min E, van Hees GS. The first absolute gravity measurements in The Netherlands: Period 1991-1999. 2002 [Google Scholar]
- 27.van Hees VT, Fang Z, Langford J, Assah F, Mohammad A, da Silva IC, Trenell MI, White T, Wareham NJ, Brage S. Autocalibration of accelerometer data for free-living physical activity assessment using local gravity and temperature: an evaluation on four continents. J Appl Physiol (1985) 2014;117(7):738–44. doi: 10.1152/japplphysiol.00421.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.White T. Physical Activity Monitor Processing. [accessed December 1st 2016];2016 https://github.com/Thomite/pampro.
- 29.Brage S, Westgate K, Wijndaele K, Godinho J, Griffin S, Wareham N. Evaluation Of A Method For Minimizing Diurnal Information Bias In Objective Sensor Data. International Conference on Ambulatory Monitoring of Physical Activity and Movement; Amherst, Massachusetts, The United States. 2013. [Google Scholar]
- 30.Kavousi M, Elias-Smale S, Rutten JH, Leening MJ, Vliegenthart R, Verwoert GC, Krestin GP, Oudkerk M, de Maat MP, Leebeek FW, Mattace-Raso FU, et al. Evaluation of newer risk markers for coronary heart disease risk classification: a cohort study. Ann Intern Med. 2012;156(6):438–44. doi: 10.7326/0003-4819-156-6-201203200-00006. [DOI] [PubMed] [Google Scholar]
- 31.Koller MT, Leening MJ, Wolbers M, Steyerberg EW, Hunink MG, Schoop R, Hofman A, Bucher HC, Psaty BM, Lloyd-Jones DM, Witteman JC. Development and validation of a coronary risk prediction model for older U.S. and European persons in the Cardiovascular Health Study and the Rotterdam Study. Ann Intern Med. 2012;157(6):389–97. doi: 10.7326/0003-4819-157-6-201209180-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Xiao Q, Keadle SK, Hollenbeck AR, Matthews CE. Sleep duration and total and cause-specific mortality in a large US cohort: interrelationships with physical activity, sedentary behavior, and body mass index. Am J Epidemiol. 2014;180(10):997–1006. doi: 10.1093/aje/kwu222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fries JF, Spitz P, Kraines RG, Holman HR. Measurement of patient outcome in arthritis. Arthritis Rheum. 1980;23(2):137–45. doi: 10.1002/art.1780230202. [DOI] [PubMed] [Google Scholar]
- 34.Odding E, Valkenburg HA, Stam HJ, Hofman A. Determinants of locomotor disability in people aged 55 years and over: the Rotterdam Study. Eur J Epidemiol. 2001;17(11):1033–41. doi: 10.1023/a:1020006909285. [DOI] [PubMed] [Google Scholar]
- 35.Ockene IS, Chiriboga DE, Stanek EJ, 3rd, Harmatz MG, Nicolosi R, Saperia G, Well AD, Freedson P, Merriam PA, Reed G, Ma Y, et al. Seasonal variation in serum cholesterol levels: treatment implications and possible mechanisms. Archives of internal medicine. 2004;164(8):863–70. doi: 10.1001/archinte.164.8.863. [DOI] [PubMed] [Google Scholar]
- 36.van Hees VT, Sabia S, Anderson KN, Denton SJ, Oliver J, Catt M, Abell JG, Kivimaki M, Trenell MI, Singh-Manoux A. A Novel, Open Access Method to Assess Sleep Duration Using a Wrist-Worn Accelerometer. PLoS One. 2015;10(11):e0142533. doi: 10.1371/journal.pone.0142533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.StataCorp. Stata Statistical Software: Release 14. College Station, TX: StataCorp LP; 2015. [Google Scholar]
- 38.Cooke JR, Ancoli-Israel S. Normal and abnormal sleep in the elderly. Handb Clin Neurol. 2011;98:653–65. doi: 10.1016/B978-0-444-52006-7.00041-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Garfield V, Llewellyn CH, Kumari M. The relationship between physical activity, sleep duration and depressive symptoms in older adults: The English Longitudinal Study of Ageing (ELSA) Prev Med Rep. 2016;4:512–6. doi: 10.1016/j.pmedr.2016.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Youngstedt SD. Effects of exercise on sleep. Clin Sports Med. 2005;24(2):355–65. doi: 10.1016/j.csm.2004.12.003. xi. [DOI] [PubMed] [Google Scholar]
- 41.Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181–8. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 42.Chen KY, Bassett DR., Jr The technology of accelerometry-based activity monitors: current and future. Med Sci Sports Exerc. 2005;37(11 Suppl):S490–500. doi: 10.1249/01.mss.0000185571.49104.82. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.